User login
In a striking trend, the rate of contralateral prophylactic mastectomy (CPM) has risen by 30% over the last 10 years in the United States.1 Many women undergo CPM because of the fear and anxiety of cancer recurrence and their perceived risk of contralateral breast cancer; however, few women have a medical condition that necessitates removal of the contralateral breast. The medical indications for CPM include having a pathogenic genetic mutation (eg, BRCA1 and BRCA2), a strong family history of breast cancer, or prior mediastina chest radiation.
The actual risk of contralateral breast cancer is much lower than perceived. In women without a genetic mutation, the 10-year risk of contralateral breast cancer is only 3% to 5%.1 Also, CPM does not prevent the development of metastatic disease and offers no survival benefit over breast conservation or unilateral mastectomy.2 Furthermore, compared with unilateral therapeutic mastectomy, the “upgrade” to a CPM carries a 2.7-fold risk of a major surgical complication.3 It is therefore important that patients receive appropriate counseling regarding CPM, and that this counseling include cancer stage at diagnosis, family history and genetic risk, and cancer versus surgical risk (see “Counseling patients on contralateral prophylactic mastectomy” for key points to cover in patient discussions).
Counseling patients on contralateral prophylactic mastectomy
Commonly, patients diagnosed with breast cancer consider having their contralateral healthy breast removed as part of a bilateral mastectomy. They often experience severe anxiety about the cancer coming back and believe that removing both breasts will enable them to live longer. Keep the following key facts in mind when discussing treatment options with breast cancer patients.
Cancer stage at diagnosis. How long a patient lives from the time of her breast cancer diagnosis depends on the stage of the cancer at diagnosis, not the type of surgery performed. A woman with early stage I or stage II breast cancer has an 80% to 90% chance of being cancer free in 5 years.1 The chance of cancer recurring in the bones, liver, or lungs (metastatic breast cancer) will not be changed by removing the healthy breast. The risk of metastatic recurrence can be reduced, however, with chemotherapy and/or with hormone-blocker therapy.
Family history and genetic risk. Few women have a strong family history of breast and/or ovarian and other cancers, and this issue should be addressed with genetic counseling and testing prior to surgery. Those who carry a cancer-causing gene, such as BRCA1 or BRCA2, are at increased risk (40% to 60%) for a second or third breast cancer, especially if they are diagnosed at a young age (<50 years).2,3 In women who have a genetic mutation, removing both breasts and sometimes the ovaries can prevent development of another breast cancer. But this will not prevent spread of the cancer that is already present. Only chemotherapy and hormone blockers can prevent the spread of cancer.
Cancer risk versus surgical risk. For women with no family history of breast cancer, no genetic mutation, and no prior chest wall radiation, the risk of developing a new breast cancer in their other breast is only 3% to 5% every 10 years.3,4 This means that they have a 95% chance of not developing a new breast cancer in their healthy breast. Notably, removing the healthy breast can double the risk of postsurgical complications, including bleeding, infection, and loss of tissue and implant. The mastectomy site will be numb and the skin and nipple areola will not have any function other than cosmetic. Finally, wound complications from surgery could delay the start of important cancer treatment, such as chemotherapy or radiation.
The bottom line. Unless a woman has a strong family history of breast cancer, is diagnosed at a very young age, or has a genetic cancer-causing mutation, removing the contralateral healthy breast is not medically necessary and is not routinely recommended.
References
- Hennigs A, Riedel F, Gondos A, et al. Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer. 2016;16(1):734.
- Graeser MK, Engel C, Rhiem K, et al. Contralateral breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2009;27(35):5887–5992.
- Curtis RE, Ron E, Hankey BF, Hoover RN. New malignancies following breast cancer. In: Curtis RE, Freedman DM, Ron E, et al, eds. New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973-2000. Bethesda, MD: National Cancer Institute. NIH Publ. No. 05-5302. 2006:181–205. http://seer.cancer.gov/archive/publications/mpmono. Accessed September 18, 2016.
- Nichols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–1569.
Women should be made aware that there are alternatives to mastectomy that have similar, or even better, outcomes with improved quality of life. Furthermore, a multi‑disciplinary, team-oriented approach with emphasis on minimally invasive biopsy and better cosmetic outcomes has enhanced quality of care. Knowledge of this team approach and of modern breast cancer treatments is essential for general ObGyns as this understanding improves the overall care and guidance—specifically regarding referral to expert, high-volume breast surgeons—provided to those women most in need.
Expanded treatment options for breast cancer
Advancements in breast surgery, better imaging, and targeted therapies are changing the paradigm of breast cancer treatment.
Image-guided biopsy is key in decision making
When an abnormality is found in the breast, surgical excision of an undiagnosed breast lesion is no longer considered an appropriate first step. Use of image-guided biopsy or minimally invasive core needle biopsy allows for accurate diagnosis of a breast lesion while avoiding a potentially breast deforming and expensive surgical operation. It is always better to go into the operating room (OR) with a diagnosis and do the right operation the first time.
A core needle biopsy, results of which demonstrate a benign lesion, helps avoid breast surgery in women who do not need it. If cancer is diagnosed on biopsy, the extent of disease can be better evaluated and decision making can be more informed, with a multidisciplinary approach used to consider the various options, including genetic counseling, plastic surgery consultation, or neoadjuvant therapy. Some lesions, such as those too close to the skin, chest wall, or an implant, may not be amenable to core needle biopsy and therefore require surgical excision for diagnosis.
Benefits of a multidisciplinary tumor conference
It is important for a multidisciplinary group of cancer specialists to review a patient’s case and discuss the ideal treatment plan prior to surgery. Some breast cancer subtypes (such as human epidermal growth factor receptor 2 [HER2]–overamplified breast cancer and many triple-negative breast cancers) are very sensitive to chemotherapy, and patients with these tumor types may benefit from receiving neoadjuvant chemotherapy prior to surgery. New types of chemotherapy may allow up to 60% of some breast cancers to diminish almost completely, with subsequent improved cosmetic results of breast surgery.4 It may also allow time for genetic counseling and testing prior to surgery. (See “How to code for a multidisciplinary tumor conference” for appropriate coding procedure.)
How to code for a multidisciplinary tumor conference
Melanie Witt, RN, MA
There are two coding choices for team conferences involving physician participation. If the patient and/or family is present, the CPT instruction is to bill a problem E/M service code (99201-99215) based on the time spent during this coordination of care/counseling. Documentation would include details about the conference decisions and implications for care, rather than history or examination.
If the patient is not present, report 99367 (Medical team conference with interdisciplinary team of health care professionals, patient and/or family not present, 30 minutes or more; participation by physician), but note that this code was developed under the assumption that the conference would be performed in a facility setting. Diagnostic coding would be breast cancer.
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
The author reports no financial relationships relevant to this article.
This is an excerpt from a companion coding resource for breast cancer–related procedures by Ms. Witt. To read the companion article, “Coding for breast cancer–related procedures: A how-to guide,” in its entirety, click here.
Image-guided lumpectomy
Advances in breast imaging have led to increased identification of nonpalpable breast cancers. Surgical excision of nonpalpable breast lesions requires image guidance, which can be done using a variety of techniques.
Wire-guided localization (WGL) has been used in practice for the past 40 years. The procedure involves placement of a hooked wire under local anesthesia using either mammographic or ultrasound guidance. This procedure is mostly done in the radiology department on the same day as the surgery and requires that the radiologist coordinate with the OR schedule. Besides scheduling conflicts and delays in surgery, this procedure can be complicated by wires becoming dislodged, transected, or migrated, and limits the surgeon’s ability to cosmetically hide the scar in relation to position of the wire. It is uncomfortable for the patient, who must be transported from the radiology department to the OR with a wire extruding from her breast.
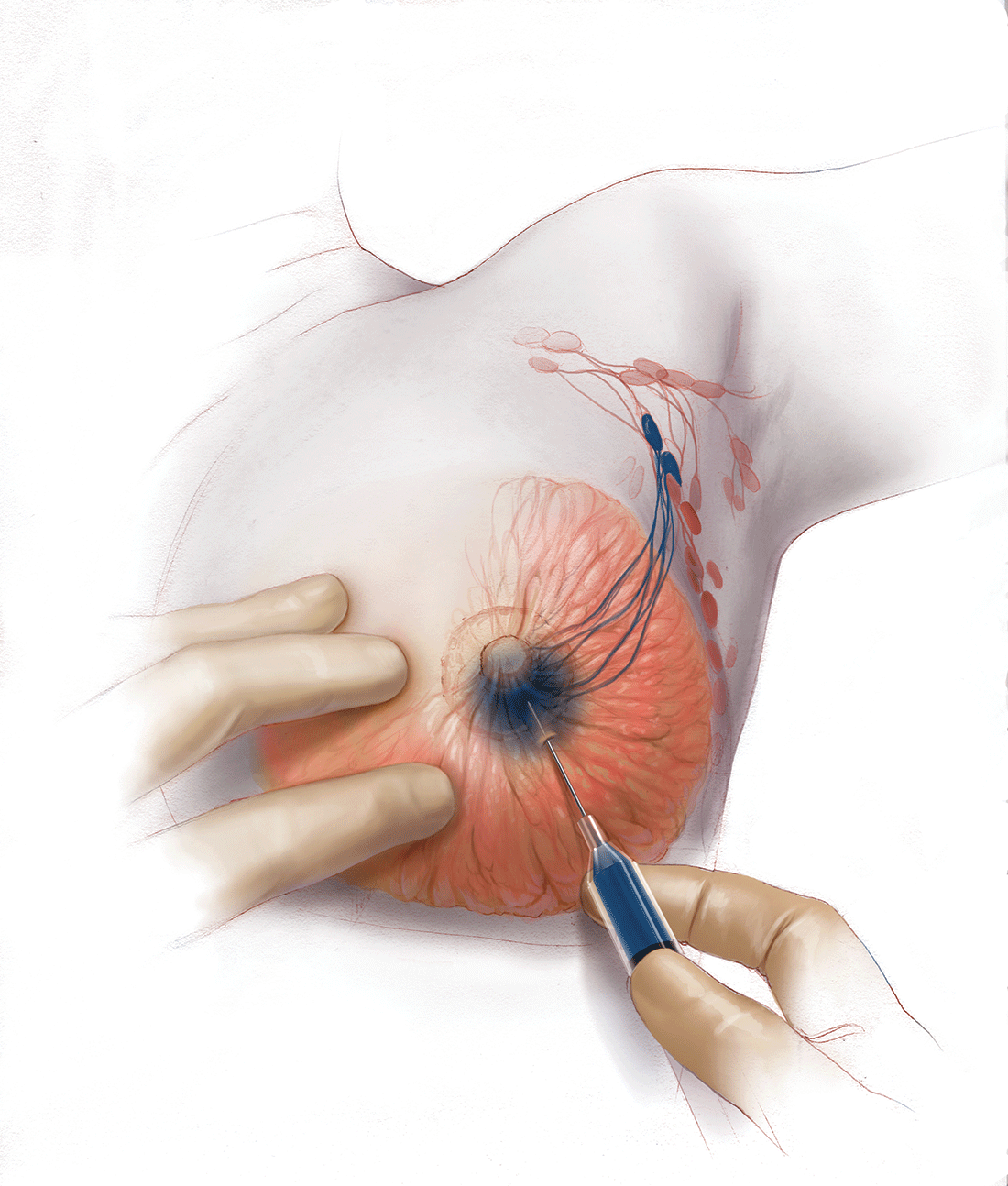
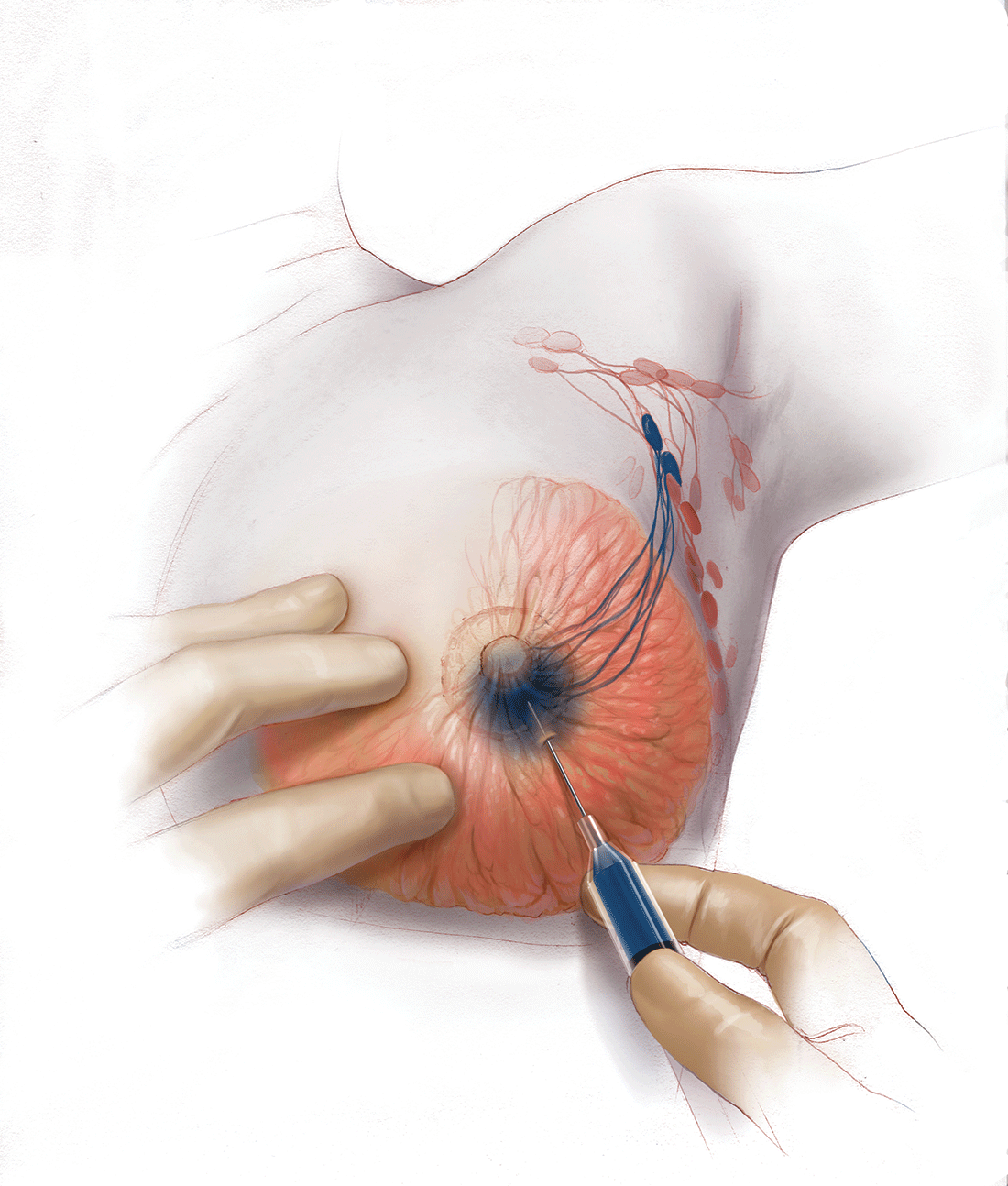
An alternative localization technique is placement of a radioactive source within the tumor, which can then be identified in the OR with a gamma probe.
