User login
A 66-year-old white woman presented to her primary care clinic with concerns about hair loss, which began 2 years ago. Recently, she had noticed some “bumps” on her cheeks, as well.
On physical examination, the physician noted hair loss in a symmetric 2-cm band-like distribution across her frontal and temporal scalp (FIGURES 1 and 2). In both areas, there was moderate perifollicular erythema, scale, and what appeared to be scarring.
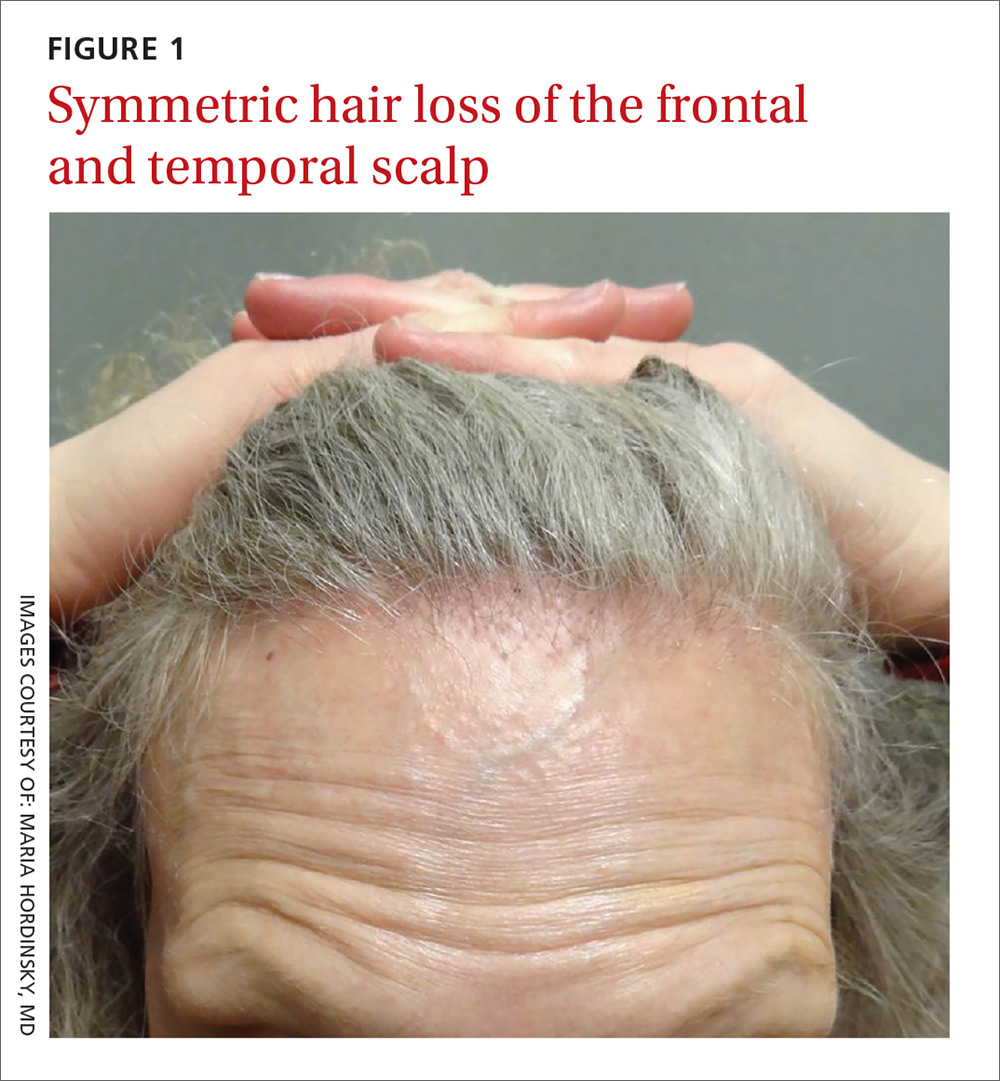
The patient had lost most of her eyebrow hairs, and had prominent temporal veins (FIGURE 2) and flesh-colored papules on her cheeks. She had no significant medical history, was emotionally stable, and recently had a satisfactory health care maintenance exam. The postmenopausal patient’s last menses was 15 years earlier, and she was not taking hormone replacement.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Frontal fibrosing alopecia
The patient was referred to our dermatology clinic, which specializes in hair loss. Based on the clinical findings, we suspected that this was a case of frontal fibrosing alopecia (FFA), a primary lymphocytic cicatricial (scarring) alopecia. A dermatopathologist confirmed the diagnosis via histologic review.
