User login
In continuing with the series, An Update in Acute Care Surgery, the following section highlights the evolution of the training process for the Acute Care Surgery fellowship.
Grace S. Rozycki, MD, FACS
The Willis D. Gatch Professor of Surgery
Associate Chair, Department of Surgery, Indiana University
Chief of Surgery, IUH-Methodist Hospital, Indianapolis
Acute Care Surgery: The Training Paradigm
BY CLAY COTHREN BURLEW, MD, FACS, AND GREGORY J. JURKOVICH, MD., FACS
The acute care surgery fellowships are designed to follow core training in general surgery (J. Trauma 2007;62:553-6). Currently, this means the acute care surgery fellowship follows the completion of an Accreditation Council for Graduate Medical Education general surgery residency program and is in alignment with the core competencies of the general surgery residency. The 2-year curriculum was defined by the AAST, and incorporates the requirements of an ACGME-approved surgical critical care fellowship.
Although there are mandatory components of this fellowship, a certain amount of latitude and creativity are encouraged so to capitalize on the strength of the individual program as well as to meet the individual needs of the fellow.
The basic principles of the training paradigm include the followi
1. The program is 2 years in length.
2. The acute care surgery fellowship programs must have the ACGME approved surgical critical care residency.
3.The fellowship must include specific surgical technical training in hepatobiliary disorders, thoracic surgery, and vascular surgery.
4. Trainees should participate in acute care surgery call for at least 12 months and 52 nights of acute care surgery call (trauma and emergency general surgery).
5. Flexibility in the rotations should be used to optimize the fellow’s training.
6. The rationale for out-of-system rotations and the structure of the 24-month training should be used to optimize the fellow’s training.
7. Participation in elective surgery, both to supplement general surgery training and experience and to serve in a supervisory role to residents, is an essential component of this fellowship training.
8. An academic environment is necessary and the fellows should be trained to teach others and conduct research in acute care surgery.
The rationale for the rotations of Thoracic Surgery, Transplant/Hepatobiliary/ Pancreatic, and Vascular (including vascular interventional) is twofold: 1) Many complex operative cases in these areas are infrequently encountered in modern trauma centers; and, 2) experts in these areas can provide mentorship and operative expertise and teaching for the fellow who obtains a focused, quality operative experience in these areas. Further, these rotations have specific competency related goals so that the fellow has specific requirements to meet. The AAST is currently revising its method of confirming this training expertise by examining specific components of operative technique and exposure as well as length of time on specific rotations (see below).
Program Application and Approval
The required background and expectations for the acute care surgery fellowship include the following: 1) Fellows must have successfully completed the core training requirements of an RRC-approved residency in General Surgery; and 2) the acute care surgery fellowship programs must provide the necessary education to qualify the fellow as an acute care surgical specialist in clinical, education, and research areas. Each program must have support from its parent institution, including administrative personnel, the chairman of the department of surgery, division chief, and participating acute care surgery faculty. The program should have all of the necessary resources to fulfill the training requirements and create an environment of inquiry and scholarship while allowing for progressive responsibility throughout the training period.
The process of becoming an approved acute care surgery fellowship program can be divided into the following steps:
1. The Program Director completes the Program Information Form (PIF) form (downloaded from the AAST website, http://www.aast.org).
2. The PIF is reviewed by three members of the AAST Acute Care Surgery Committee to determine whether it is complete and if it meets the essential requirements. If the initial review is successful, then a site visit of the program is scheduled.
3. The site visit is conducted by two members of AAST Acute Care Surgery Committee. The site visit consists of an evening business dinner meeting with the following personnel: the program director for the acute care surgery fellowship, the program director for the general surgery residency program, select administrators, and division chiefs. Current fellows in the program are also invited to participate. The following day, the site visitors tour the institution, and conduct one-on-one interviews with the personnel who were present at the site visit dinner. A chart review is conducted to assess the operative case load and the involvement of the faculty, residents, and fellows in the care of the patients. At the conclusion of the day, a summation interview is conducted with the acute care surgery fellowship program director.
