User login
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
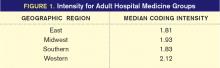
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor