User login
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
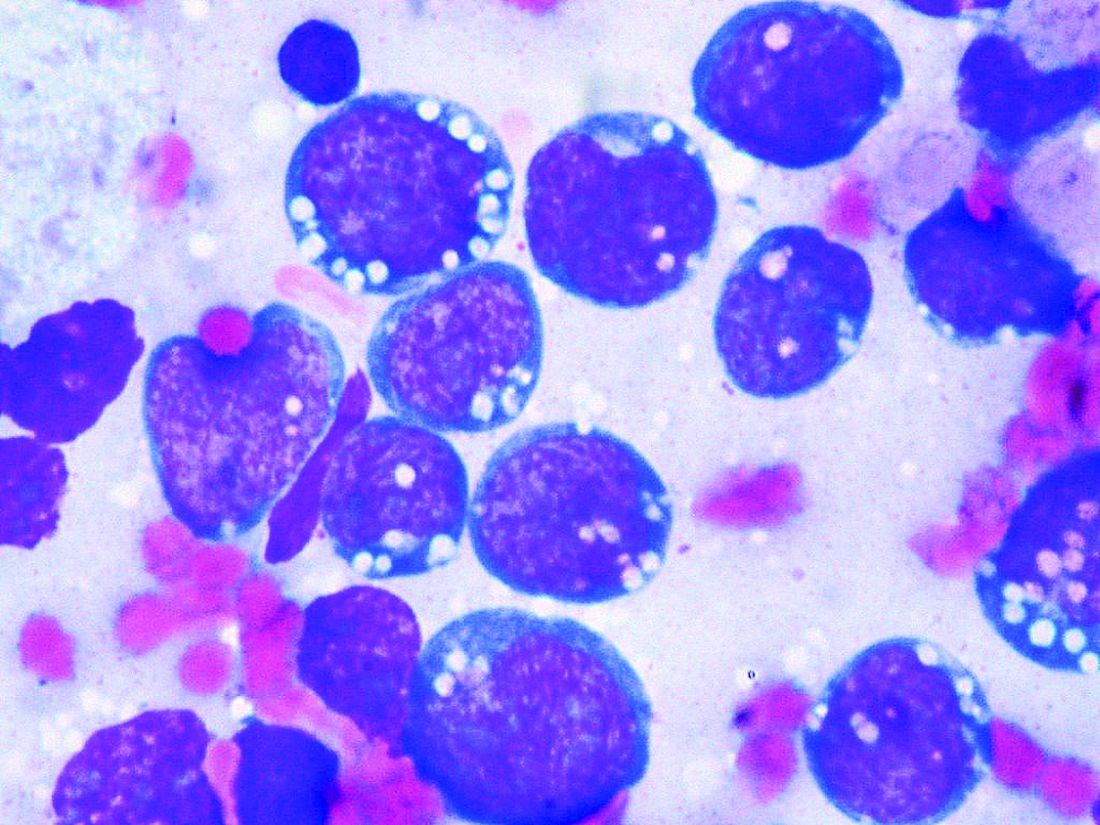
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
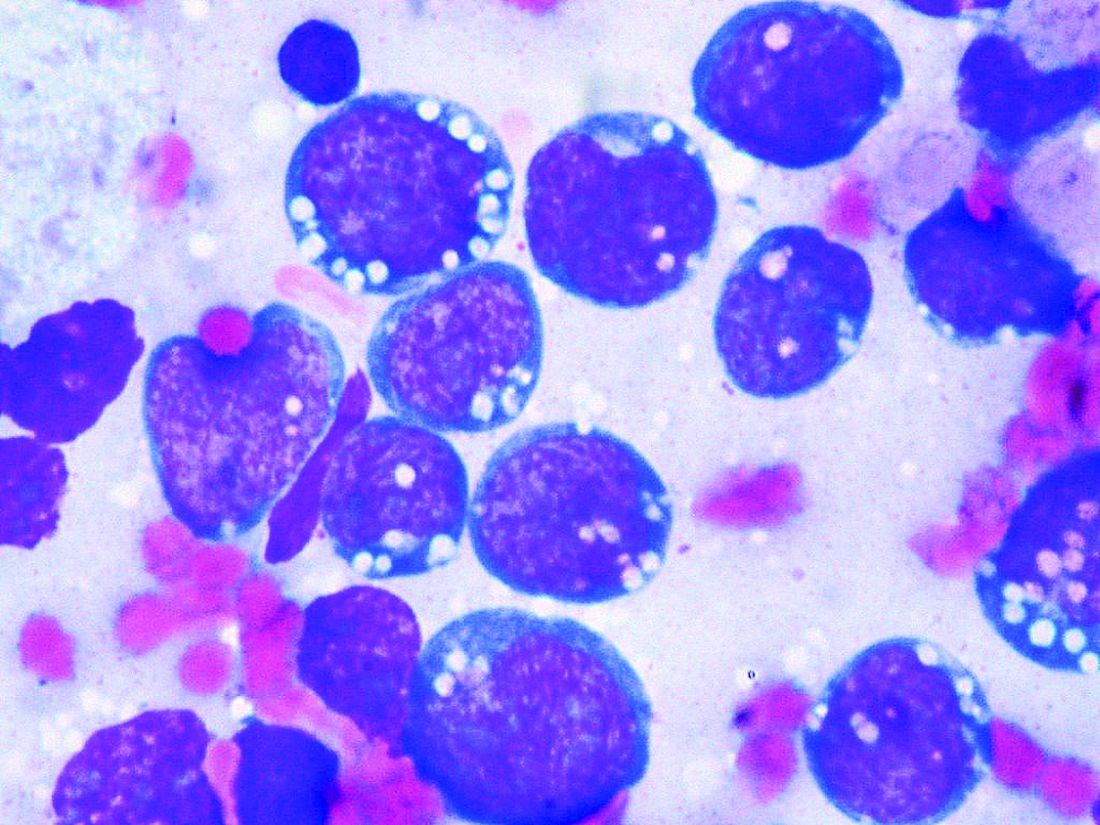
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Adult patients with Burkitt lymphoma can achieve equally sound survival outcomes with dose-adjusted chemotherapy versus high-intensity regimens, but can do so while avoiding the severe toxicities, U.S. study data shows.
