User login
Reducing the Risk of Diagnostic Error in the COVID-19 Era
As the death toll from the coronavirus disease 2019 (COVID-19) pandemic rapidly increases, the need to make a timely and accurate diagnosis has never been greater. Even before the pandemic, diagnostic errors (ie, missed, delayed, and incorrect diagnoses) had been one of the leading contributors to harm in health care.1 The COVID-19 pandemic is likely to increase the risk of such errors for several reasons. The disease itself is new and knowledge of its clinical manifestations is still evolving. Both physical and psychological safety of clinicians and health system capacity are compromised and can affect clinical decision-making.2 Situational factors such as staffing shortages and workarounds are more common, and clinicians in certain geographic areas are experiencing epic levels of stress, fatigue, and burnout. Finally, decisions in busy, chaotic and time-pressured healthcare systems with disrupted and/or newly designed care processes will be error prone.1
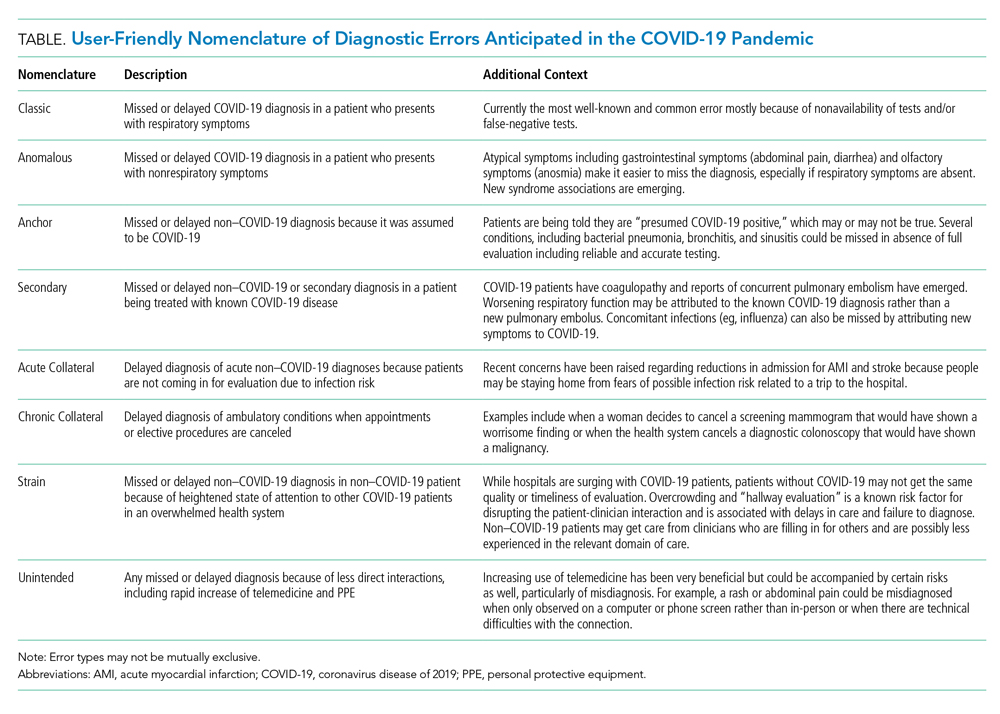
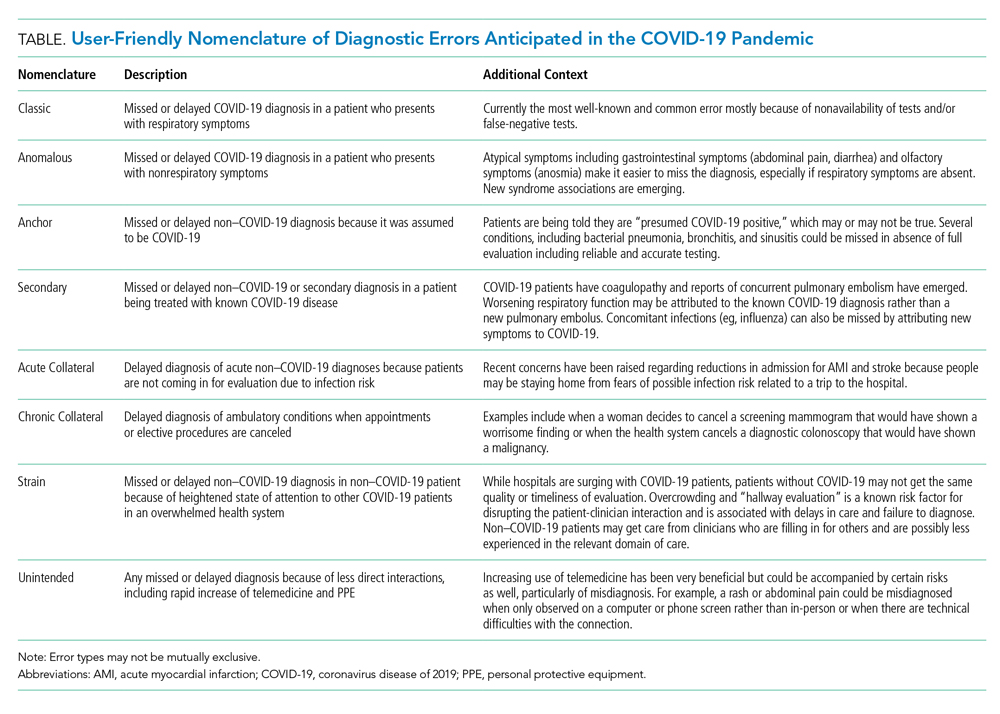
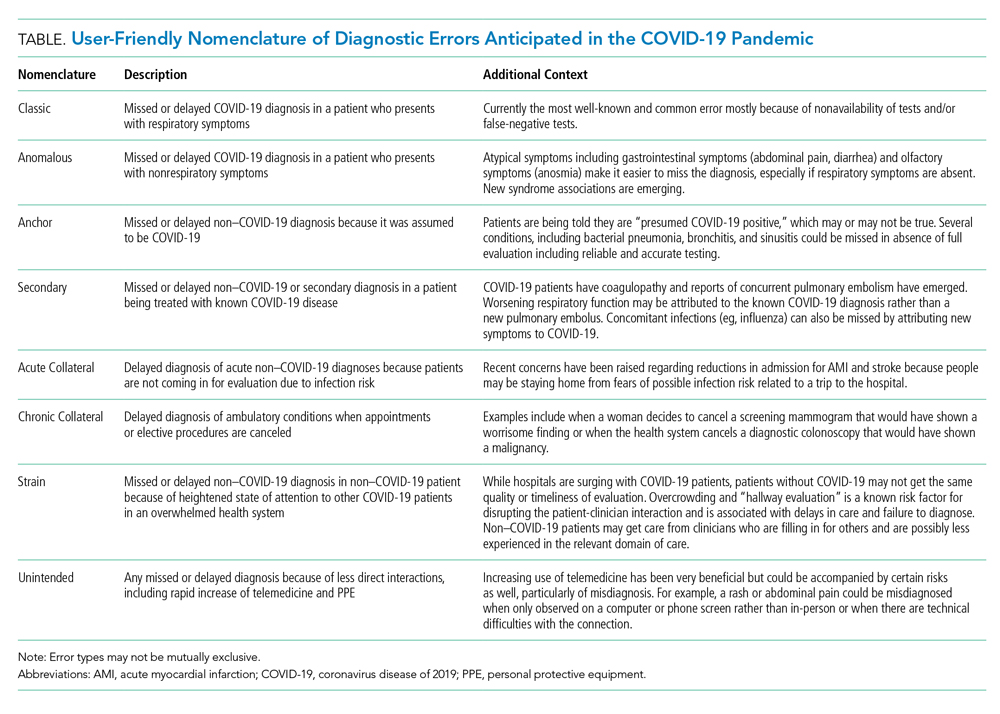
Based on emerging literature and collaborative discussions across the globe, we propose a new typology of diagnostic errors of concern in the COVID-19 era (Table). These errors span the entire continuum of care and have both systems-based and cognitive origins. While some errors arise from previously described clinical reasoning fallacies, others are unique to the pandemic. We provide a user-friendly nomenclature while describing eight types of diagnostic errors and highlight mitigation strategies to reduce potential preventable harm caused by those errors.
TYPES OF ANTICIPATED DIAGNOSTIC ERRORS
The classic COVID-19 presentation of a febrile respiratory illness warrants confirmatory testing, but testing may not be available or produce a false-negative result, leading to an error we termed “Classic.” In the United States, efforts to develop and implement testing protocols are still evolving. There is wide local and regional variation in type and availability of tests, as well as accessibility of information regarding test performance characteristics or diagnostic yield.3 Test results that are false negatives or testing that is not performed can lead to delayed diagnosis of the disease, as well as continued spread.
Testing is similarly relevant when patients present with unusual or nonrespiratory symptoms. Both predominantly olfactory4 and gastrointestinal manifestations5 have now been described, and mysterious new associations, such as multisystem inflammatory syndromes, continue to emerge. A failure to recognize atypical presentations and associations, either because of testing problems or knowledge gaps, could lead to overlooking underlying COVID-19 diagnosis, an error we termed “Anomalous.”
Another error emerging in the pandemic is mislabeling patients who do not have COVID-19 as having the disease, particularly those with respiratory symptoms. This usually occurs in absence of testing in an overwhelmed health system with limited capacity to test or treat (eg, clinicians just assume it must be COVID-19 when the test is not available). This type of labeling error, called “Anchor,” introduces the risk of missing other respiratory infections such as bacterial sinusitis and pneumonia, as well as nonrespiratory conditions.
In patients with known COVID-19, a second underlying or concurrent condition may be missed, an error we termed “Secondary.” For instance, reports of coagulopathy-related pulmonary embolism6 and strokes in young patients with minimal symptoms7 have emerged just recently. Respiratory compromise may be mistakenly attributed to COVID-19 rather than looking for a new source of worsening, such as pulmonary embolism. Similarly, clinicians may not recognize subtle stroke symptoms in patients who were otherwise feeling well at home. Such cognitive errors will likely increase as it becomes harder for clinicians or health systems to keep up with new knowledge.
Collateral effects of the COVID-19 pandemic are also emerging. For instance, patients with symptoms of new acute conditions may be unwilling to visit acute care for evaluation because of infection risk, an error we termed “Acute Collateral.” Concerns are already being raised that patients with acute myocardial infarction8 and stroke9 are not coming in for evaluation. Similarly, there may be delays in diagnosis of important ambulatory conditions, including cancer,10 when appointments or elective procedures are canceled (“Chronic Collateral”). In the United Kingdom, referrals under the 2-week wait system–in which suspected cancer patients referred by general practitioners are seen within 2-weeks–fell by 70% over March to April, 2020.
Diagnosis of non–COVID-19 patients coming into the hospital may also be affected because of the understandably heightened state of attention to COVID-19 patients, capacity, and staffing issues, an error we termed “Strain.” Physicians, including surgeons, pediatricians, and radiologists, have been “redeployed” into acute care medical specialties. Cognitive errors increase when clinicians in new roles face unfamiliar situations and disease manifestations. Although these clinicians may be highly experienced previously, they may have insufficient skills and experience in their new roles and may not feel comfortable asking for guidance.11
Lastly, clinicians are increasingly using intermediary mechanisms, such as PPE and telemedicine technologies, to interact with patients. This is new for both parties and could introduce new types of errors, which we termed “Unintended.” Furthermore, interactions mediated via telemedicine technologies or PPE, as well as PPE conservation measures such as reduced room entries and e-consultation, may reduce the ability of even well-trained clinicians to take effective histories, perform physical exams, and monitor symptoms. In fact, infection-prevention isolation has been shown to put patients at risk of preventable adverse events in hospitalized patients.12
SPECIFIC MITIGATION STRATEGIES
There are many strategies that health systems could deploy to try to minimize these eight types of diagnostic errors. We organize mitigation strategies using the Safer Dx framework, which proposes sociotechnical approaches (ie, both technology and other systems-based approaches) to reduce diagnostic error.13
Technology for Cognitive Support
Up-to-date electronic decision support is needed to optimize test interpretation. Technology can also help scale and facilitate rapid adoption of standardized safety practices and protocols to address emerging risks areas. For instance, there are early efforts to create, implement, and disseminate smart algorithms to predict risks of non–COVID-19 diagnoses such as venous thromboembolism, patient transfer protocols on how best to reduce the burden at overstressed hospitals, protocols to triage rescheduling of elective procedures based on potential risk as determined from data in the electronic health record, new rules for creating outreach to patients who have missed appointments to prevent delays in their evaluation and diagnosis, and triage protocols and follow-up systems to optimize telemedicine.14
Optimized Workflow and Communication
When in-person contact is limited, specific practices (eg, providing patients with iPads, use of reflective listening, and use of optimal nonverbal communication strategies such as eye-contact) can still facilitate comprehensive discussions with patients and families about symptoms and encourage them to speak up if and when they have concerns.15 For patients reached through telemedicine, follow-up appointments and surveys should be done to ensure that symptoms and concerns have been addressed. For clinicians working in new clinical areas unfamiliar to them (eg, surgeons on medical floors, hospitalists in ICUs), buddy systems can pair these clinicians with more experienced clinicians to make it easier for them to ask for help. Visual aids, decision support, and reliable error-prevention resources can also be helpful.16
People-Focused Interventions
Some clinicians are used to practicing solo, but this is the time to start “diagnostic huddles” for discussion of challenging cases with symptoms that are unusual or not improving as expected or for determining whether anything has been missed. In addition to encouraging patients to use reliable digital tools for self-triage, outreach to patients and the public must also advise them (with the help of public health authorities and the media) to seek medical assistance for certain important conditions such as acute myocardial infarction and stroke.
Organizational Strategies
Fundamental safety strategies must be ensured. First, it is critical to have a strong safety culture in which staff feel empowered to speak up, ask questions or ask for help, and report concerns without fear of repercussions or judgement. Culture can take years to develop, but due to rapidly changing circumstances in a crisis, there are ways for healthcare leaders to create changes more quickly. In addition to having daily huddles, leaders should be visible and communicate clearly about the behaviors and norms they are supporting. In particular, frequent leadership rounding (either virtually or in person)—during which leaders ask questions and encourage discussions of concerns in a supportive way—can foster the kind of culture that is needed. All organizations should implement peer support, counseling, limits on hours worked, and other support strategies for all clinicians to minimize the fatigue, stress, and anxiety that can impair cognitive function.17
Organizations must also be able to identify these errors to help understand root causes and prioritize interventions.18 For example, streamlined reporting systems that use apps and hotlines could be developed quickly to ensure that clinicians and patients/families can easily report these errors. Electronic triggers can help detect specific situations indicative of error or delay (eg, patient not on precautions gets switched to precautions during a hospitalization; absence of follow-up on abnormal tests).19
Learning systems—both within and across hospitals—should continue to share diagnostic challenges, the most up-to-date information, and best practices/protocols, and identify opportunities for improvement together. Many hospitals are having virtual grand rounds, journals are rapidly sharing new information via open access, regional and national cross-organizational and multidisciplinary learning networks of various groups have emerged (such as networks of oncologists, infectious disease specialists, and hospitalists), and new and transparent communication channels have developed between state and local health departments, government leaders, health systems, and the public. These forums should discuss emerging knowledge on diagnosis and strategies for risk reduction, many of which will unfold over the next few months.
State/Federal Policies and Regulations
While there is progress, additional challenges with accessibility, accuracy and performance of testing should be addressed at a national level. Guidance is needed on which asymptomatic people should be tested, both within and outside hospitals. Standardized metrics should be developed to monitor diagnostic performance and outcomes and evaluate how COVID-19 diagnosis errors affect different demographics. For instance, black and Hispanic individuals are disproportionately represented in COVID-19 cases and deaths, so metrics could be further stratified by race and ethnicity to ensure that we can understand and eliminate inequities, such as lack of access to care or testing.20
CONCLUSION
Clinicians must be provided with both cognitive and system support so they can do what they do best—diagnose and treat patients and save lives. Intermittent epidemic spikes based on location and season, including a potentially bigger spike of cases later this year, are now projected. Risks and recommendations discussed herein should therefore be rapidly shared to help redesign and strengthen the work system and protect patients from preventable diagnosis-related harm.
Disclaimer
The views expressed in this article do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
1. Singh H, Graber ML. Improving diagnosis in health care—the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. https://doi.org/10.1056/nejmp1512241.
2. Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety [online first]. BMJ Qual Saf. 2020. https://doi.org/10.1136/bmjqs-2019-010110.
3. West CP, Montori VM, Sampathkumar P. COVID-19 testing: the threat of false-negative results [online first]. Mayo Clin Proc. 2020. https://doi.org/10.1016/j.mayocp.2020.04.004.
4. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6771.
5. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620.
6. Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence [online first]. Circulation. 2020. https://doi.org/10.1161/circulationaha.120.047430.
7. Cha AE. Young and middle-aged people, barely sick with COVID-19, are dying of strokes. Washington Post. April 25, 2020. https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/. Accessed April 27, 2020.
8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [online first]. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
9. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [online first]. N Engl J Med. 2020 https://doi.org/10.1056/NEJMc2014816.
10. Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care [online first]. Lancet Oncol. 2020. https://doi.org/10.1016/s1470-2045(20)30242-4.
11. Meyer AN, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173(21):1952-1958. https://doi.org/10.1001/jamainternmed.2013.10081.
12. Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290(14):1899-1905. https://doi.org/10.1001/jama.290.14.1899.
13. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-110. https://doi.org/10.1136/bmjqs-2014-003675.
14. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual Care [online first]. J Am Med Inform Assoc. 2020. https://doi.org/10.1093/jamia/ocaa067.
15. Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296-304. https://doi.org/10.1177/2374373518803617.
16. Singh H, Zwaan L. Web Exclusives. Annals for Hospitalists Inpatient Notes – reducing diagnostic error – a new horizon of opportunities for hospital medicine. Ann Intern Med. 2016;165(8):HO2-HO4. https://doi.org/10.7326/m16-2042.
17. Wu AW, Connors C, Everly GS Jr. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. 2020. https://doi.org/10.7326/m20-1236.
18. Singh H, Bradford A, Goeschel C. Operational Measurement of Diagnostic Safety: State of the Science. Rockville, MD: Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/topics/state-of-science.pdf. Accessed May 10, 2020.
19. Murphy DR, Meyer AN, Sittig DF, Meeks DW, Thomas EJ, Singh H. Application of electronic trigger tools to identify targets for improving diagnostic safety. BMJ Qual Saf. 2019;28(2):151-159. https://doi.org/10.1136/bmjqs-2018-008086.
20. Owen WF, Carmona R, Pomeroy C. Failing another national stress test on health disparities [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547.
As the death toll from the coronavirus disease 2019 (COVID-19) pandemic rapidly increases, the need to make a timely and accurate diagnosis has never been greater. Even before the pandemic, diagnostic errors (ie, missed, delayed, and incorrect diagnoses) had been one of the leading contributors to harm in health care.1 The COVID-19 pandemic is likely to increase the risk of such errors for several reasons. The disease itself is new and knowledge of its clinical manifestations is still evolving. Both physical and psychological safety of clinicians and health system capacity are compromised and can affect clinical decision-making.2 Situational factors such as staffing shortages and workarounds are more common, and clinicians in certain geographic areas are experiencing epic levels of stress, fatigue, and burnout. Finally, decisions in busy, chaotic and time-pressured healthcare systems with disrupted and/or newly designed care processes will be error prone.1
Based on emerging literature and collaborative discussions across the globe, we propose a new typology of diagnostic errors of concern in the COVID-19 era (Table). These errors span the entire continuum of care and have both systems-based and cognitive origins. While some errors arise from previously described clinical reasoning fallacies, others are unique to the pandemic. We provide a user-friendly nomenclature while describing eight types of diagnostic errors and highlight mitigation strategies to reduce potential preventable harm caused by those errors.
TYPES OF ANTICIPATED DIAGNOSTIC ERRORS
The classic COVID-19 presentation of a febrile respiratory illness warrants confirmatory testing, but testing may not be available or produce a false-negative result, leading to an error we termed “Classic.” In the United States, efforts to develop and implement testing protocols are still evolving. There is wide local and regional variation in type and availability of tests, as well as accessibility of information regarding test performance characteristics or diagnostic yield.3 Test results that are false negatives or testing that is not performed can lead to delayed diagnosis of the disease, as well as continued spread.
Testing is similarly relevant when patients present with unusual or nonrespiratory symptoms. Both predominantly olfactory4 and gastrointestinal manifestations5 have now been described, and mysterious new associations, such as multisystem inflammatory syndromes, continue to emerge. A failure to recognize atypical presentations and associations, either because of testing problems or knowledge gaps, could lead to overlooking underlying COVID-19 diagnosis, an error we termed “Anomalous.”
Another error emerging in the pandemic is mislabeling patients who do not have COVID-19 as having the disease, particularly those with respiratory symptoms. This usually occurs in absence of testing in an overwhelmed health system with limited capacity to test or treat (eg, clinicians just assume it must be COVID-19 when the test is not available). This type of labeling error, called “Anchor,” introduces the risk of missing other respiratory infections such as bacterial sinusitis and pneumonia, as well as nonrespiratory conditions.
In patients with known COVID-19, a second underlying or concurrent condition may be missed, an error we termed “Secondary.” For instance, reports of coagulopathy-related pulmonary embolism6 and strokes in young patients with minimal symptoms7 have emerged just recently. Respiratory compromise may be mistakenly attributed to COVID-19 rather than looking for a new source of worsening, such as pulmonary embolism. Similarly, clinicians may not recognize subtle stroke symptoms in patients who were otherwise feeling well at home. Such cognitive errors will likely increase as it becomes harder for clinicians or health systems to keep up with new knowledge.
Collateral effects of the COVID-19 pandemic are also emerging. For instance, patients with symptoms of new acute conditions may be unwilling to visit acute care for evaluation because of infection risk, an error we termed “Acute Collateral.” Concerns are already being raised that patients with acute myocardial infarction8 and stroke9 are not coming in for evaluation. Similarly, there may be delays in diagnosis of important ambulatory conditions, including cancer,10 when appointments or elective procedures are canceled (“Chronic Collateral”). In the United Kingdom, referrals under the 2-week wait system–in which suspected cancer patients referred by general practitioners are seen within 2-weeks–fell by 70% over March to April, 2020.
Diagnosis of non–COVID-19 patients coming into the hospital may also be affected because of the understandably heightened state of attention to COVID-19 patients, capacity, and staffing issues, an error we termed “Strain.” Physicians, including surgeons, pediatricians, and radiologists, have been “redeployed” into acute care medical specialties. Cognitive errors increase when clinicians in new roles face unfamiliar situations and disease manifestations. Although these clinicians may be highly experienced previously, they may have insufficient skills and experience in their new roles and may not feel comfortable asking for guidance.11
Lastly, clinicians are increasingly using intermediary mechanisms, such as PPE and telemedicine technologies, to interact with patients. This is new for both parties and could introduce new types of errors, which we termed “Unintended.” Furthermore, interactions mediated via telemedicine technologies or PPE, as well as PPE conservation measures such as reduced room entries and e-consultation, may reduce the ability of even well-trained clinicians to take effective histories, perform physical exams, and monitor symptoms. In fact, infection-prevention isolation has been shown to put patients at risk of preventable adverse events in hospitalized patients.12
SPECIFIC MITIGATION STRATEGIES
There are many strategies that health systems could deploy to try to minimize these eight types of diagnostic errors. We organize mitigation strategies using the Safer Dx framework, which proposes sociotechnical approaches (ie, both technology and other systems-based approaches) to reduce diagnostic error.13
Technology for Cognitive Support
Up-to-date electronic decision support is needed to optimize test interpretation. Technology can also help scale and facilitate rapid adoption of standardized safety practices and protocols to address emerging risks areas. For instance, there are early efforts to create, implement, and disseminate smart algorithms to predict risks of non–COVID-19 diagnoses such as venous thromboembolism, patient transfer protocols on how best to reduce the burden at overstressed hospitals, protocols to triage rescheduling of elective procedures based on potential risk as determined from data in the electronic health record, new rules for creating outreach to patients who have missed appointments to prevent delays in their evaluation and diagnosis, and triage protocols and follow-up systems to optimize telemedicine.14
Optimized Workflow and Communication
When in-person contact is limited, specific practices (eg, providing patients with iPads, use of reflective listening, and use of optimal nonverbal communication strategies such as eye-contact) can still facilitate comprehensive discussions with patients and families about symptoms and encourage them to speak up if and when they have concerns.15 For patients reached through telemedicine, follow-up appointments and surveys should be done to ensure that symptoms and concerns have been addressed. For clinicians working in new clinical areas unfamiliar to them (eg, surgeons on medical floors, hospitalists in ICUs), buddy systems can pair these clinicians with more experienced clinicians to make it easier for them to ask for help. Visual aids, decision support, and reliable error-prevention resources can also be helpful.16
People-Focused Interventions
Some clinicians are used to practicing solo, but this is the time to start “diagnostic huddles” for discussion of challenging cases with symptoms that are unusual or not improving as expected or for determining whether anything has been missed. In addition to encouraging patients to use reliable digital tools for self-triage, outreach to patients and the public must also advise them (with the help of public health authorities and the media) to seek medical assistance for certain important conditions such as acute myocardial infarction and stroke.
