User login
Anemia is a potent risk factor for mortality and morbidity in surgical patients, and its management has begun to shift away from allogeneic blood transfusion in recent years. This article reviews the clinical importance of perioperative anemia, the role and shortcomings of blood transfusion, and the pros and cons of alternative approaches to managing perioperative anemia. I conclude with an overview of a program for perioperative blood product use at my institution, Cleveland Clinic.
SIGNIFICANCE OF PERIOPERATIVE ANEMIA
Prevalence depends on many factors
The reported prevalence of anemia in surgical patients varies widely—from 5% to 76%1—and depends on the patient’s disease and comorbidities, the surgical procedure and associated blood loss, and the definition of anemia used. The prevalence of preoperative anemia increases with patient age and is higher in women than in men.2
A multiplier of risk
Anemia is an important multiplier of mortality risk. For example, the presence of anemia raises the relative risk of 2-year mortality from 2.05 to 3.37 in patients with chronic kidney disease, from 2.86 to 3.78 in patients with heart failure, and from 4.86 to 6.07 in patients with concomitant heart failure and chronic kidney disease.3
Adverse effects of anemia have been demonstrated specifically in the perioperative setting as well. A large retrospective cohort study showed that a preoperative hemoglobin concentration of less than 6 g/dL increases the risk of death 30 days after surgery by a factor of 26 relative to a concentration of 12 g/dL or greater in surgical patients who declined blood transfusion for religious reasons.4 The anemia-associated mortality risk was especially pronounced among patients with cardiovascular disease.4 Other studies have demonstrated perioperative anemia to be associated with increases in the risk of death,5 cardiac events,6 pneumonia,7 and postoperative delirium.8
IS BLOOD TRANSFUSION THE ANSWER
The use of allogeneic blood transfusion to manage anemia and blood loss is a concept that originated several centuries ago and has changed little over the years.
Blood supply challenges
Blood collection has historically lagged demand, resulting in a blood supply insufficient to meet transfusion needs. According to the federal government’s 2007 National Blood Collection and Utilization Survey Report, 6.89% of US hospitals reported that they cancelled elective surgery on 1 or more days in the prior year because of a lack of blood availability, and 13.5% experienced at least 1 day in which nonsurgical blood needs could not be met.9 Unless practices are changed to increase blood donation, these unmet tranfusion needs may grow.
Joint Commission set to measure blood management
In response to this challenge, an advisory panel formed by the Joint Commission has identified 17 performance measures related to blood conservation and appropriate transfusion.10 These measures are currently in development, and we expect to see some types of metrics in the near future. Such metrics are likely to further prioritize blood management for US hospitals.
Safety of the blood supply: Viral transmission down, TRALI risk persists
The safety of the blood supply has improved markedly. Sophisticated testing and public demand have led to a dramatic decline in the risk of transfusion-related transmission of HIV, hepatitis C virus, and hepatitis B virus.11
Despite this progress, the risk of transfusion-related acute lung injury (TRALI) has persisted in recent years. TRALI is characterized by acute onset of noncardiogenic pulmonary edema within 6 hours of blood product transfusion. Believed to be immune-mediated, TRALI is thought to occur as antibodies to human leukocyte antigens develop, inducing capillary leak syndrome.12 The patients most commonly affected are those who receive plasma from multiparous female donors. A recent evaluation of transfusion-related fatalities reported to the US Food and Drug Administration (FDA) revealed a continual rise in fatal TRALI cases in the United States from 2001 to 2006.13–15 TRALI was implicated in more than half of all transfusion-related fatalities reported to the FDA in 2006, a higher number than for any other single cause.13
At the same time, there is evidence that hemovigilance can reduce TRALI risk. In the United Kingdom, the Serious Hazards of Transfusion Steering Group introduced in late 2003 a policy of using plasma from male donors as much as possible, in view of the association of TRALI with plasma from multiparous female donors. The effort appeared to pay off: whereas TRALI accounted for 6.8% of all transfusion-related adverse events reported in the United Kingdom during the period 1996–2003,16 this proportion declined to just 1.9% in 2006.17
Finally, despite the progress in screening blood for more established infections like HIV and the hepatitis viruses, some additional infections now must be considered when assessing blood supply safety. These include diseases newly recognized as being transmissible by blood, or for which blood donor screening is not currently available, or that are newly emergent infections for which the potential for spread by transfusion is unknown. For such diseases—which include malaria and West Nile virus—the risk of transmission through transfusion is low, as they are much more likely to be acquired by other means.
Transfusion and outcomes: Not a strong record
Transfusion has never undergone safety and efficacy evaluation by the FDA. Given the challenges of conducting a randomized study of transfusion in the perioperative setting, we may never have high-quality data to assess transfusion in this setting.
A few studies merit mention, however. The Transfusion Requirement in Critical Care (TRICC) trial was conducted in 838 critically ill patients in the intensive care setting.18 Patients were randomized to a strategy of either liberal transfusion (begun when hemoglobin fell below 10 g/dL) or restrictive transfusion (begun when hemoglobin fell below 7 g/dL). Thirty-day mortality was similar between patients in the two strategy groups, but the restrictive strategy was associated with significantly lower mortality in at least two subgroups: patients with myocardial infarction and patients with pulmonary edema. Further subgroup analysis found no benefit of early or aggressive transfusion in patients with coronary artery disease or in those requiring mechanical ventilation.
Rao et al performed a meta-analysis of three large international trials of patients with acute coronary syndromes to determine whether blood transfusion to correct anemia in this setting was associated with improved survival.19 They found significantly higher mortality among patients who underwent transfusion compared with those who did not, prompting them to urge caution in the use of transfusion to maintain arbitrary hematocrit levels in stable patients with ischemic heart disease.
Similarly, a risk-adjusted, propensity-matched analysis of 6,301 patients undergoing noncardiac surgery found that receipt of 4 U of blood or more was a predictor of greater mortality, higher risk of infection, and longer hospital stay.20 Moreover, in an observational cohort study of 11,963 patients who underwent isolated coronary artery bypass graft surgery, each unit of red blood cells transfused was associated with an incrementally increased risk of adverse outcome (eg, mortality, renal injury, need for ventilator support, lengthened hospital stay, infection).21 The latter study found that transfusion was the single factor most reliably associated with increased risk of postoperative morbidity.
Additional studies have echoed these findings—ie, that perioperative blood transfusion has been associated with a host of adverse outcomes, including increased morbidity and length of stay, increased rates of postoperative infection, as well as immunosuppression, viral transmission, and acute transfusion reactions.5,22,23
Outcomes and duration of blood storage
An interesting factor in the relation between transfusion and outcomes is the shelf life of the blood being transfused. The FDA currently allows storage of blood for a maximum of 42 days, but a recent study of patients who received red blood cell transfusions during cardiac surgery found that those who received “older blood” (stored for > 14 days) had significantly higher rates of sepsis, prolonged intubation, renal failure, in-hospital mortality, and 1-year mortality compared with those who received “newer blood” (stored for ≤ 14 days).24
These differing outcomes are generally attributed to the so-called storage defect: as blood gets older, it loses components such as 2,3-DPG and adenosine disphosphate, its red cells lose deformability, and it undergoes buildup of cytokines and free hemoglobin. Increased demand for newer blood in light of the storage defect could further intensify pressures on the blood supply.
MANAGEMENT OF PERIOPERATIVE ANEMIA
In light of these shortcomings of blood transfusion, how should anemia be managed perioperatively to reduce or avoid the need for transfusion?
Preoperative evaluation
Vigilance for anemia and related issues in the preoperative evaluation is fundamental. The evaluation should elicit a history of bleeding tendencies, previous transfusions, and symptoms of anemia. Medications should be reviewed with an eye toward any that may predispose to perioperative bleeding and anemia, such as aspirin, clopidogrel, and anticoagulants. During the physical examination, alertness for pallor and petechiae is key, as is attentiveness to symptoms of anemia such as shortness of breath and fatigue.
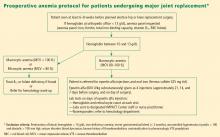
Overview of management options
Once the cause of anemia is identified, the choice for optimal medical management can be made. Choices broadly consist of pharmacologic and technological options. The former include iron supplements and erythropoiesis-stimulating agents. Among other pharmacologic options are thrombin, collagen, fibrin glue, tranexamic acid, and aminocaproic acid, but these agents are less well studied and will not be discussed here. Technological options include preoperative autologous blood donation, cell salvage, and acute normovolemic hemodilution.
