User login
Hospital in Home (HIH) is the delivery of acute care services in a patient’s home as an alternative to hospitalization.1 Compared with traditional inpatient care, HIH programs have been associated with reduced costs, as well as patient and caregiver satisfaction, diseasespecific outcomes, and mortality rates that were similar or improved compared with inpatient admissions.1-4
The US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) and other hospital systems are increasingly adopting HIH models.2-4 At the time of this writing, there were 12 HIH programs in VHA (personal communication, D. Cooper, 2/28/2022). In addition to physicians and nurses, the interdisciplinary HIH team may include a pharmacist, social worker, and registered dietitian nutritionist (RDN).2,5 HIH programs have been shown to improve nutritional status as measured by the Mini Nutritional Assessment Score, but overall, there is a paucity of published information regarding the provision of nutrition care in HIH.6 The role of the RDN has varied within VHA. Some sites, such as the Sacramento VA Medical Center in California, include a distinct RDN position on the HIH team, whereas others, such as the Spark M. Matsunaga VA Medical Center in Honolulu, Hawaii, and the James A. Haley Veterans’ Hospital in Tampa, Florida, consult clinic RDNs.
Since HIH programs typically treat conditions for which diet is an inherent part of the treatment (eg, congestive heart failure [CHF]), there is a need to precisely define the role of the RDN within the HIH model.2,3,7 Drawing from my experience as an HIH RDN, I will describe how the inclusion of an RDN position within the HIH team is optimal for health care delivery and how HIH practitioners can best utilize RDN services.
RDN Role in HIH Team
Delegating nutrition services to an RDN enhances patient care by empowering HIH team members to function at the highest level of their scope of practice. RDNs have been recognized by physicians as the most qualified health care professionals to help patients with diet-related conditions, such as obesity, and physicians also have reported a desire for additional training in nutrition.8 Although home-health nurses have frequently performed nutrition assessments and interventions, survey results have indicated that many nurses do not feel confident in teaching complex nutritional information.9 In my experience, many HIH patients are nutritionally complex, with more than one condition requiring nutrition intervention. For example, patients may be admitted to HIH for management of CHF, but they may also have diabetes mellitus (DM), obesity, and low socioeconomic status. The HIH RDN can address the nutrition aspects of these conditions, freeing time for physicians and nurses to focus on their respective areas of expertise.9,10 Moreover, the RDN can also provide dietary education to the HIH team to increase their knowledge of nutritional topics and promote consistent messaging to patients.
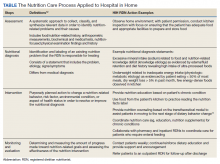
Including an RDN on the HIH team enables patients to have comprehensive, personalized nutrition care. Rather than merely offering generalized nutrition education, RDNs are trained to provide medical nutrition therapy (MNT), which has been shown to improve health outcomes and be cost-effective for conditions such as type 2 DM, chronic kidney disease, hypertension, and obesity.10,11 In MNT, RDNs use the standardized 4-stepnutrition care process (NCP).12 The Table shows examples of how the NCP can be applied in HIH settings. Furthermore, in my experience, MNT from an RDN also contributes to patient satisfaction. Subjective observations from my team have indicated that patients often express more confidence in managing their diets by the time of HIH discharge.
RDNs can guide physicians and pharmacists in ordering oral nutrition supplements (ONS). Within the VHA, a “food first” approach is preferred to increase caloric intake, and patients must meet specific criteria for prescription of an ONS.13 Furthermore, ONS designed for specific medical conditions (eg, chronic kidney disease) are considered nonformulary and require an RDN evaluation.13 Including an RDN on the HIH team allows this evaluation process to begin early in the patient’s admission to the program and ensures that provision of ONS is clinically appropriate and cost-effective.
Care Coordination
HIH is highly interdisciplinary. Team members perform their respective roles and communicate with the team throughout the day. RDNs can help monitor patients and alert physicians for changes in blood glucose, gastrointestinal concerns, and weight. This is especially helpful for patients who do not have a planned nursing visit on the day of an RDN evaluation. The HIH RDN can also collaborate with other team members to address patient needs. For example, for patients with limited financial resources, the HIH RDN can provide nutrition education regarding cooking on a budget, and the HIH social worker can arrange free or low-cost meal services.
Tips
When hiring an HIH RDN, seek candidates with experience in inpatient, outpatient, and home care settings. As a hybrid of these 3 areas, the HIH RDN position requires a unique combination of acute care skills and health coaching. Additionally, in my experience, the HIH RDN interacts more frequently with the HIH team than other RDN colleagues, so it is important that candidates can work independently and take initiative. This type of position would not be suitable for entry-level RDNs.
Stagger HIH team visits to prevent overwhelming the patient and caregivers. Early in our program, my team quickly learned that patients and caregivers can feel overwhelmed with too many home visits upon admission to HIH. After seeing multiple HIH team members the same day, they were often too tired to focus well on diet education during my visit. Staggering visits (eg, completing the initial nutrition assessment 1 day to 1 week after the initial medical and pharmacy visits) has been an effective strategy to address this problem. Furthermore, some patients prefer that the initial RDN appointment is conducted by telephone, with an inperson reassessment the following week. In my experience, HIH workflow is dynamic by nature, so it is crucial to remain flexible and accommodate individual patient needs as much as possible.
Dietary behavior change is a long-term process, and restrictive hospital diets can be challenging to replicate at home. In a hospital setting, clinicians can order a specialized diet (eg, low sodium with fluid restriction for CHF patients), whereas efforts to implement these restrictions in the home setting can be cumbersome and negatively impact quality of life.7,14 Nevertheless, the effectiveness of medical treatment is compromised when patients do not adhere to dietary recommendations. Meal delivery services that offer specialized diets can be a useful resource for patients and caregivers who are unable to cook, and the HIH RDN can assist patients in ordering these services.
HIH patients may vary in terms of readiness to make dietary changes, and in addition to nutrition education, nutrition counseling is usually needed to effect behavior change. My team has found that consideration of the transtheoretical/ stages of change model can be a helpful approach. 15 The HIH RDN can tailor nutrition interventions to the patient’s stage of change. For example, for patients in the precontemplation stage, the HIH RDN would focus on providing information and addressing emotional aspects of dietary change. In contrast, for patients in the action stage of change, the HIH RDN might emphasize behavioral skill training and social support.15 Particularly for patients in the early stages of change, it may be unrealistic to expect full adoption of the recommended diet within the 30 days of the HIH program. However, by acknowledging the reality of the patient’s stage of change, the HIH RDN and team can then collaborate to support the patient in moving toward the next stage. Patients who are not ready for dietary behavior change during the 30 days of HIH may benefit from longer-term support, and the HIH RDN can arrange followup care with an outpatient RDN.
Conclusions
As the HIH model continues to be adopted across the VHA and other health care systems, it is crucial to consider the value and expertise of an RDN for guiding nutrition care in the HIH setting. The HIH RDN contributes to optimal health care delivery by leading nutritional aspects of patient care, offering personalized MNT, and coordinating and collaborating with team members to meet individual patient needs. An RDN can serve as a valuable resource for nutrition information and enhance the team’s overall services, with the potential to impact clinical outcomes and patient satisfaction.
1. Levine DM, Ouchi K, Blanchfield B, et al. Hospitallevel care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77-85. doi:10.7326/M19-0600
2. Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs medical center hospital-in-home program. J Am Geriatr Soc. 2018;66(7):1392-1398. doi:10.1111/jgs.15382
3. Cai S, Laurel PA, Makineni R, Marks ML. Evaluation of a hospital-in-home program implemented among veterans. Am J Manag Care. 2017;23(8):482-487.
4. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. doi:10.1001/jamainternmed.2016.5974
5. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1144: Hospital in Home program, Appendix A, Hospital in Home program standards. January 19, 2021. Accessed May 5, 2022. https://www .va.gov/VHApublications/ViewPublication.asp?pub _ID=9157
6. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10.1001/archinternmed.2009.267
7. Abshire M, Xu J, Baptiste D, et al. Nutritional interventions in heart failure: a systematic review of the literature. J Card Fail. 2015;21(12):989-999. doi:10.1016/j.cardfail.2015.10.004
8. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. Published 2012 Dec 20. doi:10.1136/bmjopen-2012-001871
9. Sousa AM. Benefits of dietitian home visits. J Am Diet Assoc. 1994;94(10):1149-1151. doi:10.1016/0002-8223(94)91136-3
10. Casas-Agustench P, Megías-Rangil I, Babio N. Economic benefit of dietetic-nutritional treatment in the multidisciplinary primary care team. Beneficio económico del tratamiento dietético-nutricional en el equipo multidisciplinario de atención primaria. Nutr Hosp. 2020;37(4):863-874. doi:10.20960/nh.03025
11. Lee J, Briggs Early K, Kovesdy CP, Lancaster K, Brown N, Steiber AL. The impact of RDNs on non-communicable diseases: proceedings from The State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166-174. doi:10.1016/j.jand.2021.02.021
12. Academy of Nutrition and Dietetics. Evidence analysis library, nutrition care process. Accessed May 5, 2022. https://www.andeal.org/ncp
13. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1438, clinical nutrition management and therapy. Appendix A, nutrition support therapy. September 19, 2019. Accessed January 20, 2022. https://www.va.gov/VHAPUBLICATIONS/ViewPublication .asp?pub_ID=8512
14. Vogelzang JL. Fifteen ways to enhance client outcomes by using your registered dietitian. Home Healthc Nurse. 2002;20(4):227-229. doi:10.1097/00004045-200204000-00005
15. Kristal AR, Glanz K, Curry SJ, Patterson RE. How can stages of change be best used in dietary interventions?. J Am Diet Assoc. 1999;99(6):679-684. doi:10.1016/S0002-8223(99)00165-0
Hospital in Home (HIH) is the delivery of acute care services in a patient’s home as an alternative to hospitalization.1 Compared with traditional inpatient care, HIH programs have been associated with reduced costs, as well as patient and caregiver satisfaction, diseasespecific outcomes, and mortality rates that were similar or improved compared with inpatient admissions.1-4
The US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) and other hospital systems are increasingly adopting HIH models.2-4 At the time of this writing, there were 12 HIH programs in VHA (personal communication, D. Cooper, 2/28/2022). In addition to physicians and nurses, the interdisciplinary HIH team may include a pharmacist, social worker, and registered dietitian nutritionist (RDN).2,5 HIH programs have been shown to improve nutritional status as measured by the Mini Nutritional Assessment Score, but overall, there is a paucity of published information regarding the provision of nutrition care in HIH.6 The role of the RDN has varied within VHA. Some sites, such as the Sacramento VA Medical Center in California, include a distinct RDN position on the HIH team, whereas others, such as the Spark M. Matsunaga VA Medical Center in Honolulu, Hawaii, and the James A. Haley Veterans’ Hospital in Tampa, Florida, consult clinic RDNs.
Since HIH programs typically treat conditions for which diet is an inherent part of the treatment (eg, congestive heart failure [CHF]), there is a need to precisely define the role of the RDN within the HIH model.2,3,7 Drawing from my experience as an HIH RDN, I will describe how the inclusion of an RDN position within the HIH team is optimal for health care delivery and how HIH practitioners can best utilize RDN services.
RDN Role in HIH Team
Delegating nutrition services to an RDN enhances patient care by empowering HIH team members to function at the highest level of their scope of practice. RDNs have been recognized by physicians as the most qualified health care professionals to help patients with diet-related conditions, such as obesity, and physicians also have reported a desire for additional training in nutrition.8 Although home-health nurses have frequently performed nutrition assessments and interventions, survey results have indicated that many nurses do not feel confident in teaching complex nutritional information.9 In my experience, many HIH patients are nutritionally complex, with more than one condition requiring nutrition intervention. For example, patients may be admitted to HIH for management of CHF, but they may also have diabetes mellitus (DM), obesity, and low socioeconomic status. The HIH RDN can address the nutrition aspects of these conditions, freeing time for physicians and nurses to focus on their respective areas of expertise.9,10 Moreover, the RDN can also provide dietary education to the HIH team to increase their knowledge of nutritional topics and promote consistent messaging to patients.
Including an RDN on the HIH team enables patients to have comprehensive, personalized nutrition care. Rather than merely offering generalized nutrition education, RDNs are trained to provide medical nutrition therapy (MNT), which has been shown to improve health outcomes and be cost-effective for conditions such as type 2 DM, chronic kidney disease, hypertension, and obesity.10,11 In MNT, RDNs use the standardized 4-stepnutrition care process (NCP).12 The Table shows examples of how the NCP can be applied in HIH settings. Furthermore, in my experience, MNT from an RDN also contributes to patient satisfaction. Subjective observations from my team have indicated that patients often express more confidence in managing their diets by the time of HIH discharge.
RDNs can guide physicians and pharmacists in ordering oral nutrition supplements (ONS). Within the VHA, a “food first” approach is preferred to increase caloric intake, and patients must meet specific criteria for prescription of an ONS.13 Furthermore, ONS designed for specific medical conditions (eg, chronic kidney disease) are considered nonformulary and require an RDN evaluation.13 Including an RDN on the HIH team allows this evaluation process to begin early in the patient’s admission to the program and ensures that provision of ONS is clinically appropriate and cost-effective.
Care Coordination
HIH is highly interdisciplinary. Team members perform their respective roles and communicate with the team throughout the day. RDNs can help monitor patients and alert physicians for changes in blood glucose, gastrointestinal concerns, and weight. This is especially helpful for patients who do not have a planned nursing visit on the day of an RDN evaluation. The HIH RDN can also collaborate with other team members to address patient needs. For example, for patients with limited financial resources, the HIH RDN can provide nutrition education regarding cooking on a budget, and the HIH social worker can arrange free or low-cost meal services.
Tips
When hiring an HIH RDN, seek candidates with experience in inpatient, outpatient, and home care settings. As a hybrid of these 3 areas, the HIH RDN position requires a unique combination of acute care skills and health coaching. Additionally, in my experience, the HIH RDN interacts more frequently with the HIH team than other RDN colleagues, so it is important that candidates can work independently and take initiative. This type of position would not be suitable for entry-level RDNs.
Stagger HIH team visits to prevent overwhelming the patient and caregivers. Early in our program, my team quickly learned that patients and caregivers can feel overwhelmed with too many home visits upon admission to HIH. After seeing multiple HIH team members the same day, they were often too tired to focus well on diet education during my visit. Staggering visits (eg, completing the initial nutrition assessment 1 day to 1 week after the initial medical and pharmacy visits) has been an effective strategy to address this problem. Furthermore, some patients prefer that the initial RDN appointment is conducted by telephone, with an inperson reassessment the following week. In my experience, HIH workflow is dynamic by nature, so it is crucial to remain flexible and accommodate individual patient needs as much as possible.
Dietary behavior change is a long-term process, and restrictive hospital diets can be challenging to replicate at home. In a hospital setting, clinicians can order a specialized diet (eg, low sodium with fluid restriction for CHF patients), whereas efforts to implement these restrictions in the home setting can be cumbersome and negatively impact quality of life.7,14 Nevertheless, the effectiveness of medical treatment is compromised when patients do not adhere to dietary recommendations. Meal delivery services that offer specialized diets can be a useful resource for patients and caregivers who are unable to cook, and the HIH RDN can assist patients in ordering these services.
HIH patients may vary in terms of readiness to make dietary changes, and in addition to nutrition education, nutrition counseling is usually needed to effect behavior change. My team has found that consideration of the transtheoretical/ stages of change model can be a helpful approach. 15 The HIH RDN can tailor nutrition interventions to the patient’s stage of change. For example, for patients in the precontemplation stage, the HIH RDN would focus on providing information and addressing emotional aspects of dietary change. In contrast, for patients in the action stage of change, the HIH RDN might emphasize behavioral skill training and social support.15 Particularly for patients in the early stages of change, it may be unrealistic to expect full adoption of the recommended diet within the 30 days of the HIH program. However, by acknowledging the reality of the patient’s stage of change, the HIH RDN and team can then collaborate to support the patient in moving toward the next stage. Patients who are not ready for dietary behavior change during the 30 days of HIH may benefit from longer-term support, and the HIH RDN can arrange followup care with an outpatient RDN.
Conclusions
As the HIH model continues to be adopted across the VHA and other health care systems, it is crucial to consider the value and expertise of an RDN for guiding nutrition care in the HIH setting. The HIH RDN contributes to optimal health care delivery by leading nutritional aspects of patient care, offering personalized MNT, and coordinating and collaborating with team members to meet individual patient needs. An RDN can serve as a valuable resource for nutrition information and enhance the team’s overall services, with the potential to impact clinical outcomes and patient satisfaction.
Hospital in Home (HIH) is the delivery of acute care services in a patient’s home as an alternative to hospitalization.1 Compared with traditional inpatient care, HIH programs have been associated with reduced costs, as well as patient and caregiver satisfaction, diseasespecific outcomes, and mortality rates that were similar or improved compared with inpatient admissions.1-4
The US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) and other hospital systems are increasingly adopting HIH models.2-4 At the time of this writing, there were 12 HIH programs in VHA (personal communication, D. Cooper, 2/28/2022). In addition to physicians and nurses, the interdisciplinary HIH team may include a pharmacist, social worker, and registered dietitian nutritionist (RDN).2,5 HIH programs have been shown to improve nutritional status as measured by the Mini Nutritional Assessment Score, but overall, there is a paucity of published information regarding the provision of nutrition care in HIH.6 The role of the RDN has varied within VHA. Some sites, such as the Sacramento VA Medical Center in California, include a distinct RDN position on the HIH team, whereas others, such as the Spark M. Matsunaga VA Medical Center in Honolulu, Hawaii, and the James A. Haley Veterans’ Hospital in Tampa, Florida, consult clinic RDNs.
Since HIH programs typically treat conditions for which diet is an inherent part of the treatment (eg, congestive heart failure [CHF]), there is a need to precisely define the role of the RDN within the HIH model.2,3,7 Drawing from my experience as an HIH RDN, I will describe how the inclusion of an RDN position within the HIH team is optimal for health care delivery and how HIH practitioners can best utilize RDN services.
RDN Role in HIH Team
Delegating nutrition services to an RDN enhances patient care by empowering HIH team members to function at the highest level of their scope of practice. RDNs have been recognized by physicians as the most qualified health care professionals to help patients with diet-related conditions, such as obesity, and physicians also have reported a desire for additional training in nutrition.8 Although home-health nurses have frequently performed nutrition assessments and interventions, survey results have indicated that many nurses do not feel confident in teaching complex nutritional information.9 In my experience, many HIH patients are nutritionally complex, with more than one condition requiring nutrition intervention. For example, patients may be admitted to HIH for management of CHF, but they may also have diabetes mellitus (DM), obesity, and low socioeconomic status. The HIH RDN can address the nutrition aspects of these conditions, freeing time for physicians and nurses to focus on their respective areas of expertise.9,10 Moreover, the RDN can also provide dietary education to the HIH team to increase their knowledge of nutritional topics and promote consistent messaging to patients.
Including an RDN on the HIH team enables patients to have comprehensive, personalized nutrition care. Rather than merely offering generalized nutrition education, RDNs are trained to provide medical nutrition therapy (MNT), which has been shown to improve health outcomes and be cost-effective for conditions such as type 2 DM, chronic kidney disease, hypertension, and obesity.10,11 In MNT, RDNs use the standardized 4-stepnutrition care process (NCP).12 The Table shows examples of how the NCP can be applied in HIH settings. Furthermore, in my experience, MNT from an RDN also contributes to patient satisfaction. Subjective observations from my team have indicated that patients often express more confidence in managing their diets by the time of HIH discharge.
RDNs can guide physicians and pharmacists in ordering oral nutrition supplements (ONS). Within the VHA, a “food first” approach is preferred to increase caloric intake, and patients must meet specific criteria for prescription of an ONS.13 Furthermore, ONS designed for specific medical conditions (eg, chronic kidney disease) are considered nonformulary and require an RDN evaluation.13 Including an RDN on the HIH team allows this evaluation process to begin early in the patient’s admission to the program and ensures that provision of ONS is clinically appropriate and cost-effective.
Care Coordination
HIH is highly interdisciplinary. Team members perform their respective roles and communicate with the team throughout the day. RDNs can help monitor patients and alert physicians for changes in blood glucose, gastrointestinal concerns, and weight. This is especially helpful for patients who do not have a planned nursing visit on the day of an RDN evaluation. The HIH RDN can also collaborate with other team members to address patient needs. For example, for patients with limited financial resources, the HIH RDN can provide nutrition education regarding cooking on a budget, and the HIH social worker can arrange free or low-cost meal services.
Tips
When hiring an HIH RDN, seek candidates with experience in inpatient, outpatient, and home care settings. As a hybrid of these 3 areas, the HIH RDN position requires a unique combination of acute care skills and health coaching. Additionally, in my experience, the HIH RDN interacts more frequently with the HIH team than other RDN colleagues, so it is important that candidates can work independently and take initiative. This type of position would not be suitable for entry-level RDNs.
Stagger HIH team visits to prevent overwhelming the patient and caregivers. Early in our program, my team quickly learned that patients and caregivers can feel overwhelmed with too many home visits upon admission to HIH. After seeing multiple HIH team members the same day, they were often too tired to focus well on diet education during my visit. Staggering visits (eg, completing the initial nutrition assessment 1 day to 1 week after the initial medical and pharmacy visits) has been an effective strategy to address this problem. Furthermore, some patients prefer that the initial RDN appointment is conducted by telephone, with an inperson reassessment the following week. In my experience, HIH workflow is dynamic by nature, so it is crucial to remain flexible and accommodate individual patient needs as much as possible.
Dietary behavior change is a long-term process, and restrictive hospital diets can be challenging to replicate at home. In a hospital setting, clinicians can order a specialized diet (eg, low sodium with fluid restriction for CHF patients), whereas efforts to implement these restrictions in the home setting can be cumbersome and negatively impact quality of life.7,14 Nevertheless, the effectiveness of medical treatment is compromised when patients do not adhere to dietary recommendations. Meal delivery services that offer specialized diets can be a useful resource for patients and caregivers who are unable to cook, and the HIH RDN can assist patients in ordering these services.
HIH patients may vary in terms of readiness to make dietary changes, and in addition to nutrition education, nutrition counseling is usually needed to effect behavior change. My team has found that consideration of the transtheoretical/ stages of change model can be a helpful approach. 15 The HIH RDN can tailor nutrition interventions to the patient’s stage of change. For example, for patients in the precontemplation stage, the HIH RDN would focus on providing information and addressing emotional aspects of dietary change. In contrast, for patients in the action stage of change, the HIH RDN might emphasize behavioral skill training and social support.15 Particularly for patients in the early stages of change, it may be unrealistic to expect full adoption of the recommended diet within the 30 days of the HIH program. However, by acknowledging the reality of the patient’s stage of change, the HIH RDN and team can then collaborate to support the patient in moving toward the next stage. Patients who are not ready for dietary behavior change during the 30 days of HIH may benefit from longer-term support, and the HIH RDN can arrange followup care with an outpatient RDN.
Conclusions
As the HIH model continues to be adopted across the VHA and other health care systems, it is crucial to consider the value and expertise of an RDN for guiding nutrition care in the HIH setting. The HIH RDN contributes to optimal health care delivery by leading nutritional aspects of patient care, offering personalized MNT, and coordinating and collaborating with team members to meet individual patient needs. An RDN can serve as a valuable resource for nutrition information and enhance the team’s overall services, with the potential to impact clinical outcomes and patient satisfaction.
1. Levine DM, Ouchi K, Blanchfield B, et al. Hospitallevel care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77-85. doi:10.7326/M19-0600
2. Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs medical center hospital-in-home program. J Am Geriatr Soc. 2018;66(7):1392-1398. doi:10.1111/jgs.15382
3. Cai S, Laurel PA, Makineni R, Marks ML. Evaluation of a hospital-in-home program implemented among veterans. Am J Manag Care. 2017;23(8):482-487.
4. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. doi:10.1001/jamainternmed.2016.5974
5. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1144: Hospital in Home program, Appendix A, Hospital in Home program standards. January 19, 2021. Accessed May 5, 2022. https://www .va.gov/VHApublications/ViewPublication.asp?pub _ID=9157
6. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10.1001/archinternmed.2009.267
7. Abshire M, Xu J, Baptiste D, et al. Nutritional interventions in heart failure: a systematic review of the literature. J Card Fail. 2015;21(12):989-999. doi:10.1016/j.cardfail.2015.10.004
8. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. Published 2012 Dec 20. doi:10.1136/bmjopen-2012-001871
