User login
The architecture of the glenohumeral joint makes it the most common large joint to become dislocated, accounting for approximately 45% of all dislocations. Anterior dislocation constitutes more than 95% of glenohumeral joint dislocations; posterior dislocation, only 2% to 5%.1,2
For the family physician, determining appropriate follow-up after emergent reduction depends on several distinct variables, which we review here; subsequent treatment might involve, as we outline, physical therapy, immobilization, surgical intervention, or a combination of several modalities. Treatment decisions can make the difference between successful rehabilitation and potential disability, particularly in typically young and active patients.
Numerous mechanisms of injury
Anterior shoulder dislocations typically occur with the affected shoulder in a position of abduction and external rotation; 90% of patients are 21 to 30 years of age, and men are affected 3 times more often than women.2 Unsurprisingly, athletes are affected most frequently, with the common sports-related mechanism of injury being either sudden pressure exerted on the abducted and externally rotated arm or a fall onto an outstretched hand with the arm elevated. Repetitive microtrauma from such sports as swimming, baseball, and volleyball can also lead to instability.
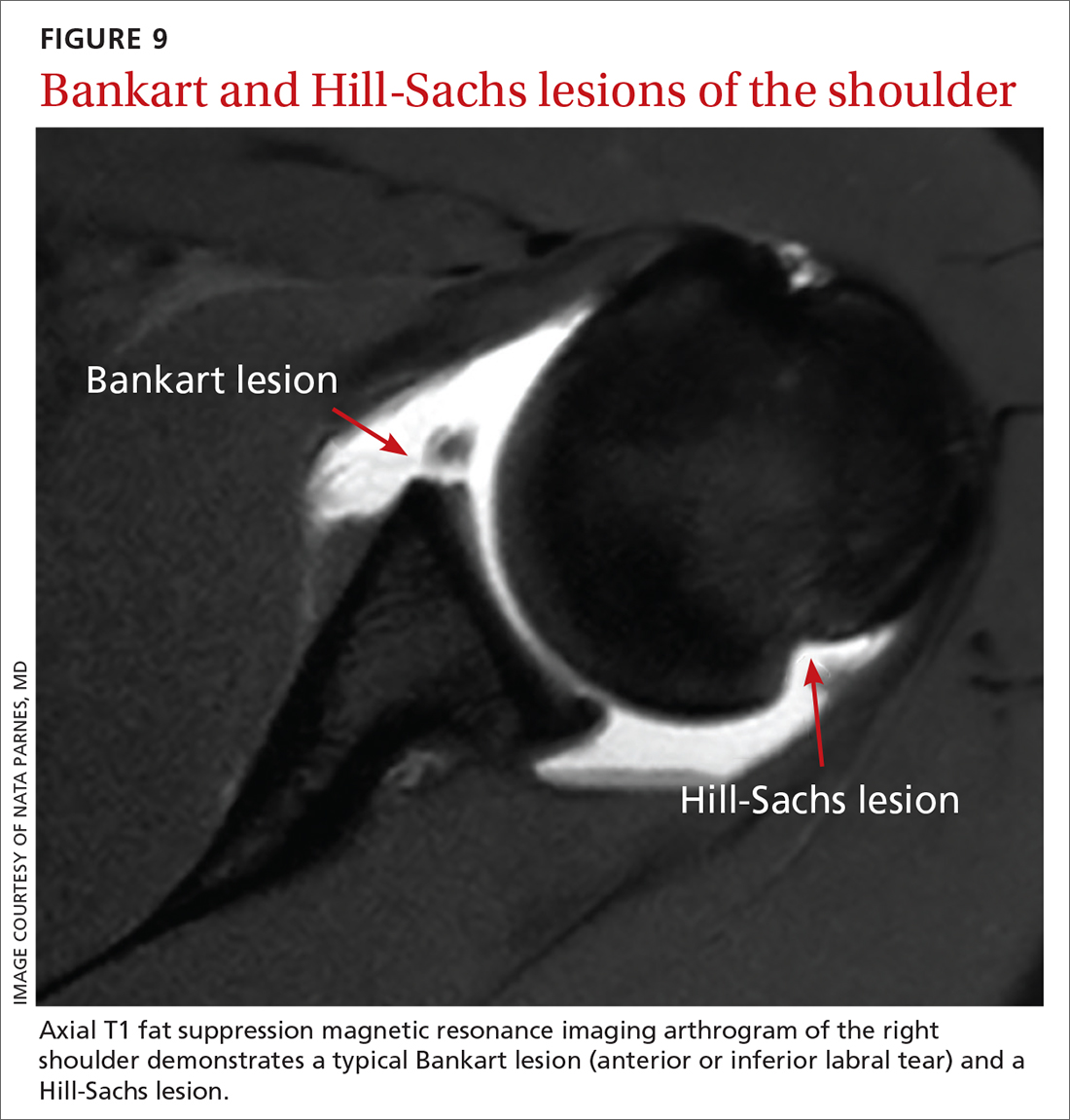
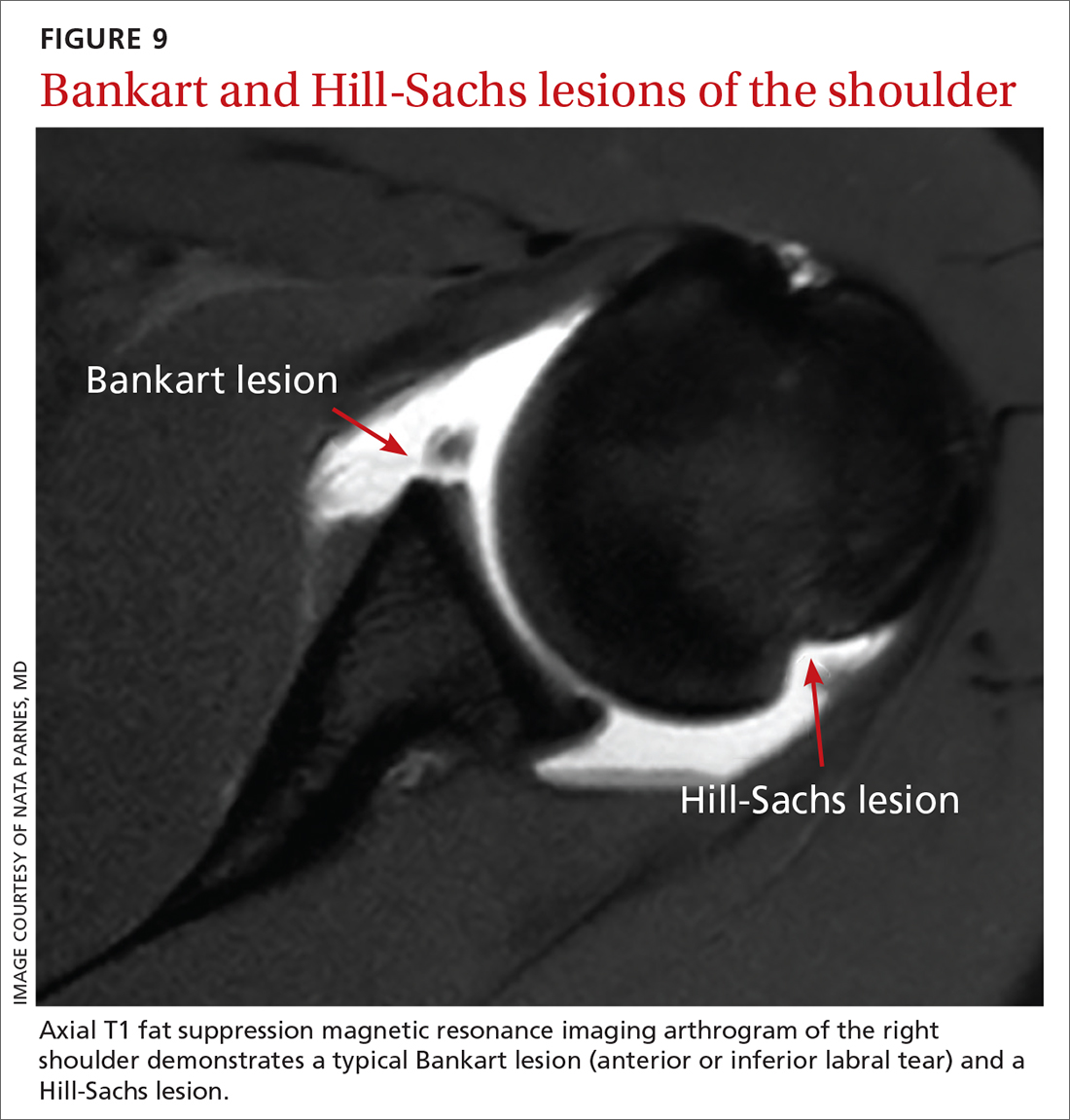
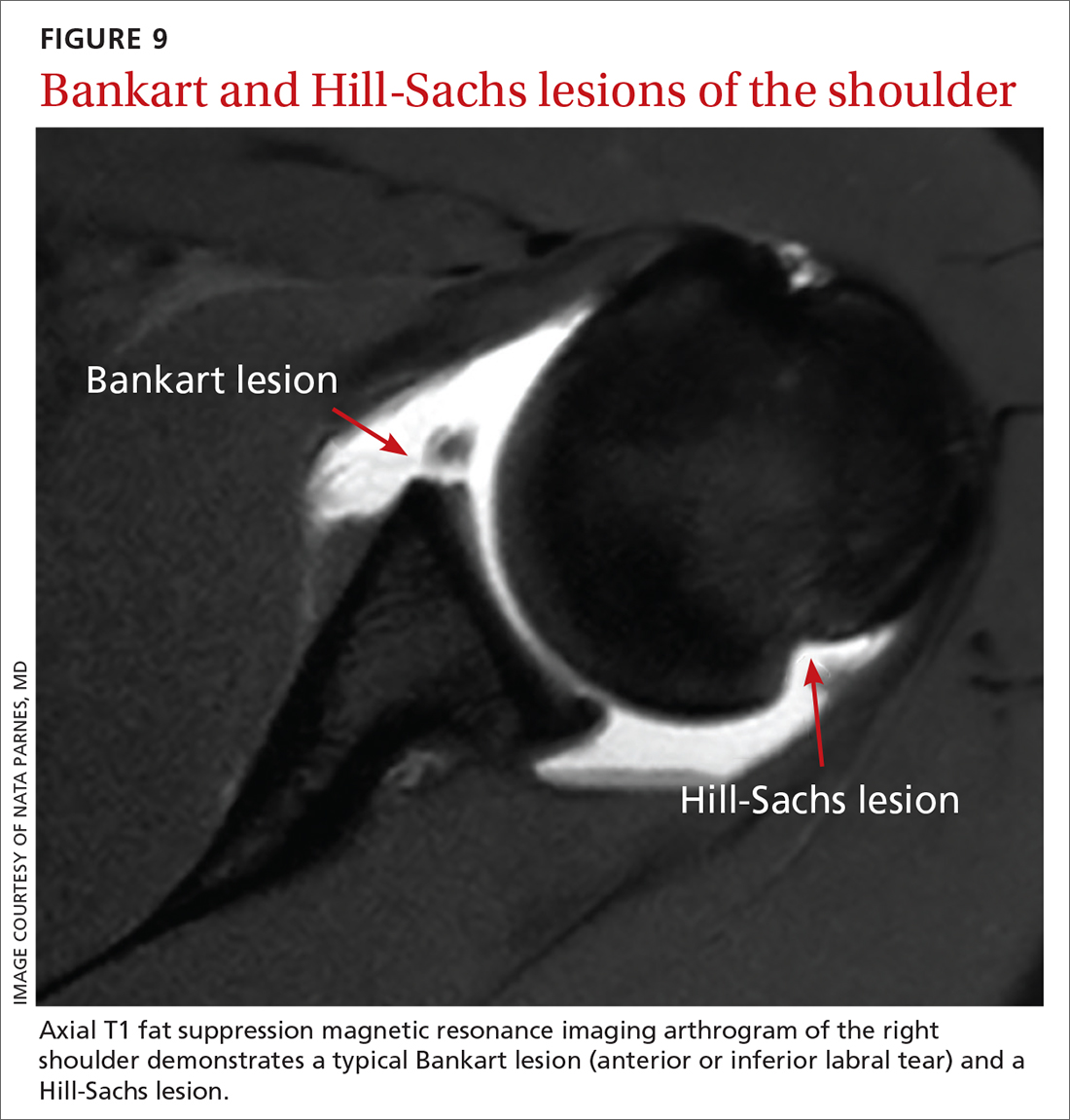
Bankart lesion. This tear of the anterior or inferior section of the labrum is the most characteristic lesion noted in anterior dislocations, found in 73% of first-time dislocations and 100% of recurrent dislocations.3,4
Hills-Sachs lesion is often associated with a Bankart lesion. The Hills-Sachs lesion is an impaction fracture of the posterolateral aspect of the humeral head resulting from its displacement over the anterior lip of the glenoid. Hill-Sachs lesions are seen in 71% of first-time and recurrent dislocations.3
Less common concomitant injuries during anterior shoulder dislocation include rupture of the rotator-cuff tendons (particularly in patients older than 40 years), glenoid and proximal humerus fractures, a tear of the superior labrum (known as a “SLAP lesion”), cartilage injury, and neurovascular injury.
Posterior instability typically occurs as a result of a strong muscle contraction, as seen in electrocution or seizure; however, it can be caused by athletic trauma, particularly in football.5 Repetitive forces exerted on the forward-flexed and internally rotated shoulder position during blocking puts football players at increased risk of posterior instability.5
Continue to: Multidirectional instability
Multidirectional instability is more frequently attributable to congenital hyperlaxity of the glenohumeral joint capsule, rather than to acute injury. However, athletes can also develop capsular laxity from repetitive microtrauma to the shoulder.5
Emergent reduction: Prompt action needed
Acute dislocation of the shoulder should be reduced as soon as possible to minimize neurovascular injury and patient discomfort. (Typically, but not always, this is done in the emergency department.) It is crucial to have effective muscle relaxation before any attempt at reduction, to minimize the risk of iatrogenic injury to bone, cartilage, tendons, and neurovascular structures.
Muscle relaxation can be facilitated with intravenous midazolam or other agents, as specified by institutional protocol. Intra-articular lidocaine injection or intravenous fentanyl is often utilized in conjunction with the sedating agent to reduce pain and further accommodate relaxation.
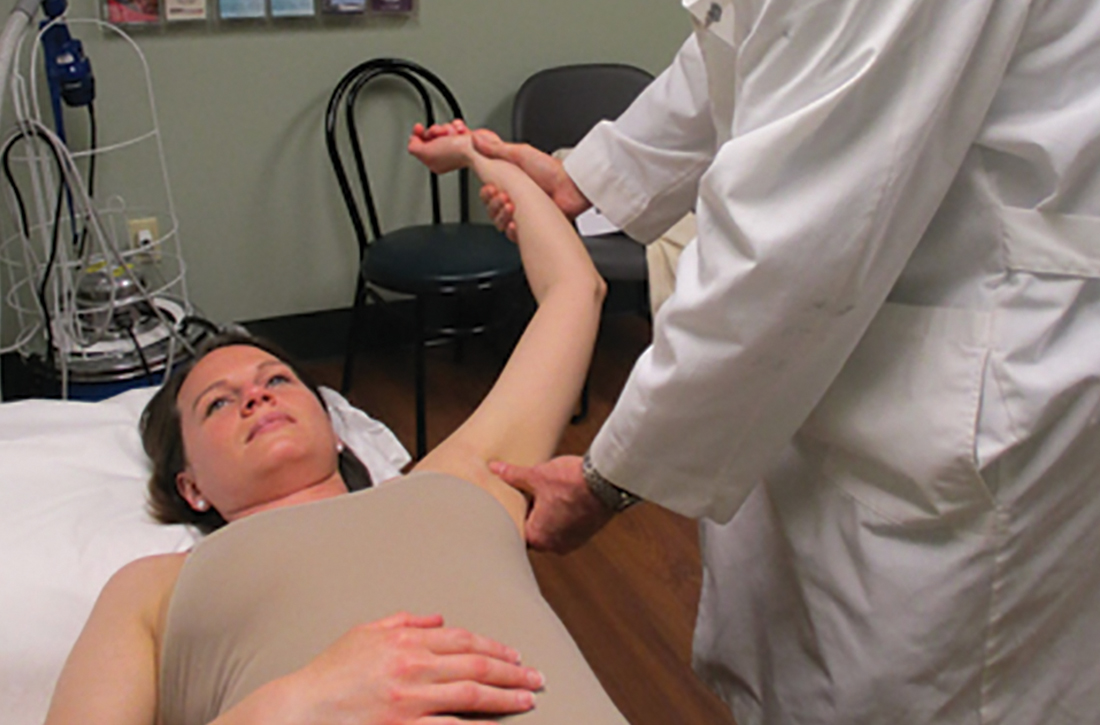
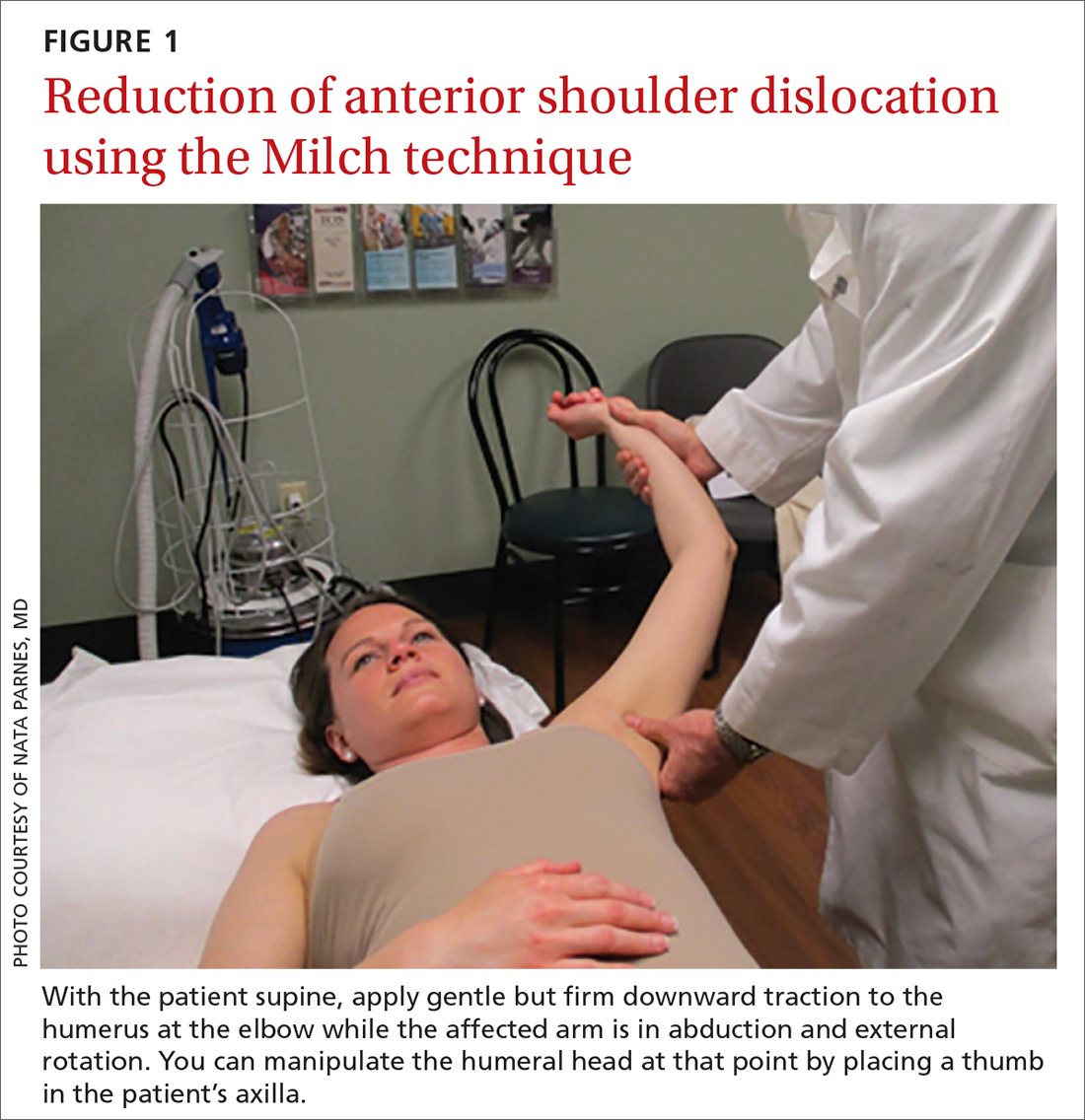
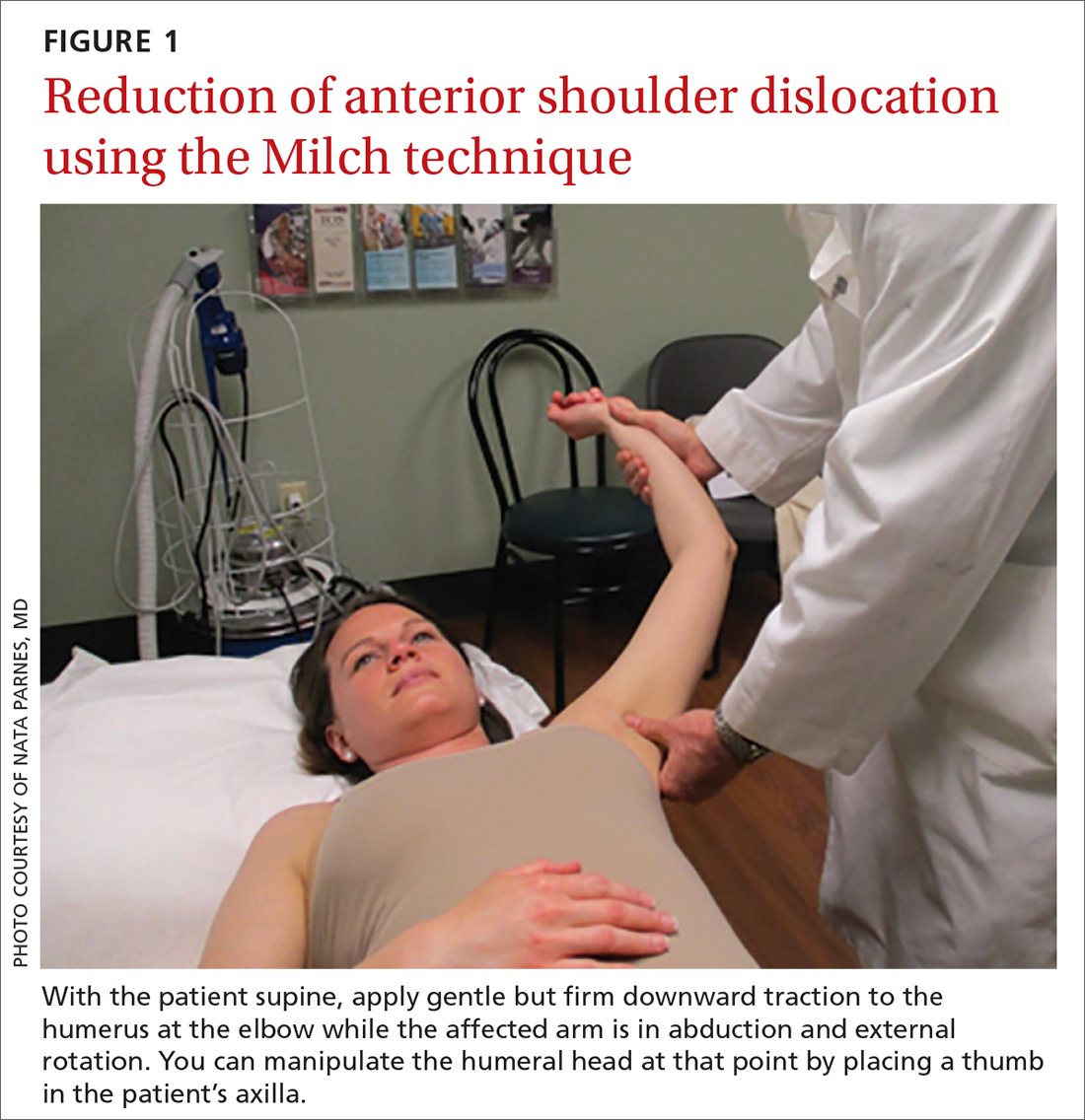
Anterior reduction. Any one of several techniques can be used to perform emergent reduction of anterior shoulder dislocations, all of which have demonstrated success. The Milch technique is among the least traumatic for effective reduction.6 In this technique (FIGURE 1), the patient is supine; gentle but firm downward traction is applied to the humerus at the elbow of the affected arm while the arm is in abduction and external rotation. The provider can manipulate the humeral head at that point by placing a thumb in the patient’s axilla; the arm can also be further internally rotated and adducted until reduction is achieved.
