User login
In 2009, the VA announced a goal of ending veteran homelessness by 2015.1 The primary focus of this new policy has been housing veterans experiencing chronic homelessness, many of whom languish outside the VA housing system. Since that time, progress has been made with point-in-time enumerations indicating that veteran homelessness has decreased nationally. Despite this progress, however, more than 55,000 veterans are still estimated to experience homelessness each night.2
Historically, the VA has offered an array of services specifically meant to alleviate veteran homelessness (grant, per diem, and other transitional housing programs; vocational rehabilitation, etc).3 The majority of these programs require some period of veteran abstinence as a condition for providing housing services. The recent move toward permanent “housing first” programs with few conditions for enrollment and participation provides new opportunities for housing veterans experiencing chronic homelessness, who are the specific target of the goal of ending veteran homelessness.4
Because veterans experiencing chronic homelessness have additional, substantial need for medical, psychiatric, and substance-abuse services, the VA also offers these services to this population.5-7 Veterans experiencing homelessness also may access parallel non-VA services.8 Information about veterans outside of traditional VA housing services, specifically those housed in low-demand shelters, is needed to develop services for this population and will be critical to success in ending veteran homelessness.
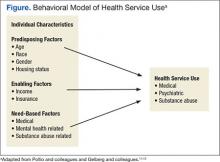
The Behavioral Model of Health Services Use9-11 and its later refinement, the Behavioral Model for Vulnerable Persons,12 have been used to conceptualize health care service use (Figure). In these models, health service use is predicted by 3 types of factors: predisposing factors (eg, age, race, gender, residential history), enabling factors (eg, availability, accessibility, affordability, acceptability), and service need factors (eg, substance-use disorders, mental health problems, physical health problems).
Studies applying these models of health care service use to both general homeless populations and, specifically to populations of veterans experiencing homelessness have found that service use is most influenced by need-based factors (eg, drug abuse, poor health, mental health problems).6,12-20 These same studies indicate that predisposing factors (eg, age, race, and gender) and enabling factors (eg, insurance, use of other services, and usual place of care) are also associated with service use, though less consistently.
Studies focused on veterans experiencing homelessness, however, included only treatment-seeking populations, which are not necessarily representative of the broader population of veterans experiencing homelessness. Additionally, none of these prior studies focused on the unique subset of veterans residing in low-demand shelters (characterized by unlimited duration of stay, no government ID or fee required for entry, and no requirement for service participation). This is a population that seems to be less engaged in services but nevertheless is challenged.21 This study, therefore, is focused on nontreatment seeking veterans residing in a low-demand shelter. The study applied the Behavioral Model of Health Services Use and the Behavioral Model for Vulnerable Persons to examine use of VA and non-VA services.
Study Parameters
This study was conducted in Fort Worth, Texas, the 17th largest city in the U.S. with more than 810,000 residents.22 In 2013, a biennial point-in-time count identified about 2,300 individuals who were homeless in Fort Worth. Most were found in emergency shelters (n = 1,126, 50%) or transitional housing (n = 965, 40%). Slightly more than 10% (n = 281) were found to be unsheltered: sleeping on the streets or in encampments, automobiles, or abandoned buildings.23 Although national estimates identify 12% of all adults who are homeless as veterans,2 only 8% (n = 189) of people experiencing homelessness in Fort Worth reported military service.23
Access to the full array of VA emergency department (ED), inpatient, and outpatient medical, psychiatric, and substance-abuse services are available to veterans experiencing homelessness at the Dallas VA Medical Center (DVAMC), located 35 miles away. Only VA outpatient medical, psychiatric, and substance-related services are available in Fort Worth through the VA Outpatient Clinic and Health Care for the Homeless Veterans (HCHV) program. If veterans experiencing homelessness seek care outside of the VA system, a comprehensive network of emergency, inpatient and outpatient medical, psychiatric, and substance-related services is available in Fort Worth.
Sample
The study sample included 110 adult male veterans randomly recruited as they awaited admission to a private, low-demand emergency shelter. The study excluded veterans with a dishonorable discharge to ensure participants were eligible for VA services. Institutional review board approvals were obtained prior to the study from the University of Texas at Arlington and DVAMC. All participants provided informed consent and were given a $5 gift for their involvement.
Instruments
Through structured interviews, experienced research staff collected demographics, history of homelessness, military service, and substance abuse in the previous 30 days. Data on alcohol and drug problems in the past 12 months were obtained using the Short Michigan Alcohol Screening Test (SMAST) and the Drug Abuse Screening Test. The Veterans RAND 12-Item Health Survey (VR-12) was used to measure physical and mental health functioning in the previous 4 weeks. Finally, participants reported their use of VA or non-VA medical (ED, inpatient, and outpatient), psychiatric (ED, inpatient, and outpatient), and substance abuse-related (inpatient and outpatient) services in the 12 months prior to the interview. These measures have been shown to be valid and reliable with acceptable psychometrics.24-26
Data Analysis
Statistical analysis was completed using IBM SPSS Statistics version 19. Descriptive data were summarized using counts, percentages, means, and standard deviations. A dichotomous variable for alcohol abuse was defined as SMAST score ≥ 3. A variable representing participant’s VR-12 mental component summary scores was used as an indicator of mental health functioning.
McNemar’s test was used to compare the use of VA and non-VA medical, psychiatric, and substance-related services using dichotomous variables for each overall sector as well as respective sector subcomponent services (emergency, inpatient, and outpatient for medical and psychiatric sectors and inpatient and outpatient for the substance-related sector). Statistical significance level was set at α = .05.
Logistic regression was used to predict psychiatric and substance abuse-related service use with separate dependent variables for VA, non-VA, and both VA and non-VA services. Need-based factors included in all models as independent variables were mental health functioning, alcohol abuse, and a dichotomous variable representing cocaine use in the previous 30 days. Independent variables for the other service sectors were included as enabling factors (eg, medical and substance-related problems predicting psychiatric service use), aligning all service use variables in the model to the same provider system (eg, VA service sector independent variables with VA service sector dependent variables).
Results
The sample mean age was 49.2 years (SD = 9.2), and fewer than half (n = 45, 41%) were white. Three-fourths (n = 82, 75%) had ever been married, and few participants (n = 5, 5%) were currently married. Total mean lifetime experience of homelessness was 3.9 years (SD = 4.3). One-third of the samples participants (n = 36, 33%) reported that their current episode of homelessness had lasted 1 year or longer. Most had an adult felony conviction (n = 78, 71%) and a history of incarceration as an adult (n = 104, 95%). All military branches were represented, with 49% serving in the Army, 23% in the Marine Corps, 17% in the Navy, 10% in the Air Force, and 1% in the Coast Guard.
