User login
Urine drug screening (UDS) is an important tool in emergency settings and substance abuse or pain management clinics. According to the 2015 National Survey on Drug Use and Health, 9.2% of individuals age ≥12 used an illicit drug other than marijuana within the previous year.1
There are 2 types of UDS: gas chromatography–mass spectroscopy (GC-MS) and enzymatic immunoassay (EIA). A GC-MS uses a 2-step mechanisms to detect chemical compounds. First the GC separate the illicit substance into molecules, which is then introduced to the MS, which then separates compounds depending on their mass and charge using magnetic fields.2,3 Although GC-MS is a more definitive means to confirm the presence of a specific drug, it rarely is used in clinical settings because it is expensive and time-consuming.
EIA is an anti-drug antibody added to the patient’s urine that causes a positive indicator reaction that can be measured.2,3 It is a rapid, accurate, and cost-effective way of detecting illicit substances.4 However, there are limitations to EIAs used in most hospital laboratories.
Limitations of EIAs
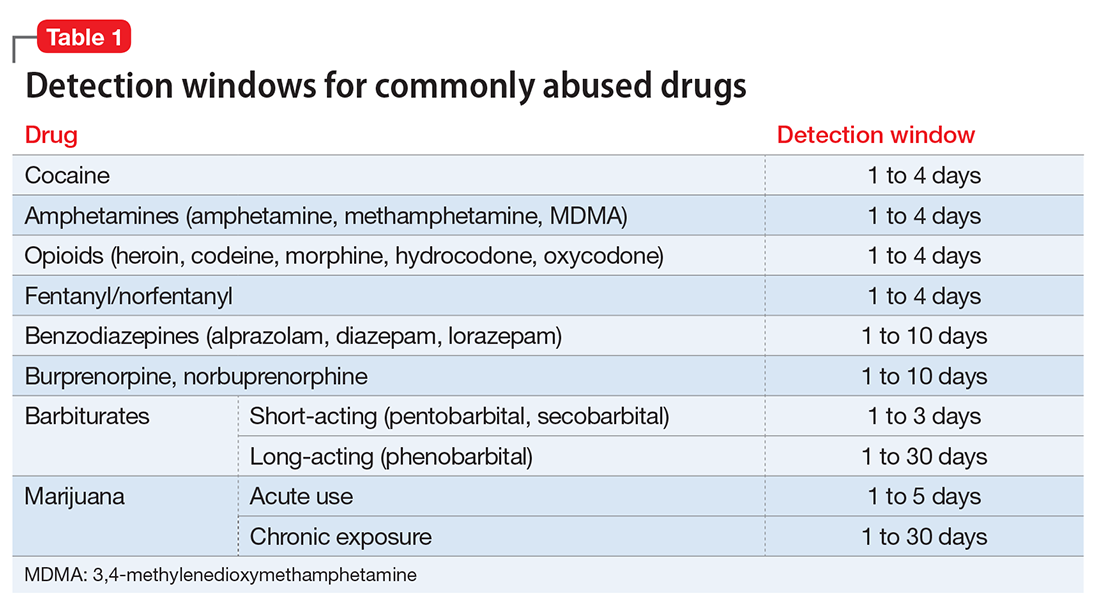
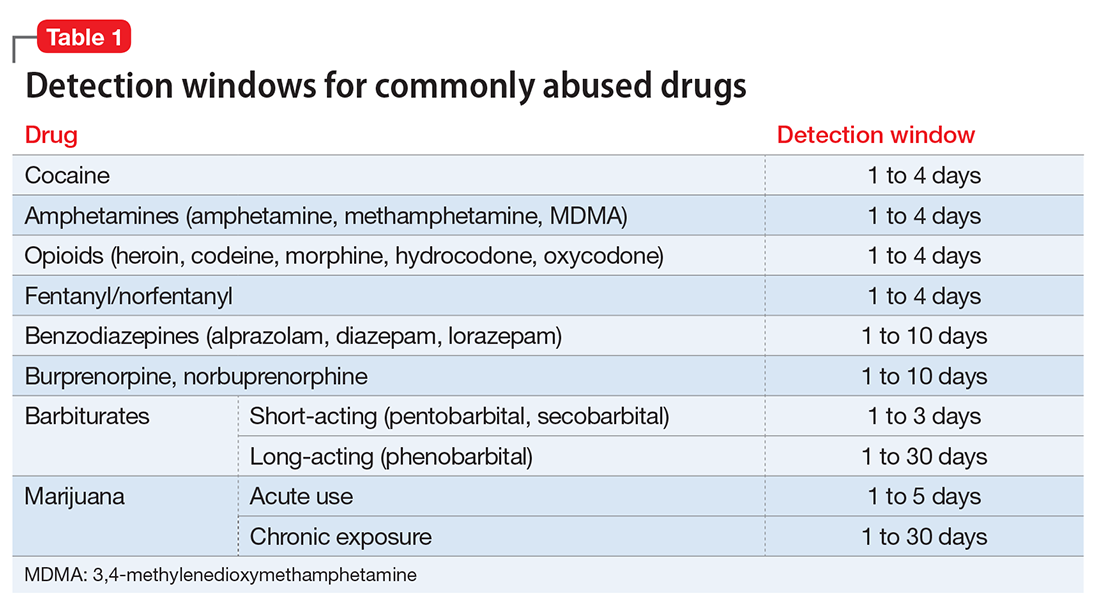
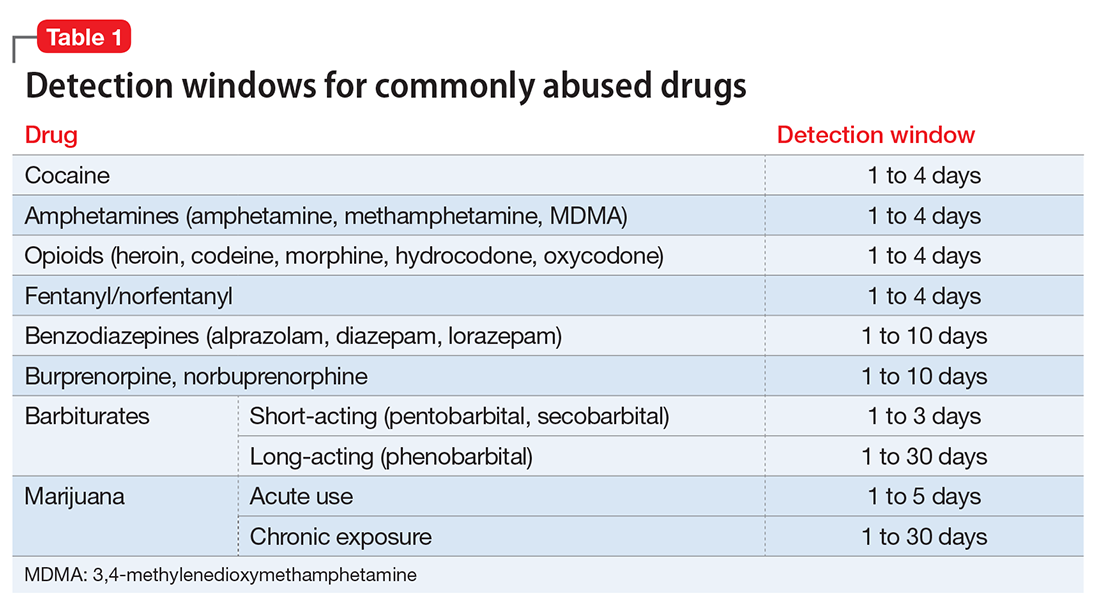