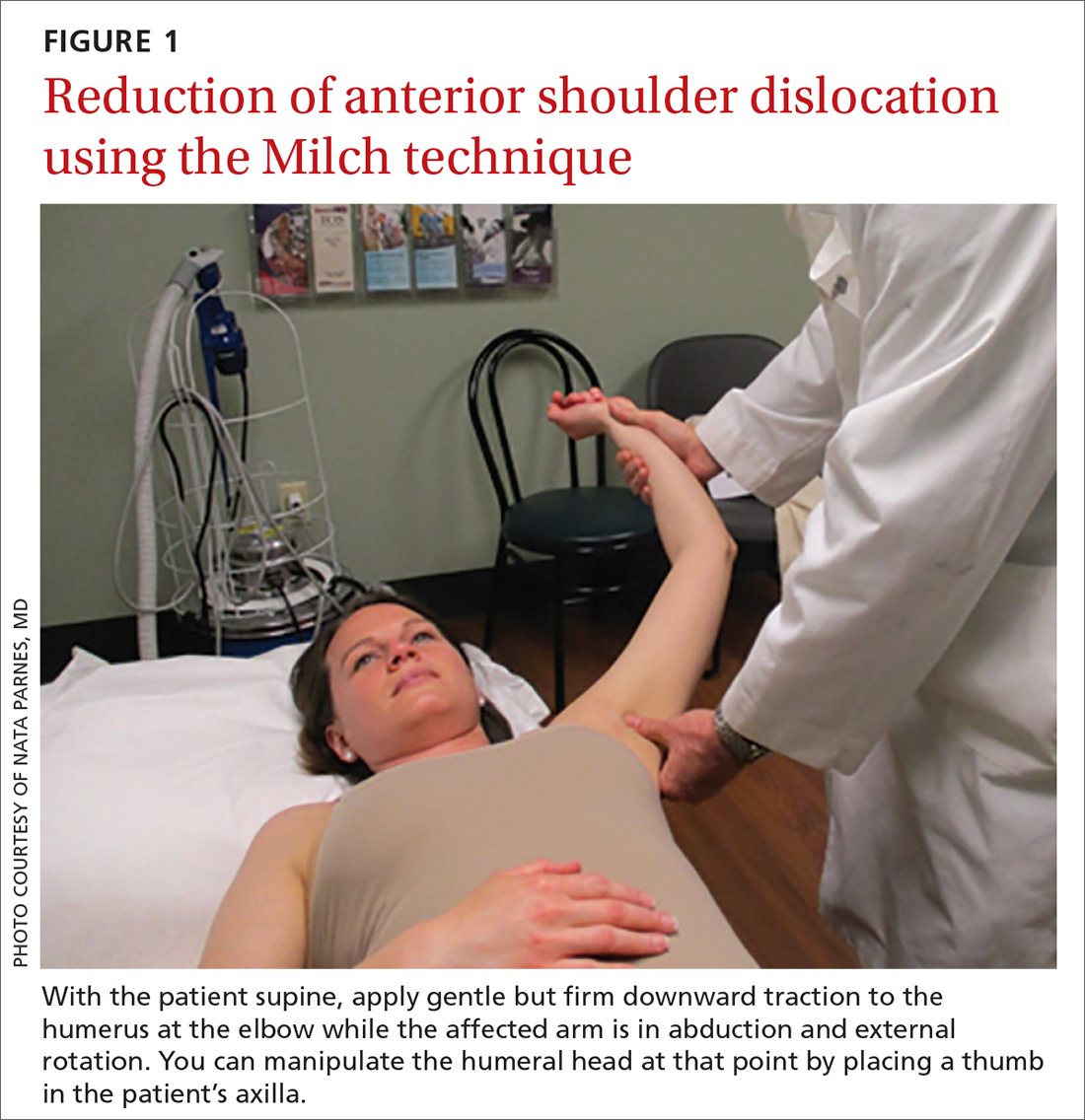
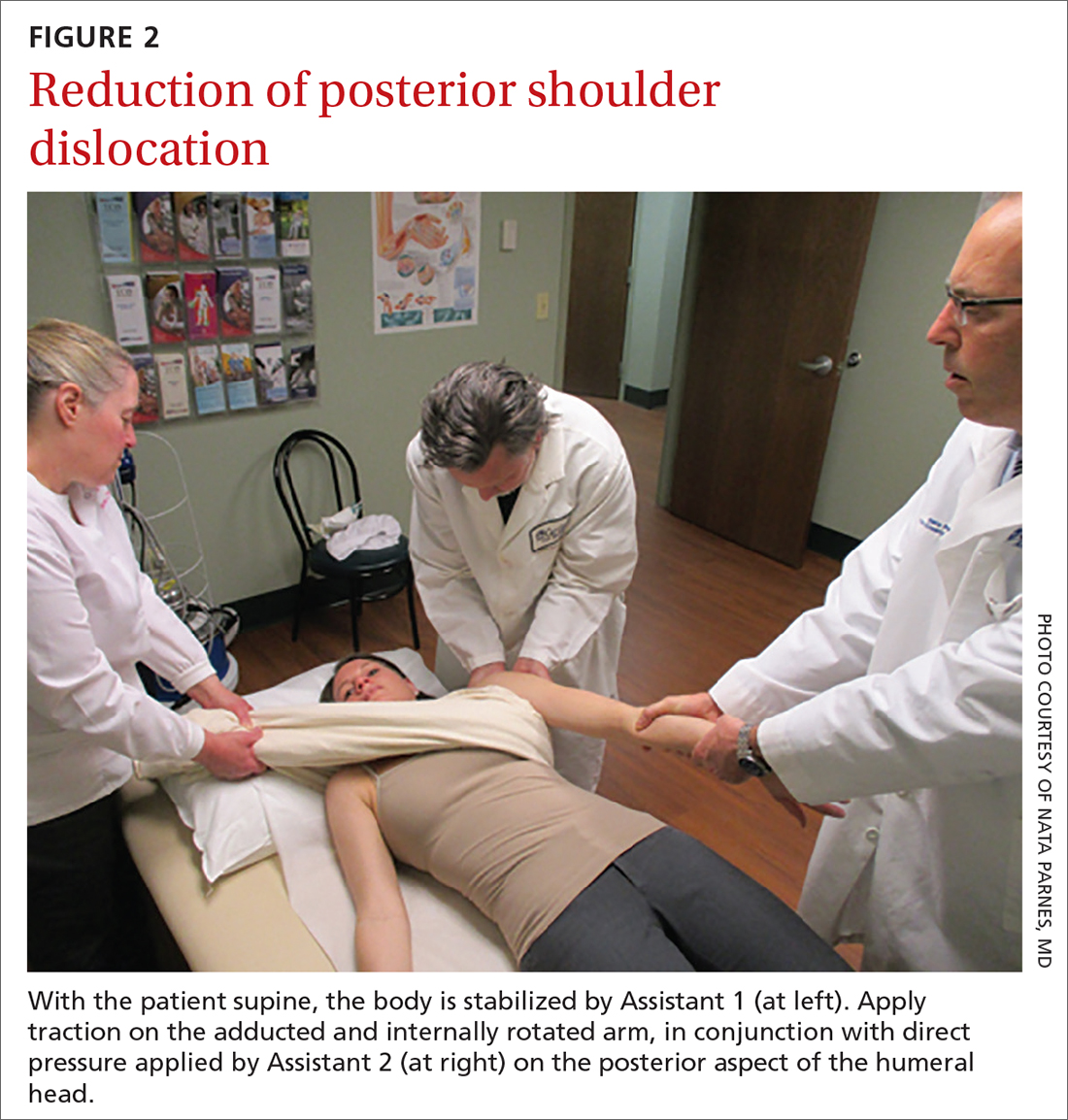
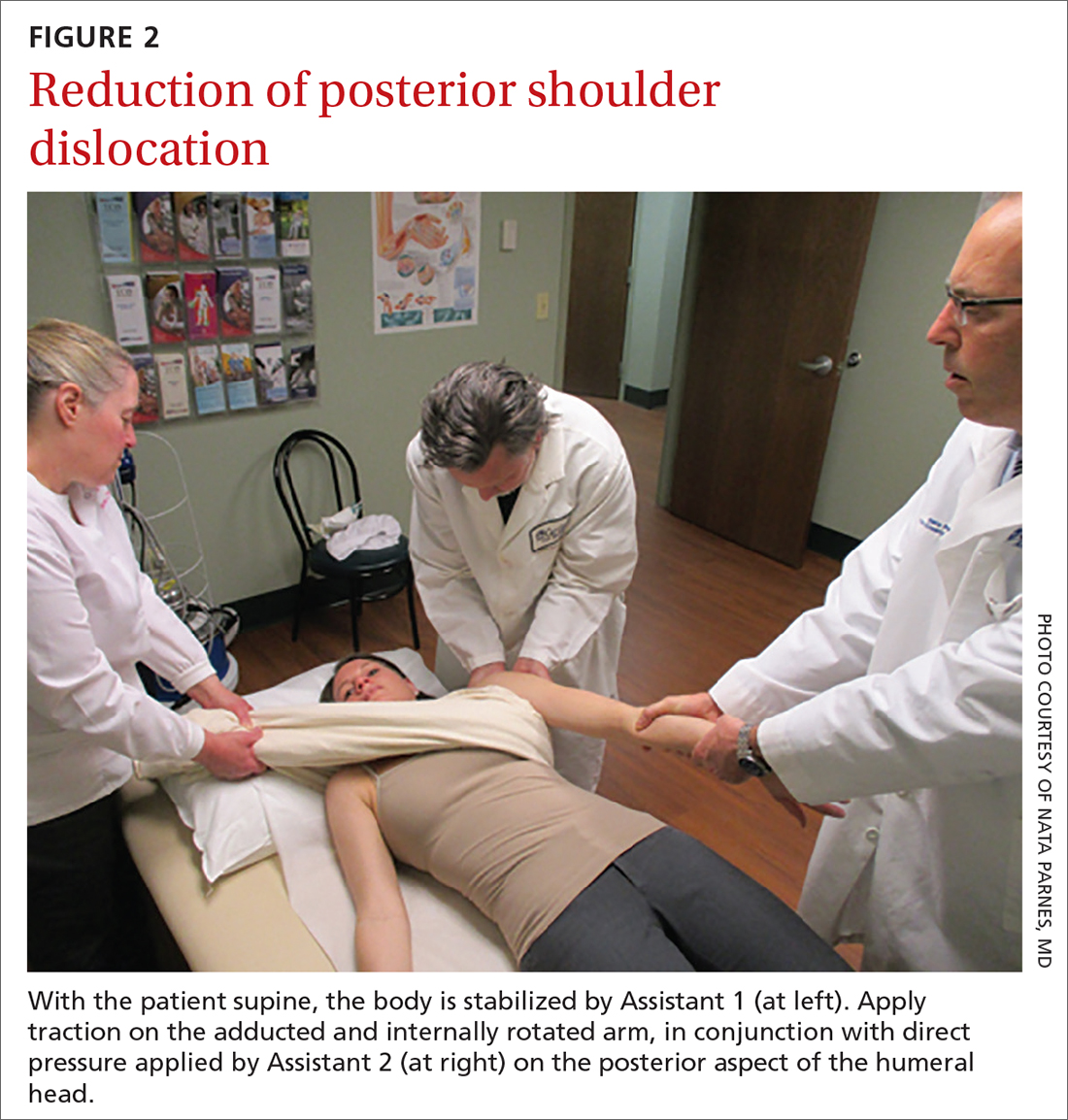
Posterior reduction of a dislocation is performed while the patient is supine, with the body stabilized. Traction is applied on the adducted and internally rotated arm in conjunction with direct pressure on the posterior aspect of the humeral head (FIGURE 2).
Continue to: Follow-up actions
Follow-up actions. Before discharging the patient after reduction of a dislocation, it is essential to:
- perform post-reduction evaluation of shoulder stability at different levels of abduction
- perform a thorough neurovascular assessment
- obtain an anteroposterior (AP) radiograph to ensure proper positioning of the glenohumeral joint.
