User login
A 63-year-old morbidly obese man presented to our clinic with a non-healing, slowly growing, painless ulcer on his right shin that he’d had for one year. It was not actively bleeding or draining, but the scab had come off one month earlier and the wound did not close. The patient denied any trauma to the area or foreign travel. Bacitracin and triamcinolone creams hadn’t helped.
Our patient’s medical history included diabetes, hypertension, hyperlipidemia, and worsening venous insufficiency. He was not currently using compression stockings, but they had helped him in the past.
On examination, we noted a 3 x 3.5 cm well-demarcated, somewhat geometric, clean-based ulceration on the patient’s right medial shin (FIGURE 1A). There was no significant erythema, purulence, tenderness, warmth, or drainage of the ulcer. The base had seemingly normal granulation tissue. Woody induration, verrucous plaques, and confluent erythematous, violaceous, indurated patches were adjacent to the ulcer (FIGURE 1B). The patient also had severe pitting edema on his lower legs.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infiltrative basal cell carcinoma
In addition to our patient’s history of venous insufficiency, he’d also had a melanoma removed from his right shoulder 6 years earlier, and a basal cell carcinoma (BCC) removed from his upper back 2 years earlier. The chronic, non-healing nature of the ulcer prompted us to perform a punch biopsy, which revealed infiltrative BCC. We also did a wound culture, which showed a secondary infection with methicillin-resistant Staphylococcus aureus (MRSA). The verrucous plaques next to the ulcer were the result of chronic venous stasis and lymphedema.
BCC is the most common type of cancer, estimated to comprise 80% of all skin cancers.1 It typically presents on the head and neck, but can occur in other locations. Eight percent of BCCs occur on the legs.2,3 Lower extremity BCC is more common in women, likely due to increased ultraviolet radiation exposure.2,4
BCC presents as erythematous and pearly macules, papules, nodules, ulcers, or scars, and can be pigmented. It may appear as a crusted ulcer (known as a “rodent ulcer”) with a rolled, translucent border and telangiectases.5 There are 5 major histologic subtypes of BCC: nodular, micronodular, superficial, morpheaform, and infiltrative.1,5 Infiltrative BCCs are an invasive subtype1,5 and may be more commonly associated with severe venous stasis,3 as was the case with our patient.
