User login
in a new study. The association was independent of other cardiometabolic risk factors and measures of adiposity such as body mass index.
The observation raises the possibility of new avenues of research aimed at modifying intramuscular fat levels as a strategy to reduce the risk of developing heart failure.
The study was published online in JACC: Heart Failure.
The authors, led by Kevin Huynh, MD, University of Texas Southwestern Medical Center, Dallas, explained that obesity is a known risk for heart failure, and has been incorporated into risk calculators for heart failure.
However, obesity is a complex and heterogeneous disease with substantial regional variability of adipose deposition in body tissues, they noted. For example, variability in visceral adipose tissue and subcutaneous adipose tissue has been shown to have a differential impact on both cardiovascular risk factors and clinical cardiovascular disease outcomes.
The fat deposition around and within nonadipose tissues (termed “ectopic fat”), such as skeletal muscle, is also a known risk factor for cardiovascular disease, independent of adiposity. However, the impact of peripheral skeletal muscle fat deposition on heart failure risk is not as well studied.
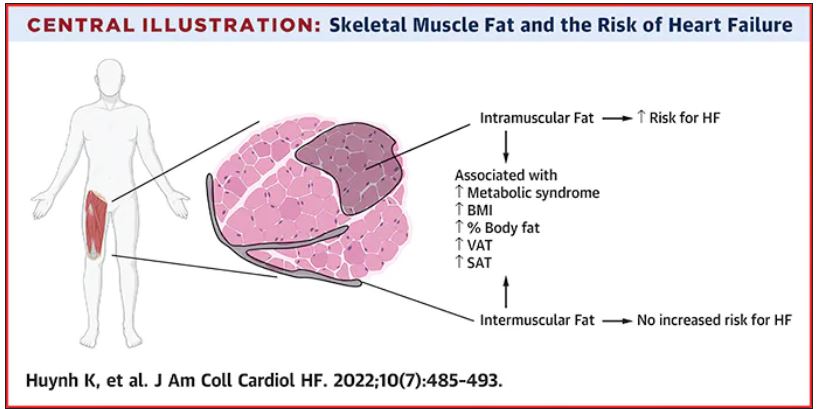
The researchers noted that ectopic fat in skeletal muscle can be measured through imaging and categorized as either intermuscular or intramuscular fat according to the location of muscle fat around or within skeletal muscle, respectively.
The researchers conducted the current study to characterize the association of both intermuscular and intramuscular fat deposition with heart failure risk in a large cohort of older adults.
They used data from 2,399 individuals aged 70-79 years without heart failure at baseline who participated in the Health ABC (Health, Aging and Body Composition) study. Measures of intramuscular and intermuscular fat in the thigh were determined by CT, and the participants were followed for an average of 12 years.
During the follow-up period, there were 485 incident heart failure events. Higher sex-specific tertiles of intramuscular and intermuscular fat were each associated with heart failure risk.
After multivariable adjustment for age, sex, race, education, blood pressure, fasting blood sugar, current smoking, prevalent coronary disease, and creatinine, higher intramuscular fat, but not intermuscular fat, was significantly associated with higher risk for heart failure.
Individuals in the highest tertile of intramuscular fat had a 34% increased risk of developing heart failure, compared with those in the lowest tertile. This finding was independent of other cardiometabolic risk factors, measures of adiposity including body mass index and percent fat, muscle strength, and muscle mass.
The association was slightly attenuated when adjusted for inflammatory markers, suggesting that inflammation may be a contributor.
The association between higher intramuscular fat and heart failure appeared specific to higher risk of incident heart failure with reduced ejection fraction, but not with heart failure with preserved ejection fraction.
The researchers noted that skeletal muscle is a pivotal endocrine organ in addition to the role it plays in the production of mechanical power.
They pointed out that there are differences in the biology of intermuscular and intramuscular fat deposition, and that excess intramuscular fat deposition is a result of dysregulated lipid metabolism and is associated with insulin resistance (a known risk factor for the development of heart failure), inflammation, and muscle wasting conditions.
