User login
• Use a validated breast cancer risk assessment tool for any woman with a suspicious family history, precancerous breast lesions, or reproductive risk factors. C
• Recommend a semi-annual clinical breast exam and an annual mammogram for women at high risk for invasive breast cancer. C
• Discuss chemoprevention with a selective estrogen-receptor modifier or aromatase inhibitor with women at high risk for breast cancer and low risk for adverse events. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Identifying patients at risk
Among the known risk factors for breast cancer, some are modifiable (use of oral contraceptives and alcohol consumption, for example); others, such as family history and age at which menopause occurs, are not (TABLE 1).4-7 Aging itself confers the greatest risk: The incidence of breast cancer comes close to doubling at each 10-year interval before menopause and continues to climb, but more slowly, thereafter.8,9
TABLE 1
Risk factors for breast cancer4-7
| Nonmodifiable | Age, atypical hyperplasia, chest wall radiation (between the ages of 10-30 y), early menarche, family history, late menopause, race, sex |
| Modifiable | Alcohol consumption, hormone therapy (for menopausal symptoms, oral contraceptives), obesity, parity (first child after age 35, nulliparity) |
Estrogen exposure: The risk is cumulative
A number of studies have linked early onset of menarche (<12 years of age) and late menopause (>55 years) to an increase in breast cancer risk. Nulliparity, or having a first child after age 35, is also associated with greater risk; oophorectomy prior to age 50 may reduce the risk by as much as 40%.4,5,10-13

The mammogram shows a malignancy in the superior portion of the breast (arrow). Oral contraceptive use is an additional risk, but the effect slowly diminishes in the 10 years after cessation.4,5 Postmenopausal hormone replacement therapy—specifically, oral conjugated equine estrogen and medroxyprogesterone acetate—was found by the Woman’s Health Initiative to increase breast cancer risk.6
Other nongenetic risk factors include:
Atypical findings on breast biopsy. Evidence of atypical ductal hyperplasia (ADH) or lobular hyperplasia (ALH) is associated with a 4-fold increase in risk.7
Environmental exposure. Radiation, especially to the chest wall (typically as a treatment for Hodgkin’s lymphoma) increases a woman’s risk for breast cancer, particularly if the exposure occurred when she was between the ages of 10 and 30.14
Lifestyle factors. Obesity, particularly in postmenopausal women, and alcohol consumption of more than a drink or two per day are both associated with an increased risk.4
Genetic mutations and breast cancer risk
An estimated 5% to 10% of breast cancers are inherited.5 Genetic susceptibility is generally transmitted as an autosomal dominant trait.
There are 2 known breast cancer genes, BRCA1 and BRCA2, located on the long arm of chromosomes 17 and 13, respectively. The genes themselves encode tumor suppressor proteins. Mutations in these genes impair the DNA repair process, resulting in increased risk.8
The chance of carrying a mutation in either BRCA1 or BRCA2 is estimated at one in 500 to 800 in women of Northern/Western European descent. Among Ashkenazi Jews, however, the frequency is about one in 50.5
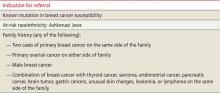
A thorough family history that takes into account both the number of affected relatives and their age at diagnosis (TABLE 2)8,15 is helpful in determining whether a patient is at low, high, or very high risk of carrying a genetic mutation. Women who have no first-degree relative with breast cancer—or a relative who was diagnosed with breast cancer after age 50—are at low risk, while those with at least one first-degree relative diagnosed with breast cancer before the age of 50 would be categorized as high risk.
A woman with a family history of early-onset breast or ovarian cancer or a relative who developed both breast and ovarian cancer, bilateral breast cancer, or male breast cancer would be classified as very high risk for a genetic mutation, as would a patient with 2 or more family members affected by breast or ovarian cancer.
Ashkenazi Jewish heritage and a relative who was diagnosed with ovarian or breast cancer indicate an increased likelihood of a BRCA mutation, as well.8 (Other genetic conditions, with mutations that are distinct from the BRCA genes, have also been linked to breast cancer, but occur less frequently.)
BRCA gene testing can confirm very high risk status, prompting the initiation of preventive measures and facilitating early detection. Such testing can also identify—and relieve the anxiety of—noncarriers in high-risk families. Recently published guidelines from the US Preventive Services Task Force (USPSTF) support testing in women with suspicious family histories with a grade B recommendation, indicating that there is at least fair evidence that testing improves important health outcomes and that the benefits of testing outweigh the harms.15
The downside of specific BRCA gene testing for patients who find that they do not have this genetic mutation may include a false sense of security and the failure to identify any other genetic mutations. Patients who learn that they do carry a BRCA gene mutation could face psychosocial or economic harm associated with aggressive surveillance and surgical intervention.5
TABLE 2
Genetic counseling for patients at high risk8,15
Tools can quantify 5-year, 10-year, and lifetime risk
A number of breast cancer risk assessment tools have been developed to help clinicians individualize patient care. None provides the basis for an all-encompassing approach to breast cancer risk or a comprehensive patient discussion of preventive strategies. We have found that, when used in combination, 2 or more predictive models can complement each other and guide the development of a targeted risk reduction approach.
When to use a predictive tool
It is not necessary to use a predictive model for patients at low risk for breast cancer. The tools detailed in TABLE 3 5,14,16-23 are better suited to women who have a suspicious family history, a history of precancerous breast lesions, or known reproductive risks. Although each model has limitations, it is important that you have a working knowledge of circumstances that favor one tool over another. For instance, the Gail model, the most widely used, can help determine if a particular patient is a candidate for chemoprevention.16-20 Others, such as the Tyrer-Cuzick model14,21,22 and the Claus model,14,23 are useful in deciding whether a patient is a candidate for breast magnetic resonance imaging (MRI) as an adjunct to mammography screening. Another useful tool is the BRCAPRO, which is used primarily by genetic counselors to assess the likelihood that a patient carries a BRCA1 or BRCA2 mutation and would benefit from genetic testing.4,5
TABLE 3
Breast cancer risk assessment tools: What you need to know5,14,16-23
| Tool | Intended use | Criteria considered | Results | Limitations | Validation | How to access |
|---|---|---|---|---|---|---|
| Gail model | Assess eligibility for chemoprevention in women >35 years | Reproductive history, history of breast biopsies, first-degree relatives with breast cancer | Estimates 5-year and lifetime risk for invasive breast cancer | Can overestimate risk in patients with previous biopsy and atypical hyperplasia results and family history | Validated in independent projects; widely used to define excess risk; modified model for minorities validated | Available at http://www.cancer.gov/bcrisktool/ |
| Tyrer-Cuzick* model | Assess need for breast MRI | Hormonal and reproductive history, history of breast biopsies, number and age of onset of first- and second-degree relatives with breast cancer | Estimates 10-year and lifetime risk for invasive breast cancer | Potential for significant overestimation of risk in patients with atypical hyperplasia findings on breast biopsy | Not validated | Go to http://www.ems-trials.org/riskevaluator Click on “software downloads” to select the appropriate version |
| Claus model | Assess need for breast MRI | Age of onset of first- and second-degree relatives with history of breast cancer | Estimates incremental 10-year and lifetime risk for invasive breast cancer | Looks only at family history, without considering hormonal or reproductive risk factors | Validation does not extend to minorities | Tables found in Cancer (1994;73:643-651) available at no charge from http://onlinelibrary.wiley.com/journal/10.1002/(ISSN)1097-0142/issues |
| BRCAPRO | Determine whether genetic testing is indicated | Family history of breast and ovarian cancer | Estimates likelihood of genetic mutation | Time-consuming; requires highly detailed family history | Validation does not extend to minorities | Not widely available; used primarily by genetic counselors |
| *Also known as the IBIS model. IBIS, International Breast Cancer Intervention Study; MRI, magnetic resonance imaging. | ||||||
Managing patients at all risk levels
Although patients with average, high, or very high risk will all be managed differently, evidence suggests that lifestyle modification as needed, imaging, and chemoprevention, in some cases, can reduce the likelihood of breast cancer for women at all levels of risk.24
For women with an average risk (a 5-year Gail model score ≤1.66% and no significant family history),19 a discussion of the benefits and risks, as well as the limitations, of annual screening mammography beginning at age 40 vs age 50 is in order. Several major organizations, the American College of Obstetricians and Gynecologists25 and American Cancer Society (ACS)16 among them, have guidelines that support annual mammography beginning at 40 years but do not specify at what age to discontinue screening. In contrast, the USPSTF26 recommends biennial mammography between the ages of 50 and 74 years (See “The mammography controvrsy: When should you screen?” J Fam Pract. 2011;60:524-531).
