User login
As the death toll from the coronavirus disease 2019 (COVID-19) pandemic rapidly increases, the need to make a timely and accurate diagnosis has never been greater. Even before the pandemic, diagnostic errors (ie, missed, delayed, and incorrect diagnoses) had been one of the leading contributors to harm in health care.1 The COVID-19 pandemic is likely to increase the risk of such errors for several reasons. The disease itself is new and knowledge of its clinical manifestations is still evolving. Both physical and psychological safety of clinicians and health system capacity are compromised and can affect clinical decision-making.2 Situational factors such as staffing shortages and workarounds are more common, and clinicians in certain geographic areas are experiencing epic levels of stress, fatigue, and burnout. Finally, decisions in busy, chaotic and time-pressured healthcare systems with disrupted and/or newly designed care processes will be error prone.1
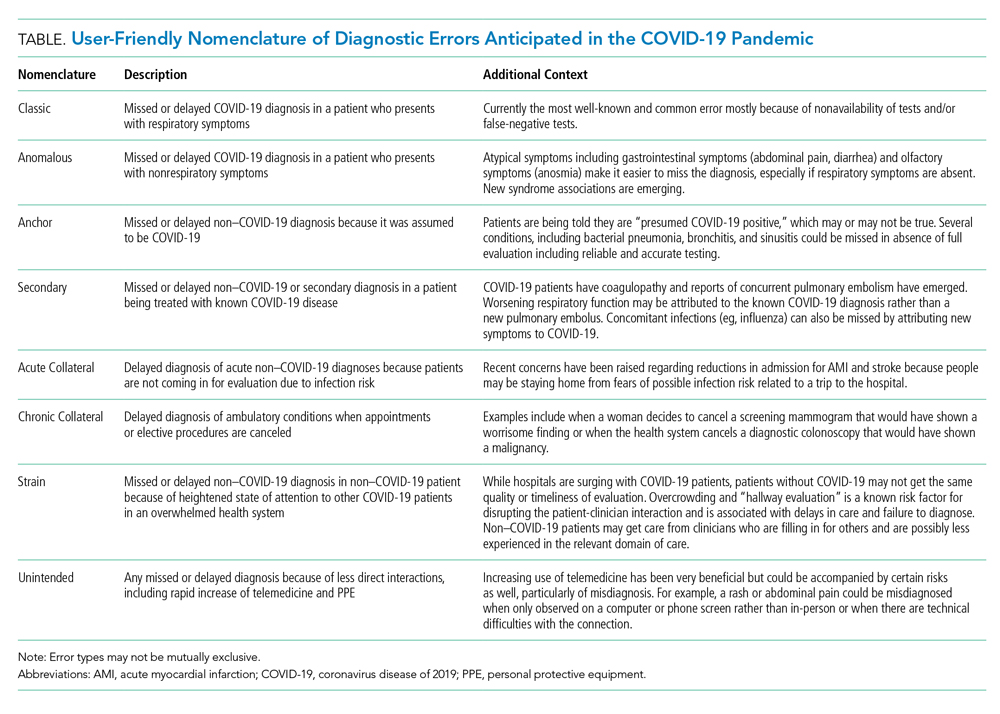
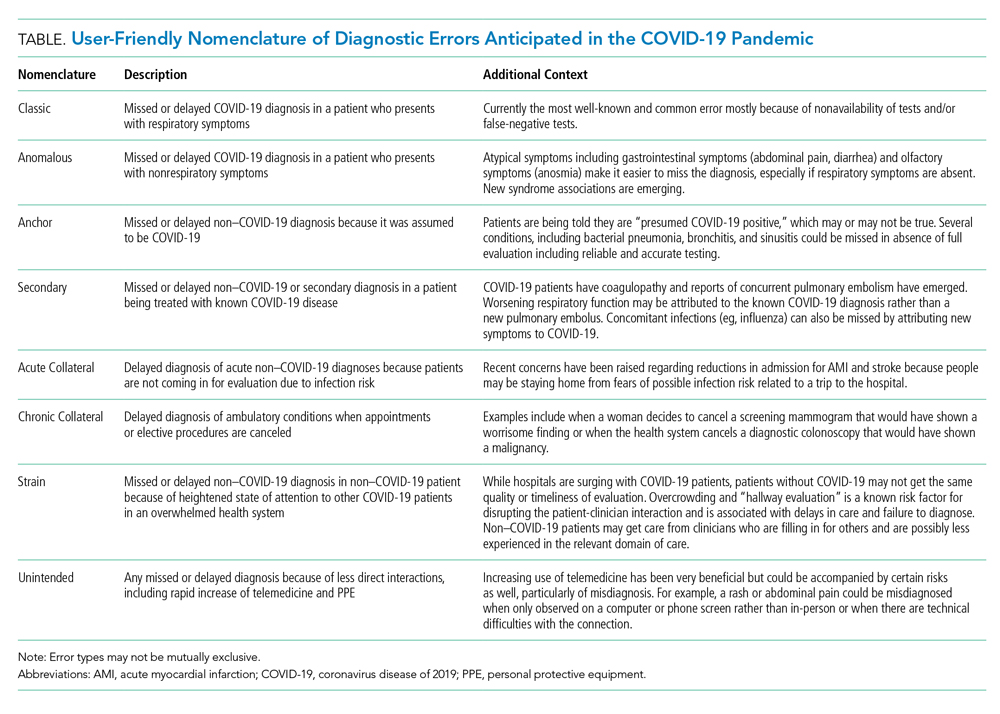
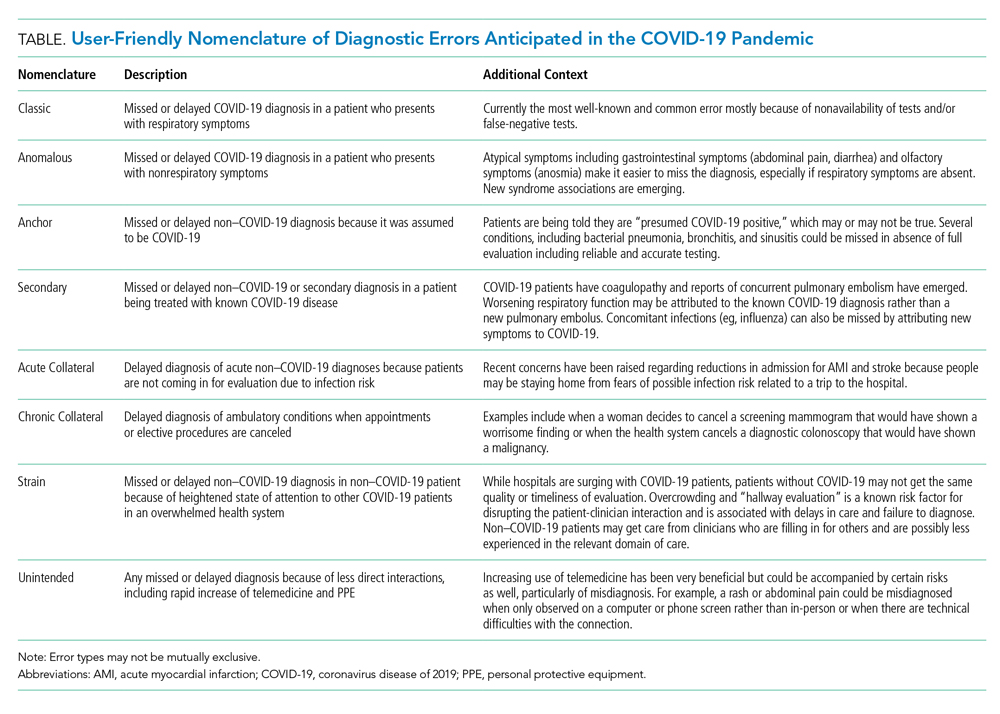
Based on emerging literature and collaborative discussions across the globe, we propose a new typology of diagnostic errors of concern in the COVID-19 era (Table). These errors span the entire continuum of care and have both systems-based and cognitive origins. While some errors arise from previously described clinical reasoning fallacies, others are unique to the pandemic. We provide a user-friendly nomenclature while describing eight types of diagnostic errors and highlight mitigation strategies to reduce potential preventable harm caused by those errors.
TYPES OF ANTICIPATED DIAGNOSTIC ERRORS
The classic COVID-19 presentation of a febrile respiratory illness warrants confirmatory testing, but testing may not be available or produce a false-negative result, leading to an error we termed “Classic.” In the United States, efforts to develop and implement testing protocols are still evolving. There is wide local and regional variation in type and availability of tests, as well as accessibility of information regarding test performance characteristics or diagnostic yield.3 Test results that are false negatives or testing that is not performed can lead to delayed diagnosis of the disease, as well as continued spread.
