User login
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.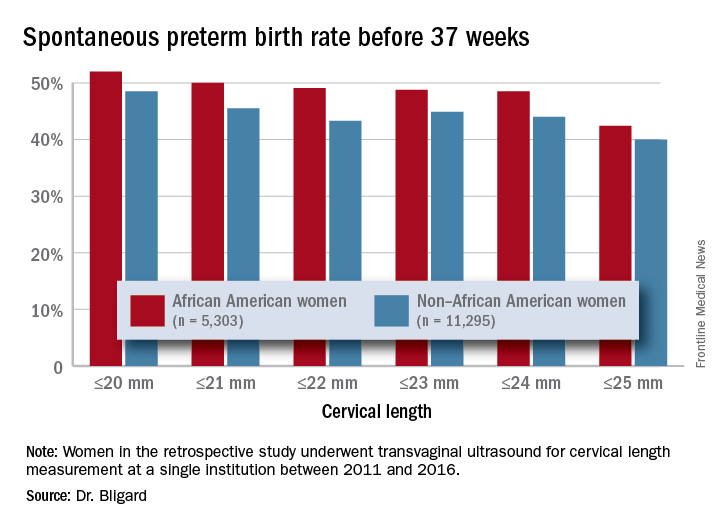
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.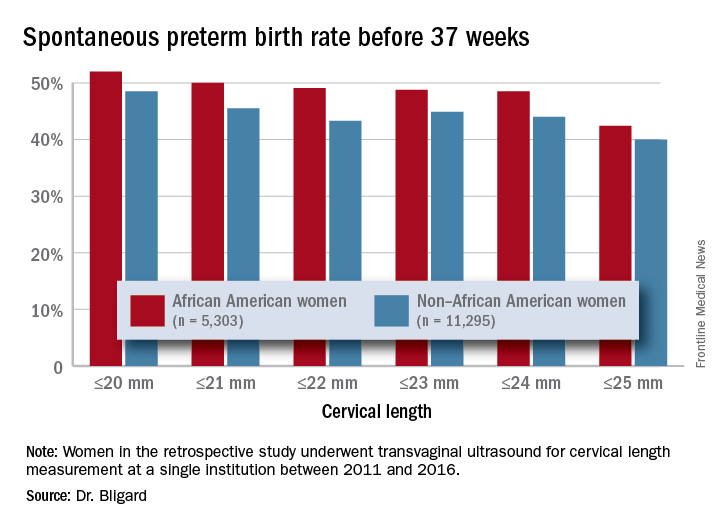
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.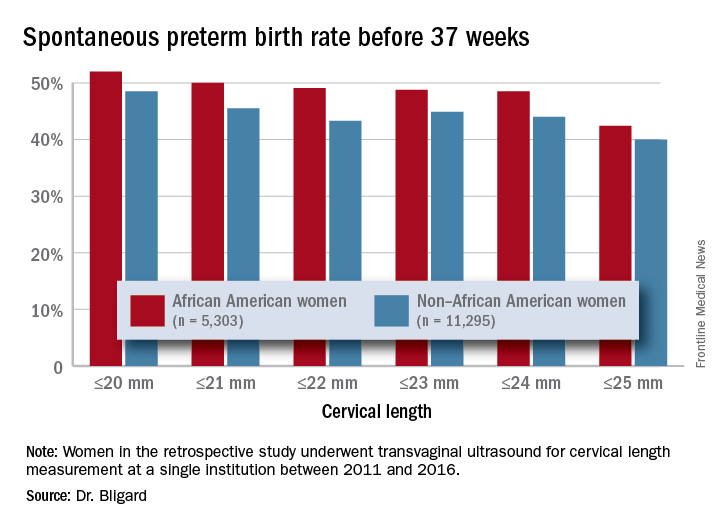
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Having a short cervix is more common among black women and more predictive of spontaneous preterm birth.
Major finding: Cervical length of 20 mm or less was 2.6 times more common among black women than it was women of other races or ethnicities.
Study details: The retrospective review comprised more than 16,500 women.
Disclosures: The study was sponsored by Washington University and the National Institutes of Health. Dr. Bligard had no financial disclosures.
Source: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.