4. Following the site visit, a written assessment of the program is performed, which covers an overview/program description, strengths/weaknesses, major deficiencies, and a summary with recommendations.
5. If no major deficiencies are noted, the senior site visitor presents the highlights of the program to the members of the AAST Acute Care Surgery Committee and, if approved subsequently to the AAST Board of Managers for final approval.
Acute Care Surgery Committee and Curriculum
BY CLAY COTHREN BURLEW, MD
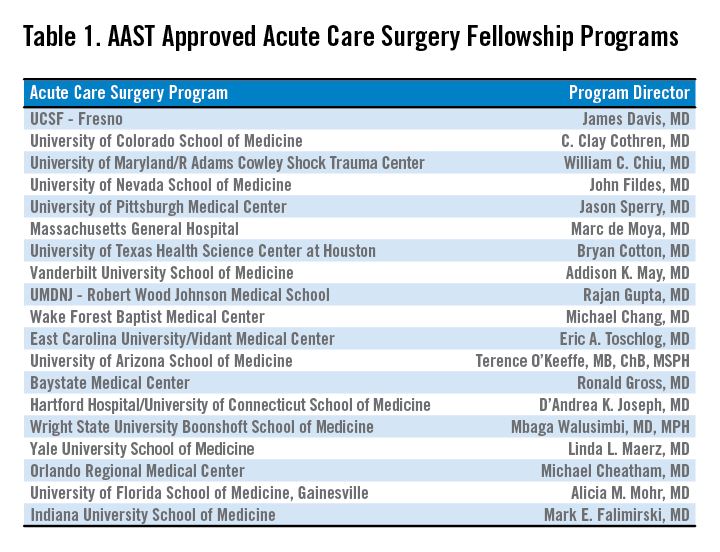
With the development of a fellowship-based training paradigm in acute care surgery, the AAST also developed an oversight committee. This committee, aptly named the Acute Care Surgery Committee, is comprised of 25 appointed AAST members. The committee represents a varied group of stakeholders including members of the senior leadership of the AAST and fellowship program directors. The Acute Care Surgery Committee’s role has evolved over the past decade. Initially the members of the Committee formulated and implemented the training paradigm for the fellowship, including the requirements enumerated above. Following the certification of several successful training fellowships in 2008-2009, the Committee encouraged additional institutions to initiate training fellows by assisting with educational development. This led to the expansion of acute care surgery training in 19 accredited programs. (see Table).
Throughout this decade of growth, the Acute Care Surgery committee has also been dedicated to the oversight and continual evaluation of the training process. Two specific measures were implemented in this regard.
First, each fellowship graduate must take not only the American Board of Surgery examination for certification in Surgical Critical Care, but also the examination in acute care surgery written by the AAST. The Acute Care Surgery Committee formed a subcommittee that has spent innumerable hours researching and writing test questions for this examination. That subcommittee is now reviewing each of the questions from the originally produced examination and reformatting the test. New questions are being created by the subcommittee, and the examination will become electronically administered.
Second, acute care surgery fellows must track their operative experience through the AAST-supported on-line case log system. Although fellows have been provided with a list of essential and desired operative cases, the case log system permits specific delineation of each fellow’s experience. Using the case log system, the Acute Care Surgery Committee was able to analyze the fellows’ experience, identify gaps in operative training, and refine the curriculum as indicated. The Committee has performed two such analyses and, based on the findings of those reports, modification of the curriculum is now underway. (J. Trauma Acute Care Surg. 2014;76:329-39.; J. Trauma Acute Care Surg. 2015;78:259-64).
One of the current initiatives of the Acute Care Surgery Committee is the revision of the acute care surgery fellowship curriculum. In revising the curriculum, several key points were considered. One observation, derived from the case log review, was that the original case list captured only a portion of the operative experience of acute care surgery fellows. Additionally, it was apparent that operative trauma cases alone do not provide adequate exposure to some of the more complex cases thought to be essential components of this specialty. Therefore, the Committee determined that incorporating specific surgical approaches or anatomic exposures performed during elective and urgent cases are valuable experiences for the fellow. The totality of training in advanced operative techniques over the breadth of anatomic locations remains the unique feature of our specialty.(J. Trauma Acute Care Surg. 2015; 78:192-196).
