User login
Discussions about cardiopulmonary resuscitation (CPR) can be difficult due to their association with end of life. The Patient Self Determination Act (H.R.4449 — 101st Congress [1989-1990]) and institutional standards mandate collaboration between care providers and patients regarding goals of care in emergency situations such as cardiopulmonary arrest. The default option is to provide CPR, which may involve chest compressions, intubation, and/or defibrillation. Yet numerous studies show that a significant number of patients have no code preference documented in their medical chart, and even fewer report a conversation with their care provider about their wishes regarding CPR.1-3 CPR is an invasive and potentially painful procedure with a higher chance of failure than success4, and yet many patients report that their provider did not discuss with them the risks and benefits of resuscitation.5,6 Further highlighting the importance of individual discussions about CPR preferences is the reality that factors such as age and disease burden further skew the likelihood of survival after cardiopulmonary arrest.7
Complicating the lack of appropriate provider and patient discussion of the risks and benefits of resuscitation are significant misunderstandings about CPR in the lay population. Patients routinely overestimate the likelihood of survival following CPR.8,9 This may be partially due to the portrayal of CPR in the lay media as highly efficacious.10 Other factors known to prevent effective provider-and-patient discussions about CPR preferences are providers’ discomfort with the subject11 and perceived time constraints.12
Informational videos have been developed to assist patients with decision making about CPR and have been shown to impact patients’ choices in the setting of life-limiting diseases such as advanced cancer,13-14 serious illness with a prognosis of less than 1 year,15 and dementia.16 While discussion of code status is vitally important in end-of-life planning for seriously ill individuals, delayed discussion of CPR preferences is associated with a significant increase in the number of invasive procedures performed at the end of life, increased length of stay in the hospital, and increased medical cost.17 Despite clear evidence that earlier discussion of resuscitation options are valuable, no studies have examined the impact of a video about code status options in the general patient population.
Here we present our findings of a randomized trial in patients hospitalized on the general medicine wards who were 65 years of age or older, regardless of illness severity or diagnosis. The video tool was a supplement for, rather than a replacement of, standard provider and patient communication about code preferences, and we compared patients who watched the video against controls who had standard discussions with their providers. Our video detailed the process of chest compressions and intubation during CPR and explained the differences between the code statuses: full code, do not resuscitate (DNR), and do not resuscitate/do not intubate (DNR/DNI). We found a significant difference between the 2 groups, with significantly more individuals in the video group choosing DNR/DNI. These findings suggest that video support tools may be a useful supplement to traditional provider discussions about code preferences in the general patient population.
METHODS
We enrolled patients from the general medicine wards at the Minneapolis VA Hospital from September 28, 2015 to October 23, 2015. Eligibility criteria included age 65 years or older, ability to provide informed consent, and ability to communicate in English. Study recruitment and data collection were performed by a study coordinator who was a house staff physician and had no role in the care of the participants. The medical charts of all general medicine patients were reviewed to determine if they met the age criteria. The physician of record for potential participants was contacted to assess if the patient was able to provide informed consent and communicate in English. Eligible patients were approached and informed consent was obtained from those who chose to participate in the study. After obtaining informed consent, patients were randomized using a random number generator to the intervention or usual-care arm of the study.
Those who were assigned to the intervention arm watched a 6-minute long video explaining the code-preference choices of full code, DNR, or DNR/DNI. Full code was described as possibly including CPR, intubation, and/or defibrillation depending on the clinical situation. Do not resuscitate was described as meaning no CPR or defibrillation but possible intubation in the case of respiratory failure. Do not resuscitate/do not intubate was explained as meaning no CPR, no defibrillation, and no intubation but rather permitting “natural death” to occur. The video showed a mock code with chest compressions, defibrillation, and intubation on a mannequin as well as palliative care specialists who discussed potential complications and survival rates of inhospital resuscitation.
The video was created at the University of Minnesota with the departments of palliative care and internal medicine (www.mmcgmeservices.org/codestat.html). After viewing the video, participants in the intervention arm filled out a questionnaire designed to assess their knowledge and beliefs about CPR and trust in their medical care providers. They were asked to circle their code preference. The participants’ medical teams were made aware of the code preferences and were counseled to discuss code preferences further if it was different from their previously documented code preference.
Participants in the control arm were assigned to usual care. At the institution where this study occurred, a discussion about code preferences between the patient and their medical team is considered the standard of care. After informed consent was obtained, participants filled out the same questionnaire as the participants in the intervention arm. They were asked to circle their code status preference. If they chose to ask questions about resuscitation, these were answered, but the study coordinator did not volunteer information about resuscitation or intervene in the medical care of the participants in any way.
All participants’ demographic characteristics and outcomes were described using proportions for categorical variables and means ± standard deviation for continuous variables. The primary outcome was participants’ stated code preference (full code, DNR, or DNR/DNI). Secondary outcomes included comparison of trust in medical providers, resuscitation beliefs, and desire for life-prolonging interventions as obtained from the questionnaire.
We analyzed code preferences between the intervention and control groups using Fisher exact test. We used analysis of variance (ANOVA) to compare questionnaire responses between the 2 groups. All reported P values are 2-sided with P < 0.05 considered significant. The project originally targeted a sample size of 194 participants for 80% power to detect a 20% difference in the code preference choices between intervention and control groups. Given the short time frame available to enroll participants, the target sample size was not reached. Propitiously, the effect size was greater than originally expected.
RESULTS
Study Participants
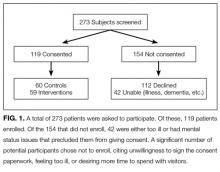
A total of 273 potentially eligible patients were approached to participate and 119 (44%) enrolled. (Figure 1). Of the 154 patients that were deemed eligible after initial screening, 42 patients were unable to give consent due to the severity of their illness or because of their mental status. Another 112 patients declined participation in the study, citing reasons such as disinterest in the consent paperwork, desire to spend time with visitors, and unease with the subject matter. Patients who declined participation did not differ significantly by age, sex, or race from those enrolled in the study.
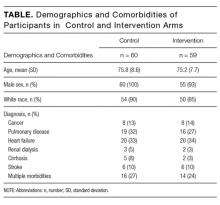
Among the 119 participants, 60 were randomized to the control arm, and 59 were randomized to the intervention arm. Participants in the 2 arms did not differ significantly in age, sex, or race (P > 0.05), although all 4 women in the study were randomized to the intervention arm. Eighty-seven percent of the study population identified as white with the remainder including black, Asian, Pacific Islander, Native American, or declining to answer. The mean age was 75.8 years in the control arm vs. 75.2 years in the intervention arm.