Organizational Strategies
Fundamental safety strategies must be ensured. First, it is critical to have a strong safety culture in which staff feel empowered to speak up, ask questions or ask for help, and report concerns without fear of repercussions or judgement. Culture can take years to develop, but due to rapidly changing circumstances in a crisis, there are ways for healthcare leaders to create changes more quickly. In addition to having daily huddles, leaders should be visible and communicate clearly about the behaviors and norms they are supporting. In particular, frequent leadership rounding (either virtually or in person)—during which leaders ask questions and encourage discussions of concerns in a supportive way—can foster the kind of culture that is needed. All organizations should implement peer support, counseling, limits on hours worked, and other support strategies for all clinicians to minimize the fatigue, stress, and anxiety that can impair cognitive function.17
Organizations must also be able to identify these errors to help understand root causes and prioritize interventions.18 For example, streamlined reporting systems that use apps and hotlines could be developed quickly to ensure that clinicians and patients/families can easily report these errors. Electronic triggers can help detect specific situations indicative of error or delay (eg, patient not on precautions gets switched to precautions during a hospitalization; absence of follow-up on abnormal tests).19
Learning systems—both within and across hospitals—should continue to share diagnostic challenges, the most up-to-date information, and best practices/protocols, and identify opportunities for improvement together. Many hospitals are having virtual grand rounds, journals are rapidly sharing new information via open access, regional and national cross-organizational and multidisciplinary learning networks of various groups have emerged (such as networks of oncologists, infectious disease specialists, and hospitalists), and new and transparent communication channels have developed between state and local health departments, government leaders, health systems, and the public. These forums should discuss emerging knowledge on diagnosis and strategies for risk reduction, many of which will unfold over the next few months.
State/Federal Policies and Regulations
While there is progress, additional challenges with accessibility, accuracy and performance of testing should be addressed at a national level. Guidance is needed on which asymptomatic people should be tested, both within and outside hospitals. Standardized metrics should be developed to monitor diagnostic performance and outcomes and evaluate how COVID-19 diagnosis errors affect different demographics. For instance, black and Hispanic individuals are disproportionately represented in COVID-19 cases and deaths, so metrics could be further stratified by race and ethnicity to ensure that we can understand and eliminate inequities, such as lack of access to care or testing.20
CONCLUSION
Clinicians must be provided with both cognitive and system support so they can do what they do best—diagnose and treat patients and save lives. Intermittent epidemic spikes based on location and season, including a potentially bigger spike of cases later this year, are now projected. Risks and recommendations discussed herein should therefore be rapidly shared to help redesign and strengthen the work system and protect patients from preventable diagnosis-related harm.
Disclaimer
The views expressed in this article do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
As the death toll from the coronavirus disease 2019 (COVID-19) pandemic rapidly increases, the need to make a timely and accurate diagnosis has never been greater. Even before the pandemic, diagnostic errors (ie, missed, delayed, and incorrect diagnoses) had been one of the leading contributors to harm in health care.1 The COVID-19 pandemic is likely to increase the risk of such errors for several reasons. The disease itself is new and knowledge of its clinical manifestations is still evolving. Both physical and psychological safety of clinicians and health system capacity are compromised and can affect clinical decision-making.2 Situational factors such as staffing shortages and workarounds are more common, and clinicians in certain geographic areas are experiencing epic levels of stress, fatigue, and burnout. Finally, decisions in busy, chaotic and time-pressured healthcare systems with disrupted and/or newly designed care processes will be error prone.1
Based on emerging literature and collaborative discussions across the globe, we propose a new typology of diagnostic errors of concern in the COVID-19 era (Table). These errors span the entire continuum of care and have both systems-based and cognitive origins. While some errors arise from previously described clinical reasoning fallacies, others are unique to the pandemic. We provide a user-friendly nomenclature while describing eight types of diagnostic errors and highlight mitigation strategies to reduce potential preventable harm caused by those errors.
TYPES OF ANTICIPATED DIAGNOSTIC ERRORS
The classic COVID-19 presentation of a febrile respiratory illness warrants confirmatory testing, but testing may not be available or produce a false-negative result, leading to an error we termed “Classic.” In the United States, efforts to develop and implement testing protocols are still evolving. There is wide local and regional variation in type and availability of tests, as well as accessibility of information regarding test performance characteristics or diagnostic yield.3 Test results that are false negatives or testing that is not performed can lead to delayed diagnosis of the disease, as well as continued spread.
Testing is similarly relevant when patients present with unusual or nonrespiratory symptoms. Both predominantly olfactory4 and gastrointestinal manifestations5 have now been described, and mysterious new associations, such as multisystem inflammatory syndromes, continue to emerge. A failure to recognize atypical presentations and associations, either because of testing problems or knowledge gaps, could lead to overlooking underlying COVID-19 diagnosis, an error we termed “Anomalous.”
Another error emerging in the pandemic is mislabeling patients who do not have COVID-19 as having the disease, particularly those with respiratory symptoms. This usually occurs in absence of testing in an overwhelmed health system with limited capacity to test or treat (eg, clinicians just assume it must be COVID-19 when the test is not available). This type of labeling error, called “Anchor,” introduces the risk of missing other respiratory infections such as bacterial sinusitis and pneumonia, as well as nonrespiratory conditions.
In patients with known COVID-19, a second underlying or concurrent condition may be missed, an error we termed “Secondary.” For instance, reports of coagulopathy-related pulmonary embolism6 and strokes in young patients with minimal symptoms7 have emerged just recently. Respiratory compromise may be mistakenly attributed to COVID-19 rather than looking for a new source of worsening, such as pulmonary embolism. Similarly, clinicians may not recognize subtle stroke symptoms in patients who were otherwise feeling well at home. Such cognitive errors will likely increase as it becomes harder for clinicians or health systems to keep up with new knowledge.
Collateral effects of the COVID-19 pandemic are also emerging. For instance, patients with symptoms of new acute conditions may be unwilling to visit acute care for evaluation because of infection risk, an error we termed “Acute Collateral.” Concerns are already being raised that patients with acute myocardial infarction8 and stroke9 are not coming in for evaluation. Similarly, there may be delays in diagnosis of important ambulatory conditions, including cancer,10 when appointments or elective procedures are canceled (“Chronic Collateral”). In the United Kingdom, referrals under the 2-week wait system–in which suspected cancer patients referred by general practitioners are seen within 2-weeks–fell by 70% over March to April, 2020.
Diagnosis of non–COVID-19 patients coming into the hospital may also be affected because of the understandably heightened state of attention to COVID-19 patients, capacity, and staffing issues, an error we termed “Strain.” Physicians, including surgeons, pediatricians, and radiologists, have been “redeployed” into acute care medical specialties. Cognitive errors increase when clinicians in new roles face unfamiliar situations and disease manifestations. Although these clinicians may be highly experienced previously, they may have insufficient skills and experience in their new roles and may not feel comfortable asking for guidance.11
Lastly, clinicians are increasingly using intermediary mechanisms, such as PPE and telemedicine technologies, to interact with patients. This is new for both parties and could introduce new types of errors, which we termed “Unintended.” Furthermore, interactions mediated via telemedicine technologies or PPE, as well as PPE conservation measures such as reduced room entries and e-consultation, may reduce the ability of even well-trained clinicians to take effective histories, perform physical exams, and monitor symptoms. In fact, infection-prevention isolation has been shown to put patients at risk of preventable adverse events in hospitalized patients.12
SPECIFIC MITIGATION STRATEGIES
There are many strategies that health systems could deploy to try to minimize these eight types of diagnostic errors. We organize mitigation strategies using the Safer Dx framework, which proposes sociotechnical approaches (ie, both technology and other systems-based approaches) to reduce diagnostic error.13
Technology for Cognitive Support
Up-to-date electronic decision support is needed to optimize test interpretation. Technology can also help scale and facilitate rapid adoption of standardized safety practices and protocols to address emerging risks areas. For instance, there are early efforts to create, implement, and disseminate smart algorithms to predict risks of non–COVID-19 diagnoses such as venous thromboembolism, patient transfer protocols on how best to reduce the burden at overstressed hospitals, protocols to triage rescheduling of elective procedures based on potential risk as determined from data in the electronic health record, new rules for creating outreach to patients who have missed appointments to prevent delays in their evaluation and diagnosis, and triage protocols and follow-up systems to optimize telemedicine.14
Optimized Workflow and Communication
When in-person contact is limited, specific practices (eg, providing patients with iPads, use of reflective listening, and use of optimal nonverbal communication strategies such as eye-contact) can still facilitate comprehensive discussions with patients and families about symptoms and encourage them to speak up if and when they have concerns.15 For patients reached through telemedicine, follow-up appointments and surveys should be done to ensure that symptoms and concerns have been addressed. For clinicians working in new clinical areas unfamiliar to them (eg, surgeons on medical floors, hospitalists in ICUs), buddy systems can pair these clinicians with more experienced clinicians to make it easier for them to ask for help. Visual aids, decision support, and reliable error-prevention resources can also be helpful.16
People-Focused Interventions
Some clinicians are used to practicing solo, but this is the time to start “diagnostic huddles” for discussion of challenging cases with symptoms that are unusual or not improving as expected or for determining whether anything has been missed. In addition to encouraging patients to use reliable digital tools for self-triage, outreach to patients and the public must also advise them (with the help of public health authorities and the media) to seek medical assistance for certain important conditions such as acute myocardial infarction and stroke.
Organizational Strategies
Fundamental safety strategies must be ensured. First, it is critical to have a strong safety culture in which staff feel empowered to speak up, ask questions or ask for help, and report concerns without fear of repercussions or judgement. Culture can take years to develop, but due to rapidly changing circumstances in a crisis, there are ways for healthcare leaders to create changes more quickly. In addition to having daily huddles, leaders should be visible and communicate clearly about the behaviors and norms they are supporting. In particular, frequent leadership rounding (either virtually or in person)—during which leaders ask questions and encourage discussions of concerns in a supportive way—can foster the kind of culture that is needed. All organizations should implement peer support, counseling, limits on hours worked, and other support strategies for all clinicians to minimize the fatigue, stress, and anxiety that can impair cognitive function.17
Organizations must also be able to identify these errors to help understand root causes and prioritize interventions.18 For example, streamlined reporting systems that use apps and hotlines could be developed quickly to ensure that clinicians and patients/families can easily report these errors. Electronic triggers can help detect specific situations indicative of error or delay (eg, patient not on precautions gets switched to precautions during a hospitalization; absence of follow-up on abnormal tests).19
Learning systems—both within and across hospitals—should continue to share diagnostic challenges, the most up-to-date information, and best practices/protocols, and identify opportunities for improvement together. Many hospitals are having virtual grand rounds, journals are rapidly sharing new information via open access, regional and national cross-organizational and multidisciplinary learning networks of various groups have emerged (such as networks of oncologists, infectious disease specialists, and hospitalists), and new and transparent communication channels have developed between state and local health departments, government leaders, health systems, and the public. These forums should discuss emerging knowledge on diagnosis and strategies for risk reduction, many of which will unfold over the next few months.
State/Federal Policies and Regulations
While there is progress, additional challenges with accessibility, accuracy and performance of testing should be addressed at a national level. Guidance is needed on which asymptomatic people should be tested, both within and outside hospitals. Standardized metrics should be developed to monitor diagnostic performance and outcomes and evaluate how COVID-19 diagnosis errors affect different demographics. For instance, black and Hispanic individuals are disproportionately represented in COVID-19 cases and deaths, so metrics could be further stratified by race and ethnicity to ensure that we can understand and eliminate inequities, such as lack of access to care or testing.20
CONCLUSION
Clinicians must be provided with both cognitive and system support so they can do what they do best—diagnose and treat patients and save lives. Intermittent epidemic spikes based on location and season, including a potentially bigger spike of cases later this year, are now projected. Risks and recommendations discussed herein should therefore be rapidly shared to help redesign and strengthen the work system and protect patients from preventable diagnosis-related harm.
Disclaimer
The views expressed in this article do not represent the views of the U.S. Department of Veterans Affairs or the United States government.
1. Singh H, Graber ML. Improving diagnosis in health care—the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. https://doi.org/10.1056/nejmp1512241.
2. Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety [online first]. BMJ Qual Saf. 2020. https://doi.org/10.1136/bmjqs-2019-010110.
3. West CP, Montori VM, Sampathkumar P. COVID-19 testing: the threat of false-negative results [online first]. Mayo Clin Proc. 2020. https://doi.org/10.1016/j.mayocp.2020.04.004.
4. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6771.
5. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620.
6. Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence [online first]. Circulation. 2020. https://doi.org/10.1161/circulationaha.120.047430.
7. Cha AE. Young and middle-aged people, barely sick with COVID-19, are dying of strokes. Washington Post. April 25, 2020. https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/. Accessed April 27, 2020.
8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [online first]. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
9. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [online first]. N Engl J Med. 2020 https://doi.org/10.1056/NEJMc2014816.
10. Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care [online first]. Lancet Oncol. 2020. https://doi.org/10.1016/s1470-2045(20)30242-4.
11. Meyer AN, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173(21):1952-1958. https://doi.org/10.1001/jamainternmed.2013.10081.
12. Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290(14):1899-1905. https://doi.org/10.1001/jama.290.14.1899.
13. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-110. https://doi.org/10.1136/bmjqs-2014-003675.
14. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual Care [online first]. J Am Med Inform Assoc. 2020. https://doi.org/10.1093/jamia/ocaa067.
15. Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296-304. https://doi.org/10.1177/2374373518803617.
16. Singh H, Zwaan L. Web Exclusives. Annals for Hospitalists Inpatient Notes – reducing diagnostic error – a new horizon of opportunities for hospital medicine. Ann Intern Med. 2016;165(8):HO2-HO4. https://doi.org/10.7326/m16-2042.
17. Wu AW, Connors C, Everly GS Jr. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. 2020. https://doi.org/10.7326/m20-1236.
18. Singh H, Bradford A, Goeschel C. Operational Measurement of Diagnostic Safety: State of the Science. Rockville, MD: Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/topics/state-of-science.pdf. Accessed May 10, 2020.
19. Murphy DR, Meyer AN, Sittig DF, Meeks DW, Thomas EJ, Singh H. Application of electronic trigger tools to identify targets for improving diagnostic safety. BMJ Qual Saf. 2019;28(2):151-159. https://doi.org/10.1136/bmjqs-2018-008086.
20. Owen WF, Carmona R, Pomeroy C. Failing another national stress test on health disparities [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547.
1. Singh H, Graber ML. Improving diagnosis in health care—the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. https://doi.org/10.1056/nejmp1512241.
2. Isbell LM, Tager J, Beals K, Liu G. Emotionally evocative patients in the emergency department: a mixed methods investigation of providers’ reported emotions and implications for patient safety [online first]. BMJ Qual Saf. 2020. https://doi.org/10.1136/bmjqs-2019-010110.
3. West CP, Montori VM, Sampathkumar P. COVID-19 testing: the threat of false-negative results [online first]. Mayo Clin Proc. 2020. https://doi.org/10.1016/j.mayocp.2020.04.004.
4. Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6771.
5. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620.
6. Poissy J, Goutay J, Caplan M, et al. Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence [online first]. Circulation. 2020. https://doi.org/10.1161/circulationaha.120.047430.
7. Cha AE. Young and middle-aged people, barely sick with COVID-19, are dying of strokes. Washington Post. April 25, 2020. https://www.washingtonpost.com/health/2020/04/24/strokes-coronavirus-young-patients/. Accessed April 27, 2020.
8. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic [online first]. J Am Coll Cardiol. 2020. https://doi.org/10.1016/j.jacc.2020.04.011.
9. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States [online first]. N Engl J Med. 2020 https://doi.org/10.1056/NEJMc2014816.
10. Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care [online first]. Lancet Oncol. 2020. https://doi.org/10.1016/s1470-2045(20)30242-4.
11. Meyer AN, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173(21):1952-1958. https://doi.org/10.1001/jamainternmed.2013.10081.
12. Stelfox HT, Bates DW, Redelmeier DA. Safety of patients isolated for infection control. JAMA. 2003;290(14):1899-1905. https://doi.org/10.1001/jama.290.14.1899.
13. Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf. 2015;24(2):103-110. https://doi.org/10.1136/bmjqs-2014-003675.
14. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual Care [online first]. J Am Med Inform Assoc. 2020. https://doi.org/10.1093/jamia/ocaa067.
15. Pappas Y, Vseteckova J, Mastellos N, Greenfield G, Randhawa G. Diagnosis and decision-making in telemedicine. J Patient Exp. 2019;6(4):296-304. https://doi.org/10.1177/2374373518803617.
16. Singh H, Zwaan L. Web Exclusives. Annals for Hospitalists Inpatient Notes – reducing diagnostic error – a new horizon of opportunities for hospital medicine. Ann Intern Med. 2016;165(8):HO2-HO4. https://doi.org/10.7326/m16-2042.
17. Wu AW, Connors C, Everly GS Jr. COVID-19: peer support and crisis communication strategies to promote institutional resilience. Ann Intern Med. 2020. https://doi.org/10.7326/m20-1236.
18. Singh H, Bradford A, Goeschel C. Operational Measurement of Diagnostic Safety: State of the Science. Rockville, MD: Agency for Healthcare Research and Quality; 2020. https://www.ahrq.gov/sites/default/files/wysiwyg/topics/state-of-science.pdf. Accessed May 10, 2020.
19. Murphy DR, Meyer AN, Sittig DF, Meeks DW, Thomas EJ, Singh H. Application of electronic trigger tools to identify targets for improving diagnostic safety. BMJ Qual Saf. 2019;28(2):151-159. https://doi.org/10.1136/bmjqs-2018-008086.
20. Owen WF, Carmona R, Pomeroy C. Failing another national stress test on health disparities [online first]. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547.
© 2020 Society of Hospital Medicine
Focused Ethnography of Diagnosis in Academic Medical Centers
Diagnostic error—defined as a failure to establish an accurate and timely explanation of the patient’s health problem—is an important source of patient harm.1 Data suggest that all patients will experience at least 1 diagnostic error in their lifetime.2-4 Not surprisingly, diagnostic errors are among the leading categories of paid malpractice claims in the United States.5
Despite diagnostic errors being morbid and sometimes deadly in the hospital,6,7 little is known about how residents and learners approach diagnostic decision making. Errors in diagnosis are believed to stem from cognitive or system failures,8 with errors in cognition believed to occur due to rapid, reflexive thinking operating in the absence of a more analytical, deliberate process. System-based problems (eg, lack of expert availability, technology barriers, and access to data) have also been cited as contributors.9 However, whether and how these apply to trainees is not known.
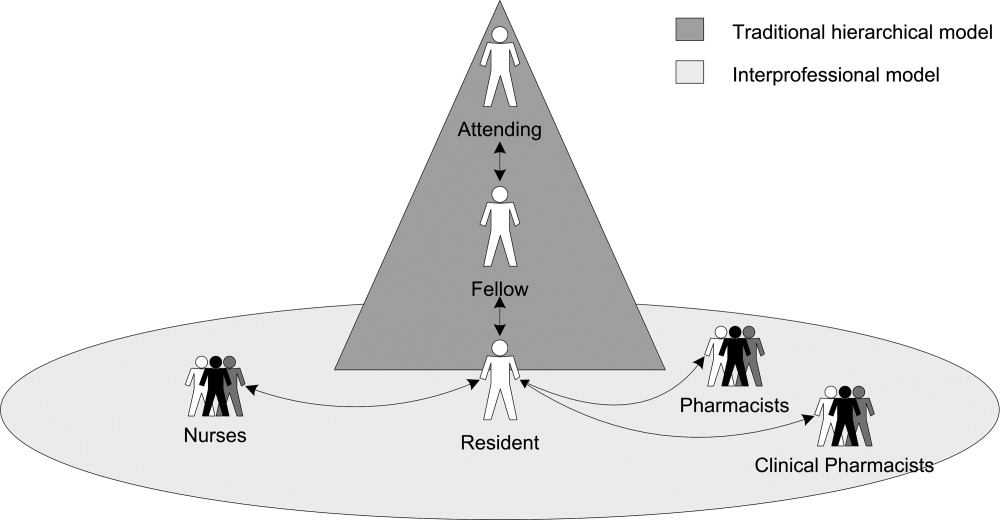
Therefore, we conducted a focused ethnography of inpatient medicine teams (ie, attendings, residents, interns, and medical students) in 2 affiliated teaching hospitals, aiming to (a) observe the process of diagnosis by trainees and (b) identify methods to improve the diagnostic process and prevent errors.
METHODS
We designed a multimethod, focused ethnographic study to examine diagnostic decision making in hospital settings.10,11 In contrast to anthropologic ethnographies that study entire fields using open-ended questions, our study was designed to examine the process of diagnosis from the perspective of clinicians engaged in this activity.11 This approach allowed us to capture diagnostic decisions and cognitive and system-based factors in a manner currently lacking in the literature.12
Setting and Participants
Between January 2016 and May 2016, we observed the members of four inpatient internal medicine teaching teams at 2 affiliated teaching hospitals. We purposefully selected teaching teams for observation because they are the primary model of care in academic settings and we have expertise in carrying out similar studies.13,14 Teaching teams typically consisted of a medical attending (senior-level physician), 1 senior resident (a second- or third-year postgraduate trainee), two interns (a trainee in their first postgraduate year), and two to four medical students. Teams were selected at random using existing schedules and followed Monday to Friday so as to permit observation of work on call and noncall days. Owing to manpower limitations, weekend and night shifts were not observed. However, overnight events were captured during morning rounds.
Most of the teams began rounds at 8:30 AM. Typically, rounds lasted for 90–120 min and concluded with a recap (ie, “running the list”) with a review of explicit plans for patients after they had been evaluated by the attending. This discussion often occurred in the team rooms, with the attending leading the discussion with the trainees.
Data Collection
A multidisciplinary team, including clinicians (eg, physicians, nurses), nonclinicians (eg, qualitative researchers, social scientists), and healthcare engineers, conducted the observations. We observed preround activities of interns and residents before arrival of the attending (7:00 AM - 8:30 AM), followed by morning rounds with the entire team, and afternoon work that included senior residents, interns, and students.
To capture multiple aspects of the diagnostic process, we collected data using field notes modeled on components of the National Academy of Science model for diagnosis (Appendix).1,15 This model encompasses phases of the diagnostic process (eg, data gathering, integration, formulation of a working diagnosis, treatment delivery, and outcomes) and the work system (team members, organization, technology and tools, physical environment, tasks).
Focus Groups and Interviews
At the end of weekly observations, we conducted focus groups with the residents and one-on- one interviews with the attendings. Focus groups with the residents were conducted to encourage a group discussion about the diagnostic process. Separate interviews with the attendings were performed to ensure that power differentials did not influence discussions. During focus groups, we specifically asked about challenges and possible solutions to improve diagnosis. Experienced qualitative methodologists (J.F., M.H., M.Q.) used semistructured interview guides for discussions (Appendix).
Data Analysis
After aggregating and reading the data, three reviewers (V.C., S.K., S.S.) began inductive analysis by handwriting notes and initial reflective thoughts to create preliminary codes. Multiple team members then reread the original field notes and the focus group/interview data to refine the preliminary codes and develop additional codes. Next, relationships between codes were identified and used to develop key themes. Triangulation of data collected from observations and interview/focus group sessions was carried out to compare data that we surmised with data that were verbalized by the team. The developed themes were discussed as a group to ensure consistency of major findings.
Ethical and Regulatory Oversight
This study was reviewed and approved by the Institutional Review Boards at the University of Michigan Health System (HUM-00106657) and the VA Ann Arbor Healthcare System (1-2016-010040).
RESULTS
Four teaching teams (4 attendings, 4 senior residents, 9 interns, and 14 medical students) were observed over 33 distinct shifts and 168 hours. Observations included morning rounds (96 h), postround call days (52 h), and postround non-call days (20 h). Morning rounds lasted an average of 127 min (range: 48-232 min) and included an average of 9 patients (range: 4-16 patients).