Based upon these observations, the new curriculum is now organized by anatomic subsections (Head/Neck, Thoracic, Abdominal, Vascular), as well as organ-based management. Each section of the curriculum now lists specific case numbers required for surgical approaches or exposures, and also addresses organ-based management. For example, within the thoracic section of the curriculum, required case numbers now exist for thoracotomy, thoracoscopy, sternotomy, and pericardotomy (exposures) as well as lung, diaphragm, heart, esophagus, and intrathoracic great vessels. In each anatomic subsection, simulation may be used to satisfy a requirement.
Opportunities to accomplish these requirements may be through the American College of Surgeons Advanced Trauma Operative Management or the Advanced Surgical Skills for Exposure in Trauma courses. Organ harvest exposures may also be used for less common surgical exposures. Fellows can choose both the exposure and the organ-based procedure code for each operative case performed when logging their cases.(J. Trauma Acute Care Surg. 2014;76:329-39). Identification of a minimum number of operative cases needed in specific body regions reflects the defined case volumes in general surgery as required by the Accreditation Council for Graduate Medical Education.
The Acute Care Surgery Committee considered that the implementation of the required case volumes would serve two purposes: First, the list would provide guidance to the fellows as to the types of cases they should actively identify and in which they should participate; and, second, it would provide guidance to program directors and subspecialty colleagues as to the cases deemed important for fellowship training. Ongoing review of the fellows’ case logs with implementation of the new curriculum will remain a focus of the Acute Care Surgery Committee as it transitions to a new case log system soon.
An earlier version of the graphic misstated the name of Clay Cothren Burlew.
In continuing with the series, An Update in Acute Care Surgery, the following section highlights the evolution of the training process for the Acute Care Surgery fellowship.
Grace S. Rozycki, MD, FACS
The Willis D. Gatch Professor of Surgery
Associate Chair, Department of Surgery, Indiana University
Chief of Surgery, IUH-Methodist Hospital, Indianapolis
Acute Care Surgery: The Training Paradigm
BY CLAY COTHREN BURLEW, MD, FACS, AND GREGORY J. JURKOVICH, MD., FACS
The acute care surgery fellowships are designed to follow core training in general surgery (J. Trauma 2007;62:553-6). Currently, this means the acute care surgery fellowship follows the completion of an Accreditation Council for Graduate Medical Education general surgery residency program and is in alignment with the core competencies of the general surgery residency. The 2-year curriculum was defined by the AAST, and incorporates the requirements of an ACGME-approved surgical critical care fellowship.
Although there are mandatory components of this fellowship, a certain amount of latitude and creativity are encouraged so to capitalize on the strength of the individual program as well as to meet the individual needs of the fellow.
The basic principles of the training paradigm include the followi
1. The program is 2 years in length.
2. The acute care surgery fellowship programs must have the ACGME approved surgical critical care residency.
3.The fellowship must include specific surgical technical training in hepatobiliary disorders, thoracic surgery, and vascular surgery.
4. Trainees should participate in acute care surgery call for at least 12 months and 52 nights of acute care surgery call (trauma and emergency general surgery).
5. Flexibility in the rotations should be used to optimize the fellow’s training.
6. The rationale for out-of-system rotations and the structure of the 24-month training should be used to optimize the fellow’s training.
7. Participation in elective surgery, both to supplement general surgery training and experience and to serve in a supervisory role to residents, is an essential component of this fellowship training.
8. An academic environment is necessary and the fellows should be trained to teach others and conduct research in acute care surgery.
The rationale for the rotations of Thoracic Surgery, Transplant/Hepatobiliary/ Pancreatic, and Vascular (including vascular interventional) is twofold: 1) Many complex operative cases in these areas are infrequently encountered in modern trauma centers; and, 2) experts in these areas can provide mentorship and operative expertise and teaching for the fellow who obtains a focused, quality operative experience in these areas. Further, these rotations have specific competency related goals so that the fellow has specific requirements to meet. The AAST is currently revising its method of confirming this training expertise by examining specific components of operative technique and exposure as well as length of time on specific rotations (see below).