In addition to these options, careful management of anticoagulant and antiplatelet medications should be provided, including discontinuation or substitution of drugs that could hamper clotting perioperatively.
PHARMACOLOGIC OPTIONS
Iron supplementation
Oral iron is available in four preparations: ferrous sulfate, ferrous gluconate, ferrous fumarate, and iron polysaccharide. Gastrointestinal side effects may limit these preparations’ tolerability. Iron supplements with a high elemental value will require fewer pills and fewer doses, reducing the risk or frequency of side effects.
Intravenous (IV) iron preparations are much safer now than they were years ago, when anaphylactic reactions were a concern. The ones generally used in the perioperative setting are iron sucrose and iron gluconate. Unlike the older IV preparations, the use of iron sucrose and iron gluconate often requires a second dose. The effect on hemoglobin levels usually occurs starting at 1 week, with the maximum effect achieved at 2 weeks. Hypotension, arthralgia, abdominal discomfort, and back pain are potential side effects of IV iron.
Efficacy and safety of iron supplementation. Evidence of the efficacy of preoperative iron supplementation is mounting. A study of 569 patients undergoing colorectal cancer surgery found that among the 116 patients who were anemic, intraoperative transfusion was needed in a significantly lower proportion of those who received 2 weeks of preoperative oral iron supplementation (200 mg) compared with those who received no iron therapy (9.4% vs 27.4%; P < .05).26 Similarly, in an uncontrolled study, 10 days of IV iron sucrose starting 4 weeks preoperatively significantly increased hemoglobin levels in 20 patients with iron-deficiency anemia prior to elective orthopedic surgery.27
Risks of infection and cancer progression have been concerns with IV iron therapy. However, no significant association between IV iron therapy and bacteremia was identified in a prospective study of 985 patients receiving chronic hemodialysis.28 The effect of IV iron administration on tumor progression has not been prospectively studied.
In general, IV iron, especially the newer forms, is a safer alternative to blood transfusion. Death occurs at a much lower rate with iron than with blood transfusion (0.4 per million vs 4 per million, respectively), as do life-threatening adverse events (4 per million vs 10 per million, respectively), according to a systematic review by the Network for Advancement of Transfusion Alternatives.29
Erythropoiesis-stimulating agents
Erythropoiesis-stimulating agents (ESAs) include epoetin alfa (erythropoietin), first approved by the FDA in 1989, and the more recently introduced darbepoetin alfa. They are approved to treat anemia in several patient populations, but only epoetin alfa is approved by the FDA explicitly for use in patients undergoing major surgery (to reduce the need for blood transfusions). The ESAs have come under intense scrutiny in recent years over their risk-to-benefit ratio, as detailed below.
The preoperative dosing schedule for epoetin alfa is usually three weekly doses (plus a fourth dose on the day of surgery) if the surgery is scheduled 3 or more weeks in advance. However, daily dosing can be used effectively if the preoperative period is less than 3 weeks, provided that it is continued until 4 days after surgery. Oral iron is necessary throughout the course of epoetin alfa therapy.
Efficacy in reducing transfusions. In a systematic review published in 1998, epoetin alfa was shown to minimize perioperative exposure to allogeneic blood transfusion in patients undergoing orthopedic or cardiac surgery.30 Its benefit was greatest in patients at the highest risk of requiring transfusion. It was effective whether given daily or weekly, and did not significantly increase the risk of thrombotic events when used in surgical patients, although some studies did find an excess of thrombotic events with its use.
In three randomized trials conducted in patients undergoing joint arthroplasty (hip or knee), epoetin alfa was associated with substantial and significant reductions in perioperative blood transfusion compared with placebo or preoperative autologous blood donation.31–33 Rates of deep vein thrombosis (DVT) did not differ significantly between the epoetin alfa and placebo groups.
Concerns over perioperative thromboembolic risk. In early 2007, the FDA was made aware of preliminary results of an open-label study in which 681 patients undergoing elective spinal surgery who did not receive prophylactic anticoagulation were randomized to epoetin alfa plus standard-of-care therapy (pneumatic compression) or standard-of-care therapy alone.34,35 The incidence of DVT was 4.7% in patients treated with epoetin alfa compared with 2.1% in those not receiving epoetin alfa. It is important to note that the available ESAs are prothrombotic and increase thrombotic risk significantly, especially in populations like this one in which pharmacologic DVT prophylaxis is not routinely used.
Based in part on this study, the FDA in 2007 required a boxed warning to be added to the ESAs’ package inserts to specify the increased risk of DVT with their use in surgical patients not receiving prophylactic anticoagulation. The warning urges consideration of the use of DVT prophylaxis in surgical patients receiving an ESA.34,35
TECHNOLOGICAL OPTIONS AND OTHER STRATEGIES
Autologous blood donation: A practice in decline
In cases of elective surgery, autologous blood donation can be used to protect against disease transmission and overcome the challenge of blood type compatibility. Preoperative autologous donation of blood has been a prevalent practice, but its use is declining. One reason is that waste is high (approximately 50% at Cleveland Clinic), which makes this practice more costly than is often realized. Also, autologous blood donation increases the likelihood that the patient will be anemic on the day of surgery, so that he or she may still need allogeneic blood after all, defeating the initial purpose. Despite these limitations, preoperative autologous blood donation remains a useful option for a subset of patients with multiple antibodies for whom donor blood may be difficult to obtain.
Cell salvage
Cell salvage is an innovative technology that recovers the patient’s own blood (after being shed from the surgical incision) for transfusion after filtering and washing. It is particularly well suited to procedures that involve massive blood loss. Cell savage requires technical expertise, however, and involves costs associated with both the machine and disposables.
Restricted postoperative phlebotomy
Phlebotomy accounts for a significant amount of blood loss, especially in intensive care patients with arterial lines. The equivalent of 30% of total blood transfused has been reported to be lost to phlebotomy during an intensive care unit stay.36 Triggers for transfusion cannot be assigned universally based on blood loss from phlebotomy but must consider the patient’s hemodynamic status, cardiac reserve, and other clinical characteristics.
PROMOTING RESPONSIBLE BLOOD PRODUCT USE
Blood is expensive, and in recent years hospitals have experienced increases in the cost of blood and blood products. To promote responsible blood use, we have developed a multipronged approach to blood management at Cleveland Clinic. The program’s cornerstone is increased awareness of the risks associated with blood transfusions. The emphasis is on educating staff physicians and other caregivers about the appropriate use of blood products. We also have implemented a new policy requiring staff authorization for all blood requested in nonemergency situations. Additionally, requests for blood components require adherence to an indication-based ordering process. Finally, data about blood use are shared transparently among physicians, encouraging good clinical practice.
In the first 7 months of the program, we observed decreased utilization of blood products in the inpatient setting. Notably, the reduction in blood use was significantly greater in the surgical population than in the medical population.
CONCULSIONS
Anemia is associated with increased morbidity and mortality in the perioperative setting. Perioperative blood transfusion is one method of raising hemoglobin levels in anemic surgical patients, but it increases perioperative morbidity in the form of acute transfusion reactions, immunosuppression, postoperative infection, and longer hospital stays. Moreover, blood collection continues to lag blood demand. For these reasons, most relevant major medical organizations—including the Association of Blood Banks, the American Red Cross, and the FDA—advise that red blood cell–containing components should not be used to treat anemias that can be corrected with medications. These medical alternatives—all of which can be used in the perioperative setting—include iron supplementation, vitamin B12, and ESAs in select patient groups.
DISCUSSION
Question from the audience: Are there risks involved with autologous blood donation? Are different hemoglobin thresholds used when a patient’s own blood is used?
Dr. Kumar: As I mentioned, preoperative autologous donation is a technique that is less frequently used in our hospital. Autologous transfusion is considered safe only for patients who come to the clinic with normal hemoglobin values. Some patients may not have recovered from their blood loss by the time they come to surgery, so you end up needing to give them more blood because they started out anemic.
Question from the audience: Is there risk to giving patients back their own blood? Do you have to worry about transfusion-induced lung injury, sepsis, or other complications?
Dr. Kumar: As with allogeneic blood, the risk of clerical or clinical error exists with autologous blood: it too needs to be kept on the shelf, taken out, and infused, and the risk of sepsis remains the same.
- Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med 2004; 116(suppl 7A):58S–69S.
- Kulier A, Gombotz H. Perioperative anemia [in German]. Anaesthesist 2001; 50:73–86.