Primary diagnoses in the study group ranged widely from relatively minor skin infections to acute pancreatitis. The control arm and the intervention arm did not differ significantly in the incidence of heart failure, pulmonary disease, renal dialysis, cirrhosis, stroke, or active cancer (P > 0.05). Patients were considered as having a stroke if they had suffered a stroke during their hospital admission or if they had long-term sequelae of prior stroke. Patients were considered as having active cancer if they were currently undergoing treatment or had metastases. Participants were considered as having multiple morbidities if they possessed 2 or more of the listed conditions. Between the control arm and the intervention arm, there was no significant difference in the number of participants with multiple morbidities (27% in the control group and 24% in the video group).
Code Status Preference
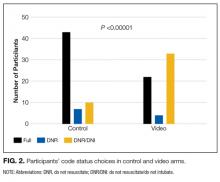
There was a significant difference in the code status preferences of the intervention arm and the control arm (P < 0.00001; Figure 2). In the control arm, 71% of participants chose full code, 12% chose DNR, and 17% chose DNR/DNI. In the intervention arm, only 37% chose full code, 7% chose DNR, and 56% chose DNR/DNI.
Secondary outcomes
Participants in the control and intervention arms were asked about their trust in their medical team (Question 1, Figure 3). There was no significant difference, but a trend towards less trust in the intervention group (P = 0.083) was seen with 93% of the control arm and 76% of the intervention arm agreeing with the statement “My doctors and healthcare team want what is best for me.”
Question 2, “If I choose to avoid resuscitation efforts, I will not receive care,” was designed to assess participants’ knowledge and perception about the care they would receive if they chose DNR/DNI as their code status. No significant difference was seen between the control and the interventions arms, with 28% of the control group agreeing with the statement, compared to 22% of the video group.
For question 3, participants were asked to respond to the statement “I would like to live as long as possible, even if I never leave the hospital.” No significant differences were seen between the control and the intervention arms, with 22% of both groups agreeing with the statement.
When we examined participant responses by the code status chosen, a significantly higher percentage of participants who chose full code agreed with the statement in question 3 (P = 0.0133). Of participants who chose full code, 27% agreed with the statement, compared to 18% of participants who chose DNR and 12% of participants who chose DNR/DNI. There was no significant difference (P > 0.05) between participant code status choice and either Question 1 or 2.
DISCUSSION
This study examined the effect of watching a video about CPR and intubation on the code status preferences of hospitalized patients. Participants who viewed a video about CPR and intubation were more likely to choose to forgo these treatments. Participants who chose CPR and intubation were more likely to agree that they would want to live as long as possible even if that time were spent in a medical setting.
To our knowledge, this is the first study to examine the role of a video decision support tool about code choices in the general hospital population, regardless of prognosis. Previous work has trialed the use of video support tools in hospitalized patients with a prognosis of less than 1 year,15 patients admitted to the ICU,18 and outpatients with cancer18 and those with dementia.16 Unlike previous studies, our study included a variety of illness severity.
Discussions about resuscitation are important for all adults admitted to the hospital because of the unpredictable nature of illness and the importance of providing high-quality care at the end of life. A recent study indicates that in-hospital cardiopulmonary arrest occurs in almost 1 per 1000 hospital days.19 These discussions are particularly salient for patients 65 years and older because of the higher incidence of death in this group. Inpatient admission is often a result of a change in health status, making it an important time for patients to reassess their resuscitation preferences based on their physical state and known comorbidities.
Video tools supplement the traditional code status discussion in several key ways. They provide a visual simulation of the procedures that occur during a typical resuscitation. These tools can help patients understand what CPR and intubation entail and transmit information that might be missed in verbal discussions. Visual media is now a common way for patients to obtain medical information20-22 and may be particularly helpful to patients who have low health literacy.23Video tools also help ensure that patients receive all the facts about resuscitation irrespective of how busy their provider may be or how comfortable the provider is with the topic. Lastly, video tools can reinforce information that is shared in the initial code status discussion. Given the significant differences in code status preference between our control and video arms, it is clear that the video tool has a significant impact on patient choices.
While we feel that our study clearly indicates the utility of video tools in code status discussion in hospitalized patients, there are some limitations. The current study enrolled participants who were predominantly white and male. All participants were recruited from the Minneapolis Veterans Affairs Health Care System, Minnesota. The relatively homogenous study population may impact the study’s generalizability. Another potential limitation of our study was the large number of eligible participants who declined to participate (41%), with many citing that they did not want to sign the consent paperwork. Additionally, the study coordinator was not blinded to the randomization of the participants, which could result in ascertainment bias. Also of concern was a trend, albeit nonsignificant, towards less trust in the healthcare team in the video group. Because the study was not designed to assess trust in the healthcare team both before and after the intervention, it is unclear if this difference was a result of the video.
Another area of potential concern is that visual images can be edited to sway viewers’ opinions based on the way content is presented. In our video, we included input from palliative care and internal medicine specialists. Cardiopulmonary resuscitation and intubation were performed on a CPR mannequin. The risks and benefits of CPR and intubation were discussed, as were the implications of choosing DNR or DNR/DNI code statuses.
The questionnaire that we used to assess participants’ knowledge and beliefs about resuscitation showed no differences between the control and the intervention arms of the study. We were surprised that a significant number of participants in the intervention group agreed with the statement, “If I choose to avoid resuscitation efforts, I will not receive care.” Our video specifically addressed the common belief that choosing DNR/DNI or DNR code statuses means that a patient will not continue to receive medical care. It is possible that participants were confused by the way the question was worded or that they understood the question to apply only to care received after a cardiopulmonary arrest had occurred.
This study and several others14-16 show that the use of video tools impacts participants’ code status preferences. There is clinical and humanistic importance in helping patients make informed decisions regarding whether or not they would want CPR and/or intubation if their heart were to stop or if they were to stop breathing. The data suggest that video tools are an efficient way to improve patient care and should be made widely available.
Disclosures: The authors report no conflicts of interest.
