User login
Is a lax medication reconciliation process producing errors at your hospital? The National Quality Forum has endorsed a new quality measure aimed at identifying medication discrepancies and the process gaps that caused them. Measure #2456, officially endorsed by the NQF in September, assesses the quality of a hospital’s medication reconciliation process by identifying errors in admission and discharge orders. Here’s how it works: At the time of admission, hospital medication orders are compared with the preadmission medication list, which is compiled by a pharmacist. At discharge, the pharmacist repeats the process using both the preadmission list and any medications ordered during the hospitalization.
This type of review can help identify both history errors and reconciliation errors. History errors occur when a mistake in the history leads to an error in the medication order. For instance, if the clinical team in the hospital didn’t know a patient was on aspirin when they were admitted, they wouldn’t order it at admission.
If the history is correct, but the medication orders don’t match the preadmission medication list, that could be an intentional change by the care team or a reconciliation error.
The pharmacist can usually determine which one it is by reviewing the chart or consulting the care team, said Dr. Jeffrey L. Schnipper, a hospitalist at Brigham and Women’s Hospital in Boston, who proposed the new NQF measure.
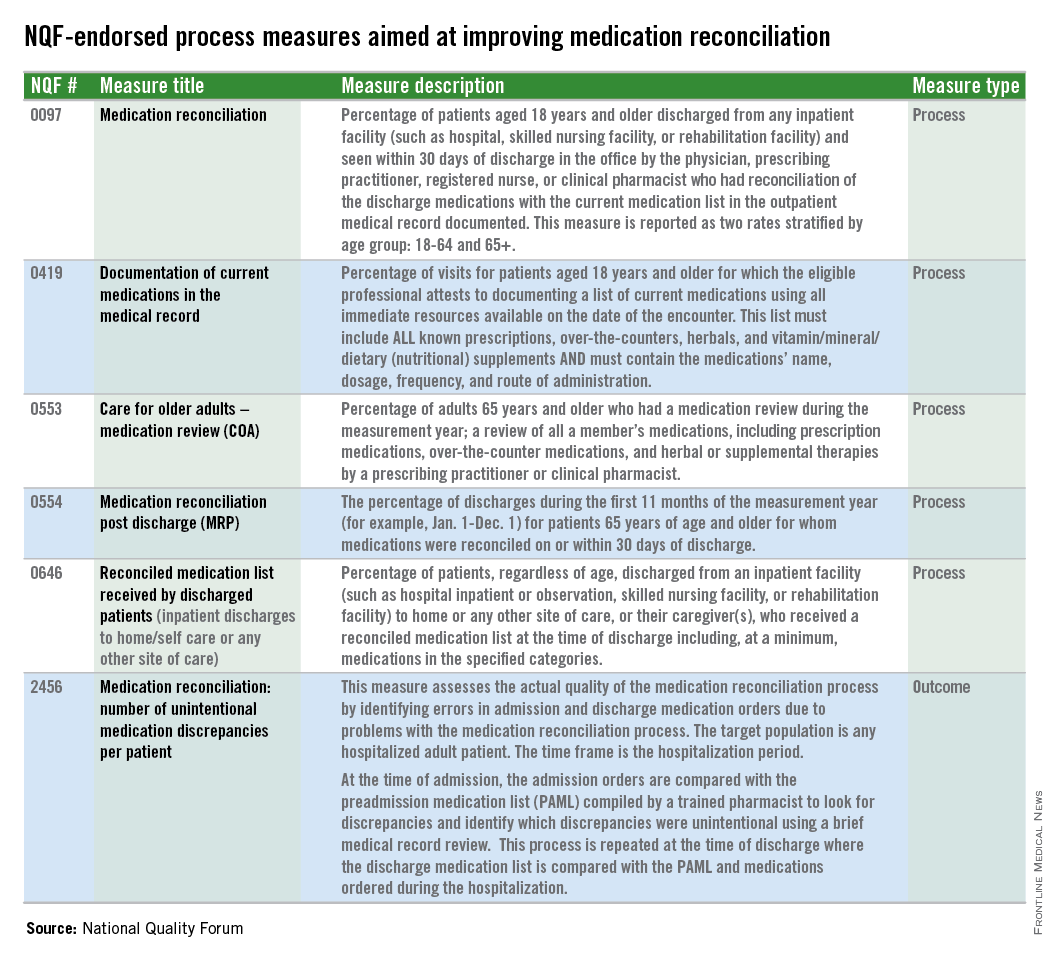
The new measure joins five NQF-endorsed process measures aimed at improving medication reconciliation. But the new measure is the first outcome measure.