- Herzog CA, Muster HA, Li S, Collins AJ. Impact of congestive heart failure, chronic kidney disease, and anemia on survival in the Medicare population. J Card Fail 2004; 10:467–472.
- Carson JL, Duff A, Poses RM, et al. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 1996; 348:1055–1060.
- Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ. The relationship between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma 2002; 16:39–44.
- Nelson AH, Fleisher LA, Rosenbaum SH. Relationship between postoperative anemia and cardiac morbidity in high-risk vascular patients in the intensive care unit. Crit Care Med 1993; 21:860–866.
- Faris PM, Spence RK, Larholt KM, Sampson AR, Frei D. The predictive power of baseline hemoglobin for transfusion risk in surgery patients. Orthopedics 1999; 22(suppl 1):s135–s140.
- Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH. The association of intraoperative factors with the development of postoperative delirium. Am J Med 1998; 105:380–384.
- US Department of Health and Human Services. The 2007 National Blood Collection and Utilization Survey. Available at: http://www.aabb.org/Documents/Programs_and_Services/Data_Center/07nbcusrpt.pdf. Accessed March 9, 2009.
- The Joint Commission. Performance measurement initiatives. Available at http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Blood+Management+-+Utilization.htm.
- Busch MP, Kleinman SH, Nemo GJ. Current and emerging infectious risks of blood transfusions. JAMA 2003; 289:959–962.
- Silliman CC, Ambruso DR, Boshkov LK. Transfusion-related acute lung injury. Blood 2005; 105:2266–2273.
- Benjamin RJ. Transfusion and transplantation safety: American Red Cross concerns. PowerPoint slides presented at Department of Health and Human Services Advisory Committee on Blood Safety and Availability meeting, May 10–11, 2007. Available at: http://www.hhs.gov/ophs/bloodsafety/presentations/Benjamin0507.pdf. Accessed March 9, 2009.
- Holness L. Transfusion related acute lung injury (TRALI): the FDA current view. PowerPoint slides presented at FDA Blood Products Advisory Committee meeting, July 22–23, 2004. Available at: http://www.fda.gov/OHRMS/DOCKETS/ac/04/briefing/2004-4057b1_01.pdf. Accessed March 9, 2009.
- Williams AE. Transfusion related acute lung injury (TRALI). PowerPoint slides presented at FDA Blood Products Advisory Committee meeting, April 27, 2007. Available at: http://www.fda.gov/ohrms/dockets/ac/07/slides/2007-4300S2-05.ppt. Accessed March 9, 2009.
- Stainsby D, Cohen H, Jones H, et al. Serious Hazards of Transfusion—Annual Report 2003. Published July 5, 2004. Available at: http://www.shotuk.org/SHOT%20Report%202003.pdf. Accessed April 29, 2009.
- Taylor C, Cohen H, Stainsby D, et al. Serious Hazards of Transfusion—Annual Report 2006. Published November 20, 2007. Available at: http://www.shotuk.org/SHOT_report_2006.pdf. Accessed April 29, 2009.
- Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 1999; 340:409–417.
- Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004; 292:1555–1562.
- Dunne JR, Malone D, Tracy JK, et al. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res 2002; 102:237–244.
- Koch CG, Li L, Duncan AI, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006; 34:1608–1616.
- Rady MY, Ryan T, Starr NJ. Perioperative determinants of morbidity and mortality in elderly patients undergoing cardiac surgery. Crit Care Med 1998; 26:225–235.
- Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. First of two parts—blood transfusion. N Engl J Med 1999; 340:438–447.
- Koch CG, Li L, Sessler DI, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 2008; 358:1229–1239.
- Goodnough LT, Shander A. Blood management. Arch Pathol Lab Med 2007; 131:695–701.
- Okuyama M, Ikeda K, Shibata T, et al. Preoperative iron supplementation and intraoperative transfusion during colorectal cancer surgery. Surg Today 2005; 35:36–40.
- Theusinger OM, Leyvraz PF, Schanz U, et al. Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology 2007; 107:923–927.
- Hoen B, Paul-Dauphin A, Kessler M. Intravenous iron administration does not significantly increase the risk of bacteremia in chronic hemodialysis patients. Clin Nephrol 2002; 57:457–461.
- Beris P, Muñoz M, García-Erce JA, et al. Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth 2008; 100:599–604.
- Laupacis A, Fergusson D. Erythropoietin to minimize perioperative blood transfusion: a systematic review of randomized trials: The International Study of Perioperative Transfusion (ISPOT) Investigators. Transfus Med 1998; 8:309–317.
- Feagan BG, Wong CJ, Kirkley A, et al. Erythropoietin with iron supplementation to prevent allogeneic blood transfusion in total hip joint arthroplasty: a randomized, controlled trial. Ann Intern Med 2000; 133:845–854.
- Stowell CP, Chandler H, Jové M, et al. An open-label, randomized study to compare the safety and efficacy of perioperative epoetin alfa with preoperative autologous blood donation in total joint arthroplasty. Orthopedics 1999; 22(suppl 1):s105–s112.
- de Andrade JR, Jové M, Landon G, et al. Baseline hemoglobin as a predictor of risk of transfusion and response to Epoetin alfa in orthopedic surgery patients. Am J Orthop 1996; 25:533–542.
- Procrit [package insert]. Raritan, NJ: Ortho Biotech Products LP; 2009.
- Epogen [package insert]. Thousand Oaks, CA: Amgen Inc.; 2009.
- Smoller BR, Kuskall MS. Phlebotomy for diagnostic laboratory tests in adults: pattern of use and effect on transfusion requirements. N Engl J Med 1986; 314:1233–1235.
Anemia is a potent risk factor for mortality and morbidity in surgical patients, and its management has begun to shift away from allogeneic blood transfusion in recent years. This article reviews the clinical importance of perioperative anemia, the role and shortcomings of blood transfusion, and the pros and cons of alternative approaches to managing perioperative anemia. I conclude with an overview of a program for perioperative blood product use at my institution, Cleveland Clinic.
SIGNIFICANCE OF PERIOPERATIVE ANEMIA
Prevalence depends on many factors
The reported prevalence of anemia in surgical patients varies widely—from 5% to 76%1—and depends on the patient’s disease and comorbidities, the surgical procedure and associated blood loss, and the definition of anemia used. The prevalence of preoperative anemia increases with patient age and is higher in women than in men.2
A multiplier of risk
Anemia is an important multiplier of mortality risk. For example, the presence of anemia raises the relative risk of 2-year mortality from 2.05 to 3.37 in patients with chronic kidney disease, from 2.86 to 3.78 in patients with heart failure, and from 4.86 to 6.07 in patients with concomitant heart failure and chronic kidney disease.3
Adverse effects of anemia have been demonstrated specifically in the perioperative setting as well. A large retrospective cohort study showed that a preoperative hemoglobin concentration of less than 6 g/dL increases the risk of death 30 days after surgery by a factor of 26 relative to a concentration of 12 g/dL or greater in surgical patients who declined blood transfusion for religious reasons.4 The anemia-associated mortality risk was especially pronounced among patients with cardiovascular disease.4 Other studies have demonstrated perioperative anemia to be associated with increases in the risk of death,5 cardiac events,6 pneumonia,7 and postoperative delirium.8
IS BLOOD TRANSFUSION THE ANSWER
The use of allogeneic blood transfusion to manage anemia and blood loss is a concept that originated several centuries ago and has changed little over the years.
Blood supply challenges
Blood collection has historically lagged demand, resulting in a blood supply insufficient to meet transfusion needs. According to the federal government’s 2007 National Blood Collection and Utilization Survey Report, 6.89% of US hospitals reported that they cancelled elective surgery on 1 or more days in the prior year because of a lack of blood availability, and 13.5% experienced at least 1 day in which nonsurgical blood needs could not be met.9 Unless practices are changed to increase blood donation, these unmet tranfusion needs may grow.
Joint Commission set to measure blood management
In response to this challenge, an advisory panel formed by the Joint Commission has identified 17 performance measures related to blood conservation and appropriate transfusion.10 These measures are currently in development, and we expect to see some types of metrics in the near future. Such metrics are likely to further prioritize blood management for US hospitals.