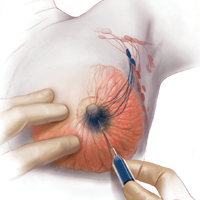
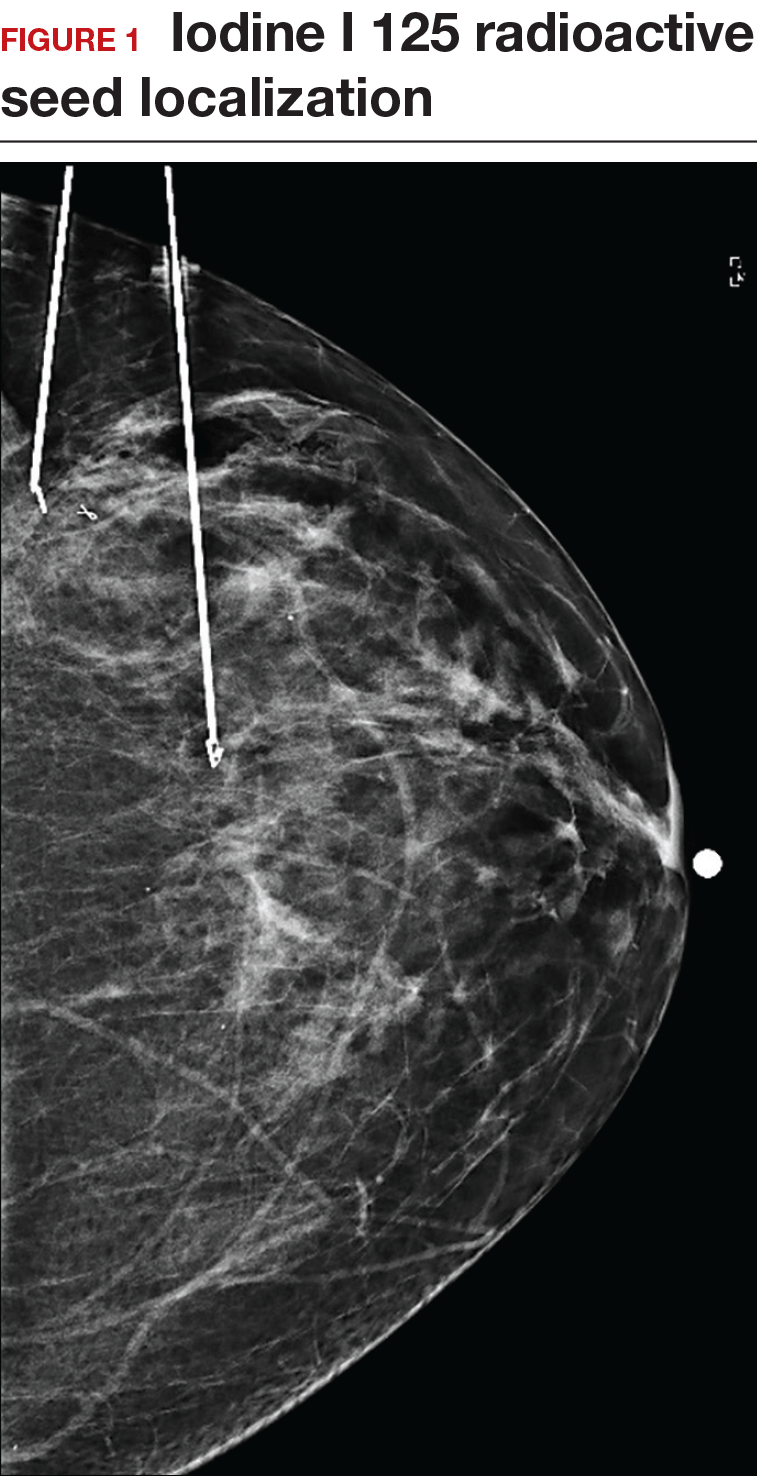
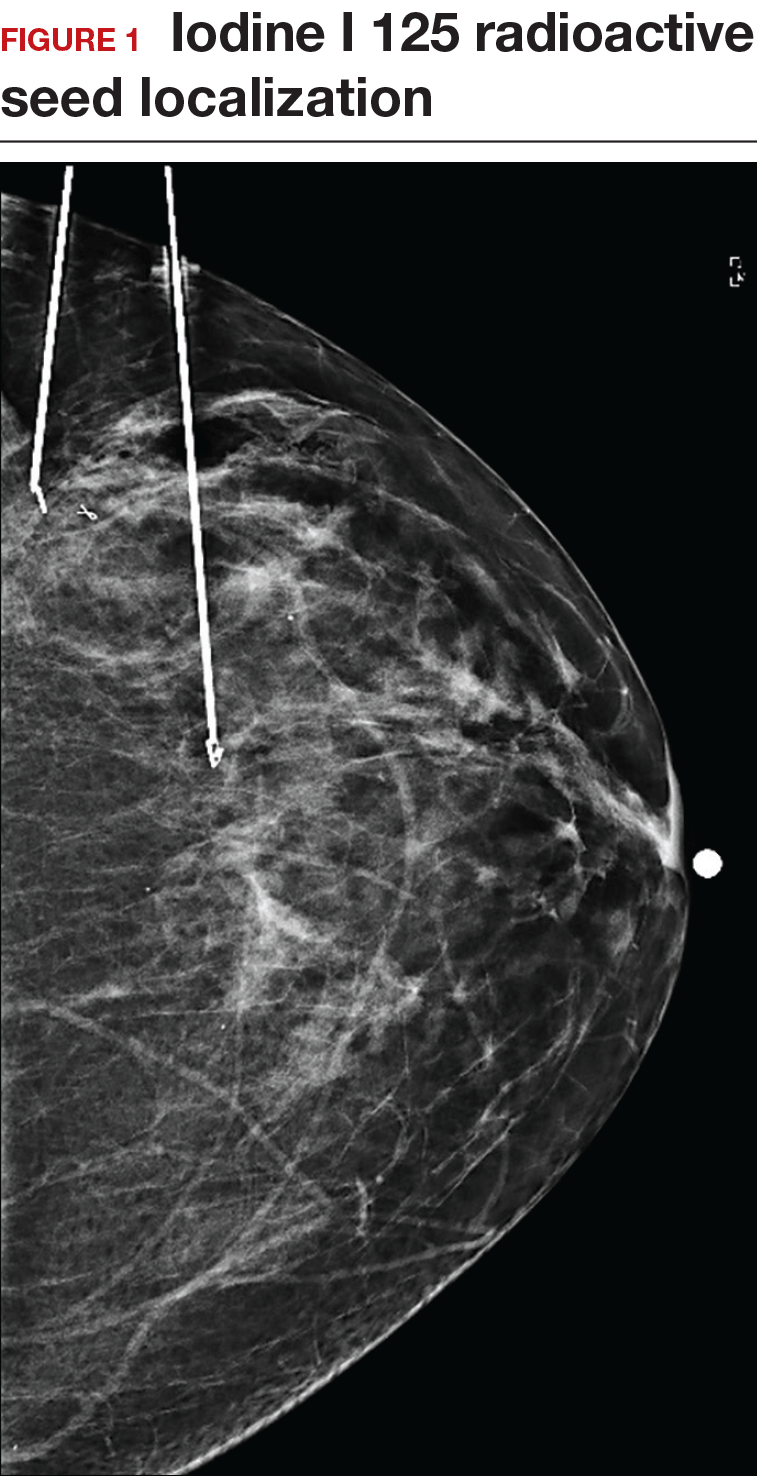
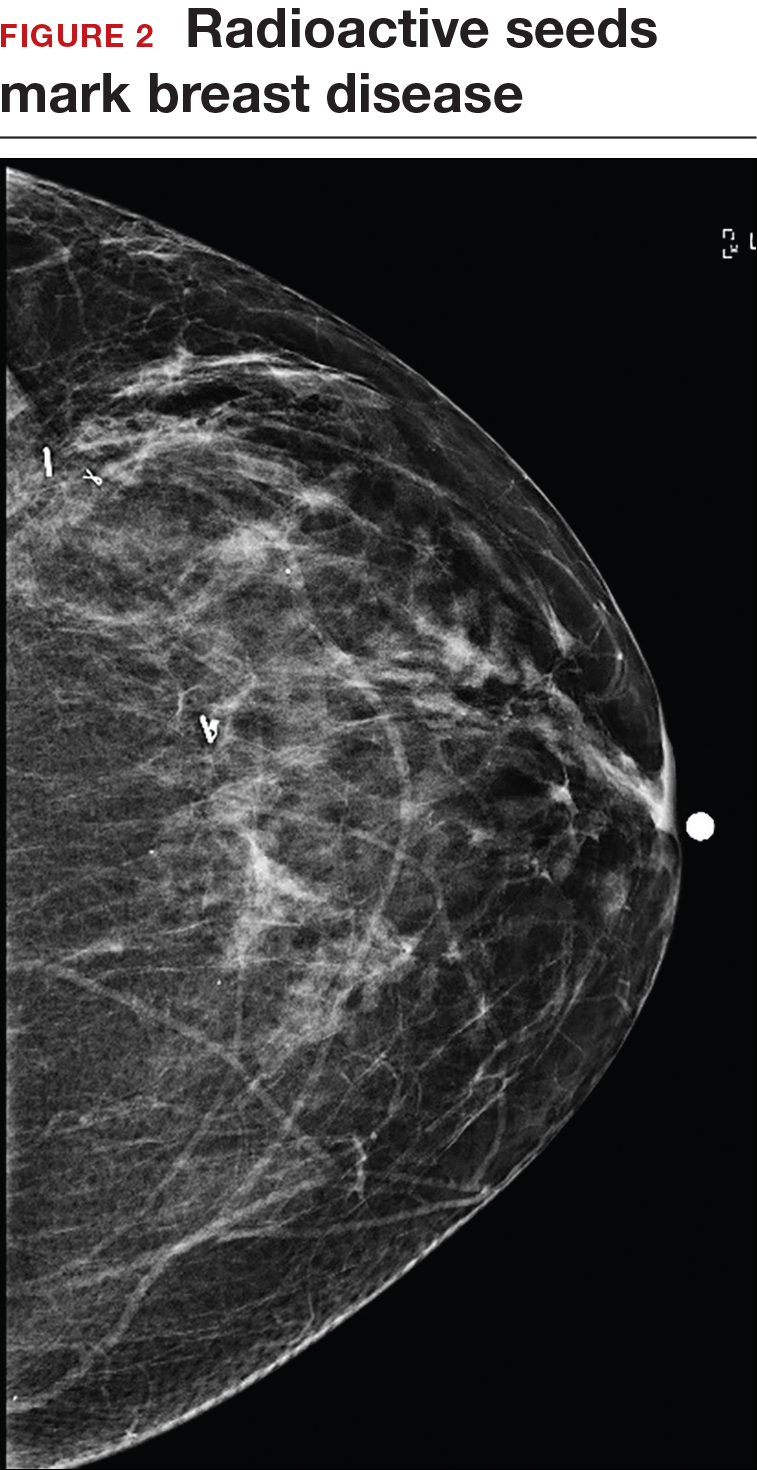
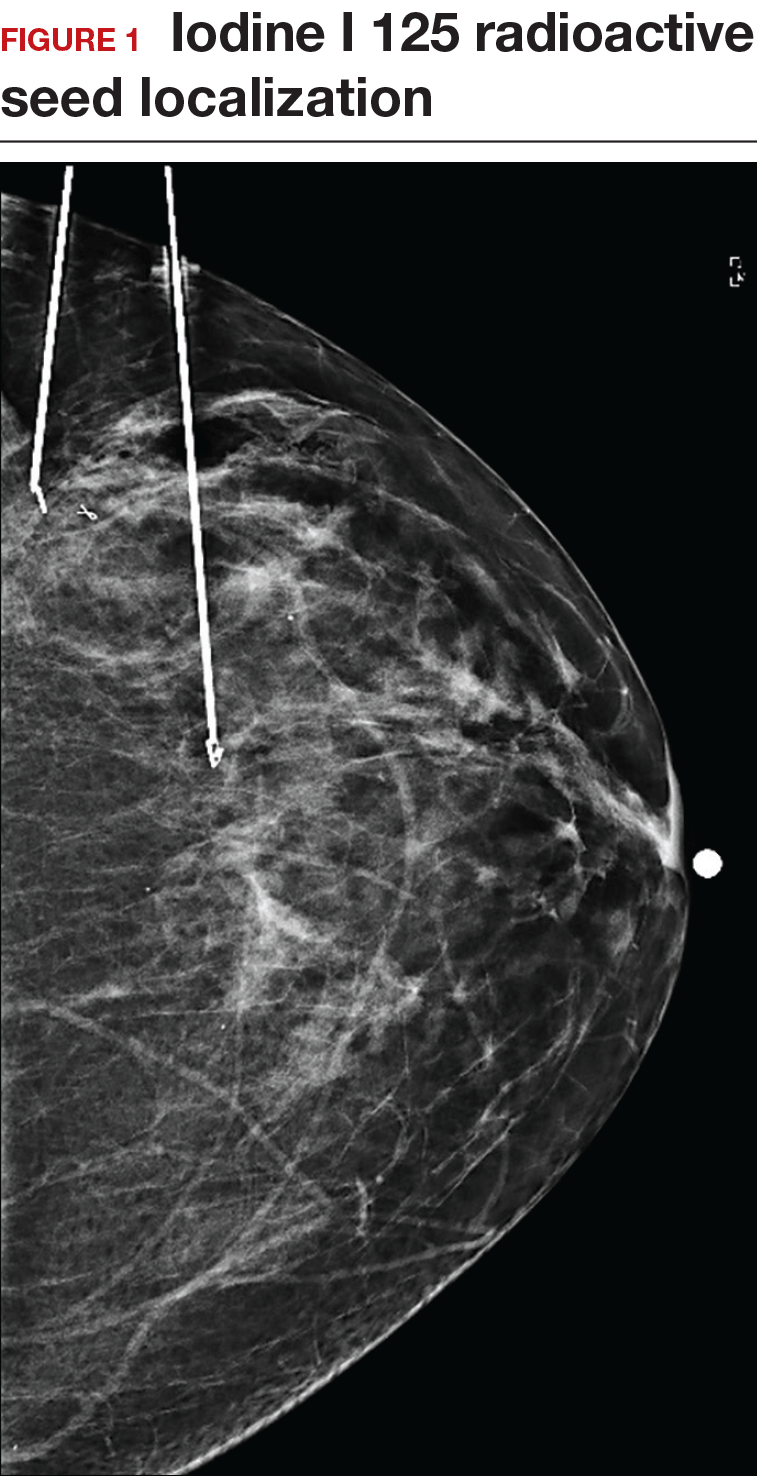
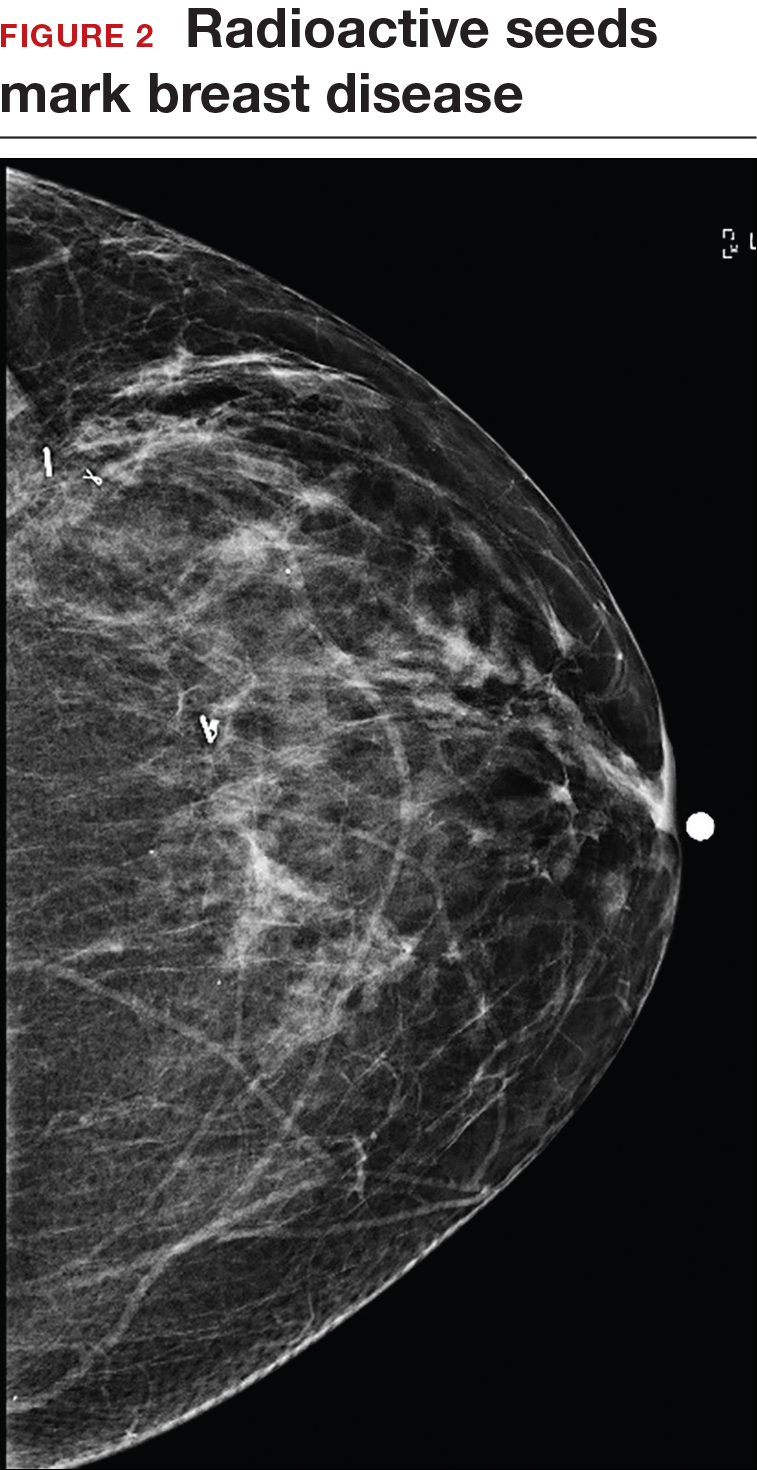
Iodine I 125 Radioactive seed localization (RSL) involves placing a 4-mm titanium radiolabeled seed into the breast lesion under mammographic or ultrasound guidance (FIGURES 1 and 2). The procedure can be performed a few days before surgery in the radiology department, and there is less chance for the seed to become displaced or dislodged. This technique provides scheduling flexibility for the radiologist and reduces OR delays. The surgeon uses the same gamma probe for sentinel node biopsy to find the lesion in the breast, using the setting specific for iodine I 125. Incisions can be tailored anywhere in the breast, and the seed is detected by a focal gamma signal. Once the lumpectomy is performed, the specimen is probed and radiographed to confirm removal of the seed and adequate margins.
Limitations of this procedure include potential loss of the seed during the operation and radiation safety issues regarding handling and disposal of the radioactive isotope. Once the seed has been placed in the patient’s body, it must be removed surgically, as the half-life of iodine I 125 is long (60 days).5 Care must therefore be taken to optimize medical clearance prior to seed placement and to avoid surgery cancellations.