1. Dunn RH, Ahn J, Bernstein J. End-of-life care planning and fragility fractures of the hip: are we missing a valuable opportunity? Clin Orthop Relat Res 2016;474(7):1736-1739. PubMed
2. Warren MB, Lapid MI, McKean AJ, Cha SS, Stevens MA, Brekke FM, et al. Code status discussions in psychiatric and medical inpatients. J Clin Psychiatry. 2015;76(1):49-53. PubMed
3. Bhatia HL, Patel NR, Choma NN, Grande J, Giuse DA, Lehmann CU. Code status and resuscitation options in the electronic health record. Resuscitation. 2015;87:14-20. PubMed
4. Singh S, Namrata, Grewal A, Gautam PL, Luthra N, Kaur A. Evaluation of cardiopulmonary resuscitation (CPR) for patient outcomes and their predictors. J Clin Diagn Res. 2016;10(1):UC01-UC04. PubMed
5. Anderson WG, Chase R, Pantilat SZ, Tulsky JA, Auerbach AD. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med. 2011;26(4):359-366. PubMed
6. Einstein DJ, Einstein KL, Mathew P. Dying for advice: code status discussions between resident physicians and patients with advanced cancer--a national survey. J Palliat Med. 2015;18(6):535-541. PubMed
7. Piscator E, Hedberg P, Göransson K, Djärv T. Survival after in-hospital cardiac arrest is highly associated with the Age-combined Charlson Co-morbidity Index in a cohort study from a two-site Swedish University hospital. Resuscitation. 2016;99:79-83. PubMed
8. Zijlstra TJ, Leenman-Dekker SJ, Oldenhuis HK, Bosveld HE, Berendsen AJ. Knowledge and preferences regarding cardiopulmonary resuscitation: A survey among older patients. Patient Educ Couns. 2016;99(1):160-163. PubMed
9. Wilson ME, Akhoundi A, Krupa AK, Hinds RF, Litell JM, Gajic O, Kashani K. Development, validation, and results of a survey to measure understanding of cardiopulmonary resuscitation choices among ICU patients and their surrogate decision makers. BMC Anesthesiol. 2014;14:15. PubMed
10. Harris D, Willoughby H. Resuscitation on television: realistic or ridiculous? A quantitative observational analysis of the portrayal of cardiopulmonary resuscitation in television medical drama. Resuscitation. 2009;80(11):1275-1279. PubMed
11. Mills LM, Rhoads C, Curtis JR. Medical student training on code status discussions: how far have we come? J Palliat Med. 2016;19(3):323-325. PubMed
12. Binder AF, Huang GC, Buss MK. Uninformed consent: do medicine residents lack the proper framework for code status discussions? J Hosp Med. 2016;11(2):111-116. PubMed
13. Volandes AE, Levin TT, Slovin S, Carvajal RD, O’Reilly EM, et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention-postintervention study. Cancer. 2012;118(17):4331-4338. PubMed
14. El-Jawahri A, Podgurski LM, Eichler AF, Plotkin SR, Temel JS, Mitchell SL, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305-310. PubMed
15. El-Jawahri A, Mitchell SL, Paasche-Orlow MK, Temel JS, Jackson VA, Rutledge RR, et al. A randomized controlled trial of a CPR and intubation video decision support tool for hospitalized patients. J Gen Intern Med. 2015;30(8):1071-1080. PubMed
16. Volandes AE, Paasche-Orlow MK, Barry MJ, Gillick MR, Minaker KL, Chang Y, et al. Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ. 2009;338:b2159. PubMed
17. Celso BG, Meenrajan S. The triad that matters: palliative medicine, code status, and health care costs. Am J Hosp Palliat Care. 2010;27(6):398-401. PubMed
18. Wilson ME, Krupa A, Hinds RF, Litell JM, Swetz KM, Akhoundi A, et al. A video to improve patient and surrogate understanding of cardiopulmonary resuscitation choices in the ICU: a randomized controlled trial. Crit Care Med. 2015;43(3):621-629. PubMed
19. Overdyk FJ, Dowling O, Marino J, Qiu J, Chien HL, Erslon M, et al. Association of opioids and sedatives with increased risk of in-hospital cardiopulmonary arrest from an administrative database. PLoS One. 2016;11(2):e0150214. PubMed
20. Stacey D, Samant R, Bennett C. Decision making in oncology: a review of patient decision aids to support patient participation. CA Cancer J Clin. 2008;58(5)293-304. PubMed
21. Lin GA, Aaronson DS, Knight SJ, Carroll PR, Dudley RA. Patient decision aids for prostate cancer treatment: a systematic review of the literature. CA Cancer J Clin. 2009;59(6):379-390. PubMed
22. O’Brien MA, Whelan TJ, Villasis-Keever M, Gafni A, Charles C, Roberts R, et al. Are cancer-related decision aids effective? A systematic review and meta-analysis. J Clin Oncol. 2009;27(6):974-985. PubMed
23. Sudore RL, Landefeld CS, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75(3):398-402. PubMed
Discussions about cardiopulmonary resuscitation (CPR) can be difficult due to their association with end of life. The Patient Self Determination Act (H.R.4449 — 101st Congress [1989-1990]) and institutional standards mandate collaboration between care providers and patients regarding goals of care in emergency situations such as cardiopulmonary arrest. The default option is to provide CPR, which may involve chest compressions, intubation, and/or defibrillation. Yet numerous studies show that a significant number of patients have no code preference documented in their medical chart, and even fewer report a conversation with their care provider about their wishes regarding CPR.1-3 CPR is an invasive and potentially painful procedure with a higher chance of failure than success4, and yet many patients report that their provider did not discuss with them the risks and benefits of resuscitation.5,6 Further highlighting the importance of individual discussions about CPR preferences is the reality that factors such as age and disease burden further skew the likelihood of survival after cardiopulmonary arrest.7
Complicating the lack of appropriate provider and patient discussion of the risks and benefits of resuscitation are significant misunderstandings about CPR in the lay population. Patients routinely overestimate the likelihood of survival following CPR.8,9 This may be partially due to the portrayal of CPR in the lay media as highly efficacious.10 Other factors known to prevent effective provider-and-patient discussions about CPR preferences are providers’ discomfort with the subject11 and perceived time constraints.12
Informational videos have been developed to assist patients with decision making about CPR and have been shown to impact patients’ choices in the setting of life-limiting diseases such as advanced cancer,13-14 serious illness with a prognosis of less than 1 year,15 and dementia.16 While discussion of code status is vitally important in end-of-life planning for seriously ill individuals, delayed discussion of CPR preferences is associated with a significant increase in the number of invasive procedures performed at the end of life, increased length of stay in the hospital, and increased medical cost.17 Despite clear evidence that earlier discussion of resuscitation options are valuable, no studies have examined the impact of a video about code status options in the general patient population.
