User login
CASE: McRobert’s maneuver fails
You are attempting an early term vaginal delivery of a 31-year-old G2P1 woman with type 2 diabetes mellitus and an estimated fetal weight of 4,100 g. The fetal head has delivered but retracted against the perineum, producing the “turtle sign.”
You call a shoulder dystocia emergency and request help. In sequence, you tell the mother to stop pushing, check for a nuchal cord, and cut a mediolateral episiotomy. Working seamlessly with your nurse, you place the patient at the edge of the bed, perform the McRobert’s maneuver, provide suprapubic pressure and apply gentle downward guidance to the fetal head. Unfortunately, with these maneuvers the baby does not deliver.
What is your next obstetric maneuver?
With alacrity, move on to an advanced maneuver. In this article, I outline your options for this advanced maneuver and describe the technique for execution. First, however, I discuss the amount of time you have to work with.
How long do you have to perform advanced maneuvers?
In managing a difficult shoulder dystocia, critical goals are to avoid permanent injury to the newborn, including brachial plexus injury, fetal asphyxia, central nervous system injury, and death. Many experts believe that the accoucheur has approximately 4 or 5 minutes to deliver the impacted fetus before the risk of these adverse outcomes rises substantially.1-3 In one study, a head-to-body delivery interval of less than 5 minutes and 5 minutes or longer were associated with rates of hypoxic ischemic encephalopathy of 0.5% and 24%, respectively.2
Stay calm, move on. Given the time pressure for management, it is important to initiate an advanced maneuver, such as rotation of the fetal body or delivery of the posterior arm, when the initial sequence of McRobert’s maneuver, suprapubic pressure, and gentle downward guidance on the fetal head do not result in delivery. Repetitively repeating these initial maneuvers will increase the risk of an adverse fetal outcome. Stay calm and quickly move on to an advanced maneuver.
Advanced maneuvers
The two advanced shoulder dystocia maneuvers that often result in a successful birth are:
- rotation of the fetal shoulders
- delivery of the posterior arm.4,5
In a prior editorial, I described in detail the Woods and Rubin rotational maneuvers.6 In this editorial, I focus on the technique for delivery of the posterior arm.
Delivery of the posterior arm
This maneuver to resolve difficult shoulder dystocia deliveries has been in the armamentarium of obstetricians since at least the mid-18th Century.7 The delivery of the posterior arm reduces the presenting fetal diameter from the larger bisacromial diameter to the smaller axilloacromial diameter. Experts estimate that this change results in a 2-cm decrease in the presenting fetal diameter, thereby facilitating delivery.8,9
In describing posterior arm delivery, it is important to clearly define the anatomy of the upper extremity. The arm is the portion of the upper extremity from the shoulder to the elbow joint. The long bone of the arm is the humerus. The forearm is the portion of the upper extremity from the elbow to the wrist. The long bones of the forearm are the radius and ulna.
Descriptions of how to deliver the posterior arm range from concise to detailed. A concise description recommends “inserting a hand in the vagina, grasping the fetal arm, and sweeping it across the chest.”9
These detailed instructions are provided by Dr. John Rodis, Chief of Obstetrics and Gynecology at St. Francis Hospital in Hartford Connecticut, in UpToDate:
Additional technical guidance. After grasping the fetal wrist and hand, pull the upper extremity against the fetal chest. Approaching the vaginal introitus, pull the wrist and hand toward the fetal ear nearest the maternal symphysis pubis.11 These maneuvers may result in a fracture to the humerus, but this complication is acceptable given the risk of fetal asphyxia and death.
Newborn injuries associated with shoulder dystocia | ||
| In a large retrospective study of 132,098 vaginal cephalic singleton births there were 2,018 cases of shoulder dystocia, representing a 1.5% rate of shoulder dystocia during vaginal birth.5A total of 101 neonatal injuries were reported in association with a shoulder dystocia, the most common being Erb’s palsy, clavicular fracture, and hypoxic ischemic encephalopathy. Some newborns incurred multiple injuries. | ||
| Type of injury | No. of newborns with injury | Rate of injury per 100 shoulder dystocias |
| Erb’s palsy | 60 | 3 |
| Clavicular fracture | 39 | 1.9 |
| Hypoxic ischemic encephalopathy | 6 | 0.3 |
| Klumpke’s palsy | 4 | 0.2 |
| Humerus fracture | 2 | 0.1 |
| Neonatal death | 0 | 0 |
Source: Hoffman, et al. Obstet Gynecol. 2011;117(6):1272–1278. | ||
Approaches to grasping the posterior arm
The posterior arm may be in one of three positions, and your approach to each position will be different.