Safety of the blood supply: Viral transmission down, TRALI risk persists
The safety of the blood supply has improved markedly. Sophisticated testing and public demand have led to a dramatic decline in the risk of transfusion-related transmission of HIV, hepatitis C virus, and hepatitis B virus.11
Despite this progress, the risk of transfusion-related acute lung injury (TRALI) has persisted in recent years. TRALI is characterized by acute onset of noncardiogenic pulmonary edema within 6 hours of blood product transfusion. Believed to be immune-mediated, TRALI is thought to occur as antibodies to human leukocyte antigens develop, inducing capillary leak syndrome.12 The patients most commonly affected are those who receive plasma from multiparous female donors. A recent evaluation of transfusion-related fatalities reported to the US Food and Drug Administration (FDA) revealed a continual rise in fatal TRALI cases in the United States from 2001 to 2006.13–15 TRALI was implicated in more than half of all transfusion-related fatalities reported to the FDA in 2006, a higher number than for any other single cause.13
At the same time, there is evidence that hemovigilance can reduce TRALI risk. In the United Kingdom, the Serious Hazards of Transfusion Steering Group introduced in late 2003 a policy of using plasma from male donors as much as possible, in view of the association of TRALI with plasma from multiparous female donors. The effort appeared to pay off: whereas TRALI accounted for 6.8% of all transfusion-related adverse events reported in the United Kingdom during the period 1996–2003,16 this proportion declined to just 1.9% in 2006.17
Finally, despite the progress in screening blood for more established infections like HIV and the hepatitis viruses, some additional infections now must be considered when assessing blood supply safety. These include diseases newly recognized as being transmissible by blood, or for which blood donor screening is not currently available, or that are newly emergent infections for which the potential for spread by transfusion is unknown. For such diseases—which include malaria and West Nile virus—the risk of transmission through transfusion is low, as they are much more likely to be acquired by other means.
Transfusion and outcomes: Not a strong record
Transfusion has never undergone safety and efficacy evaluation by the FDA. Given the challenges of conducting a randomized study of transfusion in the perioperative setting, we may never have high-quality data to assess transfusion in this setting.
A few studies merit mention, however. The Transfusion Requirement in Critical Care (TRICC) trial was conducted in 838 critically ill patients in the intensive care setting.18 Patients were randomized to a strategy of either liberal transfusion (begun when hemoglobin fell below 10 g/dL) or restrictive transfusion (begun when hemoglobin fell below 7 g/dL). Thirty-day mortality was similar between patients in the two strategy groups, but the restrictive strategy was associated with significantly lower mortality in at least two subgroups: patients with myocardial infarction and patients with pulmonary edema. Further subgroup analysis found no benefit of early or aggressive transfusion in patients with coronary artery disease or in those requiring mechanical ventilation.
Rao et al performed a meta-analysis of three large international trials of patients with acute coronary syndromes to determine whether blood transfusion to correct anemia in this setting was associated with improved survival.19 They found significantly higher mortality among patients who underwent transfusion compared with those who did not, prompting them to urge caution in the use of transfusion to maintain arbitrary hematocrit levels in stable patients with ischemic heart disease.
Similarly, a risk-adjusted, propensity-matched analysis of 6,301 patients undergoing noncardiac surgery found that receipt of 4 U of blood or more was a predictor of greater mortality, higher risk of infection, and longer hospital stay.20 Moreover, in an observational cohort study of 11,963 patients who underwent isolated coronary artery bypass graft surgery, each unit of red blood cells transfused was associated with an incrementally increased risk of adverse outcome (eg, mortality, renal injury, need for ventilator support, lengthened hospital stay, infection).21 The latter study found that transfusion was the single factor most reliably associated with increased risk of postoperative morbidity.
Additional studies have echoed these findings—ie, that perioperative blood transfusion has been associated with a host of adverse outcomes, including increased morbidity and length of stay, increased rates of postoperative infection, as well as immunosuppression, viral transmission, and acute transfusion reactions.5,22,23
Outcomes and duration of blood storage
An interesting factor in the relation between transfusion and outcomes is the shelf life of the blood being transfused. The FDA currently allows storage of blood for a maximum of 42 days, but a recent study of patients who received red blood cell transfusions during cardiac surgery found that those who received “older blood” (stored for > 14 days) had significantly higher rates of sepsis, prolonged intubation, renal failure, in-hospital mortality, and 1-year mortality compared with those who received “newer blood” (stored for ≤ 14 days).24
These differing outcomes are generally attributed to the so-called storage defect: as blood gets older, it loses components such as 2,3-DPG and adenosine disphosphate, its red cells lose deformability, and it undergoes buildup of cytokines and free hemoglobin. Increased demand for newer blood in light of the storage defect could further intensify pressures on the blood supply.
MANAGEMENT OF PERIOPERATIVE ANEMIA
In light of these shortcomings of blood transfusion, how should anemia be managed perioperatively to reduce or avoid the need for transfusion?
Preoperative evaluation
Vigilance for anemia and related issues in the preoperative evaluation is fundamental. The evaluation should elicit a history of bleeding tendencies, previous transfusions, and symptoms of anemia. Medications should be reviewed with an eye toward any that may predispose to perioperative bleeding and anemia, such as aspirin, clopidogrel, and anticoagulants. During the physical examination, alertness for pallor and petechiae is key, as is attentiveness to symptoms of anemia such as shortness of breath and fatigue.
Overview of management options
Once the cause of anemia is identified, the choice for optimal medical management can be made. Choices broadly consist of pharmacologic and technological options. The former include iron supplements and erythropoiesis-stimulating agents. Among other pharmacologic options are thrombin, collagen, fibrin glue, tranexamic acid, and aminocaproic acid, but these agents are less well studied and will not be discussed here. Technological options include preoperative autologous blood donation, cell salvage, and acute normovolemic hemodilution.
In addition to these options, careful management of anticoagulant and antiplatelet medications should be provided, including discontinuation or substitution of drugs that could hamper clotting perioperatively.
PHARMACOLOGIC OPTIONS
Iron supplementation
Oral iron is available in four preparations: ferrous sulfate, ferrous gluconate, ferrous fumarate, and iron polysaccharide. Gastrointestinal side effects may limit these preparations’ tolerability. Iron supplements with a high elemental value will require fewer pills and fewer doses, reducing the risk or frequency of side effects.
Intravenous (IV) iron preparations are much safer now than they were years ago, when anaphylactic reactions were a concern. The ones generally used in the perioperative setting are iron sucrose and iron gluconate. Unlike the older IV preparations, the use of iron sucrose and iron gluconate often requires a second dose. The effect on hemoglobin levels usually occurs starting at 1 week, with the maximum effect achieved at 2 weeks. Hypotension, arthralgia, abdominal discomfort, and back pain are potential side effects of IV iron.
Efficacy and safety of iron supplementation. Evidence of the efficacy of preoperative iron supplementation is mounting. A study of 569 patients undergoing colorectal cancer surgery found that among the 116 patients who were anemic, intraoperative transfusion was needed in a significantly lower proportion of those who received 2 weeks of preoperative oral iron supplementation (200 mg) compared with those who received no iron therapy (9.4% vs 27.4%; P < .05).26 Similarly, in an uncontrolled study, 10 days of IV iron sucrose starting 4 weeks preoperatively significantly increased hemoglobin levels in 20 patients with iron-deficiency anemia prior to elective orthopedic surgery.27
Risks of infection and cancer progression have been concerns with IV iron therapy. However, no significant association between IV iron therapy and bacteremia was identified in a prospective study of 985 patients receiving chronic hemodialysis.28 The effect of IV iron administration on tumor progression has not been prospectively studied.
In general, IV iron, especially the newer forms, is a safer alternative to blood transfusion. Death occurs at a much lower rate with iron than with blood transfusion (0.4 per million vs 4 per million, respectively), as do life-threatening adverse events (4 per million vs 10 per million, respectively), according to a systematic review by the Network for Advancement of Transfusion Alternatives.29
Erythropoiesis-stimulating agents
Erythropoiesis-stimulating agents (ESAs) include epoetin alfa (erythropoietin), first approved by the FDA in 1989, and the more recently introduced darbepoetin alfa. They are approved to treat anemia in several patient populations, but only epoetin alfa is approved by the FDA explicitly for use in patients undergoing major surgery (to reduce the need for blood transfusions). The ESAs have come under intense scrutiny in recent years over their risk-to-benefit ratio, as detailed below.
The preoperative dosing schedule for epoetin alfa is usually three weekly doses (plus a fourth dose on the day of surgery) if the surgery is scheduled 3 or more weeks in advance. However, daily dosing can be used effectively if the preoperative period is less than 3 weeks, provided that it is continued until 4 days after surgery. Oral iron is necessary throughout the course of epoetin alfa therapy.