A condition on the rise. The incidence of FFA has been steadily increasing internationally since the condition was first described in 1994.1 Among patients referred to a specialty clinic for hair loss, diagnosis of FFA has increased from 1.6% in 2000 to 17% in 2011.2
FFA is characterized by symmetric band-like hair loss with evidence of scarring in the frontal and temporal regions of the scalp. (The extent of hair loss can be assessed by retracting the patient’s hair and having the patient raise his or her eyebrows and wrinkle the forehead in a surprised look.) FFA is accompanied by eyebrow loss in 73% to 95% of patients.2,3 Mild to severe perifollicular (and possibly more generalized) erythema and scale are usually present. In addition, erythematous or skin-colored papules may appear on the face,3 and marked exaggeration of the temporal veins is a common finding.
Most patients with FFA (83%) are postmenopausal women and nearly all (98.6%) have Fitzpatrick skin type 1 or 2 (white skin that burns easily and doesn’t readily tan).4 Other pertinent findings include the absence of oral lesions, nail changes, or other skin diseases.
A subtype of another condition? Because they are similar histologically, some consider FFA to be a subtype of lichen planopilaris. (See “Scarring alopecia in a woman with psoriasis,” J Fam Pract. 2015;64:E1-E3.)
A punch biopsy to confirm the diagnosis of FFA should be taken from the leading edge of the hair loss and, ideally, reviewed by a dermatopathologist. Histologic examination will reveal a lichenoid lymphocytic infiltrate (predominantly around the hair follicle where the follicular stem cells reside), resulting in fibrosis and scarring.5
Rule out other causes of hair loss
In addition to confirming the diagnosis with histologic examination, you’ll also need to have ruled out the following conditions in the differential.
Alopecia areata may mimic the ophiasis (band-like) pattern of hair loss seen with FFA, but it is a non-scarring disorder that typically lacks any signs of inflammation.
Female pattern hair loss is characterized by a decrease in hair density and thinning. The condition is non-scarring and usually involves the frontal and vertex (crown) regions of the scalp.
Discoid lupus erythematosus is characterized by circular scarring hair loss with a central patch of inflammation, as well as depigmentation.
Central centrifugal cicatricial alopecia predominantly affects black women and is characterized by circular hair loss of the vertex, with perifollicular inflammation and scarring.
Traction alopecia can occur in the same location as FFA, but is not usually associated with perifollicular inflammation. This condition can cause scarring if traction has been longstanding and persistent. There is usually a history of certain hairstyles (such as braiding) associated with chronic tension on hair fibers.
Numerous Tx strategies exist, but they are not well studied
Because there are no published randomized clinical trials on treatment for FFA, few evidence-based treatment strategies exist.6 In addition, the prognosis is variable. Experts have employed numerous treatment strategies, including topical and intralesional steroids, immunosuppressive medications, antibiotics, and anti-androgen therapy, with varying results.4,6 For most primary care physicians, it’s best to refer patients to a dermatologist to initiate treatment.
Intralesional steroids such as triamcinolone acetonide (5-10 mg/cc), as well as high-potency topical steroids, are generally helpful to stabilize the disease. There is also some evidence of benefit from oral dutasteride or finasteride at variable doses.6 Immunosuppressants such as hydroxychloroquine may also be used as second-line treatments, although the benefit-to-risk ratio needs to be taken into consideration.7
Early detection is key. In general, treatment should be initiated as soon as possible to prevent disease progression and reduce permanent scarring and hair loss. The Lichen Planopilaris Activity Index7 is a tool that clinicians can use to measure disease severity and track changes in disease activity through patient report of symptoms and measurements of scalp inflammation.
Our patient was started on a regimen of topical high-potency steroids (clobetasol foam, 0.05%), with targeted, intralesional injection of steroids (10 mg/cc of triamcinolone acetonide) to areas with the most inflammation. The patient was advised to use ketoconazole 2% shampoo while showering.
These interventions decreased our patient’s symptoms dramatically. Her scalp erythema and scale improved, but the hair did not regrow. One year later, her hairline was clinically stable with no evidence of disease progression. She continues to see a dermatologist annually.