Timing. Results of the drug screen depend on the time and frequency of drug use (Table 1).5
Sensitivity. The immunoassay methods used vary in their ability to detect substances and depend on the test’s sensitivity; however, most of these versions have high sensitivity for detecting many illicit substances.4
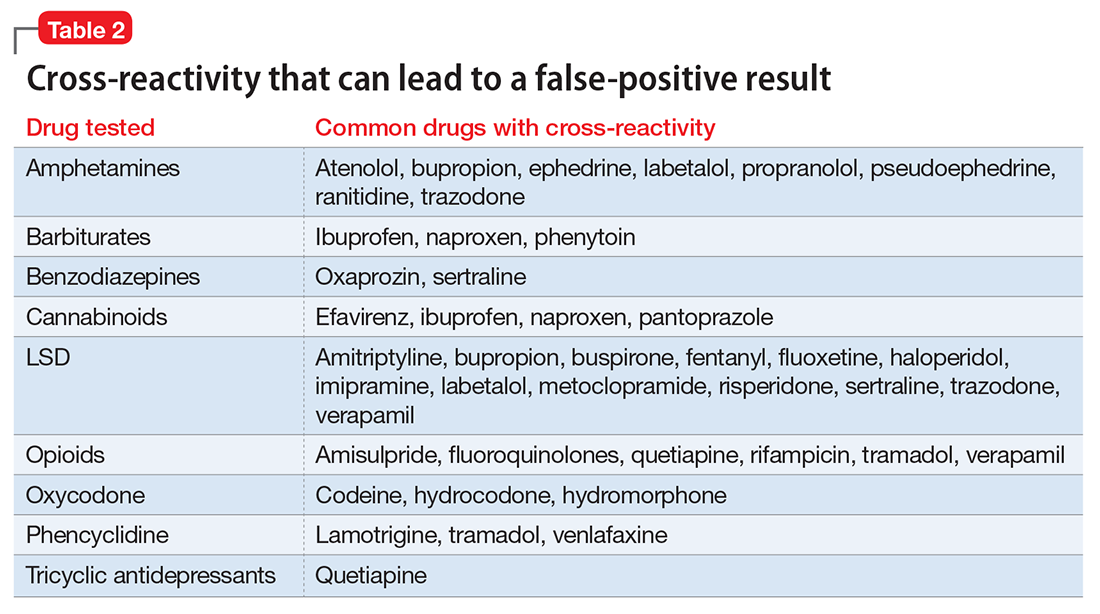
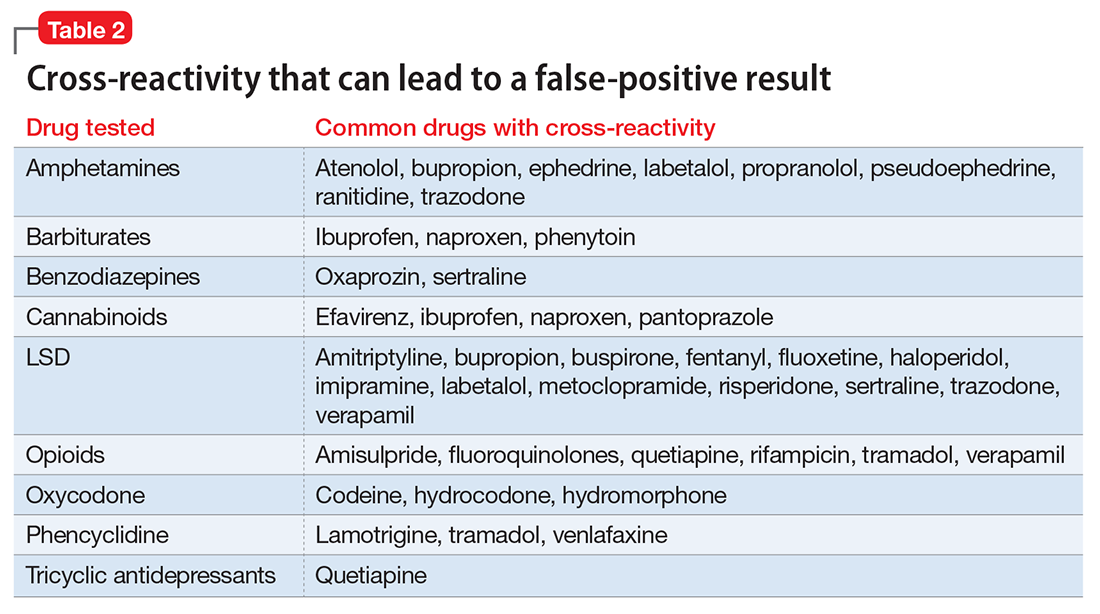
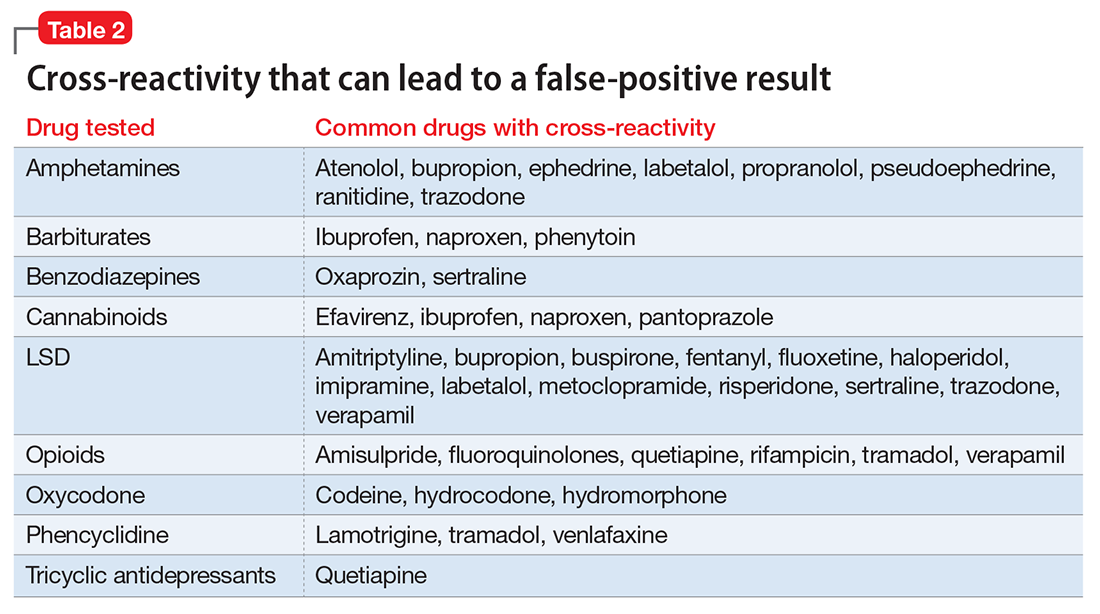
Specificity and cross-reactivity. Unfortunately, many drugs, such as opioids, amphetamines, and commonly prescribed medications, exhibit cross-reactivity that can produce false-positive results (Table 2).5,6
Synthetic cannabinoids, such as “spice” and cathinones, also known as “bath salts,” cannot be detected with standard UDS. However, some newer EIA kits can detect synthetic cannabinoids but do not detect newer designer drugs.7 Detection of specific cathinones by EIA is not yet available.7
Preventing false-negatives
Substance abusing individuals could try to avoid detection of illicit drug use by using the following techniques:
- In vivo methods, such as drinking a large amount of water or using herbal products, can lead to false-negative results because of dilution.8
