User login
Advocates of the liberal use of episiotomy have hypothesized that the procedure has many benefits, including:
Most studies do not provide strong support for these claims.
Utilization has declined. Over the past decades, the liberal use of episiotomy has given way to a pattern of practice that emphasizes restricted use.1-4 In the 1980s, in the United States, episiotomy incisions were performed in approximately 40% of vaginal deliveries5; in 2010, the rate at most obstetric facilities was <10%.
When the episiotomy rate was 40%, a median incision made sense: A very limited incision was sufficient to provide extra room for the passage of an average-sized fetus through an average-sized birth outlet. With the rate below 10% today, however, the likelihood is greater that episiotomy is being reserved for cases in which a significant clinical problem exists—most often, mismatch between the birth outlet and fetal size—and the appropriateness of median episiotomy comes into question. By restricting episiotomy incisions to the most complex clinical situations, the risk is greater that the episiotomy will be associated with a severe perineal laceration, such as a laceration of the anal sphincter (third-degree) or the rectal mucosa (fourth-degree)—or both.
A spotlight on severe lacerations. Over the past decade, practitioners of obstetrics have refocused attention on reducing the risk of third- and fourth-degree perineal lacerations—severe injuries that are associated with significant maternal morbidity. Clinical variables that increase the risk of a third- or fourth-degree perineal laceration include:
- nulliparity
- forceps delivery
- median episiotomy
- macrosomia
- persistent occiput posterior position.6
Many studies have reported that a median episiotomy is associated with a higher rate of third- and fourth-degree lacerations than either 1) deliveries without an episiotomy or 2) deliveries with a mediolateral episiotomy.1,7-9 With the modern practice of reserving episiotomy for the most complex vaginal deliveries and renewed attention to reducing the rate of third- and fourth-degree lacerations, the time has come for us to stop using the median episiotomy and switch to using a mediolateral episiotomy incision.
STOP: using the median episiotomy
Numerous studies have reported that the median episiotomy is associated with an increased risk of laceration of the anal sphincter (third-degree) and rectal mucosa (fourth-degree), compared with mediolateral episiotomy.
Randomized study of incisions. In a clinical trial, 407 nulliparous women were randomized to median or mediolateral episiotomy incision.10 The incisions were made at a time during the second stage of labor that was judged by the clinician to be most appropriate—typically immediately before delivery of the fetal head.
To perform mediolateral episiotomy, clinicians in this study used a pair of straight scissors to make an incision that began in the midline and was carried to the right side of the anal sphincter for 3 to 4 cm, at an angle >45°. Median episiotomy was performed by incision of the perineal tissues for 2 to 3 cm, directly in the midline.
The clinical protocol resulted in more women assigned to mediolateral episiotomy (n=244) than to the midline episiotomy (n=159), but the two groups were well matched on such major clinical characteristics as age, gestational age at delivery, duration of the second stage, rate of operative delivery, and anesthesia used.
Compared to what was found with mediolateral episiotomy, the median episiotomy incision was associated with a statistically significant increase in the frequency of complete third-degree tears (median, 6.1%; mediolateral, 1.6%) and fourth-degree tears (median, 5.5%; mediolateral, 0.4%).
Further comparisons. Many clinicians avoid mediolateral episiotomy. Why? Because, compared with median episiotomy, a mediolateral incision is believed to be associated with greater postpartum pain, increased severity and incidence of dyspareunia, and more disfiguring scars.11
But subjects in the randomized trial that I just described, in which mediolateral and median episiotomy were compared,10 reported postpartum pain, postpartum use of pain medicine, and impaired bowel function at similar rates regardless of the type of incision.
Investigators determined that, in the first month after delivery, more women who had a median episiotomy resumed vaginal intercourse (18.1%, compared to 6.3% who had a mediolateral incision). In the second month after delivery, however, women in both the median and mediolateral episiotomy groups reported similar resumption of sexual intercourse (median, 82.8%; mediolateral, 80.8%).
Three months after delivery, physical examination determined that a higher percentage of subjects in the median incision group (43%) had what was judged to be a “good” appearance to the scar (compared to 27% in the mediolateral group). Last, subjects in the median group had a higher rate of perineal laxity (7%) than did women in the mediolateral group (1.6%).
START: using a mediolateral incision when episiotomy is necessary
Reducing the risk of severe perineal laceration is an important clinical goal because severe lacerations are associated with significant morbidity. In a study of 390 women who had a fourth-degree perineal laceration, 5% had significant complications that, in most cases, required additional surgery.12 Furthermore, in that study:
- 1.8% of women had a breakdown of the repair
- 2.8% had infection plus breakdown of the repair
- 0.8% had infection only.
In another study, 31% of women who sustained a fourth-degree laceration reported poor bowel control postpartum.7
Given the focus on reducing the rate of severe perineal laceration, I recommend that, in most cases, you reduce the use of median episiotomy and increase the use of mediolateral episiotomy.