CORRESPONDENCE
David V. Power, MB, MPH, Department of Family Medicine and Community Health, University of Minnesota, 516 Delaware St. SE, Minneapolis, MN 55455; [email protected].
1. Kossard S. Postmenopausal frontal fibrosing alopecia: Scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774.
2. MacDonald A, Clark C, Holmes S. Frontal fibrosing alopecia: a review of 60 cases. J Am Acad Dermatol. 2012;67:955-961.
3. Ladizinski B, Bazakas A, Selim MA, et al. Frontal fibrosing alopecia: a retrospective review of 19 patients seen at Duke University. J Am Acad Dermatol. 2013;68:749-755.
4. Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, et al. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670-678.
5. Poblet E, Jiménez F, Pascual A, et al. Frontal fibrosing alopecia versus lichen planopilaris: a clinicopathological study. Int J Dermatol. 2006;45:375-380.
6. Rácz E, Gho C, Moorman PW, et al. Treatment of frontal fibrosing alopecia and lichen planopilaris: a systematic review. J Eur Acad Dermatol Venereol. 2013;27:1461-1470.
7. Chiang C, Sah D, Cho BK, et al. Hydroxychloroquine and lichen planopilaris: efficacy and introduction of Lichen Planopilaris Activity Index scoring system. J Am Acad Dermatol. 2010;62:387-392.
A 66-year-old white woman presented to her primary care clinic with concerns about hair loss, which began 2 years ago. Recently, she had noticed some “bumps” on her cheeks, as well.
On physical examination, the physician noted hair loss in a symmetric 2-cm band-like distribution across her frontal and temporal scalp (FIGURES 1 and 2). In both areas, there was moderate perifollicular erythema, scale, and what appeared to be scarring.
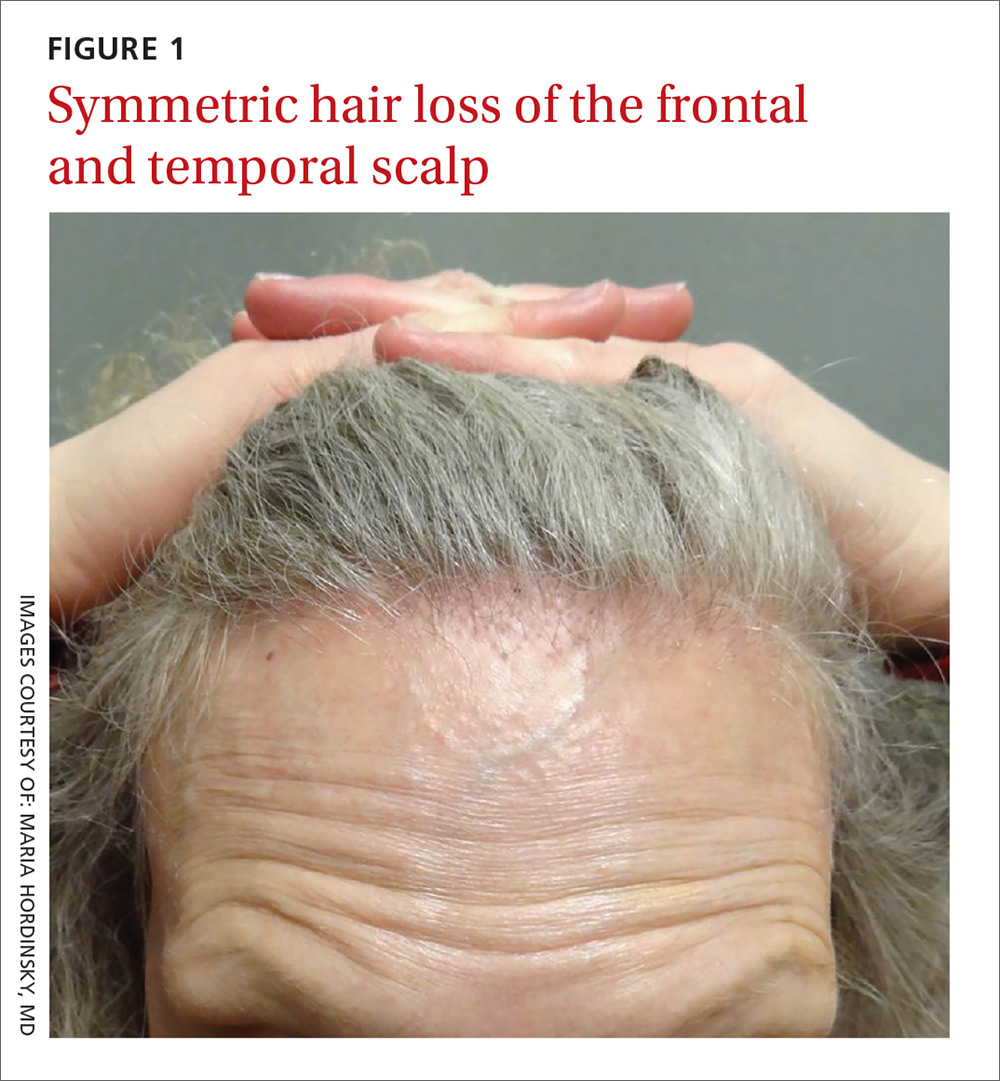
The patient had lost most of her eyebrow hairs, and had prominent temporal veins (FIGURE 2) and flesh-colored papules on her cheeks. She had no significant medical history, was emotionally stable, and recently had a satisfactory health care maintenance exam. The postmenopausal patient’s last menses was 15 years earlier, and she was not taking hormone replacement.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Frontal fibrosing alopecia
The patient was referred to our dermatology clinic, which specializes in hair loss. Based on the clinical findings, we suspected that this was a case of frontal fibrosing alopecia (FFA), a primary lymphocytic cicatricial (scarring) alopecia. A dermatopathologist confirmed the diagnosis via histologic review.
A condition on the rise. The incidence of FFA has been steadily increasing internationally since the condition was first described in 1994.1 Among patients referred to a specialty clinic for hair loss, diagnosis of FFA has increased from 1.6% in 2000 to 17% in 2011.2
