User login
Have too many low-risk U.S. patients undergone transcatheter aortic-valve replacement since the procedure became available in October 2012 to U.S. patients who are also judged eligible for surgical aortic-valve replacement?
Furthermore, regardless of the answer, are the tools currently available to cardiologists and cardiac surgeons to estimate a patient’s risk for undergoing aortic-valve surgery too limited and flawed to even allow clinicians to reasonably judge who is at high risk for surgical valve replacement and who isn’t?
And finally, have the benefits of transcatheter aortic valve replacement (TAVR) as an alternative to surgery become so compelling that patients, cardiologists, and surgeons are all now willing to ignore the possible downside that still remains to TAVR and the risk-level ground rules that the field set up just a few years ago?
Answering the third question is probably the easiest, and the answer seems to be yes, at least based on U.S. use of TAVR since the first valve system came onto the U.S. market for inoperable patients in November 2011, as well as on what happened in the latest big TAVR trial. Last November, researchers published a report on the first 7,710 U.S. TAVR patients, while results from the latest big trial, the CoreValve pivotal trial, came out in March.
A key finding in the JAMA report last November on nearly 8,000 TAVR recipients, most of whom were operable patients once this indication received U.S. approval in 2012, was that the median Predicted Risk of Operative Mortality score by the formula crafted by the Society of Thoracic Surgeons (the STS PROM score) was 7%, and a quarter of all U.S. patients had a score of 5% or less. Those risk levels are quite low relative to the levels in the first TAVR pivotal trial, the PARTNER I trial, and relative to how TAVR developers viewed the role for this technology when it first entered the U.S. market a couple of years ago.
In the first U.S. pivotal trial for TAVR in patients judged operable, a head-to-head comparison of TAVR and surgical aortic valve replacement (SAVR), all enrolled patients had to have an STS PROM score of at least 10%, and the average score of enrolled patients was 11.8%. Labeling for the first U.S. approved TAVR system was for patients with an STS PROM score of at least 8%. The follow-up trial designed to test a second-generation TAVR device, PARTNER II, launched about 3 years ago and not scheduled to finish until the end of 2015, specifically targeted "intermediate-risk" patients with aortic stenosis, those with an STS PROM of 4%-8%. Even this next-generation-device trial, PARTNER II, wasn’t designed to target patients with risk levels of less than 4%, yet patients of that very sort have already received treatment with the first-generation device based on the registry results.
It’s not just the registry that shows a shift toward lower-risk patients. The CoreValve pivotal trial that pitted a different TAVR system head to head against SAVR showed more of the same. The trial was designed to enroll operable patients with a predicted 30-day mortality risk after SAVR of at least 15%, though the study left it up to clinicians to decide how to measure risk and gave them free rein to use parameters in addition to the STS PROM score. The result was that the average STS PROM score of enrolled patients in the CoreValve trial was 7%, and roughly 10% of enrolled patients had a score of less than 4%. The temptation to use TAVR on lower-risk patients seems to have been inescapable, happening in both the CoreValve trial as well as in the registry’s Sapien experience.
Of course, the CoreValve results also showed significant survival benefit from TAVR using the CoreValve system, a game-changing result.
Part of what has been going on with risk assessment is that in the CoreValve study as well as in routine practice, clinicians have been fudging their use of the STS PROM score when sizing up patients for TAVR. I asked several interventional cardiologists about this at the ACC meeting in March, and their answers were all variants of what Dr. James Hermiller told me: "It’s frailty that often gets a patient to TAVR, and frailty is hard to quantify. Frailty can exist even when the STS score is not high." And even though labeling for the first-generation TAVR system that all 7,710 of the first U.S. patients received specified an STS PROM score of at least 8%, Dr. David Holmes told me that for Medicare reimbursement, all that’s needed is for two cardiac surgeons to sign off on saying that the patient’s status warrants TAVR. "That’s what carries the day," he said.
Data from the new CoreValve study underscore how limited the STS PROM score is right now. The average score of the patients enrolled in the surgical arm of this study was 7.5%, which means that 7.5 % of the patients who underwent SAVR were predicted by the scoring system to die during the first 30 days after surgery. But the actual rate was 4.5%, "substantially lower," said the CoreValve report. STS PROM scoring resulted in a substantial overcall on predicted risk.
