User login
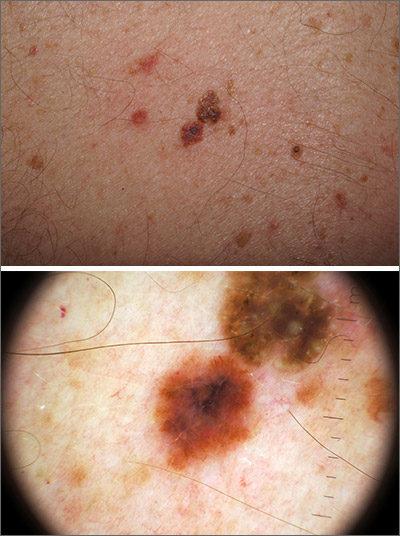
In addition to the patient’s SK, the second finding was diagnosed as a thin melanoma. The clinical appearance of SKs and nevi or melanoma can overlap. Dermoscopy is a helpful tool in distinguishing between them, even when juxtaposed in a collision lesion such as this.1
Dermoscopy of the superior portion of the lesion demonstrated a well-demarcated brown, waxy papule with milia-like cysts, consistent with an SK. Inferiorly, the dermoscopic features included atypical pigment network, asymmetrical streaks, and blue-white veil, suggestive of melanoma or an atypical melanocytic neoplasm. A deep-shave biopsy was performed of the lower section, aiming for a narrow margin (1-3 mm) of normal skin. The biopsy confirmed a superficial spreading melanoma with a Breslow depth of 0.5 mm with 0 mitoses per high-power field.
A deep-shave biopsy was chosen over a punch biopsy because the latter would be unlikely to sample the entire lesion.
One month after the initial biopsy, a wide local excision with a 1-cm margin was performed. The planned follow-up for the patient was skin exams every 3 months for the first year, every 6 months for the next 4 years, and then annually for life.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Blum A, Siggs G, Marghoob AA, et al. Collision skin lesions-results of a multicenter study of the International Dermoscopy Society (IDS). Dermatol Pract Concept. 2017;7:51-62. doi:10.5826/dpc.0704a12
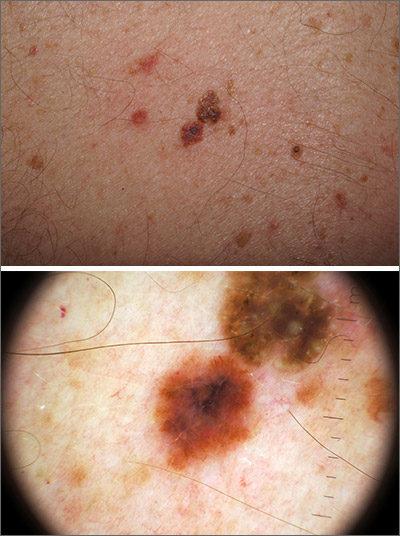
In addition to the patient’s SK, the second finding was diagnosed as a thin melanoma. The clinical appearance of SKs and nevi or melanoma can overlap. Dermoscopy is a helpful tool in distinguishing between them, even when juxtaposed in a collision lesion such as this.1
Dermoscopy of the superior portion of the lesion demonstrated a well-demarcated brown, waxy papule with milia-like cysts, consistent with an SK. Inferiorly, the dermoscopic features included atypical pigment network, asymmetrical streaks, and blue-white veil, suggestive of melanoma or an atypical melanocytic neoplasm. A deep-shave biopsy was performed of the lower section, aiming for a narrow margin (1-3 mm) of normal skin. The biopsy confirmed a superficial spreading melanoma with a Breslow depth of 0.5 mm with 0 mitoses per high-power field.
A deep-shave biopsy was chosen over a punch biopsy because the latter would be unlikely to sample the entire lesion.
One month after the initial biopsy, a wide local excision with a 1-cm margin was performed. The planned follow-up for the patient was skin exams every 3 months for the first year, every 6 months for the next 4 years, and then annually for life.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
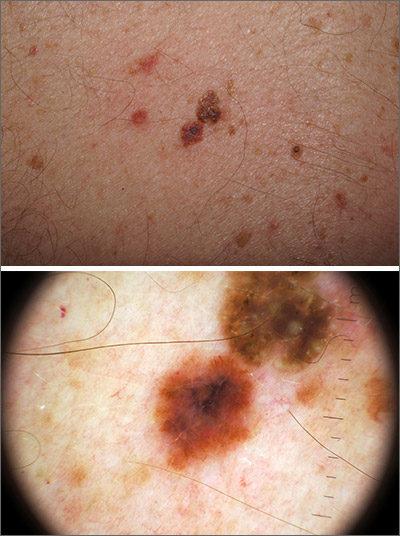
In addition to the patient’s SK, the second finding was diagnosed as a thin melanoma. The clinical appearance of SKs and nevi or melanoma can overlap. Dermoscopy is a helpful tool in distinguishing between them, even when juxtaposed in a collision lesion such as this.1
Dermoscopy of the superior portion of the lesion demonstrated a well-demarcated brown, waxy papule with milia-like cysts, consistent with an SK. Inferiorly, the dermoscopic features included atypical pigment network, asymmetrical streaks, and blue-white veil, suggestive of melanoma or an atypical melanocytic neoplasm. A deep-shave biopsy was performed of the lower section, aiming for a narrow margin (1-3 mm) of normal skin. The biopsy confirmed a superficial spreading melanoma with a Breslow depth of 0.5 mm with 0 mitoses per high-power field.
A deep-shave biopsy was chosen over a punch biopsy because the latter would be unlikely to sample the entire lesion.
One month after the initial biopsy, a wide local excision with a 1-cm margin was performed. The planned follow-up for the patient was skin exams every 3 months for the first year, every 6 months for the next 4 years, and then annually for life.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
1. Blum A, Siggs G, Marghoob AA, et al. Collision skin lesions-results of a multicenter study of the International Dermoscopy Society (IDS). Dermatol Pract Concept. 2017;7:51-62. doi:10.5826/dpc.0704a12
1. Blum A, Siggs G, Marghoob AA, et al. Collision skin lesions-results of a multicenter study of the International Dermoscopy Society (IDS). Dermatol Pract Concept. 2017;7:51-62. doi:10.5826/dpc.0704a12
