User login
CHICAGO – Researchers have developed and validated a simple two-step rule to quantify pleural effusion size on computed tomography – something currently not standardized.
Use of the rule significantly improved interobserver agreement, from a kappa coefficient of 0.56 to 0.79 (P less than .0001), among nine physicians ranging in skill from cardiothoracic radiologists and pulmonologists to radiology residents.
"It’s practical for any physician with access to the images and the referent tool, and conveys relevant information in terms of comparing effusion size and possibly guiding therapy," Dr. Matthew Moy said at the annual meeting of the Radiological Society of North America.
Computed tomography (CT) is highly sensitive for detecting small effusions, and differentiating pleural and parenchymal disease. The problem lies in the subjective grading of pleural effusion size and the wide variation in terminology between radiologists. These issues lead to confusion among physicians when reading CT reports or comparing effusions based on different reports, he said.
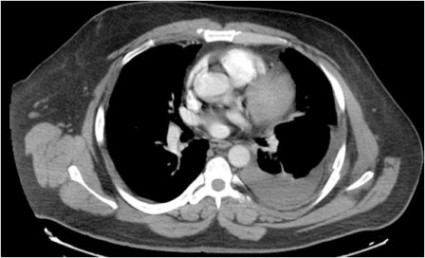
To illustrate his point, Dr. Moy showed three CT images of pleural effusions reported as being "small-moderate" to "moderate" to "large," although all three were similar in size.
In an effort to improve this communication, investigators at the Albert Einstein College of Medicine, New York, selected 34 adult CT scans, representing a wide range of pleural effusion sizes, and measured the volume of each effusion and ipsilateral hemithorax using a morphometric segmentation tool. The effusion and ipsilateral hemithorax were then manually traced on each axial slice, and the effusion volume calculated as a percent of the volume of the hemithorax to account for differences in body habitus, explained Dr. Moy.
The mean effusion volume was 37.42% of the hemithorax (range, 5.59%-89.05%). The patients’ mean age was 64 years, and 74% had undergone noncontrast CT.
Two cardiothoracic fellowship–trained radiologists then reviewed the CTs to identify qualitative and quantitative features that correlated with effusion volume. Several features emerged, but only anteroposterior (AP) quartile, maximum AP depth, and degree of atelectasis remained significant in multivariate analysis. The last was dropped, however, because it was not found to be useful for differentiating large effusions, said Dr. Moy, now with Massachusetts General Hospital in Boston.
AP quartile is calculated using the axial image where the effusion appears largest cephalad to the dome of the hemidiaphragm. The hemithorax is divided into four quartiles, and the AP quartile is then measured as the anterior-most quartile in which the effusion is seen, he explained. Maximum AP depth is measured in centimeters at the midclavicular line.
A classification rule was then developed in which first AP quartile (0%-25%) effusions are small, second quartile (25%-50%) effusions are moderate, and third or fourth AP quartile (50%-75% or 75%-100%) effusions are large. In borderline cases where it’s not easy to assess the quartile, AP depth can be measured using cutoffs of less than 3 cm (small), 3-10 cm (moderate), and more than 10 cm (large), Dr. Moy suggested.
To validate the rule, the 34 CT scans were then assessed by the nine physicians, who were not involved in the initial CT analysis. Interobserver agreement improved from a kappa of 0.59 to a kappa of 0.73 for radiology residents, 0.54 to 0.76 for pulmonologists, and 0.74 to 0.85 for cardiothoracic radiologists.
"This rule can elevate the level of agreement and consistency of both the novice radiologist and clinician to the level of cardiothoracic radiologists," Dr. Moy observed.
Session comoderator Dr. Reginald Munden, a professor of diagnostic radiology at the University of Texas M.D. Anderson Cancer Center in Houston, said in an interview, "I like anything we can do to standardize our reports, because we’re all over the place. This is particularly important, because a lot of smalls are insignificant and we don’t need to do anything with them.
"In our setting, with patients on chemotherapy, we see pleural effusions all the time," he added. "So it’s important when an effusion becomes large enough that it needs to be drained or it might be symptomatic for some other issue."
Dr. Munden went on to say that the grading scale needs to be validated in a larger population and should include a fourth subcategory, "present, but normal," to distinguish small effusions from those that are normal, but may be only 15 cc.
All effusions characterized as small in the analysis were less than 328 mL in absolute volume, Dr. Moy said in an interview. This is significant because malignant pleural effusions less than 1 cm in thickness on a lateral decubitus radiograph are a relative contraindication to thoracentesis, per American Thoracic Society guidelines (Am. J. Respir. Crit. Care Med. 2000;162:1987-2001). Pleural effusions greater than 1 cm on a lateral decubitus view have been shown to measure more than 300 mL in volume (Radiology 1994;191:681-4), he noted.