Efficacy in reducing transfusions. In a systematic review published in 1998, epoetin alfa was shown to minimize perioperative exposure to allogeneic blood transfusion in patients undergoing orthopedic or cardiac surgery.30 Its benefit was greatest in patients at the highest risk of requiring transfusion. It was effective whether given daily or weekly, and did not significantly increase the risk of thrombotic events when used in surgical patients, although some studies did find an excess of thrombotic events with its use.
In three randomized trials conducted in patients undergoing joint arthroplasty (hip or knee), epoetin alfa was associated with substantial and significant reductions in perioperative blood transfusion compared with placebo or preoperative autologous blood donation.31–33 Rates of deep vein thrombosis (DVT) did not differ significantly between the epoetin alfa and placebo groups.
Concerns over perioperative thromboembolic risk. In early 2007, the FDA was made aware of preliminary results of an open-label study in which 681 patients undergoing elective spinal surgery who did not receive prophylactic anticoagulation were randomized to epoetin alfa plus standard-of-care therapy (pneumatic compression) or standard-of-care therapy alone.34,35 The incidence of DVT was 4.7% in patients treated with epoetin alfa compared with 2.1% in those not receiving epoetin alfa. It is important to note that the available ESAs are prothrombotic and increase thrombotic risk significantly, especially in populations like this one in which pharmacologic DVT prophylaxis is not routinely used.
Based in part on this study, the FDA in 2007 required a boxed warning to be added to the ESAs’ package inserts to specify the increased risk of DVT with their use in surgical patients not receiving prophylactic anticoagulation. The warning urges consideration of the use of DVT prophylaxis in surgical patients receiving an ESA.34,35
TECHNOLOGICAL OPTIONS AND OTHER STRATEGIES
Autologous blood donation: A practice in decline
In cases of elective surgery, autologous blood donation can be used to protect against disease transmission and overcome the challenge of blood type compatibility. Preoperative autologous donation of blood has been a prevalent practice, but its use is declining. One reason is that waste is high (approximately 50% at Cleveland Clinic), which makes this practice more costly than is often realized. Also, autologous blood donation increases the likelihood that the patient will be anemic on the day of surgery, so that he or she may still need allogeneic blood after all, defeating the initial purpose. Despite these limitations, preoperative autologous blood donation remains a useful option for a subset of patients with multiple antibodies for whom donor blood may be difficult to obtain.
Cell salvage
Cell salvage is an innovative technology that recovers the patient’s own blood (after being shed from the surgical incision) for transfusion after filtering and washing. It is particularly well suited to procedures that involve massive blood loss. Cell savage requires technical expertise, however, and involves costs associated with both the machine and disposables.
Restricted postoperative phlebotomy
Phlebotomy accounts for a significant amount of blood loss, especially in intensive care patients with arterial lines. The equivalent of 30% of total blood transfused has been reported to be lost to phlebotomy during an intensive care unit stay.36 Triggers for transfusion cannot be assigned universally based on blood loss from phlebotomy but must consider the patient’s hemodynamic status, cardiac reserve, and other clinical characteristics.
PROMOTING RESPONSIBLE BLOOD PRODUCT USE
Blood is expensive, and in recent years hospitals have experienced increases in the cost of blood and blood products. To promote responsible blood use, we have developed a multipronged approach to blood management at Cleveland Clinic. The program’s cornerstone is increased awareness of the risks associated with blood transfusions. The emphasis is on educating staff physicians and other caregivers about the appropriate use of blood products. We also have implemented a new policy requiring staff authorization for all blood requested in nonemergency situations. Additionally, requests for blood components require adherence to an indication-based ordering process. Finally, data about blood use are shared transparently among physicians, encouraging good clinical practice.
In the first 7 months of the program, we observed decreased utilization of blood products in the inpatient setting. Notably, the reduction in blood use was significantly greater in the surgical population than in the medical population.
CONCULSIONS
Anemia is associated with increased morbidity and mortality in the perioperative setting. Perioperative blood transfusion is one method of raising hemoglobin levels in anemic surgical patients, but it increases perioperative morbidity in the form of acute transfusion reactions, immunosuppression, postoperative infection, and longer hospital stays. Moreover, blood collection continues to lag blood demand. For these reasons, most relevant major medical organizations—including the Association of Blood Banks, the American Red Cross, and the FDA—advise that red blood cell–containing components should not be used to treat anemias that can be corrected with medications. These medical alternatives—all of which can be used in the perioperative setting—include iron supplementation, vitamin B12, and ESAs in select patient groups.
DISCUSSION
Question from the audience: Are there risks involved with autologous blood donation? Are different hemoglobin thresholds used when a patient’s own blood is used?
Dr. Kumar: As I mentioned, preoperative autologous donation is a technique that is less frequently used in our hospital. Autologous transfusion is considered safe only for patients who come to the clinic with normal hemoglobin values. Some patients may not have recovered from their blood loss by the time they come to surgery, so you end up needing to give them more blood because they started out anemic.
Question from the audience: Is there risk to giving patients back their own blood? Do you have to worry about transfusion-induced lung injury, sepsis, or other complications?
Dr. Kumar: As with allogeneic blood, the risk of clerical or clinical error exists with autologous blood: it too needs to be kept on the shelf, taken out, and infused, and the risk of sepsis remains the same.
Anemia is a potent risk factor for mortality and morbidity in surgical patients, and its management has begun to shift away from allogeneic blood transfusion in recent years. This article reviews the clinical importance of perioperative anemia, the role and shortcomings of blood transfusion, and the pros and cons of alternative approaches to managing perioperative anemia. I conclude with an overview of a program for perioperative blood product use at my institution, Cleveland Clinic.
SIGNIFICANCE OF PERIOPERATIVE ANEMIA
Prevalence depends on many factors
The reported prevalence of anemia in surgical patients varies widely—from 5% to 76%1—and depends on the patient’s disease and comorbidities, the surgical procedure and associated blood loss, and the definition of anemia used. The prevalence of preoperative anemia increases with patient age and is higher in women than in men.2
A multiplier of risk
Anemia is an important multiplier of mortality risk. For example, the presence of anemia raises the relative risk of 2-year mortality from 2.05 to 3.37 in patients with chronic kidney disease, from 2.86 to 3.78 in patients with heart failure, and from 4.86 to 6.07 in patients with concomitant heart failure and chronic kidney disease.3
Adverse effects of anemia have been demonstrated specifically in the perioperative setting as well. A large retrospective cohort study showed that a preoperative hemoglobin concentration of less than 6 g/dL increases the risk of death 30 days after surgery by a factor of 26 relative to a concentration of 12 g/dL or greater in surgical patients who declined blood transfusion for religious reasons.4 The anemia-associated mortality risk was especially pronounced among patients with cardiovascular disease.4 Other studies have demonstrated perioperative anemia to be associated with increases in the risk of death,5 cardiac events,6 pneumonia,7 and postoperative delirium.8
IS BLOOD TRANSFUSION THE ANSWER
The use of allogeneic blood transfusion to manage anemia and blood loss is a concept that originated several centuries ago and has changed little over the years.
Blood supply challenges
Blood collection has historically lagged demand, resulting in a blood supply insufficient to meet transfusion needs. According to the federal government’s 2007 National Blood Collection and Utilization Survey Report, 6.89% of US hospitals reported that they cancelled elective surgery on 1 or more days in the prior year because of a lack of blood availability, and 13.5% experienced at least 1 day in which nonsurgical blood needs could not be met.9 Unless practices are changed to increase blood donation, these unmet tranfusion needs may grow.
Joint Commission set to measure blood management
In response to this challenge, an advisory panel formed by the Joint Commission has identified 17 performance measures related to blood conservation and appropriate transfusion.10 These measures are currently in development, and we expect to see some types of metrics in the near future. Such metrics are likely to further prioritize blood management for US hospitals.