Here we present our findings of a randomized trial in patients hospitalized on the general medicine wards who were 65 years of age or older, regardless of illness severity or diagnosis. The video tool was a supplement for, rather than a replacement of, standard provider and patient communication about code preferences, and we compared patients who watched the video against controls who had standard discussions with their providers. Our video detailed the process of chest compressions and intubation during CPR and explained the differences between the code statuses: full code, do not resuscitate (DNR), and do not resuscitate/do not intubate (DNR/DNI). We found a significant difference between the 2 groups, with significantly more individuals in the video group choosing DNR/DNI. These findings suggest that video support tools may be a useful supplement to traditional provider discussions about code preferences in the general patient population.
METHODS
We enrolled patients from the general medicine wards at the Minneapolis VA Hospital from September 28, 2015 to October 23, 2015. Eligibility criteria included age 65 years or older, ability to provide informed consent, and ability to communicate in English. Study recruitment and data collection were performed by a study coordinator who was a house staff physician and had no role in the care of the participants. The medical charts of all general medicine patients were reviewed to determine if they met the age criteria. The physician of record for potential participants was contacted to assess if the patient was able to provide informed consent and communicate in English. Eligible patients were approached and informed consent was obtained from those who chose to participate in the study. After obtaining informed consent, patients were randomized using a random number generator to the intervention or usual-care arm of the study.
Those who were assigned to the intervention arm watched a 6-minute long video explaining the code-preference choices of full code, DNR, or DNR/DNI. Full code was described as possibly including CPR, intubation, and/or defibrillation depending on the clinical situation. Do not resuscitate was described as meaning no CPR or defibrillation but possible intubation in the case of respiratory failure. Do not resuscitate/do not intubate was explained as meaning no CPR, no defibrillation, and no intubation but rather permitting “natural death” to occur. The video showed a mock code with chest compressions, defibrillation, and intubation on a mannequin as well as palliative care specialists who discussed potential complications and survival rates of inhospital resuscitation.
The video was created at the University of Minnesota with the departments of palliative care and internal medicine (www.mmcgmeservices.org/codestat.html). After viewing the video, participants in the intervention arm filled out a questionnaire designed to assess their knowledge and beliefs about CPR and trust in their medical care providers. They were asked to circle their code preference. The participants’ medical teams were made aware of the code preferences and were counseled to discuss code preferences further if it was different from their previously documented code preference.
Participants in the control arm were assigned to usual care. At the institution where this study occurred, a discussion about code preferences between the patient and their medical team is considered the standard of care. After informed consent was obtained, participants filled out the same questionnaire as the participants in the intervention arm. They were asked to circle their code status preference. If they chose to ask questions about resuscitation, these were answered, but the study coordinator did not volunteer information about resuscitation or intervene in the medical care of the participants in any way.
All participants’ demographic characteristics and outcomes were described using proportions for categorical variables and means ± standard deviation for continuous variables. The primary outcome was participants’ stated code preference (full code, DNR, or DNR/DNI). Secondary outcomes included comparison of trust in medical providers, resuscitation beliefs, and desire for life-prolonging interventions as obtained from the questionnaire.
We analyzed code preferences between the intervention and control groups using Fisher exact test. We used analysis of variance (ANOVA) to compare questionnaire responses between the 2 groups. All reported P values are 2-sided with P < 0.05 considered significant. The project originally targeted a sample size of 194 participants for 80% power to detect a 20% difference in the code preference choices between intervention and control groups. Given the short time frame available to enroll participants, the target sample size was not reached. Propitiously, the effect size was greater than originally expected.
RESULTS
Study Participants
A total of 273 potentially eligible patients were approached to participate and 119 (44%) enrolled. (Figure 1). Of the 154 patients that were deemed eligible after initial screening, 42 patients were unable to give consent due to the severity of their illness or because of their mental status. Another 112 patients declined participation in the study, citing reasons such as disinterest in the consent paperwork, desire to spend time with visitors, and unease with the subject matter. Patients who declined participation did not differ significantly by age, sex, or race from those enrolled in the study.
Among the 119 participants, 60 were randomized to the control arm, and 59 were randomized to the intervention arm. Participants in the 2 arms did not differ significantly in age, sex, or race (P > 0.05), although all 4 women in the study were randomized to the intervention arm. Eighty-seven percent of the study population identified as white with the remainder including black, Asian, Pacific Islander, Native American, or declining to answer. The mean age was 75.8 years in the control arm vs. 75.2 years in the intervention arm.
Primary diagnoses in the study group ranged widely from relatively minor skin infections to acute pancreatitis. The control arm and the intervention arm did not differ significantly in the incidence of heart failure, pulmonary disease, renal dialysis, cirrhosis, stroke, or active cancer (P > 0.05). Patients were considered as having a stroke if they had suffered a stroke during their hospital admission or if they had long-term sequelae of prior stroke. Patients were considered as having active cancer if they were currently undergoing treatment or had metastases. Participants were considered as having multiple morbidities if they possessed 2 or more of the listed conditions. Between the control arm and the intervention arm, there was no significant difference in the number of participants with multiple morbidities (27% in the control group and 24% in the video group).
Code Status Preference
There was a significant difference in the code status preferences of the intervention arm and the control arm (P < 0.00001; Figure 2). In the control arm, 71% of participants chose full code, 12% chose DNR, and 17% chose DNR/DNI. In the intervention arm, only 37% chose full code, 7% chose DNR, and 56% chose DNR/DNI.
Secondary outcomes
Participants in the control and intervention arms were asked about their trust in their medical team (Question 1, Figure 3). There was no significant difference, but a trend towards less trust in the intervention group (P = 0.083) was seen with 93% of the control arm and 76% of the intervention arm agreeing with the statement “My doctors and healthcare team want what is best for me.”
Question 2, “If I choose to avoid resuscitation efforts, I will not receive care,” was designed to assess participants’ knowledge and perception about the care they would receive if they chose DNR/DNI as their code status. No significant difference was seen between the control and the interventions arms, with 28% of the control group agreeing with the statement, compared to 22% of the video group.
For question 3, participants were asked to respond to the statement “I would like to live as long as possible, even if I never leave the hospital.” No significant differences were seen between the control and the intervention arms, with 22% of both groups agreeing with the statement.
When we examined participant responses by the code status chosen, a significantly higher percentage of participants who chose full code agreed with the statement in question 3 (P = 0.0133). Of participants who chose full code, 27% agreed with the statement, compared to 18% of participants who chose DNR and 12% of participants who chose DNR/DNI. There was no significant difference (P > 0.05) between participant code status choice and either Question 1 or 2.