Themes Regarding the Diagnostic Process
We identified the following 4 primary themes related to the diagnostic process in teaching hospitals: (1) diagnosis is a social phenomenon; (2) data necessary to make diagnoses are fragmented; (3) distractions undermine the diagnostic process; and (4) time pressures interfere with diagnostic decision making (Appendix Table 1).
(1) Diagnosis is a Social Phenomenon.
Team members viewed the process of diagnosis as a social exchange of facts, findings, and strategies within a defined structure. The opportunity to discuss impressions with others was valued as a means to share, test, and process assumptions.
“Rounds are the most important part of the process. That is where we make most decisions in a collective, collaborative way with the attending present. We bounce ideas off each other.” (Intern)
Typical of social processes, variations based on time of day and schedule were observed. For instance, during call days, learners gathered data and formed working diagnosis and treatment plans with minimal attending interaction. This separation of roles and responsibilities introduced a hierarchy within diagnosis as follows:
“The interns would not call me first; they would talk to the senior resident and then if the senior thought he should chat with me, then they would call. But for the most part, they gather information and come up with the plan.” (Attending).
The work system was suited to facilitate social interactions. For instance, designated rooms (with team members informally assigned to a computer) provided physical proximity of the resident to interns and medical students. In this space, numerous informal discussions between team members (eg, “What do you think about this test?” “I’m not sure what to do about this finding.” “Should I call a [consult] on this patient?”) were observed. Although proximity to each other was viewed as beneficial, dangers to the social nature of diagnosis in the form of anchoring (ie, a cognitive bias where emphasis is placed on the first piece of data)16 were also mentioned. Similarly, the paradox associated with social proof (ie, the pressure to assume conformity within a group) was also observed as disagreement between team members and attendings rarely occurred during observations.
“I mean, they’re the attending, right? It’s hard to argue with them when they want a test or something done. When I do push back, it’s rare that others will support me–so it’s usually me and the attending.” (Resident)
“I would push back if I think it’s really bad for the patient or could cause harm–but the truth is, it doesn’t happen much.” (Intern)
(2) Data Necessary to Make Diagnoses are Fragmented
Team members universally cited fragmentation in data delivery, retrieval, and processing as a barrier to diagnosis. Team members indicated that test results might not be looked at or acted upon in a timely manner, and participants pointed to the electronic medical record as a source of this challenge.
“Before I knew about [the app for Epic], I would literally sit on the computer to get all the information we would need on rounds. Its key to making decisions. We often say we will do something, only to find the test result doesn’t support it–and then we’re back to square 1.” (Intern)
Information used by teams came from myriad sources (eg, patients, family members, electronic records) and from various settings (eg, emergency department, patient rooms, discussions with consultants). Additionally, test results often appeared without warning. Thus, availability of information was poorly aligned with clinical duties.
“They (the lab) will call us when a blood culture is positive or something is off. That is very helpful but it often comes later in the day, when we’re done with rounds.” (Resident)
The work system was highlighted as a key contributor to data fragmentation. Peculiarities of our electronic medical record (EMR) and how data were collected, stored, or presented were described as “frustrating,” and “unsafe,” by team members. Correspondingly, we frequently observed interns asking for assistance for tasks such as ordering tests or finding information despite being “trained” to use the EMR.
“People have to learn how to filter, how to recognize the most important points and link data streams together in terms of causality. But we assume they know where to find that information. It’s actually a very hard thing to do, for both the house staff and me.” (Attending)
(3) Distractions Undermine the Diagnostic Process
Distractions often created cognitive difficulties. For example, ambient noise and interruptions from neighbors working on other teams were cited as barriers to diagnosis. In addition, we observed several team members using headphones to drown out ambient noise while working on the computer.
“I know I shouldn’t do it (wear headphones), but I have no other way of turning down the noise so I can concentrate.” (Intern)
Similarly, the unpredictable nature and the volume of pages often interrupted thinking about diagnosis.
“Sometimes the pager just goes off all the time and (after making sure its not an urgent issue), I will just ignore it for a bit, especially if I am in the middle of something. It would be great if I could finish my thought process knowing I would not be interrupted.” (Resident)
To mitigate this problem, 1 attending described how he would proactively seek out nurses caring for his patients to “head off” questions (eg, “I will renew the restraints and medications this morning,” and “Is there anything you need in terms of orders for this patient that I can take care of now?”) that might lead to pages. Another resident described his approach as follows:
“I make it a point to tell the nurses where I will be hanging out and where they can find me if they have any questions. I tell them to come talk to me rather than page me since that will be less distracting.” (Resident).
Most of the interns described documentation work such as writing admission and progress notes in negative terms (“an academic exercise,” “part of the billing activity”). However, in the context of interruptions, some described this as helpful.
“The most valuable part of the thinking process was writing the assessment and plan because that’s actually my schema for all problems. It literally is the only time where I can sit and collect my thoughts to formulate a diagnosis and plan.” (Intern)
(4) Time Pressures Interfere With Diagnostic Decision Making
All team members spoke about the challenge of finding time for diagnosis during the workday. Often, they had to skip learning sessions for this purpose.
“They tell us we should go to morning report or noon conference but when I’m running around trying to get things done. I hate having to choose between my education and doing what’s best for the patient–but that’s often what it comes down to.” (Intern)
When specifically asked whether setting aside dedicated time to specifically review and formulate diagnoses would be valuable, respondents were uniformly enthusiastic. Team members described attentional conflicts as being the worst when “cross covering” other teams on call days, as their patient load effectively doubled during this time. Of note, cross-covering occurred when teams were also on call—and thus took them away from important diagnostic activities such as data gathering or synthesis for patients they were admitting.
“If you were to ever design a system where errors were likely–this is how you would design it: take a team with little supervision, double their patient load, keep them busy with new challenging cases and then ask questions about patients they know little about.” (Resident)
DISCUSSION
Although diagnostic errors have been called “the next frontier for patient safety,”17 little is known about the process, barriers, and facilitators to diagnosis in teaching hospitals. In this focused ethnography conducted at 2 academic medical centers, we identified multiple cognitive and system-level challenges and potential strategies to improve diagnosis from trainees engaged in this activity. Key themes identified by those we observed included the social nature of diagnosis, fragmented information delivery, constant distractions and interruptions, and time pressures. In turn, these insights allow us to generate strategies that can be applied to improve the diagnostic process in teaching hospitals.
Our study underscores the importance of social interactions in diagnosis. In contrast, most of the interventions to prevent diagnostic errors target individual providers through practices such as metacognition and “thinking about thinking.”18-20 These interventions are based on Daniel Kahnemann’s work on dual thought process. Type 1 thought processes are fast, subconscious, reflexive, largely intuitive, and more vulnerable to error. In contrast, Type 2 processes are slower, deliberate, analytic, and less prone to error.21 Although an individual’s Type 2 thought capacity is limited, a major goal of cognitive interventions is to encourage Type 2 over Type 1 thinking, an approach termed “de-biasing.”22-24 Unfortunately, cognitive interventions testing such approaches have suffered mixed results–perhaps because of lack of focus on collective wisdom or group thinking, which may be key to diagnosis from our findings.9,25 In this sense, morning rounds were a social gathering used to strategize and develop care plans, but with limited time to think about diagnosis.26 Introduction of defined periods for individuals to engage in diagnostic activities such as de-biasing (ie, asking “what else could this be)27 before or after rounds may provide an opportunity for reflection and improving diagnosis. In addition, embedding tools such as diagnosis expanders and checklists within these defined time slots28,29 may prove to be useful in reflecting on diagnosis and preventing diagnostic errors.
An unexpected yet important finding from this study were the challenges posed by distractions and the physical environment. Potentially maladaptive workarounds to these interruptions included use of headphones; more productive strategies included updating nurses with plans to avert pages and creating a list of activities to ensure that key tasks were not forgotten.30,31 Applying lessons from aviation, a focused effort to limit distractions during key portions of the day, might be worth considering for diagnostic safety.32 Similarly, improving the environment in which diagnosis occurs—including creating spaces that are quiet, orderly, and optimized for thinking—may be valuable.33Our study has limitations. First, our findings are limited to direct observations; we are thus unable to comment on how unobserved aspects of care (eg, cognitive processes) might have influenced our findings. Our observations of clinical care might also have introduced a Hawthorne effect. However, because we were closely integrated with teams and conducted focus groups to corroborate our assessments, we believe that this was not the case. Second, we did not identify diagnostic errors or link processes we observed to errors. Third, our approach is limited to 2 teaching centers, thereby limiting the generalizability of findings. Relatedly, we were only able to conduct observations during weekdays; differences in weekend and night resources might affect our insights.
The cognitive and system-based barriers faced by clinicians in teaching hospitals suggest that new methods to improve diagnosis are needed. Future interventions such as defined “time-outs” for diagnosis, strategies focused on limiting distractions, and methods to improve communication between team members are novel and have parallels in other industries. As challenges to quantify diagnostic errors abound,34 improving cognitive- and system-based factors via reflection through communication, concentration, and organization is necessary to improve medical decision making in academic medical centers.
Disclosures
None declared for all coauthors.
Funding
This project was supported by grant number P30HS024385 from the Agency for Healthcare Research and Quality. The funding source played no role in study design, data acquisition, analysis or decision to report these data. Dr. Chopra is supported by a career development award from the Agency of Healthcare Research and Quality (1-K08-HS022835-01). Dr. Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). Dr. Singh is partially supported by Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the Department of Veterans Affairs.
1. National Academies of Sciences, Engineering, and Medicine. 2015. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press. http://www.nap.edu/21794. Accessed November 1; 2016:2015. https://doi.org/10.17226/21794.
2. Schiff GD, Hasan O, Kim S, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med. 2009;169(20):1881-1887. http://dx.doi.org/10.1001/archinternmed.2009.333. PubMed
3. Sonderegger-Iseli K, Burger S, Muntwyler J, Salomon F. Diagnostic errors in three medical eras: A necropsy study. Lancet. 2000;355(9220):2027-2031. http://dx.doi.org/10.1016/S0140-6736(00)02349-7. PubMed
4. Winters B, Custer J, Galvagno SM Jr, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Qual Saf. 2012;21(11):894-902. http://dx.doi.org/10.1136/bmjqs-2012-000803. PubMed
5. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680. http://dx.doi.org/10.1136/bmjqs-2012-001550. PubMed
6. Graber M, Gordon R, Franklin N. Reducing diagnostic errors in medicine: what’s the goal? Acad Med. 2002;77(10):981-992. http://dx.doi.org/10.1097/00001888-200210000-00009. PubMed
7. Gupta A, Snyder A, Kachalia A, Flanders S, Saint S, Chopra V. Malpractice claims related to diagnostic errors in the hospital. BMJ Qual Saf. 2018;27(1):53-60. 10.1136/bmjqs-2017-006774. PubMed
8. van Noord I, Eikens MP, Hamersma AM, de Bruijne MC. Application of root cause analysis on malpractice claim files related to diagnostic failures. Qual Saf Health Care. 2010;19(6):e21. http://dx.doi.org/10.1136/qshc.2008.029801. PubMed
9. Croskerry P, Petrie DA, Reilly JB, Tait G. Deciding about fast and slow decisions. Acad Med. 2014;89(2):197-200. 10.1097/ACM.0000000000000121. PubMed
10. Higginbottom GM, Pillay JJ, Boadu NY. Guidance on performing focused ethnographies with an emphasis on healthcare research. Qual Rep. 2013;18(9):1-6. https://doi.org/10.7939/R35M6287P.
11. Savage J. Participative observation: standing in the shoes of others? Qual Health Res. 2000;10(3):324-339. http://dx.doi.org/10.1177/104973200129118471. PubMed
12. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: SAGE Publications; 2002.
13. Harrod M, Weston LE, Robinson C, Tremblay A, Greenstone CL, Forman J. “It goes beyond good camaraderie”: A qualitative study of the process of becoming an interprofessional healthcare “teamlet.” J Interprof Care. 2016;30(3):295-300. http://dx.doi.org/10.3109/13561820.2015.1130028. PubMed
14. Houchens N, Harrod M, Moody S, Fowler KE, Saint S. Techniques and behaviors associated with exemplary inpatient general medicine teaching: an exploratory qualitative study. J Hosp Med. 2017;12(7):503-509. http://dx.doi.org/10.12788/jhm.2763. PubMed
15. Mulhall A. In the field: notes on observation in qualitative research. J Adv Nurs. 2003;41(3):306-313. http://dx.doi.org/10.1046/j.1365-2648.2003.02514.x. PubMed
16. Zwaan L, Monteiro S, Sherbino J, Ilgen J, Howey B, Norman G. Is bias in the eye of the beholder? A vignette study to assess recognition of cognitive biases in clinical case workups. BMJ Qual Saf. 2017;26(2):104-110. http://dx.doi.org/10.1136/bmjqs-2015-005014. PubMed
17. Singh H, Graber ML. Improving diagnosis in health care--the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. http://dx.doi.org/10.1056/NEJMp1512241. PubMed
18. Croskerry P. From mindless to mindful practice--cognitive bias and clinical decision making. N Engl J Med. 2013;368(26):2445-2448. http://dx.doi.org/10.1056/NEJMp1303712. PubMed
19. van den Berge K, Mamede S. Cognitive diagnostic error in internal medicine. Eur J Intern Med. 2013;24(6):525-529. http://dx.doi.org/10.1016/j.ejim.2013.03.006. PubMed
20. Norman G, Sherbino J, Dore K, et al. The etiology of diagnostic errors: A controlled trial of system 1 versus system 2 reasoning. Acad Med. 2014;89(2):277-284. 10.1097/ACM.0000000000000105 PubMed
21. Dhaliwal G. Premature closure? Not so fast. BMJ Qual Saf. 2017;26(2):87-89. http://dx.doi.org/10.1136/bmjqs-2016-005267. PubMed
22. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: Origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22(suppl 2):ii58-iiii64. http://dx.doi.org/10.1136/bmjqs-2012-001712. PubMed
23. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: Impediments to and strategies for change. BMJ Qual Saf. 2013;22(suppl 2):ii65-iiii72. http://dx.doi.org/10.1136/bmjqs-2012-001713. PubMed
24. Reilly JB, Ogdie AR, Von Feldt JM, Myers JS. Teaching about how doctors think: a longitudinal curriculum in cognitive bias and diagnostic error for residents. BMJ Qual Saf. 2013;22(12):1044-1050. http://dx.doi.org/10.1136/bmjqs-2013-001987. PubMed
25. Schmidt HG, Mamede S, van den Berge K, van Gog T, van Saase JL, Rikers RM. Exposure to media information about a disease can cause doctors to misdiagnose similar-looking clinical cases. Acad Med. 2014;89(2):285-291. http://dx.doi.org/10.1097/ACM.0000000000000107. PubMed
26. Hess BJ, Lipner RS, Thompson V, Holmboe ES, Graber ML. Blink or think: can further reflection improve initial diagnostic impressions? Acad Med. 2015;90(1):112-118. http://dx.doi.org/10.1097/ACM.0000000000000550. PubMed
27. Lambe KA, O’Reilly G, Kelly BD, Curristan S. Dual-process cognitive interventions to enhance diagnostic reasoning: A systematic review. BMJ Qual Saf. 2016;25(10):808-820. http://dx.doi.org/10.1136/bmjqs-2015-004417. PubMed
28. Graber ML, Kissam S, Payne VL, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf. 2012;21(7):535-557. http://dx.doi.org/10.1136/bmjqs-2011-000149. PubMed
29. McDonald KM, Matesic B, Contopoulos-Ioannidis DG, et al. Patient safety strategies targeted at diagnostic errors: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):381-389. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00004. PubMed
30. Wray CM, Chaudhry S, Pincavage A, et al. Resident shift handoff strategies in US internal medicine residency programs. JAMA. 2016;316(21):2273-2275. http://dx.doi.org/10.1001/jama.2016.17786. PubMed
31. Choo KJ, Arora VM, Barach P, Johnson JK, Farnan JM. How do supervising physicians decide to entrust residents with unsupervised tasks? A qualitative analysis. J Hosp Med. 2014;9(3):169-175. http://dx.doi.org/10.1002/jhm.2150. PubMed
32. Carayon P, Wood KE. Patient safety - the role of human factors and systems engineering. Stud Health Technol Inform. 2010;153:23-46.
.http://dx.doi.org/10.1001/jama.2015.13453 PubMed
34. McGlynn EA, McDonald KM, Cassel CK. Measurement is essential for improving diagnosis and reducing diagnostic error: A report from the Institute of Medicine. JAMA. 2015;314(23):2501-2502.
.http://dx.doi.org/10.1136/bmjqs-2013-001812 PubMed
33. Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. 2014;23(3):196-205. PubMed
Diagnostic error—defined as a failure to establish an accurate and timely explanation of the patient’s health problem—is an important source of patient harm.1 Data suggest that all patients will experience at least 1 diagnostic error in their lifetime.2-4 Not surprisingly, diagnostic errors are among the leading categories of paid malpractice claims in the United States.5
Despite diagnostic errors being morbid and sometimes deadly in the hospital,6,7 little is known about how residents and learners approach diagnostic decision making. Errors in diagnosis are believed to stem from cognitive or system failures,8 with errors in cognition believed to occur due to rapid, reflexive thinking operating in the absence of a more analytical, deliberate process. System-based problems (eg, lack of expert availability, technology barriers, and access to data) have also been cited as contributors.9 However, whether and how these apply to trainees is not known.
Therefore, we conducted a focused ethnography of inpatient medicine teams (ie, attendings, residents, interns, and medical students) in 2 affiliated teaching hospitals, aiming to (a) observe the process of diagnosis by trainees and (b) identify methods to improve the diagnostic process and prevent errors.
METHODS
We designed a multimethod, focused ethnographic study to examine diagnostic decision making in hospital settings.10,11 In contrast to anthropologic ethnographies that study entire fields using open-ended questions, our study was designed to examine the process of diagnosis from the perspective of clinicians engaged in this activity.11 This approach allowed us to capture diagnostic decisions and cognitive and system-based factors in a manner currently lacking in the literature.12
Setting and Participants
Between January 2016 and May 2016, we observed the members of four inpatient internal medicine teaching teams at 2 affiliated teaching hospitals. We purposefully selected teaching teams for observation because they are the primary model of care in academic settings and we have expertise in carrying out similar studies.13,14 Teaching teams typically consisted of a medical attending (senior-level physician), 1 senior resident (a second- or third-year postgraduate trainee), two interns (a trainee in their first postgraduate year), and two to four medical students. Teams were selected at random using existing schedules and followed Monday to Friday so as to permit observation of work on call and noncall days. Owing to manpower limitations, weekend and night shifts were not observed. However, overnight events were captured during morning rounds.
Most of the teams began rounds at 8:30 AM. Typically, rounds lasted for 90–120 min and concluded with a recap (ie, “running the list”) with a review of explicit plans for patients after they had been evaluated by the attending. This discussion often occurred in the team rooms, with the attending leading the discussion with the trainees.
Data Collection
A multidisciplinary team, including clinicians (eg, physicians, nurses), nonclinicians (eg, qualitative researchers, social scientists), and healthcare engineers, conducted the observations. We observed preround activities of interns and residents before arrival of the attending (7:00 AM - 8:30 AM), followed by morning rounds with the entire team, and afternoon work that included senior residents, interns, and students.
To capture multiple aspects of the diagnostic process, we collected data using field notes modeled on components of the National Academy of Science model for diagnosis (Appendix).1,15 This model encompasses phases of the diagnostic process (eg, data gathering, integration, formulation of a working diagnosis, treatment delivery, and outcomes) and the work system (team members, organization, technology and tools, physical environment, tasks).
Focus Groups and Interviews
At the end of weekly observations, we conducted focus groups with the residents and one-on- one interviews with the attendings. Focus groups with the residents were conducted to encourage a group discussion about the diagnostic process. Separate interviews with the attendings were performed to ensure that power differentials did not influence discussions. During focus groups, we specifically asked about challenges and possible solutions to improve diagnosis. Experienced qualitative methodologists (J.F., M.H., M.Q.) used semistructured interview guides for discussions (Appendix).
Data Analysis
After aggregating and reading the data, three reviewers (V.C., S.K., S.S.) began inductive analysis by handwriting notes and initial reflective thoughts to create preliminary codes. Multiple team members then reread the original field notes and the focus group/interview data to refine the preliminary codes and develop additional codes. Next, relationships between codes were identified and used to develop key themes. Triangulation of data collected from observations and interview/focus group sessions was carried out to compare data that we surmised with data that were verbalized by the team. The developed themes were discussed as a group to ensure consistency of major findings.
Ethical and Regulatory Oversight
This study was reviewed and approved by the Institutional Review Boards at the University of Michigan Health System (HUM-00106657) and the VA Ann Arbor Healthcare System (1-2016-010040).
RESULTS
Four teaching teams (4 attendings, 4 senior residents, 9 interns, and 14 medical students) were observed over 33 distinct shifts and 168 hours. Observations included morning rounds (96 h), postround call days (52 h), and postround non-call days (20 h). Morning rounds lasted an average of 127 min (range: 48-232 min) and included an average of 9 patients (range: 4-16 patients).
Themes Regarding the Diagnostic Process
We identified the following 4 primary themes related to the diagnostic process in teaching hospitals: (1) diagnosis is a social phenomenon; (2) data necessary to make diagnoses are fragmented; (3) distractions undermine the diagnostic process; and (4) time pressures interfere with diagnostic decision making (Appendix Table 1).
(1) Diagnosis is a Social Phenomenon.
Team members viewed the process of diagnosis as a social exchange of facts, findings, and strategies within a defined structure. The opportunity to discuss impressions with others was valued as a means to share, test, and process assumptions.
“Rounds are the most important part of the process. That is where we make most decisions in a collective, collaborative way with the attending present. We bounce ideas off each other.” (Intern)
Typical of social processes, variations based on time of day and schedule were observed. For instance, during call days, learners gathered data and formed working diagnosis and treatment plans with minimal attending interaction. This separation of roles and responsibilities introduced a hierarchy within diagnosis as follows:
“The interns would not call me first; they would talk to the senior resident and then if the senior thought he should chat with me, then they would call. But for the most part, they gather information and come up with the plan.” (Attending).
The work system was suited to facilitate social interactions. For instance, designated rooms (with team members informally assigned to a computer) provided physical proximity of the resident to interns and medical students. In this space, numerous informal discussions between team members (eg, “What do you think about this test?” “I’m not sure what to do about this finding.” “Should I call a [consult] on this patient?”) were observed. Although proximity to each other was viewed as beneficial, dangers to the social nature of diagnosis in the form of anchoring (ie, a cognitive bias where emphasis is placed on the first piece of data)16 were also mentioned. Similarly, the paradox associated with social proof (ie, the pressure to assume conformity within a group) was also observed as disagreement between team members and attendings rarely occurred during observations.
“I mean, they’re the attending, right? It’s hard to argue with them when they want a test or something done. When I do push back, it’s rare that others will support me–so it’s usually me and the attending.” (Resident)
“I would push back if I think it’s really bad for the patient or could cause harm–but the truth is, it doesn’t happen much.” (Intern)
(2) Data Necessary to Make Diagnoses are Fragmented
Team members universally cited fragmentation in data delivery, retrieval, and processing as a barrier to diagnosis. Team members indicated that test results might not be looked at or acted upon in a timely manner, and participants pointed to the electronic medical record as a source of this challenge.
“Before I knew about [the app for Epic], I would literally sit on the computer to get all the information we would need on rounds. Its key to making decisions. We often say we will do something, only to find the test result doesn’t support it–and then we’re back to square 1.” (Intern)
Information used by teams came from myriad sources (eg, patients, family members, electronic records) and from various settings (eg, emergency department, patient rooms, discussions with consultants). Additionally, test results often appeared without warning. Thus, availability of information was poorly aligned with clinical duties.
“They (the lab) will call us when a blood culture is positive or something is off. That is very helpful but it often comes later in the day, when we’re done with rounds.” (Resident)
The work system was highlighted as a key contributor to data fragmentation. Peculiarities of our electronic medical record (EMR) and how data were collected, stored, or presented were described as “frustrating,” and “unsafe,” by team members. Correspondingly, we frequently observed interns asking for assistance for tasks such as ordering tests or finding information despite being “trained” to use the EMR.
