User login
A more intensive first-line regimen of FOLFOXIRI plus bevacizumab has a 4-month overall survival benefit in patients with metastatic colorectal cancer when compared with the less intensive FOLFIRI plus bevacizumab, according to an update from the randomized phase III TRIBE trial.
“FOLFOXIRI plus bevacizumab represents a new, valuable option for the upfront treatment of metastatic colorectal cancer patients,” lead investigator Dr. Chiara Cremolini of the Tuscan Tumor Institute, Pisa, Italy, commented in a press briefing held before the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
TRIBE (Combination Chemotherapy and Bevacizumab as First-Line Therapy in Treating Patients With Metastatic Colorectal Cancer) capped eligibility at an age of 75 years, and patients generally had a good performance status. “It is not recommended to administer this kind of regimen to patients older than 75 or to those older than 70 who are not in perfect clinical condition,” she noted.
At the same time, about 80% had synchronous metastases, and most had multiple sites of disease, with only 20% having liver-limited disease. “So overall, this is a patient population in good general condition but not with good prognostic factors,” she summarized.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “This study clearly demonstrates FOLFOXIRI and bevacizumab to be a safe and effective option for patients with advanced colorectal cancer who can tolerate a triple chemotherapy regimen.”
“We have to consider that 90% of the patients on this study were asymptomatic at the time of enrollment, and patients over age 75 were not eligible,” she added. “So this regimen is not for everyone. But for the right patient, though, this is one of the most active regimens, with an impressive almost 25% survival rate at 5 years.”
The trial’s updated results will likely increase use of this regimen in the United States, according to Dr. Krishnamurthi. “When the data first came out for FOLFOXIRI versus FOLFIRI, I don’t think that uptake was high in the United States because at that time, we were already combining chemotherapy with bevacizumab standardly. But now that we have the TRIBE data for FOLFOXIRI with bevacizumab versus FOLFIRI with bevacizumab, demonstrating safety and increased efficacy, I think we will be seeing more use of FOLFOXIRI with bevacizumab,” she elaborated.
In the trial, supported in part by a research grant from F. Hoffmann-La Roche, investigators with the Italian North-West Oncology Group (GONO) randomized 508 patients with newly diagnosed, unresectable metastatic colorectal cancer to receive up to 12 cycles of either the FOLFIRI regimen (irinotecan plus 5-fluorouracil plus folinic acid) plus bevacizumab (Avastin) or the oxaliplatin-containing FOLFOXIRI regimen (irinotecan plus oxaliplatin plus 5-fluorouracil and leucovorin) plus bevacizumab. Each was followed by maintenance therapy with 5-fluorouracil and leucovorin plus bevacizumab.
Initial results, at a median follow-up of 32.2 months, showed that the trial met its primary endpoint, with a significantly better progression-free survival with FOLFOXIRI-bevacizumab (N. Engl. J. Med. 2014;371:1609-18). However, there was only a trend toward better overall survival, along with increased rates of grade 3 or 4 diarrhea, mucositis, neuropathy, and neutropenia.
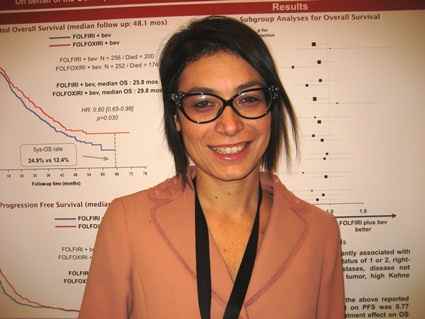
The updated results – now with a median follow-up of 48.1 months – showed persistence of the progression-free survival advantage of FOLFOXIRI-bevacizumab over FOLFIRI-bevacizumab (median 12.3 vs. 9.7 months; hazard ratio, 0.77; P = .006), Dr. Cremolini reported.
However, there was now also a significant overall survival benefit with FOLFOXIRI-bevacizumab (median, 29.8 vs. 25.8 months; HR, 0.80; P = .03). Moreover, the benefit was consistent across patient subgroups. The actuarial 5-year overall survival rate was doubled with the more intense regimen (24.9% vs. 12.4%).
The updated rate of grade 3 or 4 neuropathy was 5.2% with the oxaliplatin-containing FOLFOXIRI-bevacizumab, whereas no patients in the other group developed this toxicity, according to Dr. Cremolini. “This is similar to the doublets with oxaliplatin,” she noted.
Given the trial’s success, GONO is launching TRIBE-2, a phase III trial that will compare use of different regimens when patients have progression after receiving first-line FOLFOXIRI-bevacizumab. In addition, a pair of phase II trials – MACBETH and MOMA – are exploring modifications of the regimen with the goals of shortening the duration of the first-line therapy and improving the efficacy of the maintenance therapy.