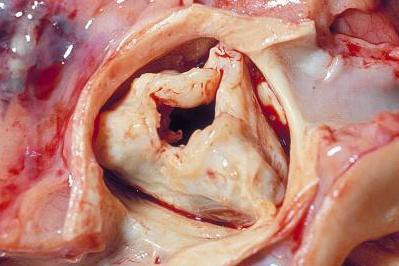
When TAVR was first introduced, experts had two caveats about its potential to completely replace SAVR. The first was uncertainty about the long-term durability (think 10 or more years) of TAVR. The second was uncertainty about the short- and intermediate-term safety and efficacy of TAVR, especially for the patients for whom conventional SAVR was a reasonable option.
Doubts about short- and intermediate-term efficacy arose with the first-generation TAVR device, Sapien, because of the issue of paravalvular leak and the inability of TAVR to surpass SAVR outcomes in the PARTNER I results, but those doubts have now been mostly swept away from by the CoreValve results, which established CoreValve as superior to SAVR and made it the current standard for essentially all patients who need their aortic valve replaced. Even if paravalvular leak is still an issue for some patients, patients treated with CoreValve, TAVR overall did significantly better after 1 year than SAVR in the CoreValve trial, which means that TAVR was best regardless of whether paravalvular leak was an issue for some patients. And this was in patients who represented a wide range of STS PROM risk, with close to 10% of enrolled patients having a score of less than 4%. A subanalysis showed that the low-risk patients derived as much benefit from CoreValve TAVR, compared with SAVR, as did higher-risk patients.
The long-term durability question still remains for now, but the substantial mortality benefit in the CoreValve trial seen after 1 year probably trumps that.
Researchers designed the TAVR trials to methodically progress through a spectrum of patient risk levels. As recently as a year ago, several experts told me that no way in the near future could TAVR be an option for low-risk patients with STS PROM scores of less than 4%. But that is not how it has worked out. Patients, cardiac surgeons, and cardiologists embraced TAVR way faster and tighter than anyone expected just a few years ago.
On Twitter @mitchelzoler
Have too many low-risk U.S. patients undergone transcatheter aortic-valve replacement since the procedure became available in October 2012 to U.S. patients who are also judged eligible for surgical aortic-valve replacement?
Furthermore, regardless of the answer, are the tools currently available to cardiologists and cardiac surgeons to estimate a patient’s risk for undergoing aortic-valve surgery too limited and flawed to even allow clinicians to reasonably judge who is at high risk for surgical valve replacement and who isn’t?
And finally, have the benefits of transcatheter aortic valve replacement (TAVR) as an alternative to surgery become so compelling that patients, cardiologists, and surgeons are all now willing to ignore the possible downside that still remains to TAVR and the risk-level ground rules that the field set up just a few years ago?
Answering the third question is probably the easiest, and the answer seems to be yes, at least based on U.S. use of TAVR since the first valve system came onto the U.S. market for inoperable patients in November 2011, as well as on what happened in the latest big TAVR trial. Last November, researchers published a report on the first 7,710 U.S. TAVR patients, while results from the latest big trial, the CoreValve pivotal trial, came out in March.
A key finding in the JAMA report last November on nearly 8,000 TAVR recipients, most of whom were operable patients once this indication received U.S. approval in 2012, was that the median Predicted Risk of Operative Mortality score by the formula crafted by the Society of Thoracic Surgeons (the STS PROM score) was 7%, and a quarter of all U.S. patients had a score of 5% or less. Those risk levels are quite low relative to the levels in the first TAVR pivotal trial, the PARTNER I trial, and relative to how TAVR developers viewed the role for this technology when it first entered the U.S. market a couple of years ago.
In the first U.S. pivotal trial for TAVR in patients judged operable, a head-to-head comparison of TAVR and surgical aortic valve replacement (SAVR), all enrolled patients had to have an STS PROM score of at least 10%, and the average score of enrolled patients was 11.8%. Labeling for the first U.S. approved TAVR system was for patients with an STS PROM score of at least 8%. The follow-up trial designed to test a second-generation TAVR device, PARTNER II, launched about 3 years ago and not scheduled to finish until the end of 2015, specifically targeted "intermediate-risk" patients with aortic stenosis, those with an STS PROM of 4%-8%. Even this next-generation-device trial, PARTNER II, wasn’t designed to target patients with risk levels of less than 4%, yet patients of that very sort have already received treatment with the first-generation device based on the registry results.
It’s not just the registry that shows a shift toward lower-risk patients. The CoreValve pivotal trial that pitted a different TAVR system head to head against SAVR showed more of the same. The trial was designed to enroll operable patients with a predicted 30-day mortality risk after SAVR of at least 15%, though the study left it up to clinicians to decide how to measure risk and gave them free rein to use parameters in addition to the STS PROM score. The result was that the average STS PROM score of enrolled patients in the CoreValve trial was 7%, and roughly 10% of enrolled patients had a score of less than 4%. The temptation to use TAVR on lower-risk patients seems to have been inescapable, happening in both the CoreValve trial as well as in the registry’s Sapien experience.