Testing is similarly relevant when patients present with unusual or nonrespiratory symptoms. Both predominantly olfactory4 and gastrointestinal manifestations5 have now been described, and mysterious new associations, such as multisystem inflammatory syndromes, continue to emerge. A failure to recognize atypical presentations and associations, either because of testing problems or knowledge gaps, could lead to overlooking underlying COVID-19 diagnosis, an error we termed “Anomalous.”
Another error emerging in the pandemic is mislabeling patients who do not have COVID-19 as having the disease, particularly those with respiratory symptoms. This usually occurs in absence of testing in an overwhelmed health system with limited capacity to test or treat (eg, clinicians just assume it must be COVID-19 when the test is not available). This type of labeling error, called “Anchor,” introduces the risk of missing other respiratory infections such as bacterial sinusitis and pneumonia, as well as nonrespiratory conditions.
In patients with known COVID-19, a second underlying or concurrent condition may be missed, an error we termed “Secondary.” For instance, reports of coagulopathy-related pulmonary embolism6 and strokes in young patients with minimal symptoms7 have emerged just recently. Respiratory compromise may be mistakenly attributed to COVID-19 rather than looking for a new source of worsening, such as pulmonary embolism. Similarly, clinicians may not recognize subtle stroke symptoms in patients who were otherwise feeling well at home. Such cognitive errors will likely increase as it becomes harder for clinicians or health systems to keep up with new knowledge.
Collateral effects of the COVID-19 pandemic are also emerging. For instance, patients with symptoms of new acute conditions may be unwilling to visit acute care for evaluation because of infection risk, an error we termed “Acute Collateral.” Concerns are already being raised that patients with acute myocardial infarction8 and stroke9 are not coming in for evaluation. Similarly, there may be delays in diagnosis of important ambulatory conditions, including cancer,10 when appointments or elective procedures are canceled (“Chronic Collateral”). In the United Kingdom, referrals under the 2-week wait system–in which suspected cancer patients referred by general practitioners are seen within 2-weeks–fell by 70% over March to April, 2020.
