User login
So-called “skip metastasis” of lung cancer to the lymph nodes – when the cancer “skips” over the N1 bronchopulmonary or hilar stage to N2 ipsilateral mediastinal metastasis – may be associated with distinct histological characteristics that can further help understand its association with longer survival and better prognosis in advanced resectable lung adenocarcinoma, according to a small study from China.
Researchers at Fudan (Shanghai ) University Cancer Center published their findings online ahead of print for the October issue of the Journal of Thoracic and Cardiovascular Surgery (2015 July 6 [doi: 10.1016/j.jtcvs.2015.03.067]). In all, they enrolled 177 patients with N2 adenocarcinoma, 45 (25.4%) of whom had skip N2 metastasis.
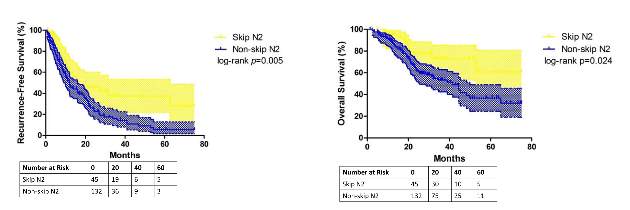
They reported that patients with skip metastasis had considerably better 5-year recurrence-free survival rates of 37.4% vs. 5.7% and better overall survival rates of 60.7% vs. 32.1% when compared with those with non-skip involvement.
“There are distinct differences in clinicopathological features and prognosis in patients with or without skip N2 metastasis,” Dr. Haiquan Chen and his colleagues said. “Considering the results of our study, subclassifications of mediastinal lymph nodes metastases would have potential clinical significance for patients with lung adenocarcinoma.”
Dr. Chen and his colleagues sought to identify specific histological features that characterized the association between skip N2 metastasis and adenocarcinoma subtypes and prognosis. “Skip N2 patients have more cases that are acinar adenocarcinoma subtype, well differentiated and located in the right lung than [do] non-skip patients,” they said.
In fact, they found the predictive value of skip N2 was more significant in patients with right-lung disease, with 5-year recurrence-free survival of 36.6% vs. 0% and overall survival of 57.2% vs. 28% in non–right-lung lesions. They also reported that tumor size of 3 cm or smaller in skip N2 was associated with significantly improved survival rates – 43% vs. 6.7% recurrence-free survival and 74.6% vs. 27.6% for overall survival, compared with patients with larger tumors.
The skip N2 lung adenocarcinoma patients had “remarkably lower incidence” of vascular invasion of the lymph nodes, Dr. Chen and his coauthors wrote. Skip N2 patients also had lower, but not statistically significant, rates of pleural invasion. The Fudan University researchers also reported that the incidence of non-skip N2 metastasis was “significantly high” in patients with papillary-predominant subtype.
“Considering our results, skip N2 should not be recognized as [a] predictor for better survival in all lung adenocarcinoma cases, but in [a] more specific group of patients,” Dr. Chen and his coauthors said.
A multivariate analysis confirmed the predictive significance of skip N2 for recurrence-free survival, but not so much for overall survival. Single N2 metastasis was also an independent predictor for better recurrence-free and overall survival, Dr. Chen and his colleagues said.
The study received funding from the Key Construction Program of the National “985” Project, Ministry of Science and Technology of China; the National Natural Science Foundation of China; the Science and Technology Commission of Shanghai Municipality; and Shanghai Hospital Development Center.
The authors had no disclosures.
“Perhaps the most interesting aspect of the study by Chen and colleagues is the novel observation that skip metastases seem to correlate with acinar histological subtype of lung adenocarcinoma,” Dr. Valerie Rusch of Memorial Sloan Kettering Cancer Center, New York, said in her invited commentary (J Thorac Cardiovasc Surg. 2015 May 8 [doi: 10.1016/j.jtcvs.2015.04.051]) .
“This nicely performed study adds to the evidence that [non–small cell lung cancer) with skip metastases are a distinct subset of stage IIIa disease,” she said.
Dr. Rusch noted that when the International Association for the Study of Lung Cancer (IASLC) revised its lung cancer staging system in 2007 (J Thorac Oncol. 2007;2:603-12), a report for which she served as lead author, it considered giving non–small cell lung cancer with skip metastases its own category. However, the authors decided not to do so because of the small numbers of patients who fall into the category.
In the updated histological classification for adenocarcinoma in 2011 from IASLC, along with the American Thoracic Society and European Respiratory Society (J Thorac Oncol. 2011;6[2]:244-85) , papillary and acinar-predominant adenocarcinomas appear to be associated with similar outcomes. However, the Fudan (Shanghai) University researchers suggest “that there may be some important differences between the two subtypes,” Dr. Rusch said.