How to proceed? Talk to patients in the 40- to 50-year age range about the benefits and risks of earlier, more frequent screening vs waiting until 50 to start mammography and opting for screening every 2 years. Breast health awareness and the role of clinical breast exams also should be included in a balanced discussion of early detection of breast cancer. A review of the patient’s reproductive status and use of hormone preparations is appropriate, as well.4,5
Patients at high risk (a Gail model score >1.66%; a history of ADH, ALH, or lobular carcinoma in situ; or a family history of breast cancer)3 should be advised to have a clinical breast exam every 6 months and annual mammograms. High-risk patients should also be offered the option of chemoprevention with tamoxifen, raloxifene,27,28 or exemestane29 if the benefits of treatment outweigh the risk of potential adverse effects. The merits of MRI breast surveillance have not been defined for women with this level of risk.14
For very high-risk patients (those with a family history that strongly suggests a genetic predisposition, a confirmed gene mutation, evidence of hereditary breast and ovarian cancer, or a personal history of chest wall irradiation between the ages of 10 and 30 years), a discussion of more aggressive risk-reduction strategies is recommended.4 A clinical breast exam and mammogram should be performed beginning at age 25—or 5 to 10 years before the earliest age at which a first-degree relative was diagnosed.
Starting at age 30, patients at very high risk should undergo annual mammography and breast MRI, either simultaneously or staggered every 6 months, along with a twice-yearly clinical breast exam.14 Breast health awareness and lifestyle modification should be emphasized, and the benefits and risks of chemoprevention should be discussed. Surgical risk-reduction strategies, such as prophylactic mastectomy and oophorectomy, should also be discussed, along with the offer of a referral to a surgeon for consultation.5
What to tell patients about chemoprevention
The USPSTF has issued a grade B recommendation to a discussion of chemoprevention for women who are at high risk for breast cancer and low risk for an adverse event.30 Counseling a patient regarding the risks and benefits of chemoprevention will depend on her age, comorbidities, whether or not she has had a hysterectomy, and her willingness to take the suggested medication.
Selective estrogen receptor modulators (SERMs). The American Society of Clinical Oncology Clinical Practice Guideline Update has reviewed the benefits and potential adverse effects of the SERMs tamoxifen and raloxifene. The Society supports the use of tamoxifen in pre- and postmenopausal women for breast cancer risk reduction; it also supports the use of raloxifene for postmenopausal women, the only patient population for which raloxifene has been approved.27
In a review of 7 placebo-controlled, randomized clinical trials and one head-to-head trial, both drugs reduced the risk for invasive, estrogen receptor–positive breast cancer by about 40% compared with placebo. Breast cancer deaths, however, did not decrease.31
Both tamoxifen and raloxifene were found to increase bone mineral density and reduce fracture risk.31 Thromboembolic events—which occurred less frequently with raloxifene than tamoxifen—was the chief adverse effect, with an incidence of 0.4% to 0.7%. In addition, fewer cases of endometrial cancer were reported with raloxifene compared with tamoxifen, making raloxifene the preferred treatment for postmenopausal women with an intact uterus.31
The National Surgical Adjuvant Breast and Bowel Project STAR study—one of the trials included in the review—initially reported that tamoxifen and raloxifene were equivalent in reducing breast cancer risk in postmenopausal women at increased risk.28 In an updated analysis based on 81 months of use, however, tamoxifen resulted in a 50% reduction in the incidence of breast cancer vs a reduction of 38% for raloxifene.32
The greater reduction in breast cancer risk seen with tamoxifen comes at a potential cost. Tamoxifen was found to have a worse adverse effect profile, leading to a higher risk for endometrial hyperplasia and hysterectomy, as well as thromboembolic events. The difference in all-cause mortality, however, was not statistically significant.32
Aromatase inhibitor therapy. The National Cancer Institute of Canada recently published a major chemoprevention trial, evaluating the effectiveness of aromatase inhibition in breast cancer risk reduction.29 This randomized, double-blind trial of exemestane vs placebo included more than 4500 women with a median follow-up of 3 years, and found that the exemestane reduced the incidence of invasive breast cancer in postmenopausal women at moderate risk by 65% (hazard ratio=0.35; 95% confidence interval, 0.18-0.70; P=.002).29
IBIS-II, a multicenter study in the United Kingdom, randomly assigned 6000 women at increased risk for breast cancer to placebo or anastrozole, an alternative aromatase inhibitor. This trial is ongoing, and breast cancer incidence is the primary endpoint.33 Aromatase inhibitors have not been approved by the US Food and Drug Administration for breast cancer prevention.34
Imaging strategies for those at risk
Although there is evidence that mammography performed on postmenopausal women can reduce breast cancer mortality by 25%, there are known limitations to this detection method.14
One drawback is that in premenopausal women, breast density lowers mammography’s sensitivity. In addition, several studies have found that mammography has a low sensitivity for detecting tumors in patients with a BRCA mutation. This has led to the use of other imaging modalities, especially MRI, for women with a family history that suggests a genetic predisposition.
The first study to demonstrate the superior sensitivity of MRI for detecting invasive breast cancer compared with clinical breast exam and mammography was published in 2004.35 A few years later, the ACS issued guidelines that call for surveillance with MRI as an adjunct to mammography, starting at age 30, for women whose family history, carrier status, or history of chest wall radiation puts them at very high risk (ie, a lifetime risk >20%-25%).14
The ACS found insufficient evidence to recommend for or against breast MRI for women with a lifetime risk of 15% to 20% (or documented high-risk lesions such as lobular carcinoma in situ, ALH, or ADH). Mammographic density, which in itself is a strong risk factor for the development of breast cancer, was not determined to be an indication for MRI screening. In deciding whether MRI is indicated for any high-risk patient, the cost, quality of imaging, and lower specificity must be considered.14
Weighing the benefits of surgery
For women who have a strong family history of breast cancer or are known carriers of a BRCA1 or BRCA gene mutation, the already high risk of developing breast cancer increases as they age. Prophylactic surgery—risk-reduction mastectomy (RRM) and/or bilateral salpingo-oophorectomy (RRSO)—has been found to lower the risk.5,36,37
RRM can reduce the risk of breast cancer by as much as 90% for such patients;38,39 RRSO yields similar results, reducing the risk of ovarian cancer by 80% to 95% and the risk of breast cancer by 40% to 59%, provided the surgery is performed before the patient is 40 years old.36,37
These potential benefits must be weighed against the harm associated with surgically induced menopause, with the attendant risks of cardiovascular disease, osteoporosis, and menopausal symptoms.40 Notably, hormone therapy use after RRSO in women with a gene mutation has not been found to increase the risk of breast cancer. In fact, it may be associated with a decreased risk.5 In general, short-term use of low-dose estrogen—up to the age of 51 or 52 years—is considered to be safe for this population,41,42 but long-term data on breast cancer risk are lacking.