Program Application and Approval
The required background and expectations for the acute care surgery fellowship include the following: 1) Fellows must have successfully completed the core training requirements of an RRC-approved residency in General Surgery; and 2) the acute care surgery fellowship programs must provide the necessary education to qualify the fellow as an acute care surgical specialist in clinical, education, and research areas. Each program must have support from its parent institution, including administrative personnel, the chairman of the department of surgery, division chief, and participating acute care surgery faculty. The program should have all of the necessary resources to fulfill the training requirements and create an environment of inquiry and scholarship while allowing for progressive responsibility throughout the training period.
The process of becoming an approved acute care surgery fellowship program can be divided into the following steps:
1. The Program Director completes the Program Information Form (PIF) form (downloaded from the AAST website, http://www.aast.org).
2. The PIF is reviewed by three members of the AAST Acute Care Surgery Committee to determine whether it is complete and if it meets the essential requirements. If the initial review is successful, then a site visit of the program is scheduled.
3. The site visit is conducted by two members of AAST Acute Care Surgery Committee. The site visit consists of an evening business dinner meeting with the following personnel: the program director for the acute care surgery fellowship, the program director for the general surgery residency program, select administrators, and division chiefs. Current fellows in the program are also invited to participate. The following day, the site visitors tour the institution, and conduct one-on-one interviews with the personnel who were present at the site visit dinner. A chart review is conducted to assess the operative case load and the involvement of the faculty, residents, and fellows in the care of the patients. At the conclusion of the day, a summation interview is conducted with the acute care surgery fellowship program director.
4. Following the site visit, a written assessment of the program is performed, which covers an overview/program description, strengths/weaknesses, major deficiencies, and a summary with recommendations.
5. If no major deficiencies are noted, the senior site visitor presents the highlights of the program to the members of the AAST Acute Care Surgery Committee and, if approved subsequently to the AAST Board of Managers for final approval.
Acute Care Surgery Committee and Curriculum
BY CLAY COTHREN BURLEW, MD
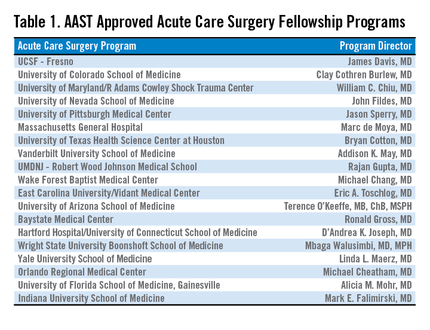
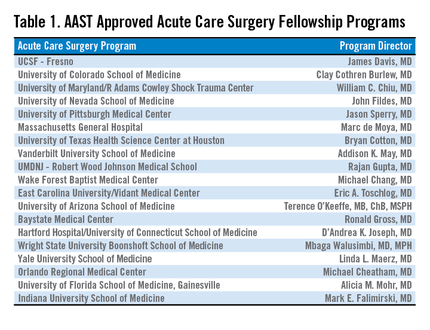
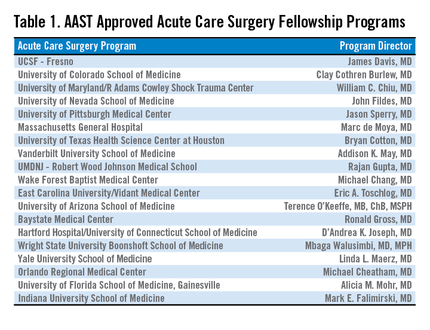
With the development of a fellowship-based training paradigm in acute care surgery, the AAST also developed an oversight committee. This committee, aptly named the Acute Care Surgery Committee, is comprised of 25 appointed AAST members. The committee represents a varied group of stakeholders including members of the senior leadership of the AAST and fellowship program directors. The Acute Care Surgery Committee’s role has evolved over the past decade. Initially the members of the Committee formulated and implemented the training paradigm for the fellowship, including the requirements enumerated above. Following the certification of several successful training fellowships in 2008-2009, the Committee encouraged additional institutions to initiate training fellows by assisting with educational development. This led to the expansion of acute care surgery training in 19 accredited programs. (see Table).