DISCUSSION
This study examined the effect of watching a video about CPR and intubation on the code status preferences of hospitalized patients. Participants who viewed a video about CPR and intubation were more likely to choose to forgo these treatments. Participants who chose CPR and intubation were more likely to agree that they would want to live as long as possible even if that time were spent in a medical setting.
To our knowledge, this is the first study to examine the role of a video decision support tool about code choices in the general hospital population, regardless of prognosis. Previous work has trialed the use of video support tools in hospitalized patients with a prognosis of less than 1 year,15 patients admitted to the ICU,18 and outpatients with cancer18 and those with dementia.16 Unlike previous studies, our study included a variety of illness severity.
Discussions about resuscitation are important for all adults admitted to the hospital because of the unpredictable nature of illness and the importance of providing high-quality care at the end of life. A recent study indicates that in-hospital cardiopulmonary arrest occurs in almost 1 per 1000 hospital days.19 These discussions are particularly salient for patients 65 years and older because of the higher incidence of death in this group. Inpatient admission is often a result of a change in health status, making it an important time for patients to reassess their resuscitation preferences based on their physical state and known comorbidities.
Video tools supplement the traditional code status discussion in several key ways. They provide a visual simulation of the procedures that occur during a typical resuscitation. These tools can help patients understand what CPR and intubation entail and transmit information that might be missed in verbal discussions. Visual media is now a common way for patients to obtain medical information20-22 and may be particularly helpful to patients who have low health literacy.23Video tools also help ensure that patients receive all the facts about resuscitation irrespective of how busy their provider may be or how comfortable the provider is with the topic. Lastly, video tools can reinforce information that is shared in the initial code status discussion. Given the significant differences in code status preference between our control and video arms, it is clear that the video tool has a significant impact on patient choices.
While we feel that our study clearly indicates the utility of video tools in code status discussion in hospitalized patients, there are some limitations. The current study enrolled participants who were predominantly white and male. All participants were recruited from the Minneapolis Veterans Affairs Health Care System, Minnesota. The relatively homogenous study population may impact the study’s generalizability. Another potential limitation of our study was the large number of eligible participants who declined to participate (41%), with many citing that they did not want to sign the consent paperwork. Additionally, the study coordinator was not blinded to the randomization of the participants, which could result in ascertainment bias. Also of concern was a trend, albeit nonsignificant, towards less trust in the healthcare team in the video group. Because the study was not designed to assess trust in the healthcare team both before and after the intervention, it is unclear if this difference was a result of the video.
Another area of potential concern is that visual images can be edited to sway viewers’ opinions based on the way content is presented. In our video, we included input from palliative care and internal medicine specialists. Cardiopulmonary resuscitation and intubation were performed on a CPR mannequin. The risks and benefits of CPR and intubation were discussed, as were the implications of choosing DNR or DNR/DNI code statuses.
The questionnaire that we used to assess participants’ knowledge and beliefs about resuscitation showed no differences between the control and the intervention arms of the study. We were surprised that a significant number of participants in the intervention group agreed with the statement, “If I choose to avoid resuscitation efforts, I will not receive care.” Our video specifically addressed the common belief that choosing DNR/DNI or DNR code statuses means that a patient will not continue to receive medical care. It is possible that participants were confused by the way the question was worded or that they understood the question to apply only to care received after a cardiopulmonary arrest had occurred.
This study and several others14-16 show that the use of video tools impacts participants’ code status preferences. There is clinical and humanistic importance in helping patients make informed decisions regarding whether or not they would want CPR and/or intubation if their heart were to stop or if they were to stop breathing. The data suggest that video tools are an efficient way to improve patient care and should be made widely available.
Disclosures: The authors report no conflicts of interest.
Discussions about cardiopulmonary resuscitation (CPR) can be difficult due to their association with end of life. The Patient Self Determination Act (H.R.4449 — 101st Congress [1989-1990]) and institutional standards mandate collaboration between care providers and patients regarding goals of care in emergency situations such as cardiopulmonary arrest. The default option is to provide CPR, which may involve chest compressions, intubation, and/or defibrillation. Yet numerous studies show that a significant number of patients have no code preference documented in their medical chart, and even fewer report a conversation with their care provider about their wishes regarding CPR.1-3 CPR is an invasive and potentially painful procedure with a higher chance of failure than success4, and yet many patients report that their provider did not discuss with them the risks and benefits of resuscitation.5,6 Further highlighting the importance of individual discussions about CPR preferences is the reality that factors such as age and disease burden further skew the likelihood of survival after cardiopulmonary arrest.7
Complicating the lack of appropriate provider and patient discussion of the risks and benefits of resuscitation are significant misunderstandings about CPR in the lay population. Patients routinely overestimate the likelihood of survival following CPR.8,9 This may be partially due to the portrayal of CPR in the lay media as highly efficacious.10 Other factors known to prevent effective provider-and-patient discussions about CPR preferences are providers’ discomfort with the subject11 and perceived time constraints.12
Informational videos have been developed to assist patients with decision making about CPR and have been shown to impact patients’ choices in the setting of life-limiting diseases such as advanced cancer,13-14 serious illness with a prognosis of less than 1 year,15 and dementia.16 While discussion of code status is vitally important in end-of-life planning for seriously ill individuals, delayed discussion of CPR preferences is associated with a significant increase in the number of invasive procedures performed at the end of life, increased length of stay in the hospital, and increased medical cost.17 Despite clear evidence that earlier discussion of resuscitation options are valuable, no studies have examined the impact of a video about code status options in the general patient population.
Here we present our findings of a randomized trial in patients hospitalized on the general medicine wards who were 65 years of age or older, regardless of illness severity or diagnosis. The video tool was a supplement for, rather than a replacement of, standard provider and patient communication about code preferences, and we compared patients who watched the video against controls who had standard discussions with their providers. Our video detailed the process of chest compressions and intubation during CPR and explained the differences between the code statuses: full code, do not resuscitate (DNR), and do not resuscitate/do not intubate (DNR/DNI). We found a significant difference between the 2 groups, with significantly more individuals in the video group choosing DNR/DNI. These findings suggest that video support tools may be a useful supplement to traditional provider discussions about code preferences in the general patient population.
