User login
The13C-urea breath test provides accurate, noninvasive diagnosis of active Helicobacter pylori infection and can document posttherapy cure. This study evaluated point-of-care testing with onsite sample analysis with the use of a desktop infrared spectrophotometer. Ambulatory patients (N = 320) underwent 13C-urea breath testing, and breath samples were analyzed immediately by clinic staff with no prior breath testing experience. Duplicate samples were sent to a reference laboratory, and the results of both methods were compared. Point-of-care testing was simple, with an overall agreement of 99.1%. Accurate near-patient 13C-urea breath testing is now practical in the primary care setting even when done by inexperienced personnel.
Helicobacter pylori infection is etiologically associated with chronic gastritis, peptic ulcer disease, and gastric cancer.1-5Helicobacter pylori infection is also a consideration in the evaluation of uninvestigated or undifferentiated dyspepsia.4-7 The steps in the management of H pylori infection include diagnosis, choice of appropriate therapy, and confirmation of cure.4,5,8 Diagnosis and confirmation of cure require diagnostic testing, and the recent consensus has been in the direction of noninvasive testing.4,5
The urea breath test (UBT) is generally considered the clinical, gold standard, noninvasive test for detection of active H pylori infection.9 The intragastric hydrolysis of orally administered urea by H pylori urease produces a change in the isotopic ratio (13CO2/12CO2) in the breath.10 The 13C-UBT has been approved by the US Food and Drug Administration for pre- and posttherapy testing.11,12
Recently the 13C-UBT has been shortened and simplified by the use of a citric acid test meal and elimination of the requirement of a 4-hour fast.13 Use of infrared mass spectrophotometry for measuring 13CO2 enrichment in breath samples makes it theoretically possible to do office-based breath testing with onsite analysis.14-16 Infrared spectrophotometry has been shown in comparative studies to be an accurate method for assessing 13CO2 enrichment in breath.17-19 No comparative studies of the 2 analytical methods have been done in the United States.
This study examined the utility of UBT testing by comparing infrared spectrophotometry with traditional gas isotope ratio mass spectrometry in the primary care environment. Our hypothesis was that the results obtained from the primary care clinics would be as accurate as those obtained from the commercial laboratory or the more experienced hospital-based clinical laboratory.
Methods
This was a multicenter, prospective study designed to compare a new infrared spectrophotometer (UBiTIR300, Otsuka Pharmaceuticals, Tokyo, Japan) for measuring 13CO2 enrichment in breath with gas isotope ratio mass spectrometry (ABCA, Europa Scientific, Cheshire, UK). Subjects were recruited at the offices or clinics of 4 physicians’ including an indigent care primary care clinic, a hospital-based gastroenterology clinic, a private practice internal medicine office, an academic family medicine clinic, and a tertiary care clinical laboratory site. The study was done between July and September 2001. Consecutive patients were enrolled in the study if they expressed interest in participating and met the inclusion and exclusion criteria. Each site was provided with an infrared spectrophotometer, a breath gas transfer device, and commercially available UBT breath test collection kits (Meretek Diagnostics, Nashville, TN). Each kit contained a 13C-urea solution (125 mg in 75 mL of water), test meal pudding, and a specimen return box containing 4 bar-coded, evacuated 10-mL sample tubes. Before enrollment, all study personnel received approximately 1 hour of training in the performance of the test and use of the equipment.
Study procedures
Subjects included in the study were medically stable, ambulatory patients between 18 and 75 years old who were asymptomatic or experiencing dyspepsia. Potential subjects were excluded from study participation if they took bismuth preparations, antibiotics (ie, amoxicillin, tetracycline, metronidazole, clarithromycin, or azithromycin) or any anti-ulcer medication in dosages indicated for ulcer disease (ie, proton pump inhibitors, type 2 histamine blockers, or misoprostol) within 2 weeks before the study breath test. Exclusion criteria also included participation in a drug study within 4 weeks, treatment for eradication of H pylori within 4 weeks of the study breath test, or a history of gastric surgery or vagotomy for ulcer disease except simple closure of a gastric perforation.
The protocol was approved by the local Institutional Review Board for Human Studies, and all subjects provided written informed consent.
Testing began with a minimum 4-hour fast from solid food. Breath samples were obtained in disposable, balloonlike, breath collection bags designed for use with the infrared spectrophotometer. One sample was obtained immediately before ingestion of the 13C-urea test solution, and the second was collected 30 minutes after substrate ingestion. Paired sample aliquots were taken for separate analyses. Results from local infrared instruments were blinded to the central laboratory.