CORRESPONDENCE
Marcia G. Ko, MD, Mayo Clinic, 13737 North 92nd Street, Scottsdale, AZ 85369; [email protected]
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277-300.
2. Smith R. Risk-based screening for breast cancer: is there a practical strategy? Semin Breast Dis. 1999;2:280-291.
3. Guerra CE, Sherman M, Armstrong K. Diffusion of breast cancer risk assessment in primary care. J Am Board Fam Med. 2009;22:272-279.
4. Pruthi S, Brandt KR, Degnim AC, et al. A multidisciplinary approach to the management of breast cancer, part 1: prevention and diagnosis. Mayo Clin Proc. 2007;82:999-1012.
5. Pruthi S, Gostout BS, Lindor NM. Identification and management of women with BRCA mutations or hereditary predisposition for breast and ovarian cancer. Mayo Clin Proc. 2010;85:1111-1120.
6. Rossouw J, Anderson G, Prentice R, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
7. Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229-237.
8. Daly MB, Axilbund JE, Buys S, et al. Genetic/familial high-risk assessment: breast and ovarian. J Natl Compr Canc Netw. 2010;8:562-594.
9. McPherson K, Steel CM, Dixon JM. ABC of breast diseases. BMJ. 2000;321:624-628.
10. Brinton LA, Schairer C, Hoover RN, et al. Menstrual factors and risk of breast cancer. Cancer Invest. 1988;6:245-254.
11. Apter D, Reinilä M, Vihko R. Some endocrine characteristics of early menarche, a risk factor for breast cancer, are preserved into adulthood. Int J Cancer. 1989;44:783-787.
12. Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616-1622.
13. Narod SA, Brunet JS, Ghadirian P, et al. Tamoxifen and risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a case-control study. Lancet. 2000;356:1876-1881.
14. Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75-89.
15. U.S. Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility. Ann Intern Med. 2005;143:355-361.
16. Gail M, Benichou J. Validation studies on a model for breast cancer risk. J Natl Cancer Inst. 1994;86:573-575.
17. Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 2005;97:1652-1662.
18. Pankratz VS, Hartmann LC, Degnim AC, et al. Assessment of the accuracy of the Gail model in women with atypical hyperplasia. J Clin Oncol. 2008;26:5374-5379.
19. Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879-1886.
20. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696-706.
21. Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111-1130.
22. Boughey JC, Hartmann LC, Anderson SS, et al. Evaluation of the Tyrer-Cuzick (International Breast Cancer Intervention Study) model for breast cancer risk prediction in women with atypical hyperplasia. J Clin Oncol. 2010;28:3591-3596.
23. Claus EB, Risch N, Thompson W. Autosomal dominant inheritance of early-onset breast cancer. Cancer. 1994;73:643-651.
24. Cummings SR, Tice JA, Bauer S, et al. Prevention of breast cancer in postmenopausal women. J Natl Cancer Inst. 2009;101:384-398.
25. American College of Obstetricians-Gynecologists. Practice bulletin no. 122: Breast cancer screening. Obstet Gynecol. 2011;118(2 pt 1):372-382.
26. U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716-726.
27. Visvanathan K, Chlebowski R, Hurley P, et al. American Society of Clinical Oncology clinical practice guideline update on the use of pharmacologic interventions including tamoxifen, raloxifene, and aromatase inhibition for breast cancer risk reduction. J Clin Oncol. 2009;27:3235-3258.
28. Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727-2741.
29. Goss PE, Ingle JN, Alés-Martínez JE, et al. Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. 2011;364:2381-2391.
30. U.S. Preventive Services Task Force. Chemoprevention of breast cancer. Ann Intern Med. 2002;137:56-58.
31. Nelson HD, Fu R, Griffin JC, et al. Systematic review: comparative effectiveness of medications to reduce risk for primary breast cancer. Ann Intern Med. 2009;151:703-715.
32. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696-706.
33. Dunn BK, Ryan A. Phase 3 trials of aromatase inhibitors for breast cancer prevention. Ann N Y Acad Sci. 2009;1155:141-161.
34. National Cancer Institute. Hormone therapy for breast cancer. Reviewed April 11, 2012. Available at: http://www.cancer.gov/cancertopics/factsheet/Therapy/hormone-therapy-breast. Accessed May 18, 2012.
35. Kriege M, Brekelmans CTM, Boetes C, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351:427-437.
36. Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304:967-975.
37. Eisen A, Lubinski J, Klijn J, et al. Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2005;23:7491-7496.
38. Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:1055-1062.
39. Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340:77-84.
40. Shuster LT, Gostout BS, Grossardt BR, Rocca WA. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause Int. 2008;14:111-116.
41. Armstrong K, Schwartz JS, Randall T, et al. Hormone replacement therapy and life expectancy after prophylactic oophorectomy in women with BRCA1/2 mutations: a decision analysis. J Clin Oncol. 2004;22:1045-1054.
42. Eisen A, Lubinski J, Gronwald J, et al. Hormone therapy and the risk of breast cancer in BRCA1 mutation carriers. J Natl Cancer Inst. 2008;100:1361-1367.
;
• Use a validated breast cancer risk assessment tool for any woman with a suspicious family history, precancerous breast lesions, or reproductive risk factors. C
• Recommend a semi-annual clinical breast exam and an annual mammogram for women at high risk for invasive breast cancer. C
• Discuss chemoprevention with a selective estrogen-receptor modifier or aromatase inhibitor with women at high risk for breast cancer and low risk for adverse events. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Identifying patients at risk
Among the known risk factors for breast cancer, some are modifiable (use of oral contraceptives and alcohol consumption, for example); others, such as family history and age at which menopause occurs, are not (TABLE 1).4-7 Aging itself confers the greatest risk: The incidence of breast cancer comes close to doubling at each 10-year interval before menopause and continues to climb, but more slowly, thereafter.8,9
TABLE 1
Risk factors for breast cancer4-7
| Nonmodifiable | Age, atypical hyperplasia, chest wall radiation (between the ages of 10-30 y), early menarche, family history, late menopause, race, sex |
| Modifiable | Alcohol consumption, hormone therapy (for menopausal symptoms, oral contraceptives), obesity, parity (first child after age 35, nulliparity) |
Estrogen exposure: The risk is cumulative
A number of studies have linked early onset of menarche (<12 years of age) and late menopause (>55 years) to an increase in breast cancer risk. Nulliparity, or having a first child after age 35, is also associated with greater risk; oophorectomy prior to age 50 may reduce the risk by as much as 40%.4,5,10-13

The mammogram shows a malignancy in the superior portion of the breast (arrow). Oral contraceptive use is an additional risk, but the effect slowly diminishes in the 10 years after cessation.4,5 Postmenopausal hormone replacement therapy—specifically, oral conjugated equine estrogen and medroxyprogesterone acetate—was found by the Woman’s Health Initiative to increase breast cancer risk.6
Other nongenetic risk factors include:
Atypical findings on breast biopsy. Evidence of atypical ductal hyperplasia (ADH) or lobular hyperplasia (ALH) is associated with a 4-fold increase in risk.7
Environmental exposure. Radiation, especially to the chest wall (typically as a treatment for Hodgkin’s lymphoma) increases a woman’s risk for breast cancer, particularly if the exposure occurred when she was between the ages of 10 and 30.14
Lifestyle factors. Obesity, particularly in postmenopausal women, and alcohol consumption of more than a drink or two per day are both associated with an increased risk.4
Genetic mutations and breast cancer risk
An estimated 5% to 10% of breast cancers are inherited.5 Genetic susceptibility is generally transmitted as an autosomal dominant trait.