METHODS
We enrolled patients from the general medicine wards at the Minneapolis VA Hospital from September 28, 2015 to October 23, 2015. Eligibility criteria included age 65 years or older, ability to provide informed consent, and ability to communicate in English. Study recruitment and data collection were performed by a study coordinator who was a house staff physician and had no role in the care of the participants. The medical charts of all general medicine patients were reviewed to determine if they met the age criteria. The physician of record for potential participants was contacted to assess if the patient was able to provide informed consent and communicate in English. Eligible patients were approached and informed consent was obtained from those who chose to participate in the study. After obtaining informed consent, patients were randomized using a random number generator to the intervention or usual-care arm of the study.
Those who were assigned to the intervention arm watched a 6-minute long video explaining the code-preference choices of full code, DNR, or DNR/DNI. Full code was described as possibly including CPR, intubation, and/or defibrillation depending on the clinical situation. Do not resuscitate was described as meaning no CPR or defibrillation but possible intubation in the case of respiratory failure. Do not resuscitate/do not intubate was explained as meaning no CPR, no defibrillation, and no intubation but rather permitting “natural death” to occur. The video showed a mock code with chest compressions, defibrillation, and intubation on a mannequin as well as palliative care specialists who discussed potential complications and survival rates of inhospital resuscitation.
The video was created at the University of Minnesota with the departments of palliative care and internal medicine (www.mmcgmeservices.org/codestat.html). After viewing the video, participants in the intervention arm filled out a questionnaire designed to assess their knowledge and beliefs about CPR and trust in their medical care providers. They were asked to circle their code preference. The participants’ medical teams were made aware of the code preferences and were counseled to discuss code preferences further if it was different from their previously documented code preference.
Participants in the control arm were assigned to usual care. At the institution where this study occurred, a discussion about code preferences between the patient and their medical team is considered the standard of care. After informed consent was obtained, participants filled out the same questionnaire as the participants in the intervention arm. They were asked to circle their code status preference. If they chose to ask questions about resuscitation, these were answered, but the study coordinator did not volunteer information about resuscitation or intervene in the medical care of the participants in any way.
All participants’ demographic characteristics and outcomes were described using proportions for categorical variables and means ± standard deviation for continuous variables. The primary outcome was participants’ stated code preference (full code, DNR, or DNR/DNI). Secondary outcomes included comparison of trust in medical providers, resuscitation beliefs, and desire for life-prolonging interventions as obtained from the questionnaire.
We analyzed code preferences between the intervention and control groups using Fisher exact test. We used analysis of variance (ANOVA) to compare questionnaire responses between the 2 groups. All reported P values are 2-sided with P < 0.05 considered significant. The project originally targeted a sample size of 194 participants for 80% power to detect a 20% difference in the code preference choices between intervention and control groups. Given the short time frame available to enroll participants, the target sample size was not reached. Propitiously, the effect size was greater than originally expected.
RESULTS
Study Participants
A total of 273 potentially eligible patients were approached to participate and 119 (44%) enrolled. (Figure 1). Of the 154 patients that were deemed eligible after initial screening, 42 patients were unable to give consent due to the severity of their illness or because of their mental status. Another 112 patients declined participation in the study, citing reasons such as disinterest in the consent paperwork, desire to spend time with visitors, and unease with the subject matter. Patients who declined participation did not differ significantly by age, sex, or race from those enrolled in the study.
Among the 119 participants, 60 were randomized to the control arm, and 59 were randomized to the intervention arm. Participants in the 2 arms did not differ significantly in age, sex, or race (P > 0.05), although all 4 women in the study were randomized to the intervention arm. Eighty-seven percent of the study population identified as white with the remainder including black, Asian, Pacific Islander, Native American, or declining to answer. The mean age was 75.8 years in the control arm vs. 75.2 years in the intervention arm.
Primary diagnoses in the study group ranged widely from relatively minor skin infections to acute pancreatitis. The control arm and the intervention arm did not differ significantly in the incidence of heart failure, pulmonary disease, renal dialysis, cirrhosis, stroke, or active cancer (P > 0.05). Patients were considered as having a stroke if they had suffered a stroke during their hospital admission or if they had long-term sequelae of prior stroke. Patients were considered as having active cancer if they were currently undergoing treatment or had metastases. Participants were considered as having multiple morbidities if they possessed 2 or more of the listed conditions. Between the control arm and the intervention arm, there was no significant difference in the number of participants with multiple morbidities (27% in the control group and 24% in the video group).
Code Status Preference
There was a significant difference in the code status preferences of the intervention arm and the control arm (P < 0.00001; Figure 2). In the control arm, 71% of participants chose full code, 12% chose DNR, and 17% chose DNR/DNI. In the intervention arm, only 37% chose full code, 7% chose DNR, and 56% chose DNR/DNI.
Secondary outcomes
Participants in the control and intervention arms were asked about their trust in their medical team (Question 1, Figure 3). There was no significant difference, but a trend towards less trust in the intervention group (P = 0.083) was seen with 93% of the control arm and 76% of the intervention arm agreeing with the statement “My doctors and healthcare team want what is best for me.”
Question 2, “If I choose to avoid resuscitation efforts, I will not receive care,” was designed to assess participants’ knowledge and perception about the care they would receive if they chose DNR/DNI as their code status. No significant difference was seen between the control and the interventions arms, with 28% of the control group agreeing with the statement, compared to 22% of the video group.
For question 3, participants were asked to respond to the statement “I would like to live as long as possible, even if I never leave the hospital.” No significant differences were seen between the control and the intervention arms, with 22% of both groups agreeing with the statement.
When we examined participant responses by the code status chosen, a significantly higher percentage of participants who chose full code agreed with the statement in question 3 (P = 0.0133). Of participants who chose full code, 27% agreed with the statement, compared to 18% of participants who chose DNR and 12% of participants who chose DNR/DNI. There was no significant difference (P > 0.05) between participant code status choice and either Question 1 or 2.
DISCUSSION
This study examined the effect of watching a video about CPR and intubation on the code status preferences of hospitalized patients. Participants who viewed a video about CPR and intubation were more likely to choose to forgo these treatments. Participants who chose CPR and intubation were more likely to agree that they would want to live as long as possible even if that time were spent in a medical setting.
To our knowledge, this is the first study to examine the role of a video decision support tool about code choices in the general hospital population, regardless of prognosis. Previous work has trialed the use of video support tools in hospitalized patients with a prognosis of less than 1 year,15 patients admitted to the ICU,18 and outpatients with cancer18 and those with dementia.16 Unlike previous studies, our study included a variety of illness severity.