They concluded that, in patients with heart failure, alterations in skeletal muscle function are most likely affected by multiple contributors, including inflammation, oxidative stress, and neurohormonal factors. “As these factors are also implicated in the pathogenesis of heart failure, intramuscular fat deposition may indicate a biological milieu that increases the risk of heart failure.”
New approaches to reduce heart failure risk?
In an accompanying editorial, Salvatore Carbone, PhD, Virginia Commonwealth University, Richmond, said the findings of the study are “exceptionally novel,” providing novel evidence that noncardiac body composition compartments, particularly intramuscular adipose tissue, can predict the risk for heart failure in a diverse population of older adults.
He called for further research to understand the mechanisms involved and to assess if this risk factor can be effectively modified to reduce the risk of developing heart failure.
Dr. Carbone reported that intramuscular adipose tissue can be influenced by dietary fat intake and can be worsened by accumulation of saturated fatty acids, which also contribute to insulin resistance.
He noted that saturated fatty acid–induced insulin resistance in the skeletal muscle appears to be mediated by proinflammatory pathways within the skeletal muscle itself, which can be reversed by monounsaturated fatty acids, like oleic acid, that can be found in the largest amount in food like olive oil, canola oil, and avocados, among others.
He added that sodium-glucose transporter 2 inhibitors, drugs used in the treatment of diabetes that have also been shown to prevent heart failure in individuals at risk, can also improve the composition of intramuscular adipose tissue by reducing its content of saturated fatty acids and increase the content of monosaturated fatty acids.
The study results suggest that the quality of intramuscular adipose tissue might also play an important role and could be targeted by therapeutic strategies, he commented.
Dr. Carbone concluded that “studies testing novel modalities of exercise training, intentional weight loss, diet quality improvements with and without weight loss (i.e., increase of dietary monounsaturated fatty acids, such as oleic acid), as well as pharmacological anti-inflammatory strategies should be encouraged in this population to test whether the reduction in intramuscular adipose tissue or improvements of its quality can ultimately reduce the risk for heart failure in this population.”
This research was supported by the National Institute on Aging and the National Institute of Nursing Research. Dr. Huynh and Dr. Carbone disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in a new study. The association was independent of other cardiometabolic risk factors and measures of adiposity such as body mass index.
The observation raises the possibility of new avenues of research aimed at modifying intramuscular fat levels as a strategy to reduce the risk of developing heart failure.
The study was published online in JACC: Heart Failure.
The authors, led by Kevin Huynh, MD, University of Texas Southwestern Medical Center, Dallas, explained that obesity is a known risk for heart failure, and has been incorporated into risk calculators for heart failure.
However, obesity is a complex and heterogeneous disease with substantial regional variability of adipose deposition in body tissues, they noted. For example, variability in visceral adipose tissue and subcutaneous adipose tissue has been shown to have a differential impact on both cardiovascular risk factors and clinical cardiovascular disease outcomes.
The fat deposition around and within nonadipose tissues (termed “ectopic fat”), such as skeletal muscle, is also a known risk factor for cardiovascular disease, independent of adiposity. However, the impact of peripheral skeletal muscle fat deposition on heart failure risk is not as well studied.
The researchers noted that ectopic fat in skeletal muscle can be measured through imaging and categorized as either intermuscular or intramuscular fat according to the location of muscle fat around or within skeletal muscle, respectively.
The researchers conducted the current study to characterize the association of both intermuscular and intramuscular fat deposition with heart failure risk in a large cohort of older adults.
They used data from 2,399 individuals aged 70-79 years without heart failure at baseline who participated in the Health ABC (Health, Aging and Body Composition) study. Measures of intramuscular and intermuscular fat in the thigh were determined by CT, and the participants were followed for an average of 12 years.
During the follow-up period, there were 485 incident heart failure events. Higher sex-specific tertiles of intramuscular and intermuscular fat were each associated with heart failure risk.
After multivariable adjustment for age, sex, race, education, blood pressure, fasting blood sugar, current smoking, prevalent coronary disease, and creatinine, higher intramuscular fat, but not intermuscular fat, was significantly associated with higher risk for heart failure.