Use a mediolateral incision for episiotomy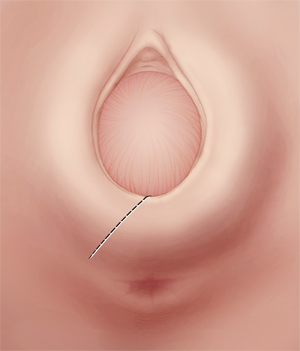
Make the incision at a 45°-angle; incisions made at >35° angle are associated with less of a risk of severe perineal laceration. Avoid using chromic sutures; rapid-absorption polyglactin 910 suture might offer better healing.
Mediolateral episiotomy: Technique
Begin the mediolateral episiotomy in the midline or slightly lateral to the midline (see the FIGURE). Insert two fingers into the vagina to distend the tissue of the birth outlet; using a pair of sharp, straight scissors, cut an incision 4 or 5 cm long at a 45° angle, directing it toward the ipsilateral ischial tuberosity. In most women, this incision cuts a portion of the bulbospongiosus muscle and, occasionally, reaches the ischioanal fossa.
Proper angle is key. The angle of the mediolateral episiotomy, in relation to the midline, is an important variable that influences the possibility that the patient will have a severe perineal laceration. Most experts recommend that the angle of the incision be at least 45° from the midline. If you use a shallow angle (<35°) from the midline to perform mediolateral episiotomy, you increase the risk of a severe perineal laceration, compared with incisions made at an angle >35° degrees from the midline (again, the FIGURE). In one report, the risk of a third-degree tear was about 10% with a 25°-angle mediolateral episiotomy, but less than 1% when the angle was >35°.13
Repairing the incision. After delivery, begin repair of a mediolateral incision by assessing the extent of vaginal, anal sphincter, rectal, and periurethral lacerations. Then, use two fingers, with or without a retractor, to spread the edges of the incision so that you can fully determine the length and depth of the episiotomy.
Place a 2-0 or 3-0 suture just above the apex of the incision. Use a running suture to close the vaginal mucosa and submucosal tissue. As you approach the introitus, suspend the running mucosal–submucosal suture and turn your attention to approximating the deeper submucosal space.
In mediolateral episiotomy, the upper-lateral edge of the incision contains more tissue than the lower-medial edge. To improve healing of the incision, use diagonal, rather than horizontal, sutures to provide better approximation of the submucosa. The fascia of the bulbocavernosus and superficial transveralis muscles might need to be reapproximated with individual sutures. Then, resume closing the skin and submucosa of the introitus and perineum.14 Perioperative antibiotic prophylaxis might be warranted—before you repair a complex perineal laceration.15
Concern about suture material. Using chromic suture to repair an episiotomy incision is associated with increased postdelivery pain, compared with the use of rapid-absorption polyglactin 910 suture (Vicryl Rapide).16 In fact, most OBs have stopped using chromic suture to repair episiotomy incisions. Rapid-absorption polyglactin 910 suture (average time to absorption, 42 days) might be associated with less of a need to remove suture that migrates through the incision than what is seen with standard-absorption polyglactin 910 sutures (average time to absorption, 63 days).16,17
When an episiotomy is indicated
There is renewed emphasis on reducing the rate of third- and fourth-degree perineal lacerations at delivery, because these adverse outcomes are associated with:
- an increased risk of wound breakdown that requires surgical repair
- incontinence of flatus or stool, or both.
At a time when the use of episiotomy has become limited, continuing to use a median incision will get you more third- and fourth-degree lacerations than if you use a mediolateral episiotomy.
A mediolateral episiotomy might cause more perineal pain immediately postpartum but, within a few months after delivery, patients mostly have recovered from either type of episiotomy.
To recap: If an episiotomy is indicated, use a mediolateral incision. I urge you to stop performing median episiotomy incisions.
For many OBs, episiotomy is one of the most common operative procedures that they will perform during their career. Precisely because the procedure is common, and because it is considered minor surgery, coding for the creation of the incision and subsequent repair is, under Current Procedural Terminology (CPT) rules, considered integral to the services provided during delivery.
Repair of an intentional episiotomy closely compares to the repair required for a first- or second-degree laceration. For that reason, payers will not reimburse separately for this level of repair—even when made necessary by laceration of tissues and not by intentional episiotomy.
On the other hand, most payers do reimburse for repair of third- and fourth-degree lacerations and, at times, for a more complex repair of an extension to an intentional episiotomy.
Details explained
Coding options for more extensive intentional episiotomies and for third- and fourth-degree lacerations vary by payer. The simplest coding option is to add modifier -22 (increased procedural services) to the delivery or the global OB care code (for example, 59400-22 or 59409-22). To support use of this modifier, your documentation must include:
- the reason for the additional work (increased intensity, time, technical difficulty of procedure, severity of patient’s condition, physical and mental effort required)
- description of the significant additional work.
Some payers allow you to bill separately for the repair; do this by reporting the integumentary repair codes by type of repair:
- 12001-12007, for simple repair
- 12041-12047, for intermediate repair
- 13131-13132, for complex repair.
Select a code based on the total length of the repair, which must be documented as part of the description of the repair.
When repair is performed at the same time as the delivery, add modifier -51 to the separate repair code because this is considered a multiple procedure.