Intraoperative ultrasound (IOUS) allows the surgeon to identify the lesion under general anesthesia in the OR, which is more comfortable for the patient. The surgical incision can be tailored cosmetically and the lumpectomy can be performed with real-time ultrasound visualization of the tumor during dissection. This technique eliminates the need for a separate preoperative seed or wire localization in radiology. However, it can be used only for lesions or clips that are visible by ultrasound. The excised specimen can be evaluated for confirmation of tumor removal and adequate margins via ultrasound and re-excision of close margins can be accomplished immediately if needed.
Results of a meta-analysis of WGL versus IOUS demonstrated a significant reduction of positive margins with the use of IOUS.6 Results of the COBALT trial, in which patients were assigned randomly to excision of palpable breast cancers with either IOUS or palpation, demonstrated a 14% reduction in positive margins in favor of IOUS.7 Surgeon-performed breast ultrasound requires advanced training and accreditation in breast ultrasound through a rigorous certification process offered by the American Society of Breast Surgeons (www.breastsurgeons.org).
Oncoplastic lumpectomy
This approach to lumpectomy combines adequate oncologist resection of the breast tumor with plastic surgery techniques to achieve superior cosmesis. This approach allows complete removal of the tumor with negative margins, yet maintains the normal shape and contour of the breast. Two techniques have been described: volume displacement and volume replacement.
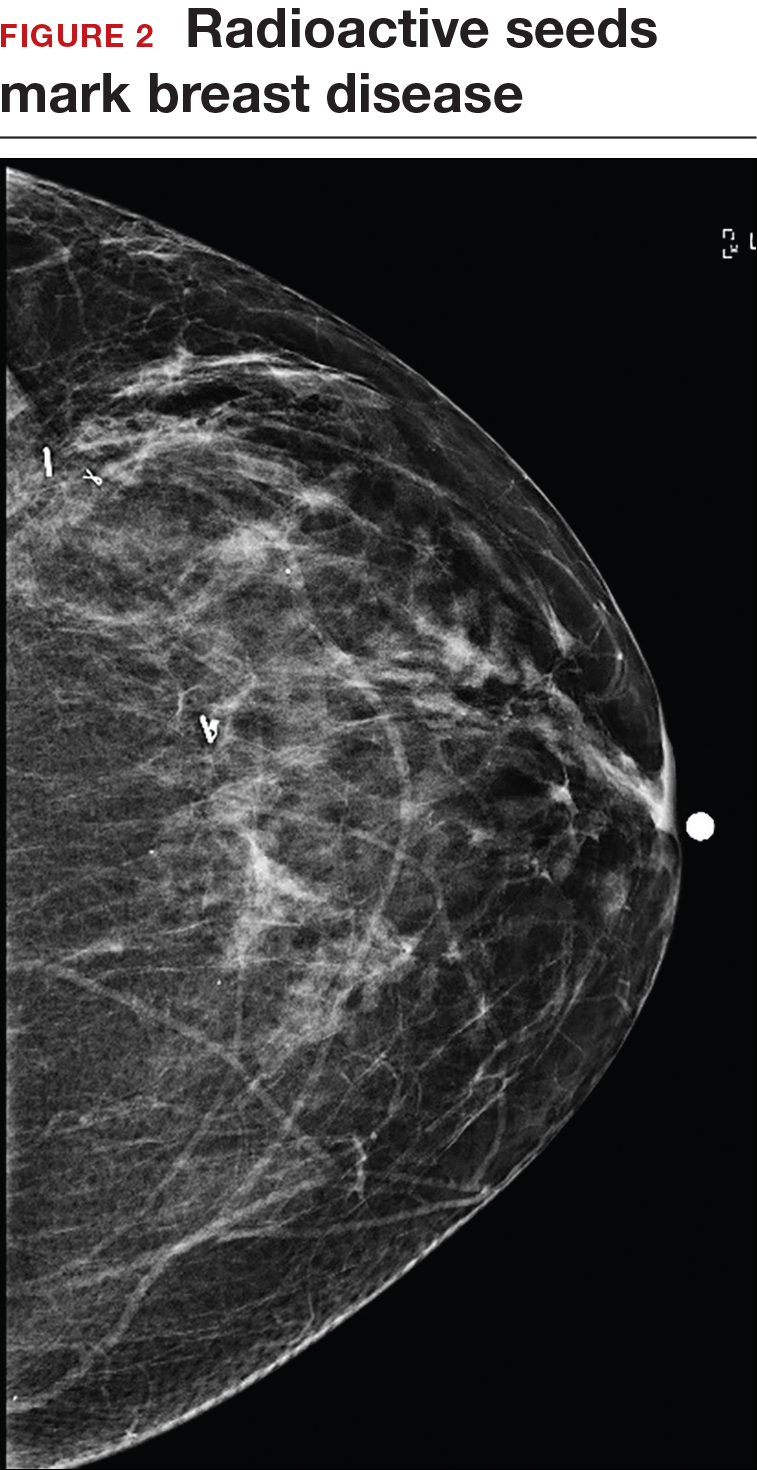
With the volume displacement technique, the surgeon uses adjacent tissue advancement to fill the lumpectomy cavity with the patient’s own surrounding breast tissue (FIGURE 3). The volume replacement technique requires the transposition of autologous tissue from elsewhere in the body.