The Joint Commission also requires hospitals to engage in medication reconciliation, but that mandate is mostly pro forma, Dr. Schnipper said.
“It’s very much a process measure,” he said. “You say that you have a med rec process. You say that you’ve done med rec. Therefore, med rec is done. There really has been no national measure out there that looks at the actual quality of the med rec process you’re doing. Are you taking accurate medication histories and are you writing the correct orders based on those histories?”
Dr. Schnipper and his colleagues have been studying the issue of unintentional medication discrepancies for the last 5 years as part of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). They found that there are about three unintentional medical discrepancies per patient on average, making reconciliation errors a larger source of medication errors than those caused by prescribing, transcribing, or administration. The error rate for potentially harmful medication discrepancies is about one-half per patient.
“There aren’t a whole lot of things out there where we tolerate a potentially harmful error in every other patient,” Dr. Schnipper said.
Hospitals won’t be required to take on the new measure right away. The measure will continue to be studied and tested over the next couple of years. But Dr. Schnipper said he’s hopeful that at the end of about 5 years, the measure could become part of some federal measurement programs, with financial incentives attached to performance on it.
One of the questions that still has to be studied is whether the measure will be adjusted for risk. More data will be available once the MARQUIS study is complete, Dr. Schnipper said, but early data suggests that it would need to be adjusted for patient age and the number of medications that a patient is taking.
Another question is whether hospitals will be evaluated based on the absolute number of medication discrepancies per patient or on their relative improvement over time. The final MARQUIS data are also expected to shed light on that issue.
Dr. Schnipper said he does not expect the new measure to be a drain on hospitals or physicians. As currently crafted, the measure would be used for about 22 patients per month and he estimates that it would take one full-time pharmacist or less to take a “gold standard” medication history and compare it with the preadmission and discharge medication lists. It would be no more labor intensive than the chart reviews undertaken by nurses to comply with the National Surgical Quality Improvement Program measures, he said.
Is a lax medication reconciliation process producing errors at your hospital? The National Quality Forum has endorsed a new quality measure aimed at identifying medication discrepancies and the process gaps that caused them. Measure #2456, officially endorsed by the NQF in September, assesses the quality of a hospital’s medication reconciliation process by identifying errors in admission and discharge orders. Here’s how it works: At the time of admission, hospital medication orders are compared with the preadmission medication list, which is compiled by a pharmacist. At discharge, the pharmacist repeats the process using both the preadmission list and any medications ordered during the hospitalization.
This type of review can help identify both history errors and reconciliation errors. History errors occur when a mistake in the history leads to an error in the medication order. For instance, if the clinical team in the hospital didn’t know a patient was on aspirin when they were admitted, they wouldn’t order it at admission.
If the history is correct, but the medication orders don’t match the preadmission medication list, that could be an intentional change by the care team or a reconciliation error.
The pharmacist can usually determine which one it is by reviewing the chart or consulting the care team, said Dr. Jeffrey L. Schnipper, a hospitalist at Brigham and Women’s Hospital in Boston, who proposed the new NQF measure.