Fetal hand near the chin. Delivery of the posterior arm is relatively easy when the fetal hand is in this position. Grasp the wrist gently and guide it out of the vagina. The fetal wrist should be pulled toward the fetal ear closest to the maternal symphysis.
Fetal hand on the abdomen. In this position, the operator can exert pressure on the antecubital fossa with the index and middle fingers, resulting in flexion of the forearm at the elbow. This will bring the fetal hand and wrist to the upper chest. The wrist then can be grasped and pronated over the fetal chest. The wrist and forearm are then pulled upward along the chest toward the fetal ear closest to the maternal symphysis.
Fetal upper extremity is extended with the hand next to the thigh. The most challenging situation is when the upper extremity of the fetus is extended along the trunk or behind the buttocks. In this situation the hand and wrist may be near the fetal thigh and very difficult to reach. In addition, the upper extremity may be tightly pinned between fetal trunk and maternal tissues, making it impossible to flex the forearm by gentle pressure on the antecubital fossa.
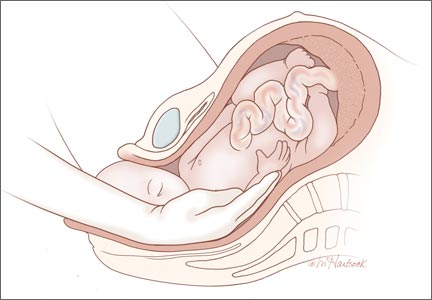
In this situation the operator’s hand must reach the fetal wrist and distal forearm, grasp these structures, and pull hard across the trunk to free the pinned upper extremity. The fetal wrist and distal forearm can be securely grasped using techniques pictured in the Figure. It can take 30 to 90 seconds for the operator to place a hand in the vagina, identify the posterior shoulder, follow the extended arm to the hand, and secure the wrist. Given the amount of time that it may take to accomplish the first steps of the maneuver, the nurse in the room should call out the time elapsed since the birth of the head at regular intervals to assist the obstetrician in pacing the speed of the intervention.
___________________________________________________________________________________________________

| 
| |

| Figure. When the fetal upper extremity is extended and the hand is near the fetal thigh the fetal upper extremity may be tightly pinned between maternal and fetal tissues. Gentle pressure in the antecubital fossa may not cause the forearm to flex toward the vaginal introitus. In this situation it may be very difficult to grasp the fetal wrist or forearm. The operator should be prepared to place their entire hand and forearm into the vagina to reach the fetal wrist (Top left). Two options for grasping the fetal wrist are with the index finger and middle finger (Top right), or by encircling the wrist with the thumb and index finger (Bottom left). For many obstetricians, the index and middle fingers extend much further from their wrist than the thumb. Consequently, when the fetal wrist and hand are against the fetal thigh it may be easier to reach the fetal wrist with the operator’s index and middle finger. However, many obstetricians find that the thumb and index finger provide a more secure grip of the fetal wrist. |
______________________________________________________________________________________________________
When the posterior arm is fully extended and pinned between fetal trunk and maternal tissues it can be very difficult to reach the fetal wrist. To help successfully complete the maneuver, the obstetrician should visualize placing his or her hand and entire forearm up to the elbow in the vagina to reach the fetal wrist. It may not be necessary to insert the entire forearm in the vagina, but the operator should visualize this step so he or she is prepared for the possibility.Surprisingly, the hollow of the sacrum often provides sufficient space for inserting the hand and entire forearm of the operator. In this process the operator’s hand and forearm may be strongly compressed by maternal and fetal tissues, cutting off circulation to the upper extremity. The operator’s upper extremity may quickly become numb, resulting in a reduction in tactile sensation and strength.
If the posterior arm is positioned behind the back of the fetus, maneuvers similar to those described above can be used to grasp the wrist and pull the arm to the anterior side of the fetal trunk, followed by delivery of the posterior arm.