“People have to learn how to filter, how to recognize the most important points and link data streams together in terms of causality. But we assume they know where to find that information. It’s actually a very hard thing to do, for both the house staff and me.” (Attending)
(3) Distractions Undermine the Diagnostic Process
Distractions often created cognitive difficulties. For example, ambient noise and interruptions from neighbors working on other teams were cited as barriers to diagnosis. In addition, we observed several team members using headphones to drown out ambient noise while working on the computer.
“I know I shouldn’t do it (wear headphones), but I have no other way of turning down the noise so I can concentrate.” (Intern)
Similarly, the unpredictable nature and the volume of pages often interrupted thinking about diagnosis.
“Sometimes the pager just goes off all the time and (after making sure its not an urgent issue), I will just ignore it for a bit, especially if I am in the middle of something. It would be great if I could finish my thought process knowing I would not be interrupted.” (Resident)
To mitigate this problem, 1 attending described how he would proactively seek out nurses caring for his patients to “head off” questions (eg, “I will renew the restraints and medications this morning,” and “Is there anything you need in terms of orders for this patient that I can take care of now?”) that might lead to pages. Another resident described his approach as follows:
“I make it a point to tell the nurses where I will be hanging out and where they can find me if they have any questions. I tell them to come talk to me rather than page me since that will be less distracting.” (Resident).
Most of the interns described documentation work such as writing admission and progress notes in negative terms (“an academic exercise,” “part of the billing activity”). However, in the context of interruptions, some described this as helpful.
“The most valuable part of the thinking process was writing the assessment and plan because that’s actually my schema for all problems. It literally is the only time where I can sit and collect my thoughts to formulate a diagnosis and plan.” (Intern)
(4) Time Pressures Interfere With Diagnostic Decision Making
All team members spoke about the challenge of finding time for diagnosis during the workday. Often, they had to skip learning sessions for this purpose.
“They tell us we should go to morning report or noon conference but when I’m running around trying to get things done. I hate having to choose between my education and doing what’s best for the patient–but that’s often what it comes down to.” (Intern)
When specifically asked whether setting aside dedicated time to specifically review and formulate diagnoses would be valuable, respondents were uniformly enthusiastic. Team members described attentional conflicts as being the worst when “cross covering” other teams on call days, as their patient load effectively doubled during this time. Of note, cross-covering occurred when teams were also on call—and thus took them away from important diagnostic activities such as data gathering or synthesis for patients they were admitting.
“If you were to ever design a system where errors were likely–this is how you would design it: take a team with little supervision, double their patient load, keep them busy with new challenging cases and then ask questions about patients they know little about.” (Resident)
DISCUSSION
Although diagnostic errors have been called “the next frontier for patient safety,”17 little is known about the process, barriers, and facilitators to diagnosis in teaching hospitals. In this focused ethnography conducted at 2 academic medical centers, we identified multiple cognitive and system-level challenges and potential strategies to improve diagnosis from trainees engaged in this activity. Key themes identified by those we observed included the social nature of diagnosis, fragmented information delivery, constant distractions and interruptions, and time pressures. In turn, these insights allow us to generate strategies that can be applied to improve the diagnostic process in teaching hospitals.
Our study underscores the importance of social interactions in diagnosis. In contrast, most of the interventions to prevent diagnostic errors target individual providers through practices such as metacognition and “thinking about thinking.”18-20 These interventions are based on Daniel Kahnemann’s work on dual thought process. Type 1 thought processes are fast, subconscious, reflexive, largely intuitive, and more vulnerable to error. In contrast, Type 2 processes are slower, deliberate, analytic, and less prone to error.21 Although an individual’s Type 2 thought capacity is limited, a major goal of cognitive interventions is to encourage Type 2 over Type 1 thinking, an approach termed “de-biasing.”22-24 Unfortunately, cognitive interventions testing such approaches have suffered mixed results–perhaps because of lack of focus on collective wisdom or group thinking, which may be key to diagnosis from our findings.9,25 In this sense, morning rounds were a social gathering used to strategize and develop care plans, but with limited time to think about diagnosis.26 Introduction of defined periods for individuals to engage in diagnostic activities such as de-biasing (ie, asking “what else could this be)27 before or after rounds may provide an opportunity for reflection and improving diagnosis. In addition, embedding tools such as diagnosis expanders and checklists within these defined time slots28,29 may prove to be useful in reflecting on diagnosis and preventing diagnostic errors.
An unexpected yet important finding from this study were the challenges posed by distractions and the physical environment. Potentially maladaptive workarounds to these interruptions included use of headphones; more productive strategies included updating nurses with plans to avert pages and creating a list of activities to ensure that key tasks were not forgotten.30,31 Applying lessons from aviation, a focused effort to limit distractions during key portions of the day, might be worth considering for diagnostic safety.32 Similarly, improving the environment in which diagnosis occurs—including creating spaces that are quiet, orderly, and optimized for thinking—may be valuable.33Our study has limitations. First, our findings are limited to direct observations; we are thus unable to comment on how unobserved aspects of care (eg, cognitive processes) might have influenced our findings. Our observations of clinical care might also have introduced a Hawthorne effect. However, because we were closely integrated with teams and conducted focus groups to corroborate our assessments, we believe that this was not the case. Second, we did not identify diagnostic errors or link processes we observed to errors. Third, our approach is limited to 2 teaching centers, thereby limiting the generalizability of findings. Relatedly, we were only able to conduct observations during weekdays; differences in weekend and night resources might affect our insights.
The cognitive and system-based barriers faced by clinicians in teaching hospitals suggest that new methods to improve diagnosis are needed. Future interventions such as defined “time-outs” for diagnosis, strategies focused on limiting distractions, and methods to improve communication between team members are novel and have parallels in other industries. As challenges to quantify diagnostic errors abound,34 improving cognitive- and system-based factors via reflection through communication, concentration, and organization is necessary to improve medical decision making in academic medical centers.
Disclosures
None declared for all coauthors.
Funding
This project was supported by grant number P30HS024385 from the Agency for Healthcare Research and Quality. The funding source played no role in study design, data acquisition, analysis or decision to report these data. Dr. Chopra is supported by a career development award from the Agency of Healthcare Research and Quality (1-K08-HS022835-01). Dr. Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). Dr. Singh is partially supported by Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the Department of Veterans Affairs.
Diagnostic error—defined as a failure to establish an accurate and timely explanation of the patient’s health problem—is an important source of patient harm.1 Data suggest that all patients will experience at least 1 diagnostic error in their lifetime.2-4 Not surprisingly, diagnostic errors are among the leading categories of paid malpractice claims in the United States.5
Despite diagnostic errors being morbid and sometimes deadly in the hospital,6,7 little is known about how residents and learners approach diagnostic decision making. Errors in diagnosis are believed to stem from cognitive or system failures,8 with errors in cognition believed to occur due to rapid, reflexive thinking operating in the absence of a more analytical, deliberate process. System-based problems (eg, lack of expert availability, technology barriers, and access to data) have also been cited as contributors.9 However, whether and how these apply to trainees is not known.
Therefore, we conducted a focused ethnography of inpatient medicine teams (ie, attendings, residents, interns, and medical students) in 2 affiliated teaching hospitals, aiming to (a) observe the process of diagnosis by trainees and (b) identify methods to improve the diagnostic process and prevent errors.
METHODS
We designed a multimethod, focused ethnographic study to examine diagnostic decision making in hospital settings.10,11 In contrast to anthropologic ethnographies that study entire fields using open-ended questions, our study was designed to examine the process of diagnosis from the perspective of clinicians engaged in this activity.11 This approach allowed us to capture diagnostic decisions and cognitive and system-based factors in a manner currently lacking in the literature.12
Setting and Participants
Between January 2016 and May 2016, we observed the members of four inpatient internal medicine teaching teams at 2 affiliated teaching hospitals. We purposefully selected teaching teams for observation because they are the primary model of care in academic settings and we have expertise in carrying out similar studies.13,14 Teaching teams typically consisted of a medical attending (senior-level physician), 1 senior resident (a second- or third-year postgraduate trainee), two interns (a trainee in their first postgraduate year), and two to four medical students. Teams were selected at random using existing schedules and followed Monday to Friday so as to permit observation of work on call and noncall days. Owing to manpower limitations, weekend and night shifts were not observed. However, overnight events were captured during morning rounds.
Most of the teams began rounds at 8:30 AM. Typically, rounds lasted for 90–120 min and concluded with a recap (ie, “running the list”) with a review of explicit plans for patients after they had been evaluated by the attending. This discussion often occurred in the team rooms, with the attending leading the discussion with the trainees.
Data Collection
A multidisciplinary team, including clinicians (eg, physicians, nurses), nonclinicians (eg, qualitative researchers, social scientists), and healthcare engineers, conducted the observations. We observed preround activities of interns and residents before arrival of the attending (7:00 AM - 8:30 AM), followed by morning rounds with the entire team, and afternoon work that included senior residents, interns, and students.
To capture multiple aspects of the diagnostic process, we collected data using field notes modeled on components of the National Academy of Science model for diagnosis (Appendix).1,15 This model encompasses phases of the diagnostic process (eg, data gathering, integration, formulation of a working diagnosis, treatment delivery, and outcomes) and the work system (team members, organization, technology and tools, physical environment, tasks).
Focus Groups and Interviews
At the end of weekly observations, we conducted focus groups with the residents and one-on- one interviews with the attendings. Focus groups with the residents were conducted to encourage a group discussion about the diagnostic process. Separate interviews with the attendings were performed to ensure that power differentials did not influence discussions. During focus groups, we specifically asked about challenges and possible solutions to improve diagnosis. Experienced qualitative methodologists (J.F., M.H., M.Q.) used semistructured interview guides for discussions (Appendix).
Data Analysis
After aggregating and reading the data, three reviewers (V.C., S.K., S.S.) began inductive analysis by handwriting notes and initial reflective thoughts to create preliminary codes. Multiple team members then reread the original field notes and the focus group/interview data to refine the preliminary codes and develop additional codes. Next, relationships between codes were identified and used to develop key themes. Triangulation of data collected from observations and interview/focus group sessions was carried out to compare data that we surmised with data that were verbalized by the team. The developed themes were discussed as a group to ensure consistency of major findings.
Ethical and Regulatory Oversight
This study was reviewed and approved by the Institutional Review Boards at the University of Michigan Health System (HUM-00106657) and the VA Ann Arbor Healthcare System (1-2016-010040).
RESULTS
Four teaching teams (4 attendings, 4 senior residents, 9 interns, and 14 medical students) were observed over 33 distinct shifts and 168 hours. Observations included morning rounds (96 h), postround call days (52 h), and postround non-call days (20 h). Morning rounds lasted an average of 127 min (range: 48-232 min) and included an average of 9 patients (range: 4-16 patients).
Themes Regarding the Diagnostic Process
We identified the following 4 primary themes related to the diagnostic process in teaching hospitals: (1) diagnosis is a social phenomenon; (2) data necessary to make diagnoses are fragmented; (3) distractions undermine the diagnostic process; and (4) time pressures interfere with diagnostic decision making (Appendix Table 1).
(1) Diagnosis is a Social Phenomenon.
Team members viewed the process of diagnosis as a social exchange of facts, findings, and strategies within a defined structure. The opportunity to discuss impressions with others was valued as a means to share, test, and process assumptions.
“Rounds are the most important part of the process. That is where we make most decisions in a collective, collaborative way with the attending present. We bounce ideas off each other.” (Intern)
Typical of social processes, variations based on time of day and schedule were observed. For instance, during call days, learners gathered data and formed working diagnosis and treatment plans with minimal attending interaction. This separation of roles and responsibilities introduced a hierarchy within diagnosis as follows:
“The interns would not call me first; they would talk to the senior resident and then if the senior thought he should chat with me, then they would call. But for the most part, they gather information and come up with the plan.” (Attending).
The work system was suited to facilitate social interactions. For instance, designated rooms (with team members informally assigned to a computer) provided physical proximity of the resident to interns and medical students. In this space, numerous informal discussions between team members (eg, “What do you think about this test?” “I’m not sure what to do about this finding.” “Should I call a [consult] on this patient?”) were observed. Although proximity to each other was viewed as beneficial, dangers to the social nature of diagnosis in the form of anchoring (ie, a cognitive bias where emphasis is placed on the first piece of data)16 were also mentioned. Similarly, the paradox associated with social proof (ie, the pressure to assume conformity within a group) was also observed as disagreement between team members and attendings rarely occurred during observations.
“I mean, they’re the attending, right? It’s hard to argue with them when they want a test or something done. When I do push back, it’s rare that others will support me–so it’s usually me and the attending.” (Resident)
“I would push back if I think it’s really bad for the patient or could cause harm–but the truth is, it doesn’t happen much.” (Intern)
(2) Data Necessary to Make Diagnoses are Fragmented
Team members universally cited fragmentation in data delivery, retrieval, and processing as a barrier to diagnosis. Team members indicated that test results might not be looked at or acted upon in a timely manner, and participants pointed to the electronic medical record as a source of this challenge.
“Before I knew about [the app for Epic], I would literally sit on the computer to get all the information we would need on rounds. Its key to making decisions. We often say we will do something, only to find the test result doesn’t support it–and then we’re back to square 1.” (Intern)
Information used by teams came from myriad sources (eg, patients, family members, electronic records) and from various settings (eg, emergency department, patient rooms, discussions with consultants). Additionally, test results often appeared without warning. Thus, availability of information was poorly aligned with clinical duties.
“They (the lab) will call us when a blood culture is positive or something is off. That is very helpful but it often comes later in the day, when we’re done with rounds.” (Resident)
The work system was highlighted as a key contributor to data fragmentation. Peculiarities of our electronic medical record (EMR) and how data were collected, stored, or presented were described as “frustrating,” and “unsafe,” by team members. Correspondingly, we frequently observed interns asking for assistance for tasks such as ordering tests or finding information despite being “trained” to use the EMR.
“People have to learn how to filter, how to recognize the most important points and link data streams together in terms of causality. But we assume they know where to find that information. It’s actually a very hard thing to do, for both the house staff and me.” (Attending)
(3) Distractions Undermine the Diagnostic Process
Distractions often created cognitive difficulties. For example, ambient noise and interruptions from neighbors working on other teams were cited as barriers to diagnosis. In addition, we observed several team members using headphones to drown out ambient noise while working on the computer.
“I know I shouldn’t do it (wear headphones), but I have no other way of turning down the noise so I can concentrate.” (Intern)
Similarly, the unpredictable nature and the volume of pages often interrupted thinking about diagnosis.
“Sometimes the pager just goes off all the time and (after making sure its not an urgent issue), I will just ignore it for a bit, especially if I am in the middle of something. It would be great if I could finish my thought process knowing I would not be interrupted.” (Resident)
To mitigate this problem, 1 attending described how he would proactively seek out nurses caring for his patients to “head off” questions (eg, “I will renew the restraints and medications this morning,” and “Is there anything you need in terms of orders for this patient that I can take care of now?”) that might lead to pages. Another resident described his approach as follows:
“I make it a point to tell the nurses where I will be hanging out and where they can find me if they have any questions. I tell them to come talk to me rather than page me since that will be less distracting.” (Resident).
Most of the interns described documentation work such as writing admission and progress notes in negative terms (“an academic exercise,” “part of the billing activity”). However, in the context of interruptions, some described this as helpful.
“The most valuable part of the thinking process was writing the assessment and plan because that’s actually my schema for all problems. It literally is the only time where I can sit and collect my thoughts to formulate a diagnosis and plan.” (Intern)
(4) Time Pressures Interfere With Diagnostic Decision Making
All team members spoke about the challenge of finding time for diagnosis during the workday. Often, they had to skip learning sessions for this purpose.
“They tell us we should go to morning report or noon conference but when I’m running around trying to get things done. I hate having to choose between my education and doing what’s best for the patient–but that’s often what it comes down to.” (Intern)
When specifically asked whether setting aside dedicated time to specifically review and formulate diagnoses would be valuable, respondents were uniformly enthusiastic. Team members described attentional conflicts as being the worst when “cross covering” other teams on call days, as their patient load effectively doubled during this time. Of note, cross-covering occurred when teams were also on call—and thus took them away from important diagnostic activities such as data gathering or synthesis for patients they were admitting.
“If you were to ever design a system where errors were likely–this is how you would design it: take a team with little supervision, double their patient load, keep them busy with new challenging cases and then ask questions about patients they know little about.” (Resident)
DISCUSSION
Although diagnostic errors have been called “the next frontier for patient safety,”17 little is known about the process, barriers, and facilitators to diagnosis in teaching hospitals. In this focused ethnography conducted at 2 academic medical centers, we identified multiple cognitive and system-level challenges and potential strategies to improve diagnosis from trainees engaged in this activity. Key themes identified by those we observed included the social nature of diagnosis, fragmented information delivery, constant distractions and interruptions, and time pressures. In turn, these insights allow us to generate strategies that can be applied to improve the diagnostic process in teaching hospitals.
Our study underscores the importance of social interactions in diagnosis. In contrast, most of the interventions to prevent diagnostic errors target individual providers through practices such as metacognition and “thinking about thinking.”18-20 These interventions are based on Daniel Kahnemann’s work on dual thought process. Type 1 thought processes are fast, subconscious, reflexive, largely intuitive, and more vulnerable to error. In contrast, Type 2 processes are slower, deliberate, analytic, and less prone to error.21 Although an individual’s Type 2 thought capacity is limited, a major goal of cognitive interventions is to encourage Type 2 over Type 1 thinking, an approach termed “de-biasing.”22-24 Unfortunately, cognitive interventions testing such approaches have suffered mixed results–perhaps because of lack of focus on collective wisdom or group thinking, which may be key to diagnosis from our findings.9,25 In this sense, morning rounds were a social gathering used to strategize and develop care plans, but with limited time to think about diagnosis.26 Introduction of defined periods for individuals to engage in diagnostic activities such as de-biasing (ie, asking “what else could this be)27 before or after rounds may provide an opportunity for reflection and improving diagnosis. In addition, embedding tools such as diagnosis expanders and checklists within these defined time slots28,29 may prove to be useful in reflecting on diagnosis and preventing diagnostic errors.
An unexpected yet important finding from this study were the challenges posed by distractions and the physical environment. Potentially maladaptive workarounds to these interruptions included use of headphones; more productive strategies included updating nurses with plans to avert pages and creating a list of activities to ensure that key tasks were not forgotten.30,31 Applying lessons from aviation, a focused effort to limit distractions during key portions of the day, might be worth considering for diagnostic safety.32 Similarly, improving the environment in which diagnosis occurs—including creating spaces that are quiet, orderly, and optimized for thinking—may be valuable.33Our study has limitations. First, our findings are limited to direct observations; we are thus unable to comment on how unobserved aspects of care (eg, cognitive processes) might have influenced our findings. Our observations of clinical care might also have introduced a Hawthorne effect. However, because we were closely integrated with teams and conducted focus groups to corroborate our assessments, we believe that this was not the case. Second, we did not identify diagnostic errors or link processes we observed to errors. Third, our approach is limited to 2 teaching centers, thereby limiting the generalizability of findings. Relatedly, we were only able to conduct observations during weekdays; differences in weekend and night resources might affect our insights.
The cognitive and system-based barriers faced by clinicians in teaching hospitals suggest that new methods to improve diagnosis are needed. Future interventions such as defined “time-outs” for diagnosis, strategies focused on limiting distractions, and methods to improve communication between team members are novel and have parallels in other industries. As challenges to quantify diagnostic errors abound,34 improving cognitive- and system-based factors via reflection through communication, concentration, and organization is necessary to improve medical decision making in academic medical centers.
Disclosures
None declared for all coauthors.
Funding
This project was supported by grant number P30HS024385 from the Agency for Healthcare Research and Quality. The funding source played no role in study design, data acquisition, analysis or decision to report these data. Dr. Chopra is supported by a career development award from the Agency of Healthcare Research and Quality (1-K08-HS022835-01). Dr. Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). Dr. Singh is partially supported by Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13-413). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the Department of Veterans Affairs.
1. National Academies of Sciences, Engineering, and Medicine. 2015. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press. http://www.nap.edu/21794. Accessed November 1; 2016:2015. https://doi.org/10.17226/21794.
2. Schiff GD, Hasan O, Kim S, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med. 2009;169(20):1881-1887. http://dx.doi.org/10.1001/archinternmed.2009.333. PubMed
3. Sonderegger-Iseli K, Burger S, Muntwyler J, Salomon F. Diagnostic errors in three medical eras: A necropsy study. Lancet. 2000;355(9220):2027-2031. http://dx.doi.org/10.1016/S0140-6736(00)02349-7. PubMed
4. Winters B, Custer J, Galvagno SM Jr, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Qual Saf. 2012;21(11):894-902. http://dx.doi.org/10.1136/bmjqs-2012-000803. PubMed
5. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680. http://dx.doi.org/10.1136/bmjqs-2012-001550. PubMed
6. Graber M, Gordon R, Franklin N. Reducing diagnostic errors in medicine: what’s the goal? Acad Med. 2002;77(10):981-992. http://dx.doi.org/10.1097/00001888-200210000-00009. PubMed
7. Gupta A, Snyder A, Kachalia A, Flanders S, Saint S, Chopra V. Malpractice claims related to diagnostic errors in the hospital. BMJ Qual Saf. 2018;27(1):53-60. 10.1136/bmjqs-2017-006774. PubMed
8. van Noord I, Eikens MP, Hamersma AM, de Bruijne MC. Application of root cause analysis on malpractice claim files related to diagnostic failures. Qual Saf Health Care. 2010;19(6):e21. http://dx.doi.org/10.1136/qshc.2008.029801. PubMed
9. Croskerry P, Petrie DA, Reilly JB, Tait G. Deciding about fast and slow decisions. Acad Med. 2014;89(2):197-200. 10.1097/ACM.0000000000000121. PubMed
10. Higginbottom GM, Pillay JJ, Boadu NY. Guidance on performing focused ethnographies with an emphasis on healthcare research. Qual Rep. 2013;18(9):1-6. https://doi.org/10.7939/R35M6287P.
11. Savage J. Participative observation: standing in the shoes of others? Qual Health Res. 2000;10(3):324-339. http://dx.doi.org/10.1177/104973200129118471. PubMed
12. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: SAGE Publications; 2002.
13. Harrod M, Weston LE, Robinson C, Tremblay A, Greenstone CL, Forman J. “It goes beyond good camaraderie”: A qualitative study of the process of becoming an interprofessional healthcare “teamlet.” J Interprof Care. 2016;30(3):295-300. http://dx.doi.org/10.3109/13561820.2015.1130028. PubMed
14. Houchens N, Harrod M, Moody S, Fowler KE, Saint S. Techniques and behaviors associated with exemplary inpatient general medicine teaching: an exploratory qualitative study. J Hosp Med. 2017;12(7):503-509. http://dx.doi.org/10.12788/jhm.2763. PubMed
15. Mulhall A. In the field: notes on observation in qualitative research. J Adv Nurs. 2003;41(3):306-313. http://dx.doi.org/10.1046/j.1365-2648.2003.02514.x. PubMed
16. Zwaan L, Monteiro S, Sherbino J, Ilgen J, Howey B, Norman G. Is bias in the eye of the beholder? A vignette study to assess recognition of cognitive biases in clinical case workups. BMJ Qual Saf. 2017;26(2):104-110. http://dx.doi.org/10.1136/bmjqs-2015-005014. PubMed
17. Singh H, Graber ML. Improving diagnosis in health care--the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. http://dx.doi.org/10.1056/NEJMp1512241. PubMed
18. Croskerry P. From mindless to mindful practice--cognitive bias and clinical decision making. N Engl J Med. 2013;368(26):2445-2448. http://dx.doi.org/10.1056/NEJMp1303712. PubMed
19. van den Berge K, Mamede S. Cognitive diagnostic error in internal medicine. Eur J Intern Med. 2013;24(6):525-529. http://dx.doi.org/10.1016/j.ejim.2013.03.006. PubMed
20. Norman G, Sherbino J, Dore K, et al. The etiology of diagnostic errors: A controlled trial of system 1 versus system 2 reasoning. Acad Med. 2014;89(2):277-284. 10.1097/ACM.0000000000000105 PubMed
21. Dhaliwal G. Premature closure? Not so fast. BMJ Qual Saf. 2017;26(2):87-89. http://dx.doi.org/10.1136/bmjqs-2016-005267. PubMed
22. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: Origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22(suppl 2):ii58-iiii64. http://dx.doi.org/10.1136/bmjqs-2012-001712. PubMed
23. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: Impediments to and strategies for change. BMJ Qual Saf. 2013;22(suppl 2):ii65-iiii72. http://dx.doi.org/10.1136/bmjqs-2012-001713. PubMed
24. Reilly JB, Ogdie AR, Von Feldt JM, Myers JS. Teaching about how doctors think: a longitudinal curriculum in cognitive bias and diagnostic error for residents. BMJ Qual Saf. 2013;22(12):1044-1050. http://dx.doi.org/10.1136/bmjqs-2013-001987. PubMed
25. Schmidt HG, Mamede S, van den Berge K, van Gog T, van Saase JL, Rikers RM. Exposure to media information about a disease can cause doctors to misdiagnose similar-looking clinical cases. Acad Med. 2014;89(2):285-291. http://dx.doi.org/10.1097/ACM.0000000000000107. PubMed
26. Hess BJ, Lipner RS, Thompson V, Holmboe ES, Graber ML. Blink or think: can further reflection improve initial diagnostic impressions? Acad Med. 2015;90(1):112-118. http://dx.doi.org/10.1097/ACM.0000000000000550. PubMed
27. Lambe KA, O’Reilly G, Kelly BD, Curristan S. Dual-process cognitive interventions to enhance diagnostic reasoning: A systematic review. BMJ Qual Saf. 2016;25(10):808-820. http://dx.doi.org/10.1136/bmjqs-2015-004417. PubMed
28. Graber ML, Kissam S, Payne VL, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf. 2012;21(7):535-557. http://dx.doi.org/10.1136/bmjqs-2011-000149. PubMed
29. McDonald KM, Matesic B, Contopoulos-Ioannidis DG, et al. Patient safety strategies targeted at diagnostic errors: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):381-389. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00004. PubMed
30. Wray CM, Chaudhry S, Pincavage A, et al. Resident shift handoff strategies in US internal medicine residency programs. JAMA. 2016;316(21):2273-2275. http://dx.doi.org/10.1001/jama.2016.17786. PubMed
31. Choo KJ, Arora VM, Barach P, Johnson JK, Farnan JM. How do supervising physicians decide to entrust residents with unsupervised tasks? A qualitative analysis. J Hosp Med. 2014;9(3):169-175. http://dx.doi.org/10.1002/jhm.2150. PubMed
32. Carayon P, Wood KE. Patient safety - the role of human factors and systems engineering. Stud Health Technol Inform. 2010;153:23-46.