Most of the sample’s veterans served during the Vietnam era (n = 43, 43%) or the post-Vietnam era (n = 49, 45%), but 12 (11%) served during the Persian Gulf era (including Operation Iraqi Freedom and Operation Enduring Freedom). Few received a nonservice connected VA pension (n = 21, 19%) or service-connected disability benefits (n = 20, 18%). The mean income earned in the previous 30 days was $466 (SD = $431). None of these predisposing factors were associated with any service variables.
The sample’s mean VR-12 physical functioning score was 43.8 (SD = 9.1), which was significantly higher (t = 6.2, df = 109, P < .001) than the 38.4 (SD = 12.2) population norm used with the instrument. The sample’s mean mental health functioning score of 39.4 (SD = 14.3) was significantly lower (t = -8.6, df = 109, P < .001) than the population norm (51.1, SD = 11.4).27 Substance-related problems were prevalent, with an identified alcohol problem in 62% (n = 68) and a drug problem in 79% (n = 87) of participants. More than half reported illicit drug use in the past 30 days (n = 61, 56%), especially cocaine (n = 42, 38%) and marijuana (n = 37, 33%).
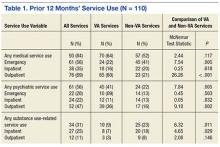
The majority of veterans (n = 96, 87%) reported using some type of service in the past 12 months (Table 1). Most survey respondents used medical services. About half used psychiatric services, and almost one-third used substance-related services. More veterans used non-VA ED services than used VA ED services. More veterans used VA outpatient medical services than used non-VA outpatient medical services. Examining service sectors indicated that more veterans used VA psychiatric services than used non-VA psychiatric services, especially VA outpatient psychiatric services. More veterans used non-VA substance abuse-related services, especially outpatient services, rather than similar services offered by the VA.
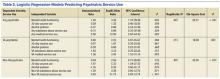
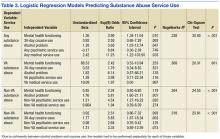
Separate logistic regression models predicted use of psychiatric and substance-abuse services with 3 models (VA, non-VA, or any service use) for each dependent variable from independent variables that reflected need and enabling factors (Tables 2 and 3). Demographic predisposing factors, which were not associated with service use, were not included as covariates in these models. For the model predicting the use of non-VA substance-abuse services, collinearity between the alcohol-abuse and cocaine-abuse variables required separate models for each of the 2 variables.
Medical sector service use predicted psychiatric sector service use in all models. In fact, VA medical service use was the only predictor of use of VA psychiatric services. Lower mental health functioning predicted the use of any (VA or non-VA) psychiatric service use. In addition to the use of medical services, 30-day cocaine use predicted non-VA psychiatric service use.
Any substance-related sector service use was predicted by lower mental health functioning, self-reported alcohol problem, and any medical services utilization. No independent variables included in the model predicted any VA substance-related service use. Non-VA substance abuse service use was predicted by non-VA psychiatric service use and alcohol abuse. In the separate analysis that replaced alcohol problems with 30-day cocaine use variable, only 30-day cocaine use predicted non-VA substance-related service utilization.
Discussion
This study examined the use of medical, psychiatric, and substance-abuse services by randomly sampled veterans from a low-demand emergency shelter. Random selection of the sample and its high (98%) participation rate virtually eliminated potential for bias within this sample. Another strength of this study is its focus on low-demand shelter users—a population that has not been well studied. This low-demand shelter-dwelling population of veterans experiencing homelessness is of interest because more substance-abuse problems and histories of incarceration seem to make them especially disadvantaged and challenged.
The limitation of the sample to users of a low-demand shelter at only 1 location may reduce generalizability to other veteran homeless populations and settings. The study also may not generalize to populations of female veterans experiencing homelessness. Another limitation of the study is that it did not use diagnostic assessments for psychiatric and substance use disorders and objective collateral information such as agency record data. Finally, although the limited size of the sample may have been insufficient to adequately test certain hypotheses, it was a relatively large sample of this population and was large enough to yield significant findings.
This study found that need-based factors predicted the use of some service sectors intended for those needs. For example, mental health functioning appropriately predicted any psychiatric service use, and presence of an alcohol problem appropriately predicted any substance abuse service use. Specifically for non-VA services, both cocaine use and presence of an alcohol problem in separate models predicted substance-abuse service use. However for VA substance-abuse services, neither cocaine use nor presence of an alcohol problem predicted service use. Despite the high need, very few veterans used substance-abuse services, and they rarely used VA substance-abuse services.
For 2 service sectors, need-based factors predicted the use of services intended for other needs. Cocaine use predicted non-VA psychiatric service use, and low mental health functioning predicted substance-abuse service use. One potential explanation for this finding could be that providers or patients incorrectly classified cocaine-related substance use problems as psychiatric. The VR-12 mental health functioning measure also may have incorrectly classified cocaine-related problems as psychiatric.
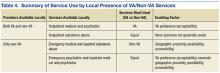
Three enabling factors predicted service use by sector and type. The first 2 are preference for VA-provided services and the geographic availability of services, which competed for veterans’ selection of service providers. When both VA and non-VA services were present in Fort Worth, a preference for VA-provided services was observed, with the exception of outpatient substance abuse services which were highly underutilized in general. No preference was observed for any non-VA services when both were present. When VA services were not present in Fort Worth, veterans used geographically available non-VA providers for some services, but for other services they used Dallas-based VA and Fort Worth-based non-VA providers equally (Table 3 and Table 4).
The third enabling factor influencing service use was through other service use as an enabling pathway. Those veterans who opted out of locally available services in favor of VA services in Dallas may have been prompted to do so by provider referrals, which were further facilitated by VA and public transportation between Fort Worth and Dallas. The most consistent enabling pathway was medical service use, which predicted all types of psychiatric service use (VA and non-VA combined, VA only, and non-VA only), and any substance-related service use. Psychiatric service use predicted substance abuse service use but only in non-VA settings; no pathways led from VA medical or psychiatric services to VA substance abuse services.
Conclusions
These findings suggest, in large part, the validity of the Andersen and Gelberg models of health care service use. Consistent with prior studies, need-based factors predicted the use of any psychiatric and substance-related sector services as well as the use of non-VA subcomponent services for both sectors. Also consistent with prior studies, enabling factors (medical sector service use) predicted service use, with the exception of VA or non-VA substance-abuse services. Unlike prior studies, however, predisposing factors (eg, age, race, marital status, and income) were not associated with service use.
This study could not determine why veterans underutilized substance-abuse services, even those available locally to them in Fort Worth. One possible barrier to care is that the services are designed or delivered in a manner that does not engage these veterans (eg, expectations regarding abstinence or service involvement). Another barrier could be that referral pathways between VA outpatient medical and psychiatric service providers and VA substance-related services are not sufficiently facilitative. Future investigations could build upon the findings of this study by collecting data that could help assess these potential barriers.