FFA is characterized by symmetric band-like hair loss with evidence of scarring in the frontal and temporal regions of the scalp. (The extent of hair loss can be assessed by retracting the patient’s hair and having the patient raise his or her eyebrows and wrinkle the forehead in a surprised look.) FFA is accompanied by eyebrow loss in 73% to 95% of patients.2,3 Mild to severe perifollicular (and possibly more generalized) erythema and scale are usually present. In addition, erythematous or skin-colored papules may appear on the face,3 and marked exaggeration of the temporal veins is a common finding.
Most patients with FFA (83%) are postmenopausal women and nearly all (98.6%) have Fitzpatrick skin type 1 or 2 (white skin that burns easily and doesn’t readily tan).4 Other pertinent findings include the absence of oral lesions, nail changes, or other skin diseases.
A subtype of another condition? Because they are similar histologically, some consider FFA to be a subtype of lichen planopilaris. (See “Scarring alopecia in a woman with psoriasis,” J Fam Pract. 2015;64:E1-E3.)
A punch biopsy to confirm the diagnosis of FFA should be taken from the leading edge of the hair loss and, ideally, reviewed by a dermatopathologist. Histologic examination will reveal a lichenoid lymphocytic infiltrate (predominantly around the hair follicle where the follicular stem cells reside), resulting in fibrosis and scarring.5
Rule out other causes of hair loss
In addition to confirming the diagnosis with histologic examination, you’ll also need to have ruled out the following conditions in the differential.
Alopecia areata may mimic the ophiasis (band-like) pattern of hair loss seen with FFA, but it is a non-scarring disorder that typically lacks any signs of inflammation.
Female pattern hair loss is characterized by a decrease in hair density and thinning. The condition is non-scarring and usually involves the frontal and vertex (crown) regions of the scalp.
Discoid lupus erythematosus is characterized by circular scarring hair loss with a central patch of inflammation, as well as depigmentation.
Central centrifugal cicatricial alopecia predominantly affects black women and is characterized by circular hair loss of the vertex, with perifollicular inflammation and scarring.
Traction alopecia can occur in the same location as FFA, but is not usually associated with perifollicular inflammation. This condition can cause scarring if traction has been longstanding and persistent. There is usually a history of certain hairstyles (such as braiding) associated with chronic tension on hair fibers.