Although considered uncommon, squamous cell carcinoma (SCC) and BCC have been discovered in chronic leg ulcers.4,6 In fact, one report suggests that as many as 10% of chronic leg ulcers are malignant (31% BCC, 56% SCC).7 Thus, it is important to maintain a high index of suspicion for malignancy in chronic leg ulcers.
Ulcerating BCC can mimic other types of leg ulcers
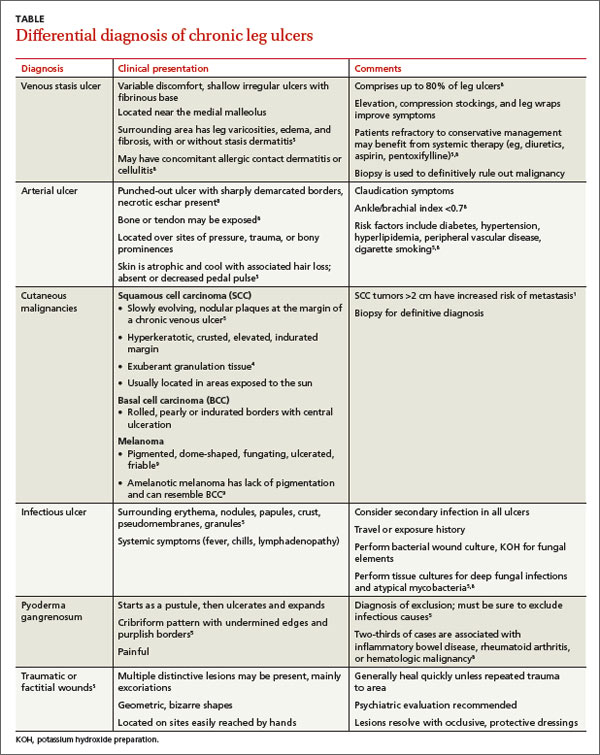
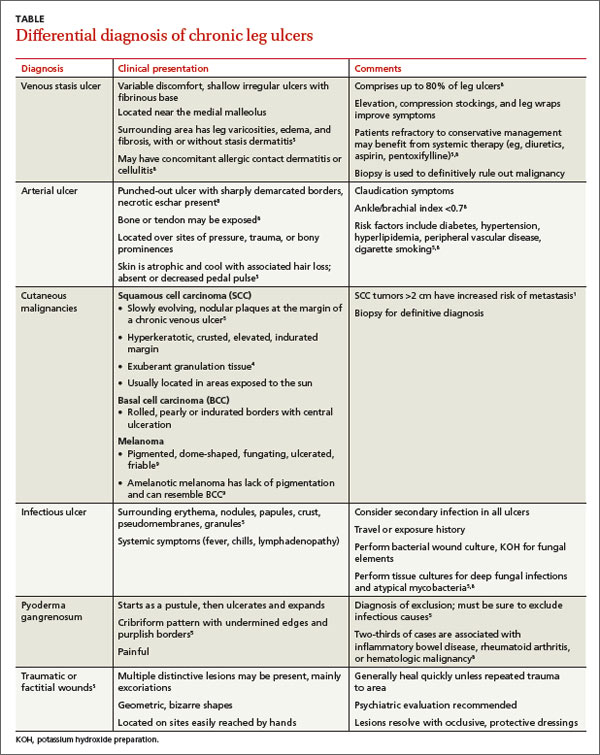
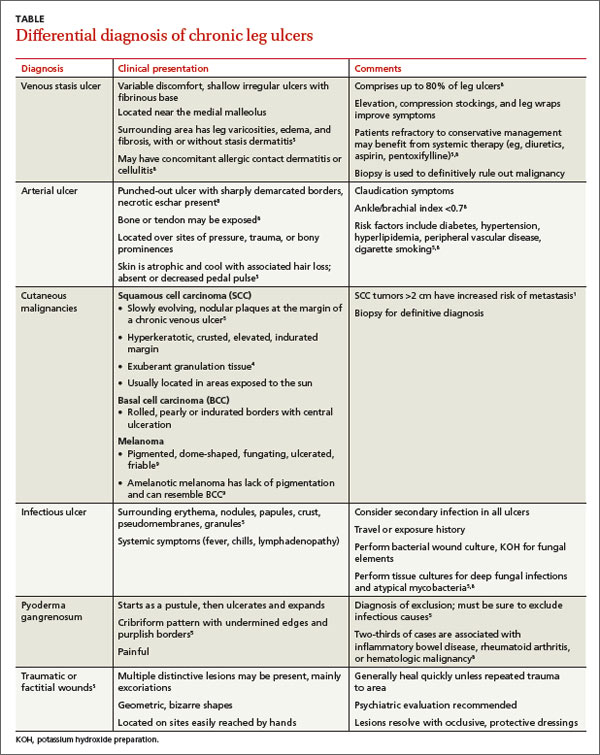
The differential diagnosis of a chronic leg ulcer includes venous or arterial ulcers, malignancies (SCC, BCC, lymphoma, melanoma), infectious ulcers (bacterial, deep fungal), pyoderma gangrenosum, and traumatic or factitial wounds (TABLE).1,4,5,8,9
Consider biopsy for ulcers that don't respond to treatment
The diagnosis of BCC in a leg ulcer is confirmed histologically. A punch or incisional biopsy should be taken at the edge of the ulcer, including the base.5,6 (For a Watch & Learn video that demonstrates how to perform a punch biopsy, go to http://bit.ly/punch_biopsy.) Providers may be concerned that biopsies could worsen a chronic wound; however, biopsy sites usually heal with no substantial complications.2,6,7 There are no guidelines on when to biopsy an ulcer, but it is reasonable to biopsy a leg ulcer that has not responded to 3 months of conservative treatment.2,7
Factors associated with malignancy in chronic leg ulcers include older age, abnormal excessive granulation tissue at wound edges, high clinical suspicion of cancer, and number of previous biopsies.7 The size and duration of the ulcer do not directly correlate with malignancy.7 The threshold for performing a diagnostic biopsy in a chronic leg ulcer should be lower for a patient who has any of the risk factors noted above. Be aware that ulcerating skin cancers may lack the classic appearance of typical skin cancers.6
For most BCCs, surgical excision will be required
Each BCC must be thoroughly evaluated for size, location, and histologic subtype. Surgical excision is the preferred treatment in most cases.5 Indications for Mohs micrographic surgery include skin cancers with aggressive histologic subtypes, such as infiltrative BCC, and tumors larger than 2 cm that are located on the extremities.1,5 Due to the limited amount of excess skin on the lower leg, skin flaps or grafts may be required.