There are 2 known breast cancer genes, BRCA1 and BRCA2, located on the long arm of chromosomes 17 and 13, respectively. The genes themselves encode tumor suppressor proteins. Mutations in these genes impair the DNA repair process, resulting in increased risk.8
The chance of carrying a mutation in either BRCA1 or BRCA2 is estimated at one in 500 to 800 in women of Northern/Western European descent. Among Ashkenazi Jews, however, the frequency is about one in 50.5
A thorough family history that takes into account both the number of affected relatives and their age at diagnosis (TABLE 2)8,15 is helpful in determining whether a patient is at low, high, or very high risk of carrying a genetic mutation. Women who have no first-degree relative with breast cancer—or a relative who was diagnosed with breast cancer after age 50—are at low risk, while those with at least one first-degree relative diagnosed with breast cancer before the age of 50 would be categorized as high risk.
A woman with a family history of early-onset breast or ovarian cancer or a relative who developed both breast and ovarian cancer, bilateral breast cancer, or male breast cancer would be classified as very high risk for a genetic mutation, as would a patient with 2 or more family members affected by breast or ovarian cancer.
Ashkenazi Jewish heritage and a relative who was diagnosed with ovarian or breast cancer indicate an increased likelihood of a BRCA mutation, as well.8 (Other genetic conditions, with mutations that are distinct from the BRCA genes, have also been linked to breast cancer, but occur less frequently.)
BRCA gene testing can confirm very high risk status, prompting the initiation of preventive measures and facilitating early detection. Such testing can also identify—and relieve the anxiety of—noncarriers in high-risk families. Recently published guidelines from the US Preventive Services Task Force (USPSTF) support testing in women with suspicious family histories with a grade B recommendation, indicating that there is at least fair evidence that testing improves important health outcomes and that the benefits of testing outweigh the harms.15
The downside of specific BRCA gene testing for patients who find that they do not have this genetic mutation may include a false sense of security and the failure to identify any other genetic mutations. Patients who learn that they do carry a BRCA gene mutation could face psychosocial or economic harm associated with aggressive surveillance and surgical intervention.5
TABLE 2
Genetic counseling for patients at high risk8,15
Tools can quantify 5-year, 10-year, and lifetime risk
A number of breast cancer risk assessment tools have been developed to help clinicians individualize patient care. None provides the basis for an all-encompassing approach to breast cancer risk or a comprehensive patient discussion of preventive strategies. We have found that, when used in combination, 2 or more predictive models can complement each other and guide the development of a targeted risk reduction approach.
When to use a predictive tool
It is not necessary to use a predictive model for patients at low risk for breast cancer. The tools detailed in TABLE 3 5,14,16-23 are better suited to women who have a suspicious family history, a history of precancerous breast lesions, or known reproductive risks. Although each model has limitations, it is important that you have a working knowledge of circumstances that favor one tool over another. For instance, the Gail model, the most widely used, can help determine if a particular patient is a candidate for chemoprevention.16-20 Others, such as the Tyrer-Cuzick model14,21,22 and the Claus model,14,23 are useful in deciding whether a patient is a candidate for breast magnetic resonance imaging (MRI) as an adjunct to mammography screening. Another useful tool is the BRCAPRO, which is used primarily by genetic counselors to assess the likelihood that a patient carries a BRCA1 or BRCA2 mutation and would benefit from genetic testing.4,5
TABLE 3
Breast cancer risk assessment tools: What you need to know5,14,16-23
| Tool | Intended use | Criteria considered | Results | Limitations | Validation | How to access |
|---|---|---|---|---|---|---|
| Gail model | Assess eligibility for chemoprevention in women >35 years | Reproductive history, history of breast biopsies, first-degree relatives with breast cancer | Estimates 5-year and lifetime risk for invasive breast cancer | Can overestimate risk in patients with previous biopsy and atypical hyperplasia results and family history | Validated in independent projects; widely used to define excess risk; modified model for minorities validated | Available at http://www.cancer.gov/bcrisktool/ |
| Tyrer-Cuzick* model | Assess need for breast MRI | Hormonal and reproductive history, history of breast biopsies, number and age of onset of first- and second-degree relatives with breast cancer | Estimates 10-year and lifetime risk for invasive breast cancer | Potential for significant overestimation of risk in patients with atypical hyperplasia findings on breast biopsy | Not validated | Go to http://www.ems-trials.org/riskevaluator Click on “software downloads” to select the appropriate version |
| Claus model | Assess need for breast MRI | Age of onset of first- and second-degree relatives with history of breast cancer | Estimates incremental 10-year and lifetime risk for invasive breast cancer | Looks only at family history, without considering hormonal or reproductive risk factors | Validation does not extend to minorities | Tables found in Cancer (1994;73:643-651) available at no charge from http://onlinelibrary.wiley.com/journal/10.1002/(ISSN)1097-0142/issues |
| BRCAPRO | Determine whether genetic testing is indicated | Family history of breast and ovarian cancer | Estimates likelihood of genetic mutation | Time-consuming; requires highly detailed family history | Validation does not extend to minorities | Not widely available; used primarily by genetic counselors |
| *Also known as the IBIS model. IBIS, International Breast Cancer Intervention Study; MRI, magnetic resonance imaging. | ||||||
Managing patients at all risk levels
Although patients with average, high, or very high risk will all be managed differently, evidence suggests that lifestyle modification as needed, imaging, and chemoprevention, in some cases, can reduce the likelihood of breast cancer for women at all levels of risk.24
For women with an average risk (a 5-year Gail model score ≤1.66% and no significant family history),19 a discussion of the benefits and risks, as well as the limitations, of annual screening mammography beginning at age 40 vs age 50 is in order. Several major organizations, the American College of Obstetricians and Gynecologists25 and American Cancer Society (ACS)16 among them, have guidelines that support annual mammography beginning at 40 years but do not specify at what age to discontinue screening. In contrast, the USPSTF26 recommends biennial mammography between the ages of 50 and 74 years (See “The mammography controvrsy: When should you screen?” J Fam Pract. 2011;60:524-531).
How to proceed? Talk to patients in the 40- to 50-year age range about the benefits and risks of earlier, more frequent screening vs waiting until 50 to start mammography and opting for screening every 2 years. Breast health awareness and the role of clinical breast exams also should be included in a balanced discussion of early detection of breast cancer. A review of the patient’s reproductive status and use of hormone preparations is appropriate, as well.4,5
Patients at high risk (a Gail model score >1.66%; a history of ADH, ALH, or lobular carcinoma in situ; or a family history of breast cancer)3 should be advised to have a clinical breast exam every 6 months and annual mammograms. High-risk patients should also be offered the option of chemoprevention with tamoxifen, raloxifene,27,28 or exemestane29 if the benefits of treatment outweigh the risk of potential adverse effects. The merits of MRI breast surveillance have not been defined for women with this level of risk.14
For very high-risk patients (those with a family history that strongly suggests a genetic predisposition, a confirmed gene mutation, evidence of hereditary breast and ovarian cancer, or a personal history of chest wall irradiation between the ages of 10 and 30 years), a discussion of more aggressive risk-reduction strategies is recommended.4 A clinical breast exam and mammogram should be performed beginning at age 25—or 5 to 10 years before the earliest age at which a first-degree relative was diagnosed.
Starting at age 30, patients at very high risk should undergo annual mammography and breast MRI, either simultaneously or staggered every 6 months, along with a twice-yearly clinical breast exam.14 Breast health awareness and lifestyle modification should be emphasized, and the benefits and risks of chemoprevention should be discussed. Surgical risk-reduction strategies, such as prophylactic mastectomy and oophorectomy, should also be discussed, along with the offer of a referral to a surgeon for consultation.5
What to tell patients about chemoprevention
The USPSTF has issued a grade B recommendation to a discussion of chemoprevention for women who are at high risk for breast cancer and low risk for an adverse event.30 Counseling a patient regarding the risks and benefits of chemoprevention will depend on her age, comorbidities, whether or not she has had a hysterectomy, and her willingness to take the suggested medication.
