User login
Toxicology reveals worse maternal and fetal outcomes with teen marijuana use
DALLAS – . Also, hypertensive disorders of pregnancy were higher in marijuana users, according to a study that incorporated universal urine toxicology testing of adolescents.
The study compared maternal and fetal/neonatal outcomes in 211 marijuana-exposed with 995 unexposed pregnancies. Christina Rodriguez, MD, and her coinvestigators found that the risk of a composite adverse pregnancy outcome was higher in marijuana users, occurring in 97/211 marijuana users (46%), and in 337/995 (33.9%) of the non–marijuana users (P less than .001).
Dr. Rodriguez said that since it used biological samples to confirm marijuana exposure, the study helps fill a gap in the literature. She presented the retrospective cohort study at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Previous work, she said, had established that up to 70% of pregnant women who had positive tests for tetrahydrocannabinol also denied marijuana use. “If marijuana use is determined by self-report, some women are misclassified as nonusers,” making it difficult to ascertain the true association between marijuana use during pregnancy and pregnancy outcomes, said Dr. Rodriguez of the University of Colorado, Denver.
Whether marijuana is associated with adverse pregnancy outcomes is an increasingly pressing question given rapidly shifting legislation, said Dr. Rodriguez. “In a state with legal access to marijuana, use is common in adolescent pregnancies,” she said.
Participants who were enrolled in prenatal care through the University of Colorado’s adolescent maternity program, where Dr. Rodriguez is a fellow, and who delivered at the University of Colorado Hospital, Aurora, were eligible to participate; adolescents were excluded for multiple gestation and for known major fetal anomalies or aneuploidy.
In addition to urine toxicology testing, participants also completed a uniformly administered substance use questionnaire. Marijuana exposure was defined as either having a positive urine toxicology result or self-reported marijuana use on the questionnaire (or both). Of the marijuana-exposed pregnancies, 133 (63%) of the adolescents tested positive on urine toxicology, 18 (9%) were positive by self-report, and 60 (28%) had both positive marijuana urine toxicology and positive self-report. Toxicology was available for 91% of participants.
Participants were negative for marijuana exposure if they had a negative toxicology screen, regardless of their response on the substance-use questionnaire.
The study’s primary outcome was a composite of adverse pregnancy outcomes, including stillbirth, defined as Apgar score of 0; any hypertensive disorder of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count); preterm birth, defined as spontaneous delivery before 37 weeks gestation; and infants born small for gestational age, defined as a birth weight below the 10th percentile after adjustment for gestational age and sex.
Secondary outcomes included pregnancy outcomes including placental abruption, mode of delivery, and gestational age at delivery. Neonatal outcomes included weight, length, and head circumference at birth, and neonatal intensive care unit admission. An Apgar score less than 7 at 5 minutes was considered an adverse neonatal outcome.
The sample size was determined by an estimate drawn from previous chart abstraction that the composite outcome would be seen in 16% of the clinic’s non–marijuana exposed patients, and 24% of the marijuana-exposed patients. The investigators also factored in that 18% of adolescents in the clinic database were marijuana users.
Dr. Rodriguez and her collaborators used a variety of models for statistical analysis, some of which included self-report alone or in conjunction with urine toxicology. In the end, they found that significant associations between their composite endpoint and marijuana use were seen when patients were dichotomized into those who had at least one positive urine toxicology test, versus those who had no positive toxicology results.
One of the study limitations was that the study didn’t permit investigators to get accurate information about the quantity, timing, or route of marijuana dosing. Also, this methodology may primarily identify heavier marijuana users, said Dr. Rodriguez.
Tobacco use was determined only by self-report, and outcomes were followed over a relatively short period of time.
Still, said Dr. Rodriguez, the study had many strengths, including the use of biological sampling to determine exposure and the near-universal participant urine toxicology testing. The investigators were able to capture and account for many important factors that could confound the results, she said. “Uncertainty regarding the impact of [marijuana] on pregnancy outcomes in the literature may result from incomplete ascertainment of exposure,” she and her coinvestigators wrote in the abstract accompanying the presentation.
SOURCE: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
DALLAS – . Also, hypertensive disorders of pregnancy were higher in marijuana users, according to a study that incorporated universal urine toxicology testing of adolescents.
The study compared maternal and fetal/neonatal outcomes in 211 marijuana-exposed with 995 unexposed pregnancies. Christina Rodriguez, MD, and her coinvestigators found that the risk of a composite adverse pregnancy outcome was higher in marijuana users, occurring in 97/211 marijuana users (46%), and in 337/995 (33.9%) of the non–marijuana users (P less than .001).
Dr. Rodriguez said that since it used biological samples to confirm marijuana exposure, the study helps fill a gap in the literature. She presented the retrospective cohort study at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Previous work, she said, had established that up to 70% of pregnant women who had positive tests for tetrahydrocannabinol also denied marijuana use. “If marijuana use is determined by self-report, some women are misclassified as nonusers,” making it difficult to ascertain the true association between marijuana use during pregnancy and pregnancy outcomes, said Dr. Rodriguez of the University of Colorado, Denver.
Whether marijuana is associated with adverse pregnancy outcomes is an increasingly pressing question given rapidly shifting legislation, said Dr. Rodriguez. “In a state with legal access to marijuana, use is common in adolescent pregnancies,” she said.
Participants who were enrolled in prenatal care through the University of Colorado’s adolescent maternity program, where Dr. Rodriguez is a fellow, and who delivered at the University of Colorado Hospital, Aurora, were eligible to participate; adolescents were excluded for multiple gestation and for known major fetal anomalies or aneuploidy.
In addition to urine toxicology testing, participants also completed a uniformly administered substance use questionnaire. Marijuana exposure was defined as either having a positive urine toxicology result or self-reported marijuana use on the questionnaire (or both). Of the marijuana-exposed pregnancies, 133 (63%) of the adolescents tested positive on urine toxicology, 18 (9%) were positive by self-report, and 60 (28%) had both positive marijuana urine toxicology and positive self-report. Toxicology was available for 91% of participants.
Participants were negative for marijuana exposure if they had a negative toxicology screen, regardless of their response on the substance-use questionnaire.
The study’s primary outcome was a composite of adverse pregnancy outcomes, including stillbirth, defined as Apgar score of 0; any hypertensive disorder of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count); preterm birth, defined as spontaneous delivery before 37 weeks gestation; and infants born small for gestational age, defined as a birth weight below the 10th percentile after adjustment for gestational age and sex.
Secondary outcomes included pregnancy outcomes including placental abruption, mode of delivery, and gestational age at delivery. Neonatal outcomes included weight, length, and head circumference at birth, and neonatal intensive care unit admission. An Apgar score less than 7 at 5 minutes was considered an adverse neonatal outcome.
The sample size was determined by an estimate drawn from previous chart abstraction that the composite outcome would be seen in 16% of the clinic’s non–marijuana exposed patients, and 24% of the marijuana-exposed patients. The investigators also factored in that 18% of adolescents in the clinic database were marijuana users.
Dr. Rodriguez and her collaborators used a variety of models for statistical analysis, some of which included self-report alone or in conjunction with urine toxicology. In the end, they found that significant associations between their composite endpoint and marijuana use were seen when patients were dichotomized into those who had at least one positive urine toxicology test, versus those who had no positive toxicology results.
One of the study limitations was that the study didn’t permit investigators to get accurate information about the quantity, timing, or route of marijuana dosing. Also, this methodology may primarily identify heavier marijuana users, said Dr. Rodriguez.
Tobacco use was determined only by self-report, and outcomes were followed over a relatively short period of time.
Still, said Dr. Rodriguez, the study had many strengths, including the use of biological sampling to determine exposure and the near-universal participant urine toxicology testing. The investigators were able to capture and account for many important factors that could confound the results, she said. “Uncertainty regarding the impact of [marijuana] on pregnancy outcomes in the literature may result from incomplete ascertainment of exposure,” she and her coinvestigators wrote in the abstract accompanying the presentation.
SOURCE: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
DALLAS – . Also, hypertensive disorders of pregnancy were higher in marijuana users, according to a study that incorporated universal urine toxicology testing of adolescents.
The study compared maternal and fetal/neonatal outcomes in 211 marijuana-exposed with 995 unexposed pregnancies. Christina Rodriguez, MD, and her coinvestigators found that the risk of a composite adverse pregnancy outcome was higher in marijuana users, occurring in 97/211 marijuana users (46%), and in 337/995 (33.9%) of the non–marijuana users (P less than .001).
Dr. Rodriguez said that since it used biological samples to confirm marijuana exposure, the study helps fill a gap in the literature. She presented the retrospective cohort study at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Previous work, she said, had established that up to 70% of pregnant women who had positive tests for tetrahydrocannabinol also denied marijuana use. “If marijuana use is determined by self-report, some women are misclassified as nonusers,” making it difficult to ascertain the true association between marijuana use during pregnancy and pregnancy outcomes, said Dr. Rodriguez of the University of Colorado, Denver.
Whether marijuana is associated with adverse pregnancy outcomes is an increasingly pressing question given rapidly shifting legislation, said Dr. Rodriguez. “In a state with legal access to marijuana, use is common in adolescent pregnancies,” she said.
Participants who were enrolled in prenatal care through the University of Colorado’s adolescent maternity program, where Dr. Rodriguez is a fellow, and who delivered at the University of Colorado Hospital, Aurora, were eligible to participate; adolescents were excluded for multiple gestation and for known major fetal anomalies or aneuploidy.
In addition to urine toxicology testing, participants also completed a uniformly administered substance use questionnaire. Marijuana exposure was defined as either having a positive urine toxicology result or self-reported marijuana use on the questionnaire (or both). Of the marijuana-exposed pregnancies, 133 (63%) of the adolescents tested positive on urine toxicology, 18 (9%) were positive by self-report, and 60 (28%) had both positive marijuana urine toxicology and positive self-report. Toxicology was available for 91% of participants.
Participants were negative for marijuana exposure if they had a negative toxicology screen, regardless of their response on the substance-use questionnaire.
The study’s primary outcome was a composite of adverse pregnancy outcomes, including stillbirth, defined as Apgar score of 0; any hypertensive disorder of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count); preterm birth, defined as spontaneous delivery before 37 weeks gestation; and infants born small for gestational age, defined as a birth weight below the 10th percentile after adjustment for gestational age and sex.