Practice, practice, and practice some more
Obstetric emergencies create a rush of adrenaline and great stress for the obstetrician. This may adversely impact motor performance, decision-making, and communication skills.12 Low- and high-fidelity simulation exercises permit the obstetrics team to practice the sequence of maneuvers necessary to successfully resolve a shoulder dystocia, thereby reducing stress and improving performance when the emergency actually occurs.13 Simulating obstetric emergencies and visualizing the steps necessary to resolve an emergency are good approaches to prepare obstetricians for the most challenging emergencies. For the difficult to resolve shoulder dystocia, my recommendation is: “Deliver the posterior arm.”
Use this checklist to document a shoulder dystocia event
-Safety Checklists
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Allen RH, Rosenbaum TC, Ghidini A, Poggi SH, Spong CY. Correlating head-to-body delivery intervals with neonatal depression in vaginal births that result in permanent brachial plexus injury. Am J Obstet Gynecol. 2002;187(4):839–842.
2. Leung TY, Stuart O, Sahota DS, Suen SS, Lau TK, Lao TT. Head-to-body delivery interval and risk of fetal acidosis and hypoxic ischaemic encephalopathy in shoulder dystocia: a retrospective review. BJOG. 2011;118(4):474–479.
3. Lerner H, Durlacher K, Smith S, Hamilton E. Relationship between head-to-body delivery interval in shoulder dystocia and neonatal depression. Obstet Gynecol. 2011;118(2 pt 1):318–322.
4. Leung TY, Stuart O, Suen SS, Sahota DS, Lau TK, Lao TT. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG. 2011;118(8):985–990.
5. Hoffman MK, Bailit KL, Branch DW, et al. A comparison of obstetric maneuvers for the acute management of should dystocia. Obstet Gynecol. 2011;117(6):1272–1278.
6. Barbieri RL. You are the second responder to a shoulder dystocia emergency. What do you do first? OBG Manag. 2013;25(????):10, 12, 15.
7. Beer E. History of extraction of the posterior arm to resolve shoulder dystocia. Obstet Gynecol Surv. 2006;61(3):149–151.
8. Kung J, Swan AV, Arulkumaran S. Delivery of the posterior arm reduces shoulder dimensions in shoulder dystocia. Int J Gynaecol Obstet. 2006;93(3):233–237.
9. Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol. 2003;101(5 pt 2):1068–1072.
10. Rodis JF. Shoulder dystocia, intrapartum diagnosis, management and outcome. UpToDate, Waltham MA.
11. Mazzanti GA. Delivery of the anterior shoulder; a neglected art. Obstet Gynecol. 1959;13(5):603–607.
12. Wetzel CM, Kneebone RL, Woloshynowych M, et al. The effects of stress on surgical performance. Am J Surg. 2006;191(1):5–10.
13. Grobman WA, Miller D, Burke C, Hornbogen A, Tam K, Costello R. Outcomes associated with introduction of a shoulder dystocia protocol. Am J Obstet Gynecol. 2011;205(6):513–517.
CASE: McRobert’s maneuver fails
You are attempting an early term vaginal delivery of a 31-year-old G2P1 woman with type 2 diabetes mellitus and an estimated fetal weight of 4,100 g. The fetal head has delivered but retracted against the perineum, producing the “turtle sign.”
You call a shoulder dystocia emergency and request help. In sequence, you tell the mother to stop pushing, check for a nuchal cord, and cut a mediolateral episiotomy. Working seamlessly with your nurse, you place the patient at the edge of the bed, perform the McRobert’s maneuver, provide suprapubic pressure and apply gentle downward guidance to the fetal head. Unfortunately, with these maneuvers the baby does not deliver.
What is your next obstetric maneuver?
With alacrity, move on to an advanced maneuver. In this article, I outline your options for this advanced maneuver and describe the technique for execution. First, however, I discuss the amount of time you have to work with.
How long do you have to perform advanced maneuvers?