When repair is made after delivery with a return to the operating room, append a modifier -78 to the repair code.
Note that the CPT code 59300, Episiotomy or vaginal repair, by other than the attending physician, can never be reported by the attending OB or a physician who is covering for this physician; doing so will always result in a denial of the service.
MELANIE WITT, RN, CPC, COBGC, MA
Faced with a difficult vaginal delivery, would you use a median or mediolateral episiotomy incision? Why?
1. American College of Obstetricians and Gynecologists. Clinical Management Guidelines for Obstetrician-Gynecologists: Episiotomy. No. 71. Obstet Gynecol. 2006;107(4):957-962.
2. Myles TD, Santolaya J. Maternal and neonatal outcomes in patients with prolonged second stage of labor. Obstet Gynecol. 2003;102(1):52-58.
3. Bodner-Adler B, Bodner K, Kimberger O, Wagenbichler P, Mayerhofer K. Management of the perineum during forceps delivery. Association of episiotomy with the frequency and severity of perineal trauma in women undergoing forceps delivery. J Reprod Med. 2003;48(4):239-242.
4. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorpe J, Jr, Lohr KN. Outcomes of routine episiotomy a systematic review. JAMA. 2005;293(17):2141-2148.
5. Barbieri RL. It’s time to restrict the use of episiotomy. OBG Manage. 2006;18(9):8-12.
6. De Leeuw JW, Struijik PC, Vierhout ME, Wallenburgh HC. Risk factors for third degree perineal ruptures during delivery. BJOG. 2001;108(4):383-387.
7. Fenner DE, Genberg B, Brahma P, Marek L, DeLancey JO. Fecal and urinary incontinence after vaginal delivery with anal sphincter disruption in an obstetrics unit in the United States. Am J Obstet Gynecol. 2003;189(6):1543-1550.
8. Shiono P, Klebenoff MA, Carey JC. Midline episiotomies: more harm than good? Obstet Gynecol. 1990;75(5):765-770.
9. Bodner-Adler B, Bodner K, Kaider A, et al. Risk factors for third-degree perineal tears in vaginal delivery, with an analysis of episiotomy types. J Reprod Med. 2001;46(8):752-756.
10. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408-412.
11. Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretive review of the English language literature, 1860–1980. Obstet Gynecol Surv. 1983;38(6):322-338.
12. Goldaber KG, Wendel PJ, McIntire DD, Wendel GD. Postpartum perineal morbidity after fourth degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489-493.
13. Eogan M, Daly L, O’Connell PR, O’Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG. 2006;113(2):190-194.
14. Hale RW, Ling FW. Episiotomy: Procedure and repair techniques. Washington DC: American College of Obstetricians and Gynecologists; 2007:1-24.
15. Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized controlled trial. Obstet Gynecol. 2008;111(6):1268-1273.
16. 1Greenberg JA, Lieberman E, Cohen AP, Ecker JL. Randomized comparison of chromic versus fast-absorbing polyglactin 910 for postpartum perineal repair. Obstet Gynecol. 2004;103(6):1308-1313.
17. Mackrodt C, Gordon B, Fern E, Ayers S, Truesdale A, Grant A. The Ipswich childbirth study 2. A randomised comparison of polyglactin 910 with chromic catgut for postpartum perineal repair. Br J Obstet Gynecol. 1998;105(4):441-445.
Advocates of the liberal use of episiotomy have hypothesized that the procedure has many benefits, including:
Most studies do not provide strong support for these claims.
Utilization has declined. Over the past decades, the liberal use of episiotomy has given way to a pattern of practice that emphasizes restricted use.1-4 In the 1980s, in the United States, episiotomy incisions were performed in approximately 40% of vaginal deliveries5; in 2010, the rate at most obstetric facilities was <10%.
When the episiotomy rate was 40%, a median incision made sense: A very limited incision was sufficient to provide extra room for the passage of an average-sized fetus through an average-sized birth outlet. With the rate below 10% today, however, the likelihood is greater that episiotomy is being reserved for cases in which a significant clinical problem exists—most often, mismatch between the birth outlet and fetal size—and the appropriateness of median episiotomy comes into question. By restricting episiotomy incisions to the most complex clinical situations, the risk is greater that the episiotomy will be associated with a severe perineal laceration, such as a laceration of the anal sphincter (third-degree) or the rectal mucosa (fourth-degree)—or both.
A spotlight on severe lacerations. Over the past decade, practitioners of obstetrics have refocused attention on reducing the risk of third- and fourth-degree perineal lacerations—severe injuries that are associated with significant maternal morbidity. Clinical variables that increase the risk of a third- or fourth-degree perineal laceration include:
- nulliparity
- forceps delivery
- median episiotomy
- macrosomia
- persistent occiput posterior position.6
Many studies have reported that a median episiotomy is associated with a higher rate of third- and fourth-degree lacerations than either 1) deliveries without an episiotomy or 2) deliveries with a mediolateral episiotomy.1,7-9 With the modern practice of reserving episiotomy for the most complex vaginal deliveries and renewed attention to reducing the rate of third- and fourth-degree lacerations, the time has come for us to stop using the median episiotomy and switch to using a mediolateral episiotomy incision.