A more intensive first-line regimen of FOLFOXIRI plus bevacizumab has a 4-month overall survival benefit in patients with metastatic colorectal cancer when compared with the less intensive FOLFIRI plus bevacizumab, according to an update from the randomized phase III TRIBE trial.
“FOLFOXIRI plus bevacizumab represents a new, valuable option for the upfront treatment of metastatic colorectal cancer patients,” lead investigator Dr. Chiara Cremolini of the Tuscan Tumor Institute, Pisa, Italy, commented in a press briefing held before the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
TRIBE (Combination Chemotherapy and Bevacizumab as First-Line Therapy in Treating Patients With Metastatic Colorectal Cancer) capped eligibility at an age of 75 years, and patients generally had a good performance status. “It is not recommended to administer this kind of regimen to patients older than 75 or to those older than 70 who are not in perfect clinical condition,” she noted.
At the same time, about 80% had synchronous metastases, and most had multiple sites of disease, with only 20% having liver-limited disease. “So overall, this is a patient population in good general condition but not with good prognostic factors,” she summarized.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “This study clearly demonstrates FOLFOXIRI and bevacizumab to be a safe and effective option for patients with advanced colorectal cancer who can tolerate a triple chemotherapy regimen.”
“We have to consider that 90% of the patients on this study were asymptomatic at the time of enrollment, and patients over age 75 were not eligible,” she added. “So this regimen is not for everyone. But for the right patient, though, this is one of the most active regimens, with an impressive almost 25% survival rate at 5 years.”
The trial’s updated results will likely increase use of this regimen in the United States, according to Dr. Krishnamurthi. “When the data first came out for FOLFOXIRI versus FOLFIRI, I don’t think that uptake was high in the United States because at that time, we were already combining chemotherapy with bevacizumab standardly. But now that we have the TRIBE data for FOLFOXIRI with bevacizumab versus FOLFIRI with bevacizumab, demonstrating safety and increased efficacy, I think we will be seeing more use of FOLFOXIRI with bevacizumab,” she elaborated.
In the trial, supported in part by a research grant from F. Hoffmann-La Roche, investigators with the Italian North-West Oncology Group (GONO) randomized 508 patients with newly diagnosed, unresectable metastatic colorectal cancer to receive up to 12 cycles of either the FOLFIRI regimen (irinotecan plus 5-fluorouracil plus folinic acid) plus bevacizumab (Avastin) or the oxaliplatin-containing FOLFOXIRI regimen (irinotecan plus oxaliplatin plus 5-fluorouracil and leucovorin) plus bevacizumab. Each was followed by maintenance therapy with 5-fluorouracil and leucovorin plus bevacizumab.
Initial results, at a median follow-up of 32.2 months, showed that the trial met its primary endpoint, with a significantly better progression-free survival with FOLFOXIRI-bevacizumab (N. Engl. J. Med. 2014;371:1609-18). However, there was only a trend toward better overall survival, along with increased rates of grade 3 or 4 diarrhea, mucositis, neuropathy, and neutropenia.
The updated results – now with a median follow-up of 48.1 months – showed persistence of the progression-free survival advantage of FOLFOXIRI-bevacizumab over FOLFIRI-bevacizumab (median 12.3 vs. 9.7 months; hazard ratio, 0.77; P = .006), Dr. Cremolini reported.
However, there was now also a significant overall survival benefit with FOLFOXIRI-bevacizumab (median, 29.8 vs. 25.8 months; HR, 0.80; P = .03). Moreover, the benefit was consistent across patient subgroups. The actuarial 5-year overall survival rate was doubled with the more intense regimen (24.9% vs. 12.4%).
The updated rate of grade 3 or 4 neuropathy was 5.2% with the oxaliplatin-containing FOLFOXIRI-bevacizumab, whereas no patients in the other group developed this toxicity, according to Dr. Cremolini. “This is similar to the doublets with oxaliplatin,” she noted.
Given the trial’s success, GONO is launching TRIBE-2, a phase III trial that will compare use of different regimens when patients have progression after receiving first-line FOLFOXIRI-bevacizumab. In addition, a pair of phase II trials – MACBETH and MOMA – are exploring modifications of the regimen with the goals of shortening the duration of the first-line therapy and improving the efficacy of the maintenance therapy.
A more intensive first-line regimen of FOLFOXIRI plus bevacizumab has a 4-month overall survival benefit in patients with metastatic colorectal cancer when compared with the less intensive FOLFIRI plus bevacizumab, according to an update from the randomized phase III TRIBE trial.