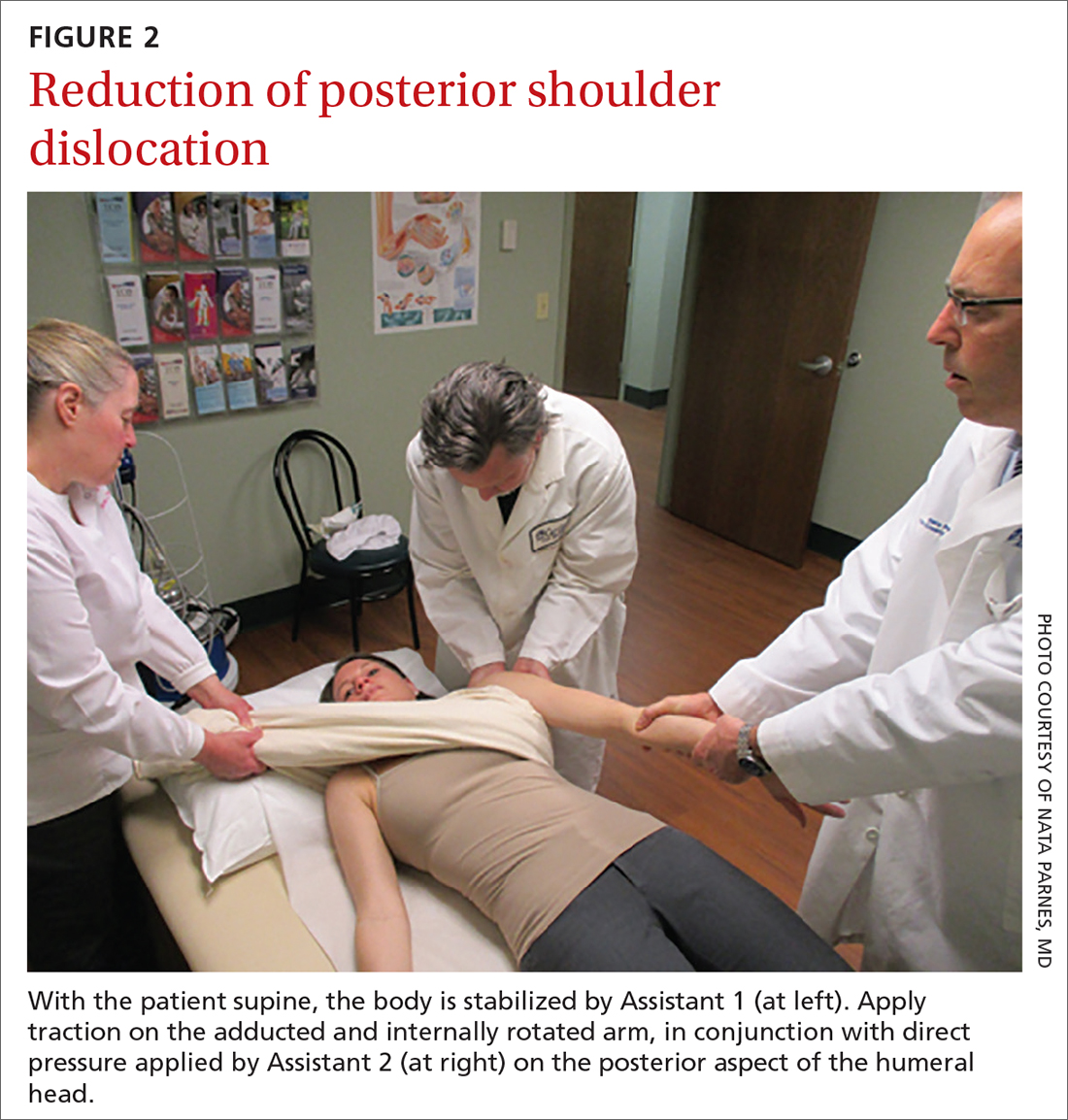
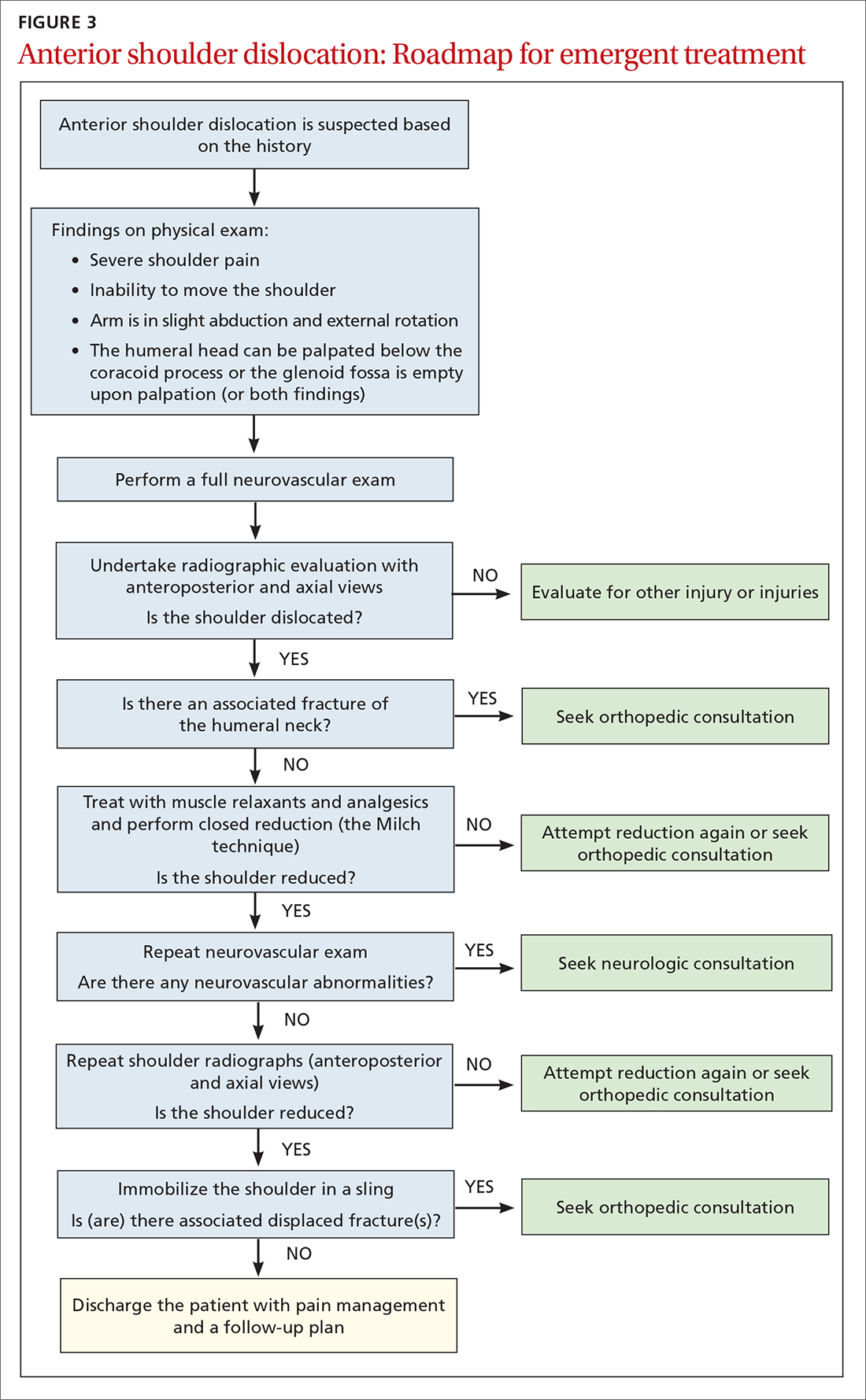
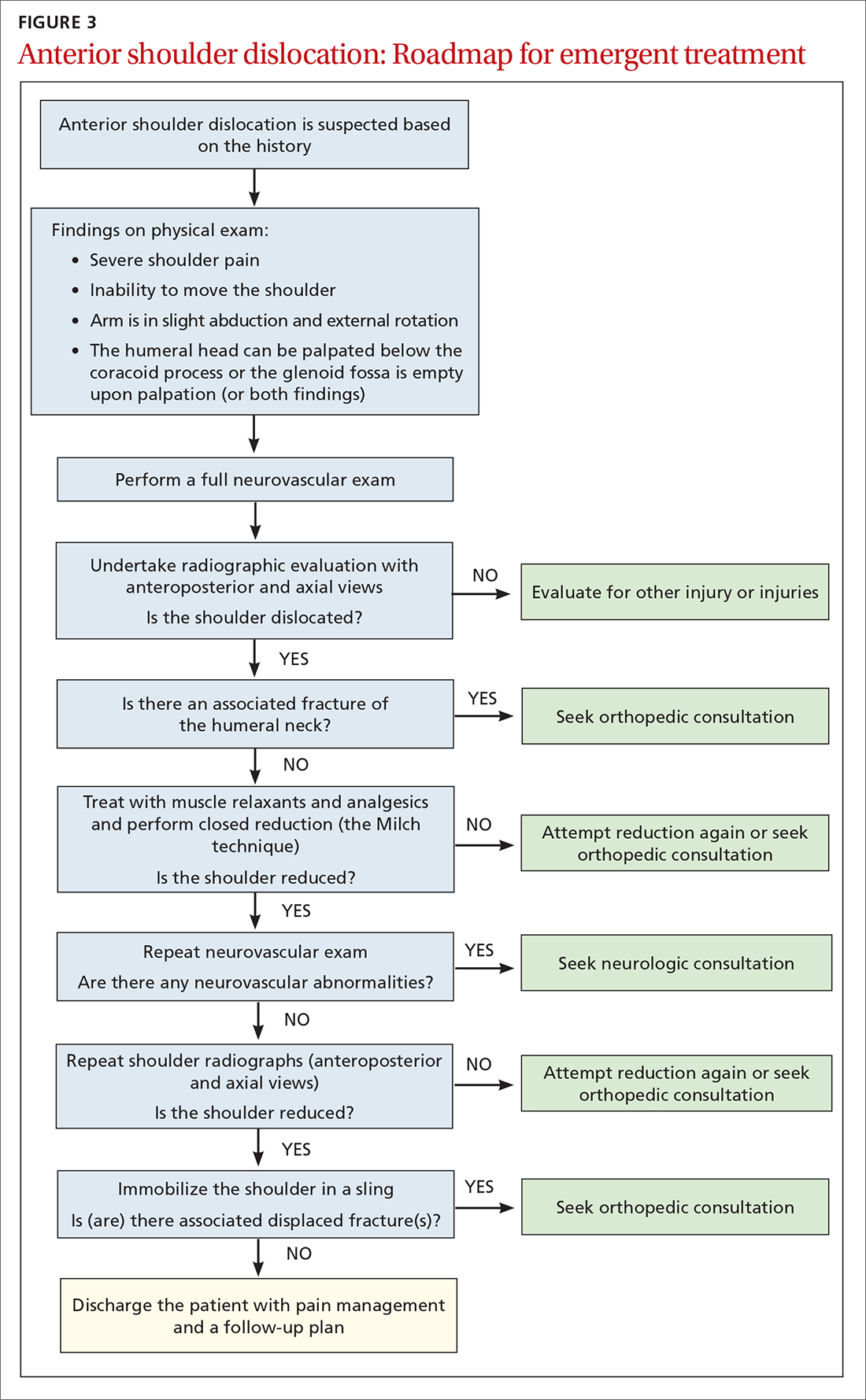
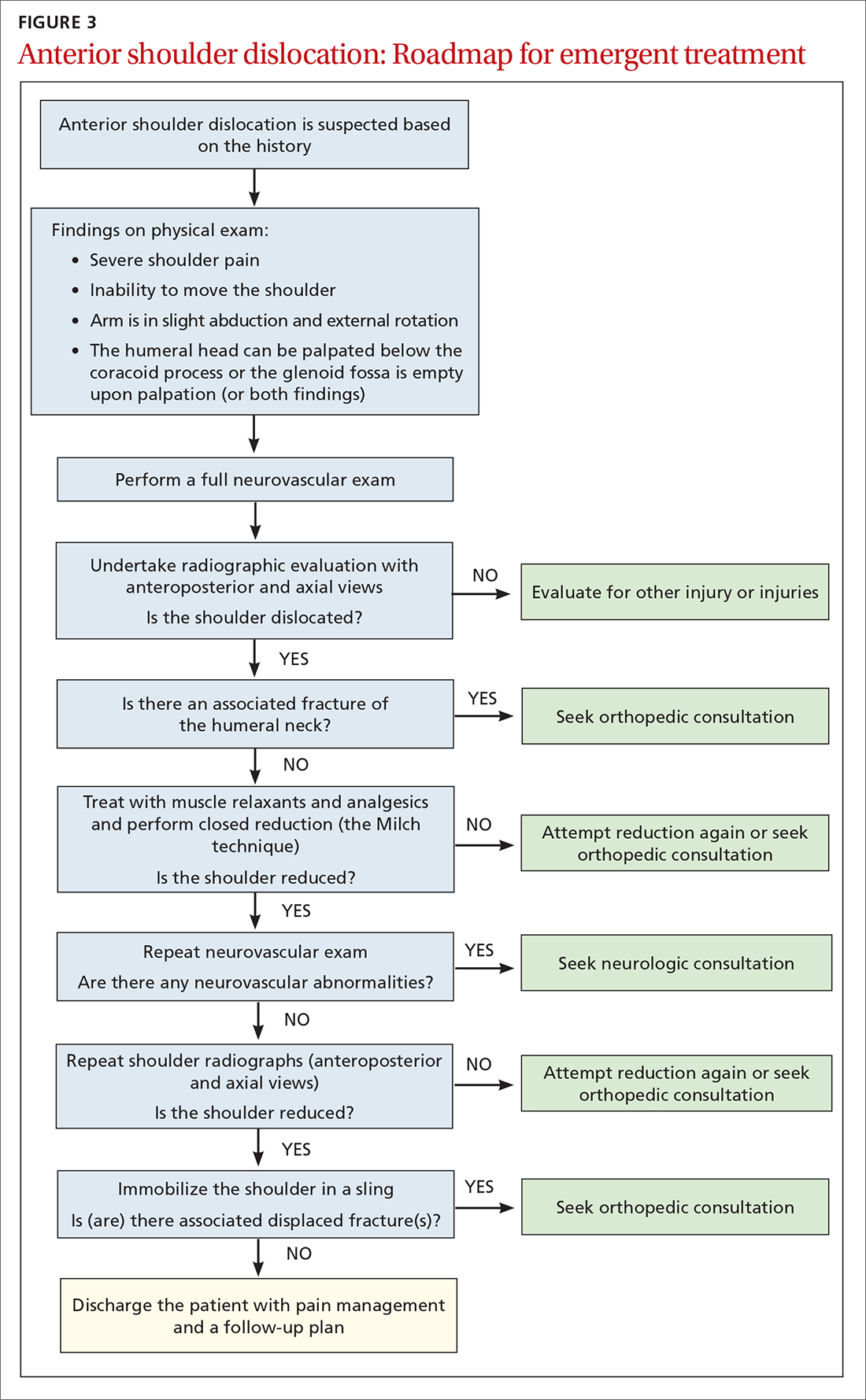
The reduced shoulder should be immobilized in a sling. The discharge plan should include pain management for several days and a follow-up appointment in 5 to 8 days with the primary care provider2 (FIGURE 3).
Follow-up evaluation by the primary care provider
History. Prior to the initial examination at follow-up, obtain a comprehensive history that includes the nature of the injury and the direction of force that was placed on the shoulder. Determine whether the shoulder was reduced spontaneously or required manual reduction in the field or an emergency department. Note any associated injury sustained concurrently and the presence (or absence) of neck pain, numbness, tingling, or weakness in the affected arm.
Physical exam starts with thorough inspection of the affected shoulder, with comparison to the contralateral side, at rest and during shoulder motion. Palpation to reveal points of tenderness should include the anterior joint line, acromioclavicular joint, bicipital groove, subacromial space, acromion, and greater tuberosity.
Following inspection and palpation, assess active and passive range of motion in forward elevation, abduction, internal and external rotation at the side of the body, and internal and external rotation in shoulder abduction. Assessment might be limited by pain and apprehension, and should be performed within the patient’s comfortable range of motion.
Continue to: Once range of motion...
Once range of motion is determined, assess7:
- muscle power of the rotator cuff in abduction (for the supraspinatus muscle)
- resisted external rotation at the side of the body (the infraspinatus)
- resisted external rotation in abduction > 60° (the teres minor)
- resisted internal rotation (the subscapularis).
Specific tests for shoulder laxity and stability
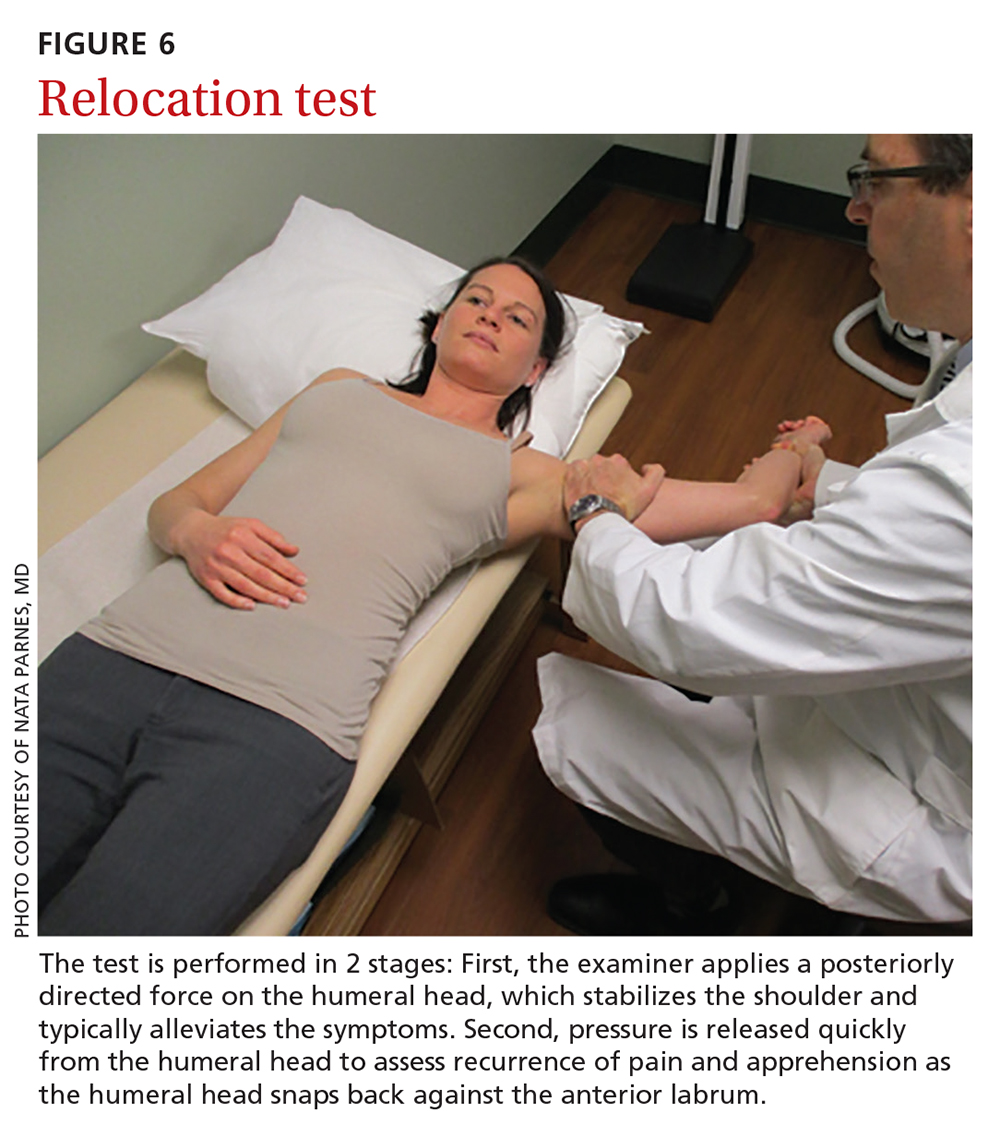
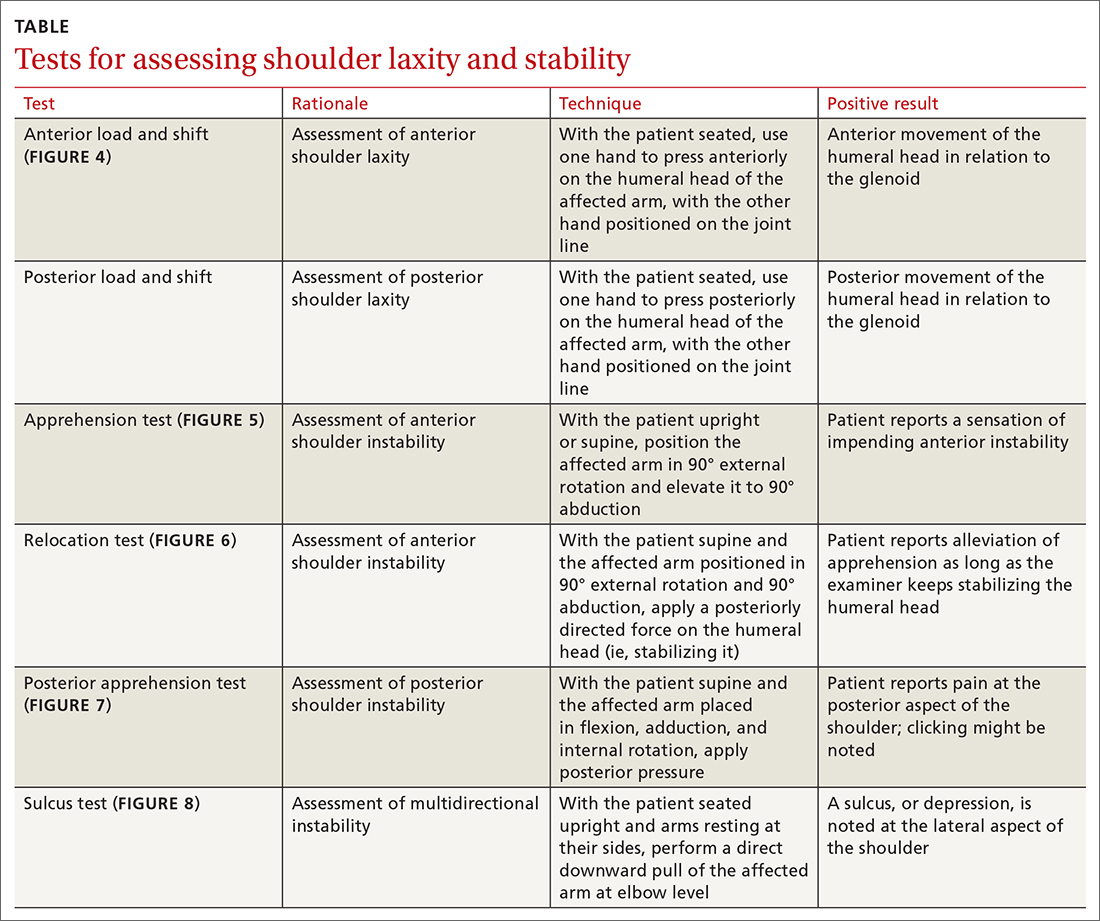
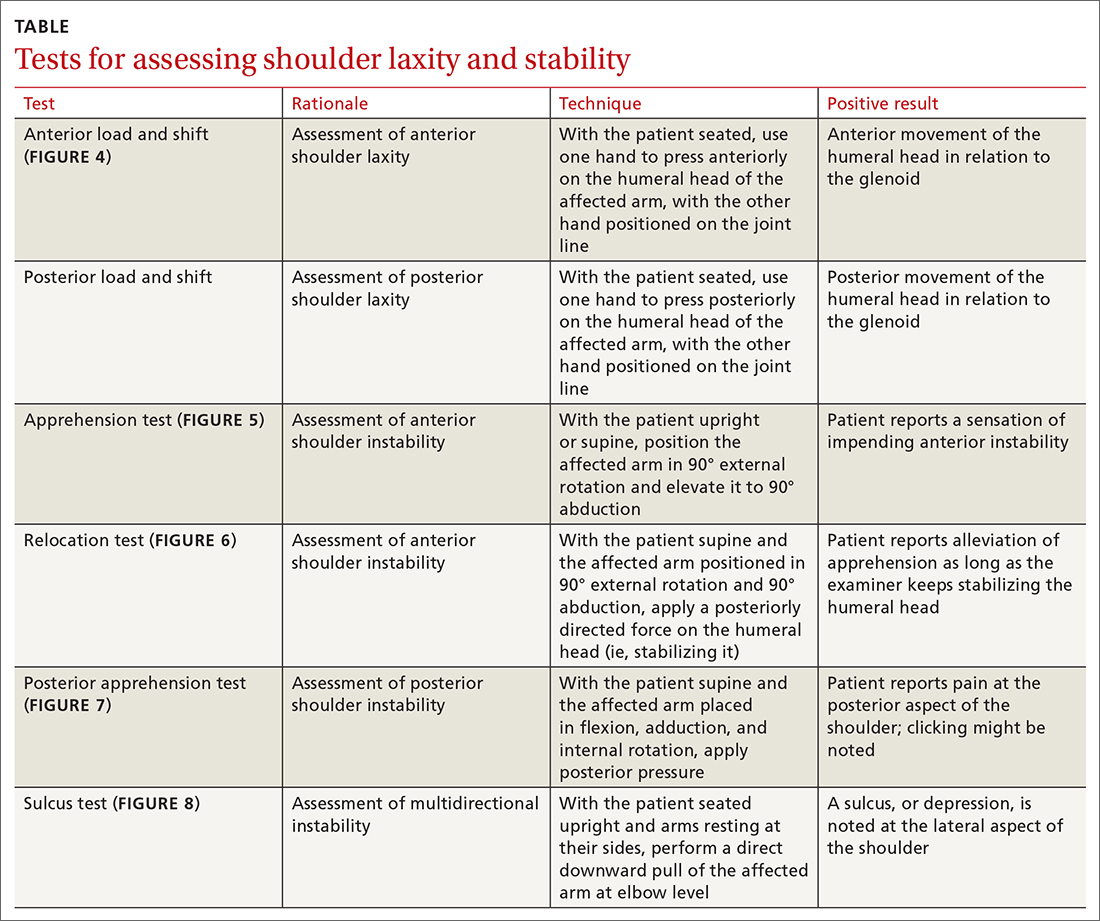
It is important during the primary care follow-up examination to differentiate true instability and shoulder hyperlaxity, particularly in young, flexible patients (TABLE). Many of these patients present with painless hypermobility of the shoulder without true injury to the labrum or ligamentous structures. It might appear to the patient, or to family, that the shoulder is subluxating; however, the humeral head returns to a centered position on the glenoid in a hypermobile state—typically, without pain. Actual shoulder instability is defined as loss of the ability of the humeral head to re-center, accompanied by pain—pathology that is frequently associated with damage to the capsulolabral complex.