Diagnosis of non–COVID-19 patients coming into the hospital may also be affected because of the understandably heightened state of attention to COVID-19 patients, capacity, and staffing issues, an error we termed “Strain.” Physicians, including surgeons, pediatricians, and radiologists, have been “redeployed” into acute care medical specialties. Cognitive errors increase when clinicians in new roles face unfamiliar situations and disease manifestations. Although these clinicians may be highly experienced previously, they may have insufficient skills and experience in their new roles and may not feel comfortable asking for guidance.11
Lastly, clinicians are increasingly using intermediary mechanisms, such as PPE and telemedicine technologies, to interact with patients. This is new for both parties and could introduce new types of errors, which we termed “Unintended.” Furthermore, interactions mediated via telemedicine technologies or PPE, as well as PPE conservation measures such as reduced room entries and e-consultation, may reduce the ability of even well-trained clinicians to take effective histories, perform physical exams, and monitor symptoms. In fact, infection-prevention isolation has been shown to put patients at risk of preventable adverse events in hospitalized patients.12
SPECIFIC MITIGATION STRATEGIES
There are many strategies that health systems could deploy to try to minimize these eight types of diagnostic errors. We organize mitigation strategies using the Safer Dx framework, which proposes sociotechnical approaches (ie, both technology and other systems-based approaches) to reduce diagnostic error.13
Technology for Cognitive Support
Up-to-date electronic decision support is needed to optimize test interpretation. Technology can also help scale and facilitate rapid adoption of standardized safety practices and protocols to address emerging risks areas. For instance, there are early efforts to create, implement, and disseminate smart algorithms to predict risks of non–COVID-19 diagnoses such as venous thromboembolism, patient transfer protocols on how best to reduce the burden at overstressed hospitals, protocols to triage rescheduling of elective procedures based on potential risk as determined from data in the electronic health record, new rules for creating outreach to patients who have missed appointments to prevent delays in their evaluation and diagnosis, and triage protocols and follow-up systems to optimize telemedicine.14
Optimized Workflow and Communication
When in-person contact is limited, specific practices (eg, providing patients with iPads, use of reflective listening, and use of optimal nonverbal communication strategies such as eye-contact) can still facilitate comprehensive discussions with patients and families about symptoms and encourage them to speak up if and when they have concerns.15 For patients reached through telemedicine, follow-up appointments and surveys should be done to ensure that symptoms and concerns have been addressed. For clinicians working in new clinical areas unfamiliar to them (eg, surgeons on medical floors, hospitalists in ICUs), buddy systems can pair these clinicians with more experienced clinicians to make it easier for them to ask for help. Visual aids, decision support, and reliable error-prevention resources can also be helpful.16
People-Focused Interventions
Some clinicians are used to practicing solo, but this is the time to start “diagnostic huddles” for discussion of challenging cases with symptoms that are unusual or not improving as expected or for determining whether anything has been missed. In addition to encouraging patients to use reliable digital tools for self-triage, outreach to patients and the public must also advise them (with the help of public health authorities and the media) to seek medical assistance for certain important conditions such as acute myocardial infarction and stroke.
Organizational Strategies
Fundamental safety strategies must be ensured. First, it is critical to have a strong safety culture in which staff feel empowered to speak up, ask questions or ask for help, and report concerns without fear of repercussions or judgement. Culture can take years to develop, but due to rapidly changing circumstances in a crisis, there are ways for healthcare leaders to create changes more quickly. In addition to having daily huddles, leaders should be visible and communicate clearly about the behaviors and norms they are supporting. In particular, frequent leadership rounding (either virtually or in person)—during which leaders ask questions and encourage discussions of concerns in a supportive way—can foster the kind of culture that is needed. All organizations should implement peer support, counseling, limits on hours worked, and other support strategies for all clinicians to minimize the fatigue, stress, and anxiety that can impair cognitive function.17
Organizations must also be able to identify these errors to help understand root causes and prioritize interventions.18 For example, streamlined reporting systems that use apps and hotlines could be developed quickly to ensure that clinicians and patients/families can easily report these errors. Electronic triggers can help detect specific situations indicative of error or delay (eg, patient not on precautions gets switched to precautions during a hospitalization; absence of follow-up on abnormal tests).19
Learning systems—both within and across hospitals—should continue to share diagnostic challenges, the most up-to-date information, and best practices/protocols, and identify opportunities for improvement together. Many hospitals are having virtual grand rounds, journals are rapidly sharing new information via open access, regional and national cross-organizational and multidisciplinary learning networks of various groups have emerged (such as networks of oncologists, infectious disease specialists, and hospitalists), and new and transparent communication channels have developed between state and local health departments, government leaders, health systems, and the public. These forums should discuss emerging knowledge on diagnosis and strategies for risk reduction, many of which will unfold over the next few months.
State/Federal Policies and Regulations
While there is progress, additional challenges with accessibility, accuracy and performance of testing should be addressed at a national level. Guidance is needed on which asymptomatic people should be tested, both within and outside hospitals. Standardized metrics should be developed to monitor diagnostic performance and outcomes and evaluate how COVID-19 diagnosis errors affect different demographics. For instance, black and Hispanic individuals are disproportionately represented in COVID-19 cases and deaths, so metrics could be further stratified by race and ethnicity to ensure that we can understand and eliminate inequities, such as lack of access to care or testing.20
CONCLUSION
Clinicians must be provided with both cognitive and system support so they can do what they do best—diagnose and treat patients and save lives. Intermittent epidemic spikes based on location and season, including a potentially bigger spike of cases later this year, are now projected. Risks and recommendations discussed herein should therefore be rapidly shared to help redesign and strengthen the work system and protect patients from preventable diagnosis-related harm.