Numerous Tx strategies exist, but they are not well studied
Because there are no published randomized clinical trials on treatment for FFA, few evidence-based treatment strategies exist.6 In addition, the prognosis is variable. Experts have employed numerous treatment strategies, including topical and intralesional steroids, immunosuppressive medications, antibiotics, and anti-androgen therapy, with varying results.4,6 For most primary care physicians, it’s best to refer patients to a dermatologist to initiate treatment.
Intralesional steroids such as triamcinolone acetonide (5-10 mg/cc), as well as high-potency topical steroids, are generally helpful to stabilize the disease. There is also some evidence of benefit from oral dutasteride or finasteride at variable doses.6 Immunosuppressants such as hydroxychloroquine may also be used as second-line treatments, although the benefit-to-risk ratio needs to be taken into consideration.7
Early detection is key. In general, treatment should be initiated as soon as possible to prevent disease progression and reduce permanent scarring and hair loss. The Lichen Planopilaris Activity Index7 is a tool that clinicians can use to measure disease severity and track changes in disease activity through patient report of symptoms and measurements of scalp inflammation.
Our patient was started on a regimen of topical high-potency steroids (clobetasol foam, 0.05%), with targeted, intralesional injection of steroids (10 mg/cc of triamcinolone acetonide) to areas with the most inflammation. The patient was advised to use ketoconazole 2% shampoo while showering.
These interventions decreased our patient’s symptoms dramatically. Her scalp erythema and scale improved, but the hair did not regrow. One year later, her hairline was clinically stable with no evidence of disease progression. She continues to see a dermatologist annually.
CORRESPONDENCE
David V. Power, MB, MPH, Department of Family Medicine and Community Health, University of Minnesota, 516 Delaware St. SE, Minneapolis, MN 55455; [email protected].
A 66-year-old white woman presented to her primary care clinic with concerns about hair loss, which began 2 years ago. Recently, she had noticed some “bumps” on her cheeks, as well.
On physical examination, the physician noted hair loss in a symmetric 2-cm band-like distribution across her frontal and temporal scalp (FIGURES 1 and 2). In both areas, there was moderate perifollicular erythema, scale, and what appeared to be scarring.
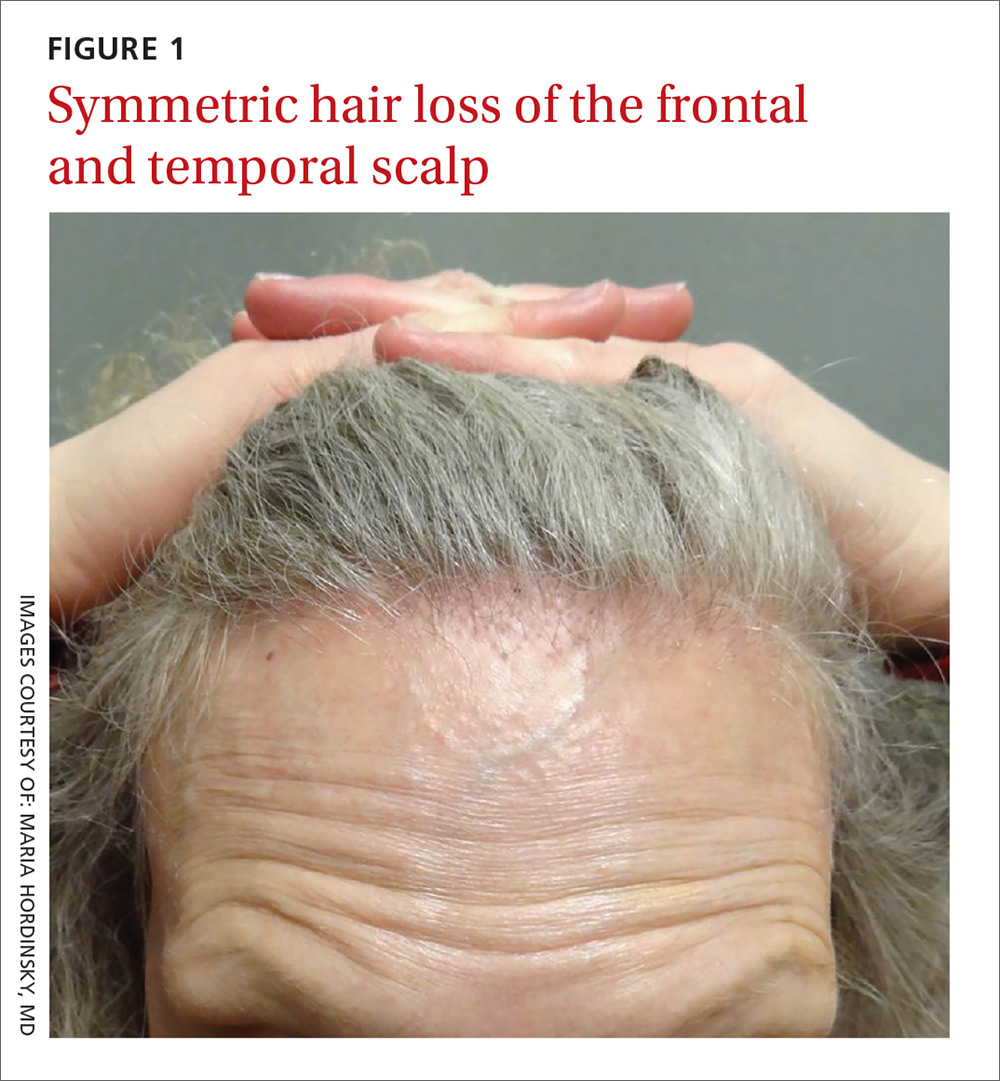
The patient had lost most of her eyebrow hairs, and had prominent temporal veins (FIGURE 2) and flesh-colored papules on her cheeks. She had no significant medical history, was emotionally stable, and recently had a satisfactory health care maintenance exam. The postmenopausal patient’s last menses was 15 years earlier, and she was not taking hormone replacement.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Frontal fibrosing alopecia
