User login
ORLANDO – Moderate aerobic exercise and a more intensive regimen proved equally effective in reducing intrahepatic triglyceride content in centrally obese patients with nonalcoholic fatty liver disease in a 12-month randomized, controlled trial.
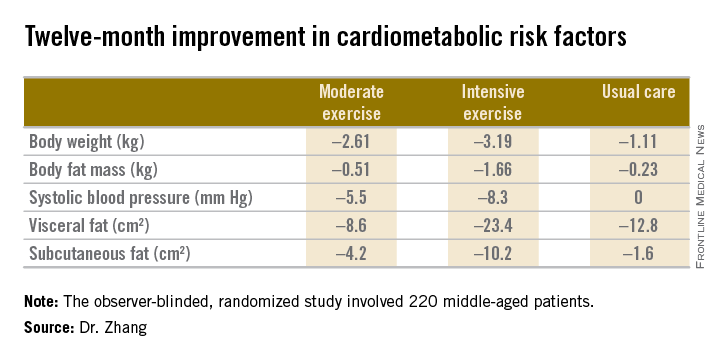
However, the more intensive exercise program had the edge in terms of favorable impact on metabolic risk factors. While both exercise prescriptions reduced body weight and blood pressure to a similar extent over the course of 12 months, the intensive-exercise group showed bigger reductions in body fat mass, visceral fat, and subcutaneous fat (see graphic), Dr. Hui-Jie Zhang of Xiamen (China) University said at the American Heart Association scientific sessions.
The observer-blinded study included 220 middle-age Chinese patients with central obesity and confirmed nonalcoholic fatty liver disease (NAFLD), a common risk factor for cardiovascular disease. They were randomized to three groups: a moderate exercise program that consisted of brisk walking for 150 minutes per week for 12 months; an intensive exercise regimen involving 30 minutes of treadmill running at 65%-80% of maximum oxygen consumption 5 days per week for 6 months, followed by 6 months of brisk walking on the same schedule as the moderate exercise group; or a usual-care control group that received lifestyle counseling.
The primary endpoint was change in intrahepatic triglyceride content as measured by proton magnetic resonance spectroscopy at 12 months. It was reduced from baseline by 6.45% in the intensive exercise group and similarly by 6.19% with moderate exercise, both significantly greater effects than the 2.85% decrease in the control group.
Dr. Zhang reported having no financial conflicts of interest regarding this study.
ORLANDO – Moderate aerobic exercise and a more intensive regimen proved equally effective in reducing intrahepatic triglyceride content in centrally obese patients with nonalcoholic fatty liver disease in a 12-month randomized, controlled trial.
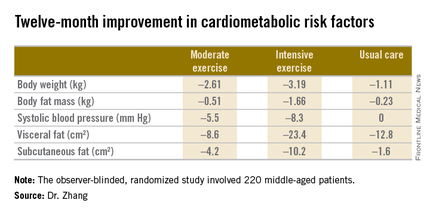
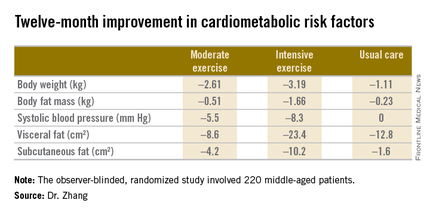
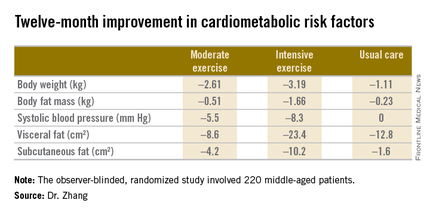
However, the more intensive exercise program had the edge in terms of favorable impact on metabolic risk factors. While both exercise prescriptions reduced body weight and blood pressure to a similar extent over the course of 12 months, the intensive-exercise group showed bigger reductions in body fat mass, visceral fat, and subcutaneous fat (see graphic), Dr. Hui-Jie Zhang of Xiamen (China) University said at the American Heart Association scientific sessions.
The observer-blinded study included 220 middle-age Chinese patients with central obesity and confirmed nonalcoholic fatty liver disease (NAFLD), a common risk factor for cardiovascular disease. They were randomized to three groups: a moderate exercise program that consisted of brisk walking for 150 minutes per week for 12 months; an intensive exercise regimen involving 30 minutes of treadmill running at 65%-80% of maximum oxygen consumption 5 days per week for 6 months, followed by 6 months of brisk walking on the same schedule as the moderate exercise group; or a usual-care control group that received lifestyle counseling.
The primary endpoint was change in intrahepatic triglyceride content as measured by proton magnetic resonance spectroscopy at 12 months. It was reduced from baseline by 6.45% in the intensive exercise group and similarly by 6.19% with moderate exercise, both significantly greater effects than the 2.85% decrease in the control group.
Dr. Zhang reported having no financial conflicts of interest regarding this study.
ORLANDO – Moderate aerobic exercise and a more intensive regimen proved equally effective in reducing intrahepatic triglyceride content in centrally obese patients with nonalcoholic fatty liver disease in a 12-month randomized, controlled trial.
However, the more intensive exercise program had the edge in terms of favorable impact on metabolic risk factors. While both exercise prescriptions reduced body weight and blood pressure to a similar extent over the course of 12 months, the intensive-exercise group showed bigger reductions in body fat mass, visceral fat, and subcutaneous fat (see graphic), Dr. Hui-Jie Zhang of Xiamen (China) University said at the American Heart Association scientific sessions.
The observer-blinded study included 220 middle-age Chinese patients with central obesity and confirmed nonalcoholic fatty liver disease (NAFLD), a common risk factor for cardiovascular disease. They were randomized to three groups: a moderate exercise program that consisted of brisk walking for 150 minutes per week for 12 months; an intensive exercise regimen involving 30 minutes of treadmill running at 65%-80% of maximum oxygen consumption 5 days per week for 6 months, followed by 6 months of brisk walking on the same schedule as the moderate exercise group; or a usual-care control group that received lifestyle counseling.
The primary endpoint was change in intrahepatic triglyceride content as measured by proton magnetic resonance spectroscopy at 12 months. It was reduced from baseline by 6.45% in the intensive exercise group and similarly by 6.19% with moderate exercise, both significantly greater effects than the 2.85% decrease in the control group.
Dr. Zhang reported having no financial conflicts of interest regarding this study.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point: Moderate and intensive aerobic exercise, done regularly, are equally effective in reducing the intrahepatic triglyceride level in patients with nonalcoholic fatty liver disease.
Major finding: Intrahepatic triglyceride concentration in patients with NAFLD was reduced by a mean of 6.19% after 12 months on a moderate exercise program and 6.45% with a more intensive exercise regimen, compared with 2.85% in usual-care controls.
Data source: A 12-month, observer-blinded randomized trial in which 220 middle-age Chinese patients with NAFLD and central obesity were randomized to a program of moderate aerobic exercise, a more intensive regimen, or a usual-care control group.
Disclosures: The presenter reported having no financial conflicts of interest regarding this study.