- In vitro adulterants are substances added to urine samples after urination to avoid drug detection. Active ingredients include glutaraldehyde (Clean-X), sodium or potassium nitrate (Klear, Whizzies), pyridinium chlorochromate (Urine Luck), andj (Stealth).9
- Other methods used to avoid drug detection include substituting a urine sample with someone else’s clean urine or adding household products, such as bleach, vinegar, or pipe cleaner.
You can spot and prevent false-negatives by:
Directly observing the patient, which helps to prevent individuals from adding foreign materials or substituting the urine sample.
Visually inspecting the urine helps identify sample tampering. Adding household adulterants can produce unusually bubbly, cloudy, clear, or dark sample.
On-site analyses and laboratory analyses of samples. Commercially sold kits can detect adulterants by on-site analysis, such as Intect 7 and AdultaCheck 4 test strips.9 Simple on-site methods can help discover tampering, such as measuring the urine’s temperature and using pigmented toilet water. The U.S. Substance Abuse and Mental Health Services Administration recommends validity checks during laboratory analysis for all urine samples, including temperature, creatinine, specific gravity, pH, and tests for oxidizing adulterants.10
Considerations
The results of UDS should not be interpreted as absolute. Knowing the sensitivity and specificity of the UDS that your institution uses and the patient’s current medication regimen is valuable in distinguishing between true results and false-positives. False-positives can strain the relationship between patient and provider, thus compromising care. When EIA is positive and patient denies substance use, confirming the result with GC-MS may be a good clinical practice.3 Ordering a GC-MS test can be helpful in situations requiring greater precision, such as in methadone or pain management clinics, to verify if the patient is taking a prescribed medication properly or to rule out illicit exposures with greater certainty.
Acknowledgment
The authors would like to thank Steven Lippmann, MD, for his mentorship, encouragement, and editorial support.
1. Substance Abuse and Mental Health Services Administration. Results from the National Survey on Drug Use and Health: detailed tables. Prevalence estimates, standard errors, P values, and sample sizes. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. Published September 8, 2016. Accessed February 7, 2017.