The patient was referred to our dermatology clinic, which specializes in hair loss. Based on the clinical findings, we suspected that this was a case of frontal fibrosing alopecia (FFA), a primary lymphocytic cicatricial (scarring) alopecia. A dermatopathologist confirmed the diagnosis via histologic review.
A condition on the rise. The incidence of FFA has been steadily increasing internationally since the condition was first described in 1994.1 Among patients referred to a specialty clinic for hair loss, diagnosis of FFA has increased from 1.6% in 2000 to 17% in 2011.2
FFA is characterized by symmetric band-like hair loss with evidence of scarring in the frontal and temporal regions of the scalp. (The extent of hair loss can be assessed by retracting the patient’s hair and having the patient raise his or her eyebrows and wrinkle the forehead in a surprised look.) FFA is accompanied by eyebrow loss in 73% to 95% of patients.2,3 Mild to severe perifollicular (and possibly more generalized) erythema and scale are usually present. In addition, erythematous or skin-colored papules may appear on the face,3 and marked exaggeration of the temporal veins is a common finding.
Most patients with FFA (83%) are postmenopausal women and nearly all (98.6%) have Fitzpatrick skin type 1 or 2 (white skin that burns easily and doesn’t readily tan).4 Other pertinent findings include the absence of oral lesions, nail changes, or other skin diseases.
A subtype of another condition? Because they are similar histologically, some consider FFA to be a subtype of lichen planopilaris. (See “Scarring alopecia in a woman with psoriasis,” J Fam Pract. 2015;64:E1-E3.)
A punch biopsy to confirm the diagnosis of FFA should be taken from the leading edge of the hair loss and, ideally, reviewed by a dermatopathologist. Histologic examination will reveal a lichenoid lymphocytic infiltrate (predominantly around the hair follicle where the follicular stem cells reside), resulting in fibrosis and scarring.5
Rule out other causes of hair loss
In addition to confirming the diagnosis with histologic examination, you’ll also need to have ruled out the following conditions in the differential.
Alopecia areata may mimic the ophiasis (band-like) pattern of hair loss seen with FFA, but it is a non-scarring disorder that typically lacks any signs of inflammation.
Female pattern hair loss is characterized by a decrease in hair density and thinning. The condition is non-scarring and usually involves the frontal and vertex (crown) regions of the scalp.
Discoid lupus erythematosus is characterized by circular scarring hair loss with a central patch of inflammation, as well as depigmentation.
Central centrifugal cicatricial alopecia predominantly affects black women and is characterized by circular hair loss of the vertex, with perifollicular inflammation and scarring.