Throughout this decade of growth, the Acute Care Surgery committee has also been dedicated to the oversight and continual evaluation of the training process. Two specific measures were implemented in this regard.
First, each fellowship graduate must take not only the American Board of Surgery examination for certification in Surgical Critical Care, but also the examination in acute care surgery written by the AAST. The Acute Care Surgery Committee formed a subcommittee that has spent innumerable hours researching and writing test questions for this examination. That subcommittee is now reviewing each of the questions from the originally produced examination and reformatting the test. New questions are being created by the subcommittee, and the examination will become electronically administered.
Second, acute care surgery fellows must track their operative experience through the AAST-supported on-line case log system. Although fellows have been provided with a list of essential and desired operative cases, the case log system permits specific delineation of each fellow’s experience. Using the case log system, the Acute Care Surgery Committee was able to analyze the fellows’ experience, identify gaps in operative training, and refine the curriculum as indicated. The Committee has performed two such analyses and, based on the findings of those reports, modification of the curriculum is now underway. (J. Trauma Acute Care Surg. 2014;76:329-39.; J. Trauma Acute Care Surg. 2015;78:259-64).
One of the current initiatives of the Acute Care Surgery Committee is the revision of the acute care surgery fellowship curriculum. In revising the curriculum, several key points were considered. One observation, derived from the case log review, was that the original case list captured only a portion of the operative experience of acute care surgery fellows. Additionally, it was apparent that operative trauma cases alone do not provide adequate exposure to some of the more complex cases thought to be essential components of this specialty. Therefore, the Committee determined that incorporating specific surgical approaches or anatomic exposures performed during elective and urgent cases are valuable experiences for the fellow. The totality of training in advanced operative techniques over the breadth of anatomic locations remains the unique feature of our specialty.(J. Trauma Acute Care Surg. 2015; 78:192-196).
Based upon these observations, the new curriculum is now organized by anatomic subsections (Head/Neck, Thoracic, Abdominal, Vascular), as well as organ-based management. Each section of the curriculum now lists specific case numbers required for surgical approaches or exposures, and also addresses organ-based management. For example, within the thoracic section of the curriculum, required case numbers now exist for thoracotomy, thoracoscopy, sternotomy, and pericardotomy (exposures) as well as lung, diaphragm, heart, esophagus, and intrathoracic great vessels. In each anatomic subsection, simulation may be used to satisfy a requirement.
Opportunities to accomplish these requirements may be through the American College of Surgeons Advanced Trauma Operative Management or the Advanced Surgical Skills for Exposure in Trauma courses. Organ harvest exposures may also be used for less common surgical exposures. Fellows can choose both the exposure and the organ-based procedure code for each operative case performed when logging their cases.(J. Trauma Acute Care Surg. 2014;76:329-39). Identification of a minimum number of operative cases needed in specific body regions reflects the defined case volumes in general surgery as required by the Accreditation Council for Graduate Medical Education.
The Acute Care Surgery Committee considered that the implementation of the required case volumes would serve two purposes: First, the list would provide guidance to the fellows as to the types of cases they should actively identify and in which they should participate; and, second, it would provide guidance to program directors and subspecialty colleagues as to the cases deemed important for fellowship training. Ongoing review of the fellows’ case logs with implementation of the new curriculum will remain a focus of the Acute Care Surgery Committee as it transitions to a new case log system soon.
An earlier version of the graphic misstated the name of Clay Cothren Burlew.
In continuing with the series, An Update in Acute Care Surgery, the following section highlights the evolution of the training process for the Acute Care Surgery fellowship.
