User login

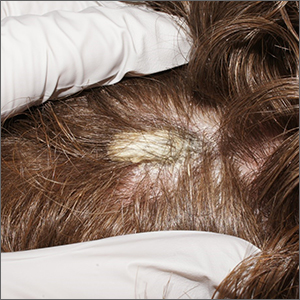
A punch biopsy was performed, and the results were consistent with pityriasis amiantacea arising from psoriasis. In an older patient, a keratinaceous horn would be worrisome for a squamous cell carcinoma. In a younger patient, like this one, it is more likely an atypical manifestation of a more common dermatosis.
Pityriasis amiantacea is an unusual disorder in which thick adherent scales form on the scalp; it is most common in children, adolescents, and young adults. There is no racial predilection. With this condition, patients complain of a fixed plaque that may shed scale but not as quickly as it accumulates. It can be an isolated finding, but more often it is a secondary manifestation of an underlying case of psoriasis, seborrheic dermatitis, tinea capitis, or atopic dermatitis.1
A punch biopsy performed on the scalp should include the skin underlying the compact keratin scale. However, to avoid excessive bleeding, use lidocaine with epinephrine. Allow 15 minutes for the anesthesia to take effect before beginning the procedure.
Treatment depends on the underlying cause but includes debridement of the aggregated scale with a topical keratolytic (such as salicylic acid or topical fluocinolone oil 0.01% applied) at night and washed out 7 to 10 hours later.
The patient was advised to use over-the-counter 2% salicylic acid shampoo daily and to apply topical clobetasol 0.05% solution nightly for 4 weeks and once weekly after clearance for another 3 months. At the 3-month follow-up, the patient’s scalp was clear.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Ettler J, Wetter DA, Pittelkow MR. Pityriasis amiantacea: a distinctive presentation of psoriasis associated with tumour necrosis factor-α inhibitor therapy. Clin Exp Dermatol. 2012;37:639-641. doi: 10.1111/j.1365-2230.2011.04286.x

A punch biopsy was performed, and the results were consistent with pityriasis amiantacea arising from psoriasis. In an older patient, a keratinaceous horn would be worrisome for a squamous cell carcinoma. In a younger patient, like this one, it is more likely an atypical manifestation of a more common dermatosis.
Pityriasis amiantacea is an unusual disorder in which thick adherent scales form on the scalp; it is most common in children, adolescents, and young adults. There is no racial predilection. With this condition, patients complain of a fixed plaque that may shed scale but not as quickly as it accumulates. It can be an isolated finding, but more often it is a secondary manifestation of an underlying case of psoriasis, seborrheic dermatitis, tinea capitis, or atopic dermatitis.1
A punch biopsy performed on the scalp should include the skin underlying the compact keratin scale. However, to avoid excessive bleeding, use lidocaine with epinephrine. Allow 15 minutes for the anesthesia to take effect before beginning the procedure.
Treatment depends on the underlying cause but includes debridement of the aggregated scale with a topical keratolytic (such as salicylic acid or topical fluocinolone oil 0.01% applied) at night and washed out 7 to 10 hours later.
The patient was advised to use over-the-counter 2% salicylic acid shampoo daily and to apply topical clobetasol 0.05% solution nightly for 4 weeks and once weekly after clearance for another 3 months. At the 3-month follow-up, the patient’s scalp was clear.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.

A punch biopsy was performed, and the results were consistent with pityriasis amiantacea arising from psoriasis. In an older patient, a keratinaceous horn would be worrisome for a squamous cell carcinoma. In a younger patient, like this one, it is more likely an atypical manifestation of a more common dermatosis.
Pityriasis amiantacea is an unusual disorder in which thick adherent scales form on the scalp; it is most common in children, adolescents, and young adults. There is no racial predilection. With this condition, patients complain of a fixed plaque that may shed scale but not as quickly as it accumulates. It can be an isolated finding, but more often it is a secondary manifestation of an underlying case of psoriasis, seborrheic dermatitis, tinea capitis, or atopic dermatitis.1
A punch biopsy performed on the scalp should include the skin underlying the compact keratin scale. However, to avoid excessive bleeding, use lidocaine with epinephrine. Allow 15 minutes for the anesthesia to take effect before beginning the procedure.
Treatment depends on the underlying cause but includes debridement of the aggregated scale with a topical keratolytic (such as salicylic acid or topical fluocinolone oil 0.01% applied) at night and washed out 7 to 10 hours later.
The patient was advised to use over-the-counter 2% salicylic acid shampoo daily and to apply topical clobetasol 0.05% solution nightly for 4 weeks and once weekly after clearance for another 3 months. At the 3-month follow-up, the patient’s scalp was clear.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Ettler J, Wetter DA, Pittelkow MR. Pityriasis amiantacea: a distinctive presentation of psoriasis associated with tumour necrosis factor-α inhibitor therapy. Clin Exp Dermatol. 2012;37:639-641. doi: 10.1111/j.1365-2230.2011.04286.x
1. Ettler J, Wetter DA, Pittelkow MR. Pityriasis amiantacea: a distinctive presentation of psoriasis associated with tumour necrosis factor-α inhibitor therapy. Clin Exp Dermatol. 2012;37:639-641. doi: 10.1111/j.1365-2230.2011.04286.x