The new two-step rule is currently in use at Albert Einstein, and has been published online (Chest 2012 Nov. 8 [doi: 10.1378/chest.12-1292]).
Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
CHICAGO – Researchers have developed and validated a simple two-step rule to quantify pleural effusion size on computed tomography – something currently not standardized.
Use of the rule significantly improved interobserver agreement, from a kappa coefficient of 0.56 to 0.79 (P less than .0001), among nine physicians ranging in skill from cardiothoracic radiologists and pulmonologists to radiology residents.
"It’s practical for any physician with access to the images and the referent tool, and conveys relevant information in terms of comparing effusion size and possibly guiding therapy," Dr. Matthew Moy said at the annual meeting of the Radiological Society of North America.
Computed tomography (CT) is highly sensitive for detecting small effusions, and differentiating pleural and parenchymal disease. The problem lies in the subjective grading of pleural effusion size and the wide variation in terminology between radiologists. These issues lead to confusion among physicians when reading CT reports or comparing effusions based on different reports, he said.
To illustrate his point, Dr. Moy showed three CT images of pleural effusions reported as being "small-moderate" to "moderate" to "large," although all three were similar in size.
In an effort to improve this communication, investigators at the Albert Einstein College of Medicine, New York, selected 34 adult CT scans, representing a wide range of pleural effusion sizes, and measured the volume of each effusion and ipsilateral hemithorax using a morphometric segmentation tool. The effusion and ipsilateral hemithorax were then manually traced on each axial slice, and the effusion volume calculated as a percent of the volume of the hemithorax to account for differences in body habitus, explained Dr. Moy.
The mean effusion volume was 37.42% of the hemithorax (range, 5.59%-89.05%). The patients’ mean age was 64 years, and 74% had undergone noncontrast CT.
Two cardiothoracic fellowship–trained radiologists then reviewed the CTs to identify qualitative and quantitative features that correlated with effusion volume. Several features emerged, but only anteroposterior (AP) quartile, maximum AP depth, and degree of atelectasis remained significant in multivariate analysis. The last was dropped, however, because it was not found to be useful for differentiating large effusions, said Dr. Moy, now with Massachusetts General Hospital in Boston.
AP quartile is calculated using the axial image where the effusion appears largest cephalad to the dome of the hemidiaphragm. The hemithorax is divided into four quartiles, and the AP quartile is then measured as the anterior-most quartile in which the effusion is seen, he explained. Maximum AP depth is measured in centimeters at the midclavicular line.
A classification rule was then developed in which first AP quartile (0%-25%) effusions are small, second quartile (25%-50%) effusions are moderate, and third or fourth AP quartile (50%-75% or 75%-100%) effusions are large. In borderline cases where it’s not easy to assess the quartile, AP depth can be measured using cutoffs of less than 3 cm (small), 3-10 cm (moderate), and more than 10 cm (large), Dr. Moy suggested.
To validate the rule, the 34 CT scans were then assessed by the nine physicians, who were not involved in the initial CT analysis. Interobserver agreement improved from a kappa of 0.59 to a kappa of 0.73 for radiology residents, 0.54 to 0.76 for pulmonologists, and 0.74 to 0.85 for cardiothoracic radiologists.
"This rule can elevate the level of agreement and consistency of both the novice radiologist and clinician to the level of cardiothoracic radiologists," Dr. Moy observed.
Session comoderator Dr. Reginald Munden, a professor of diagnostic radiology at the University of Texas M.D. Anderson Cancer Center in Houston, said in an interview, "I like anything we can do to standardize our reports, because we’re all over the place. This is particularly important, because a lot of smalls are insignificant and we don’t need to do anything with them.
"In our setting, with patients on chemotherapy, we see pleural effusions all the time," he added. "So it’s important when an effusion becomes large enough that it needs to be drained or it might be symptomatic for some other issue."
Dr. Munden went on to say that the grading scale needs to be validated in a larger population and should include a fourth subcategory, "present, but normal," to distinguish small effusions from those that are normal, but may be only 15 cc.
All effusions characterized as small in the analysis were less than 328 mL in absolute volume, Dr. Moy said in an interview. This is significant because malignant pleural effusions less than 1 cm in thickness on a lateral decubitus radiograph are a relative contraindication to thoracentesis, per American Thoracic Society guidelines (Am. J. Respir. Crit. Care Med. 2000;162:1987-2001). Pleural effusions greater than 1 cm on a lateral decubitus view have been shown to measure more than 300 mL in volume (Radiology 1994;191:681-4), he noted.
The new two-step rule is currently in use at Albert Einstein, and has been published online (Chest 2012 Nov. 8 [doi: 10.1378/chest.12-1292]).
Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
CHICAGO – Researchers have developed and validated a simple two-step rule to quantify pleural effusion size on computed tomography – something currently not standardized.
