User login
The emergency department locum tenens staff recruiter was persuasive. “It’s a quiet little ER where you can study and sleep.” I was board certified in internal medicine and had trained in a busy urban emergency department. This was just the spot to make a little folding money and study for my mock dermatology boards, I thought.
And so, on a Saturday night in rural Texas, after grinding rust out of a pipe fitter’s eye and stitching up two brawlers from the local biker bar, I was faced with treating a comatose kid brought in after a car crash. He had not been wearing a seat belt, and his car had rolled over on his head.
I was way over my skill level, but I was lucky. I was able to stabilize him and, after several long hours, I got him on an emergency helicopter into Dallas.
But the experience changed me. I realized I did not know enough to deal with this case on my own. After making it through that night in the ED, I never put myself in that position again.
I now knew what I did not know.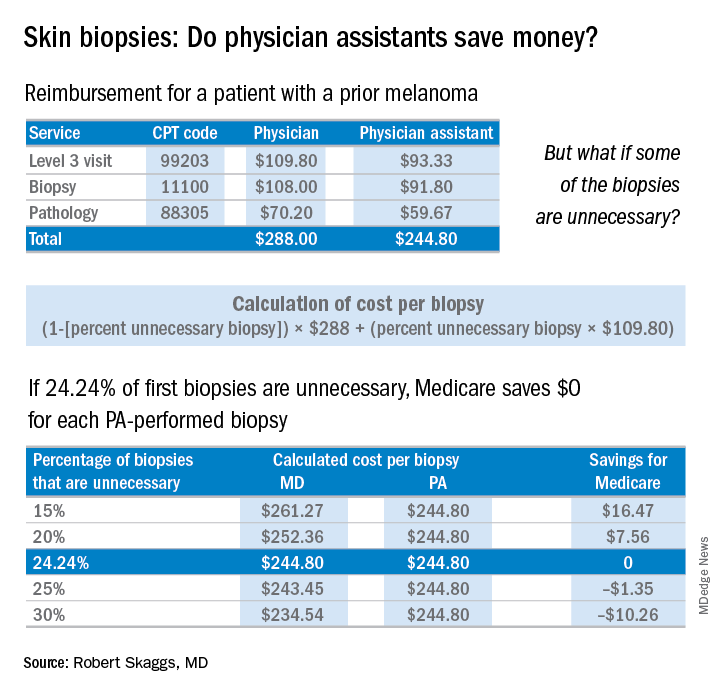
The finding that jumped out to me, though, was that patients screened by a PA were significantly less likely to be diagnosed with melanoma in situ, the stage when melanoma is 100% curable. Yet, those patients screened by PAs underwent a lot more skin biopsies – 36% more skin biopsies per melanoma in situ diagnosed, compared with patients of dermatologists. Interestingly, in the health care system studied, any PA with a question about a patient can ask an attending dermatologist to see the patient. Did that factor account for the diagnostic comparability for nonmelanoma skin cancer and invasive melanoma? Did the PAs not ask for help on the missed melanomas in situ? If so, I believe this may be a situation of PAs not knowing what they didn’t know.
Now a knowledgeable friend of mine thinks this study is biased because 17% more patients with prior melanomas were seen by a dermatologist rather than by a PA. While it’s true that patients with prior melanomas are more likely to develop new melanomas, the counterargument is that the bar for a biopsy in a patient with a prior melanoma is much lower. Patients with a history of melanoma should have more skin biopsies, but the dermatologists in this study still took many fewer biopsies to diagnose melanomas in situ.
Why do these findings matter for patients and for the health care system?
PAs billed independently for 12% of skin biopsies (including lip, ear, ear canal, vulva, penis, and eyelid) in Medicare Fee for Service in 2016. Skin biopsies paid for by Medicare have been increasing at a very rapid rate, about twice as fast as the rate reflected in the current skin cancer epidemic.
Every skin biopsy results in a pathology charge, for which Medicare pays about $70. A level 3 new patient visit pays $110. If PAs bill independently, they are paid at 85% of the fee schedule, which often is touted as a great savings. Therefore, if only 24.2% of skin biopsies by PAs were unnecessary, even at a reduced 85% reimbursement, it costs Medicare more than having these visits and biopsies provided by a dermatologist. The cost savings decrease even more with additional skin biopsies, because they pay so little ($33 for a doctor, $28 for a PA), yet the pathology charge is unchanged.