Secondary outcomes included pregnancy outcomes including placental abruption, mode of delivery, and gestational age at delivery. Neonatal outcomes included weight, length, and head circumference at birth, and neonatal intensive care unit admission. An Apgar score less than 7 at 5 minutes was considered an adverse neonatal outcome.
The sample size was determined by an estimate drawn from previous chart abstraction that the composite outcome would be seen in 16% of the clinic’s non–marijuana exposed patients, and 24% of the marijuana-exposed patients. The investigators also factored in that 18% of adolescents in the clinic database were marijuana users.
Dr. Rodriguez and her collaborators used a variety of models for statistical analysis, some of which included self-report alone or in conjunction with urine toxicology. In the end, they found that significant associations between their composite endpoint and marijuana use were seen when patients were dichotomized into those who had at least one positive urine toxicology test, versus those who had no positive toxicology results.
One of the study limitations was that the study didn’t permit investigators to get accurate information about the quantity, timing, or route of marijuana dosing. Also, this methodology may primarily identify heavier marijuana users, said Dr. Rodriguez.
Tobacco use was determined only by self-report, and outcomes were followed over a relatively short period of time.
Still, said Dr. Rodriguez, the study had many strengths, including the use of biological sampling to determine exposure and the near-universal participant urine toxicology testing. The investigators were able to capture and account for many important factors that could confound the results, she said. “Uncertainty regarding the impact of [marijuana] on pregnancy outcomes in the literature may result from incomplete ascertainment of exposure,” she and her coinvestigators wrote in the abstract accompanying the presentation.
SOURCE: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Maternal and fetal outcomes were worse when marijuana use was detected by urine toxicology.
Major finding: A composite adverse outcome occurred in 46% of adolescent marijuana users, compared with 34% of non–marijuana users (P less than .001).
Study details: Retrospective cohort study of participants in an adolescent maternity clinic.
Disclosures: The authors reported no conflicts of interest.
Source: Rodriguez C et al. Am J Obstet Gynecol. 2018 Jan;218:S37.
No clear winner in Pfannenstiel vs. vertical incision for high BMI cesareans
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
DALLAS – though enrollment difficulties limited study numbers, with almost two-thirds of eligible women declining to participate in the surgical trial.
At 6 weeks postdelivery, 21.1% of women who had a vertical incision experienced wound complications, compared with 18.6% of those who had a Pfannenstiel incision, a nonsignificant difference. This was a smaller difference than was seen at 2 weeks postpartum, when 20% of the vertical incision group had wound complications, compared with 10.4% of those who had a Pfannenstiel, also a nonsignificant difference. Maternal and fetal outcomes didn’t differ significantly with the two surgical approaches.
Though there had been several observational studies comparing vertical with Pfannenstiel incisions for cesarean delivery in women with obesity, no randomized, controlled trials had been conducted, and observational study results were mixed, said Dr. Marrs.
Each approach comes with theoretical pros and cons: For women who have a large pannus, the incision site may lie in a moist environment with a low transverse incision, and oxygen tension may be low. However, a Pfannenstiel incision usually will have better cosmesis than will a vertical incision, and generally will result in less postoperative pain.
On the other hand, said Dr. Marrs, vertical incisions can provide improved exposure of the uterus during delivery, and the moist environment underlying the pannus is avoided. However, wound tension may be higher, and subcutaneous thickness is likely to be higher than at the Pfannenstiel incision site.
The study, conducted at two academic medical centers, enrolled women with a body mass index (BMI) of at least 40 kg/m2 at a gestational age of 24 weeks or greater who required cesarean delivery. Consenting women were then randomized to receive Pfannenstiel or vertical incisions.
Women who had clinical chorioamnionitis, whose amniotic membranes had been ruptured for 18 hours or more, or who had placenta accreta were excluded. Also excluded were women with a private physician and those desiring vaginal delivery, said Dr. Marrs, a maternal-fetal medicine fellow at the University of Texas Medical Branch, Galveston.
The study’s primary outcome measure was a composite of wound complications seen within 6 weeks of delivery, including surgical site infection, whether superficial, deep, or involving an organ or tissue space; cellulitis; seroma or hematoma; and wound separation. Other maternal outcomes tracked in the study included postoperative length of stay, transfusion requirement, sepsis, readmission, and death.
Cesarean-specific secondary outcomes included operative time and time from skin incision to delivery, estimated blood loss, and any incidence of hysterectomy through a low transverse incision. Neonatal outcomes included a 5-minute Apgar score of less than 7, umbilical cord pH of less than 7, and neonatal ICU admissions.
Dr. Mars said that the goal enrollment for the study was 300 patients, to ensure adequate statistical power. However, they found enrollment a challenge, with low consent rates during the defined time period from October 2013 to May 2017. They shifted their statistical technique to a Bayesian analysis, taking into account the estimated probability of treatment benefit.
Using this approach, they found a 59% probability that a Pfannenstiel incision would lead to a lower primary outcome rate – a better result – than would a vertical incision. This result just missed the predetermined threshold of 60%, said Dr. Marrs.
Of the 789 women who met the BMI threshold for eligibility assessment, 420 (65%) who passed the screening declined to participate. Of those who consented to participation, an additional 137 women either withdrew consent or failed further screening, leaving 50 women who were randomized to the Pfannenstiel arm and 41 who were randomized to the vertical incision arm.
Baseline characteristics were similar between groups, with a mean maternal age of 30 years in the Pfannenstiel group and 28 years in the vertical incision group. Gestational age at delivery was a mean of 37 weeks in both groups, and mean BMI was 48-50 kg/m2.
Most patients (80%-90%) had public insurance. Diabetes was more common in the Pfannenstiel group (48%) than in the vertical incision cohort (32%). Just over 40% of patients were African American.
Two women in the Pfannenstiel group and three in the vertical incision group did not receive the intended incision. After accounting for patients lost to follow-up by 6 weeks, 43 women who received Pfannenstiel and 38 women who received vertical incisions were available for full evaluation.
Dr. Marrs said that the study, the first randomized trial to address this issue, had several strengths, including its being conducted at two sites with appropriate stratification for the sites. Also, an independent data safety monitoring board and two chart reviewers helped overcome some of the limitations of a surgical study, where complete blinding is impossible.
The Bayesian analysis allowed ascertainment of the probability of treatment benefit despite the lower-than-hoped-for enrollment numbers. The primary weakness of the study, said Dr. Marrs, centered around the low consent rate, which led to a small study that was prematurely terminated.
“It’s difficult to enroll women in a trial that requires random allocation of skin incision, due to their preference to choose their own incision. A larger trial would likewise be challenging, and unlikely to yield different results,” said Dr. Marrs.
Dr. Marrs reported no conflicts of interest.
SOURCE: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Wound complication rates were similar with Pfannenstiel and vertical incisions in women with obesity.
Major finding: At 6 weeks, 21.1% of vertical incision recipients and 18.6% of Pfannenstiel recipients had wound complications.
Study details: Randomized controlled trial of 91 women with obesity receiving cesarean section.
Disclosures: Dr. Marrs reported no conflicts of interest.
Source: Marrs CC et al. Am J Obstet Gynecol. 2018 Jan;218:S29.
Maternal hypertension QI initiative cuts severe morbidity by 41%
DALLAS – A statewide quality improvement initiative to address treatment strategies for women with severe maternal hypertension resulted in a 41% reduction in severe maternal morbidity, from 15% before the initiative to 9% after the suite of interventions was fully implemented.
A total of 102 Illinois hospitals participated in the quality improvement (QI) initiative, which eventually included 12,718 women with severe maternal hypertension, defined as blood pressure greater than 160/110 mm Hg.
The number of patients who were scheduled for follow-up appointments within 10 days of discharge increased from 53% to 83% after the QI initiative was implemented. The proportion of cases of severe maternal hypertension that were subject to a provider-nurse debrief analyzing time to treatment went from 2% before the intervention to 53%.
Dr. Lee King presented the findings to a receptive audience at a plenary session of the meeting sponsored by the Society for Maternal-Fetal Medicine. “We had a philosophy of ‘leave no hospital behind,’ and of ‘leave no patient behind,’ ” she said, to wide applause.
“The key prevention of maternal morbidity and mortality associated with severe maternal hypertension is timely treatment; the primary cause of maternal death associated with hypertensive disorders of pregnancy is maternal hemorrhagic stroke,” said Dr. Lee King.
The multidisciplinary, multistakeholder project was coordinated by the Illinois Perinatal Quality Collaborative (ILPQC), housed at Northwestern University, Chicago. The participating hospitals account for over 95% of the births in the state of Illinois, said Dr. Lee King, ILPQC state project director.
The approach used for implementation of the hypertension QI initiative included collaborative learning and the use of rapid response data to give near–real time feedback on how institutions were faring in meeting national guidelines to treat severe maternal hypertension.
Specific clinical interventions included both “system changes and culture changes,” said Dr. Lee King. They included adopting facility-wide protocols for timely identification and treatment of women with severe maternal hypertension; standardizing patient education and discharge planning; increasing provider and nurse education about severe maternal hypertension protocols; and creating rapid access to medication and standardized treatment order sets.
The ILPQC facilitated collaboration between hospitals in meeting these aims, including monthly web-based updates and seminars and construction of the database that gave institutions rapid access to data for ongoing QI efforts. Newsletters, website updates, and QI support were also part of the ILPQC package.
The proportion of participating hospitals meeting time-to-treatment goals for severe maternal hypertension went from 13% at baseline to 71% at the end of data collection, said Dr. Lee King.
In looking at hospital characteristics such as rurality, size, and patient mix, Dr. Lee King and her collaborators found no significant differences in time to treatment, patient education, and number of cases that were debriefed.
“These strategies helped hospitals achieve initiative goals, regardless of hospital characteristics,” said Dr. Lee King. The only significant association the research team found was that hospitals with fewer than 500 deliveries per year were less likely to reach the goal of early follow-up appointments (P less than .02).
“Participation in a statewide perinatal quality collaborative increases hospitals’ QI capacity. A statewide QI initiative can achieve significant population-level improvements in care for women with severe maternal hypertension and – more importantly – a reduction in severe maternal morbidity,” Dr. Lee King said.