Oncoplastic lumpectomy allows more women with larger tumors to undergo breast conservation with better cosmetic results. It reduces the number of mastectomies performed without compromising local control and avoids the need for extensive plastic surgery reconstruction and implants. Special effort and attention must be paid to ensure adequate margins utilizing intraoperative specimen radiograph and pathology evaluation.
This procedure requires that the surgeon acquire specialized skills and knowledge of oncologic and plastic surgery techniques, and it is best performed with the collaboration of a multidisciplinary team. Compared with conventional lumpectomy or mastectomy, oncoplastic breast conservation has been shown to reduce re-excision rates, and it has similar rates of local and distant recurrence and similar disease-free survival and overall survival.8,9
Total skin- and nipple-sparing mastectomy
Some patients do not have the option of breast conservation. Women with multicentric breast cancer (more than 1 tumor in different quadrants of the breast) are better served with mastectomy. Surgical techniques for mastectomy have improved and provide women with various options. One option is skin- and nipple-sparing mastectomy, which preserves the skin envelope overlying the breast (including the skin of the nipple and areola) while removing the glandular elements of the breast and the majority of ductal tissue beneath the nipple-areola complex (FIGURE 4). This surgery can be performed via hidden scars at the inframammary crease or periareolar and is combined with immediate reconstruction, which provides an excellent cosmetic result.
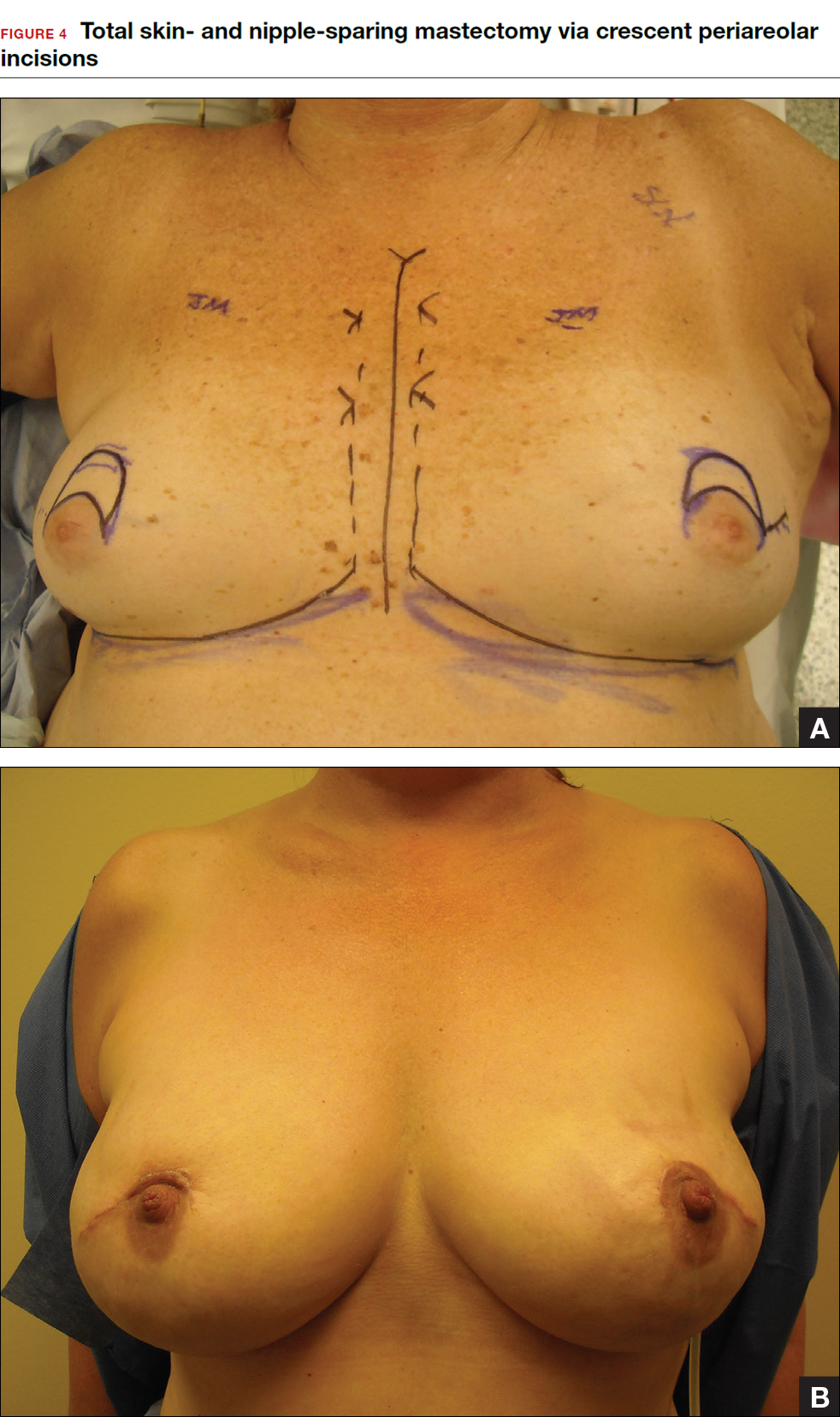
Surgical considerations include removing glandular breast tissue within its anatomic boundaries while maintaining the blood supply to the skin and nipple-areola complex. Furthermore, there must be close dissection of ductal tissue beneath the nipple-areola complex and intraoperative frozen section of the nipple margin in cancer cases. Nipple-sparing mastectomy is oncologically safe in carefully selected patients who do not have cancer near or within the skin or nipple (eg, Paget disease).10 It is also safe as a prophylactic procedure for patients with genetic mutations, such as BRCA1 and BRCA2.11 The procedure is not ideal for smokers or patients with large, pendulous breasts. There is a 3% risk of breast cancer recurrence at the nipple or in the skin or muscle.10 Surgical complications include a 10% to 20% risk of skin or nipple necrosis.12
How do we manage the lymph nodes: Axillary dissection vs sentinel node biopsy?
Evaluation of the axillary nodes is currently part of breast cancer staging and can help the clinician determine the need for adjuvant chemotherapy. It also may assist in assessing the need for extending the radiation field beyond the breast to include the regional lymph nodes. Patients with early stage (stage I and II) breast cancer who do not have abnormal palpable lymph nodes or biopsy-proven metastasis to axillary nodes qualify for sentinel lymph node (SLN) biopsy.
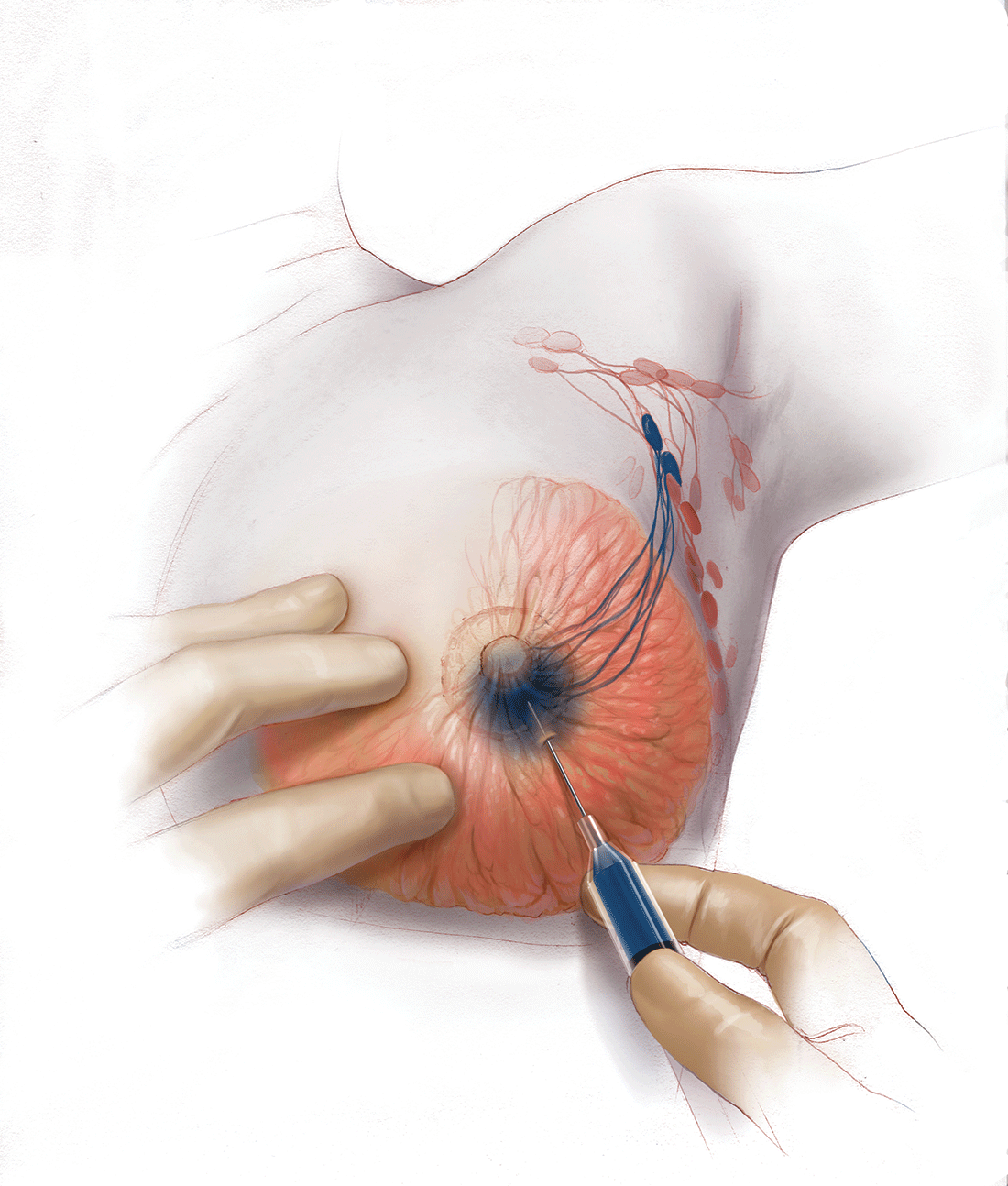
Sentinel node biopsy = less morbidity with no loss of accuracy. Compared with axillary lymph node dissection (ALND; removing all the level I and II nodes in the axilla), SLN biopsy has a 98% accuracy and is associated with less morbidity from lymphedema. The procedure involves injecting the breast with 2 tracers: a radioactive isotope, injected into the breast within 24 hours of the operation, and isosulfan blue dye, injected into the breast in the OR at the time of surgery (see illustration). Both tracers travel through the breast lymphatics and concentrate in the first few lymph nodes that drain the breast. The surgery is performed through a separate axillary incision, and the blue and radioactive lymph nodes are individually dissected and removed for pathologic evaluation. On average, 2 to 4 sentinel nodes are removed, including any suspicious palpable nodes. In experienced hands, this procedure has a false-negative rate of less than 5% to 10%.13
Axillary node dissection no longer standard of care. The indication for a completion ALND has changed based on the results of the randomized trial, ACOSOG Z0011.14 In this trial, patients with early stage breast cancer and 1 to 2 positive SLNs who were undergoing breast conservation therapy with radiation and adjuvant systemic therapy were randomly assigned to ALND or no ALND. (The trial did not include patients who were undergoing mastectomy, neoadjuvant chemotherapy, or who had more than 2 metastatic lymph nodes.) The investigators found no difference in overall or disease-free survival or local-regional recurrence between the 2 treatment groups over 9.2 years of follow up.14
Based on this practice-changing trial result, guidelines of the National Comprehensive Cancer Network no longer recommend completion ALND for patients who meet the ACOSOG Z0011 criteria. For patients who do not meet ACOSOG Z0011 criteria, we do intraoperative pathologic lymph node assessment with either frozen section or imprint cytology, and we perform immediate ALND when results are positive.
