User login
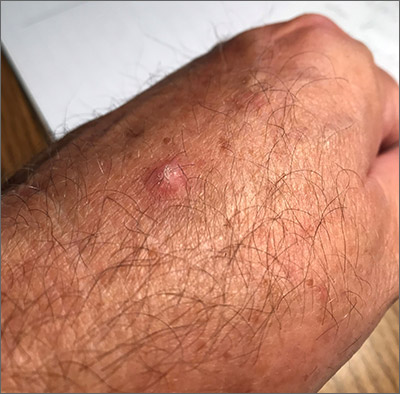
This pink raised nodule underlying a scaly surface was suspicious for squamous cell carcinoma (SCC). Since this was a virtual visit, and the lesion required pathology due to the likelihood of cancer, the patient was brought into the clinic for additional evaluation. A broad-based deep shave biopsy was performed to remove the visible lesion. Pathology showed SCC in situ, with borders uninvolved.
Patients who have had AKs are extremely likely to develop additional AKs. A notable percentage of AKs will, over time, develop into SCC in situ and then invasive SCC if not treated. While cryosurgery of an SK should not result in SCC, it’s most likely that in this case, an AK adjacent to the SK progressed to the SCC in situ.
There are multiple treatments available for SCC in situ. Topical imiquimod has been shown to be somewhat effective in stimulating the immune system, thus leading to resolution of SCC in situ. But there is a significant risk of recurrence. Topical 5-FU can be utilized on a daily or twice daily basis for 2 weeks (or up to several months). The risk of recurrence ranges from 7% to 33%. Electrodesiccation and curettage is often used for SCC in situ, with recurrence rates of 2% to 19%. Cryosurgery for SCC in situ requires an aggressive freeze, with freeze times of up to 30 seconds. Photodynamic therapy also is an option; however, it requires multiple sessions and is more costly than other treatment options.
This patient’s borders were uninvolved on pathology, but it was possible that there was some residual SCC in situ due to the standard “bread loaf slicing” used for routine pathology. To treat possible residual SCC in situ at the wound site and surrounding tissue, the patient was given a prescription for topical 5-FU to apply twice daily for 6 weeks. The patient was instructed to return for follow-up in 6 months, or sooner, if any problems arose.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Shimizu I, Cruz A, Chang KH, et al. Treatment of squamous cell carcinoma in situ: a review. Dermatol Surg. 2011;37:1394-1411.
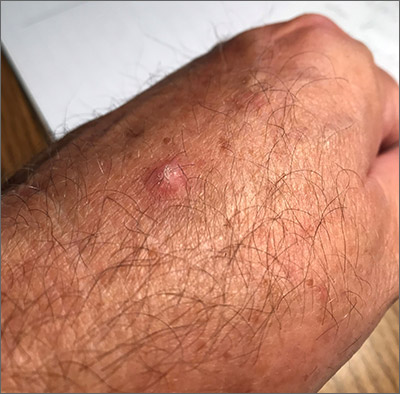
This pink raised nodule underlying a scaly surface was suspicious for squamous cell carcinoma (SCC). Since this was a virtual visit, and the lesion required pathology due to the likelihood of cancer, the patient was brought into the clinic for additional evaluation. A broad-based deep shave biopsy was performed to remove the visible lesion. Pathology showed SCC in situ, with borders uninvolved.
Patients who have had AKs are extremely likely to develop additional AKs. A notable percentage of AKs will, over time, develop into SCC in situ and then invasive SCC if not treated. While cryosurgery of an SK should not result in SCC, it’s most likely that in this case, an AK adjacent to the SK progressed to the SCC in situ.
There are multiple treatments available for SCC in situ. Topical imiquimod has been shown to be somewhat effective in stimulating the immune system, thus leading to resolution of SCC in situ. But there is a significant risk of recurrence. Topical 5-FU can be utilized on a daily or twice daily basis for 2 weeks (or up to several months). The risk of recurrence ranges from 7% to 33%. Electrodesiccation and curettage is often used for SCC in situ, with recurrence rates of 2% to 19%. Cryosurgery for SCC in situ requires an aggressive freeze, with freeze times of up to 30 seconds. Photodynamic therapy also is an option; however, it requires multiple sessions and is more costly than other treatment options.
This patient’s borders were uninvolved on pathology, but it was possible that there was some residual SCC in situ due to the standard “bread loaf slicing” used for routine pathology. To treat possible residual SCC in situ at the wound site and surrounding tissue, the patient was given a prescription for topical 5-FU to apply twice daily for 6 weeks. The patient was instructed to return for follow-up in 6 months, or sooner, if any problems arose.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
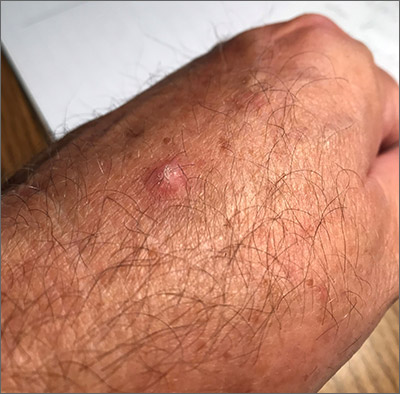
This pink raised nodule underlying a scaly surface was suspicious for squamous cell carcinoma (SCC). Since this was a virtual visit, and the lesion required pathology due to the likelihood of cancer, the patient was brought into the clinic for additional evaluation. A broad-based deep shave biopsy was performed to remove the visible lesion. Pathology showed SCC in situ, with borders uninvolved.
Patients who have had AKs are extremely likely to develop additional AKs. A notable percentage of AKs will, over time, develop into SCC in situ and then invasive SCC if not treated. While cryosurgery of an SK should not result in SCC, it’s most likely that in this case, an AK adjacent to the SK progressed to the SCC in situ.
There are multiple treatments available for SCC in situ. Topical imiquimod has been shown to be somewhat effective in stimulating the immune system, thus leading to resolution of SCC in situ. But there is a significant risk of recurrence. Topical 5-FU can be utilized on a daily or twice daily basis for 2 weeks (or up to several months). The risk of recurrence ranges from 7% to 33%. Electrodesiccation and curettage is often used for SCC in situ, with recurrence rates of 2% to 19%. Cryosurgery for SCC in situ requires an aggressive freeze, with freeze times of up to 30 seconds. Photodynamic therapy also is an option; however, it requires multiple sessions and is more costly than other treatment options.
This patient’s borders were uninvolved on pathology, but it was possible that there was some residual SCC in situ due to the standard “bread loaf slicing” used for routine pathology. To treat possible residual SCC in situ at the wound site and surrounding tissue, the patient was given a prescription for topical 5-FU to apply twice daily for 6 weeks. The patient was instructed to return for follow-up in 6 months, or sooner, if any problems arose.
Photo and text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
Shimizu I, Cruz A, Chang KH, et al. Treatment of squamous cell carcinoma in situ: a review. Dermatol Surg. 2011;37:1394-1411.
Shimizu I, Cruz A, Chang KH, et al. Treatment of squamous cell carcinoma in situ: a review. Dermatol Surg. 2011;37:1394-1411.