.http://dx.doi.org/10.1001/jama.2015.13453 PubMed
34. McGlynn EA, McDonald KM, Cassel CK. Measurement is essential for improving diagnosis and reducing diagnostic error: A report from the Institute of Medicine. JAMA. 2015;314(23):2501-2502.
.http://dx.doi.org/10.1136/bmjqs-2013-001812 PubMed
33. Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. 2014;23(3):196-205. PubMed
1. National Academies of Sciences, Engineering, and Medicine. 2015. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press. http://www.nap.edu/21794. Accessed November 1; 2016:2015. https://doi.org/10.17226/21794.
2. Schiff GD, Hasan O, Kim S, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med. 2009;169(20):1881-1887. http://dx.doi.org/10.1001/archinternmed.2009.333. PubMed
3. Sonderegger-Iseli K, Burger S, Muntwyler J, Salomon F. Diagnostic errors in three medical eras: A necropsy study. Lancet. 2000;355(9220):2027-2031. http://dx.doi.org/10.1016/S0140-6736(00)02349-7. PubMed
4. Winters B, Custer J, Galvagno SM Jr, et al. Diagnostic errors in the intensive care unit: a systematic review of autopsy studies. BMJ Qual Saf. 2012;21(11):894-902. http://dx.doi.org/10.1136/bmjqs-2012-000803. PubMed
5. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680. http://dx.doi.org/10.1136/bmjqs-2012-001550. PubMed
6. Graber M, Gordon R, Franklin N. Reducing diagnostic errors in medicine: what’s the goal? Acad Med. 2002;77(10):981-992. http://dx.doi.org/10.1097/00001888-200210000-00009. PubMed
7. Gupta A, Snyder A, Kachalia A, Flanders S, Saint S, Chopra V. Malpractice claims related to diagnostic errors in the hospital. BMJ Qual Saf. 2018;27(1):53-60. 10.1136/bmjqs-2017-006774. PubMed
8. van Noord I, Eikens MP, Hamersma AM, de Bruijne MC. Application of root cause analysis on malpractice claim files related to diagnostic failures. Qual Saf Health Care. 2010;19(6):e21. http://dx.doi.org/10.1136/qshc.2008.029801. PubMed
9. Croskerry P, Petrie DA, Reilly JB, Tait G. Deciding about fast and slow decisions. Acad Med. 2014;89(2):197-200. 10.1097/ACM.0000000000000121. PubMed
10. Higginbottom GM, Pillay JJ, Boadu NY. Guidance on performing focused ethnographies with an emphasis on healthcare research. Qual Rep. 2013;18(9):1-6. https://doi.org/10.7939/R35M6287P.
11. Savage J. Participative observation: standing in the shoes of others? Qual Health Res. 2000;10(3):324-339. http://dx.doi.org/10.1177/104973200129118471. PubMed
12. Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: SAGE Publications; 2002.
13. Harrod M, Weston LE, Robinson C, Tremblay A, Greenstone CL, Forman J. “It goes beyond good camaraderie”: A qualitative study of the process of becoming an interprofessional healthcare “teamlet.” J Interprof Care. 2016;30(3):295-300. http://dx.doi.org/10.3109/13561820.2015.1130028. PubMed
14. Houchens N, Harrod M, Moody S, Fowler KE, Saint S. Techniques and behaviors associated with exemplary inpatient general medicine teaching: an exploratory qualitative study. J Hosp Med. 2017;12(7):503-509. http://dx.doi.org/10.12788/jhm.2763. PubMed
15. Mulhall A. In the field: notes on observation in qualitative research. J Adv Nurs. 2003;41(3):306-313. http://dx.doi.org/10.1046/j.1365-2648.2003.02514.x. PubMed
16. Zwaan L, Monteiro S, Sherbino J, Ilgen J, Howey B, Norman G. Is bias in the eye of the beholder? A vignette study to assess recognition of cognitive biases in clinical case workups. BMJ Qual Saf. 2017;26(2):104-110. http://dx.doi.org/10.1136/bmjqs-2015-005014. PubMed
17. Singh H, Graber ML. Improving diagnosis in health care--the next imperative for patient safety. N Engl J Med. 2015;373(26):2493-2495. http://dx.doi.org/10.1056/NEJMp1512241. PubMed
18. Croskerry P. From mindless to mindful practice--cognitive bias and clinical decision making. N Engl J Med. 2013;368(26):2445-2448. http://dx.doi.org/10.1056/NEJMp1303712. PubMed
19. van den Berge K, Mamede S. Cognitive diagnostic error in internal medicine. Eur J Intern Med. 2013;24(6):525-529. http://dx.doi.org/10.1016/j.ejim.2013.03.006. PubMed
20. Norman G, Sherbino J, Dore K, et al. The etiology of diagnostic errors: A controlled trial of system 1 versus system 2 reasoning. Acad Med. 2014;89(2):277-284. 10.1097/ACM.0000000000000105 PubMed
21. Dhaliwal G. Premature closure? Not so fast. BMJ Qual Saf. 2017;26(2):87-89. http://dx.doi.org/10.1136/bmjqs-2016-005267. PubMed
22. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: Origins of bias and theory of debiasing. BMJ Qual Saf. 2013;22(suppl 2):ii58-iiii64. http://dx.doi.org/10.1136/bmjqs-2012-001712. PubMed
23. Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: Impediments to and strategies for change. BMJ Qual Saf. 2013;22(suppl 2):ii65-iiii72. http://dx.doi.org/10.1136/bmjqs-2012-001713. PubMed
24. Reilly JB, Ogdie AR, Von Feldt JM, Myers JS. Teaching about how doctors think: a longitudinal curriculum in cognitive bias and diagnostic error for residents. BMJ Qual Saf. 2013;22(12):1044-1050. http://dx.doi.org/10.1136/bmjqs-2013-001987. PubMed
25. Schmidt HG, Mamede S, van den Berge K, van Gog T, van Saase JL, Rikers RM. Exposure to media information about a disease can cause doctors to misdiagnose similar-looking clinical cases. Acad Med. 2014;89(2):285-291. http://dx.doi.org/10.1097/ACM.0000000000000107. PubMed
26. Hess BJ, Lipner RS, Thompson V, Holmboe ES, Graber ML. Blink or think: can further reflection improve initial diagnostic impressions? Acad Med. 2015;90(1):112-118. http://dx.doi.org/10.1097/ACM.0000000000000550. PubMed
27. Lambe KA, O’Reilly G, Kelly BD, Curristan S. Dual-process cognitive interventions to enhance diagnostic reasoning: A systematic review. BMJ Qual Saf. 2016;25(10):808-820. http://dx.doi.org/10.1136/bmjqs-2015-004417. PubMed
28. Graber ML, Kissam S, Payne VL, et al. Cognitive interventions to reduce diagnostic error: a narrative review. BMJ Qual Saf. 2012;21(7):535-557. http://dx.doi.org/10.1136/bmjqs-2011-000149. PubMed
29. McDonald KM, Matesic B, Contopoulos-Ioannidis DG, et al. Patient safety strategies targeted at diagnostic errors: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):381-389. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00004. PubMed
30. Wray CM, Chaudhry S, Pincavage A, et al. Resident shift handoff strategies in US internal medicine residency programs. JAMA. 2016;316(21):2273-2275. http://dx.doi.org/10.1001/jama.2016.17786. PubMed
31. Choo KJ, Arora VM, Barach P, Johnson JK, Farnan JM. How do supervising physicians decide to entrust residents with unsupervised tasks? A qualitative analysis. J Hosp Med. 2014;9(3):169-175. http://dx.doi.org/10.1002/jhm.2150. PubMed
32. Carayon P, Wood KE. Patient safety - the role of human factors and systems engineering. Stud Health Technol Inform. 2010;153:23-46.
.http://dx.doi.org/10.1001/jama.2015.13453 PubMed
34. McGlynn EA, McDonald KM, Cassel CK. Measurement is essential for improving diagnosis and reducing diagnostic error: A report from the Institute of Medicine. JAMA. 2015;314(23):2501-2502.
.http://dx.doi.org/10.1136/bmjqs-2013-001812 PubMed
33. Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf. 2014;23(3):196-205. PubMed
© 2018 Society of Hospital Medicine
Rethinking Resident Supervision
Close supervision of residents potentially leads to fewer errors, lower patient mortality, and improved quality of care.19 An Institute of Medicine (IOM) report3 recommended improving supervision through more frequent consultations between residents and their supervisors. Although current Accreditation Council for Graduate Medical Education (ACGME) guidelines also recommend that attending physicians (attendings) supervise residents, detailed guidance about what constitutes adequate supervision and how it should be implemented is not well defined.10, 11 The ACGME stresses that supervision should promote resident autonomy in clinical care.10 However, when trainees act independently, it might lead to critical communication breakdowns and other patient safety concerns.5, 6, 1214 Although attendings can encourage (or discourage) residents from seeking advice,15, 16 residents also play important roles in asking for help (ie, initiating their own supervision).1719 Additional research is needed on how residents walk the fine line between exercising independence and seeking supervision.
Lack of resident supervision is especially problematic in high‐risk settings such as the medical intensive care unit (ICU), where medical errors are as frequent as 1.7 errors per patient per day,20, 21 and the adverse drug event rate is twice that of non‐ICU settings.22 Because medication errors are one of the most common errors residents make,23, 24 resident interactions with nursing and pharmacy staff may significantly influence medication safety in error‐prone ICUs.2529 Studies of traditional hierarchical supervision tend to overlook how interactions with other professionals influence resident training.12, 18, 30, 31
We define supervision as a process of providing trainees with monitoring, guidance, and feedback9(p828) as they care for patients.3 Whereas traditionally, supervisors are identified by their positions of formal authority in the medical chain of command; we conceptualize supervision as a process in which professionals engaged in supervisory activities need not have formal authority over their trainees.
To examine how residents seek supervision through both the traditional medical hierarchical chain of command (including attendings, fellows and senior residents) and interprofessional communication channels (including nursing and pharmacy staff), we conducted a qualitative study of residents working in ICUs in three tertiary care hospitals. Using semi‐structured interviews, we asked residents to describe how they experienced supervision as they provided medications to patients. Two broad research questions guided data analysis:
How do residents receive supervision from physicians in the traditional medical hierarchy?
How do residents receive supervision from other professionals (ie, nurses, staff pharmacists, and clinical pharmacists)?
METHODS
Study Design and Sample
We conducted a qualitative study using data from interviews with 17 residents working in the medical ICUs of three large tertiary care hospitals (henceforth referred to as South, West, and North hospitals). The interviews were conducted as part of a longitudinal research project that examined how hospitals learn from medication errors.32 The research project focused on hospitals where medication error prevention was salient because of a vulnerable patient population and/or extensive high‐hazard drug usage. For each ICU, the research design included interviews with 6 attendings, 6 fellows, and a purposeful random sample33 of 6 residents. The goal was to reduce bias from supervisors selecting study participants, and thus enhance the credibility of the small sample, rather than generalize from it.32 Surgical residents were excluded, because of the medication focus. The local Institutional Review Boards approved the research.
Drawing on preliminary analyses of research project data, we designed the current study to examine how residents experienced supervision.33 A qualitative research design was particularly appropriate, because this study is exploratory34 and examines the processes of how supervision is implemented.33 By gathering longitudinal data from 2001 to 2007 and from ICUs in different hospitals, we were able to search for persistent patterns (and systematic variations over time) in how residents experienced supervision that might not have been revealed by a cross‐sectional study in one hospital ICU.
Data Collection
The principal investigator ([PI] M.T.) interviewed residents to gather data about their experiences with medication safety and supervision when providing medication to ICU patients. A general interview guide33 addressed residents' personal experiences with ordering medications, receiving supervision, and their perceptions of institutional medication safety programs (see Supporting Table 1 in the online version of this article). The interviewer consistently prompted residents to provide examples of their supervision experiences. The PI conducted confidential interviews in a private location near the ICU. Using confidential open‐ended, in‐depth interviews33 enabled the participating residents to provide frank answers to potentially sensitive questions.
The current study focuses on interviews with 17 residents; 8 from South Hospital, 6 from West Hospital, and 3 from North Hospital ICUs. Residents were at different training stages (years 14), and none declined participation. Interviews were audio‐recorded, transcribed professionally, checked for accuracy of transcription, and de‐identified. On average, each interview lasted about an hour, resulted in a 30‐page transcript, and focused on how residents experienced supervision for over two‐thirds of the transcript. Interviewees frequently described specific examples in vivid detail, yielding rich information. These data are consistent with Patton's observation that the validity, meaningfulness, and insights generated from qualitative inquiry have more to do with the information richness of the cases selected than with sample size.33(p245) Field notes, document review, and observations of routine activities supplemented the interviews.
Data Analysis
We coded and analyzed interview transcripts by applying the constant comparative method, in which we systematically examined and refined variations in the concepts that emerged from the data.33 To focus on the residents' perceptions of their training experiences, we began the data analysis without preexisting codes. We refined and reconstructed the coding scheme in several iterative stages. Based on the initial review by two investigators (M.T., H.S.), the PI and the coding team (T.D.G., S.M.) developed a preliminary coding scheme by induction, considering the residents' description of their experiences in the context of organizational research.34 They applied the coding scheme to three interview transcripts, and reevaluated and revised it based on comments from other investigators (H.S., E.J.T.).
The PI and the coding team met regularly to review and refine the codes. The PI and the coding team finalized the coding scheme only after it was validated by two other investigators and reapplied to the first set of interview transcripts. Constructing a detailed coding guide, we defined specific codes and classified them under seven broad themes.
We engaged in an iterative coding process to ensure credibility33 and consistent data analysis.34 Both coding team members independently coded each interview and resolved differences through consensus. The PI reviewed each coded transcript and met with the team to resolve any remaining coding disagreements. We used ATLAS.ti 5.0 software (ATLAS.ti Scientific Software Development, Berlin, Germany) to manage data, assist in detecting patterns, and compile relevant quotations.
We observed patterns in the data; we inductively identified themes that emerged from the data as well as those related to organizational research. During the period that we conducted interviews, new rules limiting residents' working hours were implemented.10 We did not discern any pattern changes before and after the new rules. To enhance data analysis credibility,34 two investigators (H.S., E.J.T.), serving as peer debriefers,35 examined whether the themes accurately reflected the data and rigorously searched for counter‐examples that contradicted the proposed themes.
RESULTS
Residents described how they were supervised not only by other physicians within the traditional medical hierarchy, but also by other professionals, including nurses, staff pharmacists, and clinical pharmacists, ie, interprofessional supervision (Figure 1). After presenting these results, we examine how physicians and other professionals used communication strategies during interprofessional supervision. Here we use the term residents to include trainees at all levels, from interns to upper‐level residents, and male pronouns for de‐identification.
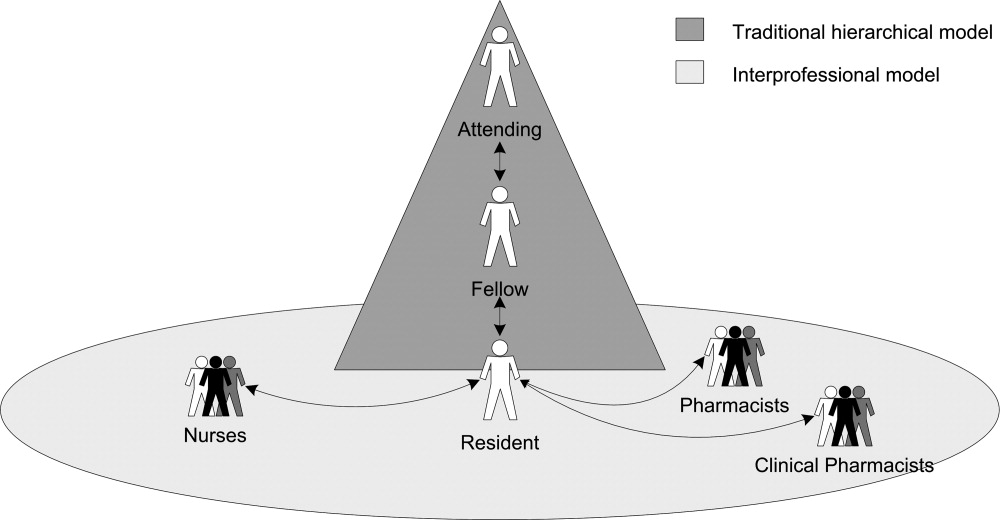
Initiating Supervision in the Traditional Medical Hierarchy
Residents described teaching rounds as the formal setting where the attending and other team members guided and gave feedback on their medication‐related decisions. After rounds, residents referred to the formal chain of command (from senior resident to fellow or attending) for their questions. However, residents also described enacting their own supervision by deciding when and how to ask for advice.
Residents developed different strategies for initiating supervision (Table 1). Some described a rule of thumb or personal decision‐making routine for determining when to approach a supervising physician with a question (eg, if the patient is in serious condition) (Table 1, columns 1 and 2). Others described how they decided when and how to ask an attending about their mistakes (Table 1, columns 3 and 4). As might be expected, residents' strategies usually reflected a desire for professional autonomy tempered with varying assessments of their own limitations (Table 1, columns 1 and 2, see Autonomy).
| Strategies for Asking Questions | Strategies for Seeking Feedback on Mistakes | ||
|---|---|---|---|
| When to Ask | When Not to Ask | When to Disclose a Mistake | How to Disclose a Mistake |
| Potential for adverse patient outcome: | Autonomy: | Potential for adverse patient outcome: | Direct: |
If you expect this is really bad, you try to cover yourselfand try to get the experience of somebody else, how to fix it .[And if it's less serious?] Yeah, then you can handle it. If I know it's a busy night, I let two or three admissions come in and then I call the fellow. But if the patient is really, really sick I call the fellow. | There's always a fellow to help us if we have questions. Being like almost a third year though, a lot of the things we kind of can handle on our own. Replacing the electrolytes and blood pressure medicines; we don't need hardly any oversight. | Well, I don't want to call a fellow. I think this medication, if it is wrong, is not going to kill a patient, is not going to adversely affect the outcome. | And I went straight up to the attending and I'll be like: Listen, this is what happened. Now I know. I know what happened, but how can I prevent this from happening again or what should I have done differently? |
| Medication choice: | Nights: | Medication choice and potential for adverse patient outcome: | Indirect: |
| If it's what type of medicine we give, then I usually contact my fellow. But most of the time I just make a decision on my own. | I never call Dr. [Attending] at night because you can get in touch with the fellow. The intern should talk to the attending, but the intern couldn't reach the attending. Sometimes it's like 2:00 or 3:00 in the morning. Then you can wait. If it's not an emergency, not in bad shape, you can wait. In the morning, when the attending physician is there, we'll talk about it. We can then ask. | If I know I have made a small mistake and I think it is inconsequential, I am not going to bother anybody. But if it is a different antibiotic that needed to be started, or what other medications might I have forgotten I would say [to the attending], I forgot to do this yesterday and I am sorry. | Instead of going up and saying, I made this mistake, you know, This is what I did and this is what happened, was it wrong? And I will let them tell me that this was a mistake, or not a mistake, and why. [If it's] really bad, you kind of talk with a fellow and say, This is what I've done. Is it okay? |
| Divergence from plan: | |||
If it's not something in the plan and we have to call someone, like an attending in a neurology service. Things that are discussed in advance, that may be potentially serious, I won't discuss, but basically anything that wasn't discussed in advance that I judge to be serious, then I will ask. | |||
We also identified patterns in how residents and their supervising physicians communicated when residents initiated supervision (Table 2, column 1). In general, residents considered attendings and fellows to be receptive to their questions. One resident explained: There is no one here who is unapproachableeven an attending. Nonetheless, residents reported using deferential language when initiating supervision (Table 2, column 1, row 2). Residents noted that attendings and fellows varied in their responses to questions and mistakes, as reflected in how they communicated with residents (Table 2, column 1, rows 1 and 3).
| Communication Strategies | Hierarchical Supervision: Resident Initiated Supervision | Interprofessional Supervision: Other Professional Initiated Supervision |
|---|---|---|
| ||
| Nonjudgmental language* | Fellow to resident: | Resident to nurse: |
| There's no dumb question. Ask. You can call me any time. | I'll say, It's not such a good idea for this reason. I feel they've [nurses] questioned you on it, so you deserve an appropriate answer. It's not okay to just be like, No, we're not gonna do that. | |
| Attending to resident: | ||
| Listen, [the mistake] could have happened to anybody . Now you know. Next time [you] do this, but [the patient is] gonna be okay. | ||
| Deferential language | Resident to difficult attending: | Pharmacist questions resident: |
| And when you call, you're polite and respectful: I'm sorry sir, I hate to bother you but I have a dumb question | The pharmacy called me up and said, Now listen, are you sure you want to give that dosage? | |
| Resident to fellow: | Nurse questions resident: | |
| Listen, in humbleness say, I don't know this, or am I doing this right? Can you help me out here? | [Nurses] might say like, Oh, you really? You sure you want to do this? | |
| Nurse guides resident: | ||
| Hey I know it's your decision, but this is what Dr. [Attending] would do. | ||
| Judgmental language | Attending response to a gross error: | Nurses questions resident: |
| What the hell were you thinking? We'll try to fix it, but God, what were you thinking? | At first [the nurses] were making fun of the resident who wrote [an unfamiliar medication order] . They just assume you're stupid until you prove them wrong, which is fine. But it gets annoying, too, because we did go to school for a long timewe actually know what the hell we're doing. | |
| Fellow response to resident question: | ||
| The cardiology fellow on call at 2 AM, when you call with a question will be like, Why would you even ask me that question? How could you not know that? | ||
Despite recognizing the importance of asking questions, several residents expressed conflicting beliefs; they raised concerns about the personal consequences of seeking assistance. For instance, one resident advocated: My point of view is I think it's wonderful when you ask questions. Cause that means you're conscientious enough to care about the patientsenough to do the right thing. However, we observed that when he interrupted the research interview to consult with a fellow, he prefaced his query with: Hey, I think this is a dumb question. Some residents expressed contradictory beliefs when they described their embarrassment over appearing stupid and fears of looking weak in front of supervising physicians, even those they perceived as being approachable. Indeed, for one resident, the attending's accessibility increased his anxiety: I don't want to lose respect by asking a stupid question.