There are other costs beyond monetary ones from unnecessary skin biopsies: scarring, follow-up procedures for uncertain diagnoses such as mild dysplastic nevi, ambiguous results, and emotional angst to patients.
If the results of this large study are to be believed, many melanomas in situ are going to be missed if PAs perform unsupervised skin cancer screenings. This is not a tenable proposition, ethically or legally. Dermatologists and PAs need to work together to ensure this does not happen.
An estimated 2,520 dermatology PAs were practicing in the United States in 2016, based on membership data from the Society of Dermatology PAs (SDPA), according to a research letter published last year (J Am Acad Dermatol. 2017 Jun;76[6]:1200-2). The SDPA, as stated in an SDPA position statement published in the winter 2017 newsletter, hopes to gain access to direct billing to public and private insurers, which would include the Centers for Medicare & Medicaid Services, and for PAs to no longer report to other health care professionals.
Many dermatologists, as well as teaching programs, use PAs to perform skin cancer screenings, sometimes unsupervised, which makes diagnostic accuracy critical. The issues at hand are the safety of patients and the accuracy of diagnosis as well as the costs to the health care system. A team effort, which includes direct supervision, is needed to ensure those issues are addressed.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
The emergency department locum tenens staff recruiter was persuasive. “It’s a quiet little ER where you can study and sleep.” I was board certified in internal medicine and had trained in a busy urban emergency department. This was just the spot to make a little folding money and study for my mock dermatology boards, I thought.
And so, on a Saturday night in rural Texas, after grinding rust out of a pipe fitter’s eye and stitching up two brawlers from the local biker bar, I was faced with treating a comatose kid brought in after a car crash. He had not been wearing a seat belt, and his car had rolled over on his head.
I was way over my skill level, but I was lucky. I was able to stabilize him and, after several long hours, I got him on an emergency helicopter into Dallas.
But the experience changed me. I realized I did not know enough to deal with this case on my own. After making it through that night in the ED, I never put myself in that position again.
I now knew what I did not know.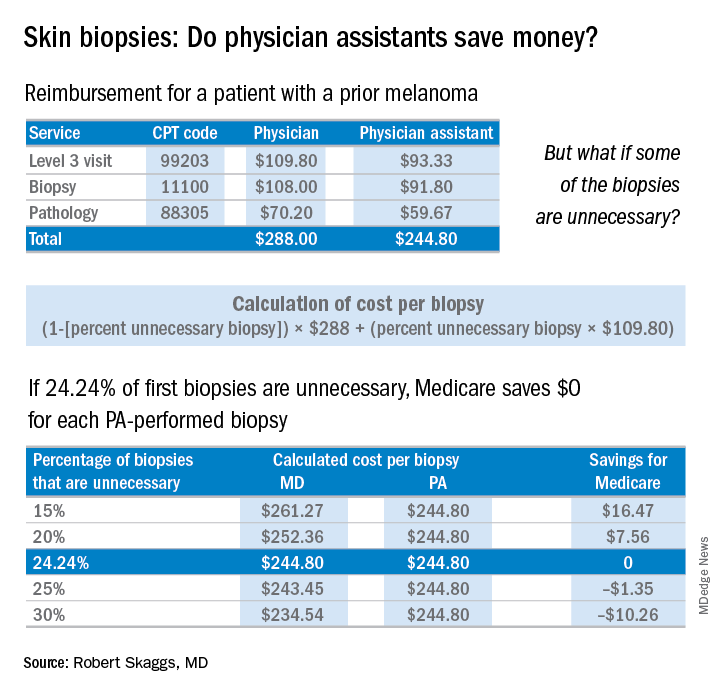
The finding that jumped out to me, though, was that patients screened by a PA were significantly less likely to be diagnosed with melanoma in situ, the stage when melanoma is 100% curable. Yet, those patients screened by PAs underwent a lot more skin biopsies – 36% more skin biopsies per melanoma in situ diagnosed, compared with patients of dermatologists. Interestingly, in the health care system studied, any PA with a question about a patient can ask an attending dermatologist to see the patient. Did that factor account for the diagnostic comparability for nonmelanoma skin cancer and invasive melanoma? Did the PAs not ask for help on the missed melanomas in situ? If so, I believe this may be a situation of PAs not knowing what they didn’t know.