Selective estrogen receptor modulators (SERMs). The American Society of Clinical Oncology Clinical Practice Guideline Update has reviewed the benefits and potential adverse effects of the SERMs tamoxifen and raloxifene. The Society supports the use of tamoxifen in pre- and postmenopausal women for breast cancer risk reduction; it also supports the use of raloxifene for postmenopausal women, the only patient population for which raloxifene has been approved.27
In a review of 7 placebo-controlled, randomized clinical trials and one head-to-head trial, both drugs reduced the risk for invasive, estrogen receptor–positive breast cancer by about 40% compared with placebo. Breast cancer deaths, however, did not decrease.31
Both tamoxifen and raloxifene were found to increase bone mineral density and reduce fracture risk.31 Thromboembolic events—which occurred less frequently with raloxifene than tamoxifen—was the chief adverse effect, with an incidence of 0.4% to 0.7%. In addition, fewer cases of endometrial cancer were reported with raloxifene compared with tamoxifen, making raloxifene the preferred treatment for postmenopausal women with an intact uterus.31
The National Surgical Adjuvant Breast and Bowel Project STAR study—one of the trials included in the review—initially reported that tamoxifen and raloxifene were equivalent in reducing breast cancer risk in postmenopausal women at increased risk.28 In an updated analysis based on 81 months of use, however, tamoxifen resulted in a 50% reduction in the incidence of breast cancer vs a reduction of 38% for raloxifene.32
The greater reduction in breast cancer risk seen with tamoxifen comes at a potential cost. Tamoxifen was found to have a worse adverse effect profile, leading to a higher risk for endometrial hyperplasia and hysterectomy, as well as thromboembolic events. The difference in all-cause mortality, however, was not statistically significant.32
Aromatase inhibitor therapy. The National Cancer Institute of Canada recently published a major chemoprevention trial, evaluating the effectiveness of aromatase inhibition in breast cancer risk reduction.29 This randomized, double-blind trial of exemestane vs placebo included more than 4500 women with a median follow-up of 3 years, and found that the exemestane reduced the incidence of invasive breast cancer in postmenopausal women at moderate risk by 65% (hazard ratio=0.35; 95% confidence interval, 0.18-0.70; P=.002).29
IBIS-II, a multicenter study in the United Kingdom, randomly assigned 6000 women at increased risk for breast cancer to placebo or anastrozole, an alternative aromatase inhibitor. This trial is ongoing, and breast cancer incidence is the primary endpoint.33 Aromatase inhibitors have not been approved by the US Food and Drug Administration for breast cancer prevention.34
Imaging strategies for those at risk
Although there is evidence that mammography performed on postmenopausal women can reduce breast cancer mortality by 25%, there are known limitations to this detection method.14
One drawback is that in premenopausal women, breast density lowers mammography’s sensitivity. In addition, several studies have found that mammography has a low sensitivity for detecting tumors in patients with a BRCA mutation. This has led to the use of other imaging modalities, especially MRI, for women with a family history that suggests a genetic predisposition.
The first study to demonstrate the superior sensitivity of MRI for detecting invasive breast cancer compared with clinical breast exam and mammography was published in 2004.35 A few years later, the ACS issued guidelines that call for surveillance with MRI as an adjunct to mammography, starting at age 30, for women whose family history, carrier status, or history of chest wall radiation puts them at very high risk (ie, a lifetime risk >20%-25%).14
The ACS found insufficient evidence to recommend for or against breast MRI for women with a lifetime risk of 15% to 20% (or documented high-risk lesions such as lobular carcinoma in situ, ALH, or ADH). Mammographic density, which in itself is a strong risk factor for the development of breast cancer, was not determined to be an indication for MRI screening. In deciding whether MRI is indicated for any high-risk patient, the cost, quality of imaging, and lower specificity must be considered.14
Weighing the benefits of surgery
For women who have a strong family history of breast cancer or are known carriers of a BRCA1 or BRCA gene mutation, the already high risk of developing breast cancer increases as they age. Prophylactic surgery—risk-reduction mastectomy (RRM) and/or bilateral salpingo-oophorectomy (RRSO)—has been found to lower the risk.5,36,37
RRM can reduce the risk of breast cancer by as much as 90% for such patients;38,39 RRSO yields similar results, reducing the risk of ovarian cancer by 80% to 95% and the risk of breast cancer by 40% to 59%, provided the surgery is performed before the patient is 40 years old.36,37
These potential benefits must be weighed against the harm associated with surgically induced menopause, with the attendant risks of cardiovascular disease, osteoporosis, and menopausal symptoms.40 Notably, hormone therapy use after RRSO in women with a gene mutation has not been found to increase the risk of breast cancer. In fact, it may be associated with a decreased risk.5 In general, short-term use of low-dose estrogen—up to the age of 51 or 52 years—is considered to be safe for this population,41,42 but long-term data on breast cancer risk are lacking.
CORRESPONDENCE
Marcia G. Ko, MD, Mayo Clinic, 13737 North 92nd Street, Scottsdale, AZ 85369; [email protected]
• Use a validated breast cancer risk assessment tool for any woman with a suspicious family history, precancerous breast lesions, or reproductive risk factors. C
• Recommend a semi-annual clinical breast exam and an annual mammogram for women at high risk for invasive breast cancer. C
• Discuss chemoprevention with a selective estrogen-receptor modifier or aromatase inhibitor with women at high risk for breast cancer and low risk for adverse events. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Identifying patients at risk
Among the known risk factors for breast cancer, some are modifiable (use of oral contraceptives and alcohol consumption, for example); others, such as family history and age at which menopause occurs, are not (TABLE 1).4-7 Aging itself confers the greatest risk: The incidence of breast cancer comes close to doubling at each 10-year interval before menopause and continues to climb, but more slowly, thereafter.8,9
TABLE 1
Risk factors for breast cancer4-7
| Nonmodifiable | Age, atypical hyperplasia, chest wall radiation (between the ages of 10-30 y), early menarche, family history, late menopause, race, sex |
| Modifiable | Alcohol consumption, hormone therapy (for menopausal symptoms, oral contraceptives), obesity, parity (first child after age 35, nulliparity) |
Estrogen exposure: The risk is cumulative
A number of studies have linked early onset of menarche (<12 years of age) and late menopause (>55 years) to an increase in breast cancer risk. Nulliparity, or having a first child after age 35, is also associated with greater risk; oophorectomy prior to age 50 may reduce the risk by as much as 40%.4,5,10-13

The mammogram shows a malignancy in the superior portion of the breast (arrow). Oral contraceptive use is an additional risk, but the effect slowly diminishes in the 10 years after cessation.4,5 Postmenopausal hormone replacement therapy—specifically, oral conjugated equine estrogen and medroxyprogesterone acetate—was found by the Woman’s Health Initiative to increase breast cancer risk.6
Other nongenetic risk factors include:
Atypical findings on breast biopsy. Evidence of atypical ductal hyperplasia (ADH) or lobular hyperplasia (ALH) is associated with a 4-fold increase in risk.7
Environmental exposure. Radiation, especially to the chest wall (typically as a treatment for Hodgkin’s lymphoma) increases a woman’s risk for breast cancer, particularly if the exposure occurred when she was between the ages of 10 and 30.14
Lifestyle factors. Obesity, particularly in postmenopausal women, and alcohol consumption of more than a drink or two per day are both associated with an increased risk.4
Genetic mutations and breast cancer risk
An estimated 5% to 10% of breast cancers are inherited.5 Genetic susceptibility is generally transmitted as an autosomal dominant trait.