Statistical analyses
Each primary care site was asked to enroll subjects until 80 positive cases were identified from among all sites. The clinical laboratory site tested a minimum of 30 positive and 30 negative cases. The primary endpoint was the percentage of agreement (overall and within positive and negative cases separately) of results from both methods. Delta-over-baseline (DOB) enrichment values below 2.4 per mil were deemed negative and values greater than or equal to 2.4 per mil were deemed positive. The predicate reference method was gas isotope ratio mass spectrometry. Equivalence was defined by the percentage of agreement for positive and negative cases based on gas isotope ratio mass spectrometry results of at least 95%, and the lower limit of the 95% confidence interval was based on a percentage of agreement of at least 90% for positive cases.
Results
The primary care centers enrolled 258 subjects and the clinical laboratory enrolled 64 subjects, for a total enrollment of 322. The subjects’ mean age was 41.5 years (range, 18–70 years), with 88 black non-Hispanics, 106 Hispanics, 92 whites, 32 Asian/Pacific Islanders, and 4 other ethnic groups. There were 215 women and 107 men. Approximately 18% had active or previous gastrointestinal ailments, including previously diagnosed H pylori infection (11%) and peptic ulcer disease (3%).
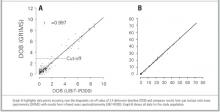
There was excellent agreement between methods (Table), with an overall agreement of 99% (95% confidence interval, 97.3–99.7). Two subjects were excluded from the analysis of the primary and secondary endpoints because 1 or both assay values were missing. The data showed close correlation between methods among all sites (Figure). Evaluation by the personnel who performed the tests and analyses indicated that the office procedure was easy and nonintrusive.
There were 3 disagreements between the results obtained with the devices, 1 from the gastroenterology site and 2 from the clinical laboratory site. All results were near the cutoff value.
TABLE
Comparison of results between IRMS and GIRMS*
| GIRMS, % | |||
|---|---|---|---|
| IRMS, % | Negative | Positive | Total |
| Negative | 1 | 115 | 116 |
| Positive | 202 | 2 | 204 |
| Total | 203 | 117 | 320 |
| *Overall agreement, 99.1% (95% confidence interval, 97.3–99.7); positive agreement, 98.2% (95% confidence interval, 94.2–99.7); negative agreement, 99.5% (95% confidence interval, 97.3–99.9). | |||
| Kappa statistic = 0.98. | |||
| GIRMS, gas isotope ratio mass spectrometry; IRMS, infrared mass spectrophotometry. | |||
FIGURE
Comparison of results between 2 methods of analysis of 13CO2 breath sample enrichments
Discussion
13C-urea breath testing is an accurate diagnostic method for the detection of active H pylori infection12,19-21 and point-of-care assessment of curative therapy. This study confirmed the hypothesis that the infrared instrument is an easy to operate alternative to the original sendout analyses. Rapid turnaround allows for decisions regarding therapy to be made at the time of care. The currently approved UBT in the United States does not require fasting from solid food for longer than 1 hour.
Noninvasive alternatives to UBT include serology and stool antigen testing. Serology assays cannot discriminate between active and recent past infections. Stool antigen testing requires patient compliance with specimen collection and is a sendout test. In general, although studies using pretreatment stool antigen tests have shown sensitivity and specificity comparable to those of histology or UBT, it has become evident that there can be considerable lot-to-lot variation in stool antigen tests.22 The most likely explanation is that the polyclonal serum used for the capture antibody is obtained from rabbits and thus difficult to standardize.23 Stool antigen testing has also proven to be less reliable when used soon after the end of therapy, and it is now generally recommended that one must wait 6 or 8 weeks after therapy when using the stool antigen test to confirm eradication. For example, a recent study had a false negative rate of 12.5% (95% confidence interval, 1.5–33).24Recent recommendations are that the UBT is preferred where available.4
The US Food and Drug Administration recently cleared the UBiT-IR300 instrument for use with the commercial 13C-UBT. The costs of the UBT are but a fraction of those of endoscopy, not including indirect patient costs. Office-based testing has a separate reimbursement for testing, and overall the costs appear less than those of the stool antigen test. Economic impact studies comparing the tests are planned. Office-based infrared analysis for 13C makes near-patient or point-of-care UBT and analysis practical and should make accurate diagnosis of active H pylori infection readily available.
