User login
AMSTERDAM – The optimal level of systolic blood pressure in all patients above age 55 appears to be 120-139 mm Hg, according to controversial data from a large, observational, U.S. population–based cohort study.
Results from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study suggest that a systolic blood pressure (SBP) in that range is associated with the lowest rates of cardiovascular events, stroke, and all-cause mortality, even in individuals aged 75 years and up. Since REGARDS is an observational study, this proposed target SBP range should be viewed as a testable hypothesis worthy of confirmation in a large, randomized, antihypertensive treatment study in the elderly, Dr. Maciej Banach said at the annual congress of the European Society of Cardiology (ESC).
REGARDS also turned up evidence supportive of the existence of the long-controversial J-curve, with an increased rate of adverse events noted in subjects with an SBP below 120 mm Hg, added Dr. Banach, professor and head of the department of hypertension at the Medical University of Lodz (Poland).
But discussant Christi Deaton, Ph.D., was quick to slam on the brakes in response to Dr. Banach’s suggestion that 120-139 mm Hg looks like the new optimal in older patients. She noted that the REGARDS proposal is at odds with the latest ESC hypertension guidelines, issued just a couple of months ago.
The evidence-based ESC guidelines (J. Hypertens. 2013;31:1281-357) offer as a class I recommendation an SBP target of 140-150 mm Hg for elderly patients under age 80, with consideration of a target below 140 mm Hg for the subgroup of elderly patients who are fit, noted Dr. Deaton, professor of nursing at the University of Manchester (U.K.), and a member of the ESC Guidelines Committee.
The American College of Cardiology/American Heart Association guidelines, in contrast, recommend a target of less than 140/90 in 65- to 79-year-olds, and an SBP of 140-145 mm Hg, if tolerated, in those aged 80 years and up (Circulation 2011;123:2434-506).
"The hypothesis from this REGARDS analysis is a bold one," she observed. "But we need large, well-designed intervention trials in older patients, particularly in underrepresented groups, before we can set lower blood pressure targets than are currently recommended in our guidelines."
The REGARDS study is a National Institutes of Health–sponsored observational study of 30,329 U.S. subjects aged 45 years or older, with overrepresentation of blacks and residents of the nation’s southeastern "stroke belt." Dr. Banach presented an analysis of 13,948 REGARDS participants aged 55 years or older who were taking antihypertensive medications at baseline. They have thus far been followed for a median of 6 years for all-cause mortality, and slightly less for first occurrence of stroke or coronary heart disease.
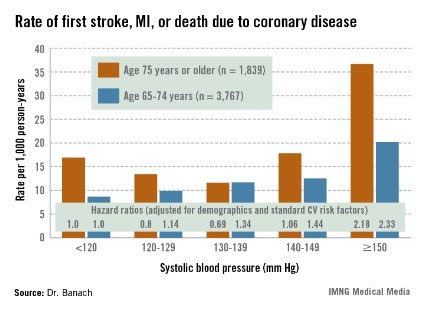
The suggestion of a J-curve was strongest for the composite endpoint of a first stroke, nonfatal myocardial infarction (MI), or death due to coronary heart disease in subjects aged 75 years or older (see graphic). There was no significant relationship between stroke and SBP category for subjects under age 75; however, over age 75, stroke rates were highest in those with an SBP less than 120 or more than 150 mm Hg.
All-cause mortality showed a linear relationship with increasing SBP in subjects aged 55-74 years, but no relationship in those over age 75.
Dr. Deaton applauded the REGARDS investigators for focusing on a high-risk population that’s "certainly underrepresented in our clinical intervention trials," but she cited several major study limitations. One is that only baseline blood pressure measurements were available.
"Importantly," she observed, "we don’t know what happened to blood pressure control during these years of follow-up."
In addition, the incidence rates of stroke, MI, and other major adverse events were relatively low in some subgroups. The planned further follow-up in REGARDS should bring greater clarity, Dr. Deaton added.
