User login
A 27-year-old man, who works as an electrician, self-refers for evaluation of changes on his left palm. He first noticed them three years ago, when a scaly patch appeared on his volar wrist. At the time, his mother sent him an unidentified cream from Mexico, which he used on the rash. Although it resolved, within a few months, his entire palm was similarly affected.
The problem has persisted despite a number of treatment attempts—with, among other things, OTC creams and lotions, topical steroids, antifungals, and two courses of oral antibiotics. He even tried a vegetarian diet. Nothing has worked.
The hand is mildly symptomatic and faintly irritated. He reports similar symptoms on the soles of both feet, which he says date to several years before his hand problem. The fingernails on the affected hand have also changed.
The skin and nails of his right hand have remained completely normal throughout this experience. His health is otherwise excellent.
EXAMINATION
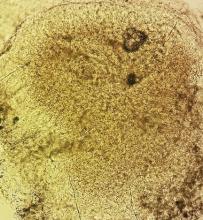
The skin on his left palm and on both soles is identical: uniformly scaly and pink, and in sharp contrast to the normal, smooth skin of his right palm. All five fingernails of his left hand are yellowed, thickened, and dystrophic. Surprisingly, all toenails are normal in appearance. His right hand is unaffected.
What is the diagnosis?
DISCUSSION
This curious phenomenon, known as “two-feet, one-hand disease,” represents a variant of dermatophytosis that is usually remarkably mild in terms of symptoms but often lasts years (if not decades) once the patient develops it. The causative organism is the same dermatophyte that causes jock itch and athlete’s foot: Trichophyton rubrum, the most commonly isolated fungal organism causing disease in humans.
There has never been a satisfactory explanation for why this fairly common condition spares one hand completely. It has been posited that the disease more often affects the dominant hand, but studies haven’t supported that theory. Neither has one hand (left or right) been shown to predominate.
What we do know is that the organisms feed on nonliving skin, which is why they cause minimal symptoms. The palms, soles, and nails represent more tissue for them to feed on and a way to escape the reach of the immune system.
Susceptibility is a key factor in why some people, but not others, develop two-foot-one-hand disease. It is thought that the inability to fend off this organism is related to an inherited, qualitative deficiency of cell-mediated immunity—coupled in some cases with environmental factors such as heat, humidity, and choice of shoes.
We also know that as common and well known as this diagnosis is in dermatology circles, it is far more obscure to nondermatology providers. As a result, the uninitiated provider tends to treat it as he or she would eczema or psoriasis (both of which belong in the differential): with steroids, which are the very thing certain to worsen the condition.
In some cases, before seeking professional care, patients attempt to treat their problem with steroids prescribed for another condition—or even for another patient. The condition will appear to improve but then worsen over time, as the steroids suppress what little immune response exists. The overall effect is thus to worsen the situation considerably, making the condition more difficult to treat.
In the absence of a definite diagnosis, even when antifungals are tried, they are often relatively weak products (eg, tolnaftate or undecylenic acid) that afford little if any relief. The patient (and sometimes provider) then interprets this as a sign that the problem is not of fungal origin and proceeds to other, truly ineffective treatments.
The two key factors that solve the mystery of two-foot-one-hand disease are: knowledge of its existence and the performance of a KOH examination of scrapings from the palm or sole. In this case, KOH revealed numerous fungal hyphae, confirming the diagnosis. Then—and only then—could effective treatment be provided.
This patient was treated with miconazole cream (bid application) and a month-long course oral terbinafine (250 mg/d). The good news is that this will help control the disease. The bad news? The problem will continue to lurk in the background, because we can do little or nothing to make the patient less susceptible. At least he now knows what he has, and he has the weapons to ward it off in the future.
TAKE-HOME LEARNING POINTS
• “Two feet, one hand” disease is a form of dermatophytosis that affects both feet and one hand while completely sparing the other hand. To date, no one has explained this pattern of distribution.
• As with many dermatologic conditions, the diagnosis of two-feet-one-hand disease is simple if you know it exists and completely obscure if you don’t.
• Individual susceptibility appears to explain why some people develop it and many more (including family/household members of affected individuals) don’t.
• Besides knowledge of its existence, the key to diagnosis is the confirmatory KOH prep.