The data from this study suggest 3 opportunities to improve the utilization of services most needed by this population. The first opportunity would be to accurately differentiate between substance abuse and psychiatric problems in clinical assessment and identify the most appropriate type of care. Another opportunity, linked closely to the first, would be to facilitate more effective and efficient referral pathways among VA service sectors, especially from medical and psychiatric services to substance-abuse services. Another strategy to improve referral pathways would be for VA service networks to systematically examine local service systems for factors or processes that may disrupt integrated care and implement program improvements.28 For homeless veterans navigating an inherently complex VA health care system, peer-to-peer and patient navigator programs have helped improve service efficiency and service outcomes.29 The third opportunity to improve utilization of services would be to ensure geographic availability and accessibility by strategic placement of these services.
The results from this study, while informative, point directly to needed areas for further inquiry to inform public health response. Although the low-demand shelter users are a particularly challenging subgroup of veterans experiencing chronic homelessness, other equally challenging populations warrant additional study. For example, veterans outside of both VA and community services (eg, unsheltered populations) are likely to require different approaches to engage in appropriate services. Additionally, changes to the homeless policy implemented in the period after this sample was recruited suggest the need to revisit the service-using behaviors of this population. Finally, interventions developed as part of the national response need to be assessed for their ability to engage these difficult-to-reach veterans.
Acknowledgements
This study was funded by a U.S. Department of Veterans Affairs Office of Academic Affiliations Pre-Doctoral Social Work Research Fellowship award.
1. U.S. Department of Veterans Affairs. Homeless veterans: VA is working to end homelessness among veterans. U.S. Department of Veterans Affairs Website. www.va.gov/homeless/about_the_initiative.asp#one. Updated January 26, 2016. Accessed February 16, 2016.
2. Henry M, Cortes A, Morris S, Abt Associates; U. S. Department of Housing and Urban Development Office of Community Planning and Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1 Point-in-Time Estimates of Homelessness. HUD Exchange Website. https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Published October 2014. Accessed February 16, 2016.
3. U.S. Department of Veterans Affairs. Homeless Veterans: Housing Assistance. U.S. Department of Veterans Affairs Web site. http://www.va.gov/homeless/housing.asp. Updated November 5, 2015. Accessed February 16, 2016.
4. Austin EL, Pollio DE, Holmes S, et al. VA's expansion of supportive housing: successes and challenges on the path to Housing First. Psychiatr Serv. 2014;65(5):641-647.
5. Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455-460.
6. Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33(11):1132-1144.
7. McQuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental health illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
8. Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27-31.
9. Andersen RM. A behavioral model of families use of health services: Research Series No. 25. Chicago, IL: University of Chicago Center for Health Administrative Studies; 1968.
10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
11. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
12. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302.
13. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
14. Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212-230.
15. Gamache G, Rosenheck RA, Tessler R. Factors predicting choice of provider among homeless veterans with mental illness. Psychiatr Serv. 2000;51(8):1024-1028.
16. Wenzel SL, Audrey Burnam, M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158-1169.
17. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
18. Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381-393.
19. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Anderson Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20-30.
20. Linton KF, Shafer MS. Factors associated with the health service use of unsheltered, chronically homeless adults. Soc Work Public Health. 2013;29(1):73-80.
21. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psych Serv. 2014;65(6):751-757.
22. U.S. Census Bureau. State & County Quick Facts: Fort Worth (city), Texas. U.S. Census Bureau Website. http://quickfacts.census.gov/qfd/states/48/4827000.html. Revised December 2, 2015. Accessed February 17, 2016.
23. Tarrant County Homeless Coalition. 2014 point in time count results. Tarrant County Homeless Coalition Website. http://www.ahomewithhope.org/staff/local-data-research/2014-homeless-count/. Accessed February 16, 2016.
24. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses. Int J Method Psychiatr Res. 2004;13(3):184-191.
25. Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): What it is and how it is Used. Washington, DC: Veterans Health Administration; 2009.
26. Fischer J, Corcoran K, eds. Measures for Clinical Practice and Research: A Sourcebook. 4th ed. New York, NY: Oxford University Press; 2013.
27. Selim AJ, Rogers W, Fleishman JA, Qian SX, Finke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18(1):43-52.
28. Blue-Howells J, McQuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219-231.
29. Piette JD, Holtz B, Beard AJ, et al; Ann Arbor PACT Steering Committee. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1(4):615-623.
In 2009, the VA announced a goal of ending veteran homelessness by 2015.1 The primary focus of this new policy has been housing veterans experiencing chronic homelessness, many of whom languish outside the VA housing system. Since that time, progress has been made with point-in-time enumerations indicating that veteran homelessness has decreased nationally. Despite this progress, however, more than 55,000 veterans are still estimated to experience homelessness each night.2
Historically, the VA has offered an array of services specifically meant to alleviate veteran homelessness (grant, per diem, and other transitional housing programs; vocational rehabilitation, etc).3 The majority of these programs require some period of veteran abstinence as a condition for providing housing services. The recent move toward permanent “housing first” programs with few conditions for enrollment and participation provides new opportunities for housing veterans experiencing chronic homelessness, who are the specific target of the goal of ending veteran homelessness.4
Because veterans experiencing chronic homelessness have additional, substantial need for medical, psychiatric, and substance-abuse services, the VA also offers these services to this population.5-7 Veterans experiencing homelessness also may access parallel non-VA services.8 Information about veterans outside of traditional VA housing services, specifically those housed in low-demand shelters, is needed to develop services for this population and will be critical to success in ending veteran homelessness.
The Behavioral Model of Health Services Use9-11 and its later refinement, the Behavioral Model for Vulnerable Persons,12 have been used to conceptualize health care service use (Figure). In these models, health service use is predicted by 3 types of factors: predisposing factors (eg, age, race, gender, residential history), enabling factors (eg, availability, accessibility, affordability, acceptability), and service need factors (eg, substance-use disorders, mental health problems, physical health problems).
Studies applying these models of health care service use to both general homeless populations and, specifically to populations of veterans experiencing homelessness have found that service use is most influenced by need-based factors (eg, drug abuse, poor health, mental health problems).6,12-20 These same studies indicate that predisposing factors (eg, age, race, and gender) and enabling factors (eg, insurance, use of other services, and usual place of care) are also associated with service use, though less consistently.
Studies focused on veterans experiencing homelessness, however, included only treatment-seeking populations, which are not necessarily representative of the broader population of veterans experiencing homelessness. Additionally, none of these prior studies focused on the unique subset of veterans residing in low-demand shelters (characterized by unlimited duration of stay, no government ID or fee required for entry, and no requirement for service participation). This is a population that seems to be less engaged in services but nevertheless is challenged.21 This study, therefore, is focused on nontreatment seeking veterans residing in a low-demand shelter. The study applied the Behavioral Model of Health Services Use and the Behavioral Model for Vulnerable Persons to examine use of VA and non-VA services.