Dr. Banach and Dr. Deaton reported having no financial conflicts of interest.
AMSTERDAM – The optimal level of systolic blood pressure in all patients above age 55 appears to be 120-139 mm Hg, according to controversial data from a large, observational, U.S. population–based cohort study.
Results from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study suggest that a systolic blood pressure (SBP) in that range is associated with the lowest rates of cardiovascular events, stroke, and all-cause mortality, even in individuals aged 75 years and up. Since REGARDS is an observational study, this proposed target SBP range should be viewed as a testable hypothesis worthy of confirmation in a large, randomized, antihypertensive treatment study in the elderly, Dr. Maciej Banach said at the annual congress of the European Society of Cardiology (ESC).
REGARDS also turned up evidence supportive of the existence of the long-controversial J-curve, with an increased rate of adverse events noted in subjects with an SBP below 120 mm Hg, added Dr. Banach, professor and head of the department of hypertension at the Medical University of Lodz (Poland).
But discussant Christi Deaton, Ph.D., was quick to slam on the brakes in response to Dr. Banach’s suggestion that 120-139 mm Hg looks like the new optimal in older patients. She noted that the REGARDS proposal is at odds with the latest ESC hypertension guidelines, issued just a couple of months ago.
The evidence-based ESC guidelines (J. Hypertens. 2013;31:1281-357) offer as a class I recommendation an SBP target of 140-150 mm Hg for elderly patients under age 80, with consideration of a target below 140 mm Hg for the subgroup of elderly patients who are fit, noted Dr. Deaton, professor of nursing at the University of Manchester (U.K.), and a member of the ESC Guidelines Committee.
The American College of Cardiology/American Heart Association guidelines, in contrast, recommend a target of less than 140/90 in 65- to 79-year-olds, and an SBP of 140-145 mm Hg, if tolerated, in those aged 80 years and up (Circulation 2011;123:2434-506).
"The hypothesis from this REGARDS analysis is a bold one," she observed. "But we need large, well-designed intervention trials in older patients, particularly in underrepresented groups, before we can set lower blood pressure targets than are currently recommended in our guidelines."
The REGARDS study is a National Institutes of Health–sponsored observational study of 30,329 U.S. subjects aged 45 years or older, with overrepresentation of blacks and residents of the nation’s southeastern "stroke belt." Dr. Banach presented an analysis of 13,948 REGARDS participants aged 55 years or older who were taking antihypertensive medications at baseline. They have thus far been followed for a median of 6 years for all-cause mortality, and slightly less for first occurrence of stroke or coronary heart disease.
The suggestion of a J-curve was strongest for the composite endpoint of a first stroke, nonfatal myocardial infarction (MI), or death due to coronary heart disease in subjects aged 75 years or older (see graphic). There was no significant relationship between stroke and SBP category for subjects under age 75; however, over age 75, stroke rates were highest in those with an SBP less than 120 or more than 150 mm Hg.
All-cause mortality showed a linear relationship with increasing SBP in subjects aged 55-74 years, but no relationship in those over age 75.
Dr. Deaton applauded the REGARDS investigators for focusing on a high-risk population that’s "certainly underrepresented in our clinical intervention trials," but she cited several major study limitations. One is that only baseline blood pressure measurements were available.
"Importantly," she observed, "we don’t know what happened to blood pressure control during these years of follow-up."
In addition, the incidence rates of stroke, MI, and other major adverse events were relatively low in some subgroups. The planned further follow-up in REGARDS should bring greater clarity, Dr. Deaton added.
Dr. Banach and Dr. Deaton reported having no financial conflicts of interest.
AMSTERDAM – The optimal level of systolic blood pressure in all patients above age 55 appears to be 120-139 mm Hg, according to controversial data from a large, observational, U.S. population–based cohort study.