The QI initiative and the follow-up study were conducted by the Illinois Perinatal Quality Collaborative, and the work was funded by the Centers for Disease Control and Prevention, the Illinois Department of Health, and the Alliance for Intervention on Maternal Health. Materials related to the maternal hypertension initiative are available at http://ilpqc.org/?q=Hypertension. Dr. Lee King reported no conflicts of interest.
SOURCE: Lee King P et al. Am J Obstet Gynecol. 2018 Jan;218:S4.
DALLAS – A statewide quality improvement initiative to address treatment strategies for women with severe maternal hypertension resulted in a 41% reduction in severe maternal morbidity, from 15% before the initiative to 9% after the suite of interventions was fully implemented.
A total of 102 Illinois hospitals participated in the quality improvement (QI) initiative, which eventually included 12,718 women with severe maternal hypertension, defined as blood pressure greater than 160/110 mm Hg.
The number of patients who were scheduled for follow-up appointments within 10 days of discharge increased from 53% to 83% after the QI initiative was implemented. The proportion of cases of severe maternal hypertension that were subject to a provider-nurse debrief analyzing time to treatment went from 2% before the intervention to 53%.
Dr. Lee King presented the findings to a receptive audience at a plenary session of the meeting sponsored by the Society for Maternal-Fetal Medicine. “We had a philosophy of ‘leave no hospital behind,’ and of ‘leave no patient behind,’ ” she said, to wide applause.
“The key prevention of maternal morbidity and mortality associated with severe maternal hypertension is timely treatment; the primary cause of maternal death associated with hypertensive disorders of pregnancy is maternal hemorrhagic stroke,” said Dr. Lee King.
The multidisciplinary, multistakeholder project was coordinated by the Illinois Perinatal Quality Collaborative (ILPQC), housed at Northwestern University, Chicago. The participating hospitals account for over 95% of the births in the state of Illinois, said Dr. Lee King, ILPQC state project director.
The approach used for implementation of the hypertension QI initiative included collaborative learning and the use of rapid response data to give near–real time feedback on how institutions were faring in meeting national guidelines to treat severe maternal hypertension.
Specific clinical interventions included both “system changes and culture changes,” said Dr. Lee King. They included adopting facility-wide protocols for timely identification and treatment of women with severe maternal hypertension; standardizing patient education and discharge planning; increasing provider and nurse education about severe maternal hypertension protocols; and creating rapid access to medication and standardized treatment order sets.
The ILPQC facilitated collaboration between hospitals in meeting these aims, including monthly web-based updates and seminars and construction of the database that gave institutions rapid access to data for ongoing QI efforts. Newsletters, website updates, and QI support were also part of the ILPQC package.
The proportion of participating hospitals meeting time-to-treatment goals for severe maternal hypertension went from 13% at baseline to 71% at the end of data collection, said Dr. Lee King.
In looking at hospital characteristics such as rurality, size, and patient mix, Dr. Lee King and her collaborators found no significant differences in time to treatment, patient education, and number of cases that were debriefed.
“These strategies helped hospitals achieve initiative goals, regardless of hospital characteristics,” said Dr. Lee King. The only significant association the research team found was that hospitals with fewer than 500 deliveries per year were less likely to reach the goal of early follow-up appointments (P less than .02).
“Participation in a statewide perinatal quality collaborative increases hospitals’ QI capacity. A statewide QI initiative can achieve significant population-level improvements in care for women with severe maternal hypertension and – more importantly – a reduction in severe maternal morbidity,” Dr. Lee King said.
The QI initiative and the follow-up study were conducted by the Illinois Perinatal Quality Collaborative, and the work was funded by the Centers for Disease Control and Prevention, the Illinois Department of Health, and the Alliance for Intervention on Maternal Health. Materials related to the maternal hypertension initiative are available at http://ilpqc.org/?q=Hypertension. Dr. Lee King reported no conflicts of interest.
SOURCE: Lee King P et al. Am J Obstet Gynecol. 2018 Jan;218:S4.
DALLAS – A statewide quality improvement initiative to address treatment strategies for women with severe maternal hypertension resulted in a 41% reduction in severe maternal morbidity, from 15% before the initiative to 9% after the suite of interventions was fully implemented.
A total of 102 Illinois hospitals participated in the quality improvement (QI) initiative, which eventually included 12,718 women with severe maternal hypertension, defined as blood pressure greater than 160/110 mm Hg.
The number of patients who were scheduled for follow-up appointments within 10 days of discharge increased from 53% to 83% after the QI initiative was implemented. The proportion of cases of severe maternal hypertension that were subject to a provider-nurse debrief analyzing time to treatment went from 2% before the intervention to 53%.
Dr. Lee King presented the findings to a receptive audience at a plenary session of the meeting sponsored by the Society for Maternal-Fetal Medicine. “We had a philosophy of ‘leave no hospital behind,’ and of ‘leave no patient behind,’ ” she said, to wide applause.
“The key prevention of maternal morbidity and mortality associated with severe maternal hypertension is timely treatment; the primary cause of maternal death associated with hypertensive disorders of pregnancy is maternal hemorrhagic stroke,” said Dr. Lee King.
The multidisciplinary, multistakeholder project was coordinated by the Illinois Perinatal Quality Collaborative (ILPQC), housed at Northwestern University, Chicago. The participating hospitals account for over 95% of the births in the state of Illinois, said Dr. Lee King, ILPQC state project director.
The approach used for implementation of the hypertension QI initiative included collaborative learning and the use of rapid response data to give near–real time feedback on how institutions were faring in meeting national guidelines to treat severe maternal hypertension.
Specific clinical interventions included both “system changes and culture changes,” said Dr. Lee King. They included adopting facility-wide protocols for timely identification and treatment of women with severe maternal hypertension; standardizing patient education and discharge planning; increasing provider and nurse education about severe maternal hypertension protocols; and creating rapid access to medication and standardized treatment order sets.
The ILPQC facilitated collaboration between hospitals in meeting these aims, including monthly web-based updates and seminars and construction of the database that gave institutions rapid access to data for ongoing QI efforts. Newsletters, website updates, and QI support were also part of the ILPQC package.
The proportion of participating hospitals meeting time-to-treatment goals for severe maternal hypertension went from 13% at baseline to 71% at the end of data collection, said Dr. Lee King.
In looking at hospital characteristics such as rurality, size, and patient mix, Dr. Lee King and her collaborators found no significant differences in time to treatment, patient education, and number of cases that were debriefed.
“These strategies helped hospitals achieve initiative goals, regardless of hospital characteristics,” said Dr. Lee King. The only significant association the research team found was that hospitals with fewer than 500 deliveries per year were less likely to reach the goal of early follow-up appointments (P less than .02).
“Participation in a statewide perinatal quality collaborative increases hospitals’ QI capacity. A statewide QI initiative can achieve significant population-level improvements in care for women with severe maternal hypertension and – more importantly – a reduction in severe maternal morbidity,” Dr. Lee King said.
The QI initiative and the follow-up study were conducted by the Illinois Perinatal Quality Collaborative, and the work was funded by the Centers for Disease Control and Prevention, the Illinois Department of Health, and the Alliance for Intervention on Maternal Health. Materials related to the maternal hypertension initiative are available at http://ilpqc.org/?q=Hypertension. Dr. Lee King reported no conflicts of interest.
SOURCE: Lee King P et al. Am J Obstet Gynecol. 2018 Jan;218:S4.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: The statewide QI initiative targeted treatment of women with severe maternal hypertension.
Major finding: Severe maternal morbidity fell 41%, from 15% to 9%, with the initiative.
Study details: Pre-post QI initiative analysis of data from 102 Illinois hospitals treating 12,718 women with severe maternal hypertension.
Disclosures: The study was funded by the Centers for Disease Control and Prevention, the Illinois Department of Health, and the Alliance for Intervention on Mental Health. Dr. Lee King is employed by the Illinois Perinatal Quality Collaborative, which conducted the study.
Source: Lee King P et al. Am J Obstet Gynecol. 2018 Jan;218:S4.
Salpingectomy at cesarean feasible, but adds to operative time
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
DALLAS – Salpingectomy – which can reduce the risk for later ovarian cancer – was completed successfully in about two-thirds of women who desired permanent contraception at cesarean delivery and were randomized to receive this procedure rather than simple tubal ligation.
In a study of 80 patients, operative times were longer by 15 minutes for those who received salpingectomy, and neither group had adverse outcomes or serious complications, according to Akila Subramaniam, MD, who presented the findings of the single-site Salpingectomy at Cesarean Delivery for Ovarian Cancer Reduction (SCORE) trial at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The strategy to perform salpingectomy during cesarean delivery may be one way to reduce the incidence of ovarian cancer, “the most lethal gynecologic malignancy in the United States,” said Dr. Subramaniam, a maternal-fetal medicine specialist at the University of Alabama at Birmingham. “Primary prevention is the focus to reduce the ovarian cancer burden.”
However, Dr. Subramaniam said, there had been limited prospective data on salpingectomy performed at the time of cesarean delivery. One theoretical concern is an increased risk of bleeding; another is the additional operative time required for a potentially difficult dissection of the entire fallopian tube.
Dr. Subramaniam and her colleagues constructed a clinical trial that asked patients who were receiving cesarean delivery and who desired surgical sterilization to agree to randomization to complete salpingectomy or standard tubal ligation. Patient allocation was determined by computer-generated numbers, placed in a sealed envelope, and revealed to the surgeon only at the time of the opening incision for the cesarean procedure. Patients were unaware of the allocation until hospital discharge.
The single-center trial enrolled women undergoing a planned cesarean delivery at 35 or more weeks’ gestation, including those who had previous cesareans and women with multiple gestations or fetal malpresentations. Women who went on to cesarean after a trial of labor after prior cesarean were also eligible.
Patients younger than 25 years and patients with known fetal anomalies or fetal demise were excluded, as were women with previous tubal surgery and those who were anticoagulated or had immunodeficiency. The study did not enroll women who were known to carry the BRCA mutation.
Patients who were randomized to the intervention arm received a complete salpingectomy involving excision from the fimbriae to within 1 cm of the cornua, when technically feasible. The control arm participants received a standard bilateral tubal ligation using either the modified Pomeroy technique or the Parkland technique.
All study participants received routine pre- and postoperative care and instructions, and had study follow-up visits at 1 and 6 weeks post partum.