Disclaimer
The views expressed in this article do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
1. Singh H, Graber ML. Improving diagnosis in health care—the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. https://doi.org/10.1056/nejmp1512241.
2. Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety [online first]. BMJ Qual Saf. 2020. https://doi.org/10.1136/bmjqs-2019-010110.
3. West CP, Montori VM, Sampathkumar P. COVID-19 testing: the threat of false-negative results [online first]. Mayo Clin Proc. 2020. https://doi.org/10.1016/j.mayocp.2020.04.004.
4. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6771.
5. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620.
6. Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence [online first]. Circulation. 2020. https://doi.org/10.1161/circulationaha.120.047430.
7. Cha AE. Young and middle-aged people, barely sick with COVID-19, are dying of strokes. Washington Post. April 25, 2020. https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/. Accessed April 27, 2020.
8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [online first]. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
9. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [online first]. N Engl J Med. 2020 https://doi.org/10.1056/NEJMc2014816.
10. Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care [online first]. Lancet Oncol. 2020. https://doi.org/10.1016/s1470-2045(20)30242-4.
11. Meyer AN, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173(21):1952-1958. https://doi.org/10.1001/jamainternmed.2013.10081.
12. Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290(14):1899-1905. https://doi.org/10.1001/jama.290.14.1899.
13. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-110. https://doi.org/10.1136/bmjqs-2014-003675.
14. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual Care [online first]. J Am Med Inform Assoc. 2020. https://doi.org/10.1093/jamia/ocaa067.
15. Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296-304. https://doi.org/10.1177/2374373518803617.
16. Singh H, Zwaan L. Web Exclusives. Annals for Hospitalists Inpatient Notes – reducing diagnostic error – a new horizon of opportunities for hospital medicine. Ann Intern Med. 2016;165(8):HO2-HO4. https://doi.org/10.7326/m16-2042.
17. Wu AW, Connors C, Everly GS Jr. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. 2020. https://doi.org/10.7326/m20-1236.
18. Singh H, Bradford A, Goeschel C. Operational Measurement of Diagnostic Safety: State of the Science. Rockville, MD: Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/topics/state-of-science.pdf. Accessed May 10, 2020.
19. Murphy DR, Meyer AN, Sittig DF, Meeks DW, Thomas EJ, Singh H. Application of electronic trigger tools to identify targets for improving diagnostic safety. BMJ Qual Saf. 2019;28(2):151-159. https://doi.org/10.1136/bmjqs-2018-008086.
20. Owen WF, Carmona R, Pomeroy C. Failing another national stress test on health disparities [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547.
As the death toll from the coronavirus disease 2019 (COVID-19) pandemic rapidly increases, the need to make a timely and accurate diagnosis has never been greater. Even before the pandemic, diagnostic errors (ie, missed, delayed, and incorrect diagnoses) had been one of the leading contributors to harm in health care.1 The COVID-19 pandemic is likely to increase the risk of such errors for several reasons. The disease itself is new and knowledge of its clinical manifestations is still evolving. Both physical and psychological safety of clinicians and health system capacity are compromised and can affect clinical decision-making.2 Situational factors such as staffing shortages and workarounds are more common, and clinicians in certain geographic areas are experiencing epic levels of stress, fatigue, and burnout. Finally, decisions in busy, chaotic and time-pressured healthcare systems with disrupted and/or newly designed care processes will be error prone.1
Based on emerging literature and collaborative discussions across the globe, we propose a new typology of diagnostic errors of concern in the COVID-19 era (Table). These errors span the entire continuum of care and have both systems-based and cognitive origins. While some errors arise from previously described clinical reasoning fallacies, others are unique to the pandemic. We provide a user-friendly nomenclature while describing eight types of diagnostic errors and highlight mitigation strategies to reduce potential preventable harm caused by those errors.
TYPES OF ANTICIPATED DIAGNOSTIC ERRORS
The classic COVID-19 presentation of a febrile respiratory illness warrants confirmatory testing, but testing may not be available or produce a false-negative result, leading to an error we termed “Classic.” In the United States, efforts to develop and implement testing protocols are still evolving. There is wide local and regional variation in type and availability of tests, as well as accessibility of information regarding test performance characteristics or diagnostic yield.3 Test results that are false negatives or testing that is not performed can lead to delayed diagnosis of the disease, as well as continued spread.
Testing is similarly relevant when patients present with unusual or nonrespiratory symptoms. Both predominantly olfactory4 and gastrointestinal manifestations5 have now been described, and mysterious new associations, such as multisystem inflammatory syndromes, continue to emerge. A failure to recognize atypical presentations and associations, either because of testing problems or knowledge gaps, could lead to overlooking underlying COVID-19 diagnosis, an error we termed “Anomalous.”
Another error emerging in the pandemic is mislabeling patients who do not have COVID-19 as having the disease, particularly those with respiratory symptoms. This usually occurs in absence of testing in an overwhelmed health system with limited capacity to test or treat (eg, clinicians just assume it must be COVID-19 when the test is not available). This type of labeling error, called “Anchor,” introduces the risk of missing other respiratory infections such as bacterial sinusitis and pneumonia, as well as nonrespiratory conditions.