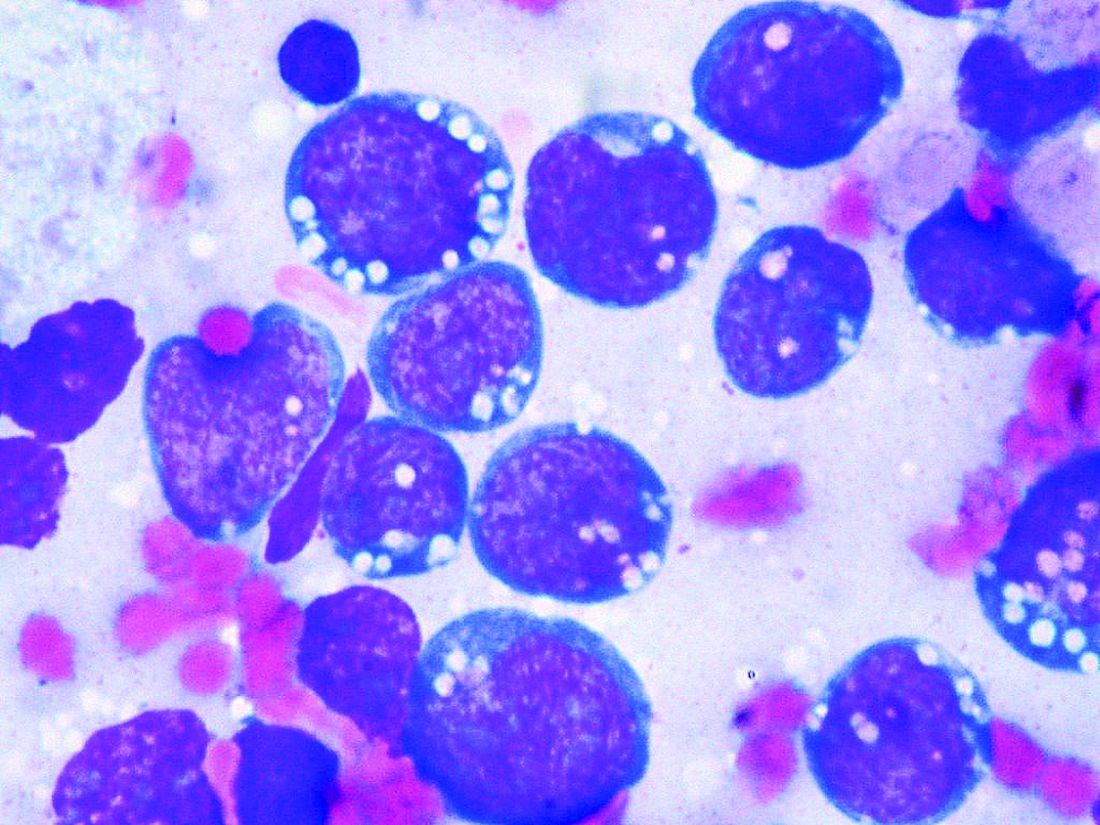
Although Burkitt lymphoma is the most common B-cell non-Hodgkin lymphoma in children, it accounts for only 1% to 2% of adult lymphoma cases.
Highly dose-intensive chemotherapy regimens, developed for children and young adults, have rendered the disease curable. But older patients in particular, and patients with comorbidities such as HIV, can suffer severe adverse effects, as well as late sequelae like second malignancies.
Mark Roschewski, MD, from the lymphoid malignancies branch at the National Cancer Institute in Bethesda, Md., and colleagues therefore examined whether a dose-adjusted regimen would maintain outcomes while reducing toxicities.
Tailoring treatment with etoposide, doxorubicin, and vincristine with prednisone, cyclophosphamide, and rituximab (EPOCH-R) to whether patients had high- or low-risk disease, they achieved 4-year survival rates of higher than 85%.