Acknowledgments
The authors thank the clinical study coordinators, including Ms Rebecca Garza, Ms Flora Godard, and Mr Zachary Patton for their conscientious efforts.
1. Levine TS, Price AB. Helicobacter pylori: enough to give anyone an ulcer. Br J Clin Pract 1993;47:328-32.
2. Staat MA, Kruszon-Moran D, McQuillan GM, Kaslow RA. A population-based survey of Helicobacter pylori infection in children and adolescents in the United States. J Infect Dis 1996;174:1120-3.
3. Opekun AR, Gilger MA, Denyes SM, et al. Helicobacter pylori infection in children of Texas. J Pediatr Gastroenterol Nutr 2000;31:405-10.
4. Malfertheiner P, Megraud F, O’Morain C, et al. Current concepts in the management of Helicobacter pylori infection—the Maastricht 2-2000 Consensus Report. Aliment Pharmacol Ther 2002;16:167-80.
5. Shiotani A, Nurgalieva ZZ, Yamaoka Y, Graham DY. Helicobacter pylori Med Clin North Am 2000;84:1125-36.
6. Meuer LN. Treatment of peptic ulcer disease and nonulcer dyspepsia. J Fam Pract 2001;50:614-9.
7. Greenberg PD, Koch J, Cello JP. Clinical utility of cost effectiveness of Helicobacter pylori testing for patients with duodenal and gastric ulcers. Am J Gastroenterol 1996;91:228-32.
8. Meurer LN, Bower DJ. Management of Helicobacter pylori infection. Am Fam Phys 2002;65:1327-36.
9. Megraud F. Diagnosis of Helicobacter pylori. Scand J Gastroenterol 1996;31(suppl):214-46.
10. Graham DY, Klein PD, Evans DJ, et al. Campylobacter pylori detected noninvasively by the 13C-urea breath test. Lancet 1987;1:1174-7.
11. Klein PD, Malaty HM, Martin RF, Graham KS, Genta RM, Graham DY. Noninvasive detection of Helicobacter pylori infection in clinical practice: the 13C urea breath test. Am J Gastroenterol 1996;91:690-4.
12. Graham DY, Klein PD. Accurate diagnosis of Helicobacter pylori: 13C-urea breath test. Gastroenterol Clin North Am 2000;29:885-93.
13. Graham DY, Runke D, Anderson-SY, Malaty HM, Klein PD. Citric acid as the test meal for the 13C-urea breath test. Am J Gastroenterol 1999;94:1214-7.
14. Braden B, Haisch M, Duan LP, Lembcke B, Caspary WF, Hering P. Clinically feasible stable isotope techniques at a reasonable price: analysis of 13CO2/12CO2-abundance in breath samples with a new isotope selective non-dispersive infrared spectrometer. Z Gastroenterol 1994;32:675-8.
15. Mion F, Ecochard R, Guitton J, Ponchon T. 13CO(2) breath tests: comparison of isotope-ratio mass spectrometry and non-dispersive infrared spectrometry results. Gastroenterol Clin Bio 2001;25:345-9.
16. Sheu BS, Lee SC, Yang HB, et al. Lower-dose 13C-urea breath test to detect Helicobacter pylori infection-comparison between infrared spectrometer and mass spectrometer. Aliment Pharmacol Ther 2000;10:1359-63.
17. Mansfield CD, Rutt HN. The application of infrared spectrometry to breath CO2 isotope-ratio measurements and the risk of spurious results. Phys Med Biol 1998;43:1225-39.
18. Ohara S, Kato M, Asaka M, Toyota T. The UbiT-100 13CO2 infrared analyzer: comparison between infrared spectrometric analysis and mass spectrometric analysis. Helicobacter 1998;3:49-53.
19. Savarino V, Mela GS, Zentilin P, et al. Comparison of isotope-ratio mass spectrometry and non-dispersive isotope-selective infrared spectroscopy for 13C-urea breath test. Am J Gastroenterol 1999;94:1203-8.
20. Goddard AF, Logan RPH. Review article: urea breath tests for detecting Helicobacter pylori. Aliment Pharmacol Ther 1997;11:641-9.