Indications for SLN biopsy include:
- invasive breast cancer with clinically negative axillary nodes
- ductal carcinoma in situ (DCIS) with microinvasion or extensive enough to require mastectomy
- clinically negative axillary nodes after neoadjuvant chemotherapy.
Contraindications for SLN biopsy include:
- bulky palpable lymphadenopathy
- pregnancy, as the safety of radioactive isotope and blue dye is not well studied; in isotope mapping the radiation dose is small and within safety limits for pregnant patients
- inflammatory breast cancer.
Complications of any axillary surgery may include risk of lymphedema (5% with SLN biopsy and 30% to 40% with ALND).15 Other complications include neuropathy of the affected arm with chronic pain and numbness of the skin.
Positive trends: Improved patient outcomes, specialized clinician training
Management of breast cancer has changed dramatically over the past several decades. More women are surviving breast cancer thanks to improvements in early detection, an individualized treatment approach with less aggressive surgery, and more effective targeted systemic therapies. A multidisciplinary, team-oriented approach with emphasis on minimally invasive biopsy and better cosmetic outcomes has enhanced quality of care.
Complexity in breast disease management has led to the development of formal fellowship training in breast surgical oncology. Studies have demonstrated that patients treated by high-volume breast surgeons are more satisfied with their care and have improved cancer outcomes.16,17 Women should be aware that they have different options for their breast cancer care, and surgeons with advanced specialization in this field may provide optimal results and better quality of care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Nichols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–1569.
- Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer [published online ahead of print March 8, 2016]. Ann Surg. doi:10.1097/SLA.0000000000001698.
- Miller ME, Czechura T, Martz B, et al. Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Ann Surg Oncol. 2013;20(13):4113–4120.
- Zhang X, Zhang XJ, Zhang TY, et al. Effect and safety of dual anti-human epidermal growth factor receptor 2 therapy compared to monotherapy in patients with human epidermal growth factor receptor 2-positive breast cancer: a systematic review. BMC Cancer. 2014;14:625.
- Ahmed M, Rubio IT, Klaase JM, Douek M. Surgical treatment of nonpalpable primary invasive and in situ breast cancer. Nat Rev Clin Oncol. 2015;12(11):645–663.
- Ahmed M, Douek M. Intra-operative ultrasound versus wire-guided localization in the surgical management of non-palpable breast cancers: systemic review and meta-analysis. Breast Cancer Res Treat. 2013;140(3):435–446.
- Krekel NM, Haloua MH, Lopes Cardozo AM, et al. Intraoperative ultrasound guidance for palpable breast cancer excision (COBALT trial): a multicentre, randomised controlled trial. Lancet Oncol. 2013;14(1):48–54.
- Chakravorty A, Shrestha AK, Sanmugalingam N, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol. 2012;38(5):395–398.
- De Lorenzi F, Hubner G, Rotmensz N, et al. Oncological results of oncoplastic breast-conserving surgery: long term follow-up of a large series at a single institution: a matched-cohort analysis. Eur J Surg Oncol. 2016;42(1):71–77.
- De La Cruz L, Moody AM, Tappy EE, Blankenship AA, Hecht EM. Overall survival, disease-free survival, local recurrence, and nipple-areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol. 2015;22(10):3241–3249.
- Yao K, Liederbach E, Tang R, et al. Nipple-sparing mastectomy in BRCA1/2 mutation carriers: an interim analysis and review of the literature. Ann Surg Oncol. 2015;22(2):370–376.
- Fortunato L, Loreti A, Andrich R, et al. When mastectomy is needed: is the nipple-sparing procedure a new standard with very few contraindications? J Surg Oncol. 2013;108(4):207–212.
- Veronesi U, Viale G, Paganelli G, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg. 2010;251(4):595–600.
- Giuliano AE, Hunt K, Ballman KV, et al. Ten-year survival results of ACOSOG Z0011: a randomized trial of axillary node dissection in women with clinical T1-2 N0 M0 breast cancer who have a positive sentinel node (Alliance). In: 2016 ASCO Annual Meeting; June 3-7, 2016. J Clin Oncol. 2016;34(15; May 20 suppl): Abstract 1007.
- DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–515.
- Skinner KA, Helsper JT, Deapen D, Ye W, Sposto R. Breast cancer: do specialists make a difference? Ann Surg Oncol. 2003;10(6):606–615.
- Waljee JF, Hawley S, Alderman AK, Morrow M, Katz SJ. Patient satisfaction with treatment of breast cancer: does surgeon specialization matter? J Clin Oncol. 2007;25(24):3694–3698.
In a striking trend, the rate of contralateral prophylactic mastectomy (CPM) has risen by 30% over the last 10 years in the United States.1 Many women undergo CPM because of the fear and anxiety of cancer recurrence and their perceived risk of contralateral breast cancer; however, few women have a medical condition that necessitates removal of the contralateral breast. The medical indications for CPM include having a pathogenic genetic mutation (eg, BRCA1 and BRCA2), a strong family history of breast cancer, or prior mediastina chest radiation.
The actual risk of contralateral breast cancer is much lower than perceived. In women without a genetic mutation, the 10-year risk of contralateral breast cancer is only 3% to 5%.1 Also, CPM does not prevent the development of metastatic disease and offers no survival benefit over breast conservation or unilateral mastectomy.2 Furthermore, compared with unilateral therapeutic mastectomy, the “upgrade” to a CPM carries a 2.7-fold risk of a major surgical complication.3 It is therefore important that patients receive appropriate counseling regarding CPM, and that this counseling include cancer stage at diagnosis, family history and genetic risk, and cancer versus surgical risk (see “Counseling patients on contralateral prophylactic mastectomy” for key points to cover in patient discussions).
Counseling patients on contralateral prophylactic mastectomy
Commonly, patients diagnosed with breast cancer consider having their contralateral healthy breast removed as part of a bilateral mastectomy. They often experience severe anxiety about the cancer coming back and believe that removing both breasts will enable them to live longer. Keep the following key facts in mind when discussing treatment options with breast cancer patients.
Cancer stage at diagnosis. How long a patient lives from the time of her breast cancer diagnosis depends on the stage of the cancer at diagnosis, not the type of surgery performed. A woman with early stage I or stage II breast cancer has an 80% to 90% chance of being cancer free in 5 years.1 The chance of cancer recurring in the bones, liver, or lungs (metastatic breast cancer) will not be changed by removing the healthy breast. The risk of metastatic recurrence can be reduced, however, with chemotherapy and/or with hormone-blocker therapy.
Family history and genetic risk. Few women have a strong family history of breast and/or ovarian and other cancers, and this issue should be addressed with genetic counseling and testing prior to surgery. Those who carry a cancer-causing gene, such as BRCA1 or BRCA2, are at increased risk (40% to 60%) for a second or third breast cancer, especially if they are diagnosed at a young age (<50 years).2,3 In women who have a genetic mutation, removing both breasts and sometimes the ovaries can prevent development of another breast cancer. But this will not prevent spread of the cancer that is already present. Only chemotherapy and hormone blockers can prevent the spread of cancer.
Cancer risk versus surgical risk. For women with no family history of breast cancer, no genetic mutation, and no prior chest wall radiation, the risk of developing a new breast cancer in their other breast is only 3% to 5% every 10 years.3,4 This means that they have a 95% chance of not developing a new breast cancer in their healthy breast. Notably, removing the healthy breast can double the risk of postsurgical complications, including bleeding, infection, and loss of tissue and implant. The mastectomy site will be numb and the skin and nipple areola will not have any function other than cosmetic. Finally, wound complications from surgery could delay the start of important cancer treatment, such as chemotherapy or radiation.
The bottom line. Unless a woman has a strong family history of breast cancer, is diagnosed at a very young age, or has a genetic cancer-causing mutation, removing the contralateral healthy breast is not medically necessary and is not routinely recommended.
References
- Hennigs A, Riedel F, Gondos A, et al. Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer. 2016;16(1):734.
- Graeser MK, Engel C, Rhiem K, et al. Contralateral breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2009;27(35):5887–5992.
- Curtis RE, Ron E, Hankey BF, Hoover RN. New malignancies following breast cancer. In: Curtis RE, Freedman DM, Ron E, et al, eds. New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973-2000. Bethesda, MD: National Cancer Institute. NIH Publ. No. 05-5302. 2006:181–205. http://seer.cancer.gov/archive/publications/mpmono. Accessed September 18, 2016.
- Nichols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–1569.
Women should be made aware that there are alternatives to mastectomy that have similar, or even better, outcomes with improved quality of life. Furthermore, a multi‑disciplinary, team-oriented approach with emphasis on minimally invasive biopsy and better cosmetic outcomes has enhanced quality of care. Knowledge of this team approach and of modern breast cancer treatments is essential for general ObGyns as this understanding improves the overall care and guidance—specifically regarding referral to expert, high-volume breast surgeons—provided to those women most in need.
Expanded treatment options for breast cancer
Advancements in breast surgery, better imaging, and targeted therapies are changing the paradigm of breast cancer treatment.
Image-guided biopsy is key in decision making
When an abnormality is found in the breast, surgical excision of an undiagnosed breast lesion is no longer considered an appropriate first step. Use of image-guided biopsy or minimally invasive core needle biopsy allows for accurate diagnosis of a breast lesion while avoiding a potentially breast deforming and expensive surgical operation. It is always better to go into the operating room (OR) with a diagnosis and do the right operation the first time.
A core needle biopsy, results of which demonstrate a benign lesion, helps avoid breast surgery in women who do not need it. If cancer is diagnosed on biopsy, the extent of disease can be better evaluated and decision making can be more informed, with a multidisciplinary approach used to consider the various options, including genetic counseling, plastic surgery consultation, or neoadjuvant therapy. Some lesions, such as those too close to the skin, chest wall, or an implant, may not be amenable to core needle biopsy and therefore require surgical excision for diagnosis.
Benefits of a multidisciplinary tumor conference
It is important for a multidisciplinary group of cancer specialists to review a patient’s case and discuss the ideal treatment plan prior to surgery. Some breast cancer subtypes (such as human epidermal growth factor receptor 2 [HER2]–overamplified breast cancer and many triple-negative breast cancers) are very sensitive to chemotherapy, and patients with these tumor types may benefit from receiving neoadjuvant chemotherapy prior to surgery. New types of chemotherapy may allow up to 60% of some breast cancers to diminish almost completely, with subsequent improved cosmetic results of breast surgery.4 It may also allow time for genetic counseling and testing prior to surgery. (See “How to code for a multidisciplinary tumor conference” for appropriate coding procedure.)
How to code for a multidisciplinary tumor conference
Melanie Witt, RN, MA
There are two coding choices for team conferences involving physician participation. If the patient and/or family is present, the CPT instruction is to bill a problem E/M service code (99201-99215) based on the time spent during this coordination of care/counseling. Documentation would include details about the conference decisions and implications for care, rather than history or examination.
If the patient is not present, report 99367 (Medical team conference with interdisciplinary team of health care professionals, patient and/or family not present, 30 minutes or more; participation by physician), but note that this code was developed under the assumption that the conference would be performed in a facility setting. Diagnostic coding would be breast cancer.
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
The author reports no financial relationships relevant to this article.
This is an excerpt from a companion coding resource for breast cancer–related procedures by Ms. Witt. To read the companion article, “Coding for breast cancer–related procedures: A how-to guide,” in its entirety, click here.
Image-guided lumpectomy
Advances in breast imaging have led to increased identification of nonpalpable breast cancers. Surgical excision of nonpalpable breast lesions requires image guidance, which can be done using a variety of techniques.
Wire-guided localization (WGL) has been used in practice for the past 40 years. The procedure involves placement of a hooked wire under local anesthesia using either mammographic or ultrasound guidance. This procedure is mostly done in the radiology department on the same day as the surgery and requires that the radiologist coordinate with the OR schedule. Besides scheduling conflicts and delays in surgery, this procedure can be complicated by wires becoming dislodged, transected, or migrated, and limits the surgeon’s ability to cosmetically hide the scar in relation to position of the wire. It is uncomfortable for the patient, who must be transported from the radiology department to the OR with a wire extruding from her breast.
An alternative localization technique is placement of a radioactive source within the tumor, which can then be identified in the OR with a gamma probe.