The study had two primary endpoints: rate of bilateral completion of the randomized procedure, and mean total operative time measured from skin incision to closure. Secondary outcomes included assessments of blood loss and surgical complications, followed through the 6-week postpartum visit.
The study just met the predetermined statistical power needed to detect a 10-minute difference in operative time, enrolling 80 patients and randomizing 40 to each arm.
Of the 40 patients randomized to salpingectomy, 27 (67.5%) received the intended complete salpingectomy. Three had a unilateral salpingectomy, with a tubal ligation contralaterally. Eight patients received bilateral tubal ligations, and in two patients, the surgeon was unable to perform any sterilization procedure at all.
In the tubal ligation arm, 38 patients (95%) received bilateral tubal ligation, 1 patient received a unilateral tubal ligation and a unilateral salpingectomy, and 1 patient received no procedure. The difference in success of completing the intended procedures between the two study arms was statistically significant (P = .002); in both groups, adhesions and scarring were the primary impediments to successful completion of the intended procedure, Dr. Subramaniam said.
Operative times were longer by about 15 minutes in the salpingectomy arm, with the difference accounted for by the longer duration of the sterilization procedure. No significant differences were seen in estimated blood loss or decrease in hematocrit between the two groups, and pain scores were similar.
The study, which successfully recruited 80 women from 221 approached, “may be underpowered for safety outcomes,” said Dr. Subramaniam. She also pointed out that there was no assessment of ovarian reserve, and that it’s not possible to assess the true risk reduction of salpingectomy in this study design.
Still, “It’s reasonable to consider this surgical sterilization method during cesarean as an ovarian cancer risk-reducing strategy.” One impediment to study recruitment, she said, was that after receiving education about salpingectomy, many patients desired salpingectomy and were not willing to risk randomization to simple tubal ligation.
Dr. Subramaniam reported receiving research funding for the study from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
SOURCE: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Salpingectomy was successful in two-thirds of patients but added 15 minutes to operative time.
Major finding: The intended procedure was successful in 27 of 40 salpingectomy patients (67.5%) and 38 of 40 tubal ligation patients (95%; P = .02).
Study details: Randomized controlled trial of 80 women receiving bilateral salpingectomy or tubal ligation at cesarean delivery.
Disclosures: Study funding was received from the Debra Kogan Lyda Memorial Ovarian Cancer Fund.
Source: Subramaniam A et al. Am J Obstet Gynecol. 2018 Jan;218:S27-8.
Postcesarean SSI rate declines with care bundle*
DALLAS – A surgical site infection care bundle reduced the rate of surgical site infections (SSIs) after cesarean delivery by more than half, according to a case-control study examining data from more than 2,000 patients.
At the health center where the SSI bundle was implemented, rates per 1,000 women undergoing cesarean delivery fell from 2.44 to 1.10 (P = .013).
The study showed the effectiveness of implementing evidence-based and -supported recommendations, and of having standardized protocols with little variation, said Christina Davidson, MD, presenting the pre-post findings during a plenary session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The bundle of interventions was developed over the course of 3 months in late 2013 and early 2014 by a multidisciplinary task force, drawing from colorectal surgery literature about SSI prevention. Both nurses and physicians were on the task force, and representatives came from the departments of obstetrics and gynecology, anesthesia, and infection prevention, said Dr. Davidson of the Baylor College of Medicine, Houston. All inpatient and outpatient clinical care sites had representation.
After the bundle elements were identified, a full month was devoted to education and team training, with full bundle implementation occurring in April 2014. “Visual aids were placed in close proximity to the operating rooms,” said Dr. Davidson. For example, antimicrobial prophylaxis cards were placed on all anesthetic carts.
“A surgical checklist was placed in the chart for each patient undergoing cesarean delivery and compliance was tracked for the first 12 months of implementation,” said Dr. Davidson. Additionally, members of the care team received feedback in the form of quarterly reports on SSI rates and statistics about bundle compliance.
Care bundle elements included a set of instructions for pre- and postoperative antiseptic skin cleaning, wound care, and glycemic control in patients. Women were given chlorhexidine cleanser and asked to use it when showering the day before and the morning of surgery for planned deliveries. Forced warm-air blankets maintained patient normothermia in the preoperative holding area.
A group of intraoperative interventions included use of antiseptic skin and vaginal preparations, double-gloving, and having all scrubbed members of the surgical team change their outer gloves for fascial closure. A new instrument tray also was used for fascial closure. Prophylactic antibiotics were administered within 1 hour of skin incision, and doses were readministered based on the length of the procedure.
Postoperatively, said Dr. Davidson, “a set of insulin orders within the electronic medical record [was] used to maintain euglycemia in all diabetic patients.”
After the surgical dressing was removed on the 2nd postoperative day, patients were given a handout and education about wound control and infection prevention.
Finally, all patients received postdischarge follow-up calls from nurses within 72 hours after discharge.
Patient characteristics generally were similar before (n = 1,085) and after (n = 1,261) SSI bundle implementation. Body mass index was slightly higher in the postbundle group, and women in this group also were less likely to have had a prior cesarean delivery. There were no significant differences in age, gravidity, ethnicity, or race.
The study showed that with continued tracking, data-sharing, and reeducation efforts, “The SSI rate was sustained after bundle implementation,” said Dr. Davidson. The implementation team, working with hospital departments, was able to achieve a high compliance rate. And, she said, the effect size of the intervention was large enough to show significant reduction from an already low SSI rate.
However, Dr. Davidson also noted some limitations: All of the bundle elements were implemented simultaneously, so it wasn’t possible to tell which components had the greatest effect. Also, not all demographic data were available, and the type of SSI was sometimes unavailable from the deidentified data repository used for analysis, she said. “We weren’t able to tease out individual patient-level characteristics” about the timing and type of SSI in a patient-by-patient fashion, she said during discussion following her presentation.
All in all, she said, the bundle’s effectiveness “supports the synergistic effects of multiple strategies and the impact of a multidisciplinary team approach.”
The study authors reported no conflicts of interest.
SOURCE: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Correction, 3/5/18: An earlier version of this article omitted the word "rate" from the headline and Vitals section.
DALLAS – A surgical site infection care bundle reduced the rate of surgical site infections (SSIs) after cesarean delivery by more than half, according to a case-control study examining data from more than 2,000 patients.
At the health center where the SSI bundle was implemented, rates per 1,000 women undergoing cesarean delivery fell from 2.44 to 1.10 (P = .013).
The study showed the effectiveness of implementing evidence-based and -supported recommendations, and of having standardized protocols with little variation, said Christina Davidson, MD, presenting the pre-post findings during a plenary session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The bundle of interventions was developed over the course of 3 months in late 2013 and early 2014 by a multidisciplinary task force, drawing from colorectal surgery literature about SSI prevention. Both nurses and physicians were on the task force, and representatives came from the departments of obstetrics and gynecology, anesthesia, and infection prevention, said Dr. Davidson of the Baylor College of Medicine, Houston. All inpatient and outpatient clinical care sites had representation.
After the bundle elements were identified, a full month was devoted to education and team training, with full bundle implementation occurring in April 2014. “Visual aids were placed in close proximity to the operating rooms,” said Dr. Davidson. For example, antimicrobial prophylaxis cards were placed on all anesthetic carts.
“A surgical checklist was placed in the chart for each patient undergoing cesarean delivery and compliance was tracked for the first 12 months of implementation,” said Dr. Davidson. Additionally, members of the care team received feedback in the form of quarterly reports on SSI rates and statistics about bundle compliance.
Care bundle elements included a set of instructions for pre- and postoperative antiseptic skin cleaning, wound care, and glycemic control in patients. Women were given chlorhexidine cleanser and asked to use it when showering the day before and the morning of surgery for planned deliveries. Forced warm-air blankets maintained patient normothermia in the preoperative holding area.
A group of intraoperative interventions included use of antiseptic skin and vaginal preparations, double-gloving, and having all scrubbed members of the surgical team change their outer gloves for fascial closure. A new instrument tray also was used for fascial closure. Prophylactic antibiotics were administered within 1 hour of skin incision, and doses were readministered based on the length of the procedure.
Postoperatively, said Dr. Davidson, “a set of insulin orders within the electronic medical record [was] used to maintain euglycemia in all diabetic patients.”
After the surgical dressing was removed on the 2nd postoperative day, patients were given a handout and education about wound control and infection prevention.
Finally, all patients received postdischarge follow-up calls from nurses within 72 hours after discharge.
Patient characteristics generally were similar before (n = 1,085) and after (n = 1,261) SSI bundle implementation. Body mass index was slightly higher in the postbundle group, and women in this group also were less likely to have had a prior cesarean delivery. There were no significant differences in age, gravidity, ethnicity, or race.
The study showed that with continued tracking, data-sharing, and reeducation efforts, “The SSI rate was sustained after bundle implementation,” said Dr. Davidson. The implementation team, working with hospital departments, was able to achieve a high compliance rate. And, she said, the effect size of the intervention was large enough to show significant reduction from an already low SSI rate.
However, Dr. Davidson also noted some limitations: All of the bundle elements were implemented simultaneously, so it wasn’t possible to tell which components had the greatest effect. Also, not all demographic data were available, and the type of SSI was sometimes unavailable from the deidentified data repository used for analysis, she said. “We weren’t able to tease out individual patient-level characteristics” about the timing and type of SSI in a patient-by-patient fashion, she said during discussion following her presentation.
All in all, she said, the bundle’s effectiveness “supports the synergistic effects of multiple strategies and the impact of a multidisciplinary team approach.”
The study authors reported no conflicts of interest.
SOURCE: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Correction, 3/5/18: An earlier version of this article omitted the word "rate" from the headline and Vitals section.
DALLAS – A surgical site infection care bundle reduced the rate of surgical site infections (SSIs) after cesarean delivery by more than half, according to a case-control study examining data from more than 2,000 patients.
At the health center where the SSI bundle was implemented, rates per 1,000 women undergoing cesarean delivery fell from 2.44 to 1.10 (P = .013).
The study showed the effectiveness of implementing evidence-based and -supported recommendations, and of having standardized protocols with little variation, said Christina Davidson, MD, presenting the pre-post findings during a plenary session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The bundle of interventions was developed over the course of 3 months in late 2013 and early 2014 by a multidisciplinary task force, drawing from colorectal surgery literature about SSI prevention. Both nurses and physicians were on the task force, and representatives came from the departments of obstetrics and gynecology, anesthesia, and infection prevention, said Dr. Davidson of the Baylor College of Medicine, Houston. All inpatient and outpatient clinical care sites had representation.