21. Goodwin CS, Mendall MM, Northfield TC. Helicobacter pylori infection. Lancet 1997;349:265-9.
22. Vaira D, Vakil N, Menegatti, et al. The stool antigen test for detection of Helicobacter pylori after eradication therapy. Ann Intern Med 2002;136:280-7.
23. Graham DY, Qureshi WA. Markers of infection. In: Mobley HLT, Mendz GL, Hazell SL, eds. Helicobacter pylori: physiology and genetics. Washington, DC: ASM Press; 2001;499-510.
24. Lopez Penas D, Naranjo Rodriguez A, Munoz Molinero J, et al. Efficacy of fecal detection of Helicobacter pylori with the HpSA technique in patients with upper digestive hemorrhage. Gastroenterol Hepatol 2001;24:5-8.
The13C-urea breath test provides accurate, noninvasive diagnosis of active Helicobacter pylori infection and can document posttherapy cure. This study evaluated point-of-care testing with onsite sample analysis with the use of a desktop infrared spectrophotometer. Ambulatory patients (N = 320) underwent 13C-urea breath testing, and breath samples were analyzed immediately by clinic staff with no prior breath testing experience. Duplicate samples were sent to a reference laboratory, and the results of both methods were compared. Point-of-care testing was simple, with an overall agreement of 99.1%. Accurate near-patient 13C-urea breath testing is now practical in the primary care setting even when done by inexperienced personnel.
Helicobacter pylori infection is etiologically associated with chronic gastritis, peptic ulcer disease, and gastric cancer.1-5Helicobacter pylori infection is also a consideration in the evaluation of uninvestigated or undifferentiated dyspepsia.4-7 The steps in the management of H pylori infection include diagnosis, choice of appropriate therapy, and confirmation of cure.4,5,8 Diagnosis and confirmation of cure require diagnostic testing, and the recent consensus has been in the direction of noninvasive testing.4,5
The urea breath test (UBT) is generally considered the clinical, gold standard, noninvasive test for detection of active H pylori infection.9 The intragastric hydrolysis of orally administered urea by H pylori urease produces a change in the isotopic ratio (13CO2/12CO2) in the breath.10 The 13C-UBT has been approved by the US Food and Drug Administration for pre- and posttherapy testing.11,12
Recently the 13C-UBT has been shortened and simplified by the use of a citric acid test meal and elimination of the requirement of a 4-hour fast.13 Use of infrared mass spectrophotometry for measuring 13CO2 enrichment in breath samples makes it theoretically possible to do office-based breath testing with onsite analysis.14-16 Infrared spectrophotometry has been shown in comparative studies to be an accurate method for assessing 13CO2 enrichment in breath.17-19 No comparative studies of the 2 analytical methods have been done in the United States.
This study examined the utility of UBT testing by comparing infrared spectrophotometry with traditional gas isotope ratio mass spectrometry in the primary care environment. Our hypothesis was that the results obtained from the primary care clinics would be as accurate as those obtained from the commercial laboratory or the more experienced hospital-based clinical laboratory.
Methods
This was a multicenter, prospective study designed to compare a new infrared spectrophotometer (UBiTIR300, Otsuka Pharmaceuticals, Tokyo, Japan) for measuring 13CO2 enrichment in breath with gas isotope ratio mass spectrometry (ABCA, Europa Scientific, Cheshire, UK). Subjects were recruited at the offices or clinics of 4 physicians’ including an indigent care primary care clinic, a hospital-based gastroenterology clinic, a private practice internal medicine office, an academic family medicine clinic, and a tertiary care clinical laboratory site. The study was done between July and September 2001. Consecutive patients were enrolled in the study if they expressed interest in participating and met the inclusion and exclusion criteria. Each site was provided with an infrared spectrophotometer, a breath gas transfer device, and commercially available UBT breath test collection kits (Meretek Diagnostics, Nashville, TN). Each kit contained a 13C-urea solution (125 mg in 75 mL of water), test meal pudding, and a specimen return box containing 4 bar-coded, evacuated 10-mL sample tubes. Before enrollment, all study personnel received approximately 1 hour of training in the performance of the test and use of the equipment.