In managing a difficult shoulder dystocia, critical goals are to avoid permanent injury to the newborn, including brachial plexus injury, fetal asphyxia, central nervous system injury, and death. Many experts believe that the accoucheur has approximately 4 or 5 minutes to deliver the impacted fetus before the risk of these adverse outcomes rises substantially.1-3 In one study, a head-to-body delivery interval of less than 5 minutes and 5 minutes or longer were associated with rates of hypoxic ischemic encephalopathy of 0.5% and 24%, respectively.2
Stay calm, move on. Given the time pressure for management, it is important to initiate an advanced maneuver, such as rotation of the fetal body or delivery of the posterior arm, when the initial sequence of McRobert’s maneuver, suprapubic pressure, and gentle downward guidance on the fetal head do not result in delivery. Repetitively repeating these initial maneuvers will increase the risk of an adverse fetal outcome. Stay calm and quickly move on to an advanced maneuver.
Advanced maneuvers
The two advanced shoulder dystocia maneuvers that often result in a successful birth are:
- rotation of the fetal shoulders
- delivery of the posterior arm.4,5
In a prior editorial, I described in detail the Woods and Rubin rotational maneuvers.6 In this editorial, I focus on the technique for delivery of the posterior arm.
Delivery of the posterior arm
This maneuver to resolve difficult shoulder dystocia deliveries has been in the armamentarium of obstetricians since at least the mid-18th Century.7 The delivery of the posterior arm reduces the presenting fetal diameter from the larger bisacromial diameter to the smaller axilloacromial diameter. Experts estimate that this change results in a 2-cm decrease in the presenting fetal diameter, thereby facilitating delivery.8,9
In describing posterior arm delivery, it is important to clearly define the anatomy of the upper extremity. The arm is the portion of the upper extremity from the shoulder to the elbow joint. The long bone of the arm is the humerus. The forearm is the portion of the upper extremity from the elbow to the wrist. The long bones of the forearm are the radius and ulna.
Descriptions of how to deliver the posterior arm range from concise to detailed. A concise description recommends “inserting a hand in the vagina, grasping the fetal arm, and sweeping it across the chest.”9
These detailed instructions are provided by Dr. John Rodis, Chief of Obstetrics and Gynecology at St. Francis Hospital in Hartford Connecticut, in UpToDate:
Additional technical guidance. After grasping the fetal wrist and hand, pull the upper extremity against the fetal chest. Approaching the vaginal introitus, pull the wrist and hand toward the fetal ear nearest the maternal symphysis pubis.11 These maneuvers may result in a fracture to the humerus, but this complication is acceptable given the risk of fetal asphyxia and death.
Newborn injuries associated with shoulder dystocia | ||
| In a large retrospective study of 132,098 vaginal cephalic singleton births there were 2,018 cases of shoulder dystocia, representing a 1.5% rate of shoulder dystocia during vaginal birth.5A total of 101 neonatal injuries were reported in association with a shoulder dystocia, the most common being Erb’s palsy, clavicular fracture, and hypoxic ischemic encephalopathy. Some newborns incurred multiple injuries. | ||
| Type of injury | No. of newborns with injury | Rate of injury per 100 shoulder dystocias |
| Erb’s palsy | 60 | 3 |
| Clavicular fracture | 39 | 1.9 |
| Hypoxic ischemic encephalopathy | 6 | 0.3 |
| Klumpke’s palsy | 4 | 0.2 |
| Humerus fracture | 2 | 0.1 |
| Neonatal death | 0 | 0 |
Source: Hoffman, et al. Obstet Gynecol. 2011;117(6):1272–1278. | ||
Approaches to grasping the posterior arm
The posterior arm may be in one of three positions, and your approach to each position will be different.
Fetal hand near the chin. Delivery of the posterior arm is relatively easy when the fetal hand is in this position. Grasp the wrist gently and guide it out of the vagina. The fetal wrist should be pulled toward the fetal ear closest to the maternal symphysis.
Fetal hand on the abdomen. In this position, the operator can exert pressure on the antecubital fossa with the index and middle fingers, resulting in flexion of the forearm at the elbow. This will bring the fetal hand and wrist to the upper chest. The wrist then can be grasped and pronated over the fetal chest. The wrist and forearm are then pulled upward along the chest toward the fetal ear closest to the maternal symphysis.