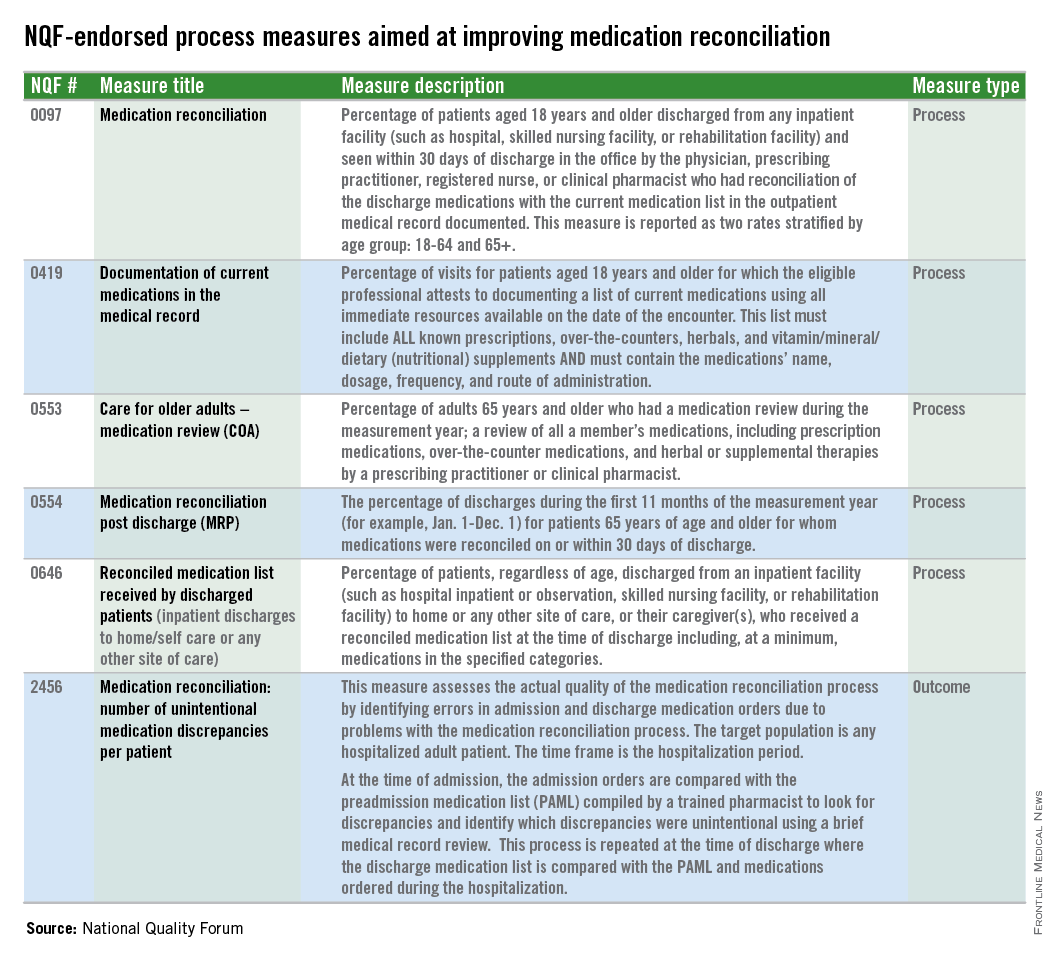
The new measure joins five NQF-endorsed process measures aimed at improving medication reconciliation. But the new measure is the first outcome measure.
The Joint Commission also requires hospitals to engage in medication reconciliation, but that mandate is mostly pro forma, Dr. Schnipper said.
“It’s very much a process measure,” he said. “You say that you have a med rec process. You say that you’ve done med rec. Therefore, med rec is done. There really has been no national measure out there that looks at the actual quality of the med rec process you’re doing. Are you taking accurate medication histories and are you writing the correct orders based on those histories?”
Dr. Schnipper and his colleagues have been studying the issue of unintentional medication discrepancies for the last 5 years as part of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). They found that there are about three unintentional medical discrepancies per patient on average, making reconciliation errors a larger source of medication errors than those caused by prescribing, transcribing, or administration. The error rate for potentially harmful medication discrepancies is about one-half per patient.