Safety of the blood supply: Viral transmission down, TRALI risk persists
The safety of the blood supply has improved markedly. Sophisticated testing and public demand have led to a dramatic decline in the risk of transfusion-related transmission of HIV, hepatitis C virus, and hepatitis B virus.11
Despite this progress, the risk of transfusion-related acute lung injury (TRALI) has persisted in recent years. TRALI is characterized by acute onset of noncardiogenic pulmonary edema within 6 hours of blood product transfusion. Believed to be immune-mediated, TRALI is thought to occur as antibodies to human leukocyte antigens develop, inducing capillary leak syndrome.12 The patients most commonly affected are those who receive plasma from multiparous female donors. A recent evaluation of transfusion-related fatalities reported to the US Food and Drug Administration (FDA) revealed a continual rise in fatal TRALI cases in the United States from 2001 to 2006.13–15 TRALI was implicated in more than half of all transfusion-related fatalities reported to the FDA in 2006, a higher number than for any other single cause.13
At the same time, there is evidence that hemovigilance can reduce TRALI risk. In the United Kingdom, the Serious Hazards of Transfusion Steering Group introduced in late 2003 a policy of using plasma from male donors as much as possible, in view of the association of TRALI with plasma from multiparous female donors. The effort appeared to pay off: whereas TRALI accounted for 6.8% of all transfusion-related adverse events reported in the United Kingdom during the period 1996–2003,16 this proportion declined to just 1.9% in 2006.17
Finally, despite the progress in screening blood for more established infections like HIV and the hepatitis viruses, some additional infections now must be considered when assessing blood supply safety. These include diseases newly recognized as being transmissible by blood, or for which blood donor screening is not currently available, or that are newly emergent infections for which the potential for spread by transfusion is unknown. For such diseases—which include malaria and West Nile virus—the risk of transmission through transfusion is low, as they are much more likely to be acquired by other means.
Transfusion and outcomes: Not a strong record
Transfusion has never undergone safety and efficacy evaluation by the FDA. Given the challenges of conducting a randomized study of transfusion in the perioperative setting, we may never have high-quality data to assess transfusion in this setting.
A few studies merit mention, however. The Transfusion Requirement in Critical Care (TRICC) trial was conducted in 838 critically ill patients in the intensive care setting.18 Patients were randomized to a strategy of either liberal transfusion (begun when hemoglobin fell below 10 g/dL) or restrictive transfusion (begun when hemoglobin fell below 7 g/dL). Thirty-day mortality was similar between patients in the two strategy groups, but the restrictive strategy was associated with significantly lower mortality in at least two subgroups: patients with myocardial infarction and patients with pulmonary edema. Further subgroup analysis found no benefit of early or aggressive transfusion in patients with coronary artery disease or in those requiring mechanical ventilation.
Rao et al performed a meta-analysis of three large international trials of patients with acute coronary syndromes to determine whether blood transfusion to correct anemia in this setting was associated with improved survival.19 They found significantly higher mortality among patients who underwent transfusion compared with those who did not, prompting them to urge caution in the use of transfusion to maintain arbitrary hematocrit levels in stable patients with ischemic heart disease.
Similarly, a risk-adjusted, propensity-matched analysis of 6,301 patients undergoing noncardiac surgery found that receipt of 4 U of blood or more was a predictor of greater mortality, higher risk of infection, and longer hospital stay.20 Moreover, in an observational cohort study of 11,963 patients who underwent isolated coronary artery bypass graft surgery, each unit of red blood cells transfused was associated with an incrementally increased risk of adverse outcome (eg, mortality, renal injury, need for ventilator support, lengthened hospital stay, infection).21 The latter study found that transfusion was the single factor most reliably associated with increased risk of postoperative morbidity.
Additional studies have echoed these findings—ie, that perioperative blood transfusion has been associated with a host of adverse outcomes, including increased morbidity and length of stay, increased rates of postoperative infection, as well as immunosuppression, viral transmission, and acute transfusion reactions.5,22,23
Outcomes and duration of blood storage
An interesting factor in the relation between transfusion and outcomes is the shelf life of the blood being transfused. The FDA currently allows storage of blood for a maximum of 42 days, but a recent study of patients who received red blood cell transfusions during cardiac surgery found that those who received “older blood” (stored for > 14 days) had significantly higher rates of sepsis, prolonged intubation, renal failure, in-hospital mortality, and 1-year mortality compared with those who received “newer blood” (stored for ≤ 14 days).24
These differing outcomes are generally attributed to the so-called storage defect: as blood gets older, it loses components such as 2,3-DPG and adenosine disphosphate, its red cells lose deformability, and it undergoes buildup of cytokines and free hemoglobin. Increased demand for newer blood in light of the storage defect could further intensify pressures on the blood supply.
MANAGEMENT OF PERIOPERATIVE ANEMIA
In light of these shortcomings of blood transfusion, how should anemia be managed perioperatively to reduce or avoid the need for transfusion?
Preoperative evaluation
Vigilance for anemia and related issues in the preoperative evaluation is fundamental. The evaluation should elicit a history of bleeding tendencies, previous transfusions, and symptoms of anemia. Medications should be reviewed with an eye toward any that may predispose to perioperative bleeding and anemia, such as aspirin, clopidogrel, and anticoagulants. During the physical examination, alertness for pallor and petechiae is key, as is attentiveness to symptoms of anemia such as shortness of breath and fatigue.
Overview of management options
Once the cause of anemia is identified, the choice for optimal medical management can be made. Choices broadly consist of pharmacologic and technological options. The former include iron supplements and erythropoiesis-stimulating agents. Among other pharmacologic options are thrombin, collagen, fibrin glue, tranexamic acid, and aminocaproic acid, but these agents are less well studied and will not be discussed here. Technological options include preoperative autologous blood donation, cell salvage, and acute normovolemic hemodilution.
In addition to these options, careful management of anticoagulant and antiplatelet medications should be provided, including discontinuation or substitution of drugs that could hamper clotting perioperatively.
PHARMACOLOGIC OPTIONS
Iron supplementation
Oral iron is available in four preparations: ferrous sulfate, ferrous gluconate, ferrous fumarate, and iron polysaccharide. Gastrointestinal side effects may limit these preparations’ tolerability. Iron supplements with a high elemental value will require fewer pills and fewer doses, reducing the risk or frequency of side effects.
Intravenous (IV) iron preparations are much safer now than they were years ago, when anaphylactic reactions were a concern. The ones generally used in the perioperative setting are iron sucrose and iron gluconate. Unlike the older IV preparations, the use of iron sucrose and iron gluconate often requires a second dose. The effect on hemoglobin levels usually occurs starting at 1 week, with the maximum effect achieved at 2 weeks. Hypotension, arthralgia, abdominal discomfort, and back pain are potential side effects of IV iron.
Efficacy and safety of iron supplementation. Evidence of the efficacy of preoperative iron supplementation is mounting. A study of 569 patients undergoing colorectal cancer surgery found that among the 116 patients who were anemic, intraoperative transfusion was needed in a significantly lower proportion of those who received 2 weeks of preoperative oral iron supplementation (200 mg) compared with those who received no iron therapy (9.4% vs 27.4%; P < .05).26 Similarly, in an uncontrolled study, 10 days of IV iron sucrose starting 4 weeks preoperatively significantly increased hemoglobin levels in 20 patients with iron-deficiency anemia prior to elective orthopedic surgery.27
Risks of infection and cancer progression have been concerns with IV iron therapy. However, no significant association between IV iron therapy and bacteremia was identified in a prospective study of 985 patients receiving chronic hemodialysis.28 The effect of IV iron administration on tumor progression has not been prospectively studied.
In general, IV iron, especially the newer forms, is a safer alternative to blood transfusion. Death occurs at a much lower rate with iron than with blood transfusion (0.4 per million vs 4 per million, respectively), as do life-threatening adverse events (4 per million vs 10 per million, respectively), according to a systematic review by the Network for Advancement of Transfusion Alternatives.29
Erythropoiesis-stimulating agents
Erythropoiesis-stimulating agents (ESAs) include epoetin alfa (erythropoietin), first approved by the FDA in 1989, and the more recently introduced darbepoetin alfa. They are approved to treat anemia in several patient populations, but only epoetin alfa is approved by the FDA explicitly for use in patients undergoing major surgery (to reduce the need for blood transfusions). The ESAs have come under intense scrutiny in recent years over their risk-to-benefit ratio, as detailed below.
The preoperative dosing schedule for epoetin alfa is usually three weekly doses (plus a fourth dose on the day of surgery) if the surgery is scheduled 3 or more weeks in advance. However, daily dosing can be used effectively if the preoperative period is less than 3 weeks, provided that it is continued until 4 days after surgery. Oral iron is necessary throughout the course of epoetin alfa therapy.
Efficacy in reducing transfusions. In a systematic review published in 1998, epoetin alfa was shown to minimize perioperative exposure to allogeneic blood transfusion in patients undergoing orthopedic or cardiac surgery.30 Its benefit was greatest in patients at the highest risk of requiring transfusion. It was effective whether given daily or weekly, and did not significantly increase the risk of thrombotic events when used in surgical patients, although some studies did find an excess of thrombotic events with its use.