Study Parameters
This study was conducted in Fort Worth, Texas, the 17th largest city in the U.S. with more than 810,000 residents.22 In 2013, a biennial point-in-time count identified about 2,300 individuals who were homeless in Fort Worth. Most were found in emergency shelters (n = 1,126, 50%) or transitional housing (n = 965, 40%). Slightly more than 10% (n = 281) were found to be unsheltered: sleeping on the streets or in encampments, automobiles, or abandoned buildings.23 Although national estimates identify 12% of all adults who are homeless as veterans,2 only 8% (n = 189) of people experiencing homelessness in Fort Worth reported military service.23
Access to the full array of VA emergency department (ED), inpatient, and outpatient medical, psychiatric, and substance-abuse services are available to veterans experiencing homelessness at the Dallas VA Medical Center (DVAMC), located 35 miles away. Only VA outpatient medical, psychiatric, and substance-related services are available in Fort Worth through the VA Outpatient Clinic and Health Care for the Homeless Veterans (HCHV) program. If veterans experiencing homelessness seek care outside of the VA system, a comprehensive network of emergency, inpatient and outpatient medical, psychiatric, and substance-related services is available in Fort Worth.
Sample
The study sample included 110 adult male veterans randomly recruited as they awaited admission to a private, low-demand emergency shelter. The study excluded veterans with a dishonorable discharge to ensure participants were eligible for VA services. Institutional review board approvals were obtained prior to the study from the University of Texas at Arlington and DVAMC. All participants provided informed consent and were given a $5 gift for their involvement.
Instruments
Through structured interviews, experienced research staff collected demographics, history of homelessness, military service, and substance abuse in the previous 30 days. Data on alcohol and drug problems in the past 12 months were obtained using the Short Michigan Alcohol Screening Test (SMAST) and the Drug Abuse Screening Test. The Veterans RAND 12-Item Health Survey (VR-12) was used to measure physical and mental health functioning in the previous 4 weeks. Finally, participants reported their use of VA or non-VA medical (ED, inpatient, and outpatient), psychiatric (ED, inpatient, and outpatient), and substance abuse-related (inpatient and outpatient) services in the 12 months prior to the interview. These measures have been shown to be valid and reliable with acceptable psychometrics.24-26
Data Analysis
Statistical analysis was completed using IBM SPSS Statistics version 19. Descriptive data were summarized using counts, percentages, means, and standard deviations. A dichotomous variable for alcohol abuse was defined as SMAST score ≥ 3. A variable representing participant’s VR-12 mental component summary scores was used as an indicator of mental health functioning.
McNemar’s test was used to compare the use of VA and non-VA medical, psychiatric, and substance-related services using dichotomous variables for each overall sector as well as respective sector subcomponent services (emergency, inpatient, and outpatient for medical and psychiatric sectors and inpatient and outpatient for the substance-related sector). Statistical significance level was set at α = .05.
Logistic regression was used to predict psychiatric and substance abuse-related service use with separate dependent variables for VA, non-VA, and both VA and non-VA services. Need-based factors included in all models as independent variables were mental health functioning, alcohol abuse, and a dichotomous variable representing cocaine use in the previous 30 days. Independent variables for the other service sectors were included as enabling factors (eg, medical and substance-related problems predicting psychiatric service use), aligning all service use variables in the model to the same provider system (eg, VA service sector independent variables with VA service sector dependent variables).
Results
The sample mean age was 49.2 years (SD = 9.2), and fewer than half (n = 45, 41%) were white. Three-fourths (n = 82, 75%) had ever been married, and few participants (n = 5, 5%) were currently married. Total mean lifetime experience of homelessness was 3.9 years (SD = 4.3). One-third of the samples participants (n = 36, 33%) reported that their current episode of homelessness had lasted 1 year or longer. Most had an adult felony conviction (n = 78, 71%) and a history of incarceration as an adult (n = 104, 95%). All military branches were represented, with 49% serving in the Army, 23% in the Marine Corps, 17% in the Navy, 10% in the Air Force, and 1% in the Coast Guard.
Most of the sample’s veterans served during the Vietnam era (n = 43, 43%) or the post-Vietnam era (n = 49, 45%), but 12 (11%) served during the Persian Gulf era (including Operation Iraqi Freedom and Operation Enduring Freedom). Few received a nonservice connected VA pension (n = 21, 19%) or service-connected disability benefits (n = 20, 18%). The mean income earned in the previous 30 days was $466 (SD = $431). None of these predisposing factors were associated with any service variables.
The sample’s mean VR-12 physical functioning score was 43.8 (SD = 9.1), which was significantly higher (t = 6.2, df = 109, P < .001) than the 38.4 (SD = 12.2) population norm used with the instrument. The sample’s mean mental health functioning score of 39.4 (SD = 14.3) was significantly lower (t = -8.6, df = 109, P < .001) than the population norm (51.1, SD = 11.4).27 Substance-related problems were prevalent, with an identified alcohol problem in 62% (n = 68) and a drug problem in 79% (n = 87) of participants. More than half reported illicit drug use in the past 30 days (n = 61, 56%), especially cocaine (n = 42, 38%) and marijuana (n = 37, 33%).
The majority of veterans (n = 96, 87%) reported using some type of service in the past 12 months (Table 1). Most survey respondents used medical services. About half used psychiatric services, and almost one-third used substance-related services. More veterans used non-VA ED services than used VA ED services. More veterans used VA outpatient medical services than used non-VA outpatient medical services. Examining service sectors indicated that more veterans used VA psychiatric services than used non-VA psychiatric services, especially VA outpatient psychiatric services. More veterans used non-VA substance abuse-related services, especially outpatient services, rather than similar services offered by the VA.
Separate logistic regression models predicted use of psychiatric and substance-abuse services with 3 models (VA, non-VA, or any service use) for each dependent variable from independent variables that reflected need and enabling factors (Tables 2 and 3). Demographic predisposing factors, which were not associated with service use, were not included as covariates in these models. For the model predicting the use of non-VA substance-abuse services, collinearity between the alcohol-abuse and cocaine-abuse variables required separate models for each of the 2 variables.
Medical sector service use predicted psychiatric sector service use in all models. In fact, VA medical service use was the only predictor of use of VA psychiatric services. Lower mental health functioning predicted the use of any (VA or non-VA) psychiatric service use. In addition to the use of medical services, 30-day cocaine use predicted non-VA psychiatric service use.
Any substance-related sector service use was predicted by lower mental health functioning, self-reported alcohol problem, and any medical services utilization. No independent variables included in the model predicted any VA substance-related service use. Non-VA substance abuse service use was predicted by non-VA psychiatric service use and alcohol abuse. In the separate analysis that replaced alcohol problems with 30-day cocaine use variable, only 30-day cocaine use predicted non-VA substance-related service utilization.