In patients with known COVID-19, a second underlying or concurrent condition may be missed, an error we termed “Secondary.” For instance, reports of coagulopathy-related pulmonary embolism6 and strokes in young patients with minimal symptoms7 have emerged just recently. Respiratory compromise may be mistakenly attributed to COVID-19 rather than looking for a new source of worsening, such as pulmonary embolism. Similarly, clinicians may not recognize subtle stroke symptoms in patients who were otherwise feeling well at home. Such cognitive errors will likely increase as it becomes harder for clinicians or health systems to keep up with new knowledge.
Collateral effects of the COVID-19 pandemic are also emerging. For instance, patients with symptoms of new acute conditions may be unwilling to visit acute care for evaluation because of infection risk, an error we termed “Acute Collateral.” Concerns are already being raised that patients with acute myocardial infarction8 and stroke9 are not coming in for evaluation. Similarly, there may be delays in diagnosis of important ambulatory conditions, including cancer,10 when appointments or elective procedures are canceled (“Chronic Collateral”). In the United Kingdom, referrals under the 2-week wait system–in which suspected cancer patients referred by general practitioners are seen within 2-weeks–fell by 70% over March to April, 2020.
Diagnosis of non–COVID-19 patients coming into the hospital may also be affected because of the understandably heightened state of attention to COVID-19 patients, capacity, and staffing issues, an error we termed “Strain.” Physicians, including surgeons, pediatricians, and radiologists, have been “redeployed” into acute care medical specialties. Cognitive errors increase when clinicians in new roles face unfamiliar situations and disease manifestations. Although these clinicians may be highly experienced previously, they may have insufficient skills and experience in their new roles and may not feel comfortable asking for guidance.11
Lastly, clinicians are increasingly using intermediary mechanisms, such as PPE and telemedicine technologies, to interact with patients. This is new for both parties and could introduce new types of errors, which we termed “Unintended.” Furthermore, interactions mediated via telemedicine technologies or PPE, as well as PPE conservation measures such as reduced room entries and e-consultation, may reduce the ability of even well-trained clinicians to take effective histories, perform physical exams, and monitor symptoms. In fact, infection-prevention isolation has been shown to put patients at risk of preventable adverse events in hospitalized patients.12
SPECIFIC MITIGATION STRATEGIES
There are many strategies that health systems could deploy to try to minimize these eight types of diagnostic errors. We organize mitigation strategies using the Safer Dx framework, which proposes sociotechnical approaches (ie, both technology and other systems-based approaches) to reduce diagnostic error.13
Technology for Cognitive Support
Up-to-date electronic decision support is needed to optimize test interpretation. Technology can also help scale and facilitate rapid adoption of standardized safety practices and protocols to address emerging risks areas. For instance, there are early efforts to create, implement, and disseminate smart algorithms to predict risks of non–COVID-19 diagnoses such as venous thromboembolism, patient transfer protocols on how best to reduce the burden at overstressed hospitals, protocols to triage rescheduling of elective procedures based on potential risk as determined from data in the electronic health record, new rules for creating outreach to patients who have missed appointments to prevent delays in their evaluation and diagnosis, and triage protocols and follow-up systems to optimize telemedicine.14
Optimized Workflow and Communication
When in-person contact is limited, specific practices (eg, providing patients with iPads, use of reflective listening, and use of optimal nonverbal communication strategies such as eye-contact) can still facilitate comprehensive discussions with patients and families about symptoms and encourage them to speak up if and when they have concerns.15 For patients reached through telemedicine, follow-up appointments and surveys should be done to ensure that symptoms and concerns have been addressed. For clinicians working in new clinical areas unfamiliar to them (eg, surgeons on medical floors, hospitalists in ICUs), buddy systems can pair these clinicians with more experienced clinicians to make it easier for them to ask for help. Visual aids, decision support, and reliable error-prevention resources can also be helpful.16
People-Focused Interventions
Some clinicians are used to practicing solo, but this is the time to start “diagnostic huddles” for discussion of challenging cases with symptoms that are unusual or not improving as expected or for determining whether anything has been missed. In addition to encouraging patients to use reliable digital tools for self-triage, outreach to patients and the public must also advise them (with the help of public health authorities and the media) to seek medical assistance for certain important conditions such as acute myocardial infarction and stroke.
Organizational Strategies
Fundamental safety strategies must be ensured. First, it is critical to have a strong safety culture in which staff feel empowered to speak up, ask questions or ask for help, and report concerns without fear of repercussions or judgement. Culture can take years to develop, but due to rapidly changing circumstances in a crisis, there are ways for healthcare leaders to create changes more quickly. In addition to having daily huddles, leaders should be visible and communicate clearly about the behaviors and norms they are supporting. In particular, frequent leadership rounding (either virtually or in person)—during which leaders ask questions and encourage discussions of concerns in a supportive way—can foster the kind of culture that is needed. All organizations should implement peer support, counseling, limits on hours worked, and other support strategies for all clinicians to minimize the fatigue, stress, and anxiety that can impair cognitive function.17
Organizations must also be able to identify these errors to help understand root causes and prioritize interventions.18 For example, streamlined reporting systems that use apps and hotlines could be developed quickly to ensure that clinicians and patients/families can easily report these errors. Electronic triggers can help detect specific situations indicative of error or delay (eg, patient not on precautions gets switched to precautions during a hospitalization; absence of follow-up on abnormal tests).19
Learning systems—both within and across hospitals—should continue to share diagnostic challenges, the most up-to-date information, and best practices/protocols, and identify opportunities for improvement together. Many hospitals are having virtual grand rounds, journals are rapidly sharing new information via open access, regional and national cross-organizational and multidisciplinary learning networks of various groups have emerged (such as networks of oncologists, infectious disease specialists, and hospitalists), and new and transparent communication channels have developed between state and local health departments, government leaders, health systems, and the public. These forums should discuss emerging knowledge on diagnosis and strategies for risk reduction, many of which will unfold over the next few months.
State/Federal Policies and Regulations
While there is progress, additional challenges with accessibility, accuracy and performance of testing should be addressed at a national level. Guidance is needed on which asymptomatic people should be tested, both within and outside hospitals. Standardized metrics should be developed to monitor diagnostic performance and outcomes and evaluate how COVID-19 diagnosis errors affect different demographics. For instance, black and Hispanic individuals are disproportionately represented in COVID-19 cases and deaths, so metrics could be further stratified by race and ethnicity to ensure that we can understand and eliminate inequities, such as lack of access to care or testing.20
CONCLUSION
Clinicians must be provided with both cognitive and system support so they can do what they do best—diagnose and treat patients and save lives. Intermittent epidemic spikes based on location and season, including a potentially bigger spike of cases later this year, are now projected. Risks and recommendations discussed herein should therefore be rapidly shared to help redesign and strengthen the work system and protect patients from preventable diagnosis-related harm.
Disclaimer
The views expressed in this article do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
As the death toll from the coronavirus disease 2019 (COVID-19) pandemic rapidly increases, the need to make a timely and accurate diagnosis has never been greater. Even before the pandemic, diagnostic errors (ie, missed, delayed, and incorrect diagnoses) had been one of the leading contributors to harm in health care.1 The COVID-19 pandemic is likely to increase the risk of such errors for several reasons. The disease itself is new and knowledge of its clinical manifestations is still evolving. Both physical and psychological safety of clinicians and health system capacity are compromised and can affect clinical decision-making.2 Situational factors such as staffing shortages and workarounds are more common, and clinicians in certain geographic areas are experiencing epic levels of stress, fatigue, and burnout. Finally, decisions in busy, chaotic and time-pressured healthcare systems with disrupted and/or newly designed care processes will be error prone.1
Based on emerging literature and collaborative discussions across the globe, we propose a new typology of diagnostic errors of concern in the COVID-19 era (Table). These errors span the entire continuum of care and have both systems-based and cognitive origins. While some errors arise from previously described clinical reasoning fallacies, others are unique to the pandemic. We provide a user-friendly nomenclature while describing eight types of diagnostic errors and highlight mitigation strategies to reduce potential preventable harm caused by those errors.
TYPES OF ANTICIPATED DIAGNOSTIC ERRORS
The classic COVID-19 presentation of a febrile respiratory illness warrants confirmatory testing, but testing may not be available or produce a false-negative result, leading to an error we termed “Classic.” In the United States, efforts to develop and implement testing protocols are still evolving. There is wide local and regional variation in type and availability of tests, as well as accessibility of information regarding test performance characteristics or diagnostic yield.3 Test results that are false negatives or testing that is not performed can lead to delayed diagnosis of the disease, as well as continued spread.
Testing is similarly relevant when patients present with unusual or nonrespiratory symptoms. Both predominantly olfactory4 and gastrointestinal manifestations5 have now been described, and mysterious new associations, such as multisystem inflammatory syndromes, continue to emerge. A failure to recognize atypical presentations and associations, either because of testing problems or knowledge gaps, could lead to overlooking underlying COVID-19 diagnosis, an error we termed “Anomalous.”
Another error emerging in the pandemic is mislabeling patients who do not have COVID-19 as having the disease, particularly those with respiratory symptoms. This usually occurs in absence of testing in an overwhelmed health system with limited capacity to test or treat (eg, clinicians just assume it must be COVID-19 when the test is not available). This type of labeling error, called “Anchor,” introduces the risk of missing other respiratory infections such as bacterial sinusitis and pneumonia, as well as nonrespiratory conditions.
In patients with known COVID-19, a second underlying or concurrent condition may be missed, an error we termed “Secondary.” For instance, reports of coagulopathy-related pulmonary embolism6 and strokes in young patients with minimal symptoms7 have emerged just recently. Respiratory compromise may be mistakenly attributed to COVID-19 rather than looking for a new source of worsening, such as pulmonary embolism. Similarly, clinicians may not recognize subtle stroke symptoms in patients who were otherwise feeling well at home. Such cognitive errors will likely increase as it becomes harder for clinicians or health systems to keep up with new knowledge.
Collateral effects of the COVID-19 pandemic are also emerging. For instance, patients with symptoms of new acute conditions may be unwilling to visit acute care for evaluation because of infection risk, an error we termed “Acute Collateral.” Concerns are already being raised that patients with acute myocardial infarction8 and stroke9 are not coming in for evaluation. Similarly, there may be delays in diagnosis of important ambulatory conditions, including cancer,10 when appointments or elective procedures are canceled (“Chronic Collateral”). In the United Kingdom, referrals under the 2-week wait system–in which suspected cancer patients referred by general practitioners are seen within 2-weeks–fell by 70% over March to April, 2020.
