User login
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
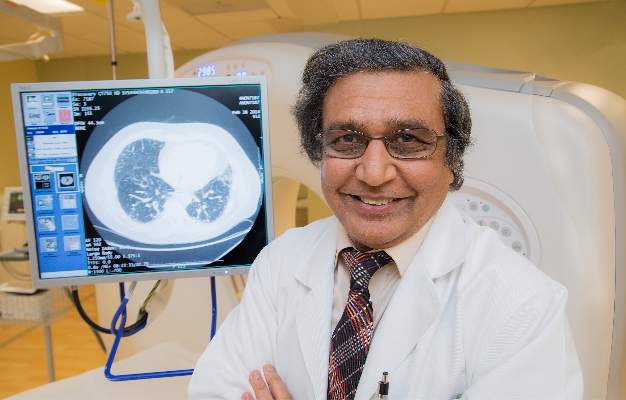
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
The new IPF guidelines set a critical framework for the path forward. The international task force that formulated the 2015 update of the clinical practice guidelines for IPF have done tremendous work, moving much further toward answering the kinds of questions that the research and clinical community will not be able to address unless they work together. These guidelines are a critical appraisal of where we are and of the need to push forward.

|
Dr. Gregory P. Cosgrove |
As we push as fast as we can toward more and better treatments, we should be aware that care of IPF patients should be multifaceted, and not just pharmacologic. In order to address the suffering associated with this disease, we need to use all available modalities: supplemental oxygen; physical therapy; and psychological support. We can help patients in so many different ways; lung fibrosis is a heterogeneous disease, and by focusing on how individual patients are affected, we can help meet their needs. The fund of available knowledge has been addressed in an evidence-based fashion. Unfortunately, this is the state of affairs; however, now we can begin to answer the questions that need to be answered.
Dr. Gregory P. Cosgrove is the chief medical officer of the Pulmonary Fibrosis Foundation and holds the endowed chair of interstitial lung disease at National Jewish Health in Denver. His comments are summarized from an interview.
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
Idiopathic pulmonary fibrosis patients and physicians have two new medication choices but fewer options among established treatments, according to updated clinical practice guidelines published by an international working group. The update of the 2011 guidelines was released by the American Thoracic Society in conjunction with the European Respiratory Society, the Japanese Respiratory Society, and the Latin American Thoracic Association.
The tyrosine kinase inhibitor nintedanib (Ofev) received a conditional recommendation for use in idiopathic pulmonary fibrosis (IPF), a progressive, restrictive lung disorder characterized by increasing fibrosis and findings of usual interstitial pneumonia on CT scan. Pirfenidone (Esbriet), an orally administered pleiotropic antifibrotic medication, also received a conditional positive recommendation in the guidelines (Am J Respir Crit Care Med. 2015;192[2]:e3-19), which were formulated by a panel led by first author Dr. Ganesh Raghu of the University of Washington, Seattle.
Antacid therapy to reduce the potentially harmful effects of microaspiration of acidic stomach contents from gastroesophageal reflux received a conditional positive recommendation. Abnormal gastroesophageal reflux occurs in up to 90% of IPF patients, according to Dr. Raghu and his coauthors.
No other treatments show efficacy when rigorously examined, Dr. Raghu said. “We haven’t shown that any treatment regimen affects how patients feel or function. We haven’t improved survivability or quality of life.”
Dr. Raghu and the guideline coauthors issued a strong recommendation against use of prednisone, azathioprine, and N-acetylcysteine as triple therapy, noting “a clear negative effect…for multiple patient–important outcomes” in a trial that was stopped early for harm. In discussion, they recommended revisiting the diagnosis in instances where IPF patients seem to be receiving benefit from triple therapy.
The use of N-acetylcysteine as monotherapy for IPF showed no improvement in mortality, lung function studies, or quality of life in three studies, although two studies showed improvement on the 6-minute walk test. Dr. Raghu and his coauthors thus issued a conditional recommendation against using N-acetylcysteine as monotherapy.
The 2015 clinical practice guidelines also strengthened the recommendation against using warfarin for anticoagulation to treat IPF; Warfarin had received a conditional recommendation against treatment in the previous guidelines released in 2011. Although studies provide “biological plausibility for a mechanistic link between thrombosis and lung fibrosis,” Dr. Raghu and his coauthors noted increased mortality and no improvement in lung function in some studies comparing warfarin with placebo as an IPF treatment. However, warfarin should still be used as clinically indicated in patients with other indications for its use as an anticoagulant.
Endothelin receptors (ERs) can promote epithelial to mesenchymal transition via cytokine mediators, a process associated with organ fibrosis. Thus, ER antagonists have been studied to treat IPF. Ambrisentan (Letairis) is a selective ER type-A antagonist that, in a single, randomized, controlled trial, was associated with worsening respiratory function and increased mortality. The guidelines thus strongly recommend against the use of ambrisentan for IPF.
The dual-acting ER antagonists bosentan (Tracleer) and macitentan (Opsumit) target both ER-A and ER-B sites and were examined together in the guidelines. Dr. Raghu and his coauthors pooled results of three studies examining one or the other of the two dual-acting ER antagonists, finding no overall effect on mortality but a small improvement in the composite outcome of death or disease; they issued a conditional recommendation against using either bosentan or macitentan. For the subset of IPF patients with pulmonary hypertension (PH), “[t]he committee felt that patients with PH secondary to IPF might benefit … however, the evidence did not allow a specific subgroup recommendation.”
Sildenafil (Revatio) is a phosphodiesterase-5 inhibitor that has been used in patients with PH and right ventricular dysfunction; however, in the limited data available for its use in patients with IPF, no benefit on mortality, dyspnea, or IPF exacerbations was seen. There was a slight benefit on quality of life, but Dr. Raghu and his fellow committee members gave sildenafil a qualified negative recommendation. No specific subgroup recommendations were made for patients with PH and/or right ventricular dysfunction.
Finally, Dr. Raghu and his coauthors did not make a recommendation regarding single, compared with bilateral, lung transplantation for individuals with moderate or severe IPF. “The shortage of organs is a universal problem, and the decision to give bilateral lung transplantation to a single patient rather than give single-lung transplantation to two patients, including the effect on health inequity, must be considered,” they said, calling for randomized, controlled trials to address the question.
“Evidence surrounding the clinical management of IPF is rapidly evolving,” Dr. Raghu and his coauthors said; accordingly, they envision the guideline as a “ ‘living document,’ allowing new evidence to be incorporated as available.”
The authors of the guidelines followed a strict protocol to recuse themselves from deliberation or voting when conflicts existed. Dr. Raghu said, “The non-IPF experts were able to make unbiased recommendations.”
A patient with IPF, William Cunningham, was also a fully involved panel member, bringing his perspective into the guideline formation process. “Mr. Cunningham was incredible and he was a gentleman and a scholar. When he spoke, everyone just listened, and his input was always well thought out. He really was instrumental in the guideline-development process.” Mr. Cunningham died from his disease shortly after the committee’s work was completed. The full list of conflicts of interest and a detailed protocol description may be found in the full text of the guidelines.
On Twitter @karioakes
FROM THE AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE