User login
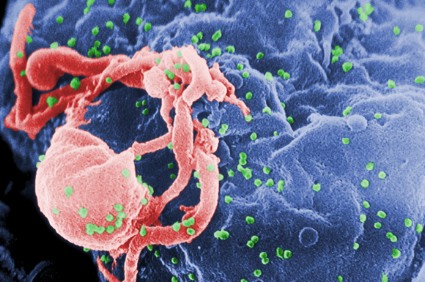
Curbing the high rates of anal cancer in HIV-infected individuals won’t be accomplished through targeted efforts focused on HIV-positive men who have sex with men, according to Dr. Michel Janier, head of dermatology at Saint Joseph Hospital in Paris and the French representative to the International Union Against Sexually Transmitted Infections – Europe.
Anal cancer rates among HIV-infected persons are indeed highest among men who have sex with men (MSM), but anal cancer rates also are quite high among other HIV-infected men and women, based on results of a large study.
The findings take on added significance given the availability of the HPV vaccine, although the efficacy of the vaccine in HIV-positive individuals remains to be seen. In addition, pilot projects testing the benefits of periodic anal histology screening in HIV-infected individuals are underway, Dr. Janier observed at the annual congress of the European Academy of Dermatology and Venereology.
The study by Dr. Michael J. Silverberg of Kaiser Permanente, Oakland, Calif., and the North American AIDS Cohort Collaboration on Research and Design (NA–ACCORD) of IeDEA included 36,189 HIV-infected North Americans and 114,260 uninfected controls followed during 1996-2007. The HIV-positive group comprised 55% MSM, 19% heterosexual men, and 26% women.
The unadjusted anal cancer incidence rates per 100,000 person-years were 131 for HIV-positive MSM, 46 for HIV-infected heterosexual men, and 2 for uninfected men. This translated to a demographically adjusted rate ratio of 80.3 for MSM compared with uninfected men, and to a 26.7-fold increased risk of anal cancer in HIV-infected straight men compared with uninfected heterosexual men.
HIV-infected women had an anal cancer incidence rate of 30 cases per 100,000 person-years. A rate ratio could not be determined because no cases occurred in uninfected women (Clin. Infect. Dis. 2012;54:1026-34).
Among HIV-infected individuals, the adjusted relative risk of anal cancer doubled from 1996-1999 to 2000-2003, then leveled off. This is in line with the findings of the large French Hospital Database Study, which also observed a jump in anal cancer rates among HIV-infected individuals in the late 1990s followed by more recent stabilization in the era of widely available antiretroviral therapy (AIDS 2008;22:1203-11).
The National Institutes of Health was the chief sponsor of the study. Dr. Janier reported having no financial conflicts.
Curbing the high rates of anal cancer in HIV-infected individuals won’t be accomplished through targeted efforts focused on HIV-positive men who have sex with men, according to Dr. Michel Janier, head of dermatology at Saint Joseph Hospital in Paris and the French representative to the International Union Against Sexually Transmitted Infections – Europe.
Anal cancer rates among HIV-infected persons are indeed highest among men who have sex with men (MSM), but anal cancer rates also are quite high among other HIV-infected men and women, based on results of a large study.
The findings take on added significance given the availability of the HPV vaccine, although the efficacy of the vaccine in HIV-positive individuals remains to be seen. In addition, pilot projects testing the benefits of periodic anal histology screening in HIV-infected individuals are underway, Dr. Janier observed at the annual congress of the European Academy of Dermatology and Venereology.
The study by Dr. Michael J. Silverberg of Kaiser Permanente, Oakland, Calif., and the North American AIDS Cohort Collaboration on Research and Design (NA–ACCORD) of IeDEA included 36,189 HIV-infected North Americans and 114,260 uninfected controls followed during 1996-2007. The HIV-positive group comprised 55% MSM, 19% heterosexual men, and 26% women.
The unadjusted anal cancer incidence rates per 100,000 person-years were 131 for HIV-positive MSM, 46 for HIV-infected heterosexual men, and 2 for uninfected men. This translated to a demographically adjusted rate ratio of 80.3 for MSM compared with uninfected men, and to a 26.7-fold increased risk of anal cancer in HIV-infected straight men compared with uninfected heterosexual men.
HIV-infected women had an anal cancer incidence rate of 30 cases per 100,000 person-years. A rate ratio could not be determined because no cases occurred in uninfected women (Clin. Infect. Dis. 2012;54:1026-34).
Among HIV-infected individuals, the adjusted relative risk of anal cancer doubled from 1996-1999 to 2000-2003, then leveled off. This is in line with the findings of the large French Hospital Database Study, which also observed a jump in anal cancer rates among HIV-infected individuals in the late 1990s followed by more recent stabilization in the era of widely available antiretroviral therapy (AIDS 2008;22:1203-11).
The National Institutes of Health was the chief sponsor of the study. Dr. Janier reported having no financial conflicts.
Curbing the high rates of anal cancer in HIV-infected individuals won’t be accomplished through targeted efforts focused on HIV-positive men who have sex with men, according to Dr. Michel Janier, head of dermatology at Saint Joseph Hospital in Paris and the French representative to the International Union Against Sexually Transmitted Infections – Europe.
Anal cancer rates among HIV-infected persons are indeed highest among men who have sex with men (MSM), but anal cancer rates also are quite high among other HIV-infected men and women, based on results of a large study.
The findings take on added significance given the availability of the HPV vaccine, although the efficacy of the vaccine in HIV-positive individuals remains to be seen. In addition, pilot projects testing the benefits of periodic anal histology screening in HIV-infected individuals are underway, Dr. Janier observed at the annual congress of the European Academy of Dermatology and Venereology.
The study by Dr. Michael J. Silverberg of Kaiser Permanente, Oakland, Calif., and the North American AIDS Cohort Collaboration on Research and Design (NA–ACCORD) of IeDEA included 36,189 HIV-infected North Americans and 114,260 uninfected controls followed during 1996-2007. The HIV-positive group comprised 55% MSM, 19% heterosexual men, and 26% women.
The unadjusted anal cancer incidence rates per 100,000 person-years were 131 for HIV-positive MSM, 46 for HIV-infected heterosexual men, and 2 for uninfected men. This translated to a demographically adjusted rate ratio of 80.3 for MSM compared with uninfected men, and to a 26.7-fold increased risk of anal cancer in HIV-infected straight men compared with uninfected heterosexual men.
HIV-infected women had an anal cancer incidence rate of 30 cases per 100,000 person-years. A rate ratio could not be determined because no cases occurred in uninfected women (Clin. Infect. Dis. 2012;54:1026-34).
Among HIV-infected individuals, the adjusted relative risk of anal cancer doubled from 1996-1999 to 2000-2003, then leveled off. This is in line with the findings of the large French Hospital Database Study, which also observed a jump in anal cancer rates among HIV-infected individuals in the late 1990s followed by more recent stabilization in the era of widely available antiretroviral therapy (AIDS 2008;22:1203-11).
The National Institutes of Health was the chief sponsor of the study. Dr. Janier reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANNUAL CONGRESS OF THE EUROPEAN ACADEMY OF DERMATOLOGY AND VENEREOLOGY