• This is a perfect example of the principle of “correct diagnosis dictates correct treatment.”
A 27-year-old man, who works as an electrician, self-refers for evaluation of changes on his left palm. He first noticed them three years ago, when a scaly patch appeared on his volar wrist. At the time, his mother sent him an unidentified cream from Mexico, which he used on the rash. Although it resolved, within a few months, his entire palm was similarly affected.
The problem has persisted despite a number of treatment attempts—with, among other things, OTC creams and lotions, topical steroids, antifungals, and two courses of oral antibiotics. He even tried a vegetarian diet. Nothing has worked.
The hand is mildly symptomatic and faintly irritated. He reports similar symptoms on the soles of both feet, which he says date to several years before his hand problem. The fingernails on the affected hand have also changed.
The skin and nails of his right hand have remained completely normal throughout this experience. His health is otherwise excellent.
EXAMINATION
The skin on his left palm and on both soles is identical: uniformly scaly and pink, and in sharp contrast to the normal, smooth skin of his right palm. All five fingernails of his left hand are yellowed, thickened, and dystrophic. Surprisingly, all toenails are normal in appearance. His right hand is unaffected.
What is the diagnosis?
DISCUSSION
This curious phenomenon, known as “two-feet, one-hand disease,” represents a variant of dermatophytosis that is usually remarkably mild in terms of symptoms but often lasts years (if not decades) once the patient develops it. The causative organism is the same dermatophyte that causes jock itch and athlete’s foot: Trichophyton rubrum, the most commonly isolated fungal organism causing disease in humans.
There has never been a satisfactory explanation for why this fairly common condition spares one hand completely. It has been posited that the disease more often affects the dominant hand, but studies haven’t supported that theory. Neither has one hand (left or right) been shown to predominate.
What we do know is that the organisms feed on nonliving skin, which is why they cause minimal symptoms. The palms, soles, and nails represent more tissue for them to feed on and a way to escape the reach of the immune system.
Susceptibility is a key factor in why some people, but not others, develop two-foot-one-hand disease. It is thought that the inability to fend off this organism is related to an inherited, qualitative deficiency of cell-mediated immunity—coupled in some cases with environmental factors such as heat, humidity, and choice of shoes.
We also know that as common and well known as this diagnosis is in dermatology circles, it is far more obscure to nondermatology providers. As a result, the uninitiated provider tends to treat it as he or she would eczema or psoriasis (both of which belong in the differential): with steroids, which are the very thing certain to worsen the condition.
In some cases, before seeking professional care, patients attempt to treat their problem with steroids prescribed for another condition—or even for another patient. The condition will appear to improve but then worsen over time, as the steroids suppress what little immune response exists. The overall effect is thus to worsen the situation considerably, making the condition more difficult to treat.
In the absence of a definite diagnosis, even when antifungals are tried, they are often relatively weak products (eg, tolnaftate or undecylenic acid) that afford little if any relief. The patient (and sometimes provider) then interprets this as a sign that the problem is not of fungal origin and proceeds to other, truly ineffective treatments.
The two key factors that solve the mystery of two-foot-one-hand disease are: knowledge of its existence and the performance of a KOH examination of scrapings from the palm or sole. In this case, KOH revealed numerous fungal hyphae, confirming the diagnosis. Then—and only then—could effective treatment be provided.
This patient was treated with miconazole cream (bid application) and a month-long course oral terbinafine (250 mg/d). The good news is that this will help control the disease. The bad news? The problem will continue to lurk in the background, because we can do little or nothing to make the patient less susceptible. At least he now knows what he has, and he has the weapons to ward it off in the future.
TAKE-HOME LEARNING POINTS
• “Two feet, one hand” disease is a form of dermatophytosis that affects both feet and one hand while completely sparing the other hand. To date, no one has explained this pattern of distribution.
• As with many dermatologic conditions, the diagnosis of two-feet-one-hand disease is simple if you know it exists and completely obscure if you don’t.
• Individual susceptibility appears to explain why some people develop it and many more (including family/household members of affected individuals) don’t.
• Besides knowledge of its existence, the key to diagnosis is the confirmatory KOH prep.