Study procedures
Subjects included in the study were medically stable, ambulatory patients between 18 and 75 years old who were asymptomatic or experiencing dyspepsia. Potential subjects were excluded from study participation if they took bismuth preparations, antibiotics (ie, amoxicillin, tetracycline, metronidazole, clarithromycin, or azithromycin) or any anti-ulcer medication in dosages indicated for ulcer disease (ie, proton pump inhibitors, type 2 histamine blockers, or misoprostol) within 2 weeks before the study breath test. Exclusion criteria also included participation in a drug study within 4 weeks, treatment for eradication of H pylori within 4 weeks of the study breath test, or a history of gastric surgery or vagotomy for ulcer disease except simple closure of a gastric perforation.
The protocol was approved by the local Institutional Review Board for Human Studies, and all subjects provided written informed consent.
Testing began with a minimum 4-hour fast from solid food. Breath samples were obtained in disposable, balloonlike, breath collection bags designed for use with the infrared spectrophotometer. One sample was obtained immediately before ingestion of the 13C-urea test solution, and the second was collected 30 minutes after substrate ingestion. Paired sample aliquots were taken for separate analyses. Results from local infrared instruments were blinded to the central laboratory.
Statistical analyses
Each primary care site was asked to enroll subjects until 80 positive cases were identified from among all sites. The clinical laboratory site tested a minimum of 30 positive and 30 negative cases. The primary endpoint was the percentage of agreement (overall and within positive and negative cases separately) of results from both methods. Delta-over-baseline (DOB) enrichment values below 2.4 per mil were deemed negative and values greater than or equal to 2.4 per mil were deemed positive. The predicate reference method was gas isotope ratio mass spectrometry. Equivalence was defined by the percentage of agreement for positive and negative cases based on gas isotope ratio mass spectrometry results of at least 95%, and the lower limit of the 95% confidence interval was based on a percentage of agreement of at least 90% for positive cases.
Results
The primary care centers enrolled 258 subjects and the clinical laboratory enrolled 64 subjects, for a total enrollment of 322. The subjects’ mean age was 41.5 years (range, 18–70 years), with 88 black non-Hispanics, 106 Hispanics, 92 whites, 32 Asian/Pacific Islanders, and 4 other ethnic groups. There were 215 women and 107 men. Approximately 18% had active or previous gastrointestinal ailments, including previously diagnosed H pylori infection (11%) and peptic ulcer disease (3%).
There was excellent agreement between methods (Table), with an overall agreement of 99% (95% confidence interval, 97.3–99.7). Two subjects were excluded from the analysis of the primary and secondary endpoints because 1 or both assay values were missing. The data showed close correlation between methods among all sites (Figure). Evaluation by the personnel who performed the tests and analyses indicated that the office procedure was easy and nonintrusive.
There were 3 disagreements between the results obtained with the devices, 1 from the gastroenterology site and 2 from the clinical laboratory site. All results were near the cutoff value.
TABLE
Comparison of results between IRMS and GIRMS*
| GIRMS, % | |||
|---|---|---|---|
| IRMS, % | Negative | Positive | Total |
| Negative | 1 | 115 | 116 |
| Positive | 202 | 2 | 204 |
| Total | 203 | 117 | 320 |
| *Overall agreement, 99.1% (95% confidence interval, 97.3–99.7); positive agreement, 98.2% (95% confidence interval, 94.2–99.7); negative agreement, 99.5% (95% confidence interval, 97.3–99.9). | |||
| Kappa statistic = 0.98. | |||
| GIRMS, gas isotope ratio mass spectrometry; IRMS, infrared mass spectrophotometry. | |||
FIGURE
Comparison of results between 2 methods of analysis of 13CO2 breath sample enrichments
Discussion
13C-urea breath testing is an accurate diagnostic method for the detection of active H pylori infection12,19-21 and point-of-care assessment of curative therapy. This study confirmed the hypothesis that the infrared instrument is an easy to operate alternative to the original sendout analyses. Rapid turnaround allows for decisions regarding therapy to be made at the time of care. The currently approved UBT in the United States does not require fasting from solid food for longer than 1 hour.