Fetal upper extremity is extended with the hand next to the thigh. The most challenging situation is when the upper extremity of the fetus is extended along the trunk or behind the buttocks. In this situation the hand and wrist may be near the fetal thigh and very difficult to reach. In addition, the upper extremity may be tightly pinned between fetal trunk and maternal tissues, making it impossible to flex the forearm by gentle pressure on the antecubital fossa.
In this situation the operator’s hand must reach the fetal wrist and distal forearm, grasp these structures, and pull hard across the trunk to free the pinned upper extremity. The fetal wrist and distal forearm can be securely grasped using techniques pictured in the Figure. It can take 30 to 90 seconds for the operator to place a hand in the vagina, identify the posterior shoulder, follow the extended arm to the hand, and secure the wrist. Given the amount of time that it may take to accomplish the first steps of the maneuver, the nurse in the room should call out the time elapsed since the birth of the head at regular intervals to assist the obstetrician in pacing the speed of the intervention.
___________________________________________________________________________________________________

| 
| |

| Figure. When the fetal upper extremity is extended and the hand is near the fetal thigh the fetal upper extremity may be tightly pinned between maternal and fetal tissues. Gentle pressure in the antecubital fossa may not cause the forearm to flex toward the vaginal introitus. In this situation it may be very difficult to grasp the fetal wrist or forearm. The operator should be prepared to place their entire hand and forearm into the vagina to reach the fetal wrist (Top left). Two options for grasping the fetal wrist are with the index finger and middle finger (Top right), or by encircling the wrist with the thumb and index finger (Bottom left). For many obstetricians, the index and middle fingers extend much further from their wrist than the thumb. Consequently, when the fetal wrist and hand are against the fetal thigh it may be easier to reach the fetal wrist with the operator’s index and middle finger. However, many obstetricians find that the thumb and index finger provide a more secure grip of the fetal wrist. |
______________________________________________________________________________________________________
When the posterior arm is fully extended and pinned between fetal trunk and maternal tissues it can be very difficult to reach the fetal wrist. To help successfully complete the maneuver, the obstetrician should visualize placing his or her hand and entire forearm up to the elbow in the vagina to reach the fetal wrist. It may not be necessary to insert the entire forearm in the vagina, but the operator should visualize this step so he or she is prepared for the possibility.Surprisingly, the hollow of the sacrum often provides sufficient space for inserting the hand and entire forearm of the operator. In this process the operator’s hand and forearm may be strongly compressed by maternal and fetal tissues, cutting off circulation to the upper extremity. The operator’s upper extremity may quickly become numb, resulting in a reduction in tactile sensation and strength.
If the posterior arm is positioned behind the back of the fetus, maneuvers similar to those described above can be used to grasp the wrist and pull the arm to the anterior side of the fetal trunk, followed by delivery of the posterior arm.
Practice, practice, and practice some more
Obstetric emergencies create a rush of adrenaline and great stress for the obstetrician. This may adversely impact motor performance, decision-making, and communication skills.12 Low- and high-fidelity simulation exercises permit the obstetrics team to practice the sequence of maneuvers necessary to successfully resolve a shoulder dystocia, thereby reducing stress and improving performance when the emergency actually occurs.13 Simulating obstetric emergencies and visualizing the steps necessary to resolve an emergency are good approaches to prepare obstetricians for the most challenging emergencies. For the difficult to resolve shoulder dystocia, my recommendation is: “Deliver the posterior arm.”
Use this checklist to document a shoulder dystocia event
-Safety Checklists
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE: McRobert’s maneuver fails
You are attempting an early term vaginal delivery of a 31-year-old G2P1 woman with type 2 diabetes mellitus and an estimated fetal weight of 4,100 g. The fetal head has delivered but retracted against the perineum, producing the “turtle sign.”
You call a shoulder dystocia emergency and request help. In sequence, you tell the mother to stop pushing, check for a nuchal cord, and cut a mediolateral episiotomy. Working seamlessly with your nurse, you place the patient at the edge of the bed, perform the McRobert’s maneuver, provide suprapubic pressure and apply gentle downward guidance to the fetal head. Unfortunately, with these maneuvers the baby does not deliver.
What is your next obstetric maneuver?
With alacrity, move on to an advanced maneuver. In this article, I outline your options for this advanced maneuver and describe the technique for execution. First, however, I discuss the amount of time you have to work with.