STOP: using the median episiotomy
Numerous studies have reported that the median episiotomy is associated with an increased risk of laceration of the anal sphincter (third-degree) and rectal mucosa (fourth-degree), compared with mediolateral episiotomy.
Randomized study of incisions. In a clinical trial, 407 nulliparous women were randomized to median or mediolateral episiotomy incision.10 The incisions were made at a time during the second stage of labor that was judged by the clinician to be most appropriate—typically immediately before delivery of the fetal head.
To perform mediolateral episiotomy, clinicians in this study used a pair of straight scissors to make an incision that began in the midline and was carried to the right side of the anal sphincter for 3 to 4 cm, at an angle >45°. Median episiotomy was performed by incision of the perineal tissues for 2 to 3 cm, directly in the midline.
The clinical protocol resulted in more women assigned to mediolateral episiotomy (n=244) than to the midline episiotomy (n=159), but the two groups were well matched on such major clinical characteristics as age, gestational age at delivery, duration of the second stage, rate of operative delivery, and anesthesia used.
Compared to what was found with mediolateral episiotomy, the median episiotomy incision was associated with a statistically significant increase in the frequency of complete third-degree tears (median, 6.1%; mediolateral, 1.6%) and fourth-degree tears (median, 5.5%; mediolateral, 0.4%).
Further comparisons. Many clinicians avoid mediolateral episiotomy. Why? Because, compared with median episiotomy, a mediolateral incision is believed to be associated with greater postpartum pain, increased severity and incidence of dyspareunia, and more disfiguring scars.11
But subjects in the randomized trial that I just described, in which mediolateral and median episiotomy were compared,10 reported postpartum pain, postpartum use of pain medicine, and impaired bowel function at similar rates regardless of the type of incision.
Investigators determined that, in the first month after delivery, more women who had a median episiotomy resumed vaginal intercourse (18.1%, compared to 6.3% who had a mediolateral incision). In the second month after delivery, however, women in both the median and mediolateral episiotomy groups reported similar resumption of sexual intercourse (median, 82.8%; mediolateral, 80.8%).
Three months after delivery, physical examination determined that a higher percentage of subjects in the median incision group (43%) had what was judged to be a “good” appearance to the scar (compared to 27% in the mediolateral group). Last, subjects in the median group had a higher rate of perineal laxity (7%) than did women in the mediolateral group (1.6%).
START: using a mediolateral incision when episiotomy is necessary
Reducing the risk of severe perineal laceration is an important clinical goal because severe lacerations are associated with significant morbidity. In a study of 390 women who had a fourth-degree perineal laceration, 5% had significant complications that, in most cases, required additional surgery.12 Furthermore, in that study:
- 1.8% of women had a breakdown of the repair
- 2.8% had infection plus breakdown of the repair
- 0.8% had infection only.
In another study, 31% of women who sustained a fourth-degree laceration reported poor bowel control postpartum.7
Given the focus on reducing the rate of severe perineal laceration, I recommend that, in most cases, you reduce the use of median episiotomy and increase the use of mediolateral episiotomy.
Use a mediolateral incision for episiotomy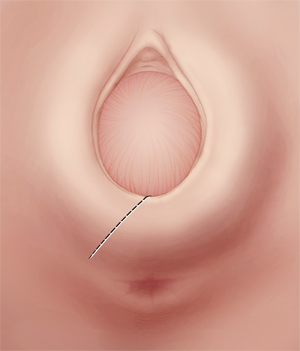
Make the incision at a 45°-angle; incisions made at >35° angle are associated with less of a risk of severe perineal laceration. Avoid using chromic sutures; rapid-absorption polyglactin 910 suture might offer better healing.
Mediolateral episiotomy: Technique
Begin the mediolateral episiotomy in the midline or slightly lateral to the midline (see the FIGURE). Insert two fingers into the vagina to distend the tissue of the birth outlet; using a pair of sharp, straight scissors, cut an incision 4 or 5 cm long at a 45° angle, directing it toward the ipsilateral ischial tuberosity. In most women, this incision cuts a portion of the bulbospongiosus muscle and, occasionally, reaches the ischioanal fossa.
Proper angle is key. The angle of the mediolateral episiotomy, in relation to the midline, is an important variable that influences the possibility that the patient will have a severe perineal laceration. Most experts recommend that the angle of the incision be at least 45° from the midline. If you use a shallow angle (<35°) from the midline to perform mediolateral episiotomy, you increase the risk of a severe perineal laceration, compared with incisions made at an angle >35° degrees from the midline (again, the FIGURE). In one report, the risk of a third-degree tear was about 10% with a 25°-angle mediolateral episiotomy, but less than 1% when the angle was >35°.13
Repairing the incision. After delivery, begin repair of a mediolateral incision by assessing the extent of vaginal, anal sphincter, rectal, and periurethral lacerations. Then, use two fingers, with or without a retractor, to spread the edges of the incision so that you can fully determine the length and depth of the episiotomy.