Electrodessication and curettage, topical therapy with 5% imiquimod or 5-fluorouracil, and cryotherapy are reserved for certain low-risk superficial and nodular BCCs.1,5 Radiation therapy is an option for tumors that are not amenable to surgery. Treatment is tailored to the patient’s needs based on age, medical history, and the characteristics of the skin cancer.
Inadequate treatment of BCCs can result in recurrences, which may appear 4 to 12 months after treatment.5 Close followup with regular full body skin exams is indicated.
Our patient was treated with Bactrim DS (800 mg sulfamethoxazole and 160 mg trimethoprim) one tablet PO BID for 10 days and acetic acid soaks for the MRSA. While it was clear that the patient needed Mohs surgery, it was important to first address his lower extremity edema. He was evaluated by a vascular surgeon and resumed using compression stockings regularly.
The patient then underwent Mohs surgery.
After 2 stages of the surgery, the patient’s ulcer healed partially by secondary intention. After 5 months, the ulcer was covered with a split-thickness skin graft. Nine months after diagnosis, the patient had no clinical recurrence.
Physicians subsequently identified 2 BCCs on his face and scalp that were also treated with Mohs surgery. Our patient continues to have regular skin examinations.
CORRESPONDENCE
Jane Hwang, MD, Capt, USAF, MC, Kunsan Air Base, PSC 2 Box 205, APO, AP 96264; [email protected]
1. Firnhaber JM. Diagnosis and treatment of Basal cell carcinoma and squamous cell carcinoma. Am Fam Physician. 2012;86:161-168.
2. Phillips TJ, Salman SM, Rogers GS. Nonhealing leg ulcers: a manifestation of basal cell carcinoma. J Am Acad Dermatol. 1991;25;47-49.
3. Lutz ME, Davis MD, Otley CC. Infiltrating basal cell carcinoma in the setting of a venous ulcer. Int J Dermatol. 2000;39:519-520.
4. Jankovic A, Binic I, Ljubenovic M. Basal cell carcinoma is not granulation tissue in the venous leg ulcer. Int J Low Extrem Wounds. 2008;7:182-184.
5. James WD, Berger TG, Elston DM. Chapter 29. Epidermal nevi, neoplasms, and cysts. In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin Clinical Dermatology. 11th ed. Philadelphia, PA: Elsevier, Inc; 2011.
6. Yang D, Morrison BD, Vandongen YK, et al. Malignancy in chronic leg ulcers. Med J Aust. 1996;164:718-720.
7. Senet P, Combemale P, Debure C, et al; Angio-Dermatology Group Of The French Society Of Dermatology. Malignancy and chronic leg ulcers: the value of systematic wound biopsies: a prospective, multicenter, cross-sectional study. Arch Dermatol. 2012;148:704-708.
8. Valencia IC, Falabella A, Kirsner RS, et al. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol. 2001;44:401-421.
9. James WD, Berger TG, Elston DM. Chapter 30. Melanocytic nevi and neoplasms. In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin Clinical Dermatology. 11th ed. Philadelphia, PA: Elsevier, Inc; 2011.
A 63-year-old morbidly obese man presented to our clinic with a non-healing, slowly growing, painless ulcer on his right shin that he’d had for one year. It was not actively bleeding or draining, but the scab had come off one month earlier and the wound did not close. The patient denied any trauma to the area or foreign travel. Bacitracin and triamcinolone creams hadn’t helped.
Our patient’s medical history included diabetes, hypertension, hyperlipidemia, and worsening venous insufficiency. He was not currently using compression stockings, but they had helped him in the past.
On examination, we noted a 3 x 3.5 cm well-demarcated, somewhat geometric, clean-based ulceration on the patient’s right medial shin (FIGURE 1A). There was no significant erythema, purulence, tenderness, warmth, or drainage of the ulcer. The base had seemingly normal granulation tissue. Woody induration, verrucous plaques, and confluent erythematous, violaceous, indurated patches were adjacent to the ulcer (FIGURE 1B). The patient also had severe pitting edema on his lower legs.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infiltrative basal cell carcinoma
In addition to our patient’s history of venous insufficiency, he’d also had a melanoma removed from his right shoulder 6 years earlier, and a basal cell carcinoma (BCC) removed from his upper back 2 years earlier. The chronic, non-healing nature of the ulcer prompted us to perform a punch biopsy, which revealed infiltrative BCC. We also did a wound culture, which showed a secondary infection with methicillin-resistant Staphylococcus aureus (MRSA). The verrucous plaques next to the ulcer were the result of chronic venous stasis and lymphedema.