“There aren’t a whole lot of things out there where we tolerate a potentially harmful error in every other patient,” Dr. Schnipper said.
Hospitals won’t be required to take on the new measure right away. The measure will continue to be studied and tested over the next couple of years. But Dr. Schnipper said he’s hopeful that at the end of about 5 years, the measure could become part of some federal measurement programs, with financial incentives attached to performance on it.
One of the questions that still has to be studied is whether the measure will be adjusted for risk. More data will be available once the MARQUIS study is complete, Dr. Schnipper said, but early data suggests that it would need to be adjusted for patient age and the number of medications that a patient is taking.
Another question is whether hospitals will be evaluated based on the absolute number of medication discrepancies per patient or on their relative improvement over time. The final MARQUIS data are also expected to shed light on that issue.
Dr. Schnipper said he does not expect the new measure to be a drain on hospitals or physicians. As currently crafted, the measure would be used for about 22 patients per month and he estimates that it would take one full-time pharmacist or less to take a “gold standard” medication history and compare it with the preadmission and discharge medication lists. It would be no more labor intensive than the chart reviews undertaken by nurses to comply with the National Surgical Quality Improvement Program measures, he said.
Is a lax medication reconciliation process producing errors at your hospital? The National Quality Forum has endorsed a new quality measure aimed at identifying medication discrepancies and the process gaps that caused them. Measure #2456, officially endorsed by the NQF in September, assesses the quality of a hospital’s medication reconciliation process by identifying errors in admission and discharge orders. Here’s how it works: At the time of admission, hospital medication orders are compared with the preadmission medication list, which is compiled by a pharmacist. At discharge, the pharmacist repeats the process using both the preadmission list and any medications ordered during the hospitalization.
This type of review can help identify both history errors and reconciliation errors. History errors occur when a mistake in the history leads to an error in the medication order. For instance, if the clinical team in the hospital didn’t know a patient was on aspirin when they were admitted, they wouldn’t order it at admission.
If the history is correct, but the medication orders don’t match the preadmission medication list, that could be an intentional change by the care team or a reconciliation error.
The pharmacist can usually determine which one it is by reviewing the chart or consulting the care team, said Dr. Jeffrey L. Schnipper, a hospitalist at Brigham and Women’s Hospital in Boston, who proposed the new NQF measure.