After the bundle elements were identified, a full month was devoted to education and team training, with full bundle implementation occurring in April 2014. “Visual aids were placed in close proximity to the operating rooms,” said Dr. Davidson. For example, antimicrobial prophylaxis cards were placed on all anesthetic carts.
“A surgical checklist was placed in the chart for each patient undergoing cesarean delivery and compliance was tracked for the first 12 months of implementation,” said Dr. Davidson. Additionally, members of the care team received feedback in the form of quarterly reports on SSI rates and statistics about bundle compliance.
Care bundle elements included a set of instructions for pre- and postoperative antiseptic skin cleaning, wound care, and glycemic control in patients. Women were given chlorhexidine cleanser and asked to use it when showering the day before and the morning of surgery for planned deliveries. Forced warm-air blankets maintained patient normothermia in the preoperative holding area.
A group of intraoperative interventions included use of antiseptic skin and vaginal preparations, double-gloving, and having all scrubbed members of the surgical team change their outer gloves for fascial closure. A new instrument tray also was used for fascial closure. Prophylactic antibiotics were administered within 1 hour of skin incision, and doses were readministered based on the length of the procedure.
Postoperatively, said Dr. Davidson, “a set of insulin orders within the electronic medical record [was] used to maintain euglycemia in all diabetic patients.”
After the surgical dressing was removed on the 2nd postoperative day, patients were given a handout and education about wound control and infection prevention.
Finally, all patients received postdischarge follow-up calls from nurses within 72 hours after discharge.
Patient characteristics generally were similar before (n = 1,085) and after (n = 1,261) SSI bundle implementation. Body mass index was slightly higher in the postbundle group, and women in this group also were less likely to have had a prior cesarean delivery. There were no significant differences in age, gravidity, ethnicity, or race.
The study showed that with continued tracking, data-sharing, and reeducation efforts, “The SSI rate was sustained after bundle implementation,” said Dr. Davidson. The implementation team, working with hospital departments, was able to achieve a high compliance rate. And, she said, the effect size of the intervention was large enough to show significant reduction from an already low SSI rate.
However, Dr. Davidson also noted some limitations: All of the bundle elements were implemented simultaneously, so it wasn’t possible to tell which components had the greatest effect. Also, not all demographic data were available, and the type of SSI was sometimes unavailable from the deidentified data repository used for analysis, she said. “We weren’t able to tease out individual patient-level characteristics” about the timing and type of SSI in a patient-by-patient fashion, she said during discussion following her presentation.
All in all, she said, the bundle’s effectiveness “supports the synergistic effects of multiple strategies and the impact of a multidisciplinary team approach.”
The study authors reported no conflicts of interest.
SOURCE: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Correction, 3/5/18: An earlier version of this article omitted the word "rate" from the headline and Vitals section.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: The postcesarean surgical site infection rate dropped by more than half after a multicomponent care bundle was put in place.*
Major finding: SSIs patients went from 2.44 to 1.10/1,000 after the bundle was implemented (P = .013).
Study details: Case-control study of 1,085 women pre– and 1,261 women post–care bundle implementation.
Disclosures: The authors reported no conflicts of interest.
Source: Davidson C et al. Am J Obstet Gynecol. 2018 Jan;218:S46.
Short cervical length more common among black women, and more predictive of preterm birth
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.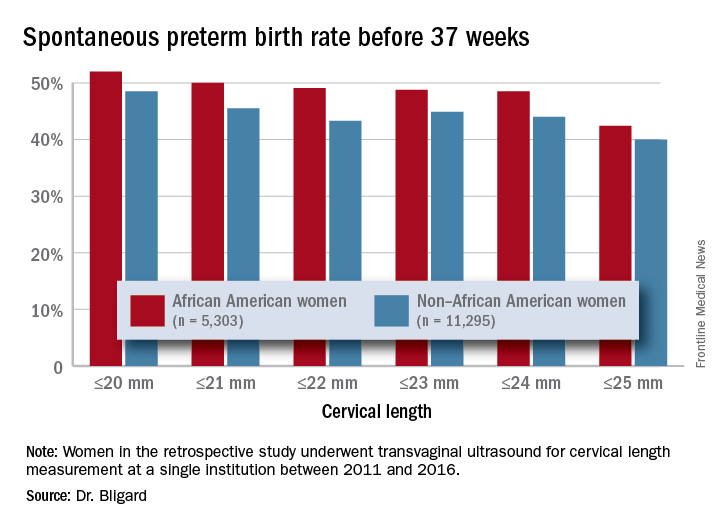
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.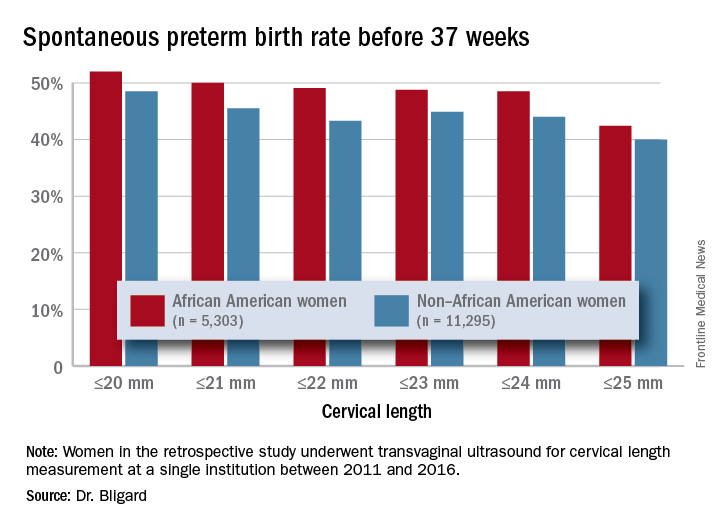
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
DALLAS – Black women are more than twice as likely as nonblacks to have a short cervix in midpregnancy – a finding that may bear some responsibility for their consistently higher rates of spontaneous preterm birth.
A large retrospective study of more than 16,500 women determined that having a cervical length of 20 mm or less was 2.6 times more common among black women than it was among women of other races or ethnicities, Katherine Bligard, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. And no matter what the cervical length cutoff – from 20 mm or less all the way up to 25 mm – having a short cervix conferred a significantly higher risk of spontaneous preterm birth upon black women than it did upon the comparator groups.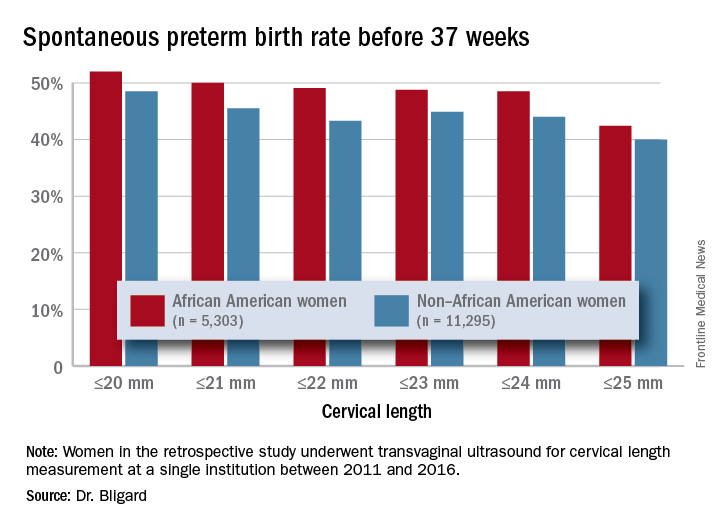
Dr. Bligard and her colleagues retrospectively examined the prevalence of short cervical length in a cohort of 16,598 women who underwent transvaginal ultrasound for cervical length measurement at a single institution between 2011 and 2016. Of these, 5,303 identified as black. These women were significantly younger than were the women who were not black (27 vs. 31 years, respectively) and were seen at a later gestational age (20.2 vs. 19.8 weeks). They were more likely to be smokers (10% vs. 5%), to be obese (40% vs. 25%), to be multiparous (70% vs. 65%), and to have a history of spontaneous preterm birth (6% vs. 3%).
The mean cervical length was significantly shorter in black women (40.3 vs. 41.1 mm). Significantly more had a cervical length of 25 mm or less (3% vs. 1.2%) or 20 mm or less (1.9% vs. 0.6%). After adjusting for gestational age at scan, tobacco use, and history of preterm birth, black women were twice as likely to have a cervical length of 25 mm or less and 2.6 times more likely to have one of 20 mm or less.
An area-under-the-curve analysis showed that shorter cervical length was significantly more predictive of spontaneous preterm birth for black women than it was for nonblack women (AUC, 0.66 vs. 0.62).
Dr. Bligard also looked at sensitivity and specificity for preterm birth at different gestational ages. At a 20 mm or less cutoff, cervical length in black women was just as specific for preterm birth occurring at less than 24 weeks, less than 28 weeks, less than 34 weeks, and less than 37 weeks (98%-99%), but it had a much higher sensitivity (44% vs. 26%, 36% vs. 23%, 26% vs.13%, and 12% vs. 5%, respectively).
The rate of preterm birth was higher for black women at every cervical length cutoff examined, Dr. Bligard noted.
The results should guide current therapy and inform future investigations, she suggested.
“Our data also suggest that race-based cervical length cutoffs may be beneficial in driving treatment, especially in light of the therapies that are available,” Dr. Bligard said. “Future studies should evaluate the efficacy of currently available therapies at a longer cervical length in African American women.”
Washington University sponsored the study, which was also funded by a training grant from the National Institutes of Health. Dr. Bligard had no financial disclosures.
SOURCE: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Having a short cervix is more common among black women and more predictive of spontaneous preterm birth.
Major finding: Cervical length of 20 mm or less was 2.6 times more common among black women than it was women of other races or ethnicities.
Study details: The retrospective review comprised more than 16,500 women.
Disclosures: The study was sponsored by Washington University and the National Institutes of Health. Dr. Bligard had no financial disclosures.
Source: Bligard K et al. Am J Obstet Gynecol. 2018;218:S62-3.