BCC is the most common type of cancer, estimated to comprise 80% of all skin cancers.1 It typically presents on the head and neck, but can occur in other locations. Eight percent of BCCs occur on the legs.2,3 Lower extremity BCC is more common in women, likely due to increased ultraviolet radiation exposure.2,4
BCC presents as erythematous and pearly macules, papules, nodules, ulcers, or scars, and can be pigmented. It may appear as a crusted ulcer (known as a “rodent ulcer”) with a rolled, translucent border and telangiectases.5 There are 5 major histologic subtypes of BCC: nodular, micronodular, superficial, morpheaform, and infiltrative.1,5 Infiltrative BCCs are an invasive subtype1,5 and may be more commonly associated with severe venous stasis,3 as was the case with our patient.
Although considered uncommon, squamous cell carcinoma (SCC) and BCC have been discovered in chronic leg ulcers.4,6 In fact, one report suggests that as many as 10% of chronic leg ulcers are malignant (31% BCC, 56% SCC).7 Thus, it is important to maintain a high index of suspicion for malignancy in chronic leg ulcers.
Ulcerating BCC can mimic other types of leg ulcers
The differential diagnosis of a chronic leg ulcer includes venous or arterial ulcers, malignancies (SCC, BCC, lymphoma, melanoma), infectious ulcers (bacterial, deep fungal), pyoderma gangrenosum, and traumatic or factitial wounds (TABLE).1,4,5,8,9
Consider biopsy for ulcers that don't respond to treatment
The diagnosis of BCC in a leg ulcer is confirmed histologically. A punch or incisional biopsy should be taken at the edge of the ulcer, including the base.5,6 (For a Watch & Learn video that demonstrates how to perform a punch biopsy, go to http://bit.ly/punch_biopsy.) Providers may be concerned that biopsies could worsen a chronic wound; however, biopsy sites usually heal with no substantial complications.2,6,7 There are no guidelines on when to biopsy an ulcer, but it is reasonable to biopsy a leg ulcer that has not responded to 3 months of conservative treatment.2,7
Factors associated with malignancy in chronic leg ulcers include older age, abnormal excessive granulation tissue at wound edges, high clinical suspicion of cancer, and number of previous biopsies.7 The size and duration of the ulcer do not directly correlate with malignancy.7 The threshold for performing a diagnostic biopsy in a chronic leg ulcer should be lower for a patient who has any of the risk factors noted above. Be aware that ulcerating skin cancers may lack the classic appearance of typical skin cancers.6
For most BCCs, surgical excision will be required
Each BCC must be thoroughly evaluated for size, location, and histologic subtype. Surgical excision is the preferred treatment in most cases.5 Indications for Mohs micrographic surgery include skin cancers with aggressive histologic subtypes, such as infiltrative BCC, and tumors larger than 2 cm that are located on the extremities.1,5 Due to the limited amount of excess skin on the lower leg, skin flaps or grafts may be required.
Electrodessication and curettage, topical therapy with 5% imiquimod or 5-fluorouracil, and cryotherapy are reserved for certain low-risk superficial and nodular BCCs.1,5 Radiation therapy is an option for tumors that are not amenable to surgery. Treatment is tailored to the patient’s needs based on age, medical history, and the characteristics of the skin cancer.
Inadequate treatment of BCCs can result in recurrences, which may appear 4 to 12 months after treatment.5 Close followup with regular full body skin exams is indicated.
Our patient was treated with Bactrim DS (800 mg sulfamethoxazole and 160 mg trimethoprim) one tablet PO BID for 10 days and acetic acid soaks for the MRSA. While it was clear that the patient needed Mohs surgery, it was important to first address his lower extremity edema. He was evaluated by a vascular surgeon and resumed using compression stockings regularly.
The patient then underwent Mohs surgery.
After 2 stages of the surgery, the patient’s ulcer healed partially by secondary intention. After 5 months, the ulcer was covered with a split-thickness skin graft. Nine months after diagnosis, the patient had no clinical recurrence.
Physicians subsequently identified 2 BCCs on his face and scalp that were also treated with Mohs surgery. Our patient continues to have regular skin examinations.
CORRESPONDENCE
Jane Hwang, MD, Capt, USAF, MC, Kunsan Air Base, PSC 2 Box 205, APO, AP 96264; [email protected]
A 63-year-old morbidly obese man presented to our clinic with a non-healing, slowly growing, painless ulcer on his right shin that he’d had for one year. It was not actively bleeding or draining, but the scab had come off one month earlier and the wound did not close. The patient denied any trauma to the area or foreign travel. Bacitracin and triamcinolone creams hadn’t helped.