Because the study population was so small, the results cannot be considered “definitive,” Dr. Rusch said. “In this era of increasingly high throughput molecular medicine, future, much larger-scale analyses are needed to prove or refute these initial results.”
“Perhaps the most interesting aspect of the study by Chen and colleagues is the novel observation that skip metastases seem to correlate with acinar histological subtype of lung adenocarcinoma,” Dr. Valerie Rusch of Memorial Sloan Kettering Cancer Center, New York, said in her invited commentary (J Thorac Cardiovasc Surg. 2015 May 8 [doi: 10.1016/j.jtcvs.2015.04.051]) .
“This nicely performed study adds to the evidence that [non–small cell lung cancer) with skip metastases are a distinct subset of stage IIIa disease,” she said.
Dr. Rusch noted that when the International Association for the Study of Lung Cancer (IASLC) revised its lung cancer staging system in 2007 (J Thorac Oncol. 2007;2:603-12), a report for which she served as lead author, it considered giving non–small cell lung cancer with skip metastases its own category. However, the authors decided not to do so because of the small numbers of patients who fall into the category.
In the updated histological classification for adenocarcinoma in 2011 from IASLC, along with the American Thoracic Society and European Respiratory Society (J Thorac Oncol. 2011;6[2]:244-85) , papillary and acinar-predominant adenocarcinomas appear to be associated with similar outcomes. However, the Fudan (Shanghai) University researchers suggest “that there may be some important differences between the two subtypes,” Dr. Rusch said.
Because the study population was so small, the results cannot be considered “definitive,” Dr. Rusch said. “In this era of increasingly high throughput molecular medicine, future, much larger-scale analyses are needed to prove or refute these initial results.”
“Perhaps the most interesting aspect of the study by Chen and colleagues is the novel observation that skip metastases seem to correlate with acinar histological subtype of lung adenocarcinoma,” Dr. Valerie Rusch of Memorial Sloan Kettering Cancer Center, New York, said in her invited commentary (J Thorac Cardiovasc Surg. 2015 May 8 [doi: 10.1016/j.jtcvs.2015.04.051]) .
“This nicely performed study adds to the evidence that [non–small cell lung cancer) with skip metastases are a distinct subset of stage IIIa disease,” she said.
Dr. Rusch noted that when the International Association for the Study of Lung Cancer (IASLC) revised its lung cancer staging system in 2007 (J Thorac Oncol. 2007;2:603-12), a report for which she served as lead author, it considered giving non–small cell lung cancer with skip metastases its own category. However, the authors decided not to do so because of the small numbers of patients who fall into the category.
In the updated histological classification for adenocarcinoma in 2011 from IASLC, along with the American Thoracic Society and European Respiratory Society (J Thorac Oncol. 2011;6[2]:244-85) , papillary and acinar-predominant adenocarcinomas appear to be associated with similar outcomes. However, the Fudan (Shanghai) University researchers suggest “that there may be some important differences between the two subtypes,” Dr. Rusch said.
Because the study population was so small, the results cannot be considered “definitive,” Dr. Rusch said. “In this era of increasingly high throughput molecular medicine, future, much larger-scale analyses are needed to prove or refute these initial results.”
So-called “skip metastasis” of lung cancer to the lymph nodes – when the cancer “skips” over the N1 bronchopulmonary or hilar stage to N2 ipsilateral mediastinal metastasis – may be associated with distinct histological characteristics that can further help understand its association with longer survival and better prognosis in advanced resectable lung adenocarcinoma, according to a small study from China.
Researchers at Fudan (Shanghai ) University Cancer Center published their findings online ahead of print for the October issue of the Journal of Thoracic and Cardiovascular Surgery (2015 July 6 [doi: 10.1016/j.jtcvs.2015.03.067]). In all, they enrolled 177 patients with N2 adenocarcinoma, 45 (25.4%) of whom had skip N2 metastasis.
They reported that patients with skip metastasis had considerably better 5-year recurrence-free survival rates of 37.4% vs. 5.7% and better overall survival rates of 60.7% vs. 32.1% when compared with those with non-skip involvement.
“There are distinct differences in clinicopathological features and prognosis in patients with or without skip N2 metastasis,” Dr. Haiquan Chen and his colleagues said. “Considering the results of our study, subclassifications of mediastinal lymph nodes metastases would have potential clinical significance for patients with lung adenocarcinoma.”
Dr. Chen and his colleagues sought to identify specific histological features that characterized the association between skip N2 metastasis and adenocarcinoma subtypes and prognosis. “Skip N2 patients have more cases that are acinar adenocarcinoma subtype, well differentiated and located in the right lung than [do] non-skip patients,” they said.
