User login
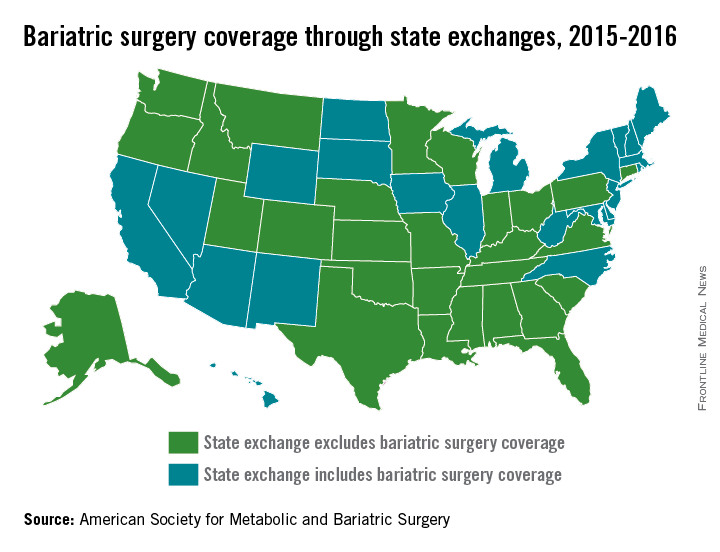
The majority of state exchanges are not covering bariatric surgery for 2015-2016, but one state is set to make the switch to limited coverage in 2017, according to the American Society for Metabolic and Bariatric Surgery.
There are currently 28 states with benchmark plans on their insurance exchanges that exclude coverage of bariatric surgery, but Colorado will add coverage for bariatric surgery when it replaces the state’s current essential health benefits benchmark for 2017, the ASMBS reported.
Among the states not covering bariatric surgery are Texas, Florida, Ohio, and Pennsylvania. Those that do have coverage on their state exchanges include California, New York, and Illinois, the ASMBS noted. Four states – California, New Mexico, Massachusetts, and Michigan – and the District of Columbia have benchmark plans that cover weight-loss programs.
The ASMBS said that “state health exchange plans continue to utilize blanket exclusions for weight loss programs or any obesity management services [even though] such blanket exclusions for these services are contradictory to ACA-mandated coverage for [U.S. Preventive Services Task Force] recommended preventive services.”
Meanwhile, the society added, the U.S. Department of Health & Human Services “continues to sidestep its oversight authority in favor of letting states work out these issues – instructing advocates to contact state insurance commissioners for any kind of recourse.”
The majority of state exchanges are not covering bariatric surgery for 2015-2016, but one state is set to make the switch to limited coverage in 2017, according to the American Society for Metabolic and Bariatric Surgery.
There are currently 28 states with benchmark plans on their insurance exchanges that exclude coverage of bariatric surgery, but Colorado will add coverage for bariatric surgery when it replaces the state’s current essential health benefits benchmark for 2017, the ASMBS reported.
Among the states not covering bariatric surgery are Texas, Florida, Ohio, and Pennsylvania. Those that do have coverage on their state exchanges include California, New York, and Illinois, the ASMBS noted. Four states – California, New Mexico, Massachusetts, and Michigan – and the District of Columbia have benchmark plans that cover weight-loss programs.
The ASMBS said that “state health exchange plans continue to utilize blanket exclusions for weight loss programs or any obesity management services [even though] such blanket exclusions for these services are contradictory to ACA-mandated coverage for [U.S. Preventive Services Task Force] recommended preventive services.”
Meanwhile, the society added, the U.S. Department of Health & Human Services “continues to sidestep its oversight authority in favor of letting states work out these issues – instructing advocates to contact state insurance commissioners for any kind of recourse.”
The majority of state exchanges are not covering bariatric surgery for 2015-2016, but one state is set to make the switch to limited coverage in 2017, according to the American Society for Metabolic and Bariatric Surgery.
There are currently 28 states with benchmark plans on their insurance exchanges that exclude coverage of bariatric surgery, but Colorado will add coverage for bariatric surgery when it replaces the state’s current essential health benefits benchmark for 2017, the ASMBS reported.
Among the states not covering bariatric surgery are Texas, Florida, Ohio, and Pennsylvania. Those that do have coverage on their state exchanges include California, New York, and Illinois, the ASMBS noted. Four states – California, New Mexico, Massachusetts, and Michigan – and the District of Columbia have benchmark plans that cover weight-loss programs.
The ASMBS said that “state health exchange plans continue to utilize blanket exclusions for weight loss programs or any obesity management services [even though] such blanket exclusions for these services are contradictory to ACA-mandated coverage for [U.S. Preventive Services Task Force] recommended preventive services.”
Meanwhile, the society added, the U.S. Department of Health & Human Services “continues to sidestep its oversight authority in favor of letting states work out these issues – instructing advocates to contact state insurance commissioners for any kind of recourse.”