2. Schweitzer BN. An assessment of lateral flow immunoassay testing and gas chromatography mass spectrometry as methods for the detection of five drugs of abuse in forensic bloodstains. https://open.bu.edu/bitstream/handle/2144/19477/Schweitzer_bu_0017N_12357.pdf?sequence=1. Published 2016. Accessed February 7, 2017.
3. Pawlowski J, Ellingrod VL. Urine drug screens: when might a test result be false-positive? Current Psychiatry. 2015;14(10):17,22-24.
4. Tenore PL. Advanced urine toxicology testing. J Addict Dis. 2010;29(4):436-448.
5. AIT Laboratories. Physician’s reference for urine and blood drug testing and interpretation. http://web.archive.org/web/20160312195526/http://aitlabs.com/uploadedfiles/services/pocket_guide_smr086.pdf. Published 2011. Accessed February 7, 2017.
6. Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38(7):387-396.
7. Namera A, Kawamura M, Nakamoto A, et al. Comprehensive review of the detection methods for synthetic cannabinoids and cathinones. Forensic Toxicol. 2015;33(2):175-194.
8. Cone EJ, Lange R, Darwin WD. In vivo adulteration: excess fluid ingestion causes false-negative marijuana and cocaine urine test results. J Anal Toxicol. 1998;22(6):460-473.
9. Jaffee WB, Trucco E, Levy S, et al. Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat. 2007;33(1):33-42.
10. Substance Abuse and Mental Health Services Administration. Mandatory guidelines for federal workplace drug testing programs. Federal Register. 2004;69:19644-19673.
Urine drug screening (UDS) is an important tool in emergency settings and substance abuse or pain management clinics. According to the 2015 National Survey on Drug Use and Health, 9.2% of individuals age ≥12 used an illicit drug other than marijuana within the previous year.1
There are 2 types of UDS: gas chromatography–mass spectroscopy (GC-MS) and enzymatic immunoassay (EIA). A GC-MS uses a 2-step mechanisms to detect chemical compounds. First the GC separate the illicit substance into molecules, which is then introduced to the MS, which then separates compounds depending on their mass and charge using magnetic fields.2,3 Although GC-MS is a more definitive means to confirm the presence of a specific drug, it rarely is used in clinical settings because it is expensive and time-consuming.
EIA is an anti-drug antibody added to the patient’s urine that causes a positive indicator reaction that can be measured.2,3 It is a rapid, accurate, and cost-effective way of detecting illicit substances.4 However, there are limitations to EIAs used in most hospital laboratories.
Limitations of EIAs
Timing. Results of the drug screen depend on the time and frequency of drug use (Table 1).5
Sensitivity. The immunoassay methods used vary in their ability to detect substances and depend on the test’s sensitivity; however, most of these versions have high sensitivity for detecting many illicit substances.4
Specificity and cross-reactivity. Unfortunately, many drugs, such as opioids, amphetamines, and commonly prescribed medications, exhibit cross-reactivity that can produce false-positive results (Table 2).5,6
Synthetic cannabinoids, such as “spice” and cathinones, also known as “bath salts,” cannot be detected with standard UDS. However, some newer EIA kits can detect synthetic cannabinoids but do not detect newer designer drugs.7 Detection of specific cathinones by EIA is not yet available.7
Preventing false-negatives
Substance abusing individuals could try to avoid detection of illicit drug use by using the following techniques:
- In vivo methods, such as drinking a large amount of water or using herbal products, can lead to false-negative results because of dilution.8
- In vitro adulterants are substances added to urine samples after urination to avoid drug detection. Active ingredients include glutaraldehyde (Clean-X), sodium or potassium nitrate (Klear, Whizzies), pyridinium chlorochromate (Urine Luck), andj (Stealth).9
- Other methods used to avoid drug detection include substituting a urine sample with someone else’s clean urine or adding household products, such as bleach, vinegar, or pipe cleaner.
You can spot and prevent false-negatives by:
Directly observing the patient, which helps to prevent individuals from adding foreign materials or substituting the urine sample.
Visually inspecting the urine helps identify sample tampering. Adding household adulterants can produce unusually bubbly, cloudy, clear, or dark sample.