Traction alopecia can occur in the same location as FFA, but is not usually associated with perifollicular inflammation. This condition can cause scarring if traction has been longstanding and persistent. There is usually a history of certain hairstyles (such as braiding) associated with chronic tension on hair fibers.
Numerous Tx strategies exist, but they are not well studied
Because there are no published randomized clinical trials on treatment for FFA, few evidence-based treatment strategies exist.6 In addition, the prognosis is variable. Experts have employed numerous treatment strategies, including topical and intralesional steroids, immunosuppressive medications, antibiotics, and anti-androgen therapy, with varying results.4,6 For most primary care physicians, it’s best to refer patients to a dermatologist to initiate treatment.
Intralesional steroids such as triamcinolone acetonide (5-10 mg/cc), as well as high-potency topical steroids, are generally helpful to stabilize the disease. There is also some evidence of benefit from oral dutasteride or finasteride at variable doses.6 Immunosuppressants such as hydroxychloroquine may also be used as second-line treatments, although the benefit-to-risk ratio needs to be taken into consideration.7
Early detection is key. In general, treatment should be initiated as soon as possible to prevent disease progression and reduce permanent scarring and hair loss. The Lichen Planopilaris Activity Index7 is a tool that clinicians can use to measure disease severity and track changes in disease activity through patient report of symptoms and measurements of scalp inflammation.
Our patient was started on a regimen of topical high-potency steroids (clobetasol foam, 0.05%), with targeted, intralesional injection of steroids (10 mg/cc of triamcinolone acetonide) to areas with the most inflammation. The patient was advised to use ketoconazole 2% shampoo while showering.
These interventions decreased our patient’s symptoms dramatically. Her scalp erythema and scale improved, but the hair did not regrow. One year later, her hairline was clinically stable with no evidence of disease progression. She continues to see a dermatologist annually.
CORRESPONDENCE
David V. Power, MB, MPH, Department of Family Medicine and Community Health, University of Minnesota, 516 Delaware St. SE, Minneapolis, MN 55455; [email protected].
1. Kossard S. Postmenopausal frontal fibrosing alopecia: Scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774.
2. MacDonald A, Clark C, Holmes S. Frontal fibrosing alopecia: a review of 60 cases. J Am Acad Dermatol. 2012;67:955-961.
3. Ladizinski B, Bazakas A, Selim MA, et al. Frontal fibrosing alopecia: a retrospective review of 19 patients seen at Duke University. J Am Acad Dermatol. 2013;68:749-755.
4. Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, et al. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670-678.
5. Poblet E, Jiménez F, Pascual A, et al. Frontal fibrosing alopecia versus lichen planopilaris: a clinicopathological study. Int J Dermatol. 2006;45:375-380.
6. Rácz E, Gho C, Moorman PW, et al. Treatment of frontal fibrosing alopecia and lichen planopilaris: a systematic review. J Eur Acad Dermatol Venereol. 2013;27:1461-1470.
7. Chiang C, Sah D, Cho BK, et al. Hydroxychloroquine and lichen planopilaris: efficacy and introduction of Lichen Planopilaris Activity Index scoring system. J Am Acad Dermatol. 2010;62:387-392.
1. Kossard S. Postmenopausal frontal fibrosing alopecia: Scarring alopecia in a pattern distribution. Arch Dermatol. 1994;130:770-774.
2. MacDonald A, Clark C, Holmes S. Frontal fibrosing alopecia: a review of 60 cases. J Am Acad Dermatol. 2012;67:955-961.
3. Ladizinski B, Bazakas A, Selim MA, et al. Frontal fibrosing alopecia: a retrospective review of 19 patients seen at Duke University. J Am Acad Dermatol. 2013;68:749-755.
4. Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, et al. Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol. 2014;70:670-678.
5. Poblet E, Jiménez F, Pascual A, et al. Frontal fibrosing alopecia versus lichen planopilaris: a clinicopathological study. Int J Dermatol. 2006;45:375-380.
6. Rácz E, Gho C, Moorman PW, et al. Treatment of frontal fibrosing alopecia and lichen planopilaris: a systematic review. J Eur Acad Dermatol Venereol. 2013;27:1461-1470.
7. Chiang C, Sah D, Cho BK, et al. Hydroxychloroquine and lichen planopilaris: efficacy and introduction of Lichen Planopilaris Activity Index scoring system. J Am Acad Dermatol. 2010;62:387-392.