In three randomized trials conducted in patients undergoing joint arthroplasty (hip or knee), epoetin alfa was associated with substantial and significant reductions in perioperative blood transfusion compared with placebo or preoperative autologous blood donation.31–33 Rates of deep vein thrombosis (DVT) did not differ significantly between the epoetin alfa and placebo groups.
Concerns over perioperative thromboembolic risk. In early 2007, the FDA was made aware of preliminary results of an open-label study in which 681 patients undergoing elective spinal surgery who did not receive prophylactic anticoagulation were randomized to epoetin alfa plus standard-of-care therapy (pneumatic compression) or standard-of-care therapy alone.34,35 The incidence of DVT was 4.7% in patients treated with epoetin alfa compared with 2.1% in those not receiving epoetin alfa. It is important to note that the available ESAs are prothrombotic and increase thrombotic risk significantly, especially in populations like this one in which pharmacologic DVT prophylaxis is not routinely used.
Based in part on this study, the FDA in 2007 required a boxed warning to be added to the ESAs’ package inserts to specify the increased risk of DVT with their use in surgical patients not receiving prophylactic anticoagulation. The warning urges consideration of the use of DVT prophylaxis in surgical patients receiving an ESA.34,35
TECHNOLOGICAL OPTIONS AND OTHER STRATEGIES
Autologous blood donation: A practice in decline
In cases of elective surgery, autologous blood donation can be used to protect against disease transmission and overcome the challenge of blood type compatibility. Preoperative autologous donation of blood has been a prevalent practice, but its use is declining. One reason is that waste is high (approximately 50% at Cleveland Clinic), which makes this practice more costly than is often realized. Also, autologous blood donation increases the likelihood that the patient will be anemic on the day of surgery, so that he or she may still need allogeneic blood after all, defeating the initial purpose. Despite these limitations, preoperative autologous blood donation remains a useful option for a subset of patients with multiple antibodies for whom donor blood may be difficult to obtain.
Cell salvage
Cell salvage is an innovative technology that recovers the patient’s own blood (after being shed from the surgical incision) for transfusion after filtering and washing. It is particularly well suited to procedures that involve massive blood loss. Cell savage requires technical expertise, however, and involves costs associated with both the machine and disposables.
Restricted postoperative phlebotomy
Phlebotomy accounts for a significant amount of blood loss, especially in intensive care patients with arterial lines. The equivalent of 30% of total blood transfused has been reported to be lost to phlebotomy during an intensive care unit stay.36 Triggers for transfusion cannot be assigned universally based on blood loss from phlebotomy but must consider the patient’s hemodynamic status, cardiac reserve, and other clinical characteristics.
PROMOTING RESPONSIBLE BLOOD PRODUCT USE
Blood is expensive, and in recent years hospitals have experienced increases in the cost of blood and blood products. To promote responsible blood use, we have developed a multipronged approach to blood management at Cleveland Clinic. The program’s cornerstone is increased awareness of the risks associated with blood transfusions. The emphasis is on educating staff physicians and other caregivers about the appropriate use of blood products. We also have implemented a new policy requiring staff authorization for all blood requested in nonemergency situations. Additionally, requests for blood components require adherence to an indication-based ordering process. Finally, data about blood use are shared transparently among physicians, encouraging good clinical practice.
In the first 7 months of the program, we observed decreased utilization of blood products in the inpatient setting. Notably, the reduction in blood use was significantly greater in the surgical population than in the medical population.
CONCULSIONS
Anemia is associated with increased morbidity and mortality in the perioperative setting. Perioperative blood transfusion is one method of raising hemoglobin levels in anemic surgical patients, but it increases perioperative morbidity in the form of acute transfusion reactions, immunosuppression, postoperative infection, and longer hospital stays. Moreover, blood collection continues to lag blood demand. For these reasons, most relevant major medical organizations—including the Association of Blood Banks, the American Red Cross, and the FDA—advise that red blood cell–containing components should not be used to treat anemias that can be corrected with medications. These medical alternatives—all of which can be used in the perioperative setting—include iron supplementation, vitamin B12, and ESAs in select patient groups.
DISCUSSION
Question from the audience: Are there risks involved with autologous blood donation? Are different hemoglobin thresholds used when a patient’s own blood is used?
Dr. Kumar: As I mentioned, preoperative autologous donation is a technique that is less frequently used in our hospital. Autologous transfusion is considered safe only for patients who come to the clinic with normal hemoglobin values. Some patients may not have recovered from their blood loss by the time they come to surgery, so you end up needing to give them more blood because they started out anemic.
Question from the audience: Is there risk to giving patients back their own blood? Do you have to worry about transfusion-induced lung injury, sepsis, or other complications?
Dr. Kumar: As with allogeneic blood, the risk of clerical or clinical error exists with autologous blood: it too needs to be kept on the shelf, taken out, and infused, and the risk of sepsis remains the same.
- Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med 2004; 116(suppl 7A):58S–69S.
- Kulier A, Gombotz H. Perioperative anemia [in German]. Anaesthesist 2001; 50:73–86.
- Herzog CA, Muster HA, Li S, Collins AJ. Impact of congestive heart failure, chronic kidney disease, and anemia on survival in the Medicare population. J Card Fail 2004; 10:467–472.
- Carson JL, Duff A, Poses RM, et al. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 1996; 348:1055–1060.
- Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ. The relationship between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma 2002; 16:39–44.
- Nelson AH, Fleisher LA, Rosenbaum SH. Relationship between postoperative anemia and cardiac morbidity in high-risk vascular patients in the intensive care unit. Crit Care Med 1993; 21:860–866.
- Faris PM, Spence RK, Larholt KM, Sampson AR, Frei D. The predictive power of baseline hemoglobin for transfusion risk in surgery patients. Orthopedics 1999; 22(suppl 1):s135–s140.
- Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH. The association of intraoperative factors with the development of postoperative delirium. Am J Med 1998; 105:380–384.
- US Department of Health and Human Services. The 2007 National Blood Collection and Utilization Survey. Available at: http://www.aabb.org/Documents/Programs_and_Services/Data_Center/07nbcusrpt.pdf. Accessed March 9, 2009.
- The Joint Commission. Performance measurement initiatives. Available at http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Blood+Management+-+Utilization.htm.
- Busch MP, Kleinman SH, Nemo GJ. Current and emerging infectious risks of blood transfusions. JAMA 2003; 289:959–962.
- Silliman CC, Ambruso DR, Boshkov LK. Transfusion-related acute lung injury. Blood 2005; 105:2266–2273.
- Benjamin RJ. Transfusion and transplantation safety: American Red Cross concerns. PowerPoint slides presented at Department of Health and Human Services Advisory Committee on Blood Safety and Availability meeting, May 10–11, 2007. Available at: http://www.hhs.gov/ophs/bloodsafety/presentations/Benjamin0507.pdf. Accessed March 9, 2009.
- Holness L. Transfusion related acute lung injury (TRALI): the FDA current view. PowerPoint slides presented at FDA Blood Products Advisory Committee meeting, July 22–23, 2004. Available at: http://www.fda.gov/OHRMS/DOCKETS/ac/04/briefing/2004-4057b1_01.pdf. Accessed March 9, 2009.
- Williams AE. Transfusion related acute lung injury (TRALI). PowerPoint slides presented at FDA Blood Products Advisory Committee meeting, April 27, 2007. Available at: http://www.fda.gov/ohrms/dockets/ac/07/slides/2007-4300S2-05.ppt. Accessed March 9, 2009.
- Stainsby D, Cohen H, Jones H, et al. Serious Hazards of Transfusion—Annual Report 2003. Published July 5, 2004. Available at: http://www.shotuk.org/SHOT%20Report%202003.pdf. Accessed April 29, 2009.
- Taylor C, Cohen H, Stainsby D, et al. Serious Hazards of Transfusion—Annual Report 2006. Published November 20, 2007. Available at: http://www.shotuk.org/SHOT_report_2006.pdf. Accessed April 29, 2009.
- Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 1999; 340:409–417.
- Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004; 292:1555–1562.
- Dunne JR, Malone D, Tracy JK, et al. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res 2002; 102:237–244.
- Koch CG, Li L, Duncan AI, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006; 34:1608–1616.
- Rady MY, Ryan T, Starr NJ. Perioperative determinants of morbidity and mortality in elderly patients undergoing cardiac surgery. Crit Care Med 1998; 26:225–235.
- Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. First of two parts—blood transfusion. N Engl J Med 1999; 340:438–447.
- Koch CG, Li L, Sessler DI, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 2008; 358:1229–1239.