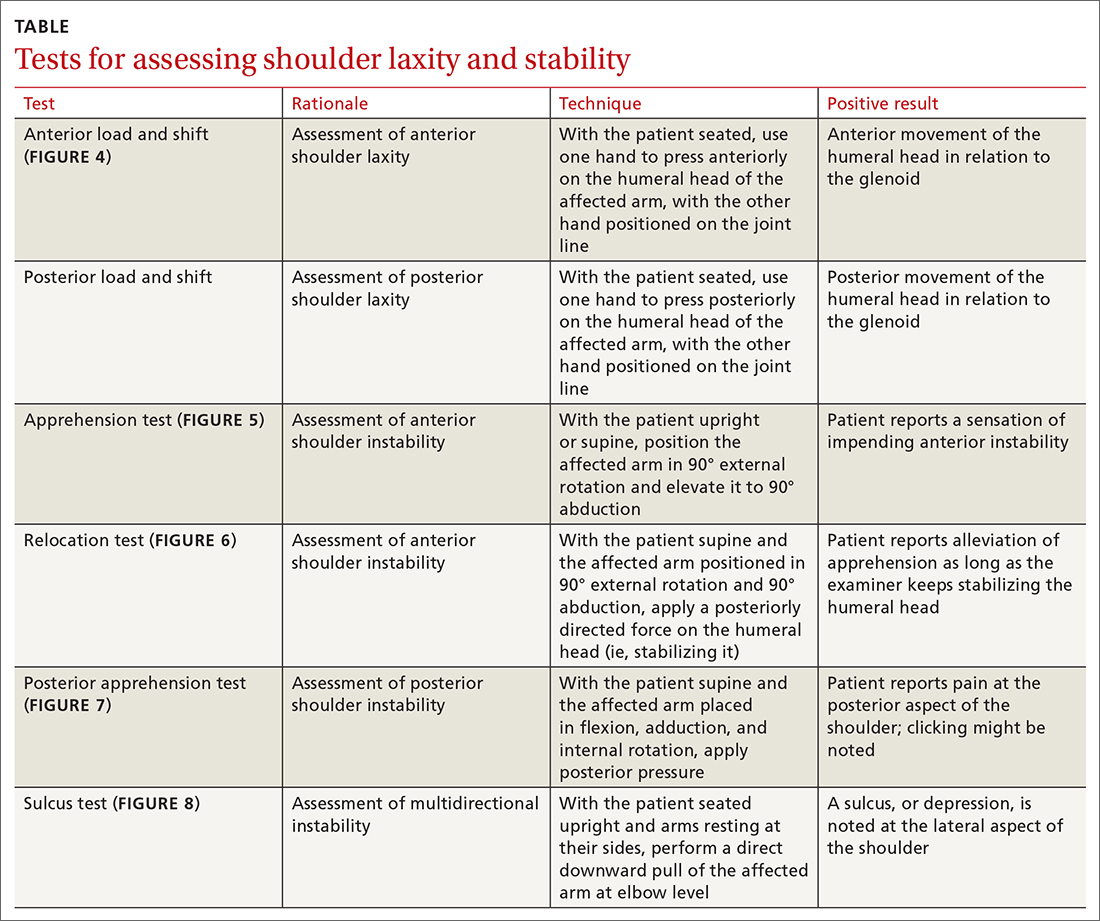
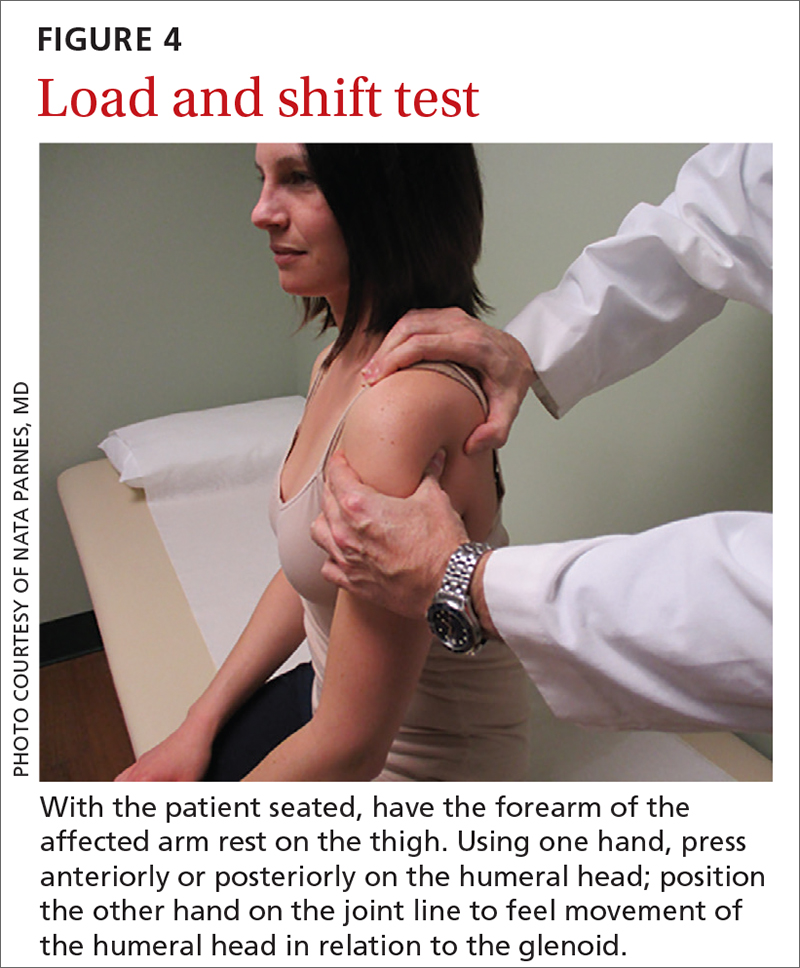
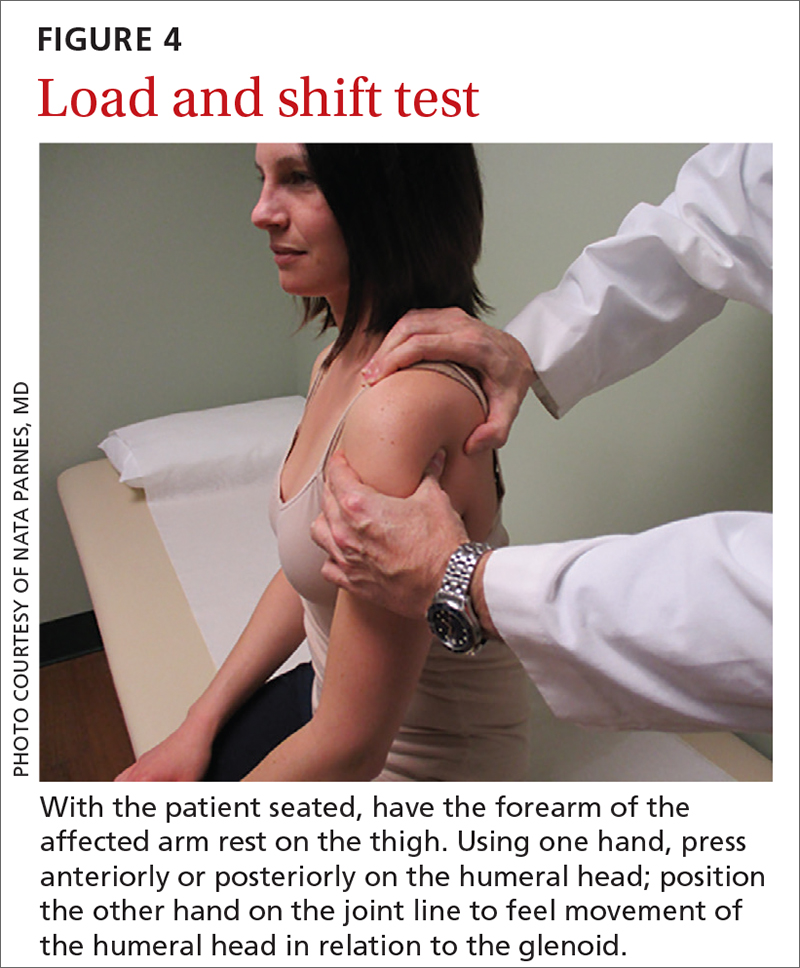
The load and shift test is used to assess anterior and posterior laxity. The patient is seated, and the forearm is allowed to rest on the thigh. Examination is performed using 1 hand to press anteriorly or posteriorly on the humeral head; the other hand is simultaneously positioned on the joint line to feel movement of the humeral head in relation to the glenoid (FIGURE 4).
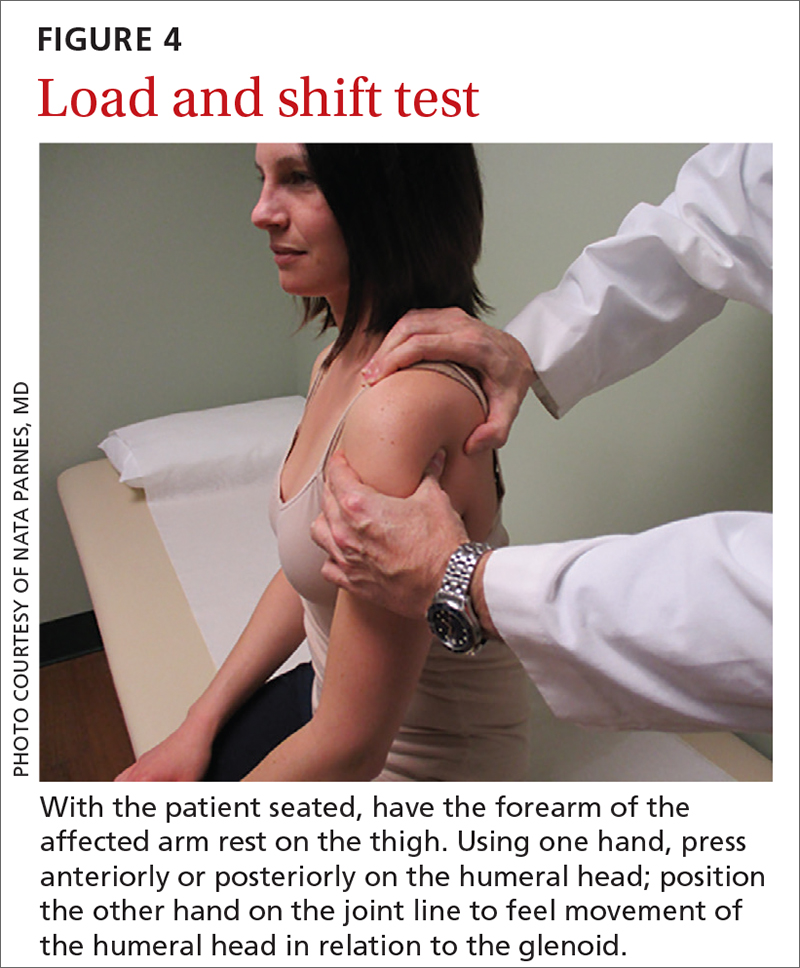
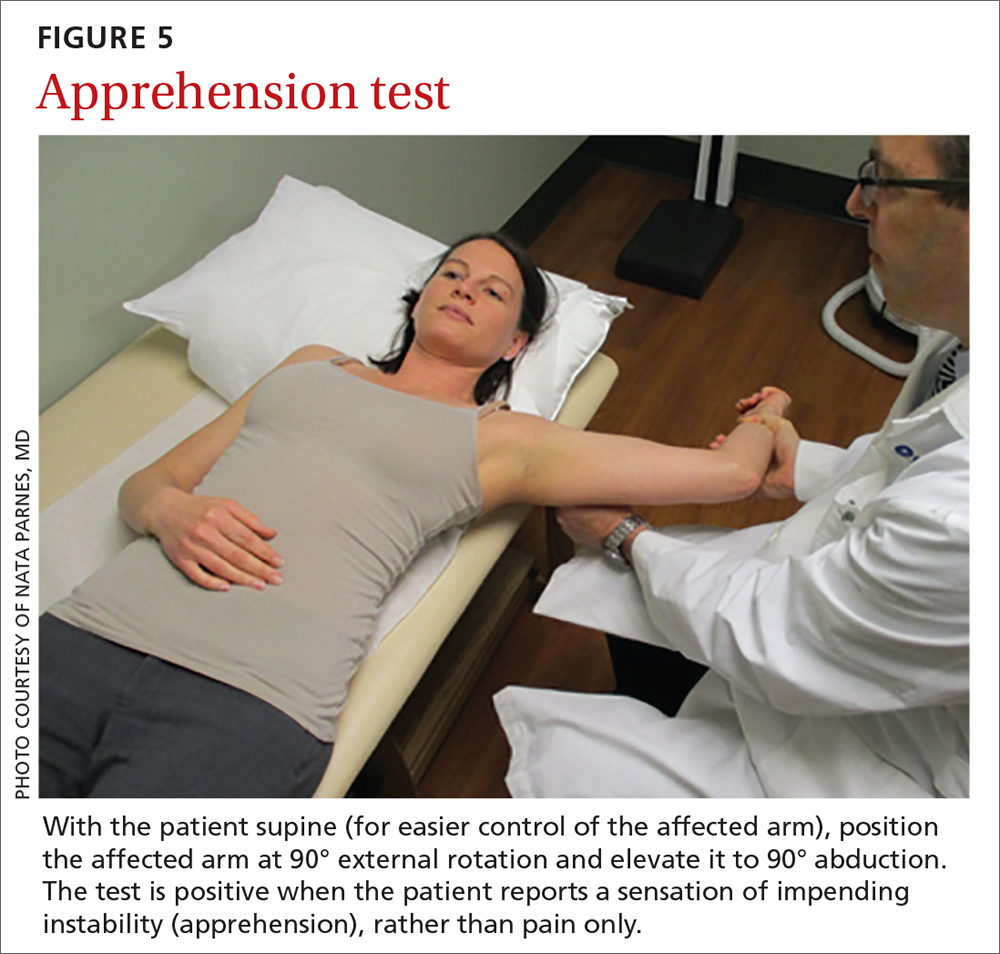
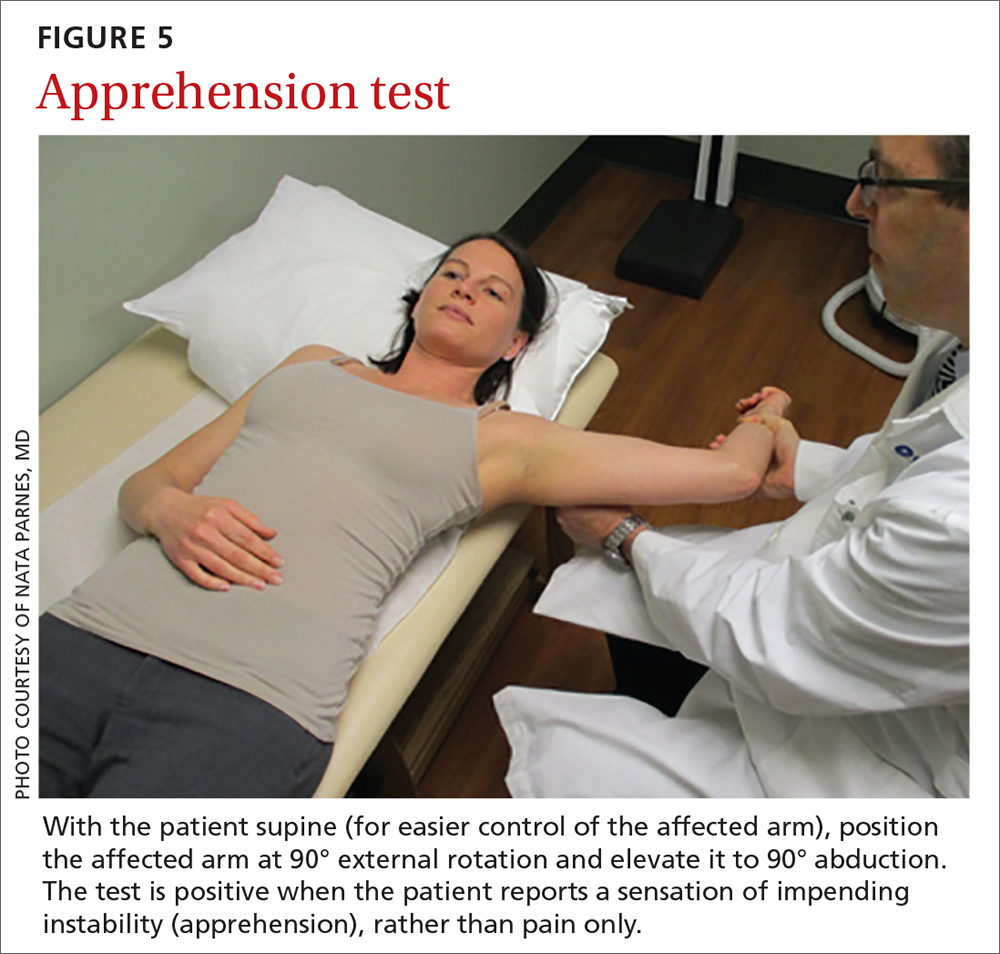
The apprehension test is a common maneuver used to assess anterior shoulder instability. It is performed by positioning the affected arm to 90° external rotation and then elevating it to 90° abduction. Although this maneuver can be performed with the patient upright, it is beneficial to have them supine, to more easily control the arm (FIGURE 5). A positive test is noted when the patient reports a sensation of impending instability (apprehension), rather than pain alone.