Of course, the CoreValve results also showed significant survival benefit from TAVR using the CoreValve system, a game-changing result.
Part of what has been going on with risk assessment is that in the CoreValve study as well as in routine practice, clinicians have been fudging their use of the STS PROM score when sizing up patients for TAVR. I asked several interventional cardiologists about this at the ACC meeting in March, and their answers were all variants of what Dr. James Hermiller told me: "It’s frailty that often gets a patient to TAVR, and frailty is hard to quantify. Frailty can exist even when the STS score is not high." And even though labeling for the first-generation TAVR system that all 7,710 of the first U.S. patients received specified an STS PROM score of at least 8%, Dr. David Holmes told me that for Medicare reimbursement, all that’s needed is for two cardiac surgeons to sign off on saying that the patient’s status warrants TAVR. "That’s what carries the day," he said.
Data from the new CoreValve study underscore how limited the STS PROM score is right now. The average score of the patients enrolled in the surgical arm of this study was 7.5%, which means that 7.5 % of the patients who underwent SAVR were predicted by the scoring system to die during the first 30 days after surgery. But the actual rate was 4.5%, "substantially lower," said the CoreValve report. STS PROM scoring resulted in a substantial overcall on predicted risk.
When TAVR was first introduced, experts had two caveats about its potential to completely replace SAVR. The first was uncertainty about the long-term durability (think 10 or more years) of TAVR. The second was uncertainty about the short- and intermediate-term safety and efficacy of TAVR, especially for the patients for whom conventional SAVR was a reasonable option.
Doubts about short- and intermediate-term efficacy arose with the first-generation TAVR device, Sapien, because of the issue of paravalvular leak and the inability of TAVR to surpass SAVR outcomes in the PARTNER I results, but those doubts have now been mostly swept away from by the CoreValve results, which established CoreValve as superior to SAVR and made it the current standard for essentially all patients who need their aortic valve replaced. Even if paravalvular leak is still an issue for some patients, patients treated with CoreValve, TAVR overall did significantly better after 1 year than SAVR in the CoreValve trial, which means that TAVR was best regardless of whether paravalvular leak was an issue for some patients. And this was in patients who represented a wide range of STS PROM risk, with close to 10% of enrolled patients having a score of less than 4%. A subanalysis showed that the low-risk patients derived as much benefit from CoreValve TAVR, compared with SAVR, as did higher-risk patients.
The long-term durability question still remains for now, but the substantial mortality benefit in the CoreValve trial seen after 1 year probably trumps that.
Researchers designed the TAVR trials to methodically progress through a spectrum of patient risk levels. As recently as a year ago, several experts told me that no way in the near future could TAVR be an option for low-risk patients with STS PROM scores of less than 4%. But that is not how it has worked out. Patients, cardiac surgeons, and cardiologists embraced TAVR way faster and tighter than anyone expected just a few years ago.
On Twitter @mitchelzoler
Have too many low-risk U.S. patients undergone transcatheter aortic-valve replacement since the procedure became available in October 2012 to U.S. patients who are also judged eligible for surgical aortic-valve replacement?
Furthermore, regardless of the answer, are the tools currently available to cardiologists and cardiac surgeons to estimate a patient’s risk for undergoing aortic-valve surgery too limited and flawed to even allow clinicians to reasonably judge who is at high risk for surgical valve replacement and who isn’t?
And finally, have the benefits of transcatheter aortic valve replacement (TAVR) as an alternative to surgery become so compelling that patients, cardiologists, and surgeons are all now willing to ignore the possible downside that still remains to TAVR and the risk-level ground rules that the field set up just a few years ago?
Answering the third question is probably the easiest, and the answer seems to be yes, at least based on U.S. use of TAVR since the first valve system came onto the U.S. market for inoperable patients in November 2011, as well as on what happened in the latest big TAVR trial. Last November, researchers published a report on the first 7,710 U.S. TAVR patients, while results from the latest big trial, the CoreValve pivotal trial, came out in March.
A key finding in the JAMA report last November on nearly 8,000 TAVR recipients, most of whom were operable patients once this indication received U.S. approval in 2012, was that the median Predicted Risk of Operative Mortality score by the formula crafted by the Society of Thoracic Surgeons (the STS PROM score) was 7%, and a quarter of all U.S. patients had a score of 5% or less. Those risk levels are quite low relative to the levels in the first TAVR pivotal trial, the PARTNER I trial, and relative to how TAVR developers viewed the role for this technology when it first entered the U.S. market a couple of years ago.