Results from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study suggest that a systolic blood pressure (SBP) in that range is associated with the lowest rates of cardiovascular events, stroke, and all-cause mortality, even in individuals aged 75 years and up. Since REGARDS is an observational study, this proposed target SBP range should be viewed as a testable hypothesis worthy of confirmation in a large, randomized, antihypertensive treatment study in the elderly, Dr. Maciej Banach said at the annual congress of the European Society of Cardiology (ESC).
REGARDS also turned up evidence supportive of the existence of the long-controversial J-curve, with an increased rate of adverse events noted in subjects with an SBP below 120 mm Hg, added Dr. Banach, professor and head of the department of hypertension at the Medical University of Lodz (Poland).
But discussant Christi Deaton, Ph.D., was quick to slam on the brakes in response to Dr. Banach’s suggestion that 120-139 mm Hg looks like the new optimal in older patients. She noted that the REGARDS proposal is at odds with the latest ESC hypertension guidelines, issued just a couple of months ago.
The evidence-based ESC guidelines (J. Hypertens. 2013;31:1281-357) offer as a class I recommendation an SBP target of 140-150 mm Hg for elderly patients under age 80, with consideration of a target below 140 mm Hg for the subgroup of elderly patients who are fit, noted Dr. Deaton, professor of nursing at the University of Manchester (U.K.), and a member of the ESC Guidelines Committee.
The American College of Cardiology/American Heart Association guidelines, in contrast, recommend a target of less than 140/90 in 65- to 79-year-olds, and an SBP of 140-145 mm Hg, if tolerated, in those aged 80 years and up (Circulation 2011;123:2434-506).
"The hypothesis from this REGARDS analysis is a bold one," she observed. "But we need large, well-designed intervention trials in older patients, particularly in underrepresented groups, before we can set lower blood pressure targets than are currently recommended in our guidelines."
The REGARDS study is a National Institutes of Health–sponsored observational study of 30,329 U.S. subjects aged 45 years or older, with overrepresentation of blacks and residents of the nation’s southeastern "stroke belt." Dr. Banach presented an analysis of 13,948 REGARDS participants aged 55 years or older who were taking antihypertensive medications at baseline. They have thus far been followed for a median of 6 years for all-cause mortality, and slightly less for first occurrence of stroke or coronary heart disease.
The suggestion of a J-curve was strongest for the composite endpoint of a first stroke, nonfatal myocardial infarction (MI), or death due to coronary heart disease in subjects aged 75 years or older (see graphic). There was no significant relationship between stroke and SBP category for subjects under age 75; however, over age 75, stroke rates were highest in those with an SBP less than 120 or more than 150 mm Hg.
All-cause mortality showed a linear relationship with increasing SBP in subjects aged 55-74 years, but no relationship in those over age 75.
Dr. Deaton applauded the REGARDS investigators for focusing on a high-risk population that’s "certainly underrepresented in our clinical intervention trials," but she cited several major study limitations. One is that only baseline blood pressure measurements were available.
"Importantly," she observed, "we don’t know what happened to blood pressure control during these years of follow-up."
In addition, the incidence rates of stroke, MI, and other major adverse events were relatively low in some subgroups. The planned further follow-up in REGARDS should bring greater clarity, Dr. Deaton added.
Dr. Banach and Dr. Deaton reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2013
Major finding: The adjusted risk of a first stroke, MI, or cardiovascular death in individuals aged 75 years or older on antihypertensive therapy was 20% lower in those with a systolic blood pressure of 120-129 mm Hg than in those with an SBP less than 120, and 31% lower in those with an SBP of 130-139 mm Hg. In contrast, the risk was 2.2-fold greater in those with an SBP of 150 mm Hg or more than in subjects with an SBP below 120 mm Hg.
Data source: This was a secondary analysis involving nearly 14,000 participants in the prospective observational REGARDS study, all at least 55 years old and on antihypertensive medication at baseline.
Disclosures: Dr. Banach and Dr. Deaton reported having no financial conflicts of interest.