Discussion
This study examined the use of medical, psychiatric, and substance-abuse services by randomly sampled veterans from a low-demand emergency shelter. Random selection of the sample and its high (98%) participation rate virtually eliminated potential for bias within this sample. Another strength of this study is its focus on low-demand shelter users—a population that has not been well studied. This low-demand shelter-dwelling population of veterans experiencing homelessness is of interest because more substance-abuse problems and histories of incarceration seem to make them especially disadvantaged and challenged.
The limitation of the sample to users of a low-demand shelter at only 1 location may reduce generalizability to other veteran homeless populations and settings. The study also may not generalize to populations of female veterans experiencing homelessness. Another limitation of the study is that it did not use diagnostic assessments for psychiatric and substance use disorders and objective collateral information such as agency record data. Finally, although the limited size of the sample may have been insufficient to adequately test certain hypotheses, it was a relatively large sample of this population and was large enough to yield significant findings.
This study found that need-based factors predicted the use of some service sectors intended for those needs. For example, mental health functioning appropriately predicted any psychiatric service use, and presence of an alcohol problem appropriately predicted any substance abuse service use. Specifically for non-VA services, both cocaine use and presence of an alcohol problem in separate models predicted substance-abuse service use. However for VA substance-abuse services, neither cocaine use nor presence of an alcohol problem predicted service use. Despite the high need, very few veterans used substance-abuse services, and they rarely used VA substance-abuse services.
For 2 service sectors, need-based factors predicted the use of services intended for other needs. Cocaine use predicted non-VA psychiatric service use, and low mental health functioning predicted substance-abuse service use. One potential explanation for this finding could be that providers or patients incorrectly classified cocaine-related substance use problems as psychiatric. The VR-12 mental health functioning measure also may have incorrectly classified cocaine-related problems as psychiatric.
Three enabling factors predicted service use by sector and type. The first 2 are preference for VA-provided services and the geographic availability of services, which competed for veterans’ selection of service providers. When both VA and non-VA services were present in Fort Worth, a preference for VA-provided services was observed, with the exception of outpatient substance abuse services which were highly underutilized in general. No preference was observed for any non-VA services when both were present. When VA services were not present in Fort Worth, veterans used geographically available non-VA providers for some services, but for other services they used Dallas-based VA and Fort Worth-based non-VA providers equally (Table 3 and Table 4).
The third enabling factor influencing service use was through other service use as an enabling pathway. Those veterans who opted out of locally available services in favor of VA services in Dallas may have been prompted to do so by provider referrals, which were further facilitated by VA and public transportation between Fort Worth and Dallas. The most consistent enabling pathway was medical service use, which predicted all types of psychiatric service use (VA and non-VA combined, VA only, and non-VA only), and any substance-related service use. Psychiatric service use predicted substance abuse service use but only in non-VA settings; no pathways led from VA medical or psychiatric services to VA substance abuse services.
Conclusions
These findings suggest, in large part, the validity of the Andersen and Gelberg models of health care service use. Consistent with prior studies, need-based factors predicted the use of any psychiatric and substance-related sector services as well as the use of non-VA subcomponent services for both sectors. Also consistent with prior studies, enabling factors (medical sector service use) predicted service use, with the exception of VA or non-VA substance-abuse services. Unlike prior studies, however, predisposing factors (eg, age, race, marital status, and income) were not associated with service use.
This study could not determine why veterans underutilized substance-abuse services, even those available locally to them in Fort Worth. One possible barrier to care is that the services are designed or delivered in a manner that does not engage these veterans (eg, expectations regarding abstinence or service involvement). Another barrier could be that referral pathways between VA outpatient medical and psychiatric service providers and VA substance-related services are not sufficiently facilitative. Future investigations could build upon the findings of this study by collecting data that could help assess these potential barriers.
The data from this study suggest 3 opportunities to improve the utilization of services most needed by this population. The first opportunity would be to accurately differentiate between substance abuse and psychiatric problems in clinical assessment and identify the most appropriate type of care. Another opportunity, linked closely to the first, would be to facilitate more effective and efficient referral pathways among VA service sectors, especially from medical and psychiatric services to substance-abuse services. Another strategy to improve referral pathways would be for VA service networks to systematically examine local service systems for factors or processes that may disrupt integrated care and implement program improvements.28 For homeless veterans navigating an inherently complex VA health care system, peer-to-peer and patient navigator programs have helped improve service efficiency and service outcomes.29 The third opportunity to improve utilization of services would be to ensure geographic availability and accessibility by strategic placement of these services.
The results from this study, while informative, point directly to needed areas for further inquiry to inform public health response. Although the low-demand shelter users are a particularly challenging subgroup of veterans experiencing chronic homelessness, other equally challenging populations warrant additional study. For example, veterans outside of both VA and community services (eg, unsheltered populations) are likely to require different approaches to engage in appropriate services. Additionally, changes to the homeless policy implemented in the period after this sample was recruited suggest the need to revisit the service-using behaviors of this population. Finally, interventions developed as part of the national response need to be assessed for their ability to engage these difficult-to-reach veterans.
Acknowledgements
This study was funded by a U.S. Department of Veterans Affairs Office of Academic Affiliations Pre-Doctoral Social Work Research Fellowship award.
In 2009, the VA announced a goal of ending veteran homelessness by 2015.1 The primary focus of this new policy has been housing veterans experiencing chronic homelessness, many of whom languish outside the VA housing system. Since that time, progress has been made with point-in-time enumerations indicating that veteran homelessness has decreased nationally. Despite this progress, however, more than 55,000 veterans are still estimated to experience homelessness each night.2
Historically, the VA has offered an array of services specifically meant to alleviate veteran homelessness (grant, per diem, and other transitional housing programs; vocational rehabilitation, etc).3 The majority of these programs require some period of veteran abstinence as a condition for providing housing services. The recent move toward permanent “housing first” programs with few conditions for enrollment and participation provides new opportunities for housing veterans experiencing chronic homelessness, who are the specific target of the goal of ending veteran homelessness.4
Because veterans experiencing chronic homelessness have additional, substantial need for medical, psychiatric, and substance-abuse services, the VA also offers these services to this population.5-7 Veterans experiencing homelessness also may access parallel non-VA services.8 Information about veterans outside of traditional VA housing services, specifically those housed in low-demand shelters, is needed to develop services for this population and will be critical to success in ending veteran homelessness.
The Behavioral Model of Health Services Use9-11 and its later refinement, the Behavioral Model for Vulnerable Persons,12 have been used to conceptualize health care service use (Figure). In these models, health service use is predicted by 3 types of factors: predisposing factors (eg, age, race, gender, residential history), enabling factors (eg, availability, accessibility, affordability, acceptability), and service need factors (eg, substance-use disorders, mental health problems, physical health problems).