Noninvasive alternatives to UBT include serology and stool antigen testing. Serology assays cannot discriminate between active and recent past infections. Stool antigen testing requires patient compliance with specimen collection and is a sendout test. In general, although studies using pretreatment stool antigen tests have shown sensitivity and specificity comparable to those of histology or UBT, it has become evident that there can be considerable lot-to-lot variation in stool antigen tests.22 The most likely explanation is that the polyclonal serum used for the capture antibody is obtained from rabbits and thus difficult to standardize.23 Stool antigen testing has also proven to be less reliable when used soon after the end of therapy, and it is now generally recommended that one must wait 6 or 8 weeks after therapy when using the stool antigen test to confirm eradication. For example, a recent study had a false negative rate of 12.5% (95% confidence interval, 1.5–33).24Recent recommendations are that the UBT is preferred where available.4
The US Food and Drug Administration recently cleared the UBiT-IR300 instrument for use with the commercial 13C-UBT. The costs of the UBT are but a fraction of those of endoscopy, not including indirect patient costs. Office-based testing has a separate reimbursement for testing, and overall the costs appear less than those of the stool antigen test. Economic impact studies comparing the tests are planned. Office-based infrared analysis for 13C makes near-patient or point-of-care UBT and analysis practical and should make accurate diagnosis of active H pylori infection readily available.
Acknowledgments
The authors thank the clinical study coordinators, including Ms Rebecca Garza, Ms Flora Godard, and Mr Zachary Patton for their conscientious efforts.
The13C-urea breath test provides accurate, noninvasive diagnosis of active Helicobacter pylori infection and can document posttherapy cure. This study evaluated point-of-care testing with onsite sample analysis with the use of a desktop infrared spectrophotometer. Ambulatory patients (N = 320) underwent 13C-urea breath testing, and breath samples were analyzed immediately by clinic staff with no prior breath testing experience. Duplicate samples were sent to a reference laboratory, and the results of both methods were compared. Point-of-care testing was simple, with an overall agreement of 99.1%. Accurate near-patient 13C-urea breath testing is now practical in the primary care setting even when done by inexperienced personnel.
Helicobacter pylori infection is etiologically associated with chronic gastritis, peptic ulcer disease, and gastric cancer.1-5Helicobacter pylori infection is also a consideration in the evaluation of uninvestigated or undifferentiated dyspepsia.4-7 The steps in the management of H pylori infection include diagnosis, choice of appropriate therapy, and confirmation of cure.4,5,8 Diagnosis and confirmation of cure require diagnostic testing, and the recent consensus has been in the direction of noninvasive testing.4,5
The urea breath test (UBT) is generally considered the clinical, gold standard, noninvasive test for detection of active H pylori infection.9 The intragastric hydrolysis of orally administered urea by H pylori urease produces a change in the isotopic ratio (13CO2/12CO2) in the breath.10 The 13C-UBT has been approved by the US Food and Drug Administration for pre- and posttherapy testing.11,12
Recently the 13C-UBT has been shortened and simplified by the use of a citric acid test meal and elimination of the requirement of a 4-hour fast.13 Use of infrared mass spectrophotometry for measuring 13CO2 enrichment in breath samples makes it theoretically possible to do office-based breath testing with onsite analysis.14-16 Infrared spectrophotometry has been shown in comparative studies to be an accurate method for assessing 13CO2 enrichment in breath.17-19 No comparative studies of the 2 analytical methods have been done in the United States.
This study examined the utility of UBT testing by comparing infrared spectrophotometry with traditional gas isotope ratio mass spectrometry in the primary care environment. Our hypothesis was that the results obtained from the primary care clinics would be as accurate as those obtained from the commercial laboratory or the more experienced hospital-based clinical laboratory.
Methods
This was a multicenter, prospective study designed to compare a new infrared spectrophotometer (UBiTIR300, Otsuka Pharmaceuticals, Tokyo, Japan) for measuring 13CO2 enrichment in breath with gas isotope ratio mass spectrometry (ABCA, Europa Scientific, Cheshire, UK). Subjects were recruited at the offices or clinics of 4 physicians’ including an indigent care primary care clinic, a hospital-based gastroenterology clinic, a private practice internal medicine office, an academic family medicine clinic, and a tertiary care clinical laboratory site. The study was done between July and September 2001. Consecutive patients were enrolled in the study if they expressed interest in participating and met the inclusion and exclusion criteria. Each site was provided with an infrared spectrophotometer, a breath gas transfer device, and commercially available UBT breath test collection kits (Meretek Diagnostics, Nashville, TN). Each kit contained a 13C-urea solution (125 mg in 75 mL of water), test meal pudding, and a specimen return box containing 4 bar-coded, evacuated 10-mL sample tubes. Before enrollment, all study personnel received approximately 1 hour of training in the performance of the test and use of the equipment.