Now a knowledgeable friend of mine thinks this study is biased because 17% more patients with prior melanomas were seen by a dermatologist rather than by a PA. While it’s true that patients with prior melanomas are more likely to develop new melanomas, the counterargument is that the bar for a biopsy in a patient with a prior melanoma is much lower. Patients with a history of melanoma should have more skin biopsies, but the dermatologists in this study still took many fewer biopsies to diagnose melanomas in situ.
Why do these findings matter for patients and for the health care system?
PAs billed independently for 12% of skin biopsies (including lip, ear, ear canal, vulva, penis, and eyelid) in Medicare Fee for Service in 2016. Skin biopsies paid for by Medicare have been increasing at a very rapid rate, about twice as fast as the rate reflected in the current skin cancer epidemic.
Every skin biopsy results in a pathology charge, for which Medicare pays about $70. A level 3 new patient visit pays $110. If PAs bill independently, they are paid at 85% of the fee schedule, which often is touted as a great savings. Therefore, if only 24.2% of skin biopsies by PAs were unnecessary, even at a reduced 85% reimbursement, it costs Medicare more than having these visits and biopsies provided by a dermatologist. The cost savings decrease even more with additional skin biopsies, because they pay so little ($33 for a doctor, $28 for a PA), yet the pathology charge is unchanged.
There are other costs beyond monetary ones from unnecessary skin biopsies: scarring, follow-up procedures for uncertain diagnoses such as mild dysplastic nevi, ambiguous results, and emotional angst to patients.
If the results of this large study are to be believed, many melanomas in situ are going to be missed if PAs perform unsupervised skin cancer screenings. This is not a tenable proposition, ethically or legally. Dermatologists and PAs need to work together to ensure this does not happen.
An estimated 2,520 dermatology PAs were practicing in the United States in 2016, based on membership data from the Society of Dermatology PAs (SDPA), according to a research letter published last year (J Am Acad Dermatol. 2017 Jun;76[6]:1200-2). The SDPA, as stated in an SDPA position statement published in the winter 2017 newsletter, hopes to gain access to direct billing to public and private insurers, which would include the Centers for Medicare & Medicaid Services, and for PAs to no longer report to other health care professionals.
Many dermatologists, as well as teaching programs, use PAs to perform skin cancer screenings, sometimes unsupervised, which makes diagnostic accuracy critical. The issues at hand are the safety of patients and the accuracy of diagnosis as well as the costs to the health care system. A team effort, which includes direct supervision, is needed to ensure those issues are addressed.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
The emergency department locum tenens staff recruiter was persuasive. “It’s a quiet little ER where you can study and sleep.” I was board certified in internal medicine and had trained in a busy urban emergency department. This was just the spot to make a little folding money and study for my mock dermatology boards, I thought.
And so, on a Saturday night in rural Texas, after grinding rust out of a pipe fitter’s eye and stitching up two brawlers from the local biker bar, I was faced with treating a comatose kid brought in after a car crash. He had not been wearing a seat belt, and his car had rolled over on his head.
I was way over my skill level, but I was lucky. I was able to stabilize him and, after several long hours, I got him on an emergency helicopter into Dallas.
But the experience changed me. I realized I did not know enough to deal with this case on my own. After making it through that night in the ED, I never put myself in that position again.