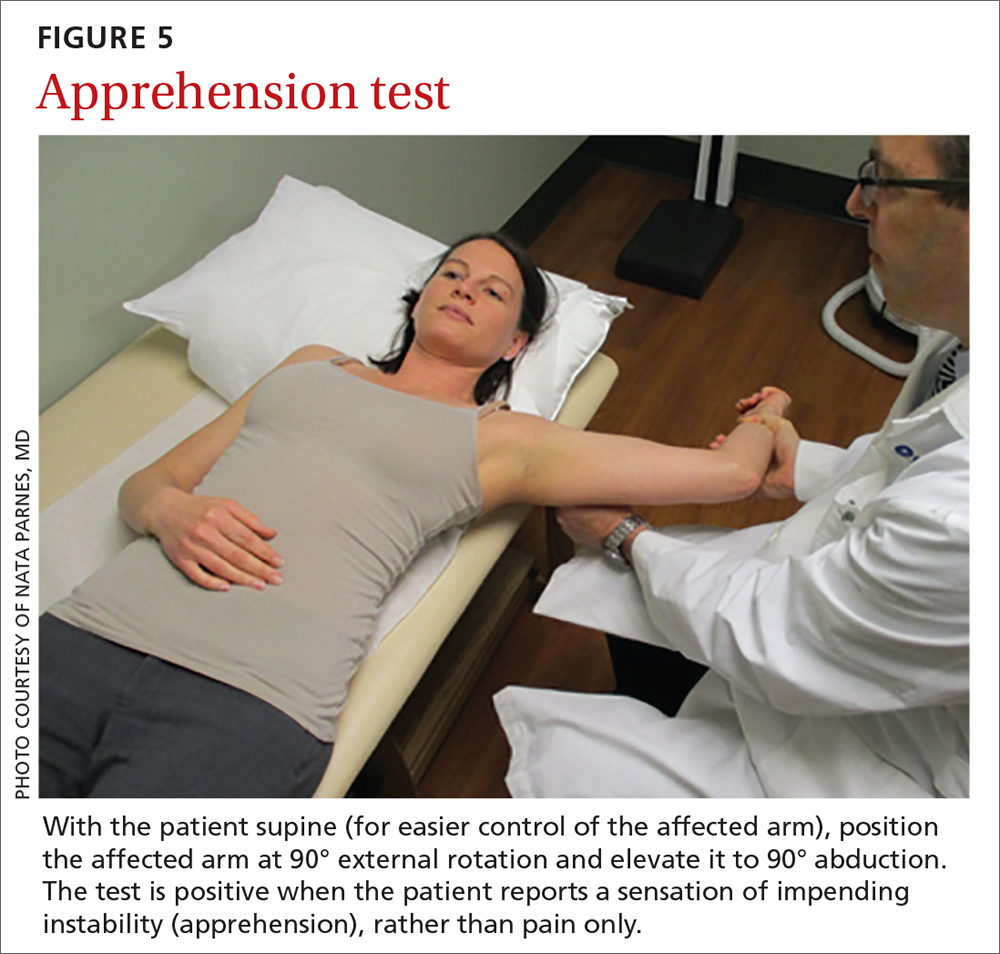
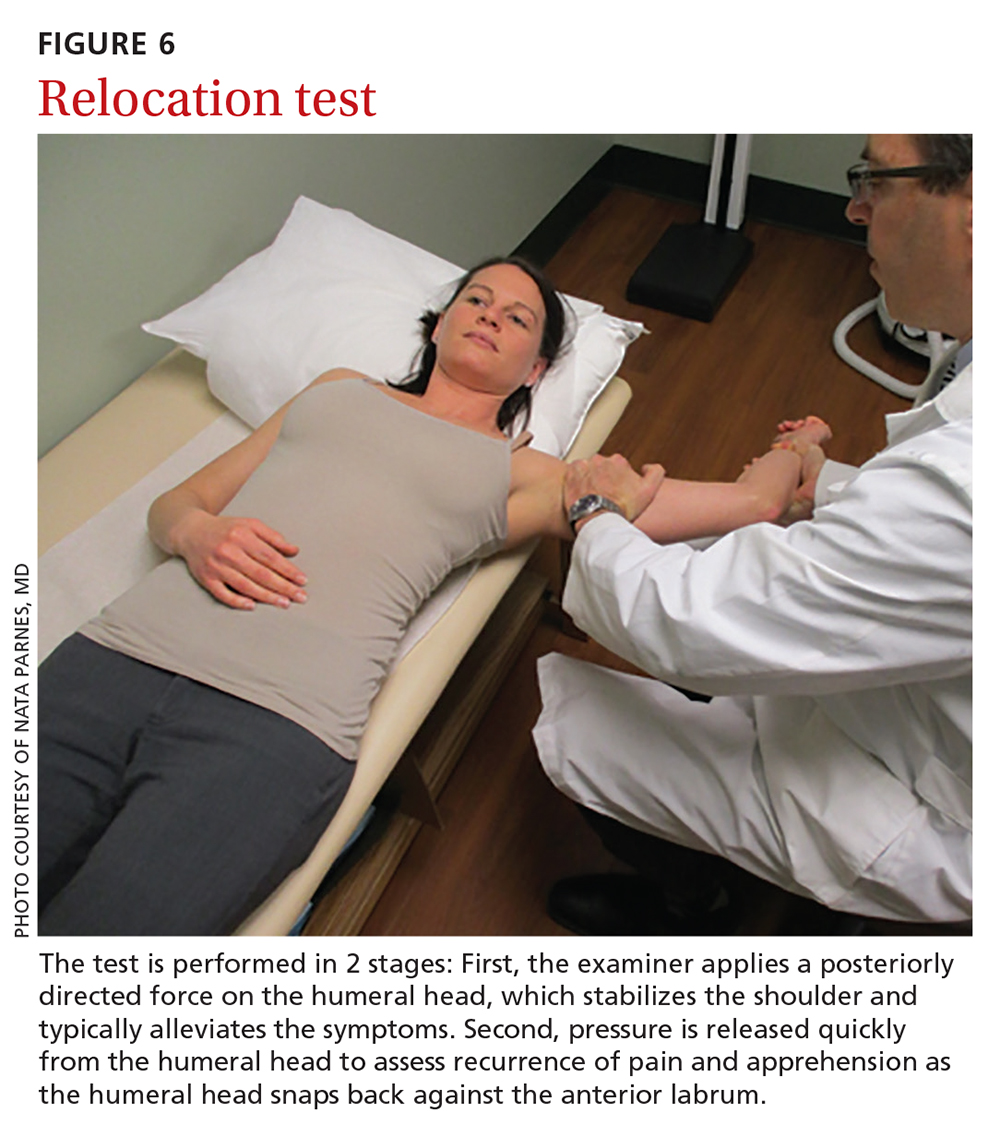
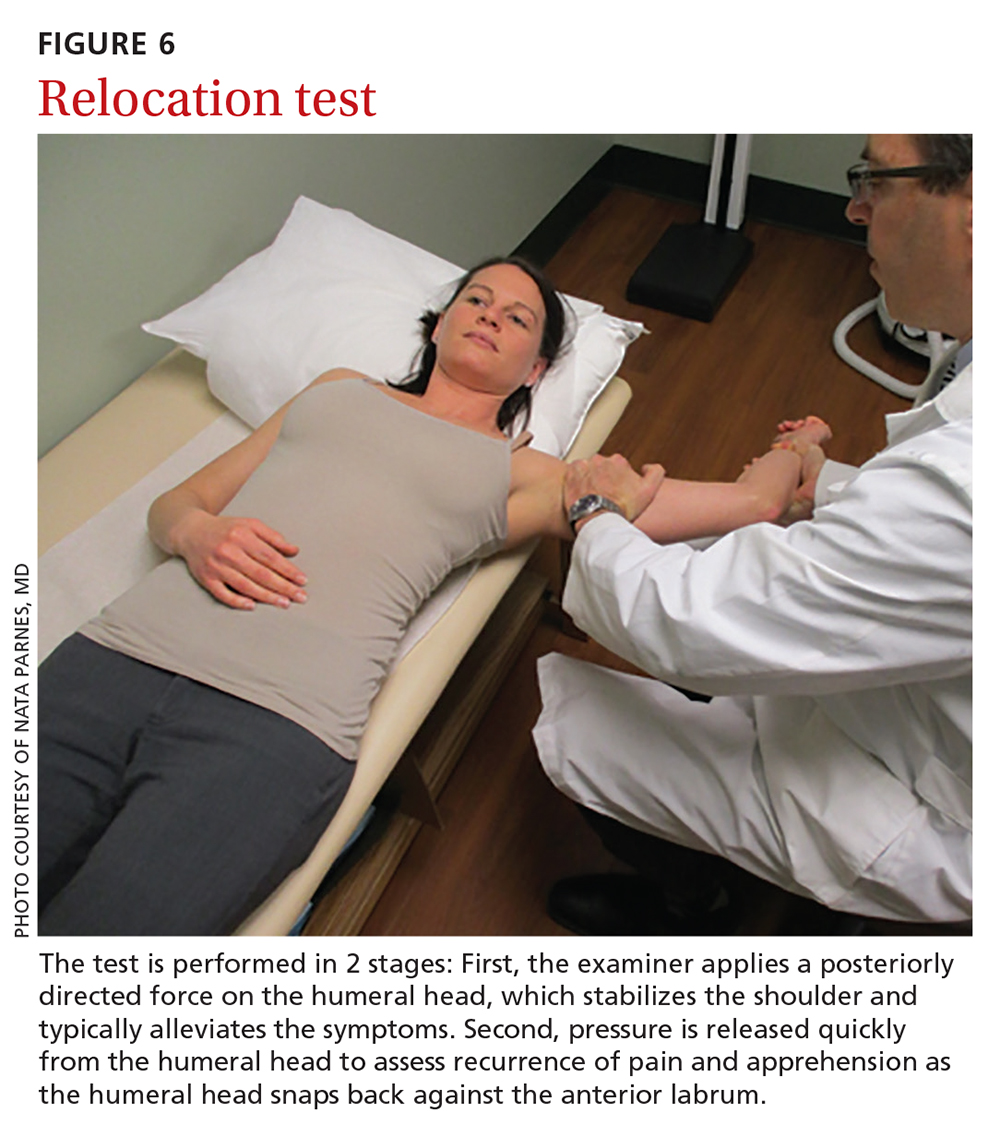
Relocation test. When the apprehension test is positive, the supine position can be exploited to further perform the relocation test, in 2 stages (FIGURE 6):
- Apply a posteriorly directed force on the humeral head, which stabilizes the shoulder and typically alleviates symptoms.
- Release pressure quickly from the humeral head to assess recurrence of pain and apprehension as the humeral head snaps back against the anterior labrum.
Continue to: Combined, apprehension and relocation...
Combined, apprehension and relocation tests to identify anterior shoulder instability have been shown to significantly improve specificity while maintaining sensitivity.8
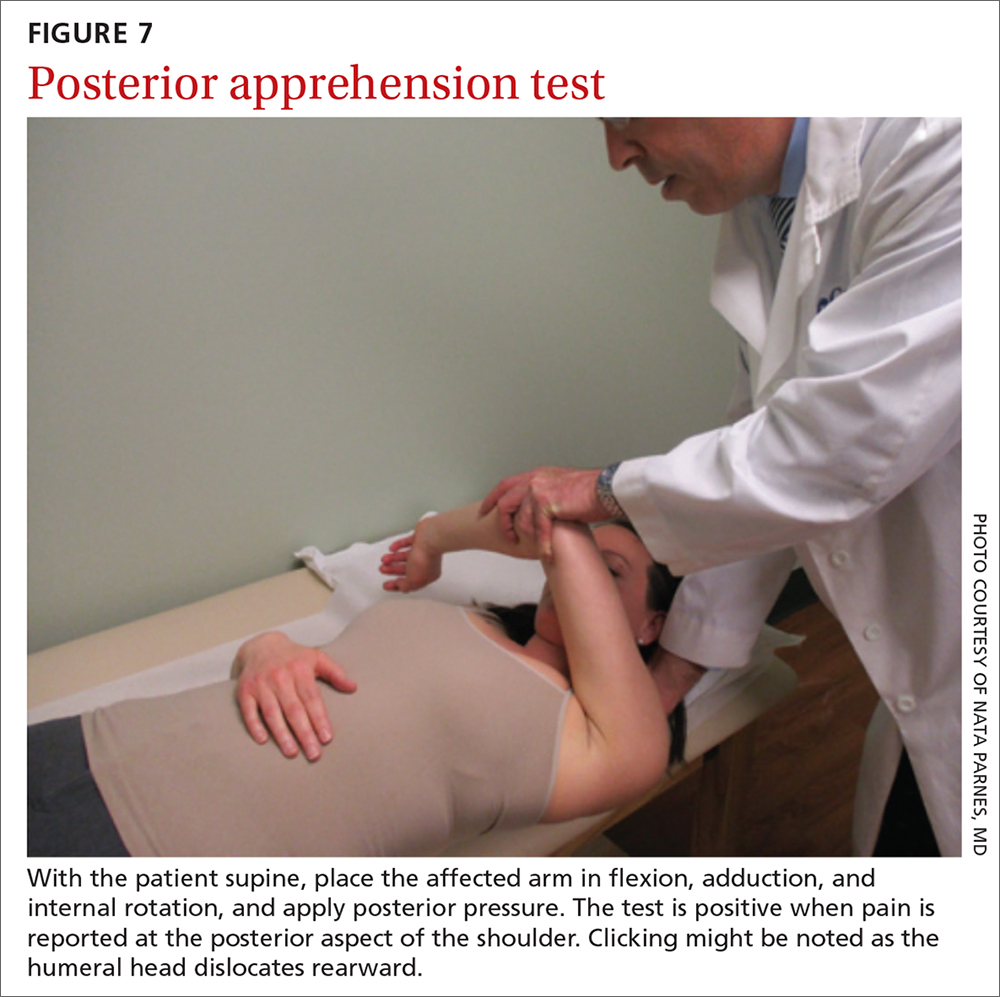
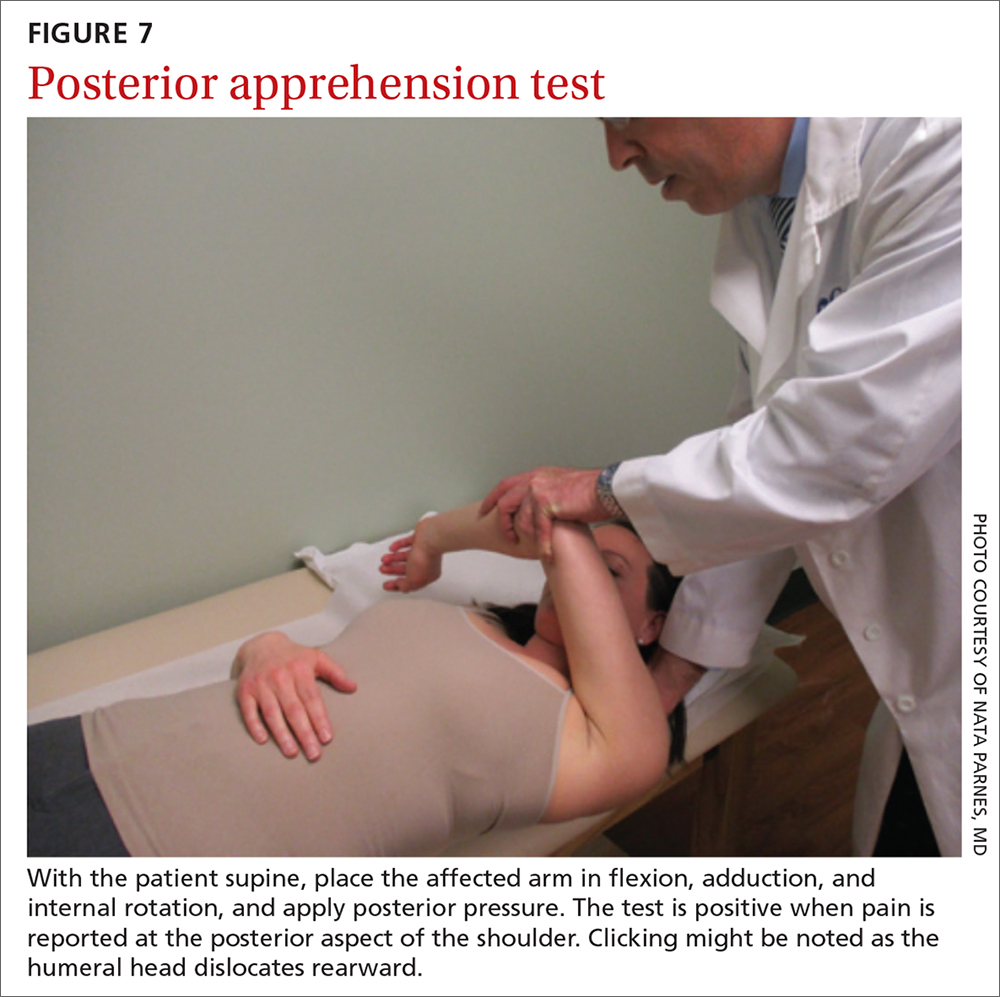
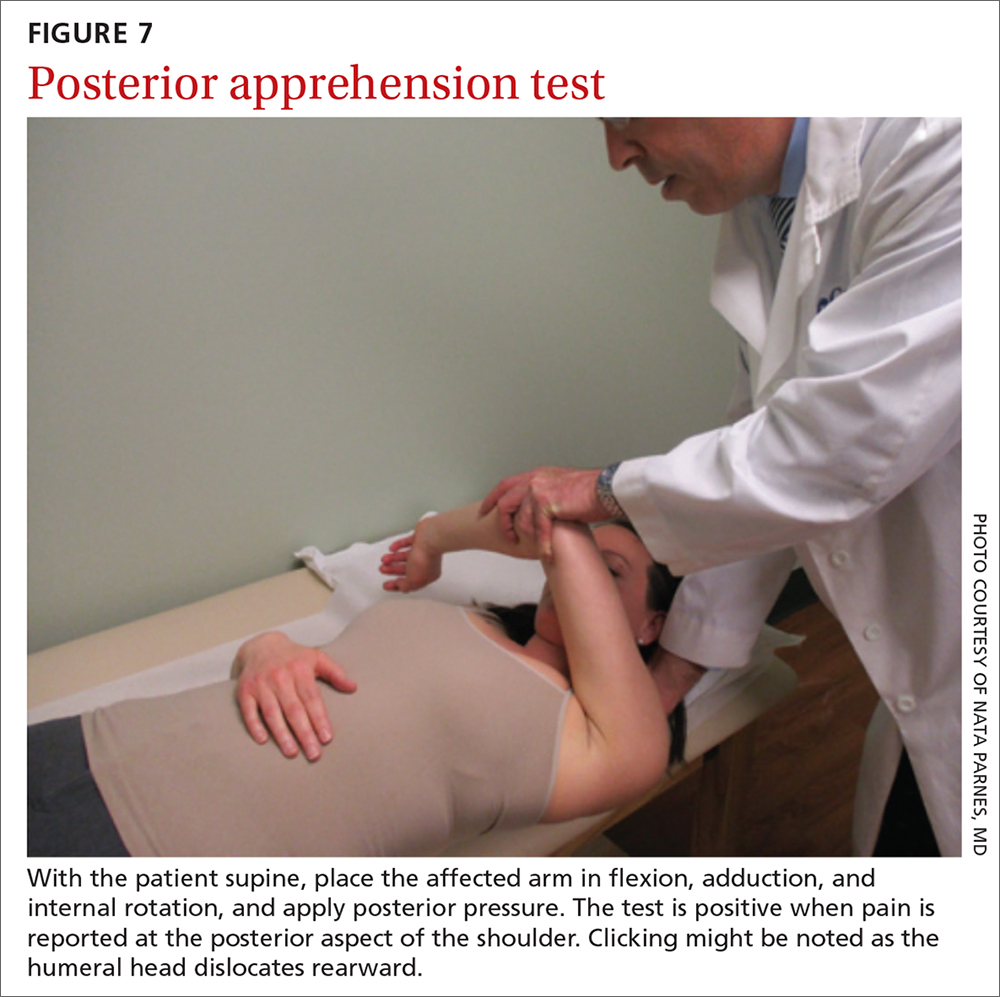
The posterior apprehension test is used to assess posterior instability. The patient is supine; the affected arm is placed in flexion, adduction, and internal rotation; and posterior pressure is applied (FIGURE 7). A positive test is noted when pain is reported at the posterior aspect of the shoulder. Clicking might be noted as the humeral head dislocates rearward.1
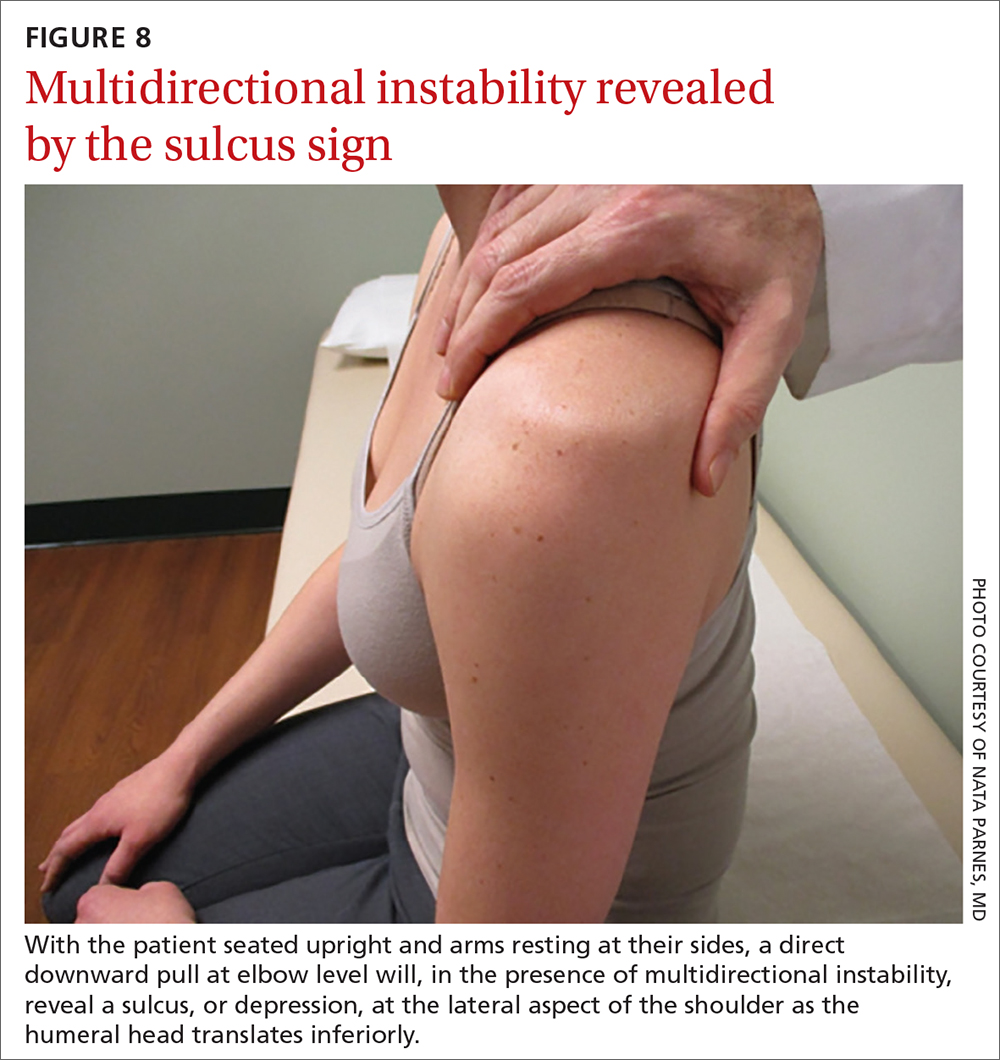
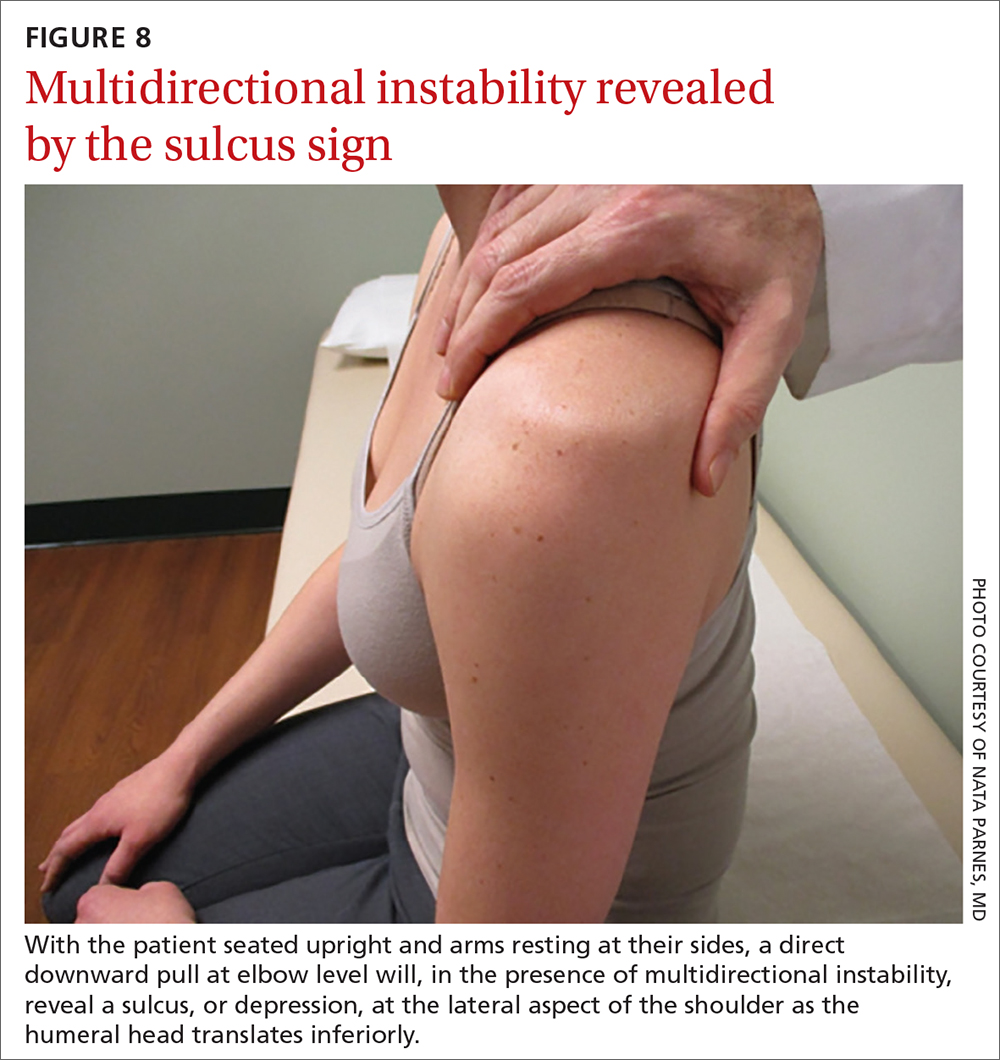
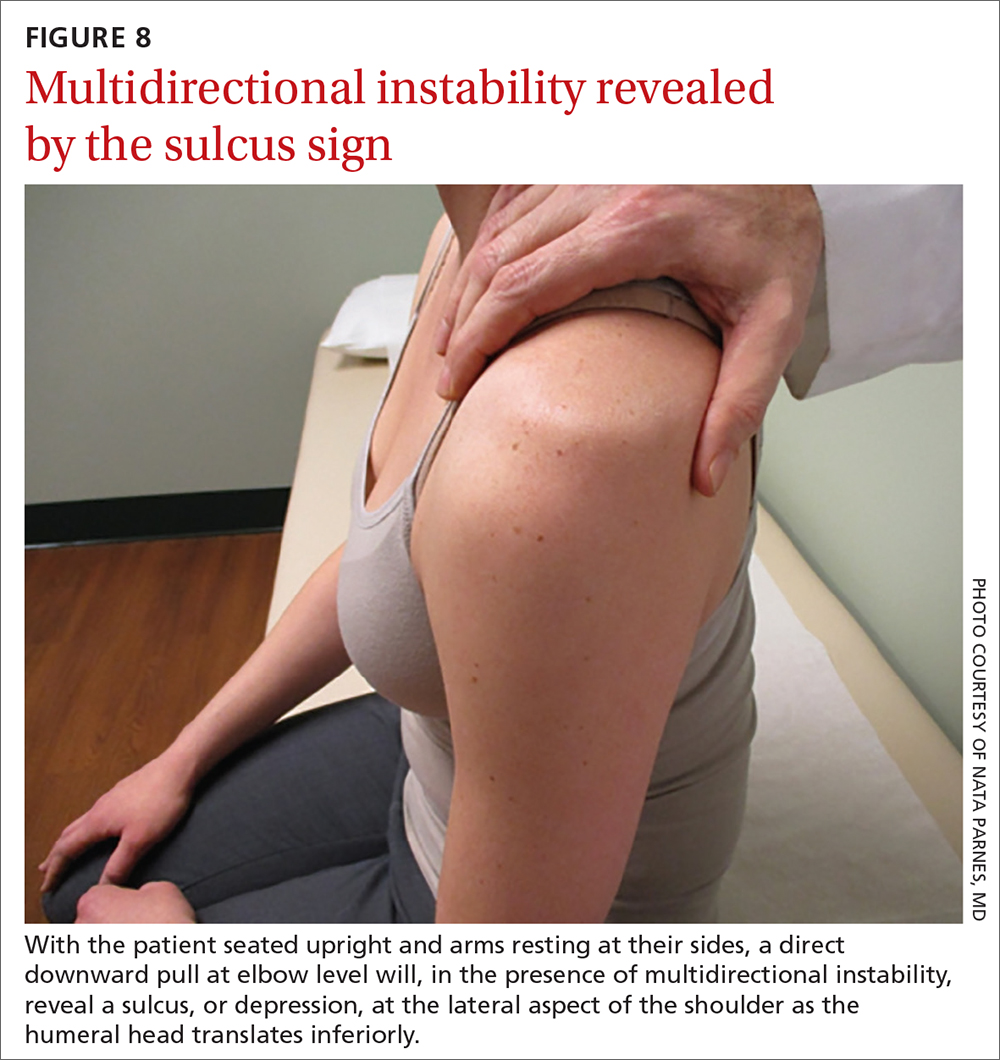
Sulcus sign. Multidirectional instability is elicited using the sulcus sign. While the patient is seated upright, arms resting at their sides, a direct downward pull at elbow level will, when positive, reveal a depression (sulcus) at the lateral aspect of the affected shoulder as the humeral head translates inferiorly (FIGURE 8). A positive sulcus sign is documented in 3 grades, according to the amount of translation1:
- Grade I: < 1 cm
- Grade II: 1-2 cm
- Grade III: > 2 cm.
Neurovascular status should be verified at every physical evaluation, with motor and sensory function tested in the axillary, musculocutaneous, median, radial, and ulnar nerve distributions. If nerve injury is suspected, electromyography and nerve-conduction testing is indicated.9-13 Vascular compromise is much less common but equally important to assess.11
Use of imaging
Post-reduction radiographs, including internal and external AP—and especially axillary—views are invaluable. Not only do they help to ensure reduction, but they also help to assess for fracture. A magnetic resonance imaging (MRI) arthrogram is the preferred imaging modality if a labral tear is suspected (FIGURE 9). Other concomitant shoulder injuries, such as subtle bone fracture, rotator cuff tear, and biceps pathology can also be reliably diagnosed with noncontrast MRI.
Continue to: Roadmap for treatment
Roadmap for treatment
The rate of recurrence after a first anterior shoulder dislocation is strongly associated with a person’s age and level of activity. Active patients younger than 20 years have a 92% to 96% recurrence rate14; patients 20 to 40 years, 25% to 48%; and patients older than 40 years, < 10%.15