How long do you have to perform advanced maneuvers?
In managing a difficult shoulder dystocia, critical goals are to avoid permanent injury to the newborn, including brachial plexus injury, fetal asphyxia, central nervous system injury, and death. Many experts believe that the accoucheur has approximately 4 or 5 minutes to deliver the impacted fetus before the risk of these adverse outcomes rises substantially.1-3 In one study, a head-to-body delivery interval of less than 5 minutes and 5 minutes or longer were associated with rates of hypoxic ischemic encephalopathy of 0.5% and 24%, respectively.2
Stay calm, move on. Given the time pressure for management, it is important to initiate an advanced maneuver, such as rotation of the fetal body or delivery of the posterior arm, when the initial sequence of McRobert’s maneuver, suprapubic pressure, and gentle downward guidance on the fetal head do not result in delivery. Repetitively repeating these initial maneuvers will increase the risk of an adverse fetal outcome. Stay calm and quickly move on to an advanced maneuver.
Advanced maneuvers
The two advanced shoulder dystocia maneuvers that often result in a successful birth are:
- rotation of the fetal shoulders
- delivery of the posterior arm.4,5
In a prior editorial, I described in detail the Woods and Rubin rotational maneuvers.6 In this editorial, I focus on the technique for delivery of the posterior arm.
Delivery of the posterior arm
This maneuver to resolve difficult shoulder dystocia deliveries has been in the armamentarium of obstetricians since at least the mid-18th Century.7 The delivery of the posterior arm reduces the presenting fetal diameter from the larger bisacromial diameter to the smaller axilloacromial diameter. Experts estimate that this change results in a 2-cm decrease in the presenting fetal diameter, thereby facilitating delivery.8,9
In describing posterior arm delivery, it is important to clearly define the anatomy of the upper extremity. The arm is the portion of the upper extremity from the shoulder to the elbow joint. The long bone of the arm is the humerus. The forearm is the portion of the upper extremity from the elbow to the wrist. The long bones of the forearm are the radius and ulna.
Descriptions of how to deliver the posterior arm range from concise to detailed. A concise description recommends “inserting a hand in the vagina, grasping the fetal arm, and sweeping it across the chest.”9
These detailed instructions are provided by Dr. John Rodis, Chief of Obstetrics and Gynecology at St. Francis Hospital in Hartford Connecticut, in UpToDate:
Additional technical guidance. After grasping the fetal wrist and hand, pull the upper extremity against the fetal chest. Approaching the vaginal introitus, pull the wrist and hand toward the fetal ear nearest the maternal symphysis pubis.11 These maneuvers may result in a fracture to the humerus, but this complication is acceptable given the risk of fetal asphyxia and death.
Newborn injuries associated with shoulder dystocia | ||
| In a large retrospective study of 132,098 vaginal cephalic singleton births there were 2,018 cases of shoulder dystocia, representing a 1.5% rate of shoulder dystocia during vaginal birth.5A total of 101 neonatal injuries were reported in association with a shoulder dystocia, the most common being Erb’s palsy, clavicular fracture, and hypoxic ischemic encephalopathy. Some newborns incurred multiple injuries. | ||
| Type of injury | No. of newborns with injury | Rate of injury per 100 shoulder dystocias |
| Erb’s palsy | 60 | 3 |
| Clavicular fracture | 39 | 1.9 |
| Hypoxic ischemic encephalopathy | 6 | 0.3 |
| Klumpke’s palsy | 4 | 0.2 |
| Humerus fracture | 2 | 0.1 |
| Neonatal death | 0 | 0 |
Source: Hoffman, et al. Obstet Gynecol. 2011;117(6):1272–1278. | ||
Approaches to grasping the posterior arm
The posterior arm may be in one of three positions, and your approach to each position will be different.
Fetal hand near the chin. Delivery of the posterior arm is relatively easy when the fetal hand is in this position. Grasp the wrist gently and guide it out of the vagina. The fetal wrist should be pulled toward the fetal ear closest to the maternal symphysis.