Discussions about resuscitation are important for all adults admitted to the hospital because of the unpredictable nature of illness and the importance of providing high-quality care at the end of life. A recent study indicates that in-hospital cardiopulmonary arrest occurs in almost 1 per 1000 hospital days.19 These discussions are particularly salient for patients 65 years and older because of the higher incidence of death in this group. Inpatient admission is often a result of a change in health status, making it an important time for patients to reassess their resuscitation preferences based on their physical state and known comorbidities.
Video tools supplement the traditional code status discussion in several key ways. They provide a visual simulation of the procedures that occur during a typical resuscitation. These tools can help patients understand what CPR and intubation entail and transmit information that might be missed in verbal discussions. Visual media is now a common way for patients to obtain medical information20-22 and may be particularly helpful to patients who have low health literacy.23Video tools also help ensure that patients receive all the facts about resuscitation irrespective of how busy their provider may be or how comfortable the provider is with the topic. Lastly, video tools can reinforce information that is shared in the initial code status discussion. Given the significant differences in code status preference between our control and video arms, it is clear that the video tool has a significant impact on patient choices.
While we feel that our study clearly indicates the utility of video tools in code status discussion in hospitalized patients, there are some limitations. The current study enrolled participants who were predominantly white and male. All participants were recruited from the Minneapolis Veterans Affairs Health Care System, Minnesota. The relatively homogenous study population may impact the study’s generalizability. Another potential limitation of our study was the large number of eligible participants who declined to participate (41%), with many citing that they did not want to sign the consent paperwork. Additionally, the study coordinator was not blinded to the randomization of the participants, which could result in ascertainment bias. Also of concern was a trend, albeit nonsignificant, towards less trust in the healthcare team in the video group. Because the study was not designed to assess trust in the healthcare team both before and after the intervention, it is unclear if this difference was a result of the video.
Another area of potential concern is that visual images can be edited to sway viewers’ opinions based on the way content is presented. In our video, we included input from palliative care and internal medicine specialists. Cardiopulmonary resuscitation and intubation were performed on a CPR mannequin. The risks and benefits of CPR and intubation were discussed, as were the implications of choosing DNR or DNR/DNI code statuses.
The questionnaire that we used to assess participants’ knowledge and beliefs about resuscitation showed no differences between the control and the intervention arms of the study. We were surprised that a significant number of participants in the intervention group agreed with the statement, “If I choose to avoid resuscitation efforts, I will not receive care.” Our video specifically addressed the common belief that choosing DNR/DNI or DNR code statuses means that a patient will not continue to receive medical care. It is possible that participants were confused by the way the question was worded or that they understood the question to apply only to care received after a cardiopulmonary arrest had occurred.
This study and several others14-16 show that the use of video tools impacts participants’ code status preferences. There is clinical and humanistic importance in helping patients make informed decisions regarding whether or not they would want CPR and/or intubation if their heart were to stop or if they were to stop breathing. The data suggest that video tools are an efficient way to improve patient care and should be made widely available.
Disclosures: The authors report no conflicts of interest.
1. Dunn RH, Ahn J, Bernstein J. End-of-life care planning and fragility fractures of the hip: are we missing a valuable opportunity? Clin Orthop Relat Res 2016;474(7):1736-1739. PubMed
2. Warren MB, Lapid MI, McKean AJ, Cha SS, Stevens MA, Brekke FM, et al. Code status discussions in psychiatric and medical inpatients. J Clin Psychiatry. 2015;76(1):49-53. PubMed
3. Bhatia HL, Patel NR, Choma NN, Grande J, Giuse DA, Lehmann CU. Code status and resuscitation options in the electronic health record. Resuscitation. 2015;87:14-20. PubMed
4. Singh S, Namrata, Grewal A, Gautam PL, Luthra N, Kaur A. Evaluation of cardiopulmonary resuscitation (CPR) for patient outcomes and their predictors. J Clin Diagn Res. 2016;10(1):UC01-UC04. PubMed
5. Anderson WG, Chase R, Pantilat SZ, Tulsky JA, Auerbach AD. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med. 2011;26(4):359-366. PubMed
6. Einstein DJ, Einstein KL, Mathew P. Dying for advice: code status discussions between resident physicians and patients with advanced cancer--a national survey. J Palliat Med. 2015;18(6):535-541. PubMed
7. Piscator E, Hedberg P, Göransson K, Djärv T. Survival after in-hospital cardiac arrest is highly associated with the Age-combined Charlson Co-morbidity Index in a cohort study from a two-site Swedish University hospital. Resuscitation. 2016;99:79-83. PubMed
8. Zijlstra TJ, Leenman-Dekker SJ, Oldenhuis HK, Bosveld HE, Berendsen AJ. Knowledge and preferences regarding cardiopulmonary resuscitation: A survey among older patients. Patient Educ Couns. 2016;99(1):160-163. PubMed
9. Wilson ME, Akhoundi A, Krupa AK, Hinds RF, Litell JM, Gajic O, Kashani K. Development, validation, and results of a survey to measure understanding of cardiopulmonary resuscitation choices among ICU patients and their surrogate decision makers. BMC Anesthesiol. 2014;14:15. PubMed
10. Harris D, Willoughby H. Resuscitation on television: realistic or ridiculous? A quantitative observational analysis of the portrayal of cardiopulmonary resuscitation in television medical drama. Resuscitation. 2009;80(11):1275-1279. PubMed
11. Mills LM, Rhoads C, Curtis JR. Medical student training on code status discussions: how far have we come? J Palliat Med. 2016;19(3):323-325. PubMed
12. Binder AF, Huang GC, Buss MK. Uninformed consent: do medicine residents lack the proper framework for code status discussions? J Hosp Med. 2016;11(2):111-116. PubMed