Diagnosis of non–COVID-19 patients coming into the hospital may also be affected because of the understandably heightened state of attention to COVID-19 patients, capacity, and staffing issues, an error we termed “Strain.” Physicians, including surgeons, pediatricians, and radiologists, have been “redeployed” into acute care medical specialties. Cognitive errors increase when clinicians in new roles face unfamiliar situations and disease manifestations. Although these clinicians may be highly experienced previously, they may have insufficient skills and experience in their new roles and may not feel comfortable asking for guidance.11
Lastly, clinicians are increasingly using intermediary mechanisms, such as PPE and telemedicine technologies, to interact with patients. This is new for both parties and could introduce new types of errors, which we termed “Unintended.” Furthermore, interactions mediated via telemedicine technologies or PPE, as well as PPE conservation measures such as reduced room entries and e-consultation, may reduce the ability of even well-trained clinicians to take effective histories, perform physical exams, and monitor symptoms. In fact, infection-prevention isolation has been shown to put patients at risk of preventable adverse events in hospitalized patients.12
SPECIFIC MITIGATION STRATEGIES
There are many strategies that health systems could deploy to try to minimize these eight types of diagnostic errors. We organize mitigation strategies using the Safer Dx framework, which proposes sociotechnical approaches (ie, both technology and other systems-based approaches) to reduce diagnostic error.13
Technology for Cognitive Support
Up-to-date electronic decision support is needed to optimize test interpretation. Technology can also help scale and facilitate rapid adoption of standardized safety practices and protocols to address emerging risks areas. For instance, there are early efforts to create, implement, and disseminate smart algorithms to predict risks of non–COVID-19 diagnoses such as venous thromboembolism, patient transfer protocols on how best to reduce the burden at overstressed hospitals, protocols to triage rescheduling of elective procedures based on potential risk as determined from data in the electronic health record, new rules for creating outreach to patients who have missed appointments to prevent delays in their evaluation and diagnosis, and triage protocols and follow-up systems to optimize telemedicine.14
Optimized Workflow and Communication
When in-person contact is limited, specific practices (eg, providing patients with iPads, use of reflective listening, and use of optimal nonverbal communication strategies such as eye-contact) can still facilitate comprehensive discussions with patients and families about symptoms and encourage them to speak up if and when they have concerns.15 For patients reached through telemedicine, follow-up appointments and surveys should be done to ensure that symptoms and concerns have been addressed. For clinicians working in new clinical areas unfamiliar to them (eg, surgeons on medical floors, hospitalists in ICUs), buddy systems can pair these clinicians with more experienced clinicians to make it easier for them to ask for help. Visual aids, decision support, and reliable error-prevention resources can also be helpful.16
People-Focused Interventions
Some clinicians are used to practicing solo, but this is the time to start “diagnostic huddles” for discussion of challenging cases with symptoms that are unusual or not improving as expected or for determining whether anything has been missed. In addition to encouraging patients to use reliable digital tools for self-triage, outreach to patients and the public must also advise them (with the help of public health authorities and the media) to seek medical assistance for certain important conditions such as acute myocardial infarction and stroke.
Organizational Strategies
Fundamental safety strategies must be ensured. First, it is critical to have a strong safety culture in which staff feel empowered to speak up, ask questions or ask for help, and report concerns without fear of repercussions or judgement. Culture can take years to develop, but due to rapidly changing circumstances in a crisis, there are ways for healthcare leaders to create changes more quickly. In addition to having daily huddles, leaders should be visible and communicate clearly about the behaviors and norms they are supporting. In particular, frequent leadership rounding (either virtually or in person)—during which leaders ask questions and encourage discussions of concerns in a supportive way—can foster the kind of culture that is needed. All organizations should implement peer support, counseling, limits on hours worked, and other support strategies for all clinicians to minimize the fatigue, stress, and anxiety that can impair cognitive function.17
Organizations must also be able to identify these errors to help understand root causes and prioritize interventions.18 For example, streamlined reporting systems that use apps and hotlines could be developed quickly to ensure that clinicians and patients/families can easily report these errors. Electronic triggers can help detect specific situations indicative of error or delay (eg, patient not on precautions gets switched to precautions during a hospitalization; absence of follow-up on abnormal tests).19
Learning systems—both within and across hospitals—should continue to share diagnostic challenges, the most up-to-date information, and best practices/protocols, and identify opportunities for improvement together. Many hospitals are having virtual grand rounds, journals are rapidly sharing new information via open access, regional and national cross-organizational and multidisciplinary learning networks of various groups have emerged (such as networks of oncologists, infectious disease specialists, and hospitalists), and new and transparent communication channels have developed between state and local health departments, government leaders, health systems, and the public. These forums should discuss emerging knowledge on diagnosis and strategies for risk reduction, many of which will unfold over the next few months.
State/Federal Policies and Regulations
While there is progress, additional challenges with accessibility, accuracy and performance of testing should be addressed at a national level. Guidance is needed on which asymptomatic people should be tested, both within and outside hospitals. Standardized metrics should be developed to monitor diagnostic performance and outcomes and evaluate how COVID-19 diagnosis errors affect different demographics. For instance, black and Hispanic individuals are disproportionately represented in COVID-19 cases and deaths, so metrics could be further stratified by race and ethnicity to ensure that we can understand and eliminate inequities, such as lack of access to care or testing.20
CONCLUSION
Clinicians must be provided with both cognitive and system support so they can do what they do best—diagnose and treat patients and save lives. Intermittent epidemic spikes based on location and season, including a potentially bigger spike of cases later this year, are now projected. Risks and recommendations discussed herein should therefore be rapidly shared to help redesign and strengthen the work system and protect patients from preventable diagnosis-related harm.