Studies applying these models of health care service use to both general homeless populations and, specifically to populations of veterans experiencing homelessness have found that service use is most influenced by need-based factors (eg, drug abuse, poor health, mental health problems).6,12-20 These same studies indicate that predisposing factors (eg, age, race, and gender) and enabling factors (eg, insurance, use of other services, and usual place of care) are also associated with service use, though less consistently.
Studies focused on veterans experiencing homelessness, however, included only treatment-seeking populations, which are not necessarily representative of the broader population of veterans experiencing homelessness. Additionally, none of these prior studies focused on the unique subset of veterans residing in low-demand shelters (characterized by unlimited duration of stay, no government ID or fee required for entry, and no requirement for service participation). This is a population that seems to be less engaged in services but nevertheless is challenged.21 This study, therefore, is focused on nontreatment seeking veterans residing in a low-demand shelter. The study applied the Behavioral Model of Health Services Use and the Behavioral Model for Vulnerable Persons to examine use of VA and non-VA services.
Study Parameters
This study was conducted in Fort Worth, Texas, the 17th largest city in the U.S. with more than 810,000 residents.22 In 2013, a biennial point-in-time count identified about 2,300 individuals who were homeless in Fort Worth. Most were found in emergency shelters (n = 1,126, 50%) or transitional housing (n = 965, 40%). Slightly more than 10% (n = 281) were found to be unsheltered: sleeping on the streets or in encampments, automobiles, or abandoned buildings.23 Although national estimates identify 12% of all adults who are homeless as veterans,2 only 8% (n = 189) of people experiencing homelessness in Fort Worth reported military service.23
Access to the full array of VA emergency department (ED), inpatient, and outpatient medical, psychiatric, and substance-abuse services are available to veterans experiencing homelessness at the Dallas VA Medical Center (DVAMC), located 35 miles away. Only VA outpatient medical, psychiatric, and substance-related services are available in Fort Worth through the VA Outpatient Clinic and Health Care for the Homeless Veterans (HCHV) program. If veterans experiencing homelessness seek care outside of the VA system, a comprehensive network of emergency, inpatient and outpatient medical, psychiatric, and substance-related services is available in Fort Worth.
Sample
The study sample included 110 adult male veterans randomly recruited as they awaited admission to a private, low-demand emergency shelter. The study excluded veterans with a dishonorable discharge to ensure participants were eligible for VA services. Institutional review board approvals were obtained prior to the study from the University of Texas at Arlington and DVAMC. All participants provided informed consent and were given a $5 gift for their involvement.
Instruments
Through structured interviews, experienced research staff collected demographics, history of homelessness, military service, and substance abuse in the previous 30 days. Data on alcohol and drug problems in the past 12 months were obtained using the Short Michigan Alcohol Screening Test (SMAST) and the Drug Abuse Screening Test. The Veterans RAND 12-Item Health Survey (VR-12) was used to measure physical and mental health functioning in the previous 4 weeks. Finally, participants reported their use of VA or non-VA medical (ED, inpatient, and outpatient), psychiatric (ED, inpatient, and outpatient), and substance abuse-related (inpatient and outpatient) services in the 12 months prior to the interview. These measures have been shown to be valid and reliable with acceptable psychometrics.24-26
Data Analysis
Statistical analysis was completed using IBM SPSS Statistics version 19. Descriptive data were summarized using counts, percentages, means, and standard deviations. A dichotomous variable for alcohol abuse was defined as SMAST score ≥ 3. A variable representing participant’s VR-12 mental component summary scores was used as an indicator of mental health functioning.
McNemar’s test was used to compare the use of VA and non-VA medical, psychiatric, and substance-related services using dichotomous variables for each overall sector as well as respective sector subcomponent services (emergency, inpatient, and outpatient for medical and psychiatric sectors and inpatient and outpatient for the substance-related sector). Statistical significance level was set at α = .05.
Logistic regression was used to predict psychiatric and substance abuse-related service use with separate dependent variables for VA, non-VA, and both VA and non-VA services. Need-based factors included in all models as independent variables were mental health functioning, alcohol abuse, and a dichotomous variable representing cocaine use in the previous 30 days. Independent variables for the other service sectors were included as enabling factors (eg, medical and substance-related problems predicting psychiatric service use), aligning all service use variables in the model to the same provider system (eg, VA service sector independent variables with VA service sector dependent variables).
Results
The sample mean age was 49.2 years (SD = 9.2), and fewer than half (n = 45, 41%) were white. Three-fourths (n = 82, 75%) had ever been married, and few participants (n = 5, 5%) were currently married. Total mean lifetime experience of homelessness was 3.9 years (SD = 4.3). One-third of the samples participants (n = 36, 33%) reported that their current episode of homelessness had lasted 1 year or longer. Most had an adult felony conviction (n = 78, 71%) and a history of incarceration as an adult (n = 104, 95%). All military branches were represented, with 49% serving in the Army, 23% in the Marine Corps, 17% in the Navy, 10% in the Air Force, and 1% in the Coast Guard.
Most of the sample’s veterans served during the Vietnam era (n = 43, 43%) or the post-Vietnam era (n = 49, 45%), but 12 (11%) served during the Persian Gulf era (including Operation Iraqi Freedom and Operation Enduring Freedom). Few received a nonservice connected VA pension (n = 21, 19%) or service-connected disability benefits (n = 20, 18%). The mean income earned in the previous 30 days was $466 (SD = $431). None of these predisposing factors were associated with any service variables.
The sample’s mean VR-12 physical functioning score was 43.8 (SD = 9.1), which was significantly higher (t = 6.2, df = 109, P < .001) than the 38.4 (SD = 12.2) population norm used with the instrument. The sample’s mean mental health functioning score of 39.4 (SD = 14.3) was significantly lower (t = -8.6, df = 109, P < .001) than the population norm (51.1, SD = 11.4).27 Substance-related problems were prevalent, with an identified alcohol problem in 62% (n = 68) and a drug problem in 79% (n = 87) of participants. More than half reported illicit drug use in the past 30 days (n = 61, 56%), especially cocaine (n = 42, 38%) and marijuana (n = 37, 33%).
The majority of veterans (n = 96, 87%) reported using some type of service in the past 12 months (Table 1). Most survey respondents used medical services. About half used psychiatric services, and almost one-third used substance-related services. More veterans used non-VA ED services than used VA ED services. More veterans used VA outpatient medical services than used non-VA outpatient medical services. Examining service sectors indicated that more veterans used VA psychiatric services than used non-VA psychiatric services, especially VA outpatient psychiatric services. More veterans used non-VA substance abuse-related services, especially outpatient services, rather than similar services offered by the VA.
Separate logistic regression models predicted use of psychiatric and substance-abuse services with 3 models (VA, non-VA, or any service use) for each dependent variable from independent variables that reflected need and enabling factors (Tables 2 and 3). Demographic predisposing factors, which were not associated with service use, were not included as covariates in these models. For the model predicting the use of non-VA substance-abuse services, collinearity between the alcohol-abuse and cocaine-abuse variables required separate models for each of the 2 variables.