I now knew what I did not know.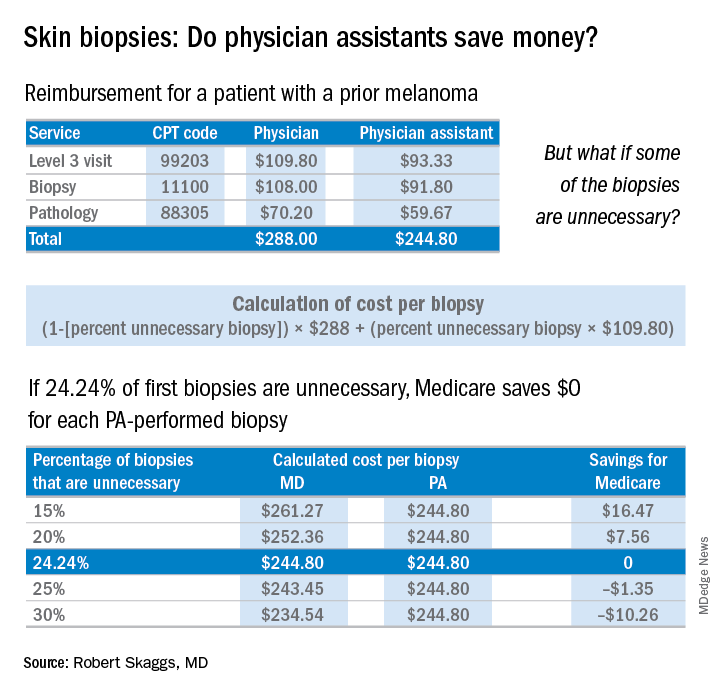
The finding that jumped out to me, though, was that patients screened by a PA were significantly less likely to be diagnosed with melanoma in situ, the stage when melanoma is 100% curable. Yet, those patients screened by PAs underwent a lot more skin biopsies – 36% more skin biopsies per melanoma in situ diagnosed, compared with patients of dermatologists. Interestingly, in the health care system studied, any PA with a question about a patient can ask an attending dermatologist to see the patient. Did that factor account for the diagnostic comparability for nonmelanoma skin cancer and invasive melanoma? Did the PAs not ask for help on the missed melanomas in situ? If so, I believe this may be a situation of PAs not knowing what they didn’t know.
Now a knowledgeable friend of mine thinks this study is biased because 17% more patients with prior melanomas were seen by a dermatologist rather than by a PA. While it’s true that patients with prior melanomas are more likely to develop new melanomas, the counterargument is that the bar for a biopsy in a patient with a prior melanoma is much lower. Patients with a history of melanoma should have more skin biopsies, but the dermatologists in this study still took many fewer biopsies to diagnose melanomas in situ.
Why do these findings matter for patients and for the health care system?
PAs billed independently for 12% of skin biopsies (including lip, ear, ear canal, vulva, penis, and eyelid) in Medicare Fee for Service in 2016. Skin biopsies paid for by Medicare have been increasing at a very rapid rate, about twice as fast as the rate reflected in the current skin cancer epidemic.
Every skin biopsy results in a pathology charge, for which Medicare pays about $70. A level 3 new patient visit pays $110. If PAs bill independently, they are paid at 85% of the fee schedule, which often is touted as a great savings. Therefore, if only 24.2% of skin biopsies by PAs were unnecessary, even at a reduced 85% reimbursement, it costs Medicare more than having these visits and biopsies provided by a dermatologist. The cost savings decrease even more with additional skin biopsies, because they pay so little ($33 for a doctor, $28 for a PA), yet the pathology charge is unchanged.
There are other costs beyond monetary ones from unnecessary skin biopsies: scarring, follow-up procedures for uncertain diagnoses such as mild dysplastic nevi, ambiguous results, and emotional angst to patients.
If the results of this large study are to be believed, many melanomas in situ are going to be missed if PAs perform unsupervised skin cancer screenings. This is not a tenable proposition, ethically or legally. Dermatologists and PAs need to work together to ensure this does not happen.
An estimated 2,520 dermatology PAs were practicing in the United States in 2016, based on membership data from the Society of Dermatology PAs (SDPA), according to a research letter published last year (J Am Acad Dermatol. 2017 Jun;76[6]:1200-2). The SDPA, as stated in an SDPA position statement published in the winter 2017 newsletter, hopes to gain access to direct billing to public and private insurers, which would include the Centers for Medicare & Medicaid Services, and for PAs to no longer report to other health care professionals.
Many dermatologists, as well as teaching programs, use PAs to perform skin cancer screenings, sometimes unsupervised, which makes diagnostic accuracy critical. The issues at hand are the safety of patients and the accuracy of diagnosis as well as the costs to the health care system. A team effort, which includes direct supervision, is needed to ensure those issues are addressed.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