Abdominal CT refines treatment in refractory puerperal fever
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
DALLAS – Abdominal CT scans changed therapeutic management in 39% of women being unsuccessfully treated for refractory puerperal fever, a retrospective study has determined.
The scans pinpointed a definite diagnosis in the majority of the cohort, allowing clinicians to reassess their treatment, Michal Fishel-Bartal, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“This study has important clinical implications for women with refractory puerperal fever,” said Dr. Fishel-Bartal of the Chaim Sheba Medical Center, Ramat Gan, Israel. “Our department now recommends that all women with refractory puerperal fever should undergo an assessment for risk factors, including urgent cesarean section, preterm delivery, and general anesthesia, and an evaluation to see if an abdominal CT may be appropriate to investigate the possibility of septic pelvic thrombophlebitis or the need for intra-abdominal drainage.”
She and her colleagues conducted a 10-year retrospective review of refractory puerperal fever cases at Chaim Sheba Medical Center. All of the patients had a CT scan within 7 days of their delivery. A radiologist reviewed each scan, looking for potential causes of the illness, including pelvic collection (a suspected pelvic abscess or collection of 4 cm or more) or signs of septic pelvic thrombophlebitis (enlargement of an involved vein, vessel wall enhancement, or a filling defect).
The primary outcome was a treatment change due to the CT results. These included switching antibiotics, starting therapeutic low-molecular-weight heparin, or a surgical intervention (intra-abdominal drainage or laparotomy).
The cohort comprised 238 women, who were a mean age of 33 years. In comparing them with the hospital’s background population, they were significantly more likely to have delivered at less than 37 weeks (25% vs. 7%), and to have had a cesarean delivery (80% vs. 25%). Dr. Fishel-Bartal also noted that 29% of the patients had experienced general anesthesia.
Most of the scans (144; 60%) were abnormal. Findings included septic pelvic thrombophlebitis (32) and pelvic collections (112). Treatment changed in 93 women (39% of the entire cohort). Changes included adding or switching antibiotics (24), adding low-molecular-weight heparin (28), laparotomy (11), and drainage insertion (30).
The investigators also performed a multivariate analysis to identify any risk factors that significantly predicted the need to change or add treatment. General anesthesia was the only factor significantly more common among those who needed a treatment switch (70% vs. 58%). This could have been a marker for an urgent C-section – something often associated with complications, Dr. Fishel-Bartal noted.
In the discussion period, Dr. Fishel-Bartal fielded a question about whether ultrasound would be a more logical and cost-effective method of assessing these patients.
“We actually do usually start with an ultrasound evaluation in our patients with refractory puerperal fever, and 68% of this group did have one,” Dr. Fishel-Bartal replied. “Findings were positive in 37%. The ultrasound actually was very good at predicting pelvic collections, but it only identified 5 of the 32 with septic thrombophlebitis. So it’s a good modality to start with, but if the patient still has fever or there is a concern for septic pelvic thrombosis, you really still need a CT.”
She had no financial disclosures.
SOURCE: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: An abdominal CT was the key to getting treatment right for women with refractory puerperal fever.
Major finding: After the scans, 39% of women got a change in treatment.
Study details: The retrospective review comprised 238 women.
Disclosures: Dr. Fishel-Bartal had no financial disclosures.
Source: Fishel-Bartal M et al. The Pregnancy Meeting. Am J Obstet Gynecol. 2018;218:S59.
Intrapartum maternal oxygen may not be beneficial for resuscitating fetuses with category II heart tracings
DALLAS – Room air was not inferior to maternal oxygen supplementation for the management of category II fetal heart tracings in a clinical trial.
Umbilical cord blood lactate – a marker of fetal acidosis caused by oxygen deprivation – was virtually identical whether the women received oxygen or remained on room air, Nandini Raghuraman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Other blood gas measures were similar as well, and there were no differences in the number of cesarean sections or operative vaginal deliveries, said Dr. Raghuraman of Washington University, St. Louis.
“Our results suggest that room air is an acceptable alternative. However, we do need further studies, including a superiority trial.”
She noted that three randomized studies have compared oxygen to room air. “None demonstrated benefit to the fetus, and some demonstrated harm, including higher rates of delivery room resuscitation and higher neonatal acidemia. Importantly, all of these studies excluded patients with abnormal fetal heart tracings, which is the primary indication for maternal oxygen during labor and delivery.”
Her study comprised 114 women in active labor with a normal singleton fetus that developed category II heart tracings. Women received either oxygen at 10 L per minute by face mask, or stayed on room air with no face mask. The intervention continued to delivery.
The primary outcome was umbilical artery lactate. Secondary outcomes were umbilical artery blood gases, C-section for nonreassuring fetal heart status, and operative vaginal delivery.
The women were a mean age of 27.5 years; about three-quarters were black. Most (70%) had a labor induction, and 89% had received oxytocin. There were no between-group differences in the need for other fetal resuscitation strategies, including IV fluid bolus, total IV fluids, discontinuation or decrease in oxytocin, maternal repositioning, amnioinfusion, and time from randomization to delivery.
There was no difference in the primary outcome: Lactate levels were 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Dr. Raghuraman also looked at lactate levels among those neonates who had recurrent decelerations and who did not. There was no significant difference in this comparison.
The secondary outcome of umbilical artery blood gases included measures of pH, base excess, partial CO2, and partial oxygen. There were no significant differences in any of these comparisons. Partial O2 was higher (though not significantly so) in the samples that had been exposed to oxygen, as would be expected, Dr. Raghuraman noted.
There were fewer cesarean deliveries among the room air group (4% vs. 12.5%), although this was not statistically significant. Two neonates in the oxygen group were delivered by C-section for nonreassuring fetal heart tracings. There were more operative vaginal deliveries in the room air group (11.8% vs. 2%), but this difference was not statistically significant, with a wide confidence interval (0.71-45.2).
“These results alone are not enough to be practice changing,” Dr. Raghuraman said. “Before we can do that, we need to address efficacy, which this study has called into question. But we also need to explore the results of safety and harm, and until we do so our nurses will likely continue their usual practice of putting these patients on supplement oxygen.”
She had no financial disclosures.
SOURCE: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
DALLAS – Room air was not inferior to maternal oxygen supplementation for the management of category II fetal heart tracings in a clinical trial.
Umbilical cord blood lactate – a marker of fetal acidosis caused by oxygen deprivation – was virtually identical whether the women received oxygen or remained on room air, Nandini Raghuraman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Other blood gas measures were similar as well, and there were no differences in the number of cesarean sections or operative vaginal deliveries, said Dr. Raghuraman of Washington University, St. Louis.
“Our results suggest that room air is an acceptable alternative. However, we do need further studies, including a superiority trial.”
She noted that three randomized studies have compared oxygen to room air. “None demonstrated benefit to the fetus, and some demonstrated harm, including higher rates of delivery room resuscitation and higher neonatal acidemia. Importantly, all of these studies excluded patients with abnormal fetal heart tracings, which is the primary indication for maternal oxygen during labor and delivery.”
Her study comprised 114 women in active labor with a normal singleton fetus that developed category II heart tracings. Women received either oxygen at 10 L per minute by face mask, or stayed on room air with no face mask. The intervention continued to delivery.
The primary outcome was umbilical artery lactate. Secondary outcomes were umbilical artery blood gases, C-section for nonreassuring fetal heart status, and operative vaginal delivery.
The women were a mean age of 27.5 years; about three-quarters were black. Most (70%) had a labor induction, and 89% had received oxytocin. There were no between-group differences in the need for other fetal resuscitation strategies, including IV fluid bolus, total IV fluids, discontinuation or decrease in oxytocin, maternal repositioning, amnioinfusion, and time from randomization to delivery.
There was no difference in the primary outcome: Lactate levels were 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Dr. Raghuraman also looked at lactate levels among those neonates who had recurrent decelerations and who did not. There was no significant difference in this comparison.
The secondary outcome of umbilical artery blood gases included measures of pH, base excess, partial CO2, and partial oxygen. There were no significant differences in any of these comparisons. Partial O2 was higher (though not significantly so) in the samples that had been exposed to oxygen, as would be expected, Dr. Raghuraman noted.
There were fewer cesarean deliveries among the room air group (4% vs. 12.5%), although this was not statistically significant. Two neonates in the oxygen group were delivered by C-section for nonreassuring fetal heart tracings. There were more operative vaginal deliveries in the room air group (11.8% vs. 2%), but this difference was not statistically significant, with a wide confidence interval (0.71-45.2).
“These results alone are not enough to be practice changing,” Dr. Raghuraman said. “Before we can do that, we need to address efficacy, which this study has called into question. But we also need to explore the results of safety and harm, and until we do so our nurses will likely continue their usual practice of putting these patients on supplement oxygen.”
She had no financial disclosures.
SOURCE: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
DALLAS – Room air was not inferior to maternal oxygen supplementation for the management of category II fetal heart tracings in a clinical trial.
Umbilical cord blood lactate – a marker of fetal acidosis caused by oxygen deprivation – was virtually identical whether the women received oxygen or remained on room air, Nandini Raghuraman, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine. Other blood gas measures were similar as well, and there were no differences in the number of cesarean sections or operative vaginal deliveries, said Dr. Raghuraman of Washington University, St. Louis.
“Our results suggest that room air is an acceptable alternative. However, we do need further studies, including a superiority trial.”
She noted that three randomized studies have compared oxygen to room air. “None demonstrated benefit to the fetus, and some demonstrated harm, including higher rates of delivery room resuscitation and higher neonatal acidemia. Importantly, all of these studies excluded patients with abnormal fetal heart tracings, which is the primary indication for maternal oxygen during labor and delivery.”
Her study comprised 114 women in active labor with a normal singleton fetus that developed category II heart tracings. Women received either oxygen at 10 L per minute by face mask, or stayed on room air with no face mask. The intervention continued to delivery.
The primary outcome was umbilical artery lactate. Secondary outcomes were umbilical artery blood gases, C-section for nonreassuring fetal heart status, and operative vaginal delivery.
The women were a mean age of 27.5 years; about three-quarters were black. Most (70%) had a labor induction, and 89% had received oxytocin. There were no between-group differences in the need for other fetal resuscitation strategies, including IV fluid bolus, total IV fluids, discontinuation or decrease in oxytocin, maternal repositioning, amnioinfusion, and time from randomization to delivery.