Grace S. Rozycki, MD, FACS
The Willis D. Gatch Professor of Surgery
Associate Chair, Department of Surgery, Indiana University
Chief of Surgery, IUH-Methodist Hospital, Indianapolis
Acute Care Surgery: The Training Paradigm
BY CLAY COTHREN BURLEW, MD, FACS, AND GREGORY J. JURKOVICH, MD., FACS
The acute care surgery fellowships are designed to follow core training in general surgery (J. Trauma 2007;62:553-6). Currently, this means the acute care surgery fellowship follows the completion of an Accreditation Council for Graduate Medical Education general surgery residency program and is in alignment with the core competencies of the general surgery residency. The 2-year curriculum was defined by the AAST, and incorporates the requirements of an ACGME-approved surgical critical care fellowship.
Although there are mandatory components of this fellowship, a certain amount of latitude and creativity are encouraged so to capitalize on the strength of the individual program as well as to meet the individual needs of the fellow.
The basic principles of the training paradigm include the followi
1. The program is 2 years in length.
2. The acute care surgery fellowship programs must have the ACGME approved surgical critical care residency.
3.The fellowship must include specific surgical technical training in hepatobiliary disorders, thoracic surgery, and vascular surgery.
4. Trainees should participate in acute care surgery call for at least 12 months and 52 nights of acute care surgery call (trauma and emergency general surgery).
5. Flexibility in the rotations should be used to optimize the fellow’s training.
6. The rationale for out-of-system rotations and the structure of the 24-month training should be used to optimize the fellow’s training.
7. Participation in elective surgery, both to supplement general surgery training and experience and to serve in a supervisory role to residents, is an essential component of this fellowship training.
8. An academic environment is necessary and the fellows should be trained to teach others and conduct research in acute care surgery.
The rationale for the rotations of Thoracic Surgery, Transplant/Hepatobiliary/ Pancreatic, and Vascular (including vascular interventional) is twofold: 1) Many complex operative cases in these areas are infrequently encountered in modern trauma centers; and, 2) experts in these areas can provide mentorship and operative expertise and teaching for the fellow who obtains a focused, quality operative experience in these areas. Further, these rotations have specific competency related goals so that the fellow has specific requirements to meet. The AAST is currently revising its method of confirming this training expertise by examining specific components of operative technique and exposure as well as length of time on specific rotations (see below).
Program Application and Approval
The required background and expectations for the acute care surgery fellowship include the following: 1) Fellows must have successfully completed the core training requirements of an RRC-approved residency in General Surgery; and 2) the acute care surgery fellowship programs must provide the necessary education to qualify the fellow as an acute care surgical specialist in clinical, education, and research areas. Each program must have support from its parent institution, including administrative personnel, the chairman of the department of surgery, division chief, and participating acute care surgery faculty. The program should have all of the necessary resources to fulfill the training requirements and create an environment of inquiry and scholarship while allowing for progressive responsibility throughout the training period.
The process of becoming an approved acute care surgery fellowship program can be divided into the following steps:
1. The Program Director completes the Program Information Form (PIF) form (downloaded from the AAST website, http://www.aast.org).
2. The PIF is reviewed by three members of the AAST Acute Care Surgery Committee to determine whether it is complete and if it meets the essential requirements. If the initial review is successful, then a site visit of the program is scheduled.
3. The site visit is conducted by two members of AAST Acute Care Surgery Committee. The site visit consists of an evening business dinner meeting with the following personnel: the program director for the acute care surgery fellowship, the program director for the general surgery residency program, select administrators, and division chiefs. Current fellows in the program are also invited to participate. The following day, the site visitors tour the institution, and conduct one-on-one interviews with the personnel who were present at the site visit dinner. A chart review is conducted to assess the operative case load and the involvement of the faculty, residents, and fellows in the care of the patients. At the conclusion of the day, a summation interview is conducted with the acute care surgery fellowship program director.
4. Following the site visit, a written assessment of the program is performed, which covers an overview/program description, strengths/weaknesses, major deficiencies, and a summary with recommendations.
5. If no major deficiencies are noted, the senior site visitor presents the highlights of the program to the members of the AAST Acute Care Surgery Committee and, if approved subsequently to the AAST Board of Managers for final approval.