“FOLFOXIRI plus bevacizumab represents a new, valuable option for the upfront treatment of metastatic colorectal cancer patients,” lead investigator Dr. Chiara Cremolini of the Tuscan Tumor Institute, Pisa, Italy, commented in a press briefing held before the annual Gastrointestinal Cancers Symposium sponsored by the American Society of Clinical Oncology.
TRIBE (Combination Chemotherapy and Bevacizumab as First-Line Therapy in Treating Patients With Metastatic Colorectal Cancer) capped eligibility at an age of 75 years, and patients generally had a good performance status. “It is not recommended to administer this kind of regimen to patients older than 75 or to those older than 70 who are not in perfect clinical condition,” she noted.
At the same time, about 80% had synchronous metastases, and most had multiple sites of disease, with only 20% having liver-limited disease. “So overall, this is a patient population in good general condition but not with good prognostic factors,” she summarized.
Press briefing moderator Dr. Smitha S. Krishnamurthi of Case Western Reserve University, Cleveland, commented, “This study clearly demonstrates FOLFOXIRI and bevacizumab to be a safe and effective option for patients with advanced colorectal cancer who can tolerate a triple chemotherapy regimen.”
“We have to consider that 90% of the patients on this study were asymptomatic at the time of enrollment, and patients over age 75 were not eligible,” she added. “So this regimen is not for everyone. But for the right patient, though, this is one of the most active regimens, with an impressive almost 25% survival rate at 5 years.”
The trial’s updated results will likely increase use of this regimen in the United States, according to Dr. Krishnamurthi. “When the data first came out for FOLFOXIRI versus FOLFIRI, I don’t think that uptake was high in the United States because at that time, we were already combining chemotherapy with bevacizumab standardly. But now that we have the TRIBE data for FOLFOXIRI with bevacizumab versus FOLFIRI with bevacizumab, demonstrating safety and increased efficacy, I think we will be seeing more use of FOLFOXIRI with bevacizumab,” she elaborated.
In the trial, supported in part by a research grant from F. Hoffmann-La Roche, investigators with the Italian North-West Oncology Group (GONO) randomized 508 patients with newly diagnosed, unresectable metastatic colorectal cancer to receive up to 12 cycles of either the FOLFIRI regimen (irinotecan plus 5-fluorouracil plus folinic acid) plus bevacizumab (Avastin) or the oxaliplatin-containing FOLFOXIRI regimen (irinotecan plus oxaliplatin plus 5-fluorouracil and leucovorin) plus bevacizumab. Each was followed by maintenance therapy with 5-fluorouracil and leucovorin plus bevacizumab.
Initial results, at a median follow-up of 32.2 months, showed that the trial met its primary endpoint, with a significantly better progression-free survival with FOLFOXIRI-bevacizumab (N. Engl. J. Med. 2014;371:1609-18). However, there was only a trend toward better overall survival, along with increased rates of grade 3 or 4 diarrhea, mucositis, neuropathy, and neutropenia.
The updated results – now with a median follow-up of 48.1 months – showed persistence of the progression-free survival advantage of FOLFOXIRI-bevacizumab over FOLFIRI-bevacizumab (median 12.3 vs. 9.7 months; hazard ratio, 0.77; P = .006), Dr. Cremolini reported.
However, there was now also a significant overall survival benefit with FOLFOXIRI-bevacizumab (median, 29.8 vs. 25.8 months; HR, 0.80; P = .03). Moreover, the benefit was consistent across patient subgroups. The actuarial 5-year overall survival rate was doubled with the more intense regimen (24.9% vs. 12.4%).
The updated rate of grade 3 or 4 neuropathy was 5.2% with the oxaliplatin-containing FOLFOXIRI-bevacizumab, whereas no patients in the other group developed this toxicity, according to Dr. Cremolini. “This is similar to the doublets with oxaliplatin,” she noted.
Given the trial’s success, GONO is launching TRIBE-2, a phase III trial that will compare use of different regimens when patients have progression after receiving first-line FOLFOXIRI-bevacizumab. In addition, a pair of phase II trials – MACBETH and MOMA – are exploring modifications of the regimen with the goals of shortening the duration of the first-line therapy and improving the efficacy of the maintenance therapy.
AT THE GASTROINTESTINAL CANCERS SYMPOSIUM
Key clinical point: Long-term survival was better with FOLFOXIRI-bevacizumab than with FOLFIRI-bevacizumab.
Major finding: Median overall survival was 29.8 months with FOLFOXIRI-bevacizumab versus 25.8 months with FOLFIRI-bevacizumab.
Data source: A randomized, phase III trial of 508 patients with newly diagnosed metastatic colorectal cancer.
Disclosures: Dr. Cremolini disclosed that she has a consulting or advisory role with Bayer and Roche, and is on the speakers’ bureau with Bayer. The trial was supported in part by a research grant from F. Hoffmann-La Roche.