Iodine I 125 Radioactive seed localization (RSL) involves placing a 4-mm titanium radiolabeled seed into the breast lesion under mammographic or ultrasound guidance (FIGURES 1 and 2). The procedure can be performed a few days before surgery in the radiology department, and there is less chance for the seed to become displaced or dislodged. This technique provides scheduling flexibility for the radiologist and reduces OR delays. The surgeon uses the same gamma probe for sentinel node biopsy to find the lesion in the breast, using the setting specific for iodine I 125. Incisions can be tailored anywhere in the breast, and the seed is detected by a focal gamma signal. Once the lumpectomy is performed, the specimen is probed and radiographed to confirm removal of the seed and adequate margins.
Limitations of this procedure include potential loss of the seed during the operation and radiation safety issues regarding handling and disposal of the radioactive isotope. Once the seed has been placed in the patient’s body, it must be removed surgically, as the half-life of iodine I 125 is long (60 days).5 Care must therefore be taken to optimize medical clearance prior to seed placement and to avoid surgery cancellations.
Intraoperative ultrasound (IOUS) allows the surgeon to identify the lesion under general anesthesia in the OR, which is more comfortable for the patient. The surgical incision can be tailored cosmetically and the lumpectomy can be performed with real-time ultrasound visualization of the tumor during dissection. This technique eliminates the need for a separate preoperative seed or wire localization in radiology. However, it can be used only for lesions or clips that are visible by ultrasound. The excised specimen can be evaluated for confirmation of tumor removal and adequate margins via ultrasound and re-excision of close margins can be accomplished immediately if needed.
Results of a meta-analysis of WGL versus IOUS demonstrated a significant reduction of positive margins with the use of IOUS.6 Results of the COBALT trial, in which patients were assigned randomly to excision of palpable breast cancers with either IOUS or palpation, demonstrated a 14% reduction in positive margins in favor of IOUS.7 Surgeon-performed breast ultrasound requires advanced training and accreditation in breast ultrasound through a rigorous certification process offered by the American Society of Breast Surgeons (www.breastsurgeons.org).
Oncoplastic lumpectomy
This approach to lumpectomy combines adequate oncologist resection of the breast tumor with plastic surgery techniques to achieve superior cosmesis. This approach allows complete removal of the tumor with negative margins, yet maintains the normal shape and contour of the breast. Two techniques have been described: volume displacement and volume replacement.
With the volume displacement technique, the surgeon uses adjacent tissue advancement to fill the lumpectomy cavity with the patient’s own surrounding breast tissue (FIGURE 3). The volume replacement technique requires the transposition of autologous tissue from elsewhere in the body.

Oncoplastic lumpectomy allows more women with larger tumors to undergo breast conservation with better cosmetic results. It reduces the number of mastectomies performed without compromising local control and avoids the need for extensive plastic surgery reconstruction and implants. Special effort and attention must be paid to ensure adequate margins utilizing intraoperative specimen radiograph and pathology evaluation.
This procedure requires that the surgeon acquire specialized skills and knowledge of oncologic and plastic surgery techniques, and it is best performed with the collaboration of a multidisciplinary team. Compared with conventional lumpectomy or mastectomy, oncoplastic breast conservation has been shown to reduce re-excision rates, and it has similar rates of local and distant recurrence and similar disease-free survival and overall survival.8,9
Total skin- and nipple-sparing mastectomy
Some patients do not have the option of breast conservation. Women with multicentric breast cancer (more than 1 tumor in different quadrants of the breast) are better served with mastectomy. Surgical techniques for mastectomy have improved and provide women with various options. One option is skin- and nipple-sparing mastectomy, which preserves the skin envelope overlying the breast (including the skin of the nipple and areola) while removing the glandular elements of the breast and the majority of ductal tissue beneath the nipple-areola complex (FIGURE 4). This surgery can be performed via hidden scars at the inframammary crease or periareolar and is combined with immediate reconstruction, which provides an excellent cosmetic result.
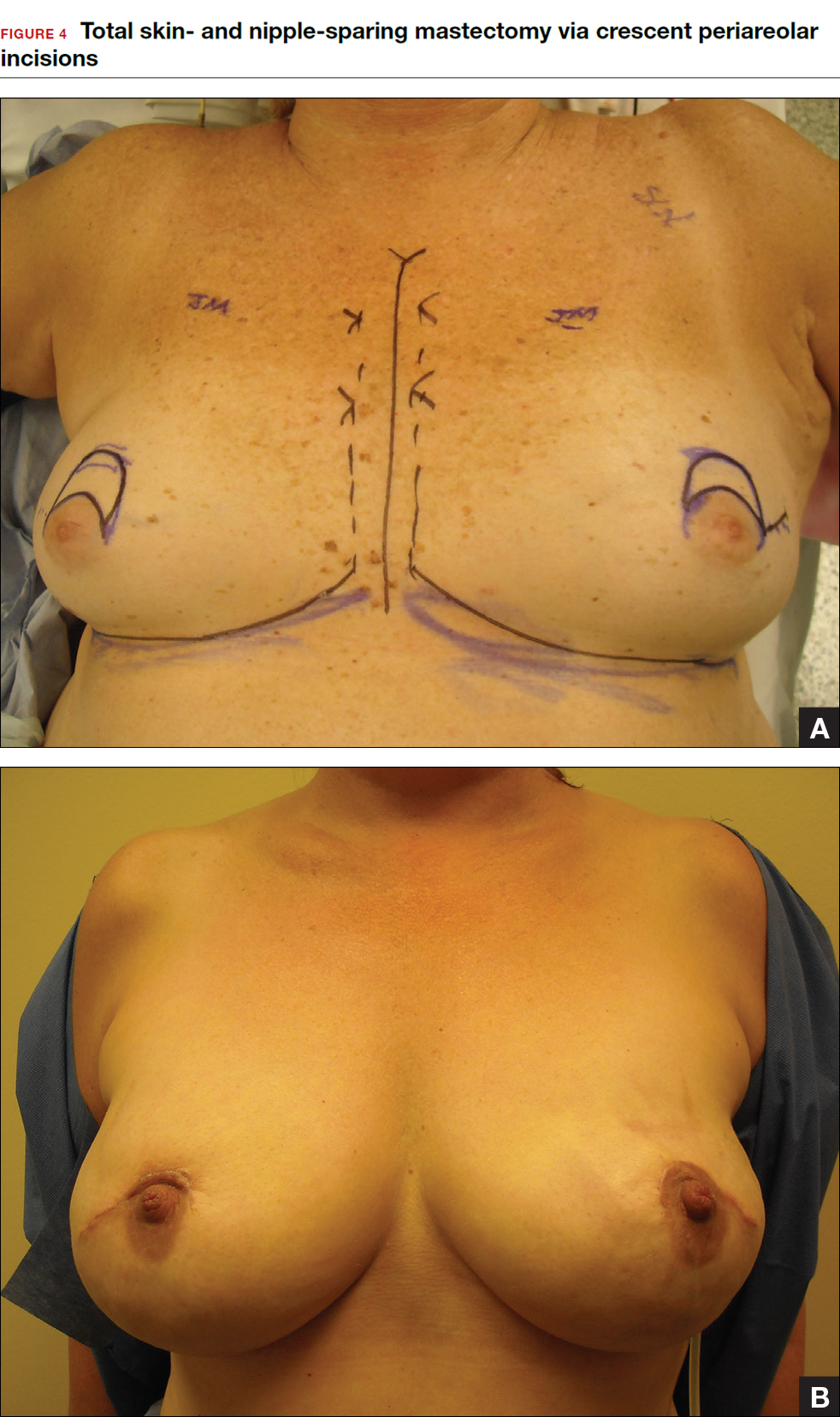
Surgical considerations include removing glandular breast tissue within its anatomic boundaries while maintaining the blood supply to the skin and nipple-areola complex. Furthermore, there must be close dissection of ductal tissue beneath the nipple-areola complex and intraoperative frozen section of the nipple margin in cancer cases. Nipple-sparing mastectomy is oncologically safe in carefully selected patients who do not have cancer near or within the skin or nipple (eg, Paget disease).10 It is also safe as a prophylactic procedure for patients with genetic mutations, such as BRCA1 and BRCA2.11 The procedure is not ideal for smokers or patients with large, pendulous breasts. There is a 3% risk of breast cancer recurrence at the nipple or in the skin or muscle.10 Surgical complications include a 10% to 20% risk of skin or nipple necrosis.12
How do we manage the lymph nodes: Axillary dissection vs sentinel node biopsy?
Evaluation of the axillary nodes is currently part of breast cancer staging and can help the clinician determine the need for adjuvant chemotherapy. It also may assist in assessing the need for extending the radiation field beyond the breast to include the regional lymph nodes. Patients with early stage (stage I and II) breast cancer who do not have abnormal palpable lymph nodes or biopsy-proven metastasis to axillary nodes qualify for sentinel lymph node (SLN) biopsy.
Sentinel node biopsy = less morbidity with no loss of accuracy. Compared with axillary lymph node dissection (ALND; removing all the level I and II nodes in the axilla), SLN biopsy has a 98% accuracy and is associated with less morbidity from lymphedema. The procedure involves injecting the breast with 2 tracers: a radioactive isotope, injected into the breast within 24 hours of the operation, and isosulfan blue dye, injected into the breast in the OR at the time of surgery (see illustration). Both tracers travel through the breast lymphatics and concentrate in the first few lymph nodes that drain the breast. The surgery is performed through a separate axillary incision, and the blue and radioactive lymph nodes are individually dissected and removed for pathologic evaluation. On average, 2 to 4 sentinel nodes are removed, including any suspicious palpable nodes. In experienced hands, this procedure has a false-negative rate of less than 5% to 10%.13
Axillary node dissection no longer standard of care. The indication for a completion ALND has changed based on the results of the randomized trial, ACOSOG Z0011.14 In this trial, patients with early stage breast cancer and 1 to 2 positive SLNs who were undergoing breast conservation therapy with radiation and adjuvant systemic therapy were randomly assigned to ALND or no ALND. (The trial did not include patients who were undergoing mastectomy, neoadjuvant chemotherapy, or who had more than 2 metastatic lymph nodes.) The investigators found no difference in overall or disease-free survival or local-regional recurrence between the 2 treatment groups over 9.2 years of follow up.14
Based on this practice-changing trial result, guidelines of the National Comprehensive Cancer Network no longer recommend completion ALND for patients who meet the ACOSOG Z0011 criteria. For patients who do not meet ACOSOG Z0011 criteria, we do intraoperative pathologic lymph node assessment with either frozen section or imprint cytology, and we perform immediate ALND when results are positive.
Indications for SLN biopsy include:
- invasive breast cancer with clinically negative axillary nodes
- ductal carcinoma in situ (DCIS) with microinvasion or extensive enough to require mastectomy
- clinically negative axillary nodes after neoadjuvant chemotherapy.
Contraindications for SLN biopsy include:
- bulky palpable lymphadenopathy
- pregnancy, as the safety of radioactive isotope and blue dye is not well studied; in isotope mapping the radiation dose is small and within safety limits for pregnant patients
- inflammatory breast cancer.
Complications of any axillary surgery may include risk of lymphedema (5% with SLN biopsy and 30% to 40% with ALND).15 Other complications include neuropathy of the affected arm with chronic pain and numbness of the skin.
Positive trends: Improved patient outcomes, specialized clinician training
Management of breast cancer has changed dramatically over the past several decades. More women are surviving breast cancer thanks to improvements in early detection, an individualized treatment approach with less aggressive surgery, and more effective targeted systemic therapies. A multidisciplinary, team-oriented approach with emphasis on minimally invasive biopsy and better cosmetic outcomes has enhanced quality of care.
Complexity in breast disease management has led to the development of formal fellowship training in breast surgical oncology. Studies have demonstrated that patients treated by high-volume breast surgeons are more satisfied with their care and have improved cancer outcomes.16,17 Women should be aware that they have different options for their breast cancer care, and surgeons with advanced specialization in this field may provide optimal results and better quality of care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In a striking trend, the rate of contralateral prophylactic mastectomy (CPM) has risen by 30% over the last 10 years in the United States.1 Many women undergo CPM because of the fear and anxiety of cancer recurrence and their perceived risk of contralateral breast cancer; however, few women have a medical condition that necessitates removal of the contralateral breast. The medical indications for CPM include having a pathogenic genetic mutation (eg, BRCA1 and BRCA2), a strong family history of breast cancer, or prior mediastina chest radiation.