13. Volandes AE, Levin TT, Slovin S, Carvajal RD, O’Reilly EM, et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention-postintervention study. Cancer. 2012;118(17):4331-4338. PubMed
14. El-Jawahri A, Podgurski LM, Eichler AF, Plotkin SR, Temel JS, Mitchell SL, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305-310. PubMed
15. El-Jawahri A, Mitchell SL, Paasche-Orlow MK, Temel JS, Jackson VA, Rutledge RR, et al. A randomized controlled trial of a CPR and intubation video decision support tool for hospitalized patients. J Gen Intern Med. 2015;30(8):1071-1080. PubMed
16. Volandes AE, Paasche-Orlow MK, Barry MJ, Gillick MR, Minaker KL, Chang Y, et al. Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ. 2009;338:b2159. PubMed
17. Celso BG, Meenrajan S. The triad that matters: palliative medicine, code status, and health care costs. Am J Hosp Palliat Care. 2010;27(6):398-401. PubMed
18. Wilson ME, Krupa A, Hinds RF, Litell JM, Swetz KM, Akhoundi A, et al. A video to improve patient and surrogate understanding of cardiopulmonary resuscitation choices in the ICU: a randomized controlled trial. Crit Care Med. 2015;43(3):621-629. PubMed
19. Overdyk FJ, Dowling O, Marino J, Qiu J, Chien HL, Erslon M, et al. Association of opioids and sedatives with increased risk of in-hospital cardiopulmonary arrest from an administrative database. PLoS One. 2016;11(2):e0150214. PubMed
20. Stacey D, Samant R, Bennett C. Decision making in oncology: a review of patient decision aids to support patient participation. CA Cancer J Clin. 2008;58(5)293-304. PubMed
21. Lin GA, Aaronson DS, Knight SJ, Carroll PR, Dudley RA. Patient decision aids for prostate cancer treatment: a systematic review of the literature. CA Cancer J Clin. 2009;59(6):379-390. PubMed
22. O’Brien MA, Whelan TJ, Villasis-Keever M, Gafni A, Charles C, Roberts R, et al. Are cancer-related decision aids effective? A systematic review and meta-analysis. J Clin Oncol. 2009;27(6):974-985. PubMed
23. Sudore RL, Landefeld CS, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75(3):398-402. PubMed
1. Dunn RH, Ahn J, Bernstein J. End-of-life care planning and fragility fractures of the hip: are we missing a valuable opportunity? Clin Orthop Relat Res 2016;474(7):1736-1739. PubMed
2. Warren MB, Lapid MI, McKean AJ, Cha SS, Stevens MA, Brekke FM, et al. Code status discussions in psychiatric and medical inpatients. J Clin Psychiatry. 2015;76(1):49-53. PubMed
3. Bhatia HL, Patel NR, Choma NN, Grande J, Giuse DA, Lehmann CU. Code status and resuscitation options in the electronic health record. Resuscitation. 2015;87:14-20. PubMed
4. Singh S, Namrata, Grewal A, Gautam PL, Luthra N, Kaur A. Evaluation of cardiopulmonary resuscitation (CPR) for patient outcomes and their predictors. J Clin Diagn Res. 2016;10(1):UC01-UC04. PubMed
5. Anderson WG, Chase R, Pantilat SZ, Tulsky JA, Auerbach AD. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med. 2011;26(4):359-366. PubMed
6. Einstein DJ, Einstein KL, Mathew P. Dying for advice: code status discussions between resident physicians and patients with advanced cancer--a national survey. J Palliat Med. 2015;18(6):535-541. PubMed
7. Piscator E, Hedberg P, Göransson K, Djärv T. Survival after in-hospital cardiac arrest is highly associated with the Age-combined Charlson Co-morbidity Index in a cohort study from a two-site Swedish University hospital. Resuscitation. 2016;99:79-83. PubMed
8. Zijlstra TJ, Leenman-Dekker SJ, Oldenhuis HK, Bosveld HE, Berendsen AJ. Knowledge and preferences regarding cardiopulmonary resuscitation: A survey among older patients. Patient Educ Couns. 2016;99(1):160-163. PubMed
9. Wilson ME, Akhoundi A, Krupa AK, Hinds RF, Litell JM, Gajic O, Kashani K. Development, validation, and results of a survey to measure understanding of cardiopulmonary resuscitation choices among ICU patients and their surrogate decision makers. BMC Anesthesiol. 2014;14:15. PubMed
10. Harris D, Willoughby H. Resuscitation on television: realistic or ridiculous? A quantitative observational analysis of the portrayal of cardiopulmonary resuscitation in television medical drama. Resuscitation. 2009;80(11):1275-1279. PubMed
11. Mills LM, Rhoads C, Curtis JR. Medical student training on code status discussions: how far have we come? J Palliat Med. 2016;19(3):323-325. PubMed
12. Binder AF, Huang GC, Buss MK. Uninformed consent: do medicine residents lack the proper framework for code status discussions? J Hosp Med. 2016;11(2):111-116. PubMed
13. Volandes AE, Levin TT, Slovin S, Carvajal RD, O’Reilly EM, et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention-postintervention study. Cancer. 2012;118(17):4331-4338. PubMed
14. El-Jawahri A, Podgurski LM, Eichler AF, Plotkin SR, Temel JS, Mitchell SL, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305-310. PubMed
15. El-Jawahri A, Mitchell SL, Paasche-Orlow MK, Temel JS, Jackson VA, Rutledge RR, et al. A randomized controlled trial of a CPR and intubation video decision support tool for hospitalized patients. J Gen Intern Med. 2015;30(8):1071-1080. PubMed
16. Volandes AE, Paasche-Orlow MK, Barry MJ, Gillick MR, Minaker KL, Chang Y, et al. Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ. 2009;338:b2159. PubMed
17. Celso BG, Meenrajan S. The triad that matters: palliative medicine, code status, and health care costs. Am J Hosp Palliat Care. 2010;27(6):398-401. PubMed
18. Wilson ME, Krupa A, Hinds RF, Litell JM, Swetz KM, Akhoundi A, et al. A video to improve patient and surrogate understanding of cardiopulmonary resuscitation choices in the ICU: a randomized controlled trial. Crit Care Med. 2015;43(3):621-629. PubMed
19. Overdyk FJ, Dowling O, Marino J, Qiu J, Chien HL, Erslon M, et al. Association of opioids and sedatives with increased risk of in-hospital cardiopulmonary arrest from an administrative database. PLoS One. 2016;11(2):e0150214. PubMed
20. Stacey D, Samant R, Bennett C. Decision making in oncology: a review of patient decision aids to support patient participation. CA Cancer J Clin. 2008;58(5)293-304. PubMed
21. Lin GA, Aaronson DS, Knight SJ, Carroll PR, Dudley RA. Patient decision aids for prostate cancer treatment: a systematic review of the literature. CA Cancer J Clin. 2009;59(6):379-390. PubMed
22. O’Brien MA, Whelan TJ, Villasis-Keever M, Gafni A, Charles C, Roberts R, et al. Are cancer-related decision aids effective? A systematic review and meta-analysis. J Clin Oncol. 2009;27(6):974-985. PubMed
23. Sudore RL, Landefeld CS, Pérez-Stable EJ, Bibbins-Domingo K, Williams BA, Schillinger D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009;75(3):398-402. PubMed
© 2017 Society of Hospital Medicine