There was no difference in the primary outcome: Lactate levels were 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Dr. Raghuraman also looked at lactate levels among those neonates who had recurrent decelerations and who did not. There was no significant difference in this comparison.
The secondary outcome of umbilical artery blood gases included measures of pH, base excess, partial CO2, and partial oxygen. There were no significant differences in any of these comparisons. Partial O2 was higher (though not significantly so) in the samples that had been exposed to oxygen, as would be expected, Dr. Raghuraman noted.
There were fewer cesarean deliveries among the room air group (4% vs. 12.5%), although this was not statistically significant. Two neonates in the oxygen group were delivered by C-section for nonreassuring fetal heart tracings. There were more operative vaginal deliveries in the room air group (11.8% vs. 2%), but this difference was not statistically significant, with a wide confidence interval (0.71-45.2).
“These results alone are not enough to be practice changing,” Dr. Raghuraman said. “Before we can do that, we need to address efficacy, which this study has called into question. But we also need to explore the results of safety and harm, and until we do so our nurses will likely continue their usual practice of putting these patients on supplement oxygen.”
She had no financial disclosures.
SOURCE: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Room air was not inferior to maternal oxygen for the resuscitation of a fetus who developed category II heart rhythms.
Major finding: Umbilical artery lactate was 3.4 mmol/L in the oxygen group and 3.5 mmol/L in the room air group.
Study details: The trial randomized 114 women.
Disclosures: The study was sponsored by the Washington University School of Medicine. Dr. Raghuraman had no financial disclosures.
Source: Raghuraman N et al. Am J Obstet Gynecol. 2018 Jan;218:S7.
Monthly vs. biweekly ultrasounds to ID fetal growth and amniotic fluid abnormalities
DALLAS – Monthly ultrasound scans in the last trimester pick up just as many fetal growth and amniotic fluid problems as do scans done every 2 weeks, Suneet P. Chauhan, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“We found that about one in three of these high-risk pregnancies was complicated by an abnormality of fetal growth or amniotic fluid,” said Dr. Chauhan of the department of obstetrics, gynecology, and reproductive sciences at the University of Texas, Houston. “But more frequent scans did not increase the frequency of identifying these abnormalities. And since there are approximately 1.7 million such high-risk pregnancies each year, these findings have significant implications on personal, departmental, and societal levels.”
However, he added, the SUN trial, which randomized women to monthly or biweekly scans, wasn’t large enough to definitively determine the optimal timing of ultrasounds in this population. “We need larger trials to determine this.”
The trial results, published in the American Journal of Obstetrics & Gynecology, comprised 228 women with singleton pregnancies complicated by medical comorbidities, putting the fetus at risk of problems with growth or amniotic fluid volume. They were randomized to ultrasound scans every 2 weeks or every 4 weeks during the last trimester. The primary outcome was identification of four pregnancy complications: fetal growth restriction, large for gestational age, oligohydramnios, or polyhydramnios.
There were also secondary outcomes of composite maternal morbidity (chorioamnionitis, wound infection, transfusion, diabetic ketoacidosis, venous thromboembolism, ICU admission, and death) and neonatal morbidity (Apgar score of less than 5 at 5 minutes, umbilical artery pH less than 7, hyperbilirubinemia, intubation, high-grade intraventricular hemorrhage, necrotizing enterocolitis, and death).
Women were eligible for the study if they had autoimmune disease, a body mass index of 40 kg/m2 or higher, a history of delivering a small for gestational age or macrosomic infant, hypertensive disease, substance abuse, or sickle cell disease.
About half had multiple risk factors, the three most common being high body mass index, diabetes (either gestational or insulin-dependent), and hypertensive disease. Their gestational age at randomization was a mean of 23 weeks. The first scan was conducted at a mean of 29 weeks.
There were 28% more scans in the 2-week group than in the 4-week group (492 vs. 382). There were also more exams for potentially concerning findings, including more scans looking at growth (359 vs. 278), biophysical profiles (99 vs. 79), and umbilical artery Dopplers (34 vs. 27). Despite the increased scans and investigations, the primary outcome was detected at similar points (31.7 vs. 32.2 weeks).
A primary outcome finding was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different. There were no significant differences in the proportion of outcomes detected in each group, including fetal growth restriction (19% vs. 16%), large for gestational age (14% each group), oligohydramnios (4% each group) and polyhydramnios (9% each group).
Infants in each group were born at about the same time – 13.5 weeks after randomization. The mean gestational age in both groups was 37 weeks, with about 28.5% less than 37 weeks at birth. There were no significant differences in the rate of cesarean deliveries, or small or large for gestational age births.
The composite maternal morbidity outcome was similar in the 2-week and 4-week groups (26% vs. 22%). There were no significant differences in any of the individual components of the outcome. No mother died.
The composite neonatal outcome was also similar between the groups (14% vs. 12%). There were no significant differences in any of the individual components. No infant died.
The study was sponsored by the University of Texas Health Science Center, Houston. Dr. Chauhan had no financial disclosures.
SOURCE: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
DALLAS – Monthly ultrasound scans in the last trimester pick up just as many fetal growth and amniotic fluid problems as do scans done every 2 weeks, Suneet P. Chauhan, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“We found that about one in three of these high-risk pregnancies was complicated by an abnormality of fetal growth or amniotic fluid,” said Dr. Chauhan of the department of obstetrics, gynecology, and reproductive sciences at the University of Texas, Houston. “But more frequent scans did not increase the frequency of identifying these abnormalities. And since there are approximately 1.7 million such high-risk pregnancies each year, these findings have significant implications on personal, departmental, and societal levels.”
However, he added, the SUN trial, which randomized women to monthly or biweekly scans, wasn’t large enough to definitively determine the optimal timing of ultrasounds in this population. “We need larger trials to determine this.”
The trial results, published in the American Journal of Obstetrics & Gynecology, comprised 228 women with singleton pregnancies complicated by medical comorbidities, putting the fetus at risk of problems with growth or amniotic fluid volume. They were randomized to ultrasound scans every 2 weeks or every 4 weeks during the last trimester. The primary outcome was identification of four pregnancy complications: fetal growth restriction, large for gestational age, oligohydramnios, or polyhydramnios.
There were also secondary outcomes of composite maternal morbidity (chorioamnionitis, wound infection, transfusion, diabetic ketoacidosis, venous thromboembolism, ICU admission, and death) and neonatal morbidity (Apgar score of less than 5 at 5 minutes, umbilical artery pH less than 7, hyperbilirubinemia, intubation, high-grade intraventricular hemorrhage, necrotizing enterocolitis, and death).
Women were eligible for the study if they had autoimmune disease, a body mass index of 40 kg/m2 or higher, a history of delivering a small for gestational age or macrosomic infant, hypertensive disease, substance abuse, or sickle cell disease.
About half had multiple risk factors, the three most common being high body mass index, diabetes (either gestational or insulin-dependent), and hypertensive disease. Their gestational age at randomization was a mean of 23 weeks. The first scan was conducted at a mean of 29 weeks.
There were 28% more scans in the 2-week group than in the 4-week group (492 vs. 382). There were also more exams for potentially concerning findings, including more scans looking at growth (359 vs. 278), biophysical profiles (99 vs. 79), and umbilical artery Dopplers (34 vs. 27). Despite the increased scans and investigations, the primary outcome was detected at similar points (31.7 vs. 32.2 weeks).
A primary outcome finding was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different. There were no significant differences in the proportion of outcomes detected in each group, including fetal growth restriction (19% vs. 16%), large for gestational age (14% each group), oligohydramnios (4% each group) and polyhydramnios (9% each group).
Infants in each group were born at about the same time – 13.5 weeks after randomization. The mean gestational age in both groups was 37 weeks, with about 28.5% less than 37 weeks at birth. There were no significant differences in the rate of cesarean deliveries, or small or large for gestational age births.
The composite maternal morbidity outcome was similar in the 2-week and 4-week groups (26% vs. 22%). There were no significant differences in any of the individual components of the outcome. No mother died.
The composite neonatal outcome was also similar between the groups (14% vs. 12%). There were no significant differences in any of the individual components. No infant died.
The study was sponsored by the University of Texas Health Science Center, Houston. Dr. Chauhan had no financial disclosures.
SOURCE: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
DALLAS – Monthly ultrasound scans in the last trimester pick up just as many fetal growth and amniotic fluid problems as do scans done every 2 weeks, Suneet P. Chauhan, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“We found that about one in three of these high-risk pregnancies was complicated by an abnormality of fetal growth or amniotic fluid,” said Dr. Chauhan of the department of obstetrics, gynecology, and reproductive sciences at the University of Texas, Houston. “But more frequent scans did not increase the frequency of identifying these abnormalities. And since there are approximately 1.7 million such high-risk pregnancies each year, these findings have significant implications on personal, departmental, and societal levels.”
However, he added, the SUN trial, which randomized women to monthly or biweekly scans, wasn’t large enough to definitively determine the optimal timing of ultrasounds in this population. “We need larger trials to determine this.”
The trial results, published in the American Journal of Obstetrics & Gynecology, comprised 228 women with singleton pregnancies complicated by medical comorbidities, putting the fetus at risk of problems with growth or amniotic fluid volume. They were randomized to ultrasound scans every 2 weeks or every 4 weeks during the last trimester. The primary outcome was identification of four pregnancy complications: fetal growth restriction, large for gestational age, oligohydramnios, or polyhydramnios.
There were also secondary outcomes of composite maternal morbidity (chorioamnionitis, wound infection, transfusion, diabetic ketoacidosis, venous thromboembolism, ICU admission, and death) and neonatal morbidity (Apgar score of less than 5 at 5 minutes, umbilical artery pH less than 7, hyperbilirubinemia, intubation, high-grade intraventricular hemorrhage, necrotizing enterocolitis, and death).
Women were eligible for the study if they had autoimmune disease, a body mass index of 40 kg/m2 or higher, a history of delivering a small for gestational age or macrosomic infant, hypertensive disease, substance abuse, or sickle cell disease.
About half had multiple risk factors, the three most common being high body mass index, diabetes (either gestational or insulin-dependent), and hypertensive disease. Their gestational age at randomization was a mean of 23 weeks. The first scan was conducted at a mean of 29 weeks.