Our patient’s medical history included diabetes, hypertension, hyperlipidemia, and worsening venous insufficiency. He was not currently using compression stockings, but they had helped him in the past.
On examination, we noted a 3 x 3.5 cm well-demarcated, somewhat geometric, clean-based ulceration on the patient’s right medial shin (FIGURE 1A). There was no significant erythema, purulence, tenderness, warmth, or drainage of the ulcer. The base had seemingly normal granulation tissue. Woody induration, verrucous plaques, and confluent erythematous, violaceous, indurated patches were adjacent to the ulcer (FIGURE 1B). The patient also had severe pitting edema on his lower legs.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infiltrative basal cell carcinoma
In addition to our patient’s history of venous insufficiency, he’d also had a melanoma removed from his right shoulder 6 years earlier, and a basal cell carcinoma (BCC) removed from his upper back 2 years earlier. The chronic, non-healing nature of the ulcer prompted us to perform a punch biopsy, which revealed infiltrative BCC. We also did a wound culture, which showed a secondary infection with methicillin-resistant Staphylococcus aureus (MRSA). The verrucous plaques next to the ulcer were the result of chronic venous stasis and lymphedema.
BCC is the most common type of cancer, estimated to comprise 80% of all skin cancers.1 It typically presents on the head and neck, but can occur in other locations. Eight percent of BCCs occur on the legs.2,3 Lower extremity BCC is more common in women, likely due to increased ultraviolet radiation exposure.2,4
BCC presents as erythematous and pearly macules, papules, nodules, ulcers, or scars, and can be pigmented. It may appear as a crusted ulcer (known as a “rodent ulcer”) with a rolled, translucent border and telangiectases.5 There are 5 major histologic subtypes of BCC: nodular, micronodular, superficial, morpheaform, and infiltrative.1,5 Infiltrative BCCs are an invasive subtype1,5 and may be more commonly associated with severe venous stasis,3 as was the case with our patient.
Although considered uncommon, squamous cell carcinoma (SCC) and BCC have been discovered in chronic leg ulcers.4,6 In fact, one report suggests that as many as 10% of chronic leg ulcers are malignant (31% BCC, 56% SCC).7 Thus, it is important to maintain a high index of suspicion for malignancy in chronic leg ulcers.
Ulcerating BCC can mimic other types of leg ulcers
The differential diagnosis of a chronic leg ulcer includes venous or arterial ulcers, malignancies (SCC, BCC, lymphoma, melanoma), infectious ulcers (bacterial, deep fungal), pyoderma gangrenosum, and traumatic or factitial wounds (TABLE).1,4,5,8,9
Consider biopsy for ulcers that don't respond to treatment
The diagnosis of BCC in a leg ulcer is confirmed histologically. A punch or incisional biopsy should be taken at the edge of the ulcer, including the base.5,6 (For a Watch & Learn video that demonstrates how to perform a punch biopsy, go to http://bit.ly/punch_biopsy.) Providers may be concerned that biopsies could worsen a chronic wound; however, biopsy sites usually heal with no substantial complications.2,6,7 There are no guidelines on when to biopsy an ulcer, but it is reasonable to biopsy a leg ulcer that has not responded to 3 months of conservative treatment.2,7
Factors associated with malignancy in chronic leg ulcers include older age, abnormal excessive granulation tissue at wound edges, high clinical suspicion of cancer, and number of previous biopsies.7 The size and duration of the ulcer do not directly correlate with malignancy.7 The threshold for performing a diagnostic biopsy in a chronic leg ulcer should be lower for a patient who has any of the risk factors noted above. Be aware that ulcerating skin cancers may lack the classic appearance of typical skin cancers.6
For most BCCs, surgical excision will be required
Each BCC must be thoroughly evaluated for size, location, and histologic subtype. Surgical excision is the preferred treatment in most cases.5 Indications for Mohs micrographic surgery include skin cancers with aggressive histologic subtypes, such as infiltrative BCC, and tumors larger than 2 cm that are located on the extremities.1,5 Due to the limited amount of excess skin on the lower leg, skin flaps or grafts may be required.
Electrodessication and curettage, topical therapy with 5% imiquimod or 5-fluorouracil, and cryotherapy are reserved for certain low-risk superficial and nodular BCCs.1,5 Radiation therapy is an option for tumors that are not amenable to surgery. Treatment is tailored to the patient’s needs based on age, medical history, and the characteristics of the skin cancer.