Use of the rule significantly improved interobserver agreement, from a kappa coefficient of 0.56 to 0.79 (P less than .0001), among nine physicians ranging in skill from cardiothoracic radiologists and pulmonologists to radiology residents.
"It’s practical for any physician with access to the images and the referent tool, and conveys relevant information in terms of comparing effusion size and possibly guiding therapy," Dr. Matthew Moy said at the annual meeting of the Radiological Society of North America.
Computed tomography (CT) is highly sensitive for detecting small effusions, and differentiating pleural and parenchymal disease. The problem lies in the subjective grading of pleural effusion size and the wide variation in terminology between radiologists. These issues lead to confusion among physicians when reading CT reports or comparing effusions based on different reports, he said.
To illustrate his point, Dr. Moy showed three CT images of pleural effusions reported as being "small-moderate" to "moderate" to "large," although all three were similar in size.
In an effort to improve this communication, investigators at the Albert Einstein College of Medicine, New York, selected 34 adult CT scans, representing a wide range of pleural effusion sizes, and measured the volume of each effusion and ipsilateral hemithorax using a morphometric segmentation tool. The effusion and ipsilateral hemithorax were then manually traced on each axial slice, and the effusion volume calculated as a percent of the volume of the hemithorax to account for differences in body habitus, explained Dr. Moy.
The mean effusion volume was 37.42% of the hemithorax (range, 5.59%-89.05%). The patients’ mean age was 64 years, and 74% had undergone noncontrast CT.
Two cardiothoracic fellowship–trained radiologists then reviewed the CTs to identify qualitative and quantitative features that correlated with effusion volume. Several features emerged, but only anteroposterior (AP) quartile, maximum AP depth, and degree of atelectasis remained significant in multivariate analysis. The last was dropped, however, because it was not found to be useful for differentiating large effusions, said Dr. Moy, now with Massachusetts General Hospital in Boston.
AP quartile is calculated using the axial image where the effusion appears largest cephalad to the dome of the hemidiaphragm. The hemithorax is divided into four quartiles, and the AP quartile is then measured as the anterior-most quartile in which the effusion is seen, he explained. Maximum AP depth is measured in centimeters at the midclavicular line.
A classification rule was then developed in which first AP quartile (0%-25%) effusions are small, second quartile (25%-50%) effusions are moderate, and third or fourth AP quartile (50%-75% or 75%-100%) effusions are large. In borderline cases where it’s not easy to assess the quartile, AP depth can be measured using cutoffs of less than 3 cm (small), 3-10 cm (moderate), and more than 10 cm (large), Dr. Moy suggested.
To validate the rule, the 34 CT scans were then assessed by the nine physicians, who were not involved in the initial CT analysis. Interobserver agreement improved from a kappa of 0.59 to a kappa of 0.73 for radiology residents, 0.54 to 0.76 for pulmonologists, and 0.74 to 0.85 for cardiothoracic radiologists.
"This rule can elevate the level of agreement and consistency of both the novice radiologist and clinician to the level of cardiothoracic radiologists," Dr. Moy observed.
Session comoderator Dr. Reginald Munden, a professor of diagnostic radiology at the University of Texas M.D. Anderson Cancer Center in Houston, said in an interview, "I like anything we can do to standardize our reports, because we’re all over the place. This is particularly important, because a lot of smalls are insignificant and we don’t need to do anything with them.
"In our setting, with patients on chemotherapy, we see pleural effusions all the time," he added. "So it’s important when an effusion becomes large enough that it needs to be drained or it might be symptomatic for some other issue."
Dr. Munden went on to say that the grading scale needs to be validated in a larger population and should include a fourth subcategory, "present, but normal," to distinguish small effusions from those that are normal, but may be only 15 cc.
All effusions characterized as small in the analysis were less than 328 mL in absolute volume, Dr. Moy said in an interview. This is significant because malignant pleural effusions less than 1 cm in thickness on a lateral decubitus radiograph are a relative contraindication to thoracentesis, per American Thoracic Society guidelines (Am. J. Respir. Crit. Care Med. 2000;162:1987-2001). Pleural effusions greater than 1 cm on a lateral decubitus view have been shown to measure more than 300 mL in volume (Radiology 1994;191:681-4), he noted.
The new two-step rule is currently in use at Albert Einstein, and has been published online (Chest 2012 Nov. 8 [doi: 10.1378/chest.12-1292]).
Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.
AT THE ANNUAL MEETING OF THE RADIOLOGICAL SOCIETY OF NORTH AMERICA
Major Finding: Use of the rule significantly improved interobserver agreement from a kappa coefficient of 0.56 to 0.79 among nine cardiothoracic radiologists, pulmonologists, and radiology residents (P less than .0001).
Data Source: Analysis of 34 adult chest CT scans.
Disclosures: Dr. Moy reported no conflicts of interest. A coauthor reported investments in Ortho Space and Kryon Systems.