In the first U.S. pivotal trial for TAVR in patients judged operable, a head-to-head comparison of TAVR and surgical aortic valve replacement (SAVR), all enrolled patients had to have an STS PROM score of at least 10%, and the average score of enrolled patients was 11.8%. Labeling for the first U.S. approved TAVR system was for patients with an STS PROM score of at least 8%. The follow-up trial designed to test a second-generation TAVR device, PARTNER II, launched about 3 years ago and not scheduled to finish until the end of 2015, specifically targeted "intermediate-risk" patients with aortic stenosis, those with an STS PROM of 4%-8%. Even this next-generation-device trial, PARTNER II, wasn’t designed to target patients with risk levels of less than 4%, yet patients of that very sort have already received treatment with the first-generation device based on the registry results.
It’s not just the registry that shows a shift toward lower-risk patients. The CoreValve pivotal trial that pitted a different TAVR system head to head against SAVR showed more of the same. The trial was designed to enroll operable patients with a predicted 30-day mortality risk after SAVR of at least 15%, though the study left it up to clinicians to decide how to measure risk and gave them free rein to use parameters in addition to the STS PROM score. The result was that the average STS PROM score of enrolled patients in the CoreValve trial was 7%, and roughly 10% of enrolled patients had a score of less than 4%. The temptation to use TAVR on lower-risk patients seems to have been inescapable, happening in both the CoreValve trial as well as in the registry’s Sapien experience.
Of course, the CoreValve results also showed significant survival benefit from TAVR using the CoreValve system, a game-changing result.
Part of what has been going on with risk assessment is that in the CoreValve study as well as in routine practice, clinicians have been fudging their use of the STS PROM score when sizing up patients for TAVR. I asked several interventional cardiologists about this at the ACC meeting in March, and their answers were all variants of what Dr. James Hermiller told me: "It’s frailty that often gets a patient to TAVR, and frailty is hard to quantify. Frailty can exist even when the STS score is not high." And even though labeling for the first-generation TAVR system that all 7,710 of the first U.S. patients received specified an STS PROM score of at least 8%, Dr. David Holmes told me that for Medicare reimbursement, all that’s needed is for two cardiac surgeons to sign off on saying that the patient’s status warrants TAVR. "That’s what carries the day," he said.
Data from the new CoreValve study underscore how limited the STS PROM score is right now. The average score of the patients enrolled in the surgical arm of this study was 7.5%, which means that 7.5 % of the patients who underwent SAVR were predicted by the scoring system to die during the first 30 days after surgery. But the actual rate was 4.5%, "substantially lower," said the CoreValve report. STS PROM scoring resulted in a substantial overcall on predicted risk.
When TAVR was first introduced, experts had two caveats about its potential to completely replace SAVR. The first was uncertainty about the long-term durability (think 10 or more years) of TAVR. The second was uncertainty about the short- and intermediate-term safety and efficacy of TAVR, especially for the patients for whom conventional SAVR was a reasonable option.
Doubts about short- and intermediate-term efficacy arose with the first-generation TAVR device, Sapien, because of the issue of paravalvular leak and the inability of TAVR to surpass SAVR outcomes in the PARTNER I results, but those doubts have now been mostly swept away from by the CoreValve results, which established CoreValve as superior to SAVR and made it the current standard for essentially all patients who need their aortic valve replaced. Even if paravalvular leak is still an issue for some patients, patients treated with CoreValve, TAVR overall did significantly better after 1 year than SAVR in the CoreValve trial, which means that TAVR was best regardless of whether paravalvular leak was an issue for some patients. And this was in patients who represented a wide range of STS PROM risk, with close to 10% of enrolled patients having a score of less than 4%. A subanalysis showed that the low-risk patients derived as much benefit from CoreValve TAVR, compared with SAVR, as did higher-risk patients.
The long-term durability question still remains for now, but the substantial mortality benefit in the CoreValve trial seen after 1 year probably trumps that.
Researchers designed the TAVR trials to methodically progress through a spectrum of patient risk levels. As recently as a year ago, several experts told me that no way in the near future could TAVR be an option for low-risk patients with STS PROM scores of less than 4%. But that is not how it has worked out. Patients, cardiac surgeons, and cardiologists embraced TAVR way faster and tighter than anyone expected just a few years ago.
On Twitter @mitchelzoler