Place a 2-0 or 3-0 suture just above the apex of the incision. Use a running suture to close the vaginal mucosa and submucosal tissue. As you approach the introitus, suspend the running mucosal–submucosal suture and turn your attention to approximating the deeper submucosal space.
In mediolateral episiotomy, the upper-lateral edge of the incision contains more tissue than the lower-medial edge. To improve healing of the incision, use diagonal, rather than horizontal, sutures to provide better approximation of the submucosa. The fascia of the bulbocavernosus and superficial transveralis muscles might need to be reapproximated with individual sutures. Then, resume closing the skin and submucosa of the introitus and perineum.14 Perioperative antibiotic prophylaxis might be warranted—before you repair a complex perineal laceration.15
Concern about suture material. Using chromic suture to repair an episiotomy incision is associated with increased postdelivery pain, compared with the use of rapid-absorption polyglactin 910 suture (Vicryl Rapide).16 In fact, most OBs have stopped using chromic suture to repair episiotomy incisions. Rapid-absorption polyglactin 910 suture (average time to absorption, 42 days) might be associated with less of a need to remove suture that migrates through the incision than what is seen with standard-absorption polyglactin 910 sutures (average time to absorption, 63 days).16,17
When an episiotomy is indicated
There is renewed emphasis on reducing the rate of third- and fourth-degree perineal lacerations at delivery, because these adverse outcomes are associated with:
- an increased risk of wound breakdown that requires surgical repair
- incontinence of flatus or stool, or both.
At a time when the use of episiotomy has become limited, continuing to use a median incision will get you more third- and fourth-degree lacerations than if you use a mediolateral episiotomy.
A mediolateral episiotomy might cause more perineal pain immediately postpartum but, within a few months after delivery, patients mostly have recovered from either type of episiotomy.
To recap: If an episiotomy is indicated, use a mediolateral incision. I urge you to stop performing median episiotomy incisions.
For many OBs, episiotomy is one of the most common operative procedures that they will perform during their career. Precisely because the procedure is common, and because it is considered minor surgery, coding for the creation of the incision and subsequent repair is, under Current Procedural Terminology (CPT) rules, considered integral to the services provided during delivery.
Repair of an intentional episiotomy closely compares to the repair required for a first- or second-degree laceration. For that reason, payers will not reimburse separately for this level of repair—even when made necessary by laceration of tissues and not by intentional episiotomy.
On the other hand, most payers do reimburse for repair of third- and fourth-degree lacerations and, at times, for a more complex repair of an extension to an intentional episiotomy.
Details explained
Coding options for more extensive intentional episiotomies and for third- and fourth-degree lacerations vary by payer. The simplest coding option is to add modifier -22 (increased procedural services) to the delivery or the global OB care code (for example, 59400-22 or 59409-22). To support use of this modifier, your documentation must include:
- the reason for the additional work (increased intensity, time, technical difficulty of procedure, severity of patient’s condition, physical and mental effort required)
- description of the significant additional work.
Some payers allow you to bill separately for the repair; do this by reporting the integumentary repair codes by type of repair:
- 12001-12007, for simple repair
- 12041-12047, for intermediate repair
- 13131-13132, for complex repair.
Select a code based on the total length of the repair, which must be documented as part of the description of the repair.
When repair is performed at the same time as the delivery, add modifier -51 to the separate repair code because this is considered a multiple procedure.
When repair is made after delivery with a return to the operating room, append a modifier -78 to the repair code.
Note that the CPT code 59300, Episiotomy or vaginal repair, by other than the attending physician, can never be reported by the attending OB or a physician who is covering for this physician; doing so will always result in a denial of the service.
MELANIE WITT, RN, CPC, COBGC, MA
Faced with a difficult vaginal delivery, would you use a median or mediolateral episiotomy incision? Why?
Advocates of the liberal use of episiotomy have hypothesized that the procedure has many benefits, including:
Most studies do not provide strong support for these claims.
Utilization has declined. Over the past decades, the liberal use of episiotomy has given way to a pattern of practice that emphasizes restricted use.1-4 In the 1980s, in the United States, episiotomy incisions were performed in approximately 40% of vaginal deliveries5; in 2010, the rate at most obstetric facilities was <10%.
When the episiotomy rate was 40%, a median incision made sense: A very limited incision was sufficient to provide extra room for the passage of an average-sized fetus through an average-sized birth outlet. With the rate below 10% today, however, the likelihood is greater that episiotomy is being reserved for cases in which a significant clinical problem exists—most often, mismatch between the birth outlet and fetal size—and the appropriateness of median episiotomy comes into question. By restricting episiotomy incisions to the most complex clinical situations, the risk is greater that the episiotomy will be associated with a severe perineal laceration, such as a laceration of the anal sphincter (third-degree) or the rectal mucosa (fourth-degree)—or both.