There were 28% more scans in the 2-week group than in the 4-week group (492 vs. 382). There were also more exams for potentially concerning findings, including more scans looking at growth (359 vs. 278), biophysical profiles (99 vs. 79), and umbilical artery Dopplers (34 vs. 27). Despite the increased scans and investigations, the primary outcome was detected at similar points (31.7 vs. 32.2 weeks).
A primary outcome finding was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different. There were no significant differences in the proportion of outcomes detected in each group, including fetal growth restriction (19% vs. 16%), large for gestational age (14% each group), oligohydramnios (4% each group) and polyhydramnios (9% each group).
Infants in each group were born at about the same time – 13.5 weeks after randomization. The mean gestational age in both groups was 37 weeks, with about 28.5% less than 37 weeks at birth. There were no significant differences in the rate of cesarean deliveries, or small or large for gestational age births.
The composite maternal morbidity outcome was similar in the 2-week and 4-week groups (26% vs. 22%). There were no significant differences in any of the individual components of the outcome. No mother died.
The composite neonatal outcome was also similar between the groups (14% vs. 12%). There were no significant differences in any of the individual components. No infant died.
The study was sponsored by the University of Texas Health Science Center, Houston. Dr. Chauhan had no financial disclosures.
SOURCE: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Ultrasound scans every 4 weeks identify just as many fetal growth of amniotic fluid problems as more frequent scans.
Major finding: A fetal or fluid abnormality was detected in 38% of the 2-week group and 32% of the 4-week group – not significantly different.
Study details: The randomized prospective trial comprised 228 women.
Disclosures: The University of Texas Medical Center, Houston, sponsored the study. Dr. Chauhan had no financial disclosures.
Source: Roberts RP et al. Am J Obstet Gynecol. 2018;218:S3.
TRAAP trial looks at tranexamic acid to prevent postpartum hemorrhage after vaginal delivery
DALLAS – An intravenous drug administered to women along with oxytocin after vaginal delivery did not reduce the risk of a large-volume hemorrhage, but it did significantly affect some other markers of postpartum blood loss.
The TRAAP trial failed to achieve its primary endpoint – reduction of postpartum hemorrhage of at least 500 ml, Loïc Sentilhes, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. But tranexamic acid’s success in the prespecified secondary endpoints suggests there still may be a place for the drug in obstetrics, said Dr. Sentilhes of the University Hospital of Bordeaux, France.
TRAAP randomized 4,079 women in labor for a planned vaginal birth to either 1 g of tranexamic acid or placebo. The interventions were added to existing IV fluids within 2 minutes after vaginal birth, after the women had also received routine oxytocin.
The study’s primary outcome was the incidence of postpartum hemorrhage, defined as a blood loss of 500 ml or more. There were a number of prespecified secondary outcomes, including clinically significant blood loss, need for additional uterotonics, severe hemorrhage (more than 1,000 mL), estimated total blood loss, transfusion, and changes in hemoglobin and hematocrit.
The study also looked at these outcomes in prespecified subgroups: women who had an episiotomy, who had an operative delivery, and who had a history of prior postpartum hemorrhage.
Women in the study were a mean age of 30 years; about half were primiparous, and 5% were attempting a vaginal birth after cesarean section. Of the women, 4% had experienced a prior postpartum hemorrhage. Labor was induced in 20%, and about 60% needed labor augmentation.
An operative vaginal delivery was necessary for 17%. Forms of assistance included forceps (55%) and vacuum extraction (45%). About a quarter had an episiotomy, and 8% had a macrosomic neonate of more than 4,000 g.
The primary endpoint of at least 500 ml blood loss occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Of the secondary endpoints, only two – clinically significant bleeding and need for additional uterotonics – were significantly better in the tranexamic acid group. The drug reduced the risk of clinically significant bleeding by 26% (RR, 0.74; P = .004) and the need for additional uterotonics by 25% (RR, 0.75; P = .006).
While the primary endpoint was not realized in the overall patient group, tranexamic acid achieved barely significant risk reductions of 34% in the risk of hemorrhage among women who had an operative delivery (RR, 0.66; P = .0498) and 27% among those who had an episiotomy (RR, 0.73; P = .049).
It was no better than placebo in women with a history of postpartum hemorrhage.
Those who received the drug were twice as likely to experience nausea and vomiting after delivery as did those who received placebo. But tranexamic acid exerted no lingering prothrombotic effects at 3 months after delivery, with no signals in deep vein thrombosis, no pulmonary embolism, and no clots in the ovarian or superficial veins.
The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
SOURCE: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
DALLAS – An intravenous drug administered to women along with oxytocin after vaginal delivery did not reduce the risk of a large-volume hemorrhage, but it did significantly affect some other markers of postpartum blood loss.
The TRAAP trial failed to achieve its primary endpoint – reduction of postpartum hemorrhage of at least 500 ml, Loïc Sentilhes, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. But tranexamic acid’s success in the prespecified secondary endpoints suggests there still may be a place for the drug in obstetrics, said Dr. Sentilhes of the University Hospital of Bordeaux, France.
TRAAP randomized 4,079 women in labor for a planned vaginal birth to either 1 g of tranexamic acid or placebo. The interventions were added to existing IV fluids within 2 minutes after vaginal birth, after the women had also received routine oxytocin.
The study’s primary outcome was the incidence of postpartum hemorrhage, defined as a blood loss of 500 ml or more. There were a number of prespecified secondary outcomes, including clinically significant blood loss, need for additional uterotonics, severe hemorrhage (more than 1,000 mL), estimated total blood loss, transfusion, and changes in hemoglobin and hematocrit.
The study also looked at these outcomes in prespecified subgroups: women who had an episiotomy, who had an operative delivery, and who had a history of prior postpartum hemorrhage.
Women in the study were a mean age of 30 years; about half were primiparous, and 5% were attempting a vaginal birth after cesarean section. Of the women, 4% had experienced a prior postpartum hemorrhage. Labor was induced in 20%, and about 60% needed labor augmentation.
An operative vaginal delivery was necessary for 17%. Forms of assistance included forceps (55%) and vacuum extraction (45%). About a quarter had an episiotomy, and 8% had a macrosomic neonate of more than 4,000 g.
The primary endpoint of at least 500 ml blood loss occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Of the secondary endpoints, only two – clinically significant bleeding and need for additional uterotonics – were significantly better in the tranexamic acid group. The drug reduced the risk of clinically significant bleeding by 26% (RR, 0.74; P = .004) and the need for additional uterotonics by 25% (RR, 0.75; P = .006).
While the primary endpoint was not realized in the overall patient group, tranexamic acid achieved barely significant risk reductions of 34% in the risk of hemorrhage among women who had an operative delivery (RR, 0.66; P = .0498) and 27% among those who had an episiotomy (RR, 0.73; P = .049).
It was no better than placebo in women with a history of postpartum hemorrhage.
Those who received the drug were twice as likely to experience nausea and vomiting after delivery as did those who received placebo. But tranexamic acid exerted no lingering prothrombotic effects at 3 months after delivery, with no signals in deep vein thrombosis, no pulmonary embolism, and no clots in the ovarian or superficial veins.
The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
SOURCE: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
DALLAS – An intravenous drug administered to women along with oxytocin after vaginal delivery did not reduce the risk of a large-volume hemorrhage, but it did significantly affect some other markers of postpartum blood loss.
The TRAAP trial failed to achieve its primary endpoint – reduction of postpartum hemorrhage of at least 500 ml, Loïc Sentilhes, MD, reported at the meeting sponsored by the Society for Maternal-Fetal Medicine. But tranexamic acid’s success in the prespecified secondary endpoints suggests there still may be a place for the drug in obstetrics, said Dr. Sentilhes of the University Hospital of Bordeaux, France.
TRAAP randomized 4,079 women in labor for a planned vaginal birth to either 1 g of tranexamic acid or placebo. The interventions were added to existing IV fluids within 2 minutes after vaginal birth, after the women had also received routine oxytocin.
The study’s primary outcome was the incidence of postpartum hemorrhage, defined as a blood loss of 500 ml or more. There were a number of prespecified secondary outcomes, including clinically significant blood loss, need for additional uterotonics, severe hemorrhage (more than 1,000 mL), estimated total blood loss, transfusion, and changes in hemoglobin and hematocrit.
The study also looked at these outcomes in prespecified subgroups: women who had an episiotomy, who had an operative delivery, and who had a history of prior postpartum hemorrhage.
Women in the study were a mean age of 30 years; about half were primiparous, and 5% were attempting a vaginal birth after cesarean section. Of the women, 4% had experienced a prior postpartum hemorrhage. Labor was induced in 20%, and about 60% needed labor augmentation.
An operative vaginal delivery was necessary for 17%. Forms of assistance included forceps (55%) and vacuum extraction (45%). About a quarter had an episiotomy, and 8% had a macrosomic neonate of more than 4,000 g.
The primary endpoint of at least 500 ml blood loss occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Of the secondary endpoints, only two – clinically significant bleeding and need for additional uterotonics – were significantly better in the tranexamic acid group. The drug reduced the risk of clinically significant bleeding by 26% (RR, 0.74; P = .004) and the need for additional uterotonics by 25% (RR, 0.75; P = .006).
While the primary endpoint was not realized in the overall patient group, tranexamic acid achieved barely significant risk reductions of 34% in the risk of hemorrhage among women who had an operative delivery (RR, 0.66; P = .0498) and 27% among those who had an episiotomy (RR, 0.73; P = .049).
It was no better than placebo in women with a history of postpartum hemorrhage.
Those who received the drug were twice as likely to experience nausea and vomiting after delivery as did those who received placebo. But tranexamic acid exerted no lingering prothrombotic effects at 3 months after delivery, with no signals in deep vein thrombosis, no pulmonary embolism, and no clots in the ovarian or superficial veins.
The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
SOURCE: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.
REPORTING FROM THE PREGNANCY MEETING
Key clinical point: Tranexamic acid didn’t significantly reduce the risk of a postpartum hemorrhage of 500 ml or more.
Major finding: Hemorrhage occurred in 8.1% of the active group and 9.8% of the placebo group – a nonsignificant difference (relative risk, 0.83; P = .07).
Study details: The randomized, placebo-controlled study comprised 4,079 women.
Disclosures: The TRAAP trial was funded by the French Ministry of Health under its clinical research hospital program. Dr. Sentilhes had no financial disclosures.
Source: Sentilhes L et al. Am J Obstet Gynecol. 2018;218:S1.