User login
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
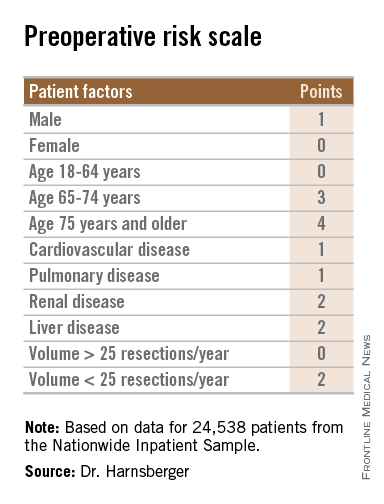
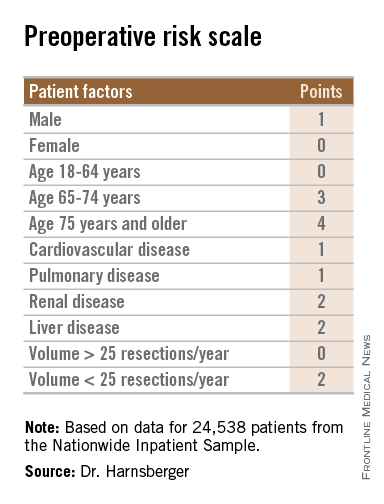
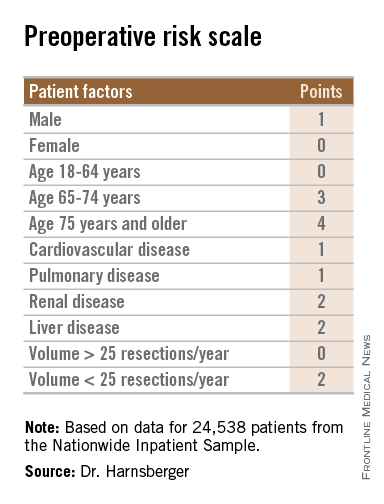
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
HOUSTON – A simple preoperative scale can accurately predict a patient’s risk for near-term death following surgery for gastric cancer, investigators say.
The scale accounts for both patient and hospital factors, and is useful as a clinical tool for preoperative counseling of patients, reported Dr. Cristina Harnsberger of the University of California San Diego.
“Male gender, increasing age, and comorbid disease increase risk of in-hospital mortality for patients who undergo gastric resection for malignancy. Additionally, low hospital volume was an independent risk factor,” she said at the annual Society of Surgical Oncology Cancer Symposium.
The scale was able to accurately classify patients as being at low or high risk, and the observed and expected mortality rates for each risk score were well correlated, she said.
Weighing risks
Perioperative mortality rates following resection for gastric malignancies range from 0.6% to 15%. Risk scales and nomograms are intended to help clinicians predict risks for individual patients, but most incorporate postoperative data rather than preoperative or hospital data, Dr. Harnsberger said.
She and her colleagues conducted a study to determine whether a simple preoperative scale based on patient and hospital factors could accurately predict risk for death following gastric resection for malignancy.
They drew on data from the Nationwide Inpatient Sample database to identify adult patients with a diagnosis of gastric cancer who underwent potentially curative partial or total gastrectomy from 1998 through 2011.
They identified a total 24,538 patients, based on International Classification of Diseases, Revision 9 (ICD-9) diagnosis and procedure codes.
They then created multivariate logistic regression models to identify independent predictors of mortality, create a predictive model, and construct a risk scale. The models controlled for sex, age, race, comorbidities, insurance status, hospital volume (less than 25 vs. 25 or more gastric resections for malignancy per year), laparoscopic vs. open approach, poverty level, alcohol abuse, tobacco use, diabetes mellitus, and year of procedure.
The mean length of stay for the patient sample was 11 days. The overall in-hospital mortality was 5.5%.
The models identified three patient-related factors and one hospital-related factor that were predictive of mortality and when combined in a risk scale proved to be accurate.
The patient factors were male sex, age 65 and older, and comorbid disease, specifically cardiovascular, pulmonary, renal, and/or hepatic.
The hospital factor, expressed as protective, was 25 or more gastric resections for cancer per year.
The maximum possible score is 13. Patients with scores lower than 6 are at low risk for perioperative mortality, while those with scores 6 and higher are at high risk. Among patients with a score of 0-5, the perioperative death rate ranged from 1.3% to 4.5%. In contrast, patients with higher scores had death rates ranging from 6.0% to 23.1%.
Clinical applications for the bedside risk scale include perioperative patient counseling, aiding in informed consent discussions, and as an adjunct to postoperative risk calculators, Dr. Harnsberger said.The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.
AT SSO 2015
Key clinical point: The bedside risk scale can be used in patient counseling prior to surgery for gastric malignancies.
Major finding: Patients with scores of 0-5 had perioperative death rates of 1.3%-4.5%. Patients with higher scores had death rates ranging from 6.0% to 23.1%.
Data source: Review of retrospective data on 24,538 adults who underwent partial or total gastric resection for malignancies.
Disclosures: The study funding source was not disclosed. Dr. Harnsberger reported having no disclosures.