A spotlight on severe lacerations. Over the past decade, practitioners of obstetrics have refocused attention on reducing the risk of third- and fourth-degree perineal lacerations—severe injuries that are associated with significant maternal morbidity. Clinical variables that increase the risk of a third- or fourth-degree perineal laceration include:
- nulliparity
- forceps delivery
- median episiotomy
- macrosomia
- persistent occiput posterior position.6
Many studies have reported that a median episiotomy is associated with a higher rate of third- and fourth-degree lacerations than either 1) deliveries without an episiotomy or 2) deliveries with a mediolateral episiotomy.1,7-9 With the modern practice of reserving episiotomy for the most complex vaginal deliveries and renewed attention to reducing the rate of third- and fourth-degree lacerations, the time has come for us to stop using the median episiotomy and switch to using a mediolateral episiotomy incision.
STOP: using the median episiotomy
Numerous studies have reported that the median episiotomy is associated with an increased risk of laceration of the anal sphincter (third-degree) and rectal mucosa (fourth-degree), compared with mediolateral episiotomy.
Randomized study of incisions. In a clinical trial, 407 nulliparous women were randomized to median or mediolateral episiotomy incision.10 The incisions were made at a time during the second stage of labor that was judged by the clinician to be most appropriate—typically immediately before delivery of the fetal head.
To perform mediolateral episiotomy, clinicians in this study used a pair of straight scissors to make an incision that began in the midline and was carried to the right side of the anal sphincter for 3 to 4 cm, at an angle >45°. Median episiotomy was performed by incision of the perineal tissues for 2 to 3 cm, directly in the midline.
The clinical protocol resulted in more women assigned to mediolateral episiotomy (n=244) than to the midline episiotomy (n=159), but the two groups were well matched on such major clinical characteristics as age, gestational age at delivery, duration of the second stage, rate of operative delivery, and anesthesia used.
Compared to what was found with mediolateral episiotomy, the median episiotomy incision was associated with a statistically significant increase in the frequency of complete third-degree tears (median, 6.1%; mediolateral, 1.6%) and fourth-degree tears (median, 5.5%; mediolateral, 0.4%).
Further comparisons. Many clinicians avoid mediolateral episiotomy. Why? Because, compared with median episiotomy, a mediolateral incision is believed to be associated with greater postpartum pain, increased severity and incidence of dyspareunia, and more disfiguring scars.11
But subjects in the randomized trial that I just described, in which mediolateral and median episiotomy were compared,10 reported postpartum pain, postpartum use of pain medicine, and impaired bowel function at similar rates regardless of the type of incision.
Investigators determined that, in the first month after delivery, more women who had a median episiotomy resumed vaginal intercourse (18.1%, compared to 6.3% who had a mediolateral incision). In the second month after delivery, however, women in both the median and mediolateral episiotomy groups reported similar resumption of sexual intercourse (median, 82.8%; mediolateral, 80.8%).
Three months after delivery, physical examination determined that a higher percentage of subjects in the median incision group (43%) had what was judged to be a “good” appearance to the scar (compared to 27% in the mediolateral group). Last, subjects in the median group had a higher rate of perineal laxity (7%) than did women in the mediolateral group (1.6%).
START: using a mediolateral incision when episiotomy is necessary
Reducing the risk of severe perineal laceration is an important clinical goal because severe lacerations are associated with significant morbidity. In a study of 390 women who had a fourth-degree perineal laceration, 5% had significant complications that, in most cases, required additional surgery.12 Furthermore, in that study:
- 1.8% of women had a breakdown of the repair
- 2.8% had infection plus breakdown of the repair
- 0.8% had infection only.
In another study, 31% of women who sustained a fourth-degree laceration reported poor bowel control postpartum.7
Given the focus on reducing the rate of severe perineal laceration, I recommend that, in most cases, you reduce the use of median episiotomy and increase the use of mediolateral episiotomy.
Use a mediolateral incision for episiotomy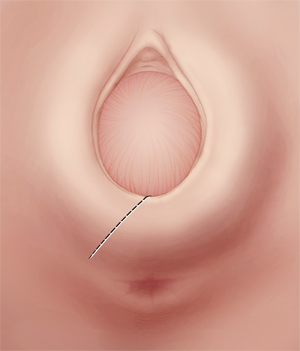
Make the incision at a 45°-angle; incisions made at >35° angle are associated with less of a risk of severe perineal laceration. Avoid using chromic sutures; rapid-absorption polyglactin 910 suture might offer better healing.
Mediolateral episiotomy: Technique
Begin the mediolateral episiotomy in the midline or slightly lateral to the midline (see the FIGURE). Insert two fingers into the vagina to distend the tissue of the birth outlet; using a pair of sharp, straight scissors, cut an incision 4 or 5 cm long at a 45° angle, directing it toward the ipsilateral ischial tuberosity. In most women, this incision cuts a portion of the bulbospongiosus muscle and, occasionally, reaches the ischioanal fossa.
Proper angle is key. The angle of the mediolateral episiotomy, in relation to the midline, is an important variable that influences the possibility that the patient will have a severe perineal laceration. Most experts recommend that the angle of the incision be at least 45° from the midline. If you use a shallow angle (<35°) from the midline to perform mediolateral episiotomy, you increase the risk of a severe perineal laceration, compared with incisions made at an angle >35° degrees from the midline (again, the FIGURE). In one report, the risk of a third-degree tear was about 10% with a 25°-angle mediolateral episiotomy, but less than 1% when the angle was >35°.13
Repairing the incision. After delivery, begin repair of a mediolateral incision by assessing the extent of vaginal, anal sphincter, rectal, and periurethral lacerations. Then, use two fingers, with or without a retractor, to spread the edges of the incision so that you can fully determine the length and depth of the episiotomy.