Young, athletic patients who are treated nonoperatively are left at an unacceptably high risk of recurrence, leading to progressive damage to bony and soft-tissue structures.16,17 Surgical labral repair after a first-time anterior dislocation produced improved outcomes in terms of recurrent dislocation (7.9%), compared to outcomes after nonsurgical treatment (52.9%),14 and has been associated with a lower incidence of future glenohumeral osteoarthritis.18 For those reasons, we recommend referral to an orthopedic surgeon for all patients younger than 20 years who sustain an anterior shoulder dislocation.
Patients older than 20 years who do not have concomitant shoulder injury, and who demonstrate full strength in abduction, external rotation, and internal rotation of the shoulder on clinical examination, have a low probability of associated rotator-cuff tear. They can be immobilized in a sling for 1 to 3 weeks, followed by a 6 to 12–week regimen of physical therapy.
Concomitant tear of the rotator cuff. Weakness on examination requires MRI or a magnetic resonance arthrogram for evaluation of associated rotator-cuff tear. A tear identified on MRI should be referred to an orthopedic surgeon because timely repair can be crucial to attaining best outcomes. Conservative treatment of traumatic full-tendon rotator-cuff tear is associated with poor results, progression in the size of the tear, and advancement of muscle atrophy.19,20 For patients younger than 40 years, arthroscopic rotator-cuff repair, with or without labral repair, produces excellent clinical outcomes, carries a low risk of complications, and results in a > 95% rate of return to a preoperative level of recreational and job activities.21
Patients who demonstrate weakness of the rotator-cuff muscles on examination, but who do not have a tear noted on MRI, should be evaluated by electromyography and nerve-conduction testing to assess nerve injury as an alternative cause of weakness.10,11 If a neurologic deficit is found on nerve-conduction testing, the patient should be referred for neurologic evaluation.10
Continue to: Patients with negative findings...
Patients with negative findings on MRI and nerve-conduction studies should be offered physical therapy. Patients with recurrent anterior shoulder dislocation should be referred to an orthopedic surgeon for surgical repair. Frequently, improper or delayed treatment with chronic instability results in degenerative arthropathy of the joint22 (FIGURE 10).

Posterior and multidirectional instability can typically be treated conservatively; however, whereas posterior dislocation typically must be immobilized for 3 to 6 weeks post reduction, multidirectional instability does not require immobilization. Instead, physical therapy should start as soon as possible. In these cases, recurrent dislocation or subluxation that persists after conservative treatment should be referred for possible surgical intervention.5
Instability with associated fracture
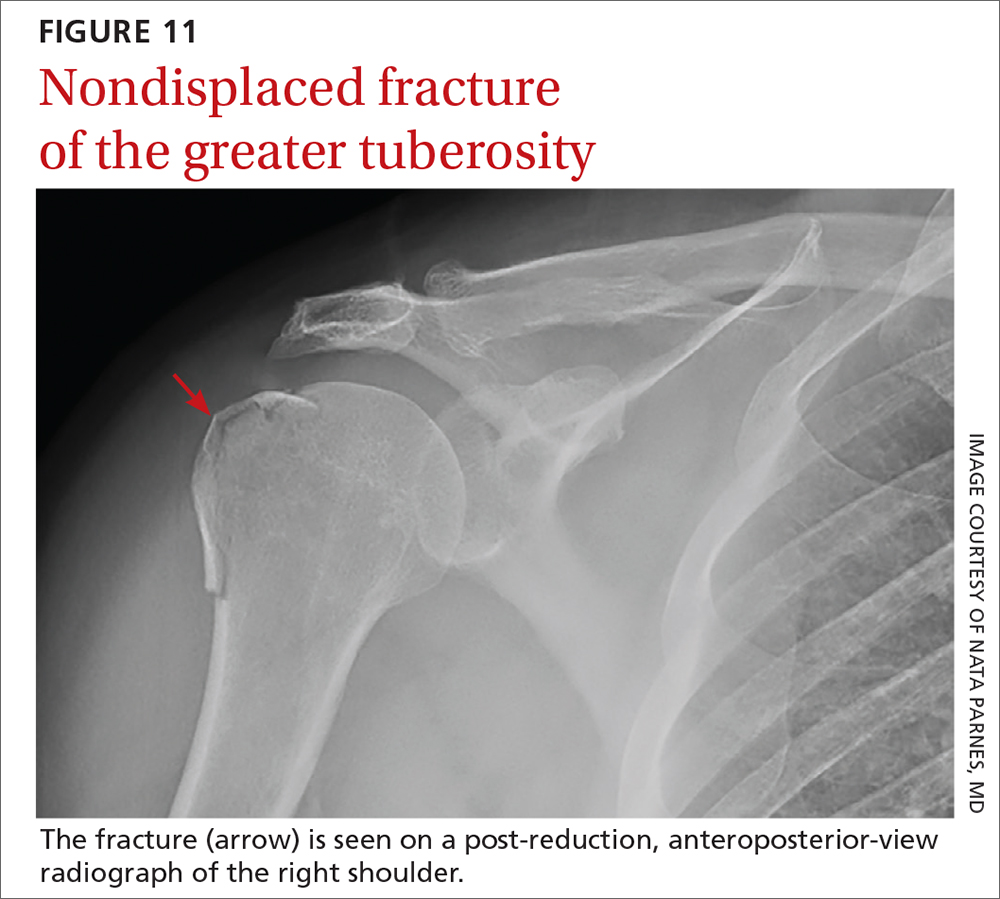
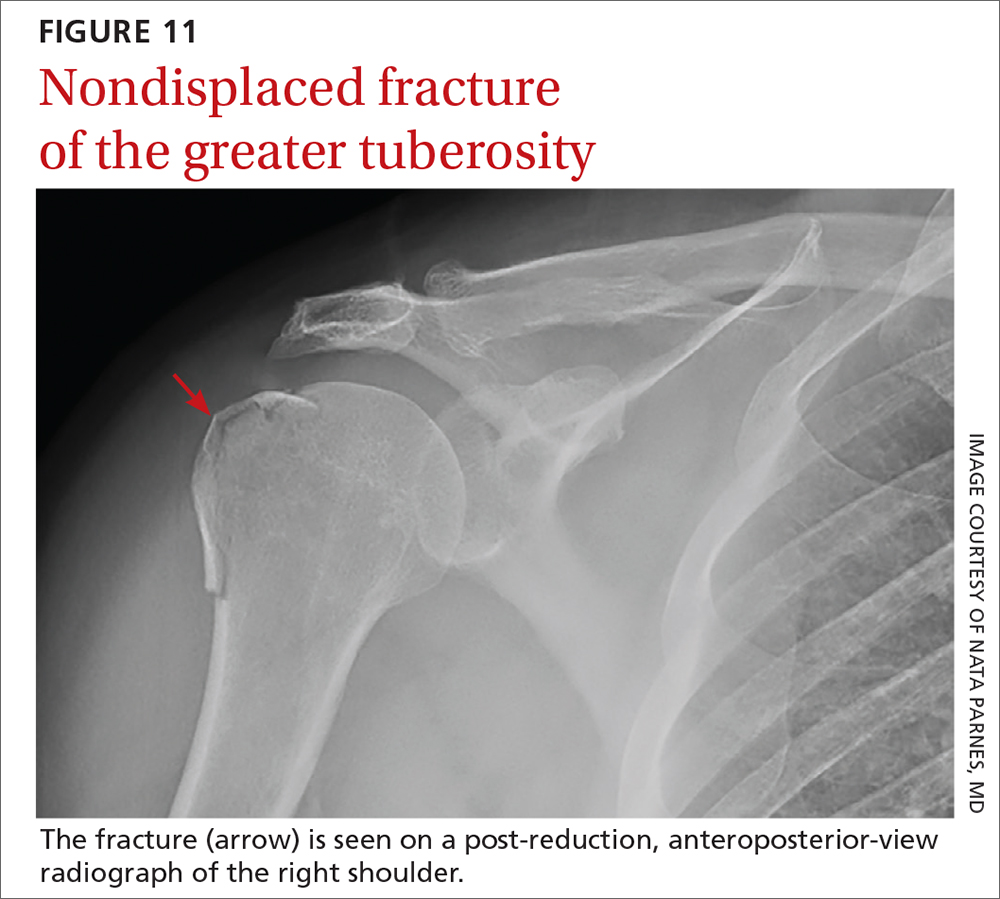
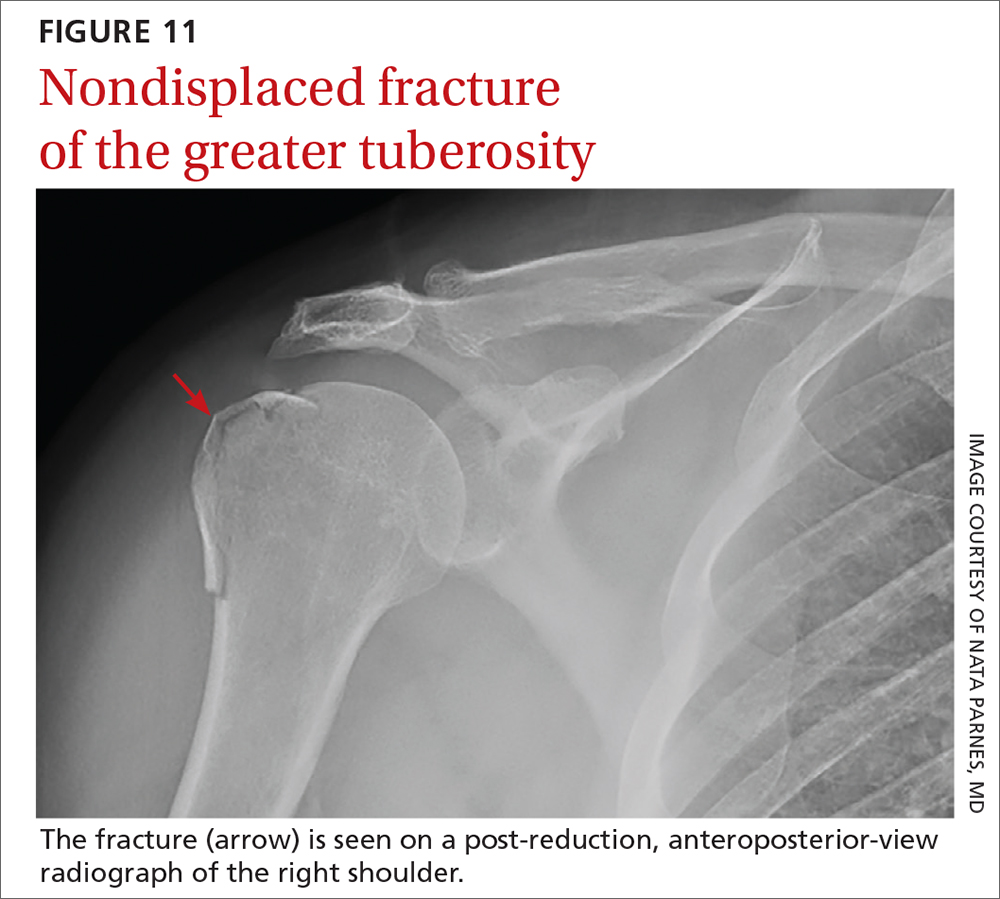
Fracture concomitant with dislocation most commonly involves the humeral neck, humeral head, greater tuberosity, or the glenoid itself.2 Clinical variables that predict a fracture associated with shoulder dislocation include23:
- first episode of dislocation
- age ≥ 40 years
- fall from higher than 1 flight of stairs
- fight or assault
- motor vehicle crash.