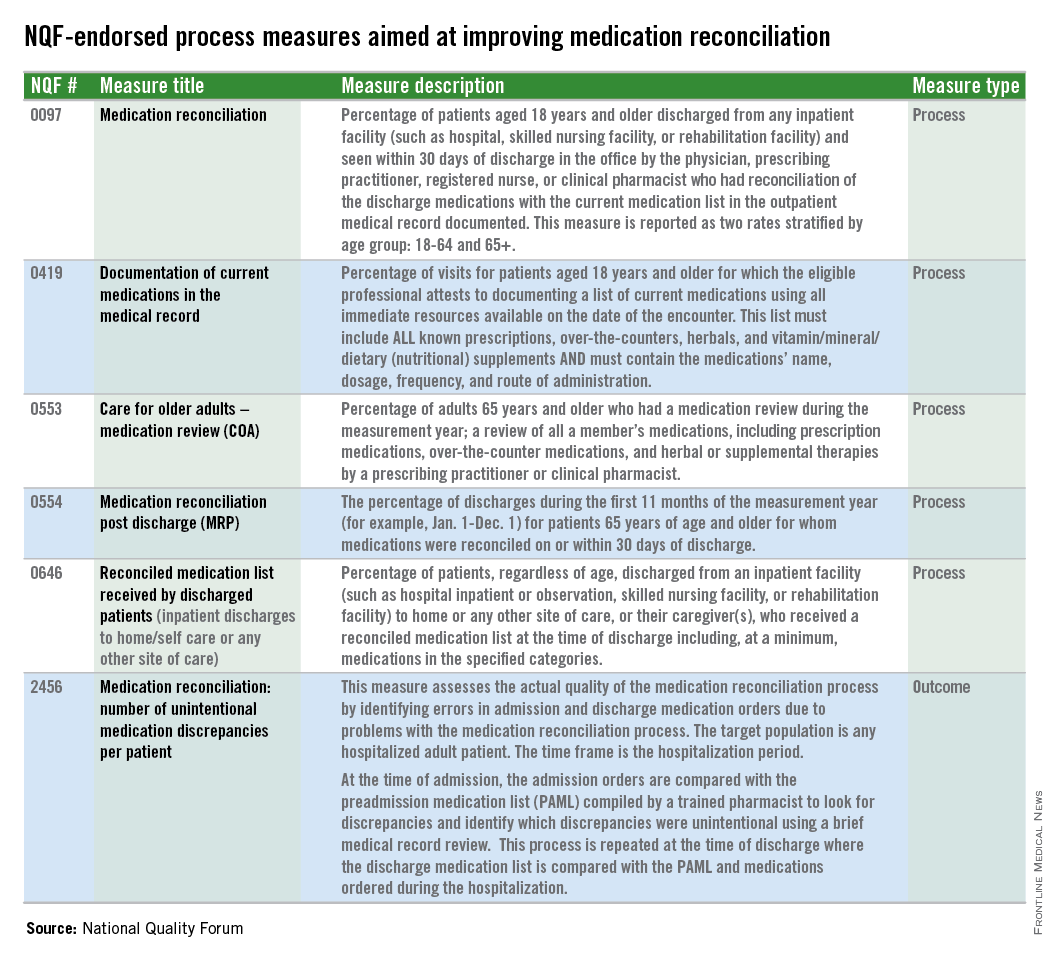
The new measure joins five NQF-endorsed process measures aimed at improving medication reconciliation. But the new measure is the first outcome measure.
The Joint Commission also requires hospitals to engage in medication reconciliation, but that mandate is mostly pro forma, Dr. Schnipper said.
“It’s very much a process measure,” he said. “You say that you have a med rec process. You say that you’ve done med rec. Therefore, med rec is done. There really has been no national measure out there that looks at the actual quality of the med rec process you’re doing. Are you taking accurate medication histories and are you writing the correct orders based on those histories?”
Dr. Schnipper and his colleagues have been studying the issue of unintentional medication discrepancies for the last 5 years as part of the Multi-Center Medication Reconciliation Quality Improvement Study (MARQUIS). They found that there are about three unintentional medical discrepancies per patient on average, making reconciliation errors a larger source of medication errors than those caused by prescribing, transcribing, or administration. The error rate for potentially harmful medication discrepancies is about one-half per patient.
“There aren’t a whole lot of things out there where we tolerate a potentially harmful error in every other patient,” Dr. Schnipper said.
Hospitals won’t be required to take on the new measure right away. The measure will continue to be studied and tested over the next couple of years. But Dr. Schnipper said he’s hopeful that at the end of about 5 years, the measure could become part of some federal measurement programs, with financial incentives attached to performance on it.
One of the questions that still has to be studied is whether the measure will be adjusted for risk. More data will be available once the MARQUIS study is complete, Dr. Schnipper said, but early data suggests that it would need to be adjusted for patient age and the number of medications that a patient is taking.
Another question is whether hospitals will be evaluated based on the absolute number of medication discrepancies per patient or on their relative improvement over time. The final MARQUIS data are also expected to shed light on that issue.
Dr. Schnipper said he does not expect the new measure to be a drain on hospitals or physicians. As currently crafted, the measure would be used for about 22 patients per month and he estimates that it would take one full-time pharmacist or less to take a “gold standard” medication history and compare it with the preadmission and discharge medication lists. It would be no more labor intensive than the chart reviews undertaken by nurses to comply with the National Surgical Quality Improvement Program measures, he said.