Acute Care Surgery Committee and Curriculum
BY CLAY COTHREN BURLEW, MD
With the development of a fellowship-based training paradigm in acute care surgery, the AAST also developed an oversight committee. This committee, aptly named the Acute Care Surgery Committee, is comprised of 25 appointed AAST members. The committee represents a varied group of stakeholders including members of the senior leadership of the AAST and fellowship program directors. The Acute Care Surgery Committee’s role has evolved over the past decade. Initially the members of the Committee formulated and implemented the training paradigm for the fellowship, including the requirements enumerated above. Following the certification of several successful training fellowships in 2008-2009, the Committee encouraged additional institutions to initiate training fellows by assisting with educational development. This led to the expansion of acute care surgery training in 19 accredited programs. (see Table).
Throughout this decade of growth, the Acute Care Surgery committee has also been dedicated to the oversight and continual evaluation of the training process. Two specific measures were implemented in this regard.
First, each fellowship graduate must take not only the American Board of Surgery examination for certification in Surgical Critical Care, but also the examination in acute care surgery written by the AAST. The Acute Care Surgery Committee formed a subcommittee that has spent innumerable hours researching and writing test questions for this examination. That subcommittee is now reviewing each of the questions from the originally produced examination and reformatting the test. New questions are being created by the subcommittee, and the examination will become electronically administered.
Second, acute care surgery fellows must track their operative experience through the AAST-supported on-line case log system. Although fellows have been provided with a list of essential and desired operative cases, the case log system permits specific delineation of each fellow’s experience. Using the case log system, the Acute Care Surgery Committee was able to analyze the fellows’ experience, identify gaps in operative training, and refine the curriculum as indicated. The Committee has performed two such analyses and, based on the findings of those reports, modification of the curriculum is now underway. (J. Trauma Acute Care Surg. 2014;76:329-39.; J. Trauma Acute Care Surg. 2015;78:259-64).
One of the current initiatives of the Acute Care Surgery Committee is the revision of the acute care surgery fellowship curriculum. In revising the curriculum, several key points were considered. One observation, derived from the case log review, was that the original case list captured only a portion of the operative experience of acute care surgery fellows. Additionally, it was apparent that operative trauma cases alone do not provide adequate exposure to some of the more complex cases thought to be essential components of this specialty. Therefore, the Committee determined that incorporating specific surgical approaches or anatomic exposures performed during elective and urgent cases are valuable experiences for the fellow. The totality of training in advanced operative techniques over the breadth of anatomic locations remains the unique feature of our specialty.(J. Trauma Acute Care Surg. 2015; 78:192-196).
Based upon these observations, the new curriculum is now organized by anatomic subsections (Head/Neck, Thoracic, Abdominal, Vascular), as well as organ-based management. Each section of the curriculum now lists specific case numbers required for surgical approaches or exposures, and also addresses organ-based management. For example, within the thoracic section of the curriculum, required case numbers now exist for thoracotomy, thoracoscopy, sternotomy, and pericardotomy (exposures) as well as lung, diaphragm, heart, esophagus, and intrathoracic great vessels. In each anatomic subsection, simulation may be used to satisfy a requirement.
Opportunities to accomplish these requirements may be through the American College of Surgeons Advanced Trauma Operative Management or the Advanced Surgical Skills for Exposure in Trauma courses. Organ harvest exposures may also be used for less common surgical exposures. Fellows can choose both the exposure and the organ-based procedure code for each operative case performed when logging their cases.(J. Trauma Acute Care Surg. 2014;76:329-39). Identification of a minimum number of operative cases needed in specific body regions reflects the defined case volumes in general surgery as required by the Accreditation Council for Graduate Medical Education.
The Acute Care Surgery Committee considered that the implementation of the required case volumes would serve two purposes: First, the list would provide guidance to the fellows as to the types of cases they should actively identify and in which they should participate; and, second, it would provide guidance to program directors and subspecialty colleagues as to the cases deemed important for fellowship training. Ongoing review of the fellows’ case logs with implementation of the new curriculum will remain a focus of the Acute Care Surgery Committee as it transitions to a new case log system soon.
An earlier version of the graphic misstated the name of Clay Cothren Burlew.