- Goodnough LT, Shander A. Blood management. Arch Pathol Lab Med 2007; 131:695–701.
- Okuyama M, Ikeda K, Shibata T, et al. Preoperative iron supplementation and intraoperative transfusion during colorectal cancer surgery. Surg Today 2005; 35:36–40.
- Theusinger OM, Leyvraz PF, Schanz U, et al. Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology 2007; 107:923–927.
- Hoen B, Paul-Dauphin A, Kessler M. Intravenous iron administration does not significantly increase the risk of bacteremia in chronic hemodialysis patients. Clin Nephrol 2002; 57:457–461.
- Beris P, Muñoz M, García-Erce JA, et al. Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth 2008; 100:599–604.
- Laupacis A, Fergusson D. Erythropoietin to minimize perioperative blood transfusion: a systematic review of randomized trials: The International Study of Perioperative Transfusion (ISPOT) Investigators. Transfus Med 1998; 8:309–317.
- Feagan BG, Wong CJ, Kirkley A, et al. Erythropoietin with iron supplementation to prevent allogeneic blood transfusion in total hip joint arthroplasty: a randomized, controlled trial. Ann Intern Med 2000; 133:845–854.
- Stowell CP, Chandler H, Jové M, et al. An open-label, randomized study to compare the safety and efficacy of perioperative epoetin alfa with preoperative autologous blood donation in total joint arthroplasty. Orthopedics 1999; 22(suppl 1):s105–s112.
- de Andrade JR, Jové M, Landon G, et al. Baseline hemoglobin as a predictor of risk of transfusion and response to Epoetin alfa in orthopedic surgery patients. Am J Orthop 1996; 25:533–542.
- Procrit [package insert]. Raritan, NJ: Ortho Biotech Products LP; 2009.
- Epogen [package insert]. Thousand Oaks, CA: Amgen Inc.; 2009.
- Smoller BR, Kuskall MS. Phlebotomy for diagnostic laboratory tests in adults: pattern of use and effect on transfusion requirements. N Engl J Med 1986; 314:1233–1235.
- Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med 2004; 116(suppl 7A):58S–69S.
- Kulier A, Gombotz H. Perioperative anemia [in German]. Anaesthesist 2001; 50:73–86.
- Herzog CA, Muster HA, Li S, Collins AJ. Impact of congestive heart failure, chronic kidney disease, and anemia on survival in the Medicare population. J Card Fail 2004; 10:467–472.
- Carson JL, Duff A, Poses RM, et al. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 1996; 348:1055–1060.
- Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ. The relationship between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma 2002; 16:39–44.
- Nelson AH, Fleisher LA, Rosenbaum SH. Relationship between postoperative anemia and cardiac morbidity in high-risk vascular patients in the intensive care unit. Crit Care Med 1993; 21:860–866.
- Faris PM, Spence RK, Larholt KM, Sampson AR, Frei D. The predictive power of baseline hemoglobin for transfusion risk in surgery patients. Orthopedics 1999; 22(suppl 1):s135–s140.
- Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH. The association of intraoperative factors with the development of postoperative delirium. Am J Med 1998; 105:380–384.
- US Department of Health and Human Services. The 2007 National Blood Collection and Utilization Survey. Available at: http://www.aabb.org/Documents/Programs_and_Services/Data_Center/07nbcusrpt.pdf. Accessed March 9, 2009.
- The Joint Commission. Performance measurement initiatives. Available at http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Blood+Management+-+Utilization.htm.
- Busch MP, Kleinman SH, Nemo GJ. Current and emerging infectious risks of blood transfusions. JAMA 2003; 289:959–962.
- Silliman CC, Ambruso DR, Boshkov LK. Transfusion-related acute lung injury. Blood 2005; 105:2266–2273.
- Benjamin RJ. Transfusion and transplantation safety: American Red Cross concerns. PowerPoint slides presented at Department of Health and Human Services Advisory Committee on Blood Safety and Availability meeting, May 10–11, 2007. Available at: http://www.hhs.gov/ophs/bloodsafety/presentations/Benjamin0507.pdf. Accessed March 9, 2009.
- Holness L. Transfusion related acute lung injury (TRALI): the FDA current view. PowerPoint slides presented at FDA Blood Products Advisory Committee meeting, July 22–23, 2004. Available at: http://www.fda.gov/OHRMS/DOCKETS/ac/04/briefing/2004-4057b1_01.pdf. Accessed March 9, 2009.
- Williams AE. Transfusion related acute lung injury (TRALI). PowerPoint slides presented at FDA Blood Products Advisory Committee meeting, April 27, 2007. Available at: http://www.fda.gov/ohrms/dockets/ac/07/slides/2007-4300S2-05.ppt. Accessed March 9, 2009.
- Stainsby D, Cohen H, Jones H, et al. Serious Hazards of Transfusion—Annual Report 2003. Published July 5, 2004. Available at: http://www.shotuk.org/SHOT%20Report%202003.pdf. Accessed April 29, 2009.
- Taylor C, Cohen H, Stainsby D, et al. Serious Hazards of Transfusion—Annual Report 2006. Published November 20, 2007. Available at: http://www.shotuk.org/SHOT_report_2006.pdf. Accessed April 29, 2009.
- Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med 1999; 340:409–417.
- Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004; 292:1555–1562.
- Dunne JR, Malone D, Tracy JK, et al. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res 2002; 102:237–244.
- Koch CG, Li L, Duncan AI, et al. Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 2006; 34:1608–1616.
- Rady MY, Ryan T, Starr NJ. Perioperative determinants of morbidity and mortality in elderly patients undergoing cardiac surgery. Crit Care Med 1998; 26:225–235.
- Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. First of two parts—blood transfusion. N Engl J Med 1999; 340:438–447.
- Koch CG, Li L, Sessler DI, et al. Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 2008; 358:1229–1239.
- Goodnough LT, Shander A. Blood management. Arch Pathol Lab Med 2007; 131:695–701.
- Okuyama M, Ikeda K, Shibata T, et al. Preoperative iron supplementation and intraoperative transfusion during colorectal cancer surgery. Surg Today 2005; 35:36–40.
- Theusinger OM, Leyvraz PF, Schanz U, et al. Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology 2007; 107:923–927.
- Hoen B, Paul-Dauphin A, Kessler M. Intravenous iron administration does not significantly increase the risk of bacteremia in chronic hemodialysis patients. Clin Nephrol 2002; 57:457–461.
- Beris P, Muñoz M, García-Erce JA, et al. Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth 2008; 100:599–604.
- Laupacis A, Fergusson D. Erythropoietin to minimize perioperative blood transfusion: a systematic review of randomized trials: The International Study of Perioperative Transfusion (ISPOT) Investigators. Transfus Med 1998; 8:309–317.
- Feagan BG, Wong CJ, Kirkley A, et al. Erythropoietin with iron supplementation to prevent allogeneic blood transfusion in total hip joint arthroplasty: a randomized, controlled trial. Ann Intern Med 2000; 133:845–854.
- Stowell CP, Chandler H, Jové M, et al. An open-label, randomized study to compare the safety and efficacy of perioperative epoetin alfa with preoperative autologous blood donation in total joint arthroplasty. Orthopedics 1999; 22(suppl 1):s105–s112.
- de Andrade JR, Jové M, Landon G, et al. Baseline hemoglobin as a predictor of risk of transfusion and response to Epoetin alfa in orthopedic surgery patients. Am J Orthop 1996; 25:533–542.
- Procrit [package insert]. Raritan, NJ: Ortho Biotech Products LP; 2009.
- Epogen [package insert]. Thousand Oaks, CA: Amgen Inc.; 2009.
- Smoller BR, Kuskall MS. Phlebotomy for diagnostic laboratory tests in adults: pattern of use and effect on transfusion requirements. N Engl J Med 1986; 314:1233–1235.
KEY POINTS
- Anemia is a potent multiplier of morbidity and mortality risk, including in the perioperative setting.
- The Joint Commission plans to implement a performance measure on blood management in the near future.
- While the safety of the blood supply has improved markedly from the standpoint of infection transmission, other risks from transfusion persist, including transfusion-related acute lung injury and emerging infections.
- The preoperative evaluation should elicit a history of bleeding tendencies, previous transfusions, and symptoms of anemia. Medications should be reviewed with an eye toward those that may need to be stopped to avoid a predisposition to bleeding (eg, antiplatelets, anticoagulants).
- Use of ESAs minimizes the need for blood transfusion in patients undergoing orthopedic and other surgeries, but they raise the risk of thromboembolism in the absence of prophylactic anticoagulation.