User login
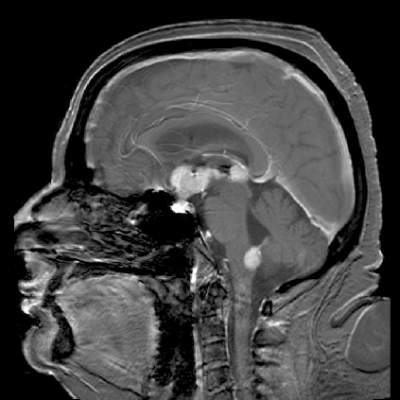
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
Single-agent therapy with temsirolimus was active in patients with relapsed/refractory primary central nervous system lymphoma, but most of the responses were short lived, results of a phase II trial show.
Among 37 patients with primary CNS lymphoma (PCNSL) for whom firstline therapy had failed, there were five complete responses (CR), three CR unconfirmed, and 12 partial responses (PR), for an overall response rate (ORR) of 54%, reported Dr. Agnieszka Korfel from Charité University Medicine Berlin (Germany) and colleagues.
The median progression-free survival (PFS), however, was just 2.1 months, although 1 patient had PFS of 15.8 months duration, and another had a response lasting for more than 44 months, the investigators noted in a study published online in the Journal of Clinical Oncology (doi: 10.1200/JCO.2015.64.9897).
The rationale for trying temsirolimus (Torisel), an inhibitor of the mammalian target of rapamycin (mTOR), came from studies showing the drug’s efficacy against relapsed/refractory mantle-cell lymphoma and against other, more aggressive forms of non-Hodgkin lymphoma. Patients with relapsed/refractory aggressive lymphomas tolerate temsirolimus relatively well, and the drug has the ability to penetrate brain tumor tissue, the authors noted.
They enrolled 37 patients with a median age of 70 years and a median time since their last treatment of 3.9 months into an open-label trial. The patients were all immuncompetent with histologically confirmed primary central nervous system lymphoma for whom high-dose methotrexate-based chemotherapy had failed and for whom high-dose chemotherapy with autologous stem cell transplant had either failed or was not an option.
The first six patients were treated with temsirolimus 25 mg intravenously once weekly, and the remaining 31 were treated with 75 mg IV once weekly until disease progression, intolerable toxicity, patient or physician decision to terminate, or death.
As noted before, ORR, the primary endpoint, was 54%. Median overall survival (OS), a secondary endpoint, was 3.7 months, and 1-year and 2-year OS were 19% and 16.2%, respectively.
The most frequently occurring toxicities include hyperglycemia, myelosuppression, pneumonias and other infections, and fatigue. A total of 28 severe adverse events occurred in 21 patients, including infectious episodes, hospitalizations because of disease progression, deep-vein thromboses, hyperglycemia, and one case each of seizures, grade 4 thrombocytopenia, drug fever, hyponatremia, renal insufficiency, and atrial fibrillation.
“Although most responses were short lived, some patients achieved long-term control. Thus, further evaluation in combination with other drugs seems reasonable. However, one has to be aware of the risk of hematotoxicity and infections necessitating primary antibiotic prophylaxis. Definition of biomarkers allowing identification of potential responders and those who are at particular risk for toxicity would be highly desirable,” the investigators concluded.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Relapsed/refractory primary CNS lymphoma has a poor prognosis and no standard treatment option.
Major finding: The overall response rate to once-weekly temsirolimus was 54%; most responses were short lived.
Data source: Open-label phase 2 study in 37 adults with relapsed/refractory primary CNS lymphoma.
Disclosures: The study was supported by Pfizer Germany. Dr. Korfel and several colleagues disclosed research support from or consulting/advising for the company.