A computed tomography scan with 3-dimensional reconstruction can help characterize associated fracture accurately—including location, size, and displacement—and can play an important role in treatment planning and prognosis in these complicated injuries. Displaced fracture should be referred to an orthopedic surgeon. Nondisplaced fracture of the humeral head or greater tuberosity (FIGURE 11) poses less risk of complications and can be treated conservatively with 6 weeks in an arm sling, followed by physical therapy.24
Summing up
Management of shoulder dislocation must, first, be tailored to the individual and, second, account for several interactive factors—including age, direction of instability, functional demands, risk of recurrence, and associated injuries. In many patients, conservative treatment produces a favorable long-term outcome. Particularly in young, active patients with anterior shoulder instability, most surgeons consider open or arthroscopic reconstruction to be the treatment of choice.2,18
Continue to: Pre-reduction and post-reduction...
Pre-reduction and post-reduction imaging should be carefully examined for the presence of concomitant injury, which might change the preferred treatment modality appreciably.
Last, communication among emergency department providers, the primary care provider, orthopedist, radiologist, and neurologist is crucial for determining an appropriate patient-centered approach to initial and long-term management.
CORRESPONDENCE
Nata Parnes, MD, Carthage Area Hospital, 3 Bridge Street, Carthage, NY; [email protected]
1. Valencia Mora M, Ruiz Ibán MA, Heredia JD, et al. Physical exam and evaluation of the unstable shoulder. Open Orthop J. 2017;11(suppl 6, M12):946-956. doi: 10.2174/1874325001711010946
2. Khiami F, A, Loriaut P. Management of recent first-time anterior shoulder dislocation. Orthop Traumatol Surg Res. 2015;101(1 suppl):S51-S57. doi: 10.1016/j.otsr.2014.06.027
3. Antonio GE, Griffith JF, Yu AB, et al. First-time shoulder dislocation: high prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007;26:983-991. doi: 10.1002/jmri.21092
4. Carrazzone OL, Tamaoki MJS, Ambra LFM, et al. Prevalence of lesions associated with traumatic recurrent shoulder dislocation. Rev Bras Ortop. 2015;46:281-287. doi: 10.1016/S2255-4971(15)30196-8
5. Mahaffey BL, Smith PA. Shoulder instability in young athletes. Am Fam Physician. 1999;59:2773-2787.
6. Amar E, Maman E, Khashan M, et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J Shoulder Elbow Surg. 2012;21:1443-1449. doi: 10.1016/j.jse.2012.01.004
7. Jain NB, Wilcox RB 3rd, Katz JN, et al. Clinical examination of the rotator cuff. PM R. 2013;5:45-56. doi: 10.1016/j.pmrj.2012.08.019
8. Lizzio VA, Meta F, Fidai M, et al. Clinical evaluation and physical exam findings in patients with anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10:434-441. doi: 10.1007/s12178-017-9434-3
9. Farber AJ, Castillo R, Clough M, et al. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am. 2006;88:1467-1474. doi: 10.2106/JBJS.E.00594
10. Robinson CM, Shur N, Sharpe T, et al. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94:18-26. doi: 10.2106/JBJS.J.01795
11. de Laat EA, Visser CP, Coene LN, et al. Nerve lesions in primary shoulder dislocations and humeral neck fractures. A prospective clinical and EMG study. J Bone Joint Surg Br. 1994;76:381-383.
12. Avis D, Power D. Axillary nerve injury associated with glenohumeral dislocation: a review and algorithm for management. EFORT Open Rev. 2018;3:70-77. doi: 10.1302/2058-5241.3.170003
13. Drury JK, Scullion JE. Vascular complications of anterior dislocation of the shoulder. Br J Surg. 1980;67:579-581. doi: 10.1002/bjs.1800670817
14. Lafuente JLA, Marco SM, Pequerul JMG. Controversies in the management of the first time shoulder dislocation. Open Orthop J. 2017;11:1001-1010. doi: 10.2174/1874325001711011001
15. te Slaa RL, Brand R, Marti RK. A prospective arthroscopic study of acute first-time anterior shoulder dislocation in the young: a five-year follow-up study. J Shoulder Elbow Surg. 2003;12:529-534. doi: 10.1016/s1058-2746(03)00218-0
16. Kavaja L, T, Malmivaara A, et al. Treatment after traumatic shoulder dislocation: a systematic review with a network meta-analysis. Br J Sports Med. 2018;52:1498-1506. doi: 10.1136/bjsports-2017-098539
17. Krych AJ, Sousa PL, King AH, et al. The effect of cartilage injury after arthroscopic stabilization for shoulder instability. Orthopedics. 2015;38:e965-e969. doi: 10.3928/01477447-20151020-03
18. Polyzois I, Dattani R, Gupta R, et al. Traumatic first time shoulder dislocation: surgery vs non-operative treatment. Arch Bone Jt Surg. 2016;4:104-108.
19. Maman E, Harris C, White L, et al. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91:1898-1906. doi: 10.2106/JBJS.G.01335
20. Safran O, Schroeder J, Bloom R, et al. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710-714. doi: 10.1177/0363546510393944
21. Parnes N, Bartoszewski NR, Defranco MJ. Arthroscopic repair of full-thickness rotator cuff tears in active patients younger than 40 years: 2- to 5-year clinical outcomes. Orthopedics 2018;41:e52-e57. doi: 10.3928/01477447-20171114-02
22. Sofu H, Gürsu S, Koçkara N, et al. Recurrent anterior shoulder instability: review of the literature and current concepts. World J Clin Cases. 2014;2:676-682. doi: 10.12998/wjcc.v2.i11.676
23. Emond M, Le Sage N, Lavoie A, et al. Clinical factors predicting fractures associated with an anterior shoulder dislocation. Acad Emerg Med. 2004;11:853-858. doi: 10.1111/j.1553-2712.2004.tb00768.x
24. Parnes N, Jupiter JB. Fixed-angle locking plating of displaced proximal humerus fractures. Instr Course Lect. 2010;59:539-552.
The architecture of the glenohumeral joint makes it the most common large joint to become dislocated, accounting for approximately 45% of all dislocations. Anterior dislocation constitutes more than 95% of glenohumeral joint dislocations; posterior dislocation, only 2% to 5%.1,2
For the family physician, determining appropriate follow-up after emergent reduction depends on several distinct variables, which we review here; subsequent treatment might involve, as we outline, physical therapy, immobilization, surgical intervention, or a combination of several modalities. Treatment decisions can make the difference between successful rehabilitation and potential disability, particularly in typically young and active patients.
Numerous mechanisms of injury
Anterior shoulder dislocations typically occur with the affected shoulder in a position of abduction and external rotation; 90% of patients are 21 to 30 years of age, and men are affected 3 times more often than women.2 Unsurprisingly, athletes are affected most frequently, with the common sports-related mechanism of injury being either sudden pressure exerted on the abducted and externally rotated arm or a fall onto an outstretched hand with the arm elevated. Repetitive microtrauma from such sports as swimming, baseball, and volleyball can also lead to instability.
Bankart lesion. This tear of the anterior or inferior section of the labrum is the most characteristic lesion noted in anterior dislocations, found in 73% of first-time dislocations and 100% of recurrent dislocations.3,4
Hills-Sachs lesion is often associated with a Bankart lesion. The Hills-Sachs lesion is an impaction fracture of the posterolateral aspect of the humeral head resulting from its displacement over the anterior lip of the glenoid. Hill-Sachs lesions are seen in 71% of first-time and recurrent dislocations.3
Less common concomitant injuries during anterior shoulder dislocation include rupture of the rotator-cuff tendons (particularly in patients older than 40 years), glenoid and proximal humerus fractures, a tear of the superior labrum (known as a “SLAP lesion”), cartilage injury, and neurovascular injury.
Posterior instability typically occurs as a result of a strong muscle contraction, as seen in electrocution or seizure; however, it can be caused by athletic trauma, particularly in football.5 Repetitive forces exerted on the forward-flexed and internally rotated shoulder position during blocking puts football players at increased risk of posterior instability.5
Continue to: Multidirectional instability
Multidirectional instability is more frequently attributable to congenital hyperlaxity of the glenohumeral joint capsule, rather than to acute injury. However, athletes can also develop capsular laxity from repetitive microtrauma to the shoulder.5
Emergent reduction: Prompt action needed
Acute dislocation of the shoulder should be reduced as soon as possible to minimize neurovascular injury and patient discomfort. (Typically, but not always, this is done in the emergency department.) It is crucial to have effective muscle relaxation before any attempt at reduction, to minimize the risk of iatrogenic injury to bone, cartilage, tendons, and neurovascular structures.
Muscle relaxation can be facilitated with intravenous midazolam or other agents, as specified by institutional protocol. Intra-articular lidocaine injection or intravenous fentanyl is often utilized in conjunction with the sedating agent to reduce pain and further accommodate relaxation.
Anterior reduction. Any one of several techniques can be used to perform emergent reduction of anterior shoulder dislocations, all of which have demonstrated success. The Milch technique is among the least traumatic for effective reduction.6 In this technique (FIGURE 1), the patient is supine; gentle but firm downward traction is applied to the humerus at the elbow of the affected arm while the arm is in abduction and external rotation. The provider can manipulate the humeral head at that point by placing a thumb in the patient’s axilla; the arm can also be further internally rotated and adducted until reduction is achieved.
Posterior reduction of a dislocation is performed while the patient is supine, with the body stabilized. Traction is applied on the adducted and internally rotated arm in conjunction with direct pressure on the posterior aspect of the humeral head (FIGURE 2).
Continue to: Follow-up actions
Follow-up actions. Before discharging the patient after reduction of a dislocation, it is essential to:
- perform post-reduction evaluation of shoulder stability at different levels of abduction
- perform a thorough neurovascular assessment
- obtain an anteroposterior (AP) radiograph to ensure proper positioning of the glenohumeral joint.
The reduced shoulder should be immobilized in a sling. The discharge plan should include pain management for several days and a follow-up appointment in 5 to 8 days with the primary care provider2 (FIGURE 3).
Follow-up evaluation by the primary care provider
History. Prior to the initial examination at follow-up, obtain a comprehensive history that includes the nature of the injury and the direction of force that was placed on the shoulder. Determine whether the shoulder was reduced spontaneously or required manual reduction in the field or an emergency department. Note any associated injury sustained concurrently and the presence (or absence) of neck pain, numbness, tingling, or weakness in the affected arm.
Physical exam starts with thorough inspection of the affected shoulder, with comparison to the contralateral side, at rest and during shoulder motion. Palpation to reveal points of tenderness should include the anterior joint line, acromioclavicular joint, bicipital groove, subacromial space, acromion, and greater tuberosity.
Following inspection and palpation, assess active and passive range of motion in forward elevation, abduction, internal and external rotation at the side of the body, and internal and external rotation in shoulder abduction. Assessment might be limited by pain and apprehension, and should be performed within the patient’s comfortable range of motion.
Continue to: Once range of motion...
Once range of motion is determined, assess7:
- muscle power of the rotator cuff in abduction (for the supraspinatus muscle)
- resisted external rotation at the side of the body (the infraspinatus)
- resisted external rotation in abduction > 60° (the teres minor)
- resisted internal rotation (the subscapularis).
Specific tests for shoulder laxity and stability
It is important during the primary care follow-up examination to differentiate true instability and shoulder hyperlaxity, particularly in young, flexible patients (TABLE). Many of these patients present with painless hypermobility of the shoulder without true injury to the labrum or ligamentous structures. It might appear to the patient, or to family, that the shoulder is subluxating; however, the humeral head returns to a centered position on the glenoid in a hypermobile state—typically, without pain. Actual shoulder instability is defined as loss of the ability of the humeral head to re-center, accompanied by pain—pathology that is frequently associated with damage to the capsulolabral complex.
The load and shift test is used to assess anterior and posterior laxity. The patient is seated, and the forearm is allowed to rest on the thigh. Examination is performed using 1 hand to press anteriorly or posteriorly on the humeral head; the other hand is simultaneously positioned on the joint line to feel movement of the humeral head in relation to the glenoid (FIGURE 4).
The apprehension test is a common maneuver used to assess anterior shoulder instability. It is performed by positioning the affected arm to 90° external rotation and then elevating it to 90° abduction. Although this maneuver can be performed with the patient upright, it is beneficial to have them supine, to more easily control the arm (FIGURE 5). A positive test is noted when the patient reports a sensation of impending instability (apprehension), rather than pain alone.
Relocation test. When the apprehension test is positive, the supine position can be exploited to further perform the relocation test, in 2 stages (FIGURE 6):
- Apply a posteriorly directed force on the humeral head, which stabilizes the shoulder and typically alleviates symptoms.
- Release pressure quickly from the humeral head to assess recurrence of pain and apprehension as the humeral head snaps back against the anterior labrum.
Continue to: Combined, apprehension and relocation...
Combined, apprehension and relocation tests to identify anterior shoulder instability have been shown to significantly improve specificity while maintaining sensitivity.8
The posterior apprehension test is used to assess posterior instability. The patient is supine; the affected arm is placed in flexion, adduction, and internal rotation; and posterior pressure is applied (FIGURE 7). A positive test is noted when pain is reported at the posterior aspect of the shoulder. Clicking might be noted as the humeral head dislocates rearward.1
Sulcus sign. Multidirectional instability is elicited using the sulcus sign. While the patient is seated upright, arms resting at their sides, a direct downward pull at elbow level will, when positive, reveal a depression (sulcus) at the lateral aspect of the affected shoulder as the humeral head translates inferiorly (FIGURE 8). A positive sulcus sign is documented in 3 grades, according to the amount of translation1:
- Grade I: < 1 cm
- Grade II: 1-2 cm
- Grade III: > 2 cm.
Neurovascular status should be verified at every physical evaluation, with motor and sensory function tested in the axillary, musculocutaneous, median, radial, and ulnar nerve distributions. If nerve injury is suspected, electromyography and nerve-conduction testing is indicated.9-13 Vascular compromise is much less common but equally important to assess.11
Use of imaging
Post-reduction radiographs, including internal and external AP—and especially axillary—views are invaluable. Not only do they help to ensure reduction, but they also help to assess for fracture. A magnetic resonance imaging (MRI) arthrogram is the preferred imaging modality if a labral tear is suspected (FIGURE 9). Other concomitant shoulder injuries, such as subtle bone fracture, rotator cuff tear, and biceps pathology can also be reliably diagnosed with noncontrast MRI.
Continue to: Roadmap for treatment
Roadmap for treatment
The rate of recurrence after a first anterior shoulder dislocation is strongly associated with a person’s age and level of activity. Active patients younger than 20 years have a 92% to 96% recurrence rate14; patients 20 to 40 years, 25% to 48%; and patients older than 40 years, < 10%.15
Young, athletic patients who are treated nonoperatively are left at an unacceptably high risk of recurrence, leading to progressive damage to bony and soft-tissue structures.16,17 Surgical labral repair after a first-time anterior dislocation produced improved outcomes in terms of recurrent dislocation (7.9%), compared to outcomes after nonsurgical treatment (52.9%),14 and has been associated with a lower incidence of future glenohumeral osteoarthritis.18 For those reasons, we recommend referral to an orthopedic surgeon for all patients younger than 20 years who sustain an anterior shoulder dislocation.
Patients older than 20 years who do not have concomitant shoulder injury, and who demonstrate full strength in abduction, external rotation, and internal rotation of the shoulder on clinical examination, have a low probability of associated rotator-cuff tear. They can be immobilized in a sling for 1 to 3 weeks, followed by a 6 to 12–week regimen of physical therapy.
Concomitant tear of the rotator cuff. Weakness on examination requires MRI or a magnetic resonance arthrogram for evaluation of associated rotator-cuff tear. A tear identified on MRI should be referred to an orthopedic surgeon because timely repair can be crucial to attaining best outcomes. Conservative treatment of traumatic full-tendon rotator-cuff tear is associated with poor results, progression in the size of the tear, and advancement of muscle atrophy.19,20 For patients younger than 40 years, arthroscopic rotator-cuff repair, with or without labral repair, produces excellent clinical outcomes, carries a low risk of complications, and results in a > 95% rate of return to a preoperative level of recreational and job activities.21
Patients who demonstrate weakness of the rotator-cuff muscles on examination, but who do not have a tear noted on MRI, should be evaluated by electromyography and nerve-conduction testing to assess nerve injury as an alternative cause of weakness.10,11 If a neurologic deficit is found on nerve-conduction testing, the patient should be referred for neurologic evaluation.10
Continue to: Patients with negative findings...
Patients with negative findings on MRI and nerve-conduction studies should be offered physical therapy. Patients with recurrent anterior shoulder dislocation should be referred to an orthopedic surgeon for surgical repair. Frequently, improper or delayed treatment with chronic instability results in degenerative arthropathy of the joint22 (FIGURE 10).

Posterior and multidirectional instability can typically be treated conservatively; however, whereas posterior dislocation typically must be immobilized for 3 to 6 weeks post reduction, multidirectional instability does not require immobilization. Instead, physical therapy should start as soon as possible. In these cases, recurrent dislocation or subluxation that persists after conservative treatment should be referred for possible surgical intervention.5
Instability with associated fracture
Fracture concomitant with dislocation most commonly involves the humeral neck, humeral head, greater tuberosity, or the glenoid itself.2 Clinical variables that predict a fracture associated with shoulder dislocation include23:
- first episode of dislocation
- age ≥ 40 years
- fall from higher than 1 flight of stairs
- fight or assault
- motor vehicle crash.
A computed tomography scan with 3-dimensional reconstruction can help characterize associated fracture accurately—including location, size, and displacement—and can play an important role in treatment planning and prognosis in these complicated injuries. Displaced fracture should be referred to an orthopedic surgeon. Nondisplaced fracture of the humeral head or greater tuberosity (FIGURE 11) poses less risk of complications and can be treated conservatively with 6 weeks in an arm sling, followed by physical therapy.24
Summing up
Management of shoulder dislocation must, first, be tailored to the individual and, second, account for several interactive factors—including age, direction of instability, functional demands, risk of recurrence, and associated injuries. In many patients, conservative treatment produces a favorable long-term outcome. Particularly in young, active patients with anterior shoulder instability, most surgeons consider open or arthroscopic reconstruction to be the treatment of choice.2,18
Continue to: Pre-reduction and post-reduction...
Pre-reduction and post-reduction imaging should be carefully examined for the presence of concomitant injury, which might change the preferred treatment modality appreciably.
Last, communication among emergency department providers, the primary care provider, orthopedist, radiologist, and neurologist is crucial for determining an appropriate patient-centered approach to initial and long-term management.
CORRESPONDENCE
Nata Parnes, MD, Carthage Area Hospital, 3 Bridge Street, Carthage, NY; [email protected]
The architecture of the glenohumeral joint makes it the most common large joint to become dislocated, accounting for approximately 45% of all dislocations. Anterior dislocation constitutes more than 95% of glenohumeral joint dislocations; posterior dislocation, only 2% to 5%.1,2
For the family physician, determining appropriate follow-up after emergent reduction depends on several distinct variables, which we review here; subsequent treatment might involve, as we outline, physical therapy, immobilization, surgical intervention, or a combination of several modalities. Treatment decisions can make the difference between successful rehabilitation and potential disability, particularly in typically young and active patients.
Numerous mechanisms of injury
Anterior shoulder dislocations typically occur with the affected shoulder in a position of abduction and external rotation; 90% of patients are 21 to 30 years of age, and men are affected 3 times more often than women.2 Unsurprisingly, athletes are affected most frequently, with the common sports-related mechanism of injury being either sudden pressure exerted on the abducted and externally rotated arm or a fall onto an outstretched hand with the arm elevated. Repetitive microtrauma from such sports as swimming, baseball, and volleyball can also lead to instability.
Bankart lesion. This tear of the anterior or inferior section of the labrum is the most characteristic lesion noted in anterior dislocations, found in 73% of first-time dislocations and 100% of recurrent dislocations.3,4
Hills-Sachs lesion is often associated with a Bankart lesion. The Hills-Sachs lesion is an impaction fracture of the posterolateral aspect of the humeral head resulting from its displacement over the anterior lip of the glenoid. Hill-Sachs lesions are seen in 71% of first-time and recurrent dislocations.3
Less common concomitant injuries during anterior shoulder dislocation include rupture of the rotator-cuff tendons (particularly in patients older than 40 years), glenoid and proximal humerus fractures, a tear of the superior labrum (known as a “SLAP lesion”), cartilage injury, and neurovascular injury.