The actual risk of contralateral breast cancer is much lower than perceived. In women without a genetic mutation, the 10-year risk of contralateral breast cancer is only 3% to 5%.1 Also, CPM does not prevent the development of metastatic disease and offers no survival benefit over breast conservation or unilateral mastectomy.2 Furthermore, compared with unilateral therapeutic mastectomy, the “upgrade” to a CPM carries a 2.7-fold risk of a major surgical complication.3 It is therefore important that patients receive appropriate counseling regarding CPM, and that this counseling include cancer stage at diagnosis, family history and genetic risk, and cancer versus surgical risk (see “Counseling patients on contralateral prophylactic mastectomy” for key points to cover in patient discussions).
Counseling patients on contralateral prophylactic mastectomy
Commonly, patients diagnosed with breast cancer consider having their contralateral healthy breast removed as part of a bilateral mastectomy. They often experience severe anxiety about the cancer coming back and believe that removing both breasts will enable them to live longer. Keep the following key facts in mind when discussing treatment options with breast cancer patients.
Cancer stage at diagnosis. How long a patient lives from the time of her breast cancer diagnosis depends on the stage of the cancer at diagnosis, not the type of surgery performed. A woman with early stage I or stage II breast cancer has an 80% to 90% chance of being cancer free in 5 years.1 The chance of cancer recurring in the bones, liver, or lungs (metastatic breast cancer) will not be changed by removing the healthy breast. The risk of metastatic recurrence can be reduced, however, with chemotherapy and/or with hormone-blocker therapy.
Family history and genetic risk. Few women have a strong family history of breast and/or ovarian and other cancers, and this issue should be addressed with genetic counseling and testing prior to surgery. Those who carry a cancer-causing gene, such as BRCA1 or BRCA2, are at increased risk (40% to 60%) for a second or third breast cancer, especially if they are diagnosed at a young age (<50 years).2,3 In women who have a genetic mutation, removing both breasts and sometimes the ovaries can prevent development of another breast cancer. But this will not prevent spread of the cancer that is already present. Only chemotherapy and hormone blockers can prevent the spread of cancer.
Cancer risk versus surgical risk. For women with no family history of breast cancer, no genetic mutation, and no prior chest wall radiation, the risk of developing a new breast cancer in their other breast is only 3% to 5% every 10 years.3,4 This means that they have a 95% chance of not developing a new breast cancer in their healthy breast. Notably, removing the healthy breast can double the risk of postsurgical complications, including bleeding, infection, and loss of tissue and implant. The mastectomy site will be numb and the skin and nipple areola will not have any function other than cosmetic. Finally, wound complications from surgery could delay the start of important cancer treatment, such as chemotherapy or radiation.
The bottom line. Unless a woman has a strong family history of breast cancer, is diagnosed at a very young age, or has a genetic cancer-causing mutation, removing the contralateral healthy breast is not medically necessary and is not routinely recommended.
References
- Hennigs A, Riedel F, Gondos A, et al. Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer. 2016;16(1):734.
- Graeser MK, Engel C, Rhiem K, et al. Contralateral breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2009;27(35):5887–5992.
- Curtis RE, Ron E, Hankey BF, Hoover RN. New malignancies following breast cancer. In: Curtis RE, Freedman DM, Ron E, et al, eds. New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973-2000. Bethesda, MD: National Cancer Institute. NIH Publ. No. 05-5302. 2006:181–205. http://seer.cancer.gov/archive/publications/mpmono. Accessed September 18, 2016.
- Nichols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–1569.
Women should be made aware that there are alternatives to mastectomy that have similar, or even better, outcomes with improved quality of life. Furthermore, a multi‑disciplinary, team-oriented approach with emphasis on minimally invasive biopsy and better cosmetic outcomes has enhanced quality of care. Knowledge of this team approach and of modern breast cancer treatments is essential for general ObGyns as this understanding improves the overall care and guidance—specifically regarding referral to expert, high-volume breast surgeons—provided to those women most in need.
Expanded treatment options for breast cancer
Advancements in breast surgery, better imaging, and targeted therapies are changing the paradigm of breast cancer treatment.
Image-guided biopsy is key in decision making
When an abnormality is found in the breast, surgical excision of an undiagnosed breast lesion is no longer considered an appropriate first step. Use of image-guided biopsy or minimally invasive core needle biopsy allows for accurate diagnosis of a breast lesion while avoiding a potentially breast deforming and expensive surgical operation. It is always better to go into the operating room (OR) with a diagnosis and do the right operation the first time.
A core needle biopsy, results of which demonstrate a benign lesion, helps avoid breast surgery in women who do not need it. If cancer is diagnosed on biopsy, the extent of disease can be better evaluated and decision making can be more informed, with a multidisciplinary approach used to consider the various options, including genetic counseling, plastic surgery consultation, or neoadjuvant therapy. Some lesions, such as those too close to the skin, chest wall, or an implant, may not be amenable to core needle biopsy and therefore require surgical excision for diagnosis.
Benefits of a multidisciplinary tumor conference
It is important for a multidisciplinary group of cancer specialists to review a patient’s case and discuss the ideal treatment plan prior to surgery. Some breast cancer subtypes (such as human epidermal growth factor receptor 2 [HER2]–overamplified breast cancer and many triple-negative breast cancers) are very sensitive to chemotherapy, and patients with these tumor types may benefit from receiving neoadjuvant chemotherapy prior to surgery. New types of chemotherapy may allow up to 60% of some breast cancers to diminish almost completely, with subsequent improved cosmetic results of breast surgery.4 It may also allow time for genetic counseling and testing prior to surgery. (See “How to code for a multidisciplinary tumor conference” for appropriate coding procedure.)
How to code for a multidisciplinary tumor conference
Melanie Witt, RN, MA
There are two coding choices for team conferences involving physician participation. If the patient and/or family is present, the CPT instruction is to bill a problem E/M service code (99201-99215) based on the time spent during this coordination of care/counseling. Documentation would include details about the conference decisions and implications for care, rather than history or examination.
If the patient is not present, report 99367 (Medical team conference with interdisciplinary team of health care professionals, patient and/or family not present, 30 minutes or more; participation by physician), but note that this code was developed under the assumption that the conference would be performed in a facility setting. Diagnostic coding would be breast cancer.
Ms. Witt is an independent coding and documentation consultant and former program manager, department of coding and nomenclature, American Congress of Obstetricians and Gynecologists.
The author reports no financial relationships relevant to this article.
This is an excerpt from a companion coding resource for breast cancer–related procedures by Ms. Witt. To read the companion article, “Coding for breast cancer–related procedures: A how-to guide,” in its entirety, click here.
Image-guided lumpectomy
Advances in breast imaging have led to increased identification of nonpalpable breast cancers. Surgical excision of nonpalpable breast lesions requires image guidance, which can be done using a variety of techniques.
Wire-guided localization (WGL) has been used in practice for the past 40 years. The procedure involves placement of a hooked wire under local anesthesia using either mammographic or ultrasound guidance. This procedure is mostly done in the radiology department on the same day as the surgery and requires that the radiologist coordinate with the OR schedule. Besides scheduling conflicts and delays in surgery, this procedure can be complicated by wires becoming dislodged, transected, or migrated, and limits the surgeon’s ability to cosmetically hide the scar in relation to position of the wire. It is uncomfortable for the patient, who must be transported from the radiology department to the OR with a wire extruding from her breast.
An alternative localization technique is placement of a radioactive source within the tumor, which can then be identified in the OR with a gamma probe.
Iodine I 125 Radioactive seed localization (RSL) involves placing a 4-mm titanium radiolabeled seed into the breast lesion under mammographic or ultrasound guidance (FIGURES 1 and 2). The procedure can be performed a few days before surgery in the radiology department, and there is less chance for the seed to become displaced or dislodged. This technique provides scheduling flexibility for the radiologist and reduces OR delays. The surgeon uses the same gamma probe for sentinel node biopsy to find the lesion in the breast, using the setting specific for iodine I 125. Incisions can be tailored anywhere in the breast, and the seed is detected by a focal gamma signal. Once the lumpectomy is performed, the specimen is probed and radiographed to confirm removal of the seed and adequate margins.
Limitations of this procedure include potential loss of the seed during the operation and radiation safety issues regarding handling and disposal of the radioactive isotope. Once the seed has been placed in the patient’s body, it must be removed surgically, as the half-life of iodine I 125 is long (60 days).5 Care must therefore be taken to optimize medical clearance prior to seed placement and to avoid surgery cancellations.
Intraoperative ultrasound (IOUS) allows the surgeon to identify the lesion under general anesthesia in the OR, which is more comfortable for the patient. The surgical incision can be tailored cosmetically and the lumpectomy can be performed with real-time ultrasound visualization of the tumor during dissection. This technique eliminates the need for a separate preoperative seed or wire localization in radiology. However, it can be used only for lesions or clips that are visible by ultrasound. The excised specimen can be evaluated for confirmation of tumor removal and adequate margins via ultrasound and re-excision of close margins can be accomplished immediately if needed.
Results of a meta-analysis of WGL versus IOUS demonstrated a significant reduction of positive margins with the use of IOUS.6 Results of the COBALT trial, in which patients were assigned randomly to excision of palpable breast cancers with either IOUS or palpation, demonstrated a 14% reduction in positive margins in favor of IOUS.7 Surgeon-performed breast ultrasound requires advanced training and accreditation in breast ultrasound through a rigorous certification process offered by the American Society of Breast Surgeons (www.breastsurgeons.org).
Oncoplastic lumpectomy
This approach to lumpectomy combines adequate oncologist resection of the breast tumor with plastic surgery techniques to achieve superior cosmesis. This approach allows complete removal of the tumor with negative margins, yet maintains the normal shape and contour of the breast. Two techniques have been described: volume displacement and volume replacement.
With the volume displacement technique, the surgeon uses adjacent tissue advancement to fill the lumpectomy cavity with the patient’s own surrounding breast tissue (FIGURE 3). The volume replacement technique requires the transposition of autologous tissue from elsewhere in the body.

Oncoplastic lumpectomy allows more women with larger tumors to undergo breast conservation with better cosmetic results. It reduces the number of mastectomies performed without compromising local control and avoids the need for extensive plastic surgery reconstruction and implants. Special effort and attention must be paid to ensure adequate margins utilizing intraoperative specimen radiograph and pathology evaluation.
This procedure requires that the surgeon acquire specialized skills and knowledge of oncologic and plastic surgery techniques, and it is best performed with the collaboration of a multidisciplinary team. Compared with conventional lumpectomy or mastectomy, oncoplastic breast conservation has been shown to reduce re-excision rates, and it has similar rates of local and distant recurrence and similar disease-free survival and overall survival.8,9
Total skin- and nipple-sparing mastectomy
Some patients do not have the option of breast conservation. Women with multicentric breast cancer (more than 1 tumor in different quadrants of the breast) are better served with mastectomy. Surgical techniques for mastectomy have improved and provide women with various options. One option is skin- and nipple-sparing mastectomy, which preserves the skin envelope overlying the breast (including the skin of the nipple and areola) while removing the glandular elements of the breast and the majority of ductal tissue beneath the nipple-areola complex (FIGURE 4). This surgery can be performed via hidden scars at the inframammary crease or periareolar and is combined with immediate reconstruction, which provides an excellent cosmetic result.