Medical sector service use predicted psychiatric sector service use in all models. In fact, VA medical service use was the only predictor of use of VA psychiatric services. Lower mental health functioning predicted the use of any (VA or non-VA) psychiatric service use. In addition to the use of medical services, 30-day cocaine use predicted non-VA psychiatric service use.
Any substance-related sector service use was predicted by lower mental health functioning, self-reported alcohol problem, and any medical services utilization. No independent variables included in the model predicted any VA substance-related service use. Non-VA substance abuse service use was predicted by non-VA psychiatric service use and alcohol abuse. In the separate analysis that replaced alcohol problems with 30-day cocaine use variable, only 30-day cocaine use predicted non-VA substance-related service utilization.
Discussion
This study examined the use of medical, psychiatric, and substance-abuse services by randomly sampled veterans from a low-demand emergency shelter. Random selection of the sample and its high (98%) participation rate virtually eliminated potential for bias within this sample. Another strength of this study is its focus on low-demand shelter users—a population that has not been well studied. This low-demand shelter-dwelling population of veterans experiencing homelessness is of interest because more substance-abuse problems and histories of incarceration seem to make them especially disadvantaged and challenged.
The limitation of the sample to users of a low-demand shelter at only 1 location may reduce generalizability to other veteran homeless populations and settings. The study also may not generalize to populations of female veterans experiencing homelessness. Another limitation of the study is that it did not use diagnostic assessments for psychiatric and substance use disorders and objective collateral information such as agency record data. Finally, although the limited size of the sample may have been insufficient to adequately test certain hypotheses, it was a relatively large sample of this population and was large enough to yield significant findings.
This study found that need-based factors predicted the use of some service sectors intended for those needs. For example, mental health functioning appropriately predicted any psychiatric service use, and presence of an alcohol problem appropriately predicted any substance abuse service use. Specifically for non-VA services, both cocaine use and presence of an alcohol problem in separate models predicted substance-abuse service use. However for VA substance-abuse services, neither cocaine use nor presence of an alcohol problem predicted service use. Despite the high need, very few veterans used substance-abuse services, and they rarely used VA substance-abuse services.
For 2 service sectors, need-based factors predicted the use of services intended for other needs. Cocaine use predicted non-VA psychiatric service use, and low mental health functioning predicted substance-abuse service use. One potential explanation for this finding could be that providers or patients incorrectly classified cocaine-related substance use problems as psychiatric. The VR-12 mental health functioning measure also may have incorrectly classified cocaine-related problems as psychiatric.
Three enabling factors predicted service use by sector and type. The first 2 are preference for VA-provided services and the geographic availability of services, which competed for veterans’ selection of service providers. When both VA and non-VA services were present in Fort Worth, a preference for VA-provided services was observed, with the exception of outpatient substance abuse services which were highly underutilized in general. No preference was observed for any non-VA services when both were present. When VA services were not present in Fort Worth, veterans used geographically available non-VA providers for some services, but for other services they used Dallas-based VA and Fort Worth-based non-VA providers equally (Table 3 and Table 4).
The third enabling factor influencing service use was through other service use as an enabling pathway. Those veterans who opted out of locally available services in favor of VA services in Dallas may have been prompted to do so by provider referrals, which were further facilitated by VA and public transportation between Fort Worth and Dallas. The most consistent enabling pathway was medical service use, which predicted all types of psychiatric service use (VA and non-VA combined, VA only, and non-VA only), and any substance-related service use. Psychiatric service use predicted substance abuse service use but only in non-VA settings; no pathways led from VA medical or psychiatric services to VA substance abuse services.
Conclusions
These findings suggest, in large part, the validity of the Andersen and Gelberg models of health care service use. Consistent with prior studies, need-based factors predicted the use of any psychiatric and substance-related sector services as well as the use of non-VA subcomponent services for both sectors. Also consistent with prior studies, enabling factors (medical sector service use) predicted service use, with the exception of VA or non-VA substance-abuse services. Unlike prior studies, however, predisposing factors (eg, age, race, marital status, and income) were not associated with service use.
This study could not determine why veterans underutilized substance-abuse services, even those available locally to them in Fort Worth. One possible barrier to care is that the services are designed or delivered in a manner that does not engage these veterans (eg, expectations regarding abstinence or service involvement). Another barrier could be that referral pathways between VA outpatient medical and psychiatric service providers and VA substance-related services are not sufficiently facilitative. Future investigations could build upon the findings of this study by collecting data that could help assess these potential barriers.
The data from this study suggest 3 opportunities to improve the utilization of services most needed by this population. The first opportunity would be to accurately differentiate between substance abuse and psychiatric problems in clinical assessment and identify the most appropriate type of care. Another opportunity, linked closely to the first, would be to facilitate more effective and efficient referral pathways among VA service sectors, especially from medical and psychiatric services to substance-abuse services. Another strategy to improve referral pathways would be for VA service networks to systematically examine local service systems for factors or processes that may disrupt integrated care and implement program improvements.28 For homeless veterans navigating an inherently complex VA health care system, peer-to-peer and patient navigator programs have helped improve service efficiency and service outcomes.29 The third opportunity to improve utilization of services would be to ensure geographic availability and accessibility by strategic placement of these services.
The results from this study, while informative, point directly to needed areas for further inquiry to inform public health response. Although the low-demand shelter users are a particularly challenging subgroup of veterans experiencing chronic homelessness, other equally challenging populations warrant additional study. For example, veterans outside of both VA and community services (eg, unsheltered populations) are likely to require different approaches to engage in appropriate services. Additionally, changes to the homeless policy implemented in the period after this sample was recruited suggest the need to revisit the service-using behaviors of this population. Finally, interventions developed as part of the national response need to be assessed for their ability to engage these difficult-to-reach veterans.
Acknowledgements
This study was funded by a U.S. Department of Veterans Affairs Office of Academic Affiliations Pre-Doctoral Social Work Research Fellowship award.
1. U.S. Department of Veterans Affairs. Homeless veterans: VA is working to end homelessness among veterans. U.S. Department of Veterans Affairs Website. www.va.gov/homeless/about_the_initiative.asp#one. Updated January 26, 2016. Accessed February 16, 2016.
2. Henry M, Cortes A, Morris S, Abt Associates; U. S. Department of Housing and Urban Development Office of Community Planning and Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1 Point-in-Time Estimates of Homelessness. HUD Exchange Website. https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Published October 2014. Accessed February 16, 2016.
3. U.S. Department of Veterans Affairs. Homeless Veterans: Housing Assistance. U.S. Department of Veterans Affairs Web site. http://www.va.gov/homeless/housing.asp. Updated November 5, 2015. Accessed February 16, 2016.