Fetal hand on the abdomen. In this position, the operator can exert pressure on the antecubital fossa with the index and middle fingers, resulting in flexion of the forearm at the elbow. This will bring the fetal hand and wrist to the upper chest. The wrist then can be grasped and pronated over the fetal chest. The wrist and forearm are then pulled upward along the chest toward the fetal ear closest to the maternal symphysis.
Fetal upper extremity is extended with the hand next to the thigh. The most challenging situation is when the upper extremity of the fetus is extended along the trunk or behind the buttocks. In this situation the hand and wrist may be near the fetal thigh and very difficult to reach. In addition, the upper extremity may be tightly pinned between fetal trunk and maternal tissues, making it impossible to flex the forearm by gentle pressure on the antecubital fossa.
In this situation the operator’s hand must reach the fetal wrist and distal forearm, grasp these structures, and pull hard across the trunk to free the pinned upper extremity. The fetal wrist and distal forearm can be securely grasped using techniques pictured in the Figure. It can take 30 to 90 seconds for the operator to place a hand in the vagina, identify the posterior shoulder, follow the extended arm to the hand, and secure the wrist. Given the amount of time that it may take to accomplish the first steps of the maneuver, the nurse in the room should call out the time elapsed since the birth of the head at regular intervals to assist the obstetrician in pacing the speed of the intervention.
___________________________________________________________________________________________________

| 
| |

| Figure. When the fetal upper extremity is extended and the hand is near the fetal thigh the fetal upper extremity may be tightly pinned between maternal and fetal tissues. Gentle pressure in the antecubital fossa may not cause the forearm to flex toward the vaginal introitus. In this situation it may be very difficult to grasp the fetal wrist or forearm. The operator should be prepared to place their entire hand and forearm into the vagina to reach the fetal wrist (Top left). Two options for grasping the fetal wrist are with the index finger and middle finger (Top right), or by encircling the wrist with the thumb and index finger (Bottom left). For many obstetricians, the index and middle fingers extend much further from their wrist than the thumb. Consequently, when the fetal wrist and hand are against the fetal thigh it may be easier to reach the fetal wrist with the operator’s index and middle finger. However, many obstetricians find that the thumb and index finger provide a more secure grip of the fetal wrist. |
______________________________________________________________________________________________________
When the posterior arm is fully extended and pinned between fetal trunk and maternal tissues it can be very difficult to reach the fetal wrist. To help successfully complete the maneuver, the obstetrician should visualize placing his or her hand and entire forearm up to the elbow in the vagina to reach the fetal wrist. It may not be necessary to insert the entire forearm in the vagina, but the operator should visualize this step so he or she is prepared for the possibility.Surprisingly, the hollow of the sacrum often provides sufficient space for inserting the hand and entire forearm of the operator. In this process the operator’s hand and forearm may be strongly compressed by maternal and fetal tissues, cutting off circulation to the upper extremity. The operator’s upper extremity may quickly become numb, resulting in a reduction in tactile sensation and strength.
If the posterior arm is positioned behind the back of the fetus, maneuvers similar to those described above can be used to grasp the wrist and pull the arm to the anterior side of the fetal trunk, followed by delivery of the posterior arm.
Practice, practice, and practice some more
Obstetric emergencies create a rush of adrenaline and great stress for the obstetrician. This may adversely impact motor performance, decision-making, and communication skills.12 Low- and high-fidelity simulation exercises permit the obstetrics team to practice the sequence of maneuvers necessary to successfully resolve a shoulder dystocia, thereby reducing stress and improving performance when the emergency actually occurs.13 Simulating obstetric emergencies and visualizing the steps necessary to resolve an emergency are good approaches to prepare obstetricians for the most challenging emergencies. For the difficult to resolve shoulder dystocia, my recommendation is: “Deliver the posterior arm.”
Use this checklist to document a shoulder dystocia event
-Safety Checklists
Share your thoughts on this article! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
1. Allen RH, Rosenbaum TC, Ghidini A, Poggi SH, Spong CY. Correlating head-to-body delivery intervals with neonatal depression in vaginal births that result in permanent brachial plexus injury. Am J Obstet Gynecol. 2002;187(4):839–842.
2. Leung TY, Stuart O, Sahota DS, Suen SS, Lau TK, Lao TT. Head-to-body delivery interval and risk of fetal acidosis and hypoxic ischaemic encephalopathy in shoulder dystocia: a retrospective review. BJOG. 2011;118(4):474–479.