There are 2 known breast cancer genes, BRCA1 and BRCA2, located on the long arm of chromosomes 17 and 13, respectively. The genes themselves encode tumor suppressor proteins. Mutations in these genes impair the DNA repair process, resulting in increased risk.8
The chance of carrying a mutation in either BRCA1 or BRCA2 is estimated at one in 500 to 800 in women of Northern/Western European descent. Among Ashkenazi Jews, however, the frequency is about one in 50.5
A thorough family history that takes into account both the number of affected relatives and their age at diagnosis (TABLE 2)8,15 is helpful in determining whether a patient is at low, high, or very high risk of carrying a genetic mutation. Women who have no first-degree relative with breast cancer—or a relative who was diagnosed with breast cancer after age 50—are at low risk, while those with at least one first-degree relative diagnosed with breast cancer before the age of 50 would be categorized as high risk.
A woman with a family history of early-onset breast or ovarian cancer or a relative who developed both breast and ovarian cancer, bilateral breast cancer, or male breast cancer would be classified as very high risk for a genetic mutation, as would a patient with 2 or more family members affected by breast or ovarian cancer.
Ashkenazi Jewish heritage and a relative who was diagnosed with ovarian or breast cancer indicate an increased likelihood of a BRCA mutation, as well.8 (Other genetic conditions, with mutations that are distinct from the BRCA genes, have also been linked to breast cancer, but occur less frequently.)
BRCA gene testing can confirm very high risk status, prompting the initiation of preventive measures and facilitating early detection. Such testing can also identify—and relieve the anxiety of—noncarriers in high-risk families. Recently published guidelines from the US Preventive Services Task Force (USPSTF) support testing in women with suspicious family histories with a grade B recommendation, indicating that there is at least fair evidence that testing improves important health outcomes and that the benefits of testing outweigh the harms.15
The downside of specific BRCA gene testing for patients who find that they do not have this genetic mutation may include a false sense of security and the failure to identify any other genetic mutations. Patients who learn that they do carry a BRCA gene mutation could face psychosocial or economic harm associated with aggressive surveillance and surgical intervention.5
TABLE 2
Genetic counseling for patients at high risk8,15
Tools can quantify 5-year, 10-year, and lifetime risk
A number of breast cancer risk assessment tools have been developed to help clinicians individualize patient care. None provides the basis for an all-encompassing approach to breast cancer risk or a comprehensive patient discussion of preventive strategies. We have found that, when used in combination, 2 or more predictive models can complement each other and guide the development of a targeted risk reduction approach.
When to use a predictive tool
It is not necessary to use a predictive model for patients at low risk for breast cancer. The tools detailed in TABLE 3 5,14,16-23 are better suited to women who have a suspicious family history, a history of precancerous breast lesions, or known reproductive risks. Although each model has limitations, it is important that you have a working knowledge of circumstances that favor one tool over another. For instance, the Gail model, the most widely used, can help determine if a particular patient is a candidate for chemoprevention.16-20 Others, such as the Tyrer-Cuzick model14,21,22 and the Claus model,14,23 are useful in deciding whether a patient is a candidate for breast magnetic resonance imaging (MRI) as an adjunct to mammography screening. Another useful tool is the BRCAPRO, which is used primarily by genetic counselors to assess the likelihood that a patient carries a BRCA1 or BRCA2 mutation and would benefit from genetic testing.4,5
TABLE 3
Breast cancer risk assessment tools: What you need to know5,14,16-23
| Tool | Intended use | Criteria considered | Results | Limitations | Validation | How to access |
|---|---|---|---|---|---|---|
| Gail model | Assess eligibility for chemoprevention in women >35 years | Reproductive history, history of breast biopsies, first-degree relatives with breast cancer | Estimates 5-year and lifetime risk for invasive breast cancer | Can overestimate risk in patients with previous biopsy and atypical hyperplasia results and family history | Validated in independent projects; widely used to define excess risk; modified model for minorities validated | Available at http://www.cancer.gov/bcrisktool/ |
| Tyrer-Cuzick* model | Assess need for breast MRI | Hormonal and reproductive history, history of breast biopsies, number and age of onset of first- and second-degree relatives with breast cancer | Estimates 10-year and lifetime risk for invasive breast cancer | Potential for significant overestimation of risk in patients with atypical hyperplasia findings on breast biopsy | Not validated | Go to http://www.ems-trials.org/riskevaluator Click on “software downloads” to select the appropriate version |
| Claus model | Assess need for breast MRI | Age of onset of first- and second-degree relatives with history of breast cancer | Estimates incremental 10-year and lifetime risk for invasive breast cancer | Looks only at family history, without considering hormonal or reproductive risk factors | Validation does not extend to minorities | Tables found in Cancer (1994;73:643-651) available at no charge from http://onlinelibrary.wiley.com/journal/10.1002/(ISSN)1097-0142/issues |
| BRCAPRO | Determine whether genetic testing is indicated | Family history of breast and ovarian cancer | Estimates likelihood of genetic mutation | Time-consuming; requires highly detailed family history | Validation does not extend to minorities | Not widely available; used primarily by genetic counselors |
| *Also known as the IBIS model. IBIS, International Breast Cancer Intervention Study; MRI, magnetic resonance imaging. | ||||||
Managing patients at all risk levels
Although patients with average, high, or very high risk will all be managed differently, evidence suggests that lifestyle modification as needed, imaging, and chemoprevention, in some cases, can reduce the likelihood of breast cancer for women at all levels of risk.24
For women with an average risk (a 5-year Gail model score ≤1.66% and no significant family history),19 a discussion of the benefits and risks, as well as the limitations, of annual screening mammography beginning at age 40 vs age 50 is in order. Several major organizations, the American College of Obstetricians and Gynecologists25 and American Cancer Society (ACS)16 among them, have guidelines that support annual mammography beginning at 40 years but do not specify at what age to discontinue screening. In contrast, the USPSTF26 recommends biennial mammography between the ages of 50 and 74 years (See “The mammography controvrsy: When should you screen?” J Fam Pract. 2011;60:524-531).
How to proceed? Talk to patients in the 40- to 50-year age range about the benefits and risks of earlier, more frequent screening vs waiting until 50 to start mammography and opting for screening every 2 years. Breast health awareness and the role of clinical breast exams also should be included in a balanced discussion of early detection of breast cancer. A review of the patient’s reproductive status and use of hormone preparations is appropriate, as well.4,5
Patients at high risk (a Gail model score >1.66%; a history of ADH, ALH, or lobular carcinoma in situ; or a family history of breast cancer)3 should be advised to have a clinical breast exam every 6 months and annual mammograms. High-risk patients should also be offered the option of chemoprevention with tamoxifen, raloxifene,27,28 or exemestane29 if the benefits of treatment outweigh the risk of potential adverse effects. The merits of MRI breast surveillance have not been defined for women with this level of risk.14
For very high-risk patients (those with a family history that strongly suggests a genetic predisposition, a confirmed gene mutation, evidence of hereditary breast and ovarian cancer, or a personal history of chest wall irradiation between the ages of 10 and 30 years), a discussion of more aggressive risk-reduction strategies is recommended.4 A clinical breast exam and mammogram should be performed beginning at age 25—or 5 to 10 years before the earliest age at which a first-degree relative was diagnosed.
Starting at age 30, patients at very high risk should undergo annual mammography and breast MRI, either simultaneously or staggered every 6 months, along with a twice-yearly clinical breast exam.14 Breast health awareness and lifestyle modification should be emphasized, and the benefits and risks of chemoprevention should be discussed. Surgical risk-reduction strategies, such as prophylactic mastectomy and oophorectomy, should also be discussed, along with the offer of a referral to a surgeon for consultation.5
What to tell patients about chemoprevention
The USPSTF has issued a grade B recommendation to a discussion of chemoprevention for women who are at high risk for breast cancer and low risk for an adverse event.30 Counseling a patient regarding the risks and benefits of chemoprevention will depend on her age, comorbidities, whether or not she has had a hysterectomy, and her willingness to take the suggested medication.
Selective estrogen receptor modulators (SERMs). The American Society of Clinical Oncology Clinical Practice Guideline Update has reviewed the benefits and potential adverse effects of the SERMs tamoxifen and raloxifene. The Society supports the use of tamoxifen in pre- and postmenopausal women for breast cancer risk reduction; it also supports the use of raloxifene for postmenopausal women, the only patient population for which raloxifene has been approved.27
In a review of 7 placebo-controlled, randomized clinical trials and one head-to-head trial, both drugs reduced the risk for invasive, estrogen receptor–positive breast cancer by about 40% compared with placebo. Breast cancer deaths, however, did not decrease.31
Both tamoxifen and raloxifene were found to increase bone mineral density and reduce fracture risk.31 Thromboembolic events—which occurred less frequently with raloxifene than tamoxifen—was the chief adverse effect, with an incidence of 0.4% to 0.7%. In addition, fewer cases of endometrial cancer were reported with raloxifene compared with tamoxifen, making raloxifene the preferred treatment for postmenopausal women with an intact uterus.31
The National Surgical Adjuvant Breast and Bowel Project STAR study—one of the trials included in the review—initially reported that tamoxifen and raloxifene were equivalent in reducing breast cancer risk in postmenopausal women at increased risk.28 In an updated analysis based on 81 months of use, however, tamoxifen resulted in a 50% reduction in the incidence of breast cancer vs a reduction of 38% for raloxifene.32
The greater reduction in breast cancer risk seen with tamoxifen comes at a potential cost. Tamoxifen was found to have a worse adverse effect profile, leading to a higher risk for endometrial hyperplasia and hysterectomy, as well as thromboembolic events. The difference in all-cause mortality, however, was not statistically significant.32
Aromatase inhibitor therapy. The National Cancer Institute of Canada recently published a major chemoprevention trial, evaluating the effectiveness of aromatase inhibition in breast cancer risk reduction.29 This randomized, double-blind trial of exemestane vs placebo included more than 4500 women with a median follow-up of 3 years, and found that the exemestane reduced the incidence of invasive breast cancer in postmenopausal women at moderate risk by 65% (hazard ratio=0.35; 95% confidence interval, 0.18-0.70; P=.002).29
IBIS-II, a multicenter study in the United Kingdom, randomly assigned 6000 women at increased risk for breast cancer to placebo or anastrozole, an alternative aromatase inhibitor. This trial is ongoing, and breast cancer incidence is the primary endpoint.33 Aromatase inhibitors have not been approved by the US Food and Drug Administration for breast cancer prevention.34
Imaging strategies for those at risk
Although there is evidence that mammography performed on postmenopausal women can reduce breast cancer mortality by 25%, there are known limitations to this detection method.14
One drawback is that in premenopausal women, breast density lowers mammography’s sensitivity. In addition, several studies have found that mammography has a low sensitivity for detecting tumors in patients with a BRCA mutation. This has led to the use of other imaging modalities, especially MRI, for women with a family history that suggests a genetic predisposition.
The first study to demonstrate the superior sensitivity of MRI for detecting invasive breast cancer compared with clinical breast exam and mammography was published in 2004.35 A few years later, the ACS issued guidelines that call for surveillance with MRI as an adjunct to mammography, starting at age 30, for women whose family history, carrier status, or history of chest wall radiation puts them at very high risk (ie, a lifetime risk >20%-25%).14
The ACS found insufficient evidence to recommend for or against breast MRI for women with a lifetime risk of 15% to 20% (or documented high-risk lesions such as lobular carcinoma in situ, ALH, or ADH). Mammographic density, which in itself is a strong risk factor for the development of breast cancer, was not determined to be an indication for MRI screening. In deciding whether MRI is indicated for any high-risk patient, the cost, quality of imaging, and lower specificity must be considered.14
Weighing the benefits of surgery
For women who have a strong family history of breast cancer or are known carriers of a BRCA1 or BRCA gene mutation, the already high risk of developing breast cancer increases as they age. Prophylactic surgery—risk-reduction mastectomy (RRM) and/or bilateral salpingo-oophorectomy (RRSO)—has been found to lower the risk.5,36,37
RRM can reduce the risk of breast cancer by as much as 90% for such patients;38,39 RRSO yields similar results, reducing the risk of ovarian cancer by 80% to 95% and the risk of breast cancer by 40% to 59%, provided the surgery is performed before the patient is 40 years old.36,37
These potential benefits must be weighed against the harm associated with surgically induced menopause, with the attendant risks of cardiovascular disease, osteoporosis, and menopausal symptoms.40 Notably, hormone therapy use after RRSO in women with a gene mutation has not been found to increase the risk of breast cancer. In fact, it may be associated with a decreased risk.5 In general, short-term use of low-dose estrogen—up to the age of 51 or 52 years—is considered to be safe for this population,41,42 but long-term data on breast cancer risk are lacking.
CORRESPONDENCE
Marcia G. Ko, MD, Mayo Clinic, 13737 North 92nd Street, Scottsdale, AZ 85369; [email protected]
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277-300.
2. Smith R. Risk-based screening for breast cancer: is there a practical strategy? Semin Breast Dis. 1999;2:280-291.
3. Guerra CE, Sherman M, Armstrong K. Diffusion of breast cancer risk assessment in primary care. J Am Board Fam Med. 2009;22:272-279.
4. Pruthi S, Brandt KR, Degnim AC, et al. A multidisciplinary approach to the management of breast cancer, part 1: prevention and diagnosis. Mayo Clin Proc. 2007;82:999-1012.
5. Pruthi S, Gostout BS, Lindor NM. Identification and management of women with BRCA mutations or hereditary predisposition for breast and ovarian cancer. Mayo Clin Proc. 2010;85:1111-1120.
6. Rossouw J, Anderson G, Prentice R, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
7. Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229-237.
8. Daly MB, Axilbund JE, Buys S, et al. Genetic/familial high-risk assessment: breast and ovarian. J Natl Compr Canc Netw. 2010;8:562-594.
9. McPherson K, Steel CM, Dixon JM. ABC of breast diseases. BMJ. 2000;321:624-628.
10. Brinton LA, Schairer C, Hoover RN, et al. Menstrual factors and risk of breast cancer. Cancer Invest. 1988;6:245-254.
11. Apter D, Reinilä M, Vihko R. Some endocrine characteristics of early menarche, a risk factor for breast cancer, are preserved into adulthood. Int J Cancer. 1989;44:783-787.
12. Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616-1622.
13. Narod SA, Brunet JS, Ghadirian P, et al. Tamoxifen and risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a case-control study. Lancet. 2000;356:1876-1881.
14. Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75-89.
15. U.S. Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility. Ann Intern Med. 2005;143:355-361.
16. Gail M, Benichou J. Validation studies on a model for breast cancer risk. J Natl Cancer Inst. 1994;86:573-575.
17. Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 2005;97:1652-1662.
18. Pankratz VS, Hartmann LC, Degnim AC, et al. Assessment of the accuracy of the Gail model in women with atypical hyperplasia. J Clin Oncol. 2008;26:5374-5379.
19. Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879-1886.
20. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696-706.
21. Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111-1130.
22. Boughey JC, Hartmann LC, Anderson SS, et al. Evaluation of the Tyrer-Cuzick (International Breast Cancer Intervention Study) model for breast cancer risk prediction in women with atypical hyperplasia. J Clin Oncol. 2010;28:3591-3596.