On-site analyses and laboratory analyses of samples. Commercially sold kits can detect adulterants by on-site analysis, such as Intect 7 and AdultaCheck 4 test strips.9 Simple on-site methods can help discover tampering, such as measuring the urine’s temperature and using pigmented toilet water. The U.S. Substance Abuse and Mental Health Services Administration recommends validity checks during laboratory analysis for all urine samples, including temperature, creatinine, specific gravity, pH, and tests for oxidizing adulterants.10
Considerations
The results of UDS should not be interpreted as absolute. Knowing the sensitivity and specificity of the UDS that your institution uses and the patient’s current medication regimen is valuable in distinguishing between true results and false-positives. False-positives can strain the relationship between patient and provider, thus compromising care. When EIA is positive and patient denies substance use, confirming the result with GC-MS may be a good clinical practice.3 Ordering a GC-MS test can be helpful in situations requiring greater precision, such as in methadone or pain management clinics, to verify if the patient is taking a prescribed medication properly or to rule out illicit exposures with greater certainty.
Acknowledgment
The authors would like to thank Steven Lippmann, MD, for his mentorship, encouragement, and editorial support.
Urine drug screening (UDS) is an important tool in emergency settings and substance abuse or pain management clinics. According to the 2015 National Survey on Drug Use and Health, 9.2% of individuals age ≥12 used an illicit drug other than marijuana within the previous year.1
There are 2 types of UDS: gas chromatography–mass spectroscopy (GC-MS) and enzymatic immunoassay (EIA). A GC-MS uses a 2-step mechanisms to detect chemical compounds. First the GC separate the illicit substance into molecules, which is then introduced to the MS, which then separates compounds depending on their mass and charge using magnetic fields.2,3 Although GC-MS is a more definitive means to confirm the presence of a specific drug, it rarely is used in clinical settings because it is expensive and time-consuming.
EIA is an anti-drug antibody added to the patient’s urine that causes a positive indicator reaction that can be measured.2,3 It is a rapid, accurate, and cost-effective way of detecting illicit substances.4 However, there are limitations to EIAs used in most hospital laboratories.
Limitations of EIAs
Timing. Results of the drug screen depend on the time and frequency of drug use (Table 1).5
Sensitivity. The immunoassay methods used vary in their ability to detect substances and depend on the test’s sensitivity; however, most of these versions have high sensitivity for detecting many illicit substances.4
Specificity and cross-reactivity. Unfortunately, many drugs, such as opioids, amphetamines, and commonly prescribed medications, exhibit cross-reactivity that can produce false-positive results (Table 2).5,6
Synthetic cannabinoids, such as “spice” and cathinones, also known as “bath salts,” cannot be detected with standard UDS. However, some newer EIA kits can detect synthetic cannabinoids but do not detect newer designer drugs.7 Detection of specific cathinones by EIA is not yet available.7
Preventing false-negatives
Substance abusing individuals could try to avoid detection of illicit drug use by using the following techniques:
- In vivo methods, such as drinking a large amount of water or using herbal products, can lead to false-negative results because of dilution.8
- In vitro adulterants are substances added to urine samples after urination to avoid drug detection. Active ingredients include glutaraldehyde (Clean-X), sodium or potassium nitrate (Klear, Whizzies), pyridinium chlorochromate (Urine Luck), andj (Stealth).9
- Other methods used to avoid drug detection include substituting a urine sample with someone else’s clean urine or adding household products, such as bleach, vinegar, or pipe cleaner.
You can spot and prevent false-negatives by:
Directly observing the patient, which helps to prevent individuals from adding foreign materials or substituting the urine sample.
Visually inspecting the urine helps identify sample tampering. Adding household adulterants can produce unusually bubbly, cloudy, clear, or dark sample.
On-site analyses and laboratory analyses of samples. Commercially sold kits can detect adulterants by on-site analysis, such as Intect 7 and AdultaCheck 4 test strips.9 Simple on-site methods can help discover tampering, such as measuring the urine’s temperature and using pigmented toilet water. The U.S. Substance Abuse and Mental Health Services Administration recommends validity checks during laboratory analysis for all urine samples, including temperature, creatinine, specific gravity, pH, and tests for oxidizing adulterants.10
Considerations
The results of UDS should not be interpreted as absolute. Knowing the sensitivity and specificity of the UDS that your institution uses and the patient’s current medication regimen is valuable in distinguishing between true results and false-positives. False-positives can strain the relationship between patient and provider, thus compromising care. When EIA is positive and patient denies substance use, confirming the result with GC-MS may be a good clinical practice.3 Ordering a GC-MS test can be helpful in situations requiring greater precision, such as in methadone or pain management clinics, to verify if the patient is taking a prescribed medication properly or to rule out illicit exposures with greater certainty.