Inadequate treatment of BCCs can result in recurrences, which may appear 4 to 12 months after treatment.5 Close followup with regular full body skin exams is indicated.
Our patient was treated with Bactrim DS (800 mg sulfamethoxazole and 160 mg trimethoprim) one tablet PO BID for 10 days and acetic acid soaks for the MRSA. While it was clear that the patient needed Mohs surgery, it was important to first address his lower extremity edema. He was evaluated by a vascular surgeon and resumed using compression stockings regularly.
The patient then underwent Mohs surgery.
After 2 stages of the surgery, the patient’s ulcer healed partially by secondary intention. After 5 months, the ulcer was covered with a split-thickness skin graft. Nine months after diagnosis, the patient had no clinical recurrence.
Physicians subsequently identified 2 BCCs on his face and scalp that were also treated with Mohs surgery. Our patient continues to have regular skin examinations.
CORRESPONDENCE
Jane Hwang, MD, Capt, USAF, MC, Kunsan Air Base, PSC 2 Box 205, APO, AP 96264; [email protected]
1. Firnhaber JM. Diagnosis and treatment of Basal cell carcinoma and squamous cell carcinoma. Am Fam Physician. 2012;86:161-168.
2. Phillips TJ, Salman SM, Rogers GS. Nonhealing leg ulcers: a manifestation of basal cell carcinoma. J Am Acad Dermatol. 1991;25;47-49.
3. Lutz ME, Davis MD, Otley CC. Infiltrating basal cell carcinoma in the setting of a venous ulcer. Int J Dermatol. 2000;39:519-520.
4. Jankovic A, Binic I, Ljubenovic M. Basal cell carcinoma is not granulation tissue in the venous leg ulcer. Int J Low Extrem Wounds. 2008;7:182-184.
5. James WD, Berger TG, Elston DM. Chapter 29. Epidermal nevi, neoplasms, and cysts. In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin Clinical Dermatology. 11th ed. Philadelphia, PA: Elsevier, Inc; 2011.
6. Yang D, Morrison BD, Vandongen YK, et al. Malignancy in chronic leg ulcers. Med J Aust. 1996;164:718-720.
7. Senet P, Combemale P, Debure C, et al; Angio-Dermatology Group Of The French Society Of Dermatology. Malignancy and chronic leg ulcers: the value of systematic wound biopsies: a prospective, multicenter, cross-sectional study. Arch Dermatol. 2012;148:704-708.
8. Valencia IC, Falabella A, Kirsner RS, et al. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol. 2001;44:401-421.
9. James WD, Berger TG, Elston DM. Chapter 30. Melanocytic nevi and neoplasms. In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin Clinical Dermatology. 11th ed. Philadelphia, PA: Elsevier, Inc; 2011.
1. Firnhaber JM. Diagnosis and treatment of Basal cell carcinoma and squamous cell carcinoma. Am Fam Physician. 2012;86:161-168.
2. Phillips TJ, Salman SM, Rogers GS. Nonhealing leg ulcers: a manifestation of basal cell carcinoma. J Am Acad Dermatol. 1991;25;47-49.
3. Lutz ME, Davis MD, Otley CC. Infiltrating basal cell carcinoma in the setting of a venous ulcer. Int J Dermatol. 2000;39:519-520.
4. Jankovic A, Binic I, Ljubenovic M. Basal cell carcinoma is not granulation tissue in the venous leg ulcer. Int J Low Extrem Wounds. 2008;7:182-184.
5. James WD, Berger TG, Elston DM. Chapter 29. Epidermal nevi, neoplasms, and cysts. In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin Clinical Dermatology. 11th ed. Philadelphia, PA: Elsevier, Inc; 2011.
6. Yang D, Morrison BD, Vandongen YK, et al. Malignancy in chronic leg ulcers. Med J Aust. 1996;164:718-720.
7. Senet P, Combemale P, Debure C, et al; Angio-Dermatology Group Of The French Society Of Dermatology. Malignancy and chronic leg ulcers: the value of systematic wound biopsies: a prospective, multicenter, cross-sectional study. Arch Dermatol. 2012;148:704-708.
8. Valencia IC, Falabella A, Kirsner RS, et al. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol. 2001;44:401-421.
9. James WD, Berger TG, Elston DM. Chapter 30. Melanocytic nevi and neoplasms. In: James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin Clinical Dermatology. 11th ed. Philadelphia, PA: Elsevier, Inc; 2011.