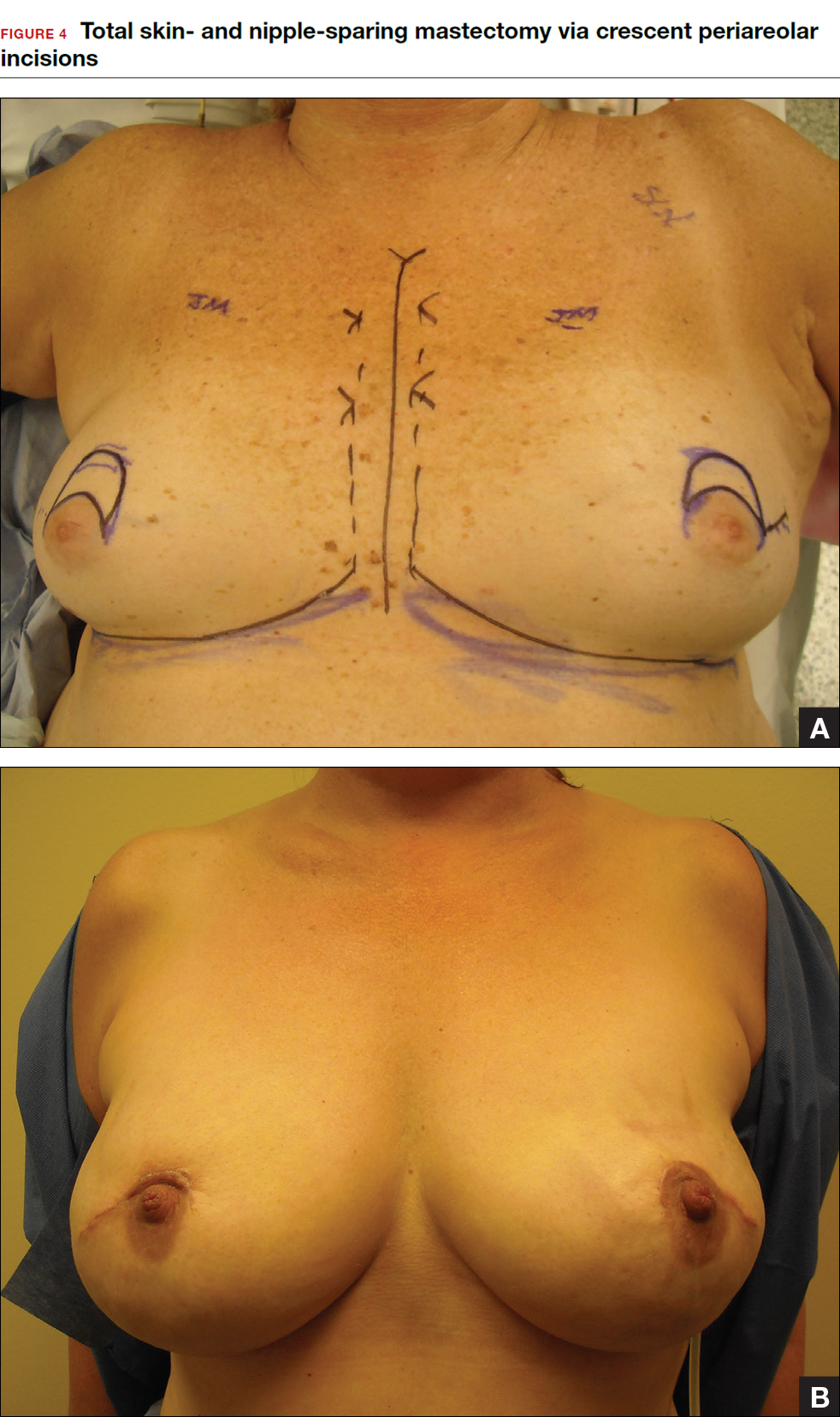
Surgical considerations include removing glandular breast tissue within its anatomic boundaries while maintaining the blood supply to the skin and nipple-areola complex. Furthermore, there must be close dissection of ductal tissue beneath the nipple-areola complex and intraoperative frozen section of the nipple margin in cancer cases. Nipple-sparing mastectomy is oncologically safe in carefully selected patients who do not have cancer near or within the skin or nipple (eg, Paget disease).10 It is also safe as a prophylactic procedure for patients with genetic mutations, such as BRCA1 and BRCA2.11 The procedure is not ideal for smokers or patients with large, pendulous breasts. There is a 3% risk of breast cancer recurrence at the nipple or in the skin or muscle.10 Surgical complications include a 10% to 20% risk of skin or nipple necrosis.12
How do we manage the lymph nodes: Axillary dissection vs sentinel node biopsy?
Evaluation of the axillary nodes is currently part of breast cancer staging and can help the clinician determine the need for adjuvant chemotherapy. It also may assist in assessing the need for extending the radiation field beyond the breast to include the regional lymph nodes. Patients with early stage (stage I and II) breast cancer who do not have abnormal palpable lymph nodes or biopsy-proven metastasis to axillary nodes qualify for sentinel lymph node (SLN) biopsy.
Sentinel node biopsy = less morbidity with no loss of accuracy. Compared with axillary lymph node dissection (ALND; removing all the level I and II nodes in the axilla), SLN biopsy has a 98% accuracy and is associated with less morbidity from lymphedema. The procedure involves injecting the breast with 2 tracers: a radioactive isotope, injected into the breast within 24 hours of the operation, and isosulfan blue dye, injected into the breast in the OR at the time of surgery (see illustration). Both tracers travel through the breast lymphatics and concentrate in the first few lymph nodes that drain the breast. The surgery is performed through a separate axillary incision, and the blue and radioactive lymph nodes are individually dissected and removed for pathologic evaluation. On average, 2 to 4 sentinel nodes are removed, including any suspicious palpable nodes. In experienced hands, this procedure has a false-negative rate of less than 5% to 10%.13
Axillary node dissection no longer standard of care. The indication for a completion ALND has changed based on the results of the randomized trial, ACOSOG Z0011.14 In this trial, patients with early stage breast cancer and 1 to 2 positive SLNs who were undergoing breast conservation therapy with radiation and adjuvant systemic therapy were randomly assigned to ALND or no ALND. (The trial did not include patients who were undergoing mastectomy, neoadjuvant chemotherapy, or who had more than 2 metastatic lymph nodes.) The investigators found no difference in overall or disease-free survival or local-regional recurrence between the 2 treatment groups over 9.2 years of follow up.14
Based on this practice-changing trial result, guidelines of the National Comprehensive Cancer Network no longer recommend completion ALND for patients who meet the ACOSOG Z0011 criteria. For patients who do not meet ACOSOG Z0011 criteria, we do intraoperative pathologic lymph node assessment with either frozen section or imprint cytology, and we perform immediate ALND when results are positive.
Indications for SLN biopsy include:
- invasive breast cancer with clinically negative axillary nodes
- ductal carcinoma in situ (DCIS) with microinvasion or extensive enough to require mastectomy
- clinically negative axillary nodes after neoadjuvant chemotherapy.
Contraindications for SLN biopsy include:
- bulky palpable lymphadenopathy
- pregnancy, as the safety of radioactive isotope and blue dye is not well studied; in isotope mapping the radiation dose is small and within safety limits for pregnant patients
- inflammatory breast cancer.
Complications of any axillary surgery may include risk of lymphedema (5% with SLN biopsy and 30% to 40% with ALND).15 Other complications include neuropathy of the affected arm with chronic pain and numbness of the skin.
Positive trends: Improved patient outcomes, specialized clinician training
Management of breast cancer has changed dramatically over the past several decades. More women are surviving breast cancer thanks to improvements in early detection, an individualized treatment approach with less aggressive surgery, and more effective targeted systemic therapies. A multidisciplinary, team-oriented approach with emphasis on minimally invasive biopsy and better cosmetic outcomes has enhanced quality of care.
Complexity in breast disease management has led to the development of formal fellowship training in breast surgical oncology. Studies have demonstrated that patients treated by high-volume breast surgeons are more satisfied with their care and have improved cancer outcomes.16,17 Women should be aware that they have different options for their breast cancer care, and surgeons with advanced specialization in this field may provide optimal results and better quality of care.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Nichols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–1569.
- Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer [published online ahead of print March 8, 2016]. Ann Surg. doi:10.1097/SLA.0000000000001698.
- Miller ME, Czechura T, Martz B, et al. Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Ann Surg Oncol. 2013;20(13):4113–4120.
- Zhang X, Zhang XJ, Zhang TY, et al. Effect and safety of dual anti-human epidermal growth factor receptor 2 therapy compared to monotherapy in patients with human epidermal growth factor receptor 2-positive breast cancer: a systematic review. BMC Cancer. 2014;14:625.
- Ahmed M, Rubio IT, Klaase JM, Douek M. Surgical treatment of nonpalpable primary invasive and in situ breast cancer. Nat Rev Clin Oncol. 2015;12(11):645–663.
- Ahmed M, Douek M. Intra-operative ultrasound versus wire-guided localization in the surgical management of non-palpable breast cancers: systemic review and meta-analysis. Breast Cancer Res Treat. 2013;140(3):435–446.
- Krekel NM, Haloua MH, Lopes Cardozo AM, et al. Intraoperative ultrasound guidance for palpable breast cancer excision (COBALT trial): a multicentre, randomised controlled trial. Lancet Oncol. 2013;14(1):48–54.
- Chakravorty A, Shrestha AK, Sanmugalingam N, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol. 2012;38(5):395–398.
- De Lorenzi F, Hubner G, Rotmensz N, et al. Oncological results of oncoplastic breast-conserving surgery: long term follow-up of a large series at a single institution: a matched-cohort analysis. Eur J Surg Oncol. 2016;42(1):71–77.
- De La Cruz L, Moody AM, Tappy EE, Blankenship AA, Hecht EM. Overall survival, disease-free survival, local recurrence, and nipple-areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol. 2015;22(10):3241–3249.
- Yao K, Liederbach E, Tang R, et al. Nipple-sparing mastectomy in BRCA1/2 mutation carriers: an interim analysis and review of the literature. Ann Surg Oncol. 2015;22(2):370–376.
- Fortunato L, Loreti A, Andrich R, et al. When mastectomy is needed: is the nipple-sparing procedure a new standard with very few contraindications? J Surg Oncol. 2013;108(4):207–212.
- Veronesi U, Viale G, Paganelli G, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg. 2010;251(4):595–600.
- Giuliano AE, Hunt K, Ballman KV, et al. Ten-year survival results of ACOSOG Z0011: a randomized trial of axillary node dissection in women with clinical T1-2 N0 M0 breast cancer who have a positive sentinel node (Alliance). In: 2016 ASCO Annual Meeting; June 3-7, 2016. J Clin Oncol. 2016;34(15; May 20 suppl): Abstract 1007.
- DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–515.
- Skinner KA, Helsper JT, Deapen D, Ye W, Sposto R. Breast cancer: do specialists make a difference? Ann Surg Oncol. 2003;10(6):606–615.
- Waljee JF, Hawley S, Alderman AK, Morrow M, Katz SJ. Patient satisfaction with treatment of breast cancer: does surgeon specialization matter? J Clin Oncol. 2007;25(24):3694–3698.
- Nichols HB, Berrington de Gonzalez A, Lacey JV Jr, Rosenberg PS, Anderson WF. Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol. 2011;29(12):1564–1569.
- Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer [published online ahead of print March 8, 2016]. Ann Surg. doi:10.1097/SLA.0000000000001698.
- Miller ME, Czechura T, Martz B, et al. Operative risks associated with contralateral prophylactic mastectomy: a single institution experience. Ann Surg Oncol. 2013;20(13):4113–4120.
- Zhang X, Zhang XJ, Zhang TY, et al. Effect and safety of dual anti-human epidermal growth factor receptor 2 therapy compared to monotherapy in patients with human epidermal growth factor receptor 2-positive breast cancer: a systematic review. BMC Cancer. 2014;14:625.
- Ahmed M, Rubio IT, Klaase JM, Douek M. Surgical treatment of nonpalpable primary invasive and in situ breast cancer. Nat Rev Clin Oncol. 2015;12(11):645–663.
- Ahmed M, Douek M. Intra-operative ultrasound versus wire-guided localization in the surgical management of non-palpable breast cancers: systemic review and meta-analysis. Breast Cancer Res Treat. 2013;140(3):435–446.
- Krekel NM, Haloua MH, Lopes Cardozo AM, et al. Intraoperative ultrasound guidance for palpable breast cancer excision (COBALT trial): a multicentre, randomised controlled trial. Lancet Oncol. 2013;14(1):48–54.
- Chakravorty A, Shrestha AK, Sanmugalingam N, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol. 2012;38(5):395–398.
- De Lorenzi F, Hubner G, Rotmensz N, et al. Oncological results of oncoplastic breast-conserving surgery: long term follow-up of a large series at a single institution: a matched-cohort analysis. Eur J Surg Oncol. 2016;42(1):71–77.
- De La Cruz L, Moody AM, Tappy EE, Blankenship AA, Hecht EM. Overall survival, disease-free survival, local recurrence, and nipple-areolar recurrence in the setting of nipple-sparing mastectomy: a meta-analysis and systematic review. Ann Surg Oncol. 2015;22(10):3241–3249.
- Yao K, Liederbach E, Tang R, et al. Nipple-sparing mastectomy in BRCA1/2 mutation carriers: an interim analysis and review of the literature. Ann Surg Oncol. 2015;22(2):370–376.
- Fortunato L, Loreti A, Andrich R, et al. When mastectomy is needed: is the nipple-sparing procedure a new standard with very few contraindications? J Surg Oncol. 2013;108(4):207–212.
- Veronesi U, Viale G, Paganelli G, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg. 2010;251(4):595–600.
- Giuliano AE, Hunt K, Ballman KV, et al. Ten-year survival results of ACOSOG Z0011: a randomized trial of axillary node dissection in women with clinical T1-2 N0 M0 breast cancer who have a positive sentinel node (Alliance). In: 2016 ASCO Annual Meeting; June 3-7, 2016. J Clin Oncol. 2016;34(15; May 20 suppl): Abstract 1007.
- DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–515.
- Skinner KA, Helsper JT, Deapen D, Ye W, Sposto R. Breast cancer: do specialists make a difference? Ann Surg Oncol. 2003;10(6):606–615.
- Waljee JF, Hawley S, Alderman AK, Morrow M, Katz SJ. Patient satisfaction with treatment of breast cancer: does surgeon specialization matter? J Clin Oncol. 2007;25(24):3694–3698.
In this Article
- Counseling patients on CPM
- Oncoplastic lumpectomy approach
- How to manage the lymph nodes