The research, published by the Journal of Clinical Oncology, also showed that patients taking the regimen, which was well tolerated, had low rates of relapse in the central nervous system.
The team reports that their results with the dose-adjusted regimen “significantly improve on the complexity, cost, and toxicity profile of other regimens,” also highlighting that it is administered on an outpatient basis.
As the outcomes also “compare favorably” with those with high intensity regimens, they say the findings “support our treatment strategies to ameliorate toxicity while maintaining efficacy.”
Importantly, they suggest highly dose-intensive chemotherapy is unnecessary for cure, and carefully defined low-risk patients may be treated with limited chemotherapy.
Dr. Roschewski said in an interview that, in patients aged 40 years and older, dose-adjusted EPOCH-R is “probably the preferred choice,” despite its “weakness” in controlling the disease in patients with active CNS involvement.
However, the “real question” is what to use in younger patients, Dr. Roschewski said, as the “unknown” is whether the additional magnitude of a high-intensity regimen that “gets into the CNS” outweighs the risk of toxicities.
“What was important about our study,” he said, was that patients with CNS involvement “did the worst but it was equally split among patients that died of toxicity and patients that progressed.”
In other words, each choice increases one risk while decreasing another. “So I would have to have that discussion with the patient, and individual patient decisions are typically based on the details,” said Dr. Roschewski.
One issue, however, that could limit the adoption of dose-adjusted EPOCH-R is that, without a randomized study comparing it directly with a high-intensity regimen, clinicians may to stick to what they know.
Dr. Roschewski said that “this is particularly true of more experienced clinicians.”
“They’re less likely, I think, to adopt something else outside of a randomized study because our natural inclination with this disease has always been dose intensity is critical. ... This is a dogma, and to shift from that probably does require a higher level of evidence, at least for some practitioners,” he explained.
Further study details
Following a pilot study of dose-adjusted EPOCH-R in 30 adult patients in which the authors say the regimen showed “high efficacy,” they enrolled 113 patients with untreated Burkitt lymphoma at 22 centers between June 2010 and May 2017.
The patients were divided into low-risk and high-risk categories, with low-risk defined as stage 1 or 2 disease, normal lactate dehydrogenase levels, ECOG performance status ≤ 1, and no tumor mass ≥ 7 cm.
High-risk patients were given six cycles of dose-adjusted EPOCH-R (with rituximab on day 1 only) along with CNS prophylaxis or active therapy with intrathecal methotrexate.
In contrast, low-risk patients were given two cycles of dose-adjusted EPOCH-R, with rituximab on days 1 and 5, followed by positron emission tomography.
If that was negative, the patients had one additional treatment cycle and no CNS prophylaxis, but if it was positive, they were given four additional cycles, plus intrathecal methotrexate.
Of the 113 patients enrolled, 79% were male, median age was 49 years, and 62% were aged at least 40 years, including 26% aged at least 60 years.
The team determined that 13% of the patients were of low risk, 87% were high risk, and 11% had cerebrospinal fluid involvement. One-quarter (24.7%) were HIV positive, with a median CD4+ T-cell count of 268 cells/mm3.
The majority (87%) of low-risk patients received three treatment cycles, and 82% of high-risk patents were administered six treatment cycles.
Over a median follow-up of 58.7 months (4.9 years), the 4-year event-free survival (EFS) rate across the whole cohort was 84.5% and overall survival was 87%.
At the time of analysis, all low-risk patients were in remission; among high-risk patients, the 4-year EFS was 82.1% and overall survival was 84.9%.
The team reports that treatment was equally effective across age groups, and irrespective of HIV status and International Prognostic Index risk group.
Only 2% of high-risk patients with no pretreatment evidence of CNS involvement had relapses in the brain parenchyma. Just over half (55%) of patients with cerebrospinal fluid involvement at presentation experienced disease progression or died.
Five patients died of treatment-related toxicity. Grade 3/4 thrombocytopenia occurred during 17% of cycles, and febrile neutropenia was seen during 16%. Tumor lysis syndrome was rare, occurring in 5% of patients.
Next, the researchers are planning on focusing on CNS disease, looking at EPOCH-R as the backbone and adding intrathecal methotrexate and an additional targeted agent with known CNS penetration.
Dr. Roschewski said that is “a very attractive strategy and ... we will initiate enrollment in that study probably in the next couple of months here at the NCI,” he added, noting that it will be an early phase 1 study.
Another issue he identified that “doesn’t get spoken about quite as much but I do think is important is potentially working on supportive care guidelines for how we manage these patients.” Dr. Roschewski explained, “One of the things you see over and over in these Burkitt lymphoma studies is that some patients don’t make it through therapy because they’re so sick at the beginning, and they have certain risks.
“I think simply improving that type of care, independent of what regimen is used, can potentially improve the outcomes across patient groups.”
The study was funded by the National Cancer Institute, National Institutes of Health, AIDS Malignancy Consortium, and the Cancer Therapy Evaluation Program and Lymphoid Malignancies Branch. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.