Individuals in the highest tertile of intramuscular fat had a 34% increased risk of developing heart failure, compared with those in the lowest tertile. This finding was independent of other cardiometabolic risk factors, measures of adiposity including body mass index and percent fat, muscle strength, and muscle mass.
The association was slightly attenuated when adjusted for inflammatory markers, suggesting that inflammation may be a contributor.
The association between higher intramuscular fat and heart failure appeared specific to higher risk of incident heart failure with reduced ejection fraction, but not with heart failure with preserved ejection fraction.
The researchers noted that skeletal muscle is a pivotal endocrine organ in addition to the role it plays in the production of mechanical power.
They pointed out that there are differences in the biology of intermuscular and intramuscular fat deposition, and that excess intramuscular fat deposition is a result of dysregulated lipid metabolism and is associated with insulin resistance (a known risk factor for the development of heart failure), inflammation, and muscle wasting conditions.
They concluded that, in patients with heart failure, alterations in skeletal muscle function are most likely affected by multiple contributors, including inflammation, oxidative stress, and neurohormonal factors. “As these factors are also implicated in the pathogenesis of heart failure, intramuscular fat deposition may indicate a biological milieu that increases the risk of heart failure.”
New approaches to reduce heart failure risk?
In an accompanying editorial, Salvatore Carbone, PhD, Virginia Commonwealth University, Richmond, said the findings of the study are “exceptionally novel,” providing novel evidence that noncardiac body composition compartments, particularly intramuscular adipose tissue, can predict the risk for heart failure in a diverse population of older adults.
He called for further research to understand the mechanisms involved and to assess if this risk factor can be effectively modified to reduce the risk of developing heart failure.
Dr. Carbone reported that intramuscular adipose tissue can be influenced by dietary fat intake and can be worsened by accumulation of saturated fatty acids, which also contribute to insulin resistance.
He noted that saturated fatty acid–induced insulin resistance in the skeletal muscle appears to be mediated by proinflammatory pathways within the skeletal muscle itself, which can be reversed by monounsaturated fatty acids, like oleic acid, that can be found in the largest amount in food like olive oil, canola oil, and avocados, among others.
He added that sodium-glucose transporter 2 inhibitors, drugs used in the treatment of diabetes that have also been shown to prevent heart failure in individuals at risk, can also improve the composition of intramuscular adipose tissue by reducing its content of saturated fatty acids and increase the content of monosaturated fatty acids.
The study results suggest that the quality of intramuscular adipose tissue might also play an important role and could be targeted by therapeutic strategies, he commented.
Dr. Carbone concluded that “studies testing novel modalities of exercise training, intentional weight loss, diet quality improvements with and without weight loss (i.e., increase of dietary monounsaturated fatty acids, such as oleic acid), as well as pharmacological anti-inflammatory strategies should be encouraged in this population to test whether the reduction in intramuscular adipose tissue or improvements of its quality can ultimately reduce the risk for heart failure in this population.”
This research was supported by the National Institute on Aging and the National Institute of Nursing Research. Dr. Huynh and Dr. Carbone disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in a new study. The association was independent of other cardiometabolic risk factors and measures of adiposity such as body mass index.
The observation raises the possibility of new avenues of research aimed at modifying intramuscular fat levels as a strategy to reduce the risk of developing heart failure.
The study was published online in JACC: Heart Failure.
The authors, led by Kevin Huynh, MD, University of Texas Southwestern Medical Center, Dallas, explained that obesity is a known risk for heart failure, and has been incorporated into risk calculators for heart failure.
However, obesity is a complex and heterogeneous disease with substantial regional variability of adipose deposition in body tissues, they noted. For example, variability in visceral adipose tissue and subcutaneous adipose tissue has been shown to have a differential impact on both cardiovascular risk factors and clinical cardiovascular disease outcomes.
The fat deposition around and within nonadipose tissues (termed “ectopic fat”), such as skeletal muscle, is also a known risk factor for cardiovascular disease, independent of adiposity. However, the impact of peripheral skeletal muscle fat deposition on heart failure risk is not as well studied.