In fact, they found the predictive value of skip N2 was more significant in patients with right-lung disease, with 5-year recurrence-free survival of 36.6% vs. 0% and overall survival of 57.2% vs. 28% in non–right-lung lesions. They also reported that tumor size of 3 cm or smaller in skip N2 was associated with significantly improved survival rates – 43% vs. 6.7% recurrence-free survival and 74.6% vs. 27.6% for overall survival, compared with patients with larger tumors.
The skip N2 lung adenocarcinoma patients had “remarkably lower incidence” of vascular invasion of the lymph nodes, Dr. Chen and his coauthors wrote. Skip N2 patients also had lower, but not statistically significant, rates of pleural invasion. The Fudan University researchers also reported that the incidence of non-skip N2 metastasis was “significantly high” in patients with papillary-predominant subtype.
“Considering our results, skip N2 should not be recognized as [a] predictor for better survival in all lung adenocarcinoma cases, but in [a] more specific group of patients,” Dr. Chen and his coauthors said.
A multivariate analysis confirmed the predictive significance of skip N2 for recurrence-free survival, but not so much for overall survival. Single N2 metastasis was also an independent predictor for better recurrence-free and overall survival, Dr. Chen and his colleagues said.
The study received funding from the Key Construction Program of the National “985” Project, Ministry of Science and Technology of China; the National Natural Science Foundation of China; the Science and Technology Commission of Shanghai Municipality; and Shanghai Hospital Development Center.
The authors had no disclosures.
So-called “skip metastasis” of lung cancer to the lymph nodes – when the cancer “skips” over the N1 bronchopulmonary or hilar stage to N2 ipsilateral mediastinal metastasis – may be associated with distinct histological characteristics that can further help understand its association with longer survival and better prognosis in advanced resectable lung adenocarcinoma, according to a small study from China.
Researchers at Fudan (Shanghai ) University Cancer Center published their findings online ahead of print for the October issue of the Journal of Thoracic and Cardiovascular Surgery (2015 July 6 [doi: 10.1016/j.jtcvs.2015.03.067]). In all, they enrolled 177 patients with N2 adenocarcinoma, 45 (25.4%) of whom had skip N2 metastasis.
They reported that patients with skip metastasis had considerably better 5-year recurrence-free survival rates of 37.4% vs. 5.7% and better overall survival rates of 60.7% vs. 32.1% when compared with those with non-skip involvement.
“There are distinct differences in clinicopathological features and prognosis in patients with or without skip N2 metastasis,” Dr. Haiquan Chen and his colleagues said. “Considering the results of our study, subclassifications of mediastinal lymph nodes metastases would have potential clinical significance for patients with lung adenocarcinoma.”
Dr. Chen and his colleagues sought to identify specific histological features that characterized the association between skip N2 metastasis and adenocarcinoma subtypes and prognosis. “Skip N2 patients have more cases that are acinar adenocarcinoma subtype, well differentiated and located in the right lung than [do] non-skip patients,” they said.
In fact, they found the predictive value of skip N2 was more significant in patients with right-lung disease, with 5-year recurrence-free survival of 36.6% vs. 0% and overall survival of 57.2% vs. 28% in non–right-lung lesions. They also reported that tumor size of 3 cm or smaller in skip N2 was associated with significantly improved survival rates – 43% vs. 6.7% recurrence-free survival and 74.6% vs. 27.6% for overall survival, compared with patients with larger tumors.
The skip N2 lung adenocarcinoma patients had “remarkably lower incidence” of vascular invasion of the lymph nodes, Dr. Chen and his coauthors wrote. Skip N2 patients also had lower, but not statistically significant, rates of pleural invasion. The Fudan University researchers also reported that the incidence of non-skip N2 metastasis was “significantly high” in patients with papillary-predominant subtype.
“Considering our results, skip N2 should not be recognized as [a] predictor for better survival in all lung adenocarcinoma cases, but in [a] more specific group of patients,” Dr. Chen and his coauthors said.
A multivariate analysis confirmed the predictive significance of skip N2 for recurrence-free survival, but not so much for overall survival. Single N2 metastasis was also an independent predictor for better recurrence-free and overall survival, Dr. Chen and his colleagues said.
The study received funding from the Key Construction Program of the National “985” Project, Ministry of Science and Technology of China; the National Natural Science Foundation of China; the Science and Technology Commission of Shanghai Municipality; and Shanghai Hospital Development Center.
The authors had no disclosures.
Key clinical point: Skip N2 metastases in resectable lung cancer have distinct histological characteristics from non-skip N2 disease.
Major finding: A subset of patients with skip N2 metastasis had higher rates of acinar adenocarcinoma subtype and right-lung disease.
Data source: Retrospective analysis of 177 patients with lung adenocarcinoma and N2 metastasis
Disclosures: The study received funding from the government of China and Shanghai Municipality as well as Shanghai Hospital Development Center. The authors have no relationships to disclose.