3. Lerner H, Durlacher K, Smith S, Hamilton E. Relationship between head-to-body delivery interval in shoulder dystocia and neonatal depression. Obstet Gynecol. 2011;118(2 pt 1):318–322.
4. Leung TY, Stuart O, Suen SS, Sahota DS, Lau TK, Lao TT. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG. 2011;118(8):985–990.
5. Hoffman MK, Bailit KL, Branch DW, et al. A comparison of obstetric maneuvers for the acute management of should dystocia. Obstet Gynecol. 2011;117(6):1272–1278.
6. Barbieri RL. You are the second responder to a shoulder dystocia emergency. What do you do first? OBG Manag. 2013;25(????):10, 12, 15.
7. Beer E. History of extraction of the posterior arm to resolve shoulder dystocia. Obstet Gynecol Surv. 2006;61(3):149–151.
8. Kung J, Swan AV, Arulkumaran S. Delivery of the posterior arm reduces shoulder dimensions in shoulder dystocia. Int J Gynaecol Obstet. 2006;93(3):233–237.
9. Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol. 2003;101(5 pt 2):1068–1072.
10. Rodis JF. Shoulder dystocia, intrapartum diagnosis, management and outcome. UpToDate, Waltham MA.
11. Mazzanti GA. Delivery of the anterior shoulder; a neglected art. Obstet Gynecol. 1959;13(5):603–607.
12. Wetzel CM, Kneebone RL, Woloshynowych M, et al. The effects of stress on surgical performance. Am J Surg. 2006;191(1):5–10.
13. Grobman WA, Miller D, Burke C, Hornbogen A, Tam K, Costello R. Outcomes associated with introduction of a shoulder dystocia protocol. Am J Obstet Gynecol. 2011;205(6):513–517.
1. Allen RH, Rosenbaum TC, Ghidini A, Poggi SH, Spong CY. Correlating head-to-body delivery intervals with neonatal depression in vaginal births that result in permanent brachial plexus injury. Am J Obstet Gynecol. 2002;187(4):839–842.
2. Leung TY, Stuart O, Sahota DS, Suen SS, Lau TK, Lao TT. Head-to-body delivery interval and risk of fetal acidosis and hypoxic ischaemic encephalopathy in shoulder dystocia: a retrospective review. BJOG. 2011;118(4):474–479.
3. Lerner H, Durlacher K, Smith S, Hamilton E. Relationship between head-to-body delivery interval in shoulder dystocia and neonatal depression. Obstet Gynecol. 2011;118(2 pt 1):318–322.
4. Leung TY, Stuart O, Suen SS, Sahota DS, Lau TK, Lao TT. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG. 2011;118(8):985–990.
5. Hoffman MK, Bailit KL, Branch DW, et al. A comparison of obstetric maneuvers for the acute management of should dystocia. Obstet Gynecol. 2011;117(6):1272–1278.
6. Barbieri RL. You are the second responder to a shoulder dystocia emergency. What do you do first? OBG Manag. 2013;25(????):10, 12, 15.
7. Beer E. History of extraction of the posterior arm to resolve shoulder dystocia. Obstet Gynecol Surv. 2006;61(3):149–151.
8. Kung J, Swan AV, Arulkumaran S. Delivery of the posterior arm reduces shoulder dimensions in shoulder dystocia. Int J Gynaecol Obstet. 2006;93(3):233–237.
9. Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol. 2003;101(5 pt 2):1068–1072.
10. Rodis JF. Shoulder dystocia, intrapartum diagnosis, management and outcome. UpToDate, Waltham MA.
11. Mazzanti GA. Delivery of the anterior shoulder; a neglected art. Obstet Gynecol. 1959;13(5):603–607.
12. Wetzel CM, Kneebone RL, Woloshynowych M, et al. The effects of stress on surgical performance. Am J Surg. 2006;191(1):5–10.
13. Grobman WA, Miller D, Burke C, Hornbogen A, Tam K, Costello R. Outcomes associated with introduction of a shoulder dystocia protocol. Am J Obstet Gynecol. 2011;205(6):513–517.