The researchers noted that ectopic fat in skeletal muscle can be measured through imaging and categorized as either intermuscular or intramuscular fat according to the location of muscle fat around or within skeletal muscle, respectively.
The researchers conducted the current study to characterize the association of both intermuscular and intramuscular fat deposition with heart failure risk in a large cohort of older adults.
They used data from 2,399 individuals aged 70-79 years without heart failure at baseline who participated in the Health ABC (Health, Aging and Body Composition) study. Measures of intramuscular and intermuscular fat in the thigh were determined by CT, and the participants were followed for an average of 12 years.
During the follow-up period, there were 485 incident heart failure events. Higher sex-specific tertiles of intramuscular and intermuscular fat were each associated with heart failure risk.
After multivariable adjustment for age, sex, race, education, blood pressure, fasting blood sugar, current smoking, prevalent coronary disease, and creatinine, higher intramuscular fat, but not intermuscular fat, was significantly associated with higher risk for heart failure.
Individuals in the highest tertile of intramuscular fat had a 34% increased risk of developing heart failure, compared with those in the lowest tertile. This finding was independent of other cardiometabolic risk factors, measures of adiposity including body mass index and percent fat, muscle strength, and muscle mass.
The association was slightly attenuated when adjusted for inflammatory markers, suggesting that inflammation may be a contributor.
The association between higher intramuscular fat and heart failure appeared specific to higher risk of incident heart failure with reduced ejection fraction, but not with heart failure with preserved ejection fraction.
The researchers noted that skeletal muscle is a pivotal endocrine organ in addition to the role it plays in the production of mechanical power.
They pointed out that there are differences in the biology of intermuscular and intramuscular fat deposition, and that excess intramuscular fat deposition is a result of dysregulated lipid metabolism and is associated with insulin resistance (a known risk factor for the development of heart failure), inflammation, and muscle wasting conditions.
They concluded that, in patients with heart failure, alterations in skeletal muscle function are most likely affected by multiple contributors, including inflammation, oxidative stress, and neurohormonal factors. “As these factors are also implicated in the pathogenesis of heart failure, intramuscular fat deposition may indicate a biological milieu that increases the risk of heart failure.”
New approaches to reduce heart failure risk?
In an accompanying editorial, Salvatore Carbone, PhD, Virginia Commonwealth University, Richmond, said the findings of the study are “exceptionally novel,” providing novel evidence that noncardiac body composition compartments, particularly intramuscular adipose tissue, can predict the risk for heart failure in a diverse population of older adults.
He called for further research to understand the mechanisms involved and to assess if this risk factor can be effectively modified to reduce the risk of developing heart failure.
Dr. Carbone reported that intramuscular adipose tissue can be influenced by dietary fat intake and can be worsened by accumulation of saturated fatty acids, which also contribute to insulin resistance.
He noted that saturated fatty acid–induced insulin resistance in the skeletal muscle appears to be mediated by proinflammatory pathways within the skeletal muscle itself, which can be reversed by monounsaturated fatty acids, like oleic acid, that can be found in the largest amount in food like olive oil, canola oil, and avocados, among others.
He added that sodium-glucose transporter 2 inhibitors, drugs used in the treatment of diabetes that have also been shown to prevent heart failure in individuals at risk, can also improve the composition of intramuscular adipose tissue by reducing its content of saturated fatty acids and increase the content of monosaturated fatty acids.
The study results suggest that the quality of intramuscular adipose tissue might also play an important role and could be targeted by therapeutic strategies, he commented.
Dr. Carbone concluded that “studies testing novel modalities of exercise training, intentional weight loss, diet quality improvements with and without weight loss (i.e., increase of dietary monounsaturated fatty acids, such as oleic acid), as well as pharmacological anti-inflammatory strategies should be encouraged in this population to test whether the reduction in intramuscular adipose tissue or improvements of its quality can ultimately reduce the risk for heart failure in this population.”
This research was supported by the National Institute on Aging and the National Institute of Nursing Research. Dr. Huynh and Dr. Carbone disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JACC: HEART FAILURE