Interprofessional Supervision
Residents described how other professionals used various methods of supervising their decision‐making (Table 3). Nurses and pharmacists intercepted medication orders and asked for clarifications, whereas clinical pharmacists also advised residents on ordering alternative medications (Table 3, row 1). Other professionals regularly double‐checked order implementation (Table 3, row 2). Nurses, in particular, routinely guided the future actions of residents by giving them cues and suggesting the next therapeutic tasks they should perform (Table 3, row 3). When assessing residents' clinical decisions, these professionals applied different guidelines (Table 4). Nurses compared residents' clinical decisions to their expectations for usual experience‐based practices (Table 4, column 1); pharmacists consulted and noticed deviations from national and hospital pharmacy standards (Table 4, column 2); and clinical pharmacists supplemented pharmacy standards with their professional judgment (Table 4, column 3).
| Provider Type | Example |
|---|---|
| Intercepting medication orders | |
| Nurses and pharmacists | Clarifying and correcting orders: |
The [pharmacist] said, How much do you really want to give? I was like, Okay. Let me take a look at it. And when I looked at it, I knew it wasn't calculated right. The nurse will call me and say, or the pharmacist will call me and say, Can you please change this? This is not the right dose. | |
| Clinical pharmacists | Suggesting alternative medications: |
| You know, this might be a better medication to use because the half life is | |
| Double‐checking order implementation | |
| Nurses | The nurses in [the unit] are wonderful about doing their own calculations, so if it's a rate, like if it's a drip, I've seen almost all the nurses go back over my drip and do the doses. |
| Clinical pharmacists | Cause even after rounds, he'll go back through and look at all, everything. And if he sees something that doesn't make sense or we could do different, he lets us know. |
| Guiding future actions | |
| Nurses | [The nurses] talk to you about everything. They see the labs before you. They see the labs in the morning and are like, His potassium is high, can you fix this? His blood pressure has been running up, do you want to give him something? They guide you towards making the right decision. |
| Clinical pharmacists | I wouldn't give these two [medications] together. There may be an interaction. |
| Nurses | Staff Pharmacists | Clinical Pharmacists |
|---|---|---|
| Experience on unit and with patients: | Standardized pharmacy guidelines for normal dosage ranges: | Standardized pharmacy guidelines for normal dosage ranges: |
| They're with the patients 12 hours a day. Some of them, they've been doing this for 30 years. | No, [the pharmacists] wouldn't have known on that one [error] because it was a normal it's within a normal range of dosing and it's not that it would cause any harm to the patient, but it was just that it needed to go to a higher dose. [I] did a very high dose, compared with the current dose. Then [the pharmacist] called me back and said, I think this is not the right dose. | [The clinical pharmacist is] the one who says, Oh, by the way, do you really want it IV or PO? Or It should be q 6 versus q 8. |
| Expectations for practice norms: | Patient‐specific dosage guidelines: | Clinical judgment based on specialized pharmacology expertise: |
| [The nurses] can pick up mistakes just as easily as anyone else because they are used to this environment and they are used to seeing all the orders that are written generally. | The [unit‐based] pharmacist came to me and said, This patient's almost in renal failure. Did you want to give them a smaller dose because of the renal failure? And I said, Oh, yeah. I didn't even think about that. | That's all [clinical pharmacists] know is medicine and research and studies, and so you know, there may be a paper that came out last week that none of us have even had a chance to read. But they would be up to date on it. So as far as all the drug trials and everything. |
| The usual practices in the unit: | ||
| An experienced nurse came to me and told me that in the unit, doctor, we used to do it 1 gram, not 0.5 gram. | ||
| The attending's preferences: | ||
| I know sometimes you'll want to start a certain pressor and the nurse will be like Well, Dr. [Attending] likes to use this pressor instead. | ||
| Formal standards: | ||
| A nurse would say, especially in the medications I wrote out to be canceled because of the antibiotic policy here . Doctor, the patient doesn't have any more doses of [antibiotic], what do you want me to start, or do you need to call the [antibiotic policy] team? |
Initiating Interprofessional Supervision
Residents, in turn, sought advice from other professionals. They actively engaged pharmacists in their supervision by asking questions ranging from basic clarifications to complex technical queries. You can just take [the clinical pharmacist] to the side and say, Hey listen. I forgot this medication. What am I supposed to give? It starts with an L, explained a resident. Other residents consulted clinical pharmacists for specialized expertise: The [clinical pharmacists] usually have a protocol that they like to follow that a lot of the residents and probably even a lot of the attendings aren't aware of. In one hospital, residents depended on the clinical pharmacists: They're always available and they really help out the team. In another hospital, unit‐based (on‐site) pharmacists served as an informal but extremely useful resource. Residents also relied on central pharmacy‐based staff, who provided essential backup, especially after‐hours: [The pharmacy is] always available, like if you have a questionthere's a medicine you've never given, but it's the middle of the night, nobody else around, you want to call the pharmacist. Residents uniformly noted that nurses monitored their decisions (Table 2, column 2; Table 4, column 1), and one specifically mentioned soliciting advice from nurses on organizing intravenous lines.
Communication Strategies for Managing Differences in Status and Expertise
Unlike the medical hierarchy that clearly differentiates among residents, fellows, and attendings, interdisciplinary differences were less clearly delineated. Residents were perceived as having higher status than other professionals, due in part to their medical education and responsibility for signing orders. Nurses and pharmacists, however, often had extensive experience and/or specialized training, and thus more expertise than residents. For instance, residents noticed their ambiguous status compared to nurses:
I don't know if some people might psychologically think it was better or worse, worse because it was coming from a nurse and maybe somebody would think that they wouldn't know as much or something like that. But other people would think of it as, they're a team member and they have the perfect right to know more. And maybe it's better because that way like maybe the fellow or attending wouldn't find out that you made a mistake [emphasis added].
To manage the ambiguous differences in their status, experience, and expertise, residents and other professionals used various communication strategies (Table 2, column 2). Residents consistently recounted that pharmacists and nurses used deferential language, for example, by asking questions, rather than directly stating their concerns (Table 2, column 2, row 2). One resident appreciated the unit‐nurses' indirect language: Over here they're really cool about it. They'll say, Is this right, are you sure about this? However, some residents also recalled that nurses used more direct language, such as I am not comfortable, especially when giving residents feedback on IV drug administration. In contrast, when asking pharmacists questions, residents consistently reported using nonjudgmental language, but not deferential language. However, some residents used judgmental language when they disagreed with a pharmacist's intervention.
Individual residents bitterly recalled their encounters with other professionals during previous rotations. One described nurses who were resident‐unfriendly and used judgmental language to mock a resident's choice of medications (Table 2, column 2, row 3). Another worked with clinical pharmacists who feel like they are teaching the residents and they are above the residents. These interactions illustrate how communication choices can create interprofessional tensions, especially when differences in status and expertise conflict or are unclear.
DISCUSSION
We analyzed interviews of residents working in medical ICUs to understand their supervision experiences related to medication safety. Although residents espoused beliefs in seeking assistance from supervising physicians and articulated strategies for doing so, many experienced difficulties in initiating supervision through the traditional medical hierarchy. Some residents were embarrassed by their mistaken decisions; others were concerned that their questions would reflect poorly on them.
Residents also received interprofessional supervision from nurses and pharmacists, who proactively monitored, intervened in, and guided residents' decisions. Other professionals evaluated residents' decisions by comparing them to distinctive professional guidelines and routinely used deferential language when conveying their concerns. Residents, in turn, asked other professionals for assistance.
We posit that interprofessional supervision clearly meets an accepted definition of supervision.3, 9 Residents received monitoring, guidance and feedback9(p828) from other professionals, who engaged in routine monitoring and in situation‐specific double‐checks of residents' clinical decisions, similar to those performed by supervising physicians.30 Moreover, other professionals demonstrated the ability to anticipate a doctor's strengths and weaknesses in particular clinical situations in order to maximize patient safety.9(p829)
Our study results have implications for graduate medical education (GME) reform. First, trainees experienced supervision as a two‐way interaction.36 Residents balanced the countervailing pressures to act independently or to seek a supervising physician's advice, in part, by developing strategies for deciding when to ask questions. Kennedy et al. identified similar rhetorical strategies.18 By asking questions about their clinical decisions, residents requested that supervising physicians guide their work; thus, they proactively initiated and thereby enacted their own supervision. Fostering the conditions for initiating supervision is essential, especially given the association between lack of effective supervision and adverse outcomes.5, 6, 1214
Second, residents expressed contradictory expectations about seeking advice from supervising physicians. Some residents were wary of approaching attending physicians for fear of appearing incompetent or being ridiculed.12, 16, 18, 31 However, we found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance. Whereas the perceived approachability of supervising physicians was important,18, 19 our exploratory findings suggest that it may be a necessary, but not a sufficient, condition for creating a learning environment. Creating a supportive learning environmentin which residents feel comfortable in revealing their perceived shortcomings to supervising physicians3begins with cultural changes, such as building medical teams,6 but such changes can be slow to develop.
Third, interprofessional supervision offers a strategy for improving supervision. The ubiquitous involvement of nursing and pharmacy staff in monitoring and intervening in residents' medication‐related decisions could result in overlooking their unique contributions to resident supervision. Mindful that supervising physicians evaluate them, residents selectively sought nonjudgmental advice from professionals outside the medical hierarchy. Therefore, improving supervision could entail offering residents ready access to other professionals who can advise them, especially during late night hours when supervising physicians might not be present.17, 27
The importance of interprofessional supervision has not been adequately recognized and emphasized in GME. Our study findings, if supported by future research, highlight how interpersonal communication techniques could influence both interprofessional supervision and hierarchical supervision among physicians. Medical team training programs3739 emphasize developing skills, such as mutual performance monitoring,40(p13) by training providers to raise and respond to potentially sensitive questions. Improving supervision by enhancing interpersonal communication skills may be important, not only when relative status differences are clear (ie, physician hierarchy), but also when status differences are ambiguous (ie, residents and other professionals). GME programs could consider incorporating these techniques into their formal curricula, as could programs for nursing and pharmacy staff.
Our study has several limitations. Because of the larger research project objectives, we focused on medication safety in medical ICU settings, where nurses and pharmacists may be especially vigilant and proactive in monitoring residents. Thus, our findings may be specific to medication issues and less relevant outside ICUs. We had a relatively small sample size and do not claim to generalize from it, although we believe it offers meaningful insights. We also did not continue enlarging our sample until reaching redundancy.35(p202) Nevertheless, the purposeful random sample of residents produced rich information. Indeed, some study results are consistent with previous resident education research,18 adding validity to our findings. Although the interview protocol was not designed specifically to investigate supervision, the resulting interviews yielded abundant data containing residents' detailed descriptions of how they experienced supervision. Whereas we were careful to note whether particular perceptions were unique to one resident, or shared by others, we recognize that the value of residents' observations is assessed by the quality of the insights they provide, not necessarily by the number of residents who described the same experience.
In conclusion, we found that residents experienced difficulties in initiating traditional hierarchical supervision related to medication safety in the ICU. However, they reported ubiquitous interprofessional supervision, albeit limited in scope, which they relied upon for nonjudgmental guidance in their therapeutic decision‐making, especially after‐hours. In our study, interprofessional supervision proved crucial to improving medication safety in the ICU.
- ,,.Resident supervision in the operating room: Does this impact on outcome?J Trauma.1993;35:556–560.
- ,.Supervision in the outpatient clinic: Effects on teaching and patient care.J Gen Intern Med.1993;8:378–380.
- Institute of Medicine (IOM).Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.Washington, DC:National Academic Press;2008.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives. Patient Safety and Graduate Medical Education. Washington, DC: Association of American Medical Colleges; 2003. Available at: https://services.aamc.org/publications/showfile.cfm?file=version13.pdf145:592–598.
- ,,,.Medical errors involving trainees: A study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167:2030–2036.
- .Resident duty hour reform and mortality in hospitalized patients.JAMA.2007;298:2865–2866.
- ,,,.Progressive independence in clinical training: A tradition worth defending?Acad Med.2005;80:S106–S111.
- ,.Effective supervision in clinical practice settings: A literature review.Med Educ.2000;34:827–840.
- Accreditation Council for Graduate Medical Education. ACGME Residency Review Committee Program Requirements in Critical Care Medicine. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/142pr707_ims.pdf Accessed August 14, 2009.
- ,.Resident supervision.Accreditation Council for Graduate Medical Education Bulletin.2005; September:15–17. Available at: http://www.acgme.org/acWebsite/bulletin/bulletin09_05. pdf. Accessed March 14,year="2009"2009.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: A qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204:533–540.
- ,,.Communication failures: An insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- ,,, et al.Attending doctors' perspectives on how residents learn.Med Educ.2007;41:1050–1058.
- ,,.Teaching but not learning: How medical residency programs handle errors.J Organiz Behav.2006;27:869–896.
- ,,,,.On‐call supervision and resident autonomy: From micromanager to absentee attending.Am J Med.2009;122:784–788.
- ,,,.Preserving professional credibility: Grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,,.Who wants feedback? An investigation of the variables influencing residents' feedback‐seeking behavior in relation to night shifts.Acad Med.2009;84:910–917.
- ,,, et al.A look into the nature and causes of human errors in the intensive care unit.Crit Care Med.1995;23:294–300.
- ,,, et al.The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care.Crit Care Med.2005;33:1694–1700.
- ,,,,,.Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units.Crit Care Med.1997;25:1289–1297.
- ,,,,,.Residents report on adverse events and their causes.Arch Intern Med.2005;165:2607–2613.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- ,,,,.Unit‐based clinical pharmacists' prevention of serious medication errors in pediatric inpatients.Am J Health Syst Pharm.2008;65:1254–1260.
- ,,,,.Improving medication safety in the ICU: The pharmacist's role.Hospital Pharmacy.2007;42:337–344.
- ,,,,,.Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting.J Interprof Care.2009;23:169–184.
- ,,,.Role of registered nurses in error prevention, discovery and correction.Qual Saf Health Care.2008;17:117–121.
- ,,, et al.Recovery from medical errors: The critical care nursing safety net.Jt Comm J Qual Patient Saf.2006;32:63–72.
- ,,,,.Clinical oversight: Conceptualizing the relationship between supervision and safety.J Gen Intern Med.2007;22:1080–1085.
- .To call or not to call: A judgment of risk by pre‐registration house officers.Med Educ.2008;42:938–944.
- ,.Classifying and interpreting threats to patient safety in hospitals: Insights from aviation.J Organiz Behav.2006;27:919–940.
- .Qualitative Research and Evaluation Methods.3rd ed.Thousand Oaks, CA:Sage Publications;2002.
- ,.Qualitative Data Analysis.2nd. ed.Thousand Oaks, CA:Sage Publications;2006.
- ,.Naturalistic Inquiry.Beverly Hills, CA:Sage Publications;1985.
- ,,.Supervision: A 2‐way street.Arch Intern Med.2008;168:1117.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: A randomized controlled trial.Obstet Gynecol.2007;109:48–55.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48:392–412.
- ,,,,,.Team training in the neonatal resuscitation program for interns: Teamwork and quality of resuscitations.Pediatrics.2010;125:539–546.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality 2005. Publication No. 05–0053. Available at: http://www.ahrq.gov/qual/medteam. Accessed October 15,2010.
Close supervision of residents potentially leads to fewer errors, lower patient mortality, and improved quality of care.19 An Institute of Medicine (IOM) report3 recommended improving supervision through more frequent consultations between residents and their supervisors. Although current Accreditation Council for Graduate Medical Education (ACGME) guidelines also recommend that attending physicians (attendings) supervise residents, detailed guidance about what constitutes adequate supervision and how it should be implemented is not well defined.10, 11 The ACGME stresses that supervision should promote resident autonomy in clinical care.10 However, when trainees act independently, it might lead to critical communication breakdowns and other patient safety concerns.5, 6, 1214 Although attendings can encourage (or discourage) residents from seeking advice,15, 16 residents also play important roles in asking for help (ie, initiating their own supervision).1719 Additional research is needed on how residents walk the fine line between exercising independence and seeking supervision.
Lack of resident supervision is especially problematic in high‐risk settings such as the medical intensive care unit (ICU), where medical errors are as frequent as 1.7 errors per patient per day,20, 21 and the adverse drug event rate is twice that of non‐ICU settings.22 Because medication errors are one of the most common errors residents make,23, 24 resident interactions with nursing and pharmacy staff may significantly influence medication safety in error‐prone ICUs.2529 Studies of traditional hierarchical supervision tend to overlook how interactions with other professionals influence resident training.12, 18, 30, 31
We define supervision as a process of providing trainees with monitoring, guidance, and feedback9(p828) as they care for patients.3 Whereas traditionally, supervisors are identified by their positions of formal authority in the medical chain of command; we conceptualize supervision as a process in which professionals engaged in supervisory activities need not have formal authority over their trainees.
To examine how residents seek supervision through both the traditional medical hierarchical chain of command (including attendings, fellows and senior residents) and interprofessional communication channels (including nursing and pharmacy staff), we conducted a qualitative study of residents working in ICUs in three tertiary care hospitals. Using semi‐structured interviews, we asked residents to describe how they experienced supervision as they provided medications to patients. Two broad research questions guided data analysis:
How do residents receive supervision from physicians in the traditional medical hierarchy?
How do residents receive supervision from other professionals (ie, nurses, staff pharmacists, and clinical pharmacists)?
METHODS
Study Design and Sample
We conducted a qualitative study using data from interviews with 17 residents working in the medical ICUs of three large tertiary care hospitals (henceforth referred to as South, West, and North hospitals). The interviews were conducted as part of a longitudinal research project that examined how hospitals learn from medication errors.32 The research project focused on hospitals where medication error prevention was salient because of a vulnerable patient population and/or extensive high‐hazard drug usage. For each ICU, the research design included interviews with 6 attendings, 6 fellows, and a purposeful random sample33 of 6 residents. The goal was to reduce bias from supervisors selecting study participants, and thus enhance the credibility of the small sample, rather than generalize from it.32 Surgical residents were excluded, because of the medication focus. The local Institutional Review Boards approved the research.
Drawing on preliminary analyses of research project data, we designed the current study to examine how residents experienced supervision.33 A qualitative research design was particularly appropriate, because this study is exploratory34 and examines the processes of how supervision is implemented.33 By gathering longitudinal data from 2001 to 2007 and from ICUs in different hospitals, we were able to search for persistent patterns (and systematic variations over time) in how residents experienced supervision that might not have been revealed by a cross‐sectional study in one hospital ICU.
Data Collection
The principal investigator ([PI] M.T.) interviewed residents to gather data about their experiences with medication safety and supervision when providing medication to ICU patients. A general interview guide33 addressed residents' personal experiences with ordering medications, receiving supervision, and their perceptions of institutional medication safety programs (see Supporting Table 1 in the online version of this article). The interviewer consistently prompted residents to provide examples of their supervision experiences. The PI conducted confidential interviews in a private location near the ICU. Using confidential open‐ended, in‐depth interviews33 enabled the participating residents to provide frank answers to potentially sensitive questions.
The current study focuses on interviews with 17 residents; 8 from South Hospital, 6 from West Hospital, and 3 from North Hospital ICUs. Residents were at different training stages (years 14), and none declined participation. Interviews were audio‐recorded, transcribed professionally, checked for accuracy of transcription, and de‐identified. On average, each interview lasted about an hour, resulted in a 30‐page transcript, and focused on how residents experienced supervision for over two‐thirds of the transcript. Interviewees frequently described specific examples in vivid detail, yielding rich information. These data are consistent with Patton's observation that the validity, meaningfulness, and insights generated from qualitative inquiry have more to do with the information richness of the cases selected than with sample size.33(p245) Field notes, document review, and observations of routine activities supplemented the interviews.
Data Analysis
We coded and analyzed interview transcripts by applying the constant comparative method, in which we systematically examined and refined variations in the concepts that emerged from the data.33 To focus on the residents' perceptions of their training experiences, we began the data analysis without preexisting codes. We refined and reconstructed the coding scheme in several iterative stages. Based on the initial review by two investigators (M.T., H.S.), the PI and the coding team (T.D.G., S.M.) developed a preliminary coding scheme by induction, considering the residents' description of their experiences in the context of organizational research.34 They applied the coding scheme to three interview transcripts, and reevaluated and revised it based on comments from other investigators (H.S., E.J.T.).
The PI and the coding team met regularly to review and refine the codes. The PI and the coding team finalized the coding scheme only after it was validated by two other investigators and reapplied to the first set of interview transcripts. Constructing a detailed coding guide, we defined specific codes and classified them under seven broad themes.
We engaged in an iterative coding process to ensure credibility33 and consistent data analysis.34 Both coding team members independently coded each interview and resolved differences through consensus. The PI reviewed each coded transcript and met with the team to resolve any remaining coding disagreements. We used ATLAS.ti 5.0 software (ATLAS.ti Scientific Software Development, Berlin, Germany) to manage data, assist in detecting patterns, and compile relevant quotations.
We observed patterns in the data; we inductively identified themes that emerged from the data as well as those related to organizational research. During the period that we conducted interviews, new rules limiting residents' working hours were implemented.10 We did not discern any pattern changes before and after the new rules. To enhance data analysis credibility,34 two investigators (H.S., E.J.T.), serving as peer debriefers,35 examined whether the themes accurately reflected the data and rigorously searched for counter‐examples that contradicted the proposed themes.
RESULTS
Residents described how they were supervised not only by other physicians within the traditional medical hierarchy, but also by other professionals, including nurses, staff pharmacists, and clinical pharmacists, ie, interprofessional supervision (Figure 1). After presenting these results, we examine how physicians and other professionals used communication strategies during interprofessional supervision. Here we use the term residents to include trainees at all levels, from interns to upper‐level residents, and male pronouns for de‐identification.
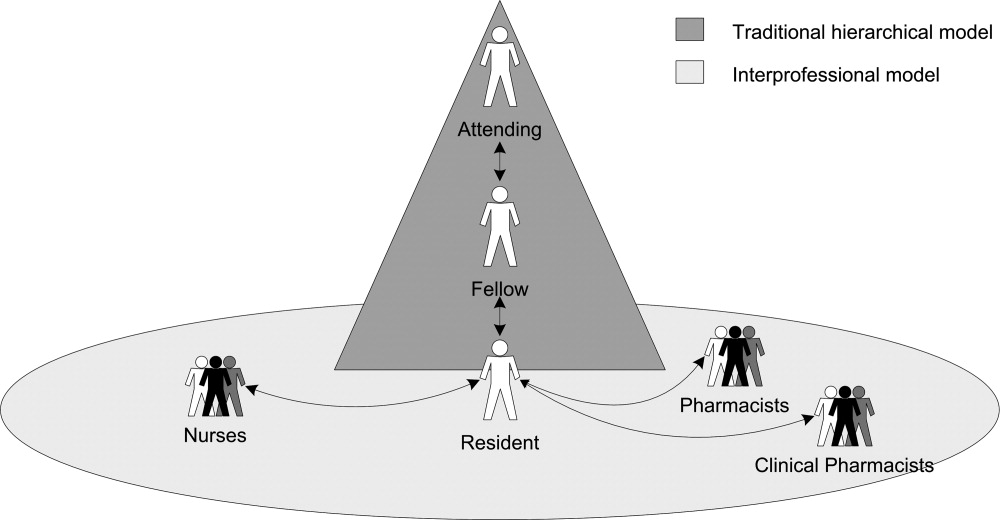
Initiating Supervision in the Traditional Medical Hierarchy
Residents described teaching rounds as the formal setting where the attending and other team members guided and gave feedback on their medication‐related decisions. After rounds, residents referred to the formal chain of command (from senior resident to fellow or attending) for their questions. However, residents also described enacting their own supervision by deciding when and how to ask for advice.