4. Austin EL, Pollio DE, Holmes S, et al. VA's expansion of supportive housing: successes and challenges on the path to Housing First. Psychiatr Serv. 2014;65(5):641-647.
5. Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455-460.
6. Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33(11):1132-1144.
7. McQuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental health illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
8. Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27-31.
9. Andersen RM. A behavioral model of families use of health services: Research Series No. 25. Chicago, IL: University of Chicago Center for Health Administrative Studies; 1968.
10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
11. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
12. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302.
13. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
14. Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212-230.
15. Gamache G, Rosenheck RA, Tessler R. Factors predicting choice of provider among homeless veterans with mental illness. Psychiatr Serv. 2000;51(8):1024-1028.
16. Wenzel SL, Audrey Burnam, M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158-1169.
17. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
18. Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381-393.
19. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Anderson Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20-30.
20. Linton KF, Shafer MS. Factors associated with the health service use of unsheltered, chronically homeless adults. Soc Work Public Health. 2013;29(1):73-80.
21. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psych Serv. 2014;65(6):751-757.
22. U.S. Census Bureau. State & County Quick Facts: Fort Worth (city), Texas. U.S. Census Bureau Website. http://quickfacts.census.gov/qfd/states/48/4827000.html. Revised December 2, 2015. Accessed February 17, 2016.
23. Tarrant County Homeless Coalition. 2014 point in time count results. Tarrant County Homeless Coalition Website. http://www.ahomewithhope.org/staff/local-data-research/2014-homeless-count/. Accessed February 16, 2016.
24. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses. Int J Method Psychiatr Res. 2004;13(3):184-191.
25. Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): What it is and how it is Used. Washington, DC: Veterans Health Administration; 2009.
26. Fischer J, Corcoran K, eds. Measures for Clinical Practice and Research: A Sourcebook. 4th ed. New York, NY: Oxford University Press; 2013.
27. Selim AJ, Rogers W, Fleishman JA, Qian SX, Finke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18(1):43-52.
28. Blue-Howells J, McQuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219-231.
29. Piette JD, Holtz B, Beard AJ, et al; Ann Arbor PACT Steering Committee. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1(4):615-623.
1. U.S. Department of Veterans Affairs. Homeless veterans: VA is working to end homelessness among veterans. U.S. Department of Veterans Affairs Website. www.va.gov/homeless/about_the_initiative.asp#one. Updated January 26, 2016. Accessed February 16, 2016.
2. Henry M, Cortes A, Morris S, Abt Associates; U. S. Department of Housing and Urban Development Office of Community Planning and Development. The 2013 Annual Homeless Assessment Report (AHAR) to Congress: Part 1 Point-in-Time Estimates of Homelessness. HUD Exchange Website. https://www.hudexchange.info/resources/documents/ahar-2013-part1.pdf. Published October 2014. Accessed February 16, 2016.
3. U.S. Department of Veterans Affairs. Homeless Veterans: Housing Assistance. U.S. Department of Veterans Affairs Web site. http://www.va.gov/homeless/housing.asp. Updated November 5, 2015. Accessed February 16, 2016.
4. Austin EL, Pollio DE, Holmes S, et al. VA's expansion of supportive housing: successes and challenges on the path to Housing First. Psychiatr Serv. 2014;65(5):641-647.
5. Tsai J, Kasprow WJ, Rosenheck RA. Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addict Behav. 2014;39(2):455-460.
6. Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33(11):1132-1144.
7. McQuire J, Gelberg L, Blue-Howells J, Rosenheck RA. Access to primary care for homeless veterans with serious mental health illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Adm Policy Ment Health. 2009;36(4):255-264.
8. Tsai J, Mares AS, Rosenheck RA. Do homeless veterans have the same needs and outcomes as non-veterans? Mil Med. 2012;177(1):27-31.
9. Andersen RM. A behavioral model of families use of health services: Research Series No. 25. Chicago, IL: University of Chicago Center for Health Administrative Studies; 1968.
10. Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36(1):1-10.
11. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
12. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273-1302.
13. Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805-821.
14. Stein JA, Andersen RM, Koegel P, Gelberg L. Predicting health services utilization among homeless adults: a prospective analysis. J Health Care Poor Underserved. 2000;11(2):212-230.
15. Gamache G, Rosenheck RA, Tessler R. Factors predicting choice of provider among homeless veterans with mental illness. Psychiatr Serv. 2000;51(8):1024-1028.
16. Wenzel SL, Audrey Burnam, M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39(11):1158-1169.
17. Pollio DE, North CS, Eyrich KM, Foster DA, Spitznagel E. Modeling service access in a homeless population. J Psychoactive Drugs. 2003;35(4):487-495.
18. Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381-393.
19. Stein JA, Andersen RM, Robertson M, Gelberg L. Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Anderson Behavioral Model for Vulnerable Populations. Health Psychol. 2012;31(1):20-30.
20. Linton KF, Shafer MS. Factors associated with the health service use of unsheltered, chronically homeless adults. Soc Work Public Health. 2013;29(1):73-80.
21. Petrovich JC, Pollio DE, North CS. Characteristics and service use of homeless veterans and nonveterans residing in a low-demand emergency shelter. Psych Serv. 2014;65(6):751-757.
22. U.S. Census Bureau. State & County Quick Facts: Fort Worth (city), Texas. U.S. Census Bureau Website. http://quickfacts.census.gov/qfd/states/48/4827000.html. Revised December 2, 2015. Accessed February 17, 2016.
23. Tarrant County Homeless Coalition. 2014 point in time count results. Tarrant County Homeless Coalition Website. http://www.ahomewithhope.org/staff/local-data-research/2014-homeless-count/. Accessed February 16, 2016.
24. North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL. The Homeless Supplement to the Diagnostic Interview Schedule: test-retest analyses. Int J Method Psychiatr Res. 2004;13(3):184-191.
25. Iqbal SU, Rogers W, Selim A, et al. The Veterans RAND 12 Item Health Survey (VR-12): What it is and how it is Used. Washington, DC: Veterans Health Administration; 2009.
26. Fischer J, Corcoran K, eds. Measures for Clinical Practice and Research: A Sourcebook. 4th ed. New York, NY: Oxford University Press; 2013.
27. Selim AJ, Rogers W, Fleishman JA, Qian SX, Finke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18(1):43-52.
28. Blue-Howells J, McQuire J, Nakashima J. Co-location of health care services for homeless veterans: a case study of innovation in program implementation. Soc Work Health Care. 2008;47(3):219-231.
29. Piette JD, Holtz B, Beard AJ, et al; Ann Arbor PACT Steering Committee. Improving chronic illness care for veterans within the framework of the Patient-Centered Medical Home: experiences from the Ann Arbor Patient-Aligned Care Team Laboratory. Transl Behav Med. 2011;1(4):615-623.