Disclaimer
The views expressed in this article do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
1. Singh H, Graber ML. Improving diagnosis in health care—the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. https://doi.org/10.1056/nejmp1512241.
2. Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety [online first]. BMJ Qual Saf. 2020. https://doi.org/10.1136/bmjqs-2019-010110.
3. West CP, Montori VM, Sampathkumar P. COVID-19 testing: the threat of false-negative results [online first]. Mayo Clin Proc. 2020. https://doi.org/10.1016/j.mayocp.2020.04.004.
4. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6771.
5. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620.
6. Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence [online first]. Circulation. 2020. https://doi.org/10.1161/circulationaha.120.047430.
7. Cha AE. Young and middle-aged people, barely sick with COVID-19, are dying of strokes. Washington Post. April 25, 2020. https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/. Accessed April 27, 2020.
8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [online first]. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
9. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [online first]. N Engl J Med. 2020 https://doi.org/10.1056/NEJMc2014816.
10. Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care [online first]. Lancet Oncol. 2020. https://doi.org/10.1016/s1470-2045(20)30242-4.
11. Meyer AN, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173(21):1952-1958. https://doi.org/10.1001/jamainternmed.2013.10081.
12. Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290(14):1899-1905. https://doi.org/10.1001/jama.290.14.1899.
13. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-110. https://doi.org/10.1136/bmjqs-2014-003675.
14. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual Care [online first]. J Am Med Inform Assoc. 2020. https://doi.org/10.1093/jamia/ocaa067.
15. Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296-304. https://doi.org/10.1177/2374373518803617.
16. Singh H, Zwaan L. Web Exclusives. Annals for Hospitalists Inpatient Notes – reducing diagnostic error – a new horizon of opportunities for hospital medicine. Ann Intern Med. 2016;165(8):HO2-HO4. https://doi.org/10.7326/m16-2042.
17. Wu AW, Connors C, Everly GS Jr. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. 2020. https://doi.org/10.7326/m20-1236.
18. Singh H, Bradford A, Goeschel C. Operational Measurement of Diagnostic Safety: State of the Science. Rockville, MD: Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/topics/state-of-science.pdf. Accessed May 10, 2020.
19. Murphy DR, Meyer AN, Sittig DF, Meeks DW, Thomas EJ, Singh H. Application of electronic trigger tools to identify targets for improving diagnostic safety. BMJ Qual Saf. 2019;28(2):151-159. https://doi.org/10.1136/bmjqs-2018-008086.
20. Owen WF, Carmona R, Pomeroy C. Failing another national stress test on health disparities [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547.
1. Singh H, Graber ML. Improving diagnosis in health care—the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. https://doi.org/10.1056/nejmp1512241.
2. Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety [online first]. BMJ Qual Saf. 2020. https://doi.org/10.1136/bmjqs-2019-010110.
3. West CP, Montori VM, Sampathkumar P. COVID-19 testing: the threat of false-negative results [online first]. Mayo Clin Proc. 2020. https://doi.org/10.1016/j.mayocp.2020.04.004.
4. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6771.
5. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620.
6. Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence [online first]. Circulation. 2020. https://doi.org/10.1161/circulationaha.120.047430.
7. Cha AE. Young and middle-aged people, barely sick with COVID-19, are dying of strokes. Washington Post. April 25, 2020. https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/. Accessed April 27, 2020.
8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [online first]. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
9. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [online first]. N Engl J Med. 2020 https://doi.org/10.1056/NEJMc2014816.
10. Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care [online first]. Lancet Oncol. 2020. https://doi.org/10.1016/s1470-2045(20)30242-4.
11. Meyer AN, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173(21):1952-1958. https://doi.org/10.1001/jamainternmed.2013.10081.
12. Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290(14):1899-1905. https://doi.org/10.1001/jama.290.14.1899.
13. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-110. https://doi.org/10.1136/bmjqs-2014-003675.
14. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual Care [online first]. J Am Med Inform Assoc. 2020. https://doi.org/10.1093/jamia/ocaa067.
15. Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296-304. https://doi.org/10.1177/2374373518803617.
16. Singh H, Zwaan L. Web Exclusives. Annals for Hospitalists Inpatient Notes – reducing diagnostic error – a new horizon of opportunities for hospital medicine. Ann Intern Med. 2016;165(8):HO2-HO4. https://doi.org/10.7326/m16-2042.
17. Wu AW, Connors C, Everly GS Jr. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. 2020. https://doi.org/10.7326/m20-1236.
18. Singh H, Bradford A, Goeschel C. Operational Measurement of Diagnostic Safety: State of the Science. Rockville, MD: Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/topics/state-of-science.pdf. Accessed May 10, 2020.
19. Murphy DR, Meyer AN, Sittig DF, Meeks DW, Thomas EJ, Singh H. Application of electronic trigger tools to identify targets for improving diagnostic safety. BMJ Qual Saf. 2019;28(2):151-159. https://doi.org/10.1136/bmjqs-2018-008086.
20. Owen WF, Carmona R, Pomeroy C. Failing another national stress test on health disparities [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547.
© 2020 Society of Hospital Medicine