Residents developed different strategies for initiating supervision (Table 1). Some described a rule of thumb or personal decision‐making routine for determining when to approach a supervising physician with a question (eg, if the patient is in serious condition) (Table 1, columns 1 and 2). Others described how they decided when and how to ask an attending about their mistakes (Table 1, columns 3 and 4). As might be expected, residents' strategies usually reflected a desire for professional autonomy tempered with varying assessments of their own limitations (Table 1, columns 1 and 2, see Autonomy).
| Strategies for Asking Questions | Strategies for Seeking Feedback on Mistakes | ||
|---|---|---|---|
| When to Ask | When Not to Ask | When to Disclose a Mistake | How to Disclose a Mistake |
| Potential for adverse patient outcome: | Autonomy: | Potential for adverse patient outcome: | Direct: |
If you expect this is really bad, you try to cover yourselfand try to get the experience of somebody else, how to fix it .[And if it's less serious?] Yeah, then you can handle it. If I know it's a busy night, I let two or three admissions come in and then I call the fellow. But if the patient is really, really sick I call the fellow. | There's always a fellow to help us if we have questions. Being like almost a third year though, a lot of the things we kind of can handle on our own. Replacing the electrolytes and blood pressure medicines; we don't need hardly any oversight. | Well, I don't want to call a fellow. I think this medication, if it is wrong, is not going to kill a patient, is not going to adversely affect the outcome. | And I went straight up to the attending and I'll be like: Listen, this is what happened. Now I know. I know what happened, but how can I prevent this from happening again or what should I have done differently? |
| Medication choice: | Nights: | Medication choice and potential for adverse patient outcome: | Indirect: |
| If it's what type of medicine we give, then I usually contact my fellow. But most of the time I just make a decision on my own. | I never call Dr. [Attending] at night because you can get in touch with the fellow. The intern should talk to the attending, but the intern couldn't reach the attending. Sometimes it's like 2:00 or 3:00 in the morning. Then you can wait. If it's not an emergency, not in bad shape, you can wait. In the morning, when the attending physician is there, we'll talk about it. We can then ask. | If I know I have made a small mistake and I think it is inconsequential, I am not going to bother anybody. But if it is a different antibiotic that needed to be started, or what other medications might I have forgotten I would say [to the attending], I forgot to do this yesterday and I am sorry. | Instead of going up and saying, I made this mistake, you know, This is what I did and this is what happened, was it wrong? And I will let them tell me that this was a mistake, or not a mistake, and why. [If it's] really bad, you kind of talk with a fellow and say, This is what I've done. Is it okay? |
| Divergence from plan: | |||
If it's not something in the plan and we have to call someone, like an attending in a neurology service. Things that are discussed in advance, that may be potentially serious, I won't discuss, but basically anything that wasn't discussed in advance that I judge to be serious, then I will ask. | |||
We also identified patterns in how residents and their supervising physicians communicated when residents initiated supervision (Table 2, column 1). In general, residents considered attendings and fellows to be receptive to their questions. One resident explained: There is no one here who is unapproachableeven an attending. Nonetheless, residents reported using deferential language when initiating supervision (Table 2, column 1, row 2). Residents noted that attendings and fellows varied in their responses to questions and mistakes, as reflected in how they communicated with residents (Table 2, column 1, rows 1 and 3).
| Communication Strategies | Hierarchical Supervision: Resident Initiated Supervision | Interprofessional Supervision: Other Professional Initiated Supervision |
|---|---|---|
| ||
| Nonjudgmental language* | Fellow to resident: | Resident to nurse: |
| There's no dumb question. Ask. You can call me any time. | I'll say, It's not such a good idea for this reason. I feel they've [nurses] questioned you on it, so you deserve an appropriate answer. It's not okay to just be like, No, we're not gonna do that. | |
| Attending to resident: | ||
| Listen, [the mistake] could have happened to anybody . Now you know. Next time [you] do this, but [the patient is] gonna be okay. | ||
| Deferential language | Resident to difficult attending: | Pharmacist questions resident: |
| And when you call, you're polite and respectful: I'm sorry sir, I hate to bother you but I have a dumb question | The pharmacy called me up and said, Now listen, are you sure you want to give that dosage? | |
| Resident to fellow: | Nurse questions resident: | |
| Listen, in humbleness say, I don't know this, or am I doing this right? Can you help me out here? | [Nurses] might say like, Oh, you really? You sure you want to do this? | |
| Nurse guides resident: | ||
| Hey I know it's your decision, but this is what Dr. [Attending] would do. | ||
| Judgmental language | Attending response to a gross error: | Nurses questions resident: |
| What the hell were you thinking? We'll try to fix it, but God, what were you thinking? | At first [the nurses] were making fun of the resident who wrote [an unfamiliar medication order] . They just assume you're stupid until you prove them wrong, which is fine. But it gets annoying, too, because we did go to school for a long timewe actually know what the hell we're doing. | |
| Fellow response to resident question: | ||
| The cardiology fellow on call at 2 AM, when you call with a question will be like, Why would you even ask me that question? How could you not know that? | ||
Despite recognizing the importance of asking questions, several residents expressed conflicting beliefs; they raised concerns about the personal consequences of seeking assistance. For instance, one resident advocated: My point of view is I think it's wonderful when you ask questions. Cause that means you're conscientious enough to care about the patientsenough to do the right thing. However, we observed that when he interrupted the research interview to consult with a fellow, he prefaced his query with: Hey, I think this is a dumb question. Some residents expressed contradictory beliefs when they described their embarrassment over appearing stupid and fears of looking weak in front of supervising physicians, even those they perceived as being approachable. Indeed, for one resident, the attending's accessibility increased his anxiety: I don't want to lose respect by asking a stupid question.
Interprofessional Supervision
Residents described how other professionals used various methods of supervising their decision‐making (Table 3). Nurses and pharmacists intercepted medication orders and asked for clarifications, whereas clinical pharmacists also advised residents on ordering alternative medications (Table 3, row 1). Other professionals regularly double‐checked order implementation (Table 3, row 2). Nurses, in particular, routinely guided the future actions of residents by giving them cues and suggesting the next therapeutic tasks they should perform (Table 3, row 3). When assessing residents' clinical decisions, these professionals applied different guidelines (Table 4). Nurses compared residents' clinical decisions to their expectations for usual experience‐based practices (Table 4, column 1); pharmacists consulted and noticed deviations from national and hospital pharmacy standards (Table 4, column 2); and clinical pharmacists supplemented pharmacy standards with their professional judgment (Table 4, column 3).
| Provider Type | Example |
|---|---|
| Intercepting medication orders | |
| Nurses and pharmacists | Clarifying and correcting orders: |
The [pharmacist] said, How much do you really want to give? I was like, Okay. Let me take a look at it. And when I looked at it, I knew it wasn't calculated right. The nurse will call me and say, or the pharmacist will call me and say, Can you please change this? This is not the right dose. | |
| Clinical pharmacists | Suggesting alternative medications: |
| You know, this might be a better medication to use because the half life is | |
| Double‐checking order implementation | |
| Nurses | The nurses in [the unit] are wonderful about doing their own calculations, so if it's a rate, like if it's a drip, I've seen almost all the nurses go back over my drip and do the doses. |
| Clinical pharmacists | Cause even after rounds, he'll go back through and look at all, everything. And if he sees something that doesn't make sense or we could do different, he lets us know. |
| Guiding future actions | |
| Nurses | [The nurses] talk to you about everything. They see the labs before you. They see the labs in the morning and are like, His potassium is high, can you fix this? His blood pressure has been running up, do you want to give him something? They guide you towards making the right decision. |
| Clinical pharmacists | I wouldn't give these two [medications] together. There may be an interaction. |
| Nurses | Staff Pharmacists | Clinical Pharmacists |
|---|---|---|
| Experience on unit and with patients: | Standardized pharmacy guidelines for normal dosage ranges: | Standardized pharmacy guidelines for normal dosage ranges: |
| They're with the patients 12 hours a day. Some of them, they've been doing this for 30 years. | No, [the pharmacists] wouldn't have known on that one [error] because it was a normal it's within a normal range of dosing and it's not that it would cause any harm to the patient, but it was just that it needed to go to a higher dose. [I] did a very high dose, compared with the current dose. Then [the pharmacist] called me back and said, I think this is not the right dose. | [The clinical pharmacist is] the one who says, Oh, by the way, do you really want it IV or PO? Or It should be q 6 versus q 8. |
| Expectations for practice norms: | Patient‐specific dosage guidelines: | Clinical judgment based on specialized pharmacology expertise: |
| [The nurses] can pick up mistakes just as easily as anyone else because they are used to this environment and they are used to seeing all the orders that are written generally. | The [unit‐based] pharmacist came to me and said, This patient's almost in renal failure. Did you want to give them a smaller dose because of the renal failure? And I said, Oh, yeah. I didn't even think about that. | That's all [clinical pharmacists] know is medicine and research and studies, and so you know, there may be a paper that came out last week that none of us have even had a chance to read. But they would be up to date on it. So as far as all the drug trials and everything. |
| The usual practices in the unit: | ||
| An experienced nurse came to me and told me that in the unit, doctor, we used to do it 1 gram, not 0.5 gram. | ||
| The attending's preferences: | ||
| I know sometimes you'll want to start a certain pressor and the nurse will be like Well, Dr. [Attending] likes to use this pressor instead. | ||
| Formal standards: | ||
| A nurse would say, especially in the medications I wrote out to be canceled because of the antibiotic policy here . Doctor, the patient doesn't have any more doses of [antibiotic], what do you want me to start, or do you need to call the [antibiotic policy] team? |
Initiating Interprofessional Supervision
Residents, in turn, sought advice from other professionals. They actively engaged pharmacists in their supervision by asking questions ranging from basic clarifications to complex technical queries. You can just take [the clinical pharmacist] to the side and say, Hey listen. I forgot this medication. What am I supposed to give? It starts with an L, explained a resident. Other residents consulted clinical pharmacists for specialized expertise: The [clinical pharmacists] usually have a protocol that they like to follow that a lot of the residents and probably even a lot of the attendings aren't aware of. In one hospital, residents depended on the clinical pharmacists: They're always available and they really help out the team. In another hospital, unit‐based (on‐site) pharmacists served as an informal but extremely useful resource. Residents also relied on central pharmacy‐based staff, who provided essential backup, especially after‐hours: [The pharmacy is] always available, like if you have a questionthere's a medicine you've never given, but it's the middle of the night, nobody else around, you want to call the pharmacist. Residents uniformly noted that nurses monitored their decisions (Table 2, column 2; Table 4, column 1), and one specifically mentioned soliciting advice from nurses on organizing intravenous lines.
Communication Strategies for Managing Differences in Status and Expertise
Unlike the medical hierarchy that clearly differentiates among residents, fellows, and attendings, interdisciplinary differences were less clearly delineated. Residents were perceived as having higher status than other professionals, due in part to their medical education and responsibility for signing orders. Nurses and pharmacists, however, often had extensive experience and/or specialized training, and thus more expertise than residents. For instance, residents noticed their ambiguous status compared to nurses:
I don't know if some people might psychologically think it was better or worse, worse because it was coming from a nurse and maybe somebody would think that they wouldn't know as much or something like that. But other people would think of it as, they're a team member and they have the perfect right to know more. And maybe it's better because that way like maybe the fellow or attending wouldn't find out that you made a mistake [emphasis added].
To manage the ambiguous differences in their status, experience, and expertise, residents and other professionals used various communication strategies (Table 2, column 2). Residents consistently recounted that pharmacists and nurses used deferential language, for example, by asking questions, rather than directly stating their concerns (Table 2, column 2, row 2). One resident appreciated the unit‐nurses' indirect language: Over here they're really cool about it. They'll say, Is this right, are you sure about this? However, some residents also recalled that nurses used more direct language, such as I am not comfortable, especially when giving residents feedback on IV drug administration. In contrast, when asking pharmacists questions, residents consistently reported using nonjudgmental language, but not deferential language. However, some residents used judgmental language when they disagreed with a pharmacist's intervention.
Individual residents bitterly recalled their encounters with other professionals during previous rotations. One described nurses who were resident‐unfriendly and used judgmental language to mock a resident's choice of medications (Table 2, column 2, row 3). Another worked with clinical pharmacists who feel like they are teaching the residents and they are above the residents. These interactions illustrate how communication choices can create interprofessional tensions, especially when differences in status and expertise conflict or are unclear.
DISCUSSION
We analyzed interviews of residents working in medical ICUs to understand their supervision experiences related to medication safety. Although residents espoused beliefs in seeking assistance from supervising physicians and articulated strategies for doing so, many experienced difficulties in initiating supervision through the traditional medical hierarchy. Some residents were embarrassed by their mistaken decisions; others were concerned that their questions would reflect poorly on them.
Residents also received interprofessional supervision from nurses and pharmacists, who proactively monitored, intervened in, and guided residents' decisions. Other professionals evaluated residents' decisions by comparing them to distinctive professional guidelines and routinely used deferential language when conveying their concerns. Residents, in turn, asked other professionals for assistance.
We posit that interprofessional supervision clearly meets an accepted definition of supervision.3, 9 Residents received monitoring, guidance and feedback9(p828) from other professionals, who engaged in routine monitoring and in situation‐specific double‐checks of residents' clinical decisions, similar to those performed by supervising physicians.30 Moreover, other professionals demonstrated the ability to anticipate a doctor's strengths and weaknesses in particular clinical situations in order to maximize patient safety.9(p829)
Our study results have implications for graduate medical education (GME) reform. First, trainees experienced supervision as a two‐way interaction.36 Residents balanced the countervailing pressures to act independently or to seek a supervising physician's advice, in part, by developing strategies for deciding when to ask questions. Kennedy et al. identified similar rhetorical strategies.18 By asking questions about their clinical decisions, residents requested that supervising physicians guide their work; thus, they proactively initiated and thereby enacted their own supervision. Fostering the conditions for initiating supervision is essential, especially given the association between lack of effective supervision and adverse outcomes.5, 6, 1214
Second, residents expressed contradictory expectations about seeking advice from supervising physicians. Some residents were wary of approaching attending physicians for fear of appearing incompetent or being ridiculed.12, 16, 18, 31 However, we found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance. Whereas the perceived approachability of supervising physicians was important,18, 19 our exploratory findings suggest that it may be a necessary, but not a sufficient, condition for creating a learning environment. Creating a supportive learning environmentin which residents feel comfortable in revealing their perceived shortcomings to supervising physicians3begins with cultural changes, such as building medical teams,6 but such changes can be slow to develop.
Third, interprofessional supervision offers a strategy for improving supervision. The ubiquitous involvement of nursing and pharmacy staff in monitoring and intervening in residents' medication‐related decisions could result in overlooking their unique contributions to resident supervision. Mindful that supervising physicians evaluate them, residents selectively sought nonjudgmental advice from professionals outside the medical hierarchy. Therefore, improving supervision could entail offering residents ready access to other professionals who can advise them, especially during late night hours when supervising physicians might not be present.17, 27
The importance of interprofessional supervision has not been adequately recognized and emphasized in GME. Our study findings, if supported by future research, highlight how interpersonal communication techniques could influence both interprofessional supervision and hierarchical supervision among physicians. Medical team training programs3739 emphasize developing skills, such as mutual performance monitoring,40(p13) by training providers to raise and respond to potentially sensitive questions. Improving supervision by enhancing interpersonal communication skills may be important, not only when relative status differences are clear (ie, physician hierarchy), but also when status differences are ambiguous (ie, residents and other professionals). GME programs could consider incorporating these techniques into their formal curricula, as could programs for nursing and pharmacy staff.
Our study has several limitations. Because of the larger research project objectives, we focused on medication safety in medical ICU settings, where nurses and pharmacists may be especially vigilant and proactive in monitoring residents. Thus, our findings may be specific to medication issues and less relevant outside ICUs. We had a relatively small sample size and do not claim to generalize from it, although we believe it offers meaningful insights. We also did not continue enlarging our sample until reaching redundancy.35(p202) Nevertheless, the purposeful random sample of residents produced rich information. Indeed, some study results are consistent with previous resident education research,18 adding validity to our findings. Although the interview protocol was not designed specifically to investigate supervision, the resulting interviews yielded abundant data containing residents' detailed descriptions of how they experienced supervision. Whereas we were careful to note whether particular perceptions were unique to one resident, or shared by others, we recognize that the value of residents' observations is assessed by the quality of the insights they provide, not necessarily by the number of residents who described the same experience.
In conclusion, we found that residents experienced difficulties in initiating traditional hierarchical supervision related to medication safety in the ICU. However, they reported ubiquitous interprofessional supervision, albeit limited in scope, which they relied upon for nonjudgmental guidance in their therapeutic decision‐making, especially after‐hours. In our study, interprofessional supervision proved crucial to improving medication safety in the ICU.
Close supervision of residents potentially leads to fewer errors, lower patient mortality, and improved quality of care.19 An Institute of Medicine (IOM) report3 recommended improving supervision through more frequent consultations between residents and their supervisors. Although current Accreditation Council for Graduate Medical Education (ACGME) guidelines also recommend that attending physicians (attendings) supervise residents, detailed guidance about what constitutes adequate supervision and how it should be implemented is not well defined.10, 11 The ACGME stresses that supervision should promote resident autonomy in clinical care.10 However, when trainees act independently, it might lead to critical communication breakdowns and other patient safety concerns.5, 6, 1214 Although attendings can encourage (or discourage) residents from seeking advice,15, 16 residents also play important roles in asking for help (ie, initiating their own supervision).1719 Additional research is needed on how residents walk the fine line between exercising independence and seeking supervision.
Lack of resident supervision is especially problematic in high‐risk settings such as the medical intensive care unit (ICU), where medical errors are as frequent as 1.7 errors per patient per day,20, 21 and the adverse drug event rate is twice that of non‐ICU settings.22 Because medication errors are one of the most common errors residents make,23, 24 resident interactions with nursing and pharmacy staff may significantly influence medication safety in error‐prone ICUs.2529 Studies of traditional hierarchical supervision tend to overlook how interactions with other professionals influence resident training.12, 18, 30, 31
We define supervision as a process of providing trainees with monitoring, guidance, and feedback9(p828) as they care for patients.3 Whereas traditionally, supervisors are identified by their positions of formal authority in the medical chain of command; we conceptualize supervision as a process in which professionals engaged in supervisory activities need not have formal authority over their trainees.
To examine how residents seek supervision through both the traditional medical hierarchical chain of command (including attendings, fellows and senior residents) and interprofessional communication channels (including nursing and pharmacy staff), we conducted a qualitative study of residents working in ICUs in three tertiary care hospitals. Using semi‐structured interviews, we asked residents to describe how they experienced supervision as they provided medications to patients. Two broad research questions guided data analysis:
How do residents receive supervision from physicians in the traditional medical hierarchy?
How do residents receive supervision from other professionals (ie, nurses, staff pharmacists, and clinical pharmacists)?
METHODS
Study Design and Sample
We conducted a qualitative study using data from interviews with 17 residents working in the medical ICUs of three large tertiary care hospitals (henceforth referred to as South, West, and North hospitals). The interviews were conducted as part of a longitudinal research project that examined how hospitals learn from medication errors.32 The research project focused on hospitals where medication error prevention was salient because of a vulnerable patient population and/or extensive high‐hazard drug usage. For each ICU, the research design included interviews with 6 attendings, 6 fellows, and a purposeful random sample33 of 6 residents. The goal was to reduce bias from supervisors selecting study participants, and thus enhance the credibility of the small sample, rather than generalize from it.32 Surgical residents were excluded, because of the medication focus. The local Institutional Review Boards approved the research.
Drawing on preliminary analyses of research project data, we designed the current study to examine how residents experienced supervision.33 A qualitative research design was particularly appropriate, because this study is exploratory34 and examines the processes of how supervision is implemented.33 By gathering longitudinal data from 2001 to 2007 and from ICUs in different hospitals, we were able to search for persistent patterns (and systematic variations over time) in how residents experienced supervision that might not have been revealed by a cross‐sectional study in one hospital ICU.
Data Collection
The principal investigator ([PI] M.T.) interviewed residents to gather data about their experiences with medication safety and supervision when providing medication to ICU patients. A general interview guide33 addressed residents' personal experiences with ordering medications, receiving supervision, and their perceptions of institutional medication safety programs (see Supporting Table 1 in the online version of this article). The interviewer consistently prompted residents to provide examples of their supervision experiences. The PI conducted confidential interviews in a private location near the ICU. Using confidential open‐ended, in‐depth interviews33 enabled the participating residents to provide frank answers to potentially sensitive questions.
The current study focuses on interviews with 17 residents; 8 from South Hospital, 6 from West Hospital, and 3 from North Hospital ICUs. Residents were at different training stages (years 14), and none declined participation. Interviews were audio‐recorded, transcribed professionally, checked for accuracy of transcription, and de‐identified. On average, each interview lasted about an hour, resulted in a 30‐page transcript, and focused on how residents experienced supervision for over two‐thirds of the transcript. Interviewees frequently described specific examples in vivid detail, yielding rich information. These data are consistent with Patton's observation that the validity, meaningfulness, and insights generated from qualitative inquiry have more to do with the information richness of the cases selected than with sample size.33(p245) Field notes, document review, and observations of routine activities supplemented the interviews.
Data Analysis
We coded and analyzed interview transcripts by applying the constant comparative method, in which we systematically examined and refined variations in the concepts that emerged from the data.33 To focus on the residents' perceptions of their training experiences, we began the data analysis without preexisting codes. We refined and reconstructed the coding scheme in several iterative stages. Based on the initial review by two investigators (M.T., H.S.), the PI and the coding team (T.D.G., S.M.) developed a preliminary coding scheme by induction, considering the residents' description of their experiences in the context of organizational research.34 They applied the coding scheme to three interview transcripts, and reevaluated and revised it based on comments from other investigators (H.S., E.J.T.).
The PI and the coding team met regularly to review and refine the codes. The PI and the coding team finalized the coding scheme only after it was validated by two other investigators and reapplied to the first set of interview transcripts. Constructing a detailed coding guide, we defined specific codes and classified them under seven broad themes.
We engaged in an iterative coding process to ensure credibility33 and consistent data analysis.34 Both coding team members independently coded each interview and resolved differences through consensus. The PI reviewed each coded transcript and met with the team to resolve any remaining coding disagreements. We used ATLAS.ti 5.0 software (ATLAS.ti Scientific Software Development, Berlin, Germany) to manage data, assist in detecting patterns, and compile relevant quotations.
We observed patterns in the data; we inductively identified themes that emerged from the data as well as those related to organizational research. During the period that we conducted interviews, new rules limiting residents' working hours were implemented.10 We did not discern any pattern changes before and after the new rules. To enhance data analysis credibility,34 two investigators (H.S., E.J.T.), serving as peer debriefers,35 examined whether the themes accurately reflected the data and rigorously searched for counter‐examples that contradicted the proposed themes.
RESULTS
Residents described how they were supervised not only by other physicians within the traditional medical hierarchy, but also by other professionals, including nurses, staff pharmacists, and clinical pharmacists, ie, interprofessional supervision (Figure 1). After presenting these results, we examine how physicians and other professionals used communication strategies during interprofessional supervision. Here we use the term residents to include trainees at all levels, from interns to upper‐level residents, and male pronouns for de‐identification.
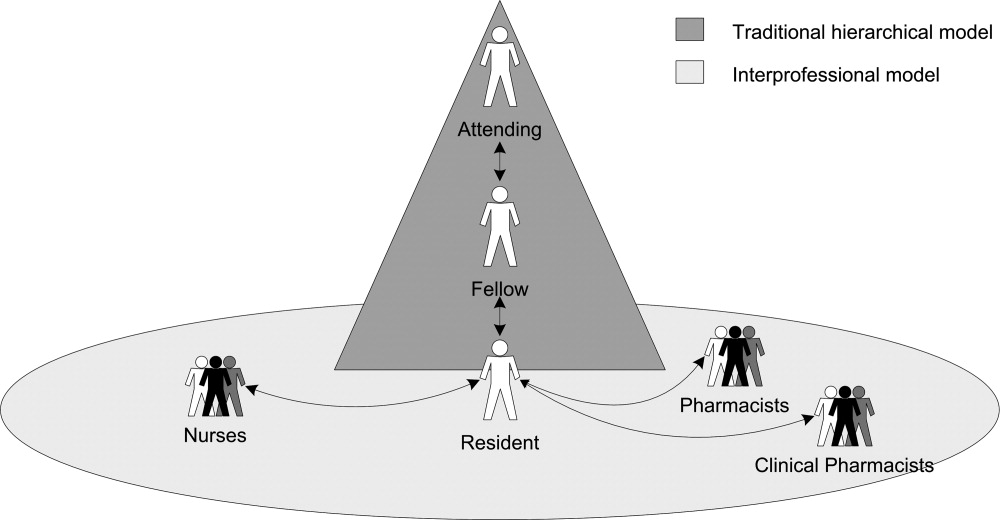
Initiating Supervision in the Traditional Medical Hierarchy
Residents described teaching rounds as the formal setting where the attending and other team members guided and gave feedback on their medication‐related decisions. After rounds, residents referred to the formal chain of command (from senior resident to fellow or attending) for their questions. However, residents also described enacting their own supervision by deciding when and how to ask for advice.