Posterior instability typically occurs as a result of a strong muscle contraction, as seen in electrocution or seizure; however, it can be caused by athletic trauma, particularly in football.5 Repetitive forces exerted on the forward-flexed and internally rotated shoulder position during blocking puts football players at increased risk of posterior instability.5
Continue to: Multidirectional instability
Multidirectional instability is more frequently attributable to congenital hyperlaxity of the glenohumeral joint capsule, rather than to acute injury. However, athletes can also develop capsular laxity from repetitive microtrauma to the shoulder.5
Emergent reduction: Prompt action needed
Acute dislocation of the shoulder should be reduced as soon as possible to minimize neurovascular injury and patient discomfort. (Typically, but not always, this is done in the emergency department.) It is crucial to have effective muscle relaxation before any attempt at reduction, to minimize the risk of iatrogenic injury to bone, cartilage, tendons, and neurovascular structures.
Muscle relaxation can be facilitated with intravenous midazolam or other agents, as specified by institutional protocol. Intra-articular lidocaine injection or intravenous fentanyl is often utilized in conjunction with the sedating agent to reduce pain and further accommodate relaxation.
Anterior reduction. Any one of several techniques can be used to perform emergent reduction of anterior shoulder dislocations, all of which have demonstrated success. The Milch technique is among the least traumatic for effective reduction.6 In this technique (FIGURE 1), the patient is supine; gentle but firm downward traction is applied to the humerus at the elbow of the affected arm while the arm is in abduction and external rotation. The provider can manipulate the humeral head at that point by placing a thumb in the patient’s axilla; the arm can also be further internally rotated and adducted until reduction is achieved.
Posterior reduction of a dislocation is performed while the patient is supine, with the body stabilized. Traction is applied on the adducted and internally rotated arm in conjunction with direct pressure on the posterior aspect of the humeral head (FIGURE 2).
Continue to: Follow-up actions
Follow-up actions. Before discharging the patient after reduction of a dislocation, it is essential to:
- perform post-reduction evaluation of shoulder stability at different levels of abduction
- perform a thorough neurovascular assessment
- obtain an anteroposterior (AP) radiograph to ensure proper positioning of the glenohumeral joint.
The reduced shoulder should be immobilized in a sling. The discharge plan should include pain management for several days and a follow-up appointment in 5 to 8 days with the primary care provider2 (FIGURE 3).
Follow-up evaluation by the primary care provider
History. Prior to the initial examination at follow-up, obtain a comprehensive history that includes the nature of the injury and the direction of force that was placed on the shoulder. Determine whether the shoulder was reduced spontaneously or required manual reduction in the field or an emergency department. Note any associated injury sustained concurrently and the presence (or absence) of neck pain, numbness, tingling, or weakness in the affected arm.
Physical exam starts with thorough inspection of the affected shoulder, with comparison to the contralateral side, at rest and during shoulder motion. Palpation to reveal points of tenderness should include the anterior joint line, acromioclavicular joint, bicipital groove, subacromial space, acromion, and greater tuberosity.
Following inspection and palpation, assess active and passive range of motion in forward elevation, abduction, internal and external rotation at the side of the body, and internal and external rotation in shoulder abduction. Assessment might be limited by pain and apprehension, and should be performed within the patient’s comfortable range of motion.
Continue to: Once range of motion...
Once range of motion is determined, assess7:
- muscle power of the rotator cuff in abduction (for the supraspinatus muscle)
- resisted external rotation at the side of the body (the infraspinatus)
- resisted external rotation in abduction > 60° (the teres minor)
- resisted internal rotation (the subscapularis).
Specific tests for shoulder laxity and stability
It is important during the primary care follow-up examination to differentiate true instability and shoulder hyperlaxity, particularly in young, flexible patients (TABLE). Many of these patients present with painless hypermobility of the shoulder without true injury to the labrum or ligamentous structures. It might appear to the patient, or to family, that the shoulder is subluxating; however, the humeral head returns to a centered position on the glenoid in a hypermobile state—typically, without pain. Actual shoulder instability is defined as loss of the ability of the humeral head to re-center, accompanied by pain—pathology that is frequently associated with damage to the capsulolabral complex.
The load and shift test is used to assess anterior and posterior laxity. The patient is seated, and the forearm is allowed to rest on the thigh. Examination is performed using 1 hand to press anteriorly or posteriorly on the humeral head; the other hand is simultaneously positioned on the joint line to feel movement of the humeral head in relation to the glenoid (FIGURE 4).
The apprehension test is a common maneuver used to assess anterior shoulder instability. It is performed by positioning the affected arm to 90° external rotation and then elevating it to 90° abduction. Although this maneuver can be performed with the patient upright, it is beneficial to have them supine, to more easily control the arm (FIGURE 5). A positive test is noted when the patient reports a sensation of impending instability (apprehension), rather than pain alone.
Relocation test. When the apprehension test is positive, the supine position can be exploited to further perform the relocation test, in 2 stages (FIGURE 6):
- Apply a posteriorly directed force on the humeral head, which stabilizes the shoulder and typically alleviates symptoms.
- Release pressure quickly from the humeral head to assess recurrence of pain and apprehension as the humeral head snaps back against the anterior labrum.
Continue to: Combined, apprehension and relocation...
Combined, apprehension and relocation tests to identify anterior shoulder instability have been shown to significantly improve specificity while maintaining sensitivity.8
The posterior apprehension test is used to assess posterior instability. The patient is supine; the affected arm is placed in flexion, adduction, and internal rotation; and posterior pressure is applied (FIGURE 7). A positive test is noted when pain is reported at the posterior aspect of the shoulder. Clicking might be noted as the humeral head dislocates rearward.1
Sulcus sign. Multidirectional instability is elicited using the sulcus sign. While the patient is seated upright, arms resting at their sides, a direct downward pull at elbow level will, when positive, reveal a depression (sulcus) at the lateral aspect of the affected shoulder as the humeral head translates inferiorly (FIGURE 8). A positive sulcus sign is documented in 3 grades, according to the amount of translation1:
- Grade I: < 1 cm
- Grade II: 1-2 cm
- Grade III: > 2 cm.
Neurovascular status should be verified at every physical evaluation, with motor and sensory function tested in the axillary, musculocutaneous, median, radial, and ulnar nerve distributions. If nerve injury is suspected, electromyography and nerve-conduction testing is indicated.9-13 Vascular compromise is much less common but equally important to assess.11
Use of imaging
Post-reduction radiographs, including internal and external AP—and especially axillary—views are invaluable. Not only do they help to ensure reduction, but they also help to assess for fracture. A magnetic resonance imaging (MRI) arthrogram is the preferred imaging modality if a labral tear is suspected (FIGURE 9). Other concomitant shoulder injuries, such as subtle bone fracture, rotator cuff tear, and biceps pathology can also be reliably diagnosed with noncontrast MRI.
Continue to: Roadmap for treatment
Roadmap for treatment
The rate of recurrence after a first anterior shoulder dislocation is strongly associated with a person’s age and level of activity. Active patients younger than 20 years have a 92% to 96% recurrence rate14; patients 20 to 40 years, 25% to 48%; and patients older than 40 years, < 10%.15
Young, athletic patients who are treated nonoperatively are left at an unacceptably high risk of recurrence, leading to progressive damage to bony and soft-tissue structures.16,17 Surgical labral repair after a first-time anterior dislocation produced improved outcomes in terms of recurrent dislocation (7.9%), compared to outcomes after nonsurgical treatment (52.9%),14 and has been associated with a lower incidence of future glenohumeral osteoarthritis.18 For those reasons, we recommend referral to an orthopedic surgeon for all patients younger than 20 years who sustain an anterior shoulder dislocation.
Patients older than 20 years who do not have concomitant shoulder injury, and who demonstrate full strength in abduction, external rotation, and internal rotation of the shoulder on clinical examination, have a low probability of associated rotator-cuff tear. They can be immobilized in a sling for 1 to 3 weeks, followed by a 6 to 12–week regimen of physical therapy.
Concomitant tear of the rotator cuff. Weakness on examination requires MRI or a magnetic resonance arthrogram for evaluation of associated rotator-cuff tear. A tear identified on MRI should be referred to an orthopedic surgeon because timely repair can be crucial to attaining best outcomes. Conservative treatment of traumatic full-tendon rotator-cuff tear is associated with poor results, progression in the size of the tear, and advancement of muscle atrophy.19,20 For patients younger than 40 years, arthroscopic rotator-cuff repair, with or without labral repair, produces excellent clinical outcomes, carries a low risk of complications, and results in a > 95% rate of return to a preoperative level of recreational and job activities.21
Patients who demonstrate weakness of the rotator-cuff muscles on examination, but who do not have a tear noted on MRI, should be evaluated by electromyography and nerve-conduction testing to assess nerve injury as an alternative cause of weakness.10,11 If a neurologic deficit is found on nerve-conduction testing, the patient should be referred for neurologic evaluation.10
Continue to: Patients with negative findings...
Patients with negative findings on MRI and nerve-conduction studies should be offered physical therapy. Patients with recurrent anterior shoulder dislocation should be referred to an orthopedic surgeon for surgical repair. Frequently, improper or delayed treatment with chronic instability results in degenerative arthropathy of the joint22 (FIGURE 10).

Posterior and multidirectional instability can typically be treated conservatively; however, whereas posterior dislocation typically must be immobilized for 3 to 6 weeks post reduction, multidirectional instability does not require immobilization. Instead, physical therapy should start as soon as possible. In these cases, recurrent dislocation or subluxation that persists after conservative treatment should be referred for possible surgical intervention.5
Instability with associated fracture
Fracture concomitant with dislocation most commonly involves the humeral neck, humeral head, greater tuberosity, or the glenoid itself.2 Clinical variables that predict a fracture associated with shoulder dislocation include23:
- first episode of dislocation
- age ≥ 40 years
- fall from higher than 1 flight of stairs
- fight or assault
- motor vehicle crash.
A computed tomography scan with 3-dimensional reconstruction can help characterize associated fracture accurately—including location, size, and displacement—and can play an important role in treatment planning and prognosis in these complicated injuries. Displaced fracture should be referred to an orthopedic surgeon. Nondisplaced fracture of the humeral head or greater tuberosity (FIGURE 11) poses less risk of complications and can be treated conservatively with 6 weeks in an arm sling, followed by physical therapy.24
Summing up
Management of shoulder dislocation must, first, be tailored to the individual and, second, account for several interactive factors—including age, direction of instability, functional demands, risk of recurrence, and associated injuries. In many patients, conservative treatment produces a favorable long-term outcome. Particularly in young, active patients with anterior shoulder instability, most surgeons consider open or arthroscopic reconstruction to be the treatment of choice.2,18
Continue to: Pre-reduction and post-reduction...
Pre-reduction and post-reduction imaging should be carefully examined for the presence of concomitant injury, which might change the preferred treatment modality appreciably.
Last, communication among emergency department providers, the primary care provider, orthopedist, radiologist, and neurologist is crucial for determining an appropriate patient-centered approach to initial and long-term management.
CORRESPONDENCE
Nata Parnes, MD, Carthage Area Hospital, 3 Bridge Street, Carthage, NY; [email protected]
1. Valencia Mora M, Ruiz Ibán MA, Heredia JD, et al. Physical exam and evaluation of the unstable shoulder. Open Orthop J. 2017;11(suppl 6, M12):946-956. doi: 10.2174/1874325001711010946
2. Khiami F, A, Loriaut P. Management of recent first-time anterior shoulder dislocation. Orthop Traumatol Surg Res. 2015;101(1 suppl):S51-S57. doi: 10.1016/j.otsr.2014.06.027
3. Antonio GE, Griffith JF, Yu AB, et al. First-time shoulder dislocation: high prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007;26:983-991. doi: 10.1002/jmri.21092
4. Carrazzone OL, Tamaoki MJS, Ambra LFM, et al. Prevalence of lesions associated with traumatic recurrent shoulder dislocation. Rev Bras Ortop. 2015;46:281-287. doi: 10.1016/S2255-4971(15)30196-8
5. Mahaffey BL, Smith PA. Shoulder instability in young athletes. Am Fam Physician. 1999;59:2773-2787.
6. Amar E, Maman E, Khashan M, et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J Shoulder Elbow Surg. 2012;21:1443-1449. doi: 10.1016/j.jse.2012.01.004
7. Jain NB, Wilcox RB 3rd, Katz JN, et al. Clinical examination of the rotator cuff. PM R. 2013;5:45-56. doi: 10.1016/j.pmrj.2012.08.019
8. Lizzio VA, Meta F, Fidai M, et al. Clinical evaluation and physical exam findings in patients with anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10:434-441. doi: 10.1007/s12178-017-9434-3
9. Farber AJ, Castillo R, Clough M, et al. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am. 2006;88:1467-1474. doi: 10.2106/JBJS.E.00594
10. Robinson CM, Shur N, Sharpe T, et al. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94:18-26. doi: 10.2106/JBJS.J.01795
11. de Laat EA, Visser CP, Coene LN, et al. Nerve lesions in primary shoulder dislocations and humeral neck fractures. A prospective clinical and EMG study. J Bone Joint Surg Br. 1994;76:381-383.
12. Avis D, Power D. Axillary nerve injury associated with glenohumeral dislocation: a review and algorithm for management. EFORT Open Rev. 2018;3:70-77. doi: 10.1302/2058-5241.3.170003
13. Drury JK, Scullion JE. Vascular complications of anterior dislocation of the shoulder. Br J Surg. 1980;67:579-581. doi: 10.1002/bjs.1800670817
14. Lafuente JLA, Marco SM, Pequerul JMG. Controversies in the management of the first time shoulder dislocation. Open Orthop J. 2017;11:1001-1010. doi: 10.2174/1874325001711011001
15. te Slaa RL, Brand R, Marti RK. A prospective arthroscopic study of acute first-time anterior shoulder dislocation in the young: a five-year follow-up study. J Shoulder Elbow Surg. 2003;12:529-534. doi: 10.1016/s1058-2746(03)00218-0
16. Kavaja L, T, Malmivaara A, et al. Treatment after traumatic shoulder dislocation: a systematic review with a network meta-analysis. Br J Sports Med. 2018;52:1498-1506. doi: 10.1136/bjsports-2017-098539
17. Krych AJ, Sousa PL, King AH, et al. The effect of cartilage injury after arthroscopic stabilization for shoulder instability. Orthopedics. 2015;38:e965-e969. doi: 10.3928/01477447-20151020-03
18. Polyzois I, Dattani R, Gupta R, et al. Traumatic first time shoulder dislocation: surgery vs non-operative treatment. Arch Bone Jt Surg. 2016;4:104-108.
19. Maman E, Harris C, White L, et al. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91:1898-1906. doi: 10.2106/JBJS.G.01335
20. Safran O, Schroeder J, Bloom R, et al. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710-714. doi: 10.1177/0363546510393944
21. Parnes N, Bartoszewski NR, Defranco MJ. Arthroscopic repair of full-thickness rotator cuff tears in active patients younger than 40 years: 2- to 5-year clinical outcomes. Orthopedics 2018;41:e52-e57. doi: 10.3928/01477447-20171114-02
22. Sofu H, Gürsu S, Koçkara N, et al. Recurrent anterior shoulder instability: review of the literature and current concepts. World J Clin Cases. 2014;2:676-682. doi: 10.12998/wjcc.v2.i11.676
23. Emond M, Le Sage N, Lavoie A, et al. Clinical factors predicting fractures associated with an anterior shoulder dislocation. Acad Emerg Med. 2004;11:853-858. doi: 10.1111/j.1553-2712.2004.tb00768.x
24. Parnes N, Jupiter JB. Fixed-angle locking plating of displaced proximal humerus fractures. Instr Course Lect. 2010;59:539-552.
1. Valencia Mora M, Ruiz Ibán MA, Heredia JD, et al. Physical exam and evaluation of the unstable shoulder. Open Orthop J. 2017;11(suppl 6, M12):946-956. doi: 10.2174/1874325001711010946
2. Khiami F, A, Loriaut P. Management of recent first-time anterior shoulder dislocation. Orthop Traumatol Surg Res. 2015;101(1 suppl):S51-S57. doi: 10.1016/j.otsr.2014.06.027
3. Antonio GE, Griffith JF, Yu AB, et al. First-time shoulder dislocation: high prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007;26:983-991. doi: 10.1002/jmri.21092
4. Carrazzone OL, Tamaoki MJS, Ambra LFM, et al. Prevalence of lesions associated with traumatic recurrent shoulder dislocation. Rev Bras Ortop. 2015;46:281-287. doi: 10.1016/S2255-4971(15)30196-8
5. Mahaffey BL, Smith PA. Shoulder instability in young athletes. Am Fam Physician. 1999;59:2773-2787.
6. Amar E, Maman E, Khashan M, et al. Milch versus Stimson technique for nonsedated reduction of anterior shoulder dislocation: a prospective randomized trial and analysis of factors affecting success. J Shoulder Elbow Surg. 2012;21:1443-1449. doi: 10.1016/j.jse.2012.01.004
7. Jain NB, Wilcox RB 3rd, Katz JN, et al. Clinical examination of the rotator cuff. PM R. 2013;5:45-56. doi: 10.1016/j.pmrj.2012.08.019
8. Lizzio VA, Meta F, Fidai M, et al. Clinical evaluation and physical exam findings in patients with anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10:434-441. doi: 10.1007/s12178-017-9434-3
9. Farber AJ, Castillo R, Clough M, et al. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am. 2006;88:1467-1474. doi: 10.2106/JBJS.E.00594
10. Robinson CM, Shur N, Sharpe T, et al. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94:18-26. doi: 10.2106/JBJS.J.01795
11. de Laat EA, Visser CP, Coene LN, et al. Nerve lesions in primary shoulder dislocations and humeral neck fractures. A prospective clinical and EMG study. J Bone Joint Surg Br. 1994;76:381-383.
12. Avis D, Power D. Axillary nerve injury associated with glenohumeral dislocation: a review and algorithm for management. EFORT Open Rev. 2018;3:70-77. doi: 10.1302/2058-5241.3.170003
13. Drury JK, Scullion JE. Vascular complications of anterior dislocation of the shoulder. Br J Surg. 1980;67:579-581. doi: 10.1002/bjs.1800670817
14. Lafuente JLA, Marco SM, Pequerul JMG. Controversies in the management of the first time shoulder dislocation. Open Orthop J. 2017;11:1001-1010. doi: 10.2174/1874325001711011001
15. te Slaa RL, Brand R, Marti RK. A prospective arthroscopic study of acute first-time anterior shoulder dislocation in the young: a five-year follow-up study. J Shoulder Elbow Surg. 2003;12:529-534. doi: 10.1016/s1058-2746(03)00218-0
16. Kavaja L, T, Malmivaara A, et al. Treatment after traumatic shoulder dislocation: a systematic review with a network meta-analysis. Br J Sports Med. 2018;52:1498-1506. doi: 10.1136/bjsports-2017-098539
17. Krych AJ, Sousa PL, King AH, et al. The effect of cartilage injury after arthroscopic stabilization for shoulder instability. Orthopedics. 2015;38:e965-e969. doi: 10.3928/01477447-20151020-03
18. Polyzois I, Dattani R, Gupta R, et al. Traumatic first time shoulder dislocation: surgery vs non-operative treatment. Arch Bone Jt Surg. 2016;4:104-108.
19. Maman E, Harris C, White L, et al. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91:1898-1906. doi: 10.2106/JBJS.G.01335
20. Safran O, Schroeder J, Bloom R, et al. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710-714. doi: 10.1177/0363546510393944
21. Parnes N, Bartoszewski NR, Defranco MJ. Arthroscopic repair of full-thickness rotator cuff tears in active patients younger than 40 years: 2- to 5-year clinical outcomes. Orthopedics 2018;41:e52-e57. doi: 10.3928/01477447-20171114-02
22. Sofu H, Gürsu S, Koçkara N, et al. Recurrent anterior shoulder instability: review of the literature and current concepts. World J Clin Cases. 2014;2:676-682. doi: 10.12998/wjcc.v2.i11.676
23. Emond M, Le Sage N, Lavoie A, et al. Clinical factors predicting fractures associated with an anterior shoulder dislocation. Acad Emerg Med. 2004;11:853-858. doi: 10.1111/j.1553-2712.2004.tb00768.x
24. Parnes N, Jupiter JB. Fixed-angle locking plating of displaced proximal humerus fractures. Instr Course Lect. 2010;59:539-552.
PRACTICE RECOMMENDATIONS
› Refer first-time dislocation in patients younger than 20 years or who have a displaced fracture to an orthopedic surgeon. A
› Order magnetic resonance imaging (MRI) for all patients with a suspected rotator cuff tear. A
› Send patients with weakness of the rotator cuff—but no tear on MRI—for evaluation by electromyography and nerve-conduction studies. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series