23. Claus EB, Risch N, Thompson W. Autosomal dominant inheritance of early-onset breast cancer. Cancer. 1994;73:643-651.
24. Cummings SR, Tice JA, Bauer S, et al. Prevention of breast cancer in postmenopausal women. J Natl Cancer Inst. 2009;101:384-398.
25. American College of Obstetricians-Gynecologists. Practice bulletin no. 122: Breast cancer screening. Obstet Gynecol. 2011;118(2 pt 1):372-382.
26. U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716-726.
27. Visvanathan K, Chlebowski R, Hurley P, et al. American Society of Clinical Oncology clinical practice guideline update on the use of pharmacologic interventions including tamoxifen, raloxifene, and aromatase inhibition for breast cancer risk reduction. J Clin Oncol. 2009;27:3235-3258.
28. Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727-2741.
29. Goss PE, Ingle JN, Alés-Martínez JE, et al. Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. 2011;364:2381-2391.
30. U.S. Preventive Services Task Force. Chemoprevention of breast cancer. Ann Intern Med. 2002;137:56-58.
31. Nelson HD, Fu R, Griffin JC, et al. Systematic review: comparative effectiveness of medications to reduce risk for primary breast cancer. Ann Intern Med. 2009;151:703-715.
32. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696-706.
33. Dunn BK, Ryan A. Phase 3 trials of aromatase inhibitors for breast cancer prevention. Ann N Y Acad Sci. 2009;1155:141-161.
34. National Cancer Institute. Hormone therapy for breast cancer. Reviewed April 11, 2012. Available at: http://www.cancer.gov/cancertopics/factsheet/Therapy/hormone-therapy-breast. Accessed May 18, 2012.
35. Kriege M, Brekelmans CTM, Boetes C, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351:427-437.
36. Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304:967-975.
37. Eisen A, Lubinski J, Klijn J, et al. Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2005;23:7491-7496.
38. Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:1055-1062.
39. Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340:77-84.
40. Shuster LT, Gostout BS, Grossardt BR, Rocca WA. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause Int. 2008;14:111-116.
41. Armstrong K, Schwartz JS, Randall T, et al. Hormone replacement therapy and life expectancy after prophylactic oophorectomy in women with BRCA1/2 mutations: a decision analysis. J Clin Oncol. 2004;22:1045-1054.
42. Eisen A, Lubinski J, Gronwald J, et al. Hormone therapy and the risk of breast cancer in BRCA1 mutation carriers. J Natl Cancer Inst. 2008;100:1361-1367.
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277-300.
2. Smith R. Risk-based screening for breast cancer: is there a practical strategy? Semin Breast Dis. 1999;2:280-291.
3. Guerra CE, Sherman M, Armstrong K. Diffusion of breast cancer risk assessment in primary care. J Am Board Fam Med. 2009;22:272-279.
4. Pruthi S, Brandt KR, Degnim AC, et al. A multidisciplinary approach to the management of breast cancer, part 1: prevention and diagnosis. Mayo Clin Proc. 2007;82:999-1012.
5. Pruthi S, Gostout BS, Lindor NM. Identification and management of women with BRCA mutations or hereditary predisposition for breast and ovarian cancer. Mayo Clin Proc. 2010;85:1111-1120.
6. Rossouw J, Anderson G, Prentice R, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
7. Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229-237.
8. Daly MB, Axilbund JE, Buys S, et al. Genetic/familial high-risk assessment: breast and ovarian. J Natl Compr Canc Netw. 2010;8:562-594.
9. McPherson K, Steel CM, Dixon JM. ABC of breast diseases. BMJ. 2000;321:624-628.
10. Brinton LA, Schairer C, Hoover RN, et al. Menstrual factors and risk of breast cancer. Cancer Invest. 1988;6:245-254.
11. Apter D, Reinilä M, Vihko R. Some endocrine characteristics of early menarche, a risk factor for breast cancer, are preserved into adulthood. Int J Cancer. 1989;44:783-787.
12. Rebbeck TR, Lynch HT, Neuhausen SL, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346:1616-1622.
13. Narod SA, Brunet JS, Ghadirian P, et al. Tamoxifen and risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a case-control study. Lancet. 2000;356:1876-1881.
14. Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75-89.
15. U.S. Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility. Ann Intern Med. 2005;143:355-361.
16. Gail M, Benichou J. Validation studies on a model for breast cancer risk. J Natl Cancer Inst. 1994;86:573-575.
17. Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 2005;97:1652-1662.
18. Pankratz VS, Hartmann LC, Degnim AC, et al. Assessment of the accuracy of the Gail model in women with atypical hyperplasia. J Clin Oncol. 2008;26:5374-5379.
19. Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879-1886.
20. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696-706.
21. Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Stat Med. 2004;23:1111-1130.
22. Boughey JC, Hartmann LC, Anderson SS, et al. Evaluation of the Tyrer-Cuzick (International Breast Cancer Intervention Study) model for breast cancer risk prediction in women with atypical hyperplasia. J Clin Oncol. 2010;28:3591-3596.
23. Claus EB, Risch N, Thompson W. Autosomal dominant inheritance of early-onset breast cancer. Cancer. 1994;73:643-651.
24. Cummings SR, Tice JA, Bauer S, et al. Prevention of breast cancer in postmenopausal women. J Natl Cancer Inst. 2009;101:384-398.
25. American College of Obstetricians-Gynecologists. Practice bulletin no. 122: Breast cancer screening. Obstet Gynecol. 2011;118(2 pt 1):372-382.
26. U.S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151:716-726.
27. Visvanathan K, Chlebowski R, Hurley P, et al. American Society of Clinical Oncology clinical practice guideline update on the use of pharmacologic interventions including tamoxifen, raloxifene, and aromatase inhibition for breast cancer risk reduction. J Clin Oncol. 2009;27:3235-3258.
28. Vogel VG, Costantino JP, Wickerham DL, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727-2741.
29. Goss PE, Ingle JN, Alés-Martínez JE, et al. Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med. 2011;364:2381-2391.
30. U.S. Preventive Services Task Force. Chemoprevention of breast cancer. Ann Intern Med. 2002;137:56-58.
31. Nelson HD, Fu R, Griffin JC, et al. Systematic review: comparative effectiveness of medications to reduce risk for primary breast cancer. Ann Intern Med. 2009;151:703-715.
32. Vogel VG, Costantino JP, Wickerham DL, et al. Update of the National Surgical Adjuvant Breast and Bowel Project Study of Tamoxifen and Raloxifene (STAR) P-2 Trial: preventing breast cancer. Cancer Prev Res (Phila). 2010;3:696-706.
33. Dunn BK, Ryan A. Phase 3 trials of aromatase inhibitors for breast cancer prevention. Ann N Y Acad Sci. 2009;1155:141-161.
34. National Cancer Institute. Hormone therapy for breast cancer. Reviewed April 11, 2012. Available at: http://www.cancer.gov/cancertopics/factsheet/Therapy/hormone-therapy-breast. Accessed May 18, 2012.
35. Kriege M, Brekelmans CTM, Boetes C, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351:427-437.
36. Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304:967-975.
37. Eisen A, Lubinski J, Klijn J, et al. Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2005;23:7491-7496.
38. Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:1055-1062.
39. Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N Engl J Med. 1999;340:77-84.
40. Shuster LT, Gostout BS, Grossardt BR, Rocca WA. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause Int. 2008;14:111-116.
41. Armstrong K, Schwartz JS, Randall T, et al. Hormone replacement therapy and life expectancy after prophylactic oophorectomy in women with BRCA1/2 mutations: a decision analysis. J Clin Oncol. 2004;22:1045-1054.
42. Eisen A, Lubinski J, Gronwald J, et al. Hormone therapy and the risk of breast cancer in BRCA1 mutation carriers. J Natl Cancer Inst. 2008;100:1361-1367.
;
;