• This is a perfect example of the principle of “correct diagnosis dictates correct treatment.”
A 27-year-old man, who works as an electrician, self-refers for evaluation of changes on his left palm. He first noticed them three years ago, when a scaly patch appeared on his volar wrist. At the time, his mother sent him an unidentified cream from Mexico, which he used on the rash. Although it resolved, within a few months, his entire palm was similarly affected.
The problem has persisted despite a number of treatment attempts—with, among other things, OTC creams and lotions, topical steroids, antifungals, and two courses of oral antibiotics. He even tried a vegetarian diet. Nothing has worked.
The hand is mildly symptomatic and faintly irritated. He reports similar symptoms on the soles of both feet, which he says date to several years before his hand problem. The fingernails on the affected hand have also changed.
The skin and nails of his right hand have remained completely normal throughout this experience. His health is otherwise excellent.
EXAMINATION
The skin on his left palm and on both soles is identical: uniformly scaly and pink, and in sharp contrast to the normal, smooth skin of his right palm. All five fingernails of his left hand are yellowed, thickened, and dystrophic. Surprisingly, all toenails are normal in appearance. His right hand is unaffected.
What is the diagnosis?
DISCUSSION
This curious phenomenon, known as “two-feet, one-hand disease,” represents a variant of dermatophytosis that is usually remarkably mild in terms of symptoms but often lasts years (if not decades) once the patient develops it. The causative organism is the same dermatophyte that causes jock itch and athlete’s foot: Trichophyton rubrum, the most commonly isolated fungal organism causing disease in humans.
There has never been a satisfactory explanation for why this fairly common condition spares one hand completely. It has been posited that the disease more often affects the dominant hand, but studies haven’t supported that theory. Neither has one hand (left or right) been shown to predominate.
What we do know is that the organisms feed on nonliving skin, which is why they cause minimal symptoms. The palms, soles, and nails represent more tissue for them to feed on and a way to escape the reach of the immune system.
Susceptibility is a key factor in why some people, but not others, develop two-foot-one-hand disease. It is thought that the inability to fend off this organism is related to an inherited, qualitative deficiency of cell-mediated immunity—coupled in some cases with environmental factors such as heat, humidity, and choice of shoes.
We also know that as common and well known as this diagnosis is in dermatology circles, it is far more obscure to nondermatology providers. As a result, the uninitiated provider tends to treat it as he or she would eczema or psoriasis (both of which belong in the differential): with steroids, which are the very thing certain to worsen the condition.
In some cases, before seeking professional care, patients attempt to treat their problem with steroids prescribed for another condition—or even for another patient. The condition will appear to improve but then worsen over time, as the steroids suppress what little immune response exists. The overall effect is thus to worsen the situation considerably, making the condition more difficult to treat.
In the absence of a definite diagnosis, even when antifungals are tried, they are often relatively weak products (eg, tolnaftate or undecylenic acid) that afford little if any relief. The patient (and sometimes provider) then interprets this as a sign that the problem is not of fungal origin and proceeds to other, truly ineffective treatments.
The two key factors that solve the mystery of two-foot-one-hand disease are: knowledge of its existence and the performance of a KOH examination of scrapings from the palm or sole. In this case, KOH revealed numerous fungal hyphae, confirming the diagnosis. Then—and only then—could effective treatment be provided.
This patient was treated with miconazole cream (bid application) and a month-long course oral terbinafine (250 mg/d). The good news is that this will help control the disease. The bad news? The problem will continue to lurk in the background, because we can do little or nothing to make the patient less susceptible. At least he now knows what he has, and he has the weapons to ward it off in the future.
TAKE-HOME LEARNING POINTS
• “Two feet, one hand” disease is a form of dermatophytosis that affects both feet and one hand while completely sparing the other hand. To date, no one has explained this pattern of distribution.
• As with many dermatologic conditions, the diagnosis of two-feet-one-hand disease is simple if you know it exists and completely obscure if you don’t.
• Individual susceptibility appears to explain why some people develop it and many more (including family/household members of affected individuals) don’t.
• Besides knowledge of its existence, the key to diagnosis is the confirmatory KOH prep.
• This is a perfect example of the principle of “correct diagnosis dictates correct treatment.”