9. Sousa AM. Benefits of dietitian home visits. J Am Diet Assoc. 1994;94(10):1149-1151. doi:10.1016/0002-8223(94)91136-3
10. Casas-Agustench P, Megías-Rangil I, Babio N. Economic benefit of dietetic-nutritional treatment in the multidisciplinary primary care team. Beneficio económico del tratamiento dietético-nutricional en el equipo multidisciplinario de atención primaria. Nutr Hosp. 2020;37(4):863-874. doi:10.20960/nh.03025
11. Lee J, Briggs Early K, Kovesdy CP, Lancaster K, Brown N, Steiber AL. The impact of RDNs on non-communicable diseases: proceedings from The State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166-174. doi:10.1016/j.jand.2021.02.021
12. Academy of Nutrition and Dietetics. Evidence analysis library, nutrition care process. Accessed May 5, 2022. https://www.andeal.org/ncp
13. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1438, clinical nutrition management and therapy. Appendix A, nutrition support therapy. September 19, 2019. Accessed January 20, 2022. https://www.va.gov/VHAPUBLICATIONS/ViewPublication .asp?pub_ID=8512
14. Vogelzang JL. Fifteen ways to enhance client outcomes by using your registered dietitian. Home Healthc Nurse. 2002;20(4):227-229. doi:10.1097/00004045-200204000-00005
15. Kristal AR, Glanz K, Curry SJ, Patterson RE. How can stages of change be best used in dietary interventions?. J Am Diet Assoc. 1999;99(6):679-684. doi:10.1016/S0002-8223(99)00165-0
1. Levine DM, Ouchi K, Blanchfield B, et al. Hospitallevel care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020;172(2):77-85. doi:10.7326/M19-0600
2. Cai S, Grubbs A, Makineni R, Kinosian B, Phibbs CS, Intrator O. Evaluation of the Cincinnati Veterans Affairs medical center hospital-in-home program. J Am Geriatr Soc. 2018;66(7):1392-1398. doi:10.1111/jgs.15382
3. Cai S, Laurel PA, Makineni R, Marks ML. Evaluation of a hospital-in-home program implemented among veterans. Am J Manag Care. 2017;23(8):482-487.
4. Conley J, O’Brien CW, Leff BA, Bolen S, Zulman D. Alternative strategies to inpatient hospitalization for acute medical conditions: a systematic review. JAMA Intern Med. 2016;176(11):1693-1702. doi:10.1001/jamainternmed.2016.5974
5. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1144: Hospital in Home program, Appendix A, Hospital in Home program standards. January 19, 2021. Accessed May 5, 2022. https://www .va.gov/VHApublications/ViewPublication.asp?pub _ID=9157
6. Tibaldi V, Isaia G, Scarafiotti C, et al. Hospital at home for elderly patients with acute decompensation of chronic heart failure: a prospective randomized controlled trial. Arch Intern Med. 2009;169(17):1569-1575. doi:10.1001/archinternmed.2009.267
7. Abshire M, Xu J, Baptiste D, et al. Nutritional interventions in heart failure: a systematic review of the literature. J Card Fail. 2015;21(12):989-999. doi:10.1016/j.cardfail.2015.10.004
8. Bleich SN, Bennett WL, Gudzune KA, Cooper LA. National survey of US primary care physicians’ perspectives about causes of obesity and solutions to improve care. BMJ Open. 2012;2(6):e001871. Published 2012 Dec 20. doi:10.1136/bmjopen-2012-001871
9. Sousa AM. Benefits of dietitian home visits. J Am Diet Assoc. 1994;94(10):1149-1151. doi:10.1016/0002-8223(94)91136-3
10. Casas-Agustench P, Megías-Rangil I, Babio N. Economic benefit of dietetic-nutritional treatment in the multidisciplinary primary care team. Beneficio económico del tratamiento dietético-nutricional en el equipo multidisciplinario de atención primaria. Nutr Hosp. 2020;37(4):863-874. doi:10.20960/nh.03025
11. Lee J, Briggs Early K, Kovesdy CP, Lancaster K, Brown N, Steiber AL. The impact of RDNs on non-communicable diseases: proceedings from The State of Food and Nutrition Series Forum. J Acad Nutr Diet. 2022;122(1):166-174. doi:10.1016/j.jand.2021.02.021
12. Academy of Nutrition and Dietetics. Evidence analysis library, nutrition care process. Accessed May 5, 2022. https://www.andeal.org/ncp
13. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1438, clinical nutrition management and therapy. Appendix A, nutrition support therapy. September 19, 2019. Accessed January 20, 2022. https://www.va.gov/VHAPUBLICATIONS/ViewPublication .asp?pub_ID=8512
14. Vogelzang JL. Fifteen ways to enhance client outcomes by using your registered dietitian. Home Healthc Nurse. 2002;20(4):227-229. doi:10.1097/00004045-200204000-00005
15. Kristal AR, Glanz K, Curry SJ, Patterson RE. How can stages of change be best used in dietary interventions?. J Am Diet Assoc. 1999;99(6):679-684. doi:10.1016/S0002-8223(99)00165-0