Place a 2-0 or 3-0 suture just above the apex of the incision. Use a running suture to close the vaginal mucosa and submucosal tissue. As you approach the introitus, suspend the running mucosal–submucosal suture and turn your attention to approximating the deeper submucosal space.
In mediolateral episiotomy, the upper-lateral edge of the incision contains more tissue than the lower-medial edge. To improve healing of the incision, use diagonal, rather than horizontal, sutures to provide better approximation of the submucosa. The fascia of the bulbocavernosus and superficial transveralis muscles might need to be reapproximated with individual sutures. Then, resume closing the skin and submucosa of the introitus and perineum.14 Perioperative antibiotic prophylaxis might be warranted—before you repair a complex perineal laceration.15
Concern about suture material. Using chromic suture to repair an episiotomy incision is associated with increased postdelivery pain, compared with the use of rapid-absorption polyglactin 910 suture (Vicryl Rapide).16 In fact, most OBs have stopped using chromic suture to repair episiotomy incisions. Rapid-absorption polyglactin 910 suture (average time to absorption, 42 days) might be associated with less of a need to remove suture that migrates through the incision than what is seen with standard-absorption polyglactin 910 sutures (average time to absorption, 63 days).16,17
When an episiotomy is indicated
There is renewed emphasis on reducing the rate of third- and fourth-degree perineal lacerations at delivery, because these adverse outcomes are associated with:
- an increased risk of wound breakdown that requires surgical repair
- incontinence of flatus or stool, or both.
At a time when the use of episiotomy has become limited, continuing to use a median incision will get you more third- and fourth-degree lacerations than if you use a mediolateral episiotomy.
A mediolateral episiotomy might cause more perineal pain immediately postpartum but, within a few months after delivery, patients mostly have recovered from either type of episiotomy.
To recap: If an episiotomy is indicated, use a mediolateral incision. I urge you to stop performing median episiotomy incisions.
For many OBs, episiotomy is one of the most common operative procedures that they will perform during their career. Precisely because the procedure is common, and because it is considered minor surgery, coding for the creation of the incision and subsequent repair is, under Current Procedural Terminology (CPT) rules, considered integral to the services provided during delivery.
Repair of an intentional episiotomy closely compares to the repair required for a first- or second-degree laceration. For that reason, payers will not reimburse separately for this level of repair—even when made necessary by laceration of tissues and not by intentional episiotomy.
On the other hand, most payers do reimburse for repair of third- and fourth-degree lacerations and, at times, for a more complex repair of an extension to an intentional episiotomy.
Details explained
Coding options for more extensive intentional episiotomies and for third- and fourth-degree lacerations vary by payer. The simplest coding option is to add modifier -22 (increased procedural services) to the delivery or the global OB care code (for example, 59400-22 or 59409-22). To support use of this modifier, your documentation must include:
- the reason for the additional work (increased intensity, time, technical difficulty of procedure, severity of patient’s condition, physical and mental effort required)
- description of the significant additional work.
Some payers allow you to bill separately for the repair; do this by reporting the integumentary repair codes by type of repair:
- 12001-12007, for simple repair
- 12041-12047, for intermediate repair
- 13131-13132, for complex repair.
Select a code based on the total length of the repair, which must be documented as part of the description of the repair.
When repair is performed at the same time as the delivery, add modifier -51 to the separate repair code because this is considered a multiple procedure.
When repair is made after delivery with a return to the operating room, append a modifier -78 to the repair code.
Note that the CPT code 59300, Episiotomy or vaginal repair, by other than the attending physician, can never be reported by the attending OB or a physician who is covering for this physician; doing so will always result in a denial of the service.
MELANIE WITT, RN, CPC, COBGC, MA
Faced with a difficult vaginal delivery, would you use a median or mediolateral episiotomy incision? Why?
1. American College of Obstetricians and Gynecologists. Clinical Management Guidelines for Obstetrician-Gynecologists: Episiotomy. No. 71. Obstet Gynecol. 2006;107(4):957-962.
2. Myles TD, Santolaya J. Maternal and neonatal outcomes in patients with prolonged second stage of labor. Obstet Gynecol. 2003;102(1):52-58.
3. Bodner-Adler B, Bodner K, Kimberger O, Wagenbichler P, Mayerhofer K. Management of the perineum during forceps delivery. Association of episiotomy with the frequency and severity of perineal trauma in women undergoing forceps delivery. J Reprod Med. 2003;48(4):239-242.
4. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorpe J, Jr, Lohr KN. Outcomes of routine episiotomy a systematic review. JAMA. 2005;293(17):2141-2148.