Acknowledgment
The authors would like to thank Steven Lippmann, MD, for his mentorship, encouragement, and editorial support.
1. Substance Abuse and Mental Health Services Administration. Results from the National Survey on Drug Use and Health: detailed tables. Prevalence estimates, standard errors, P values, and sample sizes. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. Published September 8, 2016. Accessed February 7, 2017.
2. Schweitzer BN. An assessment of lateral flow immunoassay testing and gas chromatography mass spectrometry as methods for the detection of five drugs of abuse in forensic bloodstains. https://open.bu.edu/bitstream/handle/2144/19477/Schweitzer_bu_0017N_12357.pdf?sequence=1. Published 2016. Accessed February 7, 2017.
3. Pawlowski J, Ellingrod VL. Urine drug screens: when might a test result be false-positive? Current Psychiatry. 2015;14(10):17,22-24.
4. Tenore PL. Advanced urine toxicology testing. J Addict Dis. 2010;29(4):436-448.
5. AIT Laboratories. Physician’s reference for urine and blood drug testing and interpretation. http://web.archive.org/web/20160312195526/http://aitlabs.com/uploadedfiles/services/pocket_guide_smr086.pdf. Published 2011. Accessed February 7, 2017.
6. Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38(7):387-396.
7. Namera A, Kawamura M, Nakamoto A, et al. Comprehensive review of the detection methods for synthetic cannabinoids and cathinones. Forensic Toxicol. 2015;33(2):175-194.
8. Cone EJ, Lange R, Darwin WD. In vivo adulteration: excess fluid ingestion causes false-negative marijuana and cocaine urine test results. J Anal Toxicol. 1998;22(6):460-473.
9. Jaffee WB, Trucco E, Levy S, et al. Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat. 2007;33(1):33-42.
10. Substance Abuse and Mental Health Services Administration. Mandatory guidelines for federal workplace drug testing programs. Federal Register. 2004;69:19644-19673.
1. Substance Abuse and Mental Health Services Administration. Results from the National Survey on Drug Use and Health: detailed tables. Prevalence estimates, standard errors, P values, and sample sizes. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. Published September 8, 2016. Accessed February 7, 2017.
2. Schweitzer BN. An assessment of lateral flow immunoassay testing and gas chromatography mass spectrometry as methods for the detection of five drugs of abuse in forensic bloodstains. https://open.bu.edu/bitstream/handle/2144/19477/Schweitzer_bu_0017N_12357.pdf?sequence=1. Published 2016. Accessed February 7, 2017.
3. Pawlowski J, Ellingrod VL. Urine drug screens: when might a test result be false-positive? Current Psychiatry. 2015;14(10):17,22-24.
4. Tenore PL. Advanced urine toxicology testing. J Addict Dis. 2010;29(4):436-448.
5. AIT Laboratories. Physician’s reference for urine and blood drug testing and interpretation. http://web.archive.org/web/20160312195526/http://aitlabs.com/uploadedfiles/services/pocket_guide_smr086.pdf. Published 2011. Accessed February 7, 2017.
6. Saitman A, Park HD, Fitzgerald RL. False-positive interferences of common urine drug screen immunoassays: a review. J Anal Toxicol. 2014;38(7):387-396.
7. Namera A, Kawamura M, Nakamoto A, et al. Comprehensive review of the detection methods for synthetic cannabinoids and cathinones. Forensic Toxicol. 2015;33(2):175-194.
8. Cone EJ, Lange R, Darwin WD. In vivo adulteration: excess fluid ingestion causes false-negative marijuana and cocaine urine test results. J Anal Toxicol. 1998;22(6):460-473.
9. Jaffee WB, Trucco E, Levy S, et al. Is this urine really negative? A systematic review of tampering methods in urine drug screening and testing. J Subst Abuse Treat. 2007;33(1):33-42.
10. Substance Abuse and Mental Health Services Administration. Mandatory guidelines for federal workplace drug testing programs. Federal Register. 2004;69:19644-19673.
