User login
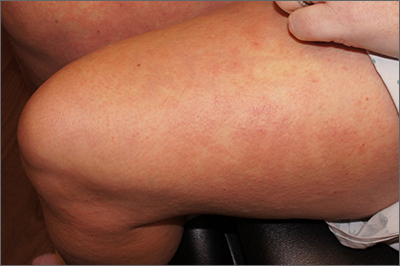
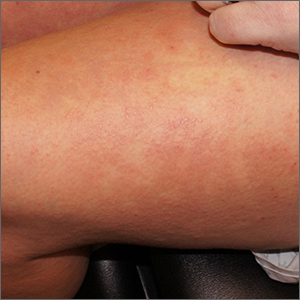
A punch biopsy revealed lichenoid interface dermatitis with eosinophils and mild spongiosis—consistent with, but not conclusive for, a drug eruption. A complete blood count (CBC) and comprehensive metabolic panel revealed elevated levels of eosinophils and transaminases which raised the possibility of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. In this patient’s case, the transaminitis suggested some mild hepatitis; the liver is the most common organ involved in DRESS.
Diagnostic criteria for DRESS syndrome need not always be met but can include fever, lymphadenopathy, facial edema, and a morbilliform rash presenting 2 to 3 weeks after drug exposure. In this case, a lack of fever, facial edema, and other systemic symptoms favored a less severe drug eruption or what has been described as mini-DRESS.1 DRESS syndrome often merits hospitalization, and in 10% of cases it can be fatal.1
The patient in this case was started on prednisone 60 mg/d and her OCPs were discontinued. One week later, a repeat CBC showed normalized levels of eosinophils and transaminases. However, shortly after a 3-week taper of the prednisone, her levels of eosinophils and transaminases rose again. A repeat prednisone taper finally led to complete resolution of rash and sustained normalization of eosinophil and transaminase levels.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
Isaacs M, Cardones AR, Rahnama-Moghadam S. DRESS syndrome: clinical myths and pearls. Cutis. 2018;102:322-326.
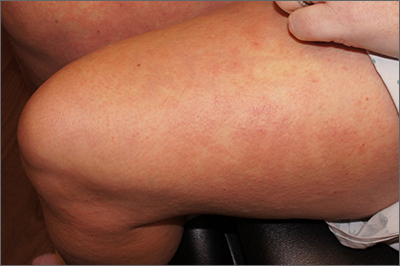
A punch biopsy revealed lichenoid interface dermatitis with eosinophils and mild spongiosis—consistent with, but not conclusive for, a drug eruption. A complete blood count (CBC) and comprehensive metabolic panel revealed elevated levels of eosinophils and transaminases which raised the possibility of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. In this patient’s case, the transaminitis suggested some mild hepatitis; the liver is the most common organ involved in DRESS.
Diagnostic criteria for DRESS syndrome need not always be met but can include fever, lymphadenopathy, facial edema, and a morbilliform rash presenting 2 to 3 weeks after drug exposure. In this case, a lack of fever, facial edema, and other systemic symptoms favored a less severe drug eruption or what has been described as mini-DRESS.1 DRESS syndrome often merits hospitalization, and in 10% of cases it can be fatal.1
The patient in this case was started on prednisone 60 mg/d and her OCPs were discontinued. One week later, a repeat CBC showed normalized levels of eosinophils and transaminases. However, shortly after a 3-week taper of the prednisone, her levels of eosinophils and transaminases rose again. A repeat prednisone taper finally led to complete resolution of rash and sustained normalization of eosinophil and transaminase levels.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
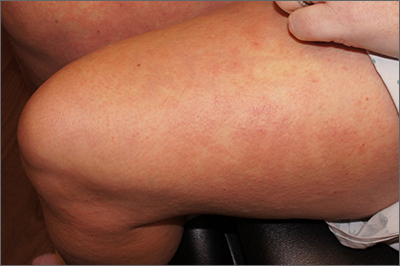
A punch biopsy revealed lichenoid interface dermatitis with eosinophils and mild spongiosis—consistent with, but not conclusive for, a drug eruption. A complete blood count (CBC) and comprehensive metabolic panel revealed elevated levels of eosinophils and transaminases which raised the possibility of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. In this patient’s case, the transaminitis suggested some mild hepatitis; the liver is the most common organ involved in DRESS.
Diagnostic criteria for DRESS syndrome need not always be met but can include fever, lymphadenopathy, facial edema, and a morbilliform rash presenting 2 to 3 weeks after drug exposure. In this case, a lack of fever, facial edema, and other systemic symptoms favored a less severe drug eruption or what has been described as mini-DRESS.1 DRESS syndrome often merits hospitalization, and in 10% of cases it can be fatal.1
The patient in this case was started on prednisone 60 mg/d and her OCPs were discontinued. One week later, a repeat CBC showed normalized levels of eosinophils and transaminases. However, shortly after a 3-week taper of the prednisone, her levels of eosinophils and transaminases rose again. A repeat prednisone taper finally led to complete resolution of rash and sustained normalization of eosinophil and transaminase levels.
Text courtesy of Jonathan Karnes, MD, medical director, MDFMR Dermatology Services, Augusta, ME. Photos courtesy of Jonathan Karnes, MD (copyright retained).
Isaacs M, Cardones AR, Rahnama-Moghadam S. DRESS syndrome: clinical myths and pearls. Cutis. 2018;102:322-326.
Isaacs M, Cardones AR, Rahnama-Moghadam S. DRESS syndrome: clinical myths and pearls. Cutis. 2018;102:322-326.