5. Barbieri RL. It’s time to restrict the use of episiotomy. OBG Manage. 2006;18(9):8-12.
6. De Leeuw JW, Struijik PC, Vierhout ME, Wallenburgh HC. Risk factors for third degree perineal ruptures during delivery. BJOG. 2001;108(4):383-387.
7. Fenner DE, Genberg B, Brahma P, Marek L, DeLancey JO. Fecal and urinary incontinence after vaginal delivery with anal sphincter disruption in an obstetrics unit in the United States. Am J Obstet Gynecol. 2003;189(6):1543-1550.
8. Shiono P, Klebenoff MA, Carey JC. Midline episiotomies: more harm than good? Obstet Gynecol. 1990;75(5):765-770.
9. Bodner-Adler B, Bodner K, Kaider A, et al. Risk factors for third-degree perineal tears in vaginal delivery, with an analysis of episiotomy types. J Reprod Med. 2001;46(8):752-756.
10. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408-412.
11. Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretive review of the English language literature, 1860–1980. Obstet Gynecol Surv. 1983;38(6):322-338.
12. Goldaber KG, Wendel PJ, McIntire DD, Wendel GD. Postpartum perineal morbidity after fourth degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489-493.
13. Eogan M, Daly L, O’Connell PR, O’Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG. 2006;113(2):190-194.
14. Hale RW, Ling FW. Episiotomy: Procedure and repair techniques. Washington DC: American College of Obstetricians and Gynecologists; 2007:1-24.
15. Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized controlled trial. Obstet Gynecol. 2008;111(6):1268-1273.
16. 1Greenberg JA, Lieberman E, Cohen AP, Ecker JL. Randomized comparison of chromic versus fast-absorbing polyglactin 910 for postpartum perineal repair. Obstet Gynecol. 2004;103(6):1308-1313.
17. Mackrodt C, Gordon B, Fern E, Ayers S, Truesdale A, Grant A. The Ipswich childbirth study 2. A randomised comparison of polyglactin 910 with chromic catgut for postpartum perineal repair. Br J Obstet Gynecol. 1998;105(4):441-445.
1. American College of Obstetricians and Gynecologists. Clinical Management Guidelines for Obstetrician-Gynecologists: Episiotomy. No. 71. Obstet Gynecol. 2006;107(4):957-962.
2. Myles TD, Santolaya J. Maternal and neonatal outcomes in patients with prolonged second stage of labor. Obstet Gynecol. 2003;102(1):52-58.
3. Bodner-Adler B, Bodner K, Kimberger O, Wagenbichler P, Mayerhofer K. Management of the perineum during forceps delivery. Association of episiotomy with the frequency and severity of perineal trauma in women undergoing forceps delivery. J Reprod Med. 2003;48(4):239-242.
4. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorpe J, Jr, Lohr KN. Outcomes of routine episiotomy a systematic review. JAMA. 2005;293(17):2141-2148.
5. Barbieri RL. It’s time to restrict the use of episiotomy. OBG Manage. 2006;18(9):8-12.
6. De Leeuw JW, Struijik PC, Vierhout ME, Wallenburgh HC. Risk factors for third degree perineal ruptures during delivery. BJOG. 2001;108(4):383-387.
7. Fenner DE, Genberg B, Brahma P, Marek L, DeLancey JO. Fecal and urinary incontinence after vaginal delivery with anal sphincter disruption in an obstetrics unit in the United States. Am J Obstet Gynecol. 2003;189(6):1543-1550.
8. Shiono P, Klebenoff MA, Carey JC. Midline episiotomies: more harm than good? Obstet Gynecol. 1990;75(5):765-770.
9. Bodner-Adler B, Bodner K, Kaider A, et al. Risk factors for third-degree perineal tears in vaginal delivery, with an analysis of episiotomy types. J Reprod Med. 2001;46(8):752-756.
10. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408-412.
11. Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretive review of the English language literature, 1860–1980. Obstet Gynecol Surv. 1983;38(6):322-338.
12. Goldaber KG, Wendel PJ, McIntire DD, Wendel GD. Postpartum perineal morbidity after fourth degree perineal repair. Am J Obstet Gynecol. 1993;168(2):489-493.
13. Eogan M, Daly L, O’Connell PR, O’Herlihy C. Does the angle of episiotomy affect the incidence of anal sphincter injury? BJOG. 2006;113(2):190-194.
14. Hale RW, Ling FW. Episiotomy: Procedure and repair techniques. Washington DC: American College of Obstetricians and Gynecologists; 2007:1-24.
15. Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention of postpartum perineal wound complications: a randomized controlled trial. Obstet Gynecol. 2008;111(6):1268-1273.
16. 1Greenberg JA, Lieberman E, Cohen AP, Ecker JL. Randomized comparison of chromic versus fast-absorbing polyglactin 910 for postpartum perineal repair. Obstet Gynecol. 2004;103(6):1308-1313.
17. Mackrodt C, Gordon B, Fern E, Ayers S, Truesdale A, Grant A. The Ipswich childbirth study 2. A randomised comparison of polyglactin 910 with chromic catgut for postpartum perineal repair. Br J Obstet Gynecol. 1998;105(4):441-445.