Residents developed different strategies for initiating supervision (Table 1). Some described a rule of thumb or personal decision‐making routine for determining when to approach a supervising physician with a question (eg, if the patient is in serious condition) (Table 1, columns 1 and 2). Others described how they decided when and how to ask an attending about their mistakes (Table 1, columns 3 and 4). As might be expected, residents' strategies usually reflected a desire for professional autonomy tempered with varying assessments of their own limitations (Table 1, columns 1 and 2, see Autonomy).
| Strategies for Asking Questions | Strategies for Seeking Feedback on Mistakes | ||
|---|---|---|---|
| When to Ask | When Not to Ask | When to Disclose a Mistake | How to Disclose a Mistake |
| Potential for adverse patient outcome: | Autonomy: | Potential for adverse patient outcome: | Direct: |
If you expect this is really bad, you try to cover yourselfand try to get the experience of somebody else, how to fix it .[And if it's less serious?] Yeah, then you can handle it. If I know it's a busy night, I let two or three admissions come in and then I call the fellow. But if the patient is really, really sick I call the fellow. | There's always a fellow to help us if we have questions. Being like almost a third year though, a lot of the things we kind of can handle on our own. Replacing the electrolytes and blood pressure medicines; we don't need hardly any oversight. | Well, I don't want to call a fellow. I think this medication, if it is wrong, is not going to kill a patient, is not going to adversely affect the outcome. | And I went straight up to the attending and I'll be like: Listen, this is what happened. Now I know. I know what happened, but how can I prevent this from happening again or what should I have done differently? |
| Medication choice: | Nights: | Medication choice and potential for adverse patient outcome: | Indirect: |
| If it's what type of medicine we give, then I usually contact my fellow. But most of the time I just make a decision on my own. | I never call Dr. [Attending] at night because you can get in touch with the fellow. The intern should talk to the attending, but the intern couldn't reach the attending. Sometimes it's like 2:00 or 3:00 in the morning. Then you can wait. If it's not an emergency, not in bad shape, you can wait. In the morning, when the attending physician is there, we'll talk about it. We can then ask. | If I know I have made a small mistake and I think it is inconsequential, I am not going to bother anybody. But if it is a different antibiotic that needed to be started, or what other medications might I have forgotten I would say [to the attending], I forgot to do this yesterday and I am sorry. | Instead of going up and saying, I made this mistake, you know, This is what I did and this is what happened, was it wrong? And I will let them tell me that this was a mistake, or not a mistake, and why. [If it's] really bad, you kind of talk with a fellow and say, This is what I've done. Is it okay? |
| Divergence from plan: | |||
If it's not something in the plan and we have to call someone, like an attending in a neurology service. Things that are discussed in advance, that may be potentially serious, I won't discuss, but basically anything that wasn't discussed in advance that I judge to be serious, then I will ask. | |||
We also identified patterns in how residents and their supervising physicians communicated when residents initiated supervision (Table 2, column 1). In general, residents considered attendings and fellows to be receptive to their questions. One resident explained: There is no one here who is unapproachableeven an attending. Nonetheless, residents reported using deferential language when initiating supervision (Table 2, column 1, row 2). Residents noted that attendings and fellows varied in their responses to questions and mistakes, as reflected in how they communicated with residents (Table 2, column 1, rows 1 and 3).
| Communication Strategies | Hierarchical Supervision: Resident Initiated Supervision | Interprofessional Supervision: Other Professional Initiated Supervision |
|---|---|---|
| ||
| Nonjudgmental language* | Fellow to resident: | Resident to nurse: |
| There's no dumb question. Ask. You can call me any time. | I'll say, It's not such a good idea for this reason. I feel they've [nurses] questioned you on it, so you deserve an appropriate answer. It's not okay to just be like, No, we're not gonna do that. | |
| Attending to resident: | ||
| Listen, [the mistake] could have happened to anybody . Now you know. Next time [you] do this, but [the patient is] gonna be okay. | ||
| Deferential language | Resident to difficult attending: | Pharmacist questions resident: |
| And when you call, you're polite and respectful: I'm sorry sir, I hate to bother you but I have a dumb question | The pharmacy called me up and said, Now listen, are you sure you want to give that dosage? | |
| Resident to fellow: | Nurse questions resident: | |
| Listen, in humbleness say, I don't know this, or am I doing this right? Can you help me out here? | [Nurses] might say like, Oh, you really? You sure you want to do this? | |
| Nurse guides resident: | ||
| Hey I know it's your decision, but this is what Dr. [Attending] would do. | ||
| Judgmental language | Attending response to a gross error: | Nurses questions resident: |
| What the hell were you thinking? We'll try to fix it, but God, what were you thinking? | At first [the nurses] were making fun of the resident who wrote [an unfamiliar medication order] . They just assume you're stupid until you prove them wrong, which is fine. But it gets annoying, too, because we did go to school for a long timewe actually know what the hell we're doing. | |
| Fellow response to resident question: | ||
| The cardiology fellow on call at 2 AM, when you call with a question will be like, Why would you even ask me that question? How could you not know that? | ||
Despite recognizing the importance of asking questions, several residents expressed conflicting beliefs; they raised concerns about the personal consequences of seeking assistance. For instance, one resident advocated: My point of view is I think it's wonderful when you ask questions. Cause that means you're conscientious enough to care about the patientsenough to do the right thing. However, we observed that when he interrupted the research interview to consult with a fellow, he prefaced his query with: Hey, I think this is a dumb question. Some residents expressed contradictory beliefs when they described their embarrassment over appearing stupid and fears of looking weak in front of supervising physicians, even those they perceived as being approachable. Indeed, for one resident, the attending's accessibility increased his anxiety: I don't want to lose respect by asking a stupid question.
Interprofessional Supervision
Residents described how other professionals used various methods of supervising their decision‐making (Table 3). Nurses and pharmacists intercepted medication orders and asked for clarifications, whereas clinical pharmacists also advised residents on ordering alternative medications (Table 3, row 1). Other professionals regularly double‐checked order implementation (Table 3, row 2). Nurses, in particular, routinely guided the future actions of residents by giving them cues and suggesting the next therapeutic tasks they should perform (Table 3, row 3). When assessing residents' clinical decisions, these professionals applied different guidelines (Table 4). Nurses compared residents' clinical decisions to their expectations for usual experience‐based practices (Table 4, column 1); pharmacists consulted and noticed deviations from national and hospital pharmacy standards (Table 4, column 2); and clinical pharmacists supplemented pharmacy standards with their professional judgment (Table 4, column 3).
| Provider Type | Example |
|---|---|
| Intercepting medication orders | |
| Nurses and pharmacists | Clarifying and correcting orders: |
The [pharmacist] said, How much do you really want to give? I was like, Okay. Let me take a look at it. And when I looked at it, I knew it wasn't calculated right. The nurse will call me and say, or the pharmacist will call me and say, Can you please change this? This is not the right dose. | |
| Clinical pharmacists | Suggesting alternative medications: |
| You know, this might be a better medication to use because the half life is | |
| Double‐checking order implementation | |
| Nurses | The nurses in [the unit] are wonderful about doing their own calculations, so if it's a rate, like if it's a drip, I've seen almost all the nurses go back over my drip and do the doses. |
| Clinical pharmacists | Cause even after rounds, he'll go back through and look at all, everything. And if he sees something that doesn't make sense or we could do different, he lets us know. |
| Guiding future actions | |
| Nurses | [The nurses] talk to you about everything. They see the labs before you. They see the labs in the morning and are like, His potassium is high, can you fix this? His blood pressure has been running up, do you want to give him something? They guide you towards making the right decision. |
| Clinical pharmacists | I wouldn't give these two [medications] together. There may be an interaction. |
| Nurses | Staff Pharmacists | Clinical Pharmacists |
|---|---|---|
| Experience on unit and with patients: | Standardized pharmacy guidelines for normal dosage ranges: | Standardized pharmacy guidelines for normal dosage ranges: |
| They're with the patients 12 hours a day. Some of them, they've been doing this for 30 years. | No, [the pharmacists] wouldn't have known on that one [error] because it was a normal it's within a normal range of dosing and it's not that it would cause any harm to the patient, but it was just that it needed to go to a higher dose. [I] did a very high dose, compared with the current dose. Then [the pharmacist] called me back and said, I think this is not the right dose. | [The clinical pharmacist is] the one who says, Oh, by the way, do you really want it IV or PO? Or It should be q 6 versus q 8. |
| Expectations for practice norms: | Patient‐specific dosage guidelines: | Clinical judgment based on specialized pharmacology expertise: |
| [The nurses] can pick up mistakes just as easily as anyone else because they are used to this environment and they are used to seeing all the orders that are written generally. | The [unit‐based] pharmacist came to me and said, This patient's almost in renal failure. Did you want to give them a smaller dose because of the renal failure? And I said, Oh, yeah. I didn't even think about that. | That's all [clinical pharmacists] know is medicine and research and studies, and so you know, there may be a paper that came out last week that none of us have even had a chance to read. But they would be up to date on it. So as far as all the drug trials and everything. |
| The usual practices in the unit: | ||
| An experienced nurse came to me and told me that in the unit, doctor, we used to do it 1 gram, not 0.5 gram. | ||
| The attending's preferences: | ||
| I know sometimes you'll want to start a certain pressor and the nurse will be like Well, Dr. [Attending] likes to use this pressor instead. | ||
| Formal standards: | ||
| A nurse would say, especially in the medications I wrote out to be canceled because of the antibiotic policy here . Doctor, the patient doesn't have any more doses of [antibiotic], what do you want me to start, or do you need to call the [antibiotic policy] team? |
Initiating Interprofessional Supervision
Residents, in turn, sought advice from other professionals. They actively engaged pharmacists in their supervision by asking questions ranging from basic clarifications to complex technical queries. You can just take [the clinical pharmacist] to the side and say, Hey listen. I forgot this medication. What am I supposed to give? It starts with an L, explained a resident. Other residents consulted clinical pharmacists for specialized expertise: The [clinical pharmacists] usually have a protocol that they like to follow that a lot of the residents and probably even a lot of the attendings aren't aware of. In one hospital, residents depended on the clinical pharmacists: They're always available and they really help out the team. In another hospital, unit‐based (on‐site) pharmacists served as an informal but extremely useful resource. Residents also relied on central pharmacy‐based staff, who provided essential backup, especially after‐hours: [The pharmacy is] always available, like if you have a questionthere's a medicine you've never given, but it's the middle of the night, nobody else around, you want to call the pharmacist. Residents uniformly noted that nurses monitored their decisions (Table 2, column 2; Table 4, column 1), and one specifically mentioned soliciting advice from nurses on organizing intravenous lines.
Communication Strategies for Managing Differences in Status and Expertise
Unlike the medical hierarchy that clearly differentiates among residents, fellows, and attendings, interdisciplinary differences were less clearly delineated. Residents were perceived as having higher status than other professionals, due in part to their medical education and responsibility for signing orders. Nurses and pharmacists, however, often had extensive experience and/or specialized training, and thus more expertise than residents. For instance, residents noticed their ambiguous status compared to nurses:
I don't know if some people might psychologically think it was better or worse, worse because it was coming from a nurse and maybe somebody would think that they wouldn't know as much or something like that. But other people would think of it as, they're a team member and they have the perfect right to know more. And maybe it's better because that way like maybe the fellow or attending wouldn't find out that you made a mistake [emphasis added].
To manage the ambiguous differences in their status, experience, and expertise, residents and other professionals used various communication strategies (Table 2, column 2). Residents consistently recounted that pharmacists and nurses used deferential language, for example, by asking questions, rather than directly stating their concerns (Table 2, column 2, row 2). One resident appreciated the unit‐nurses' indirect language: Over here they're really cool about it. They'll say, Is this right, are you sure about this? However, some residents also recalled that nurses used more direct language, such as I am not comfortable, especially when giving residents feedback on IV drug administration. In contrast, when asking pharmacists questions, residents consistently reported using nonjudgmental language, but not deferential language. However, some residents used judgmental language when they disagreed with a pharmacist's intervention.
Individual residents bitterly recalled their encounters with other professionals during previous rotations. One described nurses who were resident‐unfriendly and used judgmental language to mock a resident's choice of medications (Table 2, column 2, row 3). Another worked with clinical pharmacists who feel like they are teaching the residents and they are above the residents. These interactions illustrate how communication choices can create interprofessional tensions, especially when differences in status and expertise conflict or are unclear.
DISCUSSION
We analyzed interviews of residents working in medical ICUs to understand their supervision experiences related to medication safety. Although residents espoused beliefs in seeking assistance from supervising physicians and articulated strategies for doing so, many experienced difficulties in initiating supervision through the traditional medical hierarchy. Some residents were embarrassed by their mistaken decisions; others were concerned that their questions would reflect poorly on them.
Residents also received interprofessional supervision from nurses and pharmacists, who proactively monitored, intervened in, and guided residents' decisions. Other professionals evaluated residents' decisions by comparing them to distinctive professional guidelines and routinely used deferential language when conveying their concerns. Residents, in turn, asked other professionals for assistance.
We posit that interprofessional supervision clearly meets an accepted definition of supervision.3, 9 Residents received monitoring, guidance and feedback9(p828) from other professionals, who engaged in routine monitoring and in situation‐specific double‐checks of residents' clinical decisions, similar to those performed by supervising physicians.30 Moreover, other professionals demonstrated the ability to anticipate a doctor's strengths and weaknesses in particular clinical situations in order to maximize patient safety.9(p829)
Our study results have implications for graduate medical education (GME) reform. First, trainees experienced supervision as a two‐way interaction.36 Residents balanced the countervailing pressures to act independently or to seek a supervising physician's advice, in part, by developing strategies for deciding when to ask questions. Kennedy et al. identified similar rhetorical strategies.18 By asking questions about their clinical decisions, residents requested that supervising physicians guide their work; thus, they proactively initiated and thereby enacted their own supervision. Fostering the conditions for initiating supervision is essential, especially given the association between lack of effective supervision and adverse outcomes.5, 6, 1214
Second, residents expressed contradictory expectations about seeking advice from supervising physicians. Some residents were wary of approaching attending physicians for fear of appearing incompetent or being ridiculed.12, 16, 18, 31 However, we found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance. Whereas the perceived approachability of supervising physicians was important,18, 19 our exploratory findings suggest that it may be a necessary, but not a sufficient, condition for creating a learning environment. Creating a supportive learning environmentin which residents feel comfortable in revealing their perceived shortcomings to supervising physicians3begins with cultural changes, such as building medical teams,6 but such changes can be slow to develop.
Third, interprofessional supervision offers a strategy for improving supervision. The ubiquitous involvement of nursing and pharmacy staff in monitoring and intervening in residents' medication‐related decisions could result in overlooking their unique contributions to resident supervision. Mindful that supervising physicians evaluate them, residents selectively sought nonjudgmental advice from professionals outside the medical hierarchy. Therefore, improving supervision could entail offering residents ready access to other professionals who can advise them, especially during late night hours when supervising physicians might not be present.17, 27
The importance of interprofessional supervision has not been adequately recognized and emphasized in GME. Our study findings, if supported by future research, highlight how interpersonal communication techniques could influence both interprofessional supervision and hierarchical supervision among physicians. Medical team training programs3739 emphasize developing skills, such as mutual performance monitoring,40(p13) by training providers to raise and respond to potentially sensitive questions. Improving supervision by enhancing interpersonal communication skills may be important, not only when relative status differences are clear (ie, physician hierarchy), but also when status differences are ambiguous (ie, residents and other professionals). GME programs could consider incorporating these techniques into their formal curricula, as could programs for nursing and pharmacy staff.
Our study has several limitations. Because of the larger research project objectives, we focused on medication safety in medical ICU settings, where nurses and pharmacists may be especially vigilant and proactive in monitoring residents. Thus, our findings may be specific to medication issues and less relevant outside ICUs. We had a relatively small sample size and do not claim to generalize from it, although we believe it offers meaningful insights. We also did not continue enlarging our sample until reaching redundancy.35(p202) Nevertheless, the purposeful random sample of residents produced rich information. Indeed, some study results are consistent with previous resident education research,18 adding validity to our findings. Although the interview protocol was not designed specifically to investigate supervision, the resulting interviews yielded abundant data containing residents' detailed descriptions of how they experienced supervision. Whereas we were careful to note whether particular perceptions were unique to one resident, or shared by others, we recognize that the value of residents' observations is assessed by the quality of the insights they provide, not necessarily by the number of residents who described the same experience.
In conclusion, we found that residents experienced difficulties in initiating traditional hierarchical supervision related to medication safety in the ICU. However, they reported ubiquitous interprofessional supervision, albeit limited in scope, which they relied upon for nonjudgmental guidance in their therapeutic decision‐making, especially after‐hours. In our study, interprofessional supervision proved crucial to improving medication safety in the ICU.
- ,,.Resident supervision in the operating room: Does this impact on outcome?J Trauma.1993;35:556–560.
- ,.Supervision in the outpatient clinic: Effects on teaching and patient care.J Gen Intern Med.1993;8:378–380.
- Institute of Medicine (IOM).Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.Washington, DC:National Academic Press;2008.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives. Patient Safety and Graduate Medical Education. Washington, DC: Association of American Medical Colleges; 2003. Available at: https://services.aamc.org/publications/showfile.cfm?file=version13.pdf145:592–598.
- ,,,.Medical errors involving trainees: A study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167:2030–2036.
- .Resident duty hour reform and mortality in hospitalized patients.JAMA.2007;298:2865–2866.
- ,,,.Progressive independence in clinical training: A tradition worth defending?Acad Med.2005;80:S106–S111.
- ,.Effective supervision in clinical practice settings: A literature review.Med Educ.2000;34:827–840.
- Accreditation Council for Graduate Medical Education. ACGME Residency Review Committee Program Requirements in Critical Care Medicine. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/142pr707_ims.pdf Accessed August 14, 2009.
- ,.Resident supervision.Accreditation Council for Graduate Medical Education Bulletin.2005; September:15–17. Available at: http://www.acgme.org/acWebsite/bulletin/bulletin09_05. pdf. Accessed March 14,year="2009"2009.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: A qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204:533–540.
- ,,.Communication failures: An insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- ,,, et al.Attending doctors' perspectives on how residents learn.Med Educ.2007;41:1050–1058.
- ,,.Teaching but not learning: How medical residency programs handle errors.J Organiz Behav.2006;27:869–896.
- ,,,,.On‐call supervision and resident autonomy: From micromanager to absentee attending.Am J Med.2009;122:784–788.
- ,,,.Preserving professional credibility: Grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,,.Who wants feedback? An investigation of the variables influencing residents' feedback‐seeking behavior in relation to night shifts.Acad Med.2009;84:910–917.
- ,,, et al.A look into the nature and causes of human errors in the intensive care unit.Crit Care Med.1995;23:294–300.
- ,,, et al.The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care.Crit Care Med.2005;33:1694–1700.
- ,,,,,.Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units.Crit Care Med.1997;25:1289–1297.
- ,,,,,.Residents report on adverse events and their causes.Arch Intern Med.2005;165:2607–2613.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- ,,,,.Unit‐based clinical pharmacists' prevention of serious medication errors in pediatric inpatients.Am J Health Syst Pharm.2008;65:1254–1260.
- ,,,,.Improving medication safety in the ICU: The pharmacist's role.Hospital Pharmacy.2007;42:337–344.
- ,,,,,.Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting.J Interprof Care.2009;23:169–184.
- ,,,.Role of registered nurses in error prevention, discovery and correction.Qual Saf Health Care.2008;17:117–121.
- ,,, et al.Recovery from medical errors: The critical care nursing safety net.Jt Comm J Qual Patient Saf.2006;32:63–72.
- ,,,,.Clinical oversight: Conceptualizing the relationship between supervision and safety.J Gen Intern Med.2007;22:1080–1085.
- .To call or not to call: A judgment of risk by pre‐registration house officers.Med Educ.2008;42:938–944.
- ,.Classifying and interpreting threats to patient safety in hospitals: Insights from aviation.J Organiz Behav.2006;27:919–940.
- .Qualitative Research and Evaluation Methods.3rd ed.Thousand Oaks, CA:Sage Publications;2002.
- ,.Qualitative Data Analysis.2nd. ed.Thousand Oaks, CA:Sage Publications;2006.
- ,.Naturalistic Inquiry.Beverly Hills, CA:Sage Publications;1985.
- ,,.Supervision: A 2‐way street.Arch Intern Med.2008;168:1117.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: A randomized controlled trial.Obstet Gynecol.2007;109:48–55.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48:392–412.
- ,,,,,.Team training in the neonatal resuscitation program for interns: Teamwork and quality of resuscitations.Pediatrics.2010;125:539–546.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality 2005. Publication No. 05–0053. Available at: http://www.ahrq.gov/qual/medteam. Accessed October 15,2010.
- ,,.Resident supervision in the operating room: Does this impact on outcome?J Trauma.1993;35:556–560.
- ,.Supervision in the outpatient clinic: Effects on teaching and patient care.J Gen Intern Med.1993;8:378–380.
- Institute of Medicine (IOM).Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.Washington, DC:National Academic Press;2008.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives. Patient Safety and Graduate Medical Education. Washington, DC: Association of American Medical Colleges; 2003. Available at: https://services.aamc.org/publications/showfile.cfm?file=version13.pdf145:592–598.
- ,,,.Medical errors involving trainees: A study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167:2030–2036.
- .Resident duty hour reform and mortality in hospitalized patients.JAMA.2007;298:2865–2866.
- ,,,.Progressive independence in clinical training: A tradition worth defending?Acad Med.2005;80:S106–S111.
- ,.Effective supervision in clinical practice settings: A literature review.Med Educ.2000;34:827–840.
- Accreditation Council for Graduate Medical Education. ACGME Residency Review Committee Program Requirements in Critical Care Medicine. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/142pr707_ims.pdf Accessed August 14, 2009.
- ,.Resident supervision.Accreditation Council for Graduate Medical Education Bulletin.2005; September:15–17. Available at: http://www.acgme.org/acWebsite/bulletin/bulletin09_05. pdf. Accessed March 14,year="2009"2009.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: A qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204:533–540.
- ,,.Communication failures: An insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- ,,, et al.Attending doctors' perspectives on how residents learn.Med Educ.2007;41:1050–1058.
- ,,.Teaching but not learning: How medical residency programs handle errors.J Organiz Behav.2006;27:869–896.
- ,,,,.On‐call supervision and resident autonomy: From micromanager to absentee attending.Am J Med.2009;122:784–788.
- ,,,.Preserving professional credibility: Grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,,.Who wants feedback? An investigation of the variables influencing residents' feedback‐seeking behavior in relation to night shifts.Acad Med.2009;84:910–917.
- ,,, et al.A look into the nature and causes of human errors in the intensive care unit.Crit Care Med.1995;23:294–300.
- ,,, et al.The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care.Crit Care Med.2005;33:1694–1700.
- ,,,,,.Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units.Crit Care Med.1997;25:1289–1297.
- ,,,,,.Residents report on adverse events and their causes.Arch Intern Med.2005;165:2607–2613.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- ,,,,.Unit‐based clinical pharmacists' prevention of serious medication errors in pediatric inpatients.Am J Health Syst Pharm.2008;65:1254–1260.
- ,,,,.Improving medication safety in the ICU: The pharmacist's role.Hospital Pharmacy.2007;42:337–344.
- ,,,,,.Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting.J Interprof Care.2009;23:169–184.
- ,,,.Role of registered nurses in error prevention, discovery and correction.Qual Saf Health Care.2008;17:117–121.
- ,,, et al.Recovery from medical errors: The critical care nursing safety net.Jt Comm J Qual Patient Saf.2006;32:63–72.
- ,,,,.Clinical oversight: Conceptualizing the relationship between supervision and safety.J Gen Intern Med.2007;22:1080–1085.
- .To call or not to call: A judgment of risk by pre‐registration house officers.Med Educ.2008;42:938–944.
- ,.Classifying and interpreting threats to patient safety in hospitals: Insights from aviation.J Organiz Behav.2006;27:919–940.
- .Qualitative Research and Evaluation Methods.3rd ed.Thousand Oaks, CA:Sage Publications;2002.
- ,.Qualitative Data Analysis.2nd. ed.Thousand Oaks, CA:Sage Publications;2006.
- ,.Naturalistic Inquiry.Beverly Hills, CA:Sage Publications;1985.
- ,,.Supervision: A 2‐way street.Arch Intern Med.2008;168:1117.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: A randomized controlled trial.Obstet Gynecol.2007;109:48–55.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48:392–412.
- ,,,,,.Team training in the neonatal resuscitation program for interns: Teamwork and quality of resuscitations.Pediatrics.2010;125:539–546.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality 2005. Publication No. 05–0053. Available at: http://www.ahrq.gov/qual/medteam. Accessed October 15,2010.
Copyright © 2011 Society of Hospital Medicine