Study procedures
Subjects included in the study were medically stable, ambulatory patients between 18 and 75 years old who were asymptomatic or experiencing dyspepsia. Potential subjects were excluded from study participation if they took bismuth preparations, antibiotics (ie, amoxicillin, tetracycline, metronidazole, clarithromycin, or azithromycin) or any anti-ulcer medication in dosages indicated for ulcer disease (ie, proton pump inhibitors, type 2 histamine blockers, or misoprostol) within 2 weeks before the study breath test. Exclusion criteria also included participation in a drug study within 4 weeks, treatment for eradication of H pylori within 4 weeks of the study breath test, or a history of gastric surgery or vagotomy for ulcer disease except simple closure of a gastric perforation.
The protocol was approved by the local Institutional Review Board for Human Studies, and all subjects provided written informed consent.
Testing began with a minimum 4-hour fast from solid food. Breath samples were obtained in disposable, balloonlike, breath collection bags designed for use with the infrared spectrophotometer. One sample was obtained immediately before ingestion of the 13C-urea test solution, and the second was collected 30 minutes after substrate ingestion. Paired sample aliquots were taken for separate analyses. Results from local infrared instruments were blinded to the central laboratory.
Statistical analyses
Each primary care site was asked to enroll subjects until 80 positive cases were identified from among all sites. The clinical laboratory site tested a minimum of 30 positive and 30 negative cases. The primary endpoint was the percentage of agreement (overall and within positive and negative cases separately) of results from both methods. Delta-over-baseline (DOB) enrichment values below 2.4 per mil were deemed negative and values greater than or equal to 2.4 per mil were deemed positive. The predicate reference method was gas isotope ratio mass spectrometry. Equivalence was defined by the percentage of agreement for positive and negative cases based on gas isotope ratio mass spectrometry results of at least 95%, and the lower limit of the 95% confidence interval was based on a percentage of agreement of at least 90% for positive cases.
Results
The primary care centers enrolled 258 subjects and the clinical laboratory enrolled 64 subjects, for a total enrollment of 322. The subjects’ mean age was 41.5 years (range, 18–70 years), with 88 black non-Hispanics, 106 Hispanics, 92 whites, 32 Asian/Pacific Islanders, and 4 other ethnic groups. There were 215 women and 107 men. Approximately 18% had active or previous gastrointestinal ailments, including previously diagnosed H pylori infection (11%) and peptic ulcer disease (3%).
There was excellent agreement between methods (Table), with an overall agreement of 99% (95% confidence interval, 97.3–99.7). Two subjects were excluded from the analysis of the primary and secondary endpoints because 1 or both assay values were missing. The data showed close correlation between methods among all sites (Figure). Evaluation by the personnel who performed the tests and analyses indicated that the office procedure was easy and nonintrusive.
There were 3 disagreements between the results obtained with the devices, 1 from the gastroenterology site and 2 from the clinical laboratory site. All results were near the cutoff value.
TABLE
Comparison of results between IRMS and GIRMS*
| GIRMS, % | |||
|---|---|---|---|
| IRMS, % | Negative | Positive | Total |
| Negative | 1 | 115 | 116 |
| Positive | 202 | 2 | 204 |
| Total | 203 | 117 | 320 |
| *Overall agreement, 99.1% (95% confidence interval, 97.3–99.7); positive agreement, 98.2% (95% confidence interval, 94.2–99.7); negative agreement, 99.5% (95% confidence interval, 97.3–99.9). | |||
| Kappa statistic = 0.98. | |||
| GIRMS, gas isotope ratio mass spectrometry; IRMS, infrared mass spectrophotometry. | |||
FIGURE
Comparison of results between 2 methods of analysis of 13CO2 breath sample enrichments
Discussion
13C-urea breath testing is an accurate diagnostic method for the detection of active H pylori infection12,19-21 and point-of-care assessment of curative therapy. This study confirmed the hypothesis that the infrared instrument is an easy to operate alternative to the original sendout analyses. Rapid turnaround allows for decisions regarding therapy to be made at the time of care. The currently approved UBT in the United States does not require fasting from solid food for longer than 1 hour.
Noninvasive alternatives to UBT include serology and stool antigen testing. Serology assays cannot discriminate between active and recent past infections. Stool antigen testing requires patient compliance with specimen collection and is a sendout test. In general, although studies using pretreatment stool antigen tests have shown sensitivity and specificity comparable to those of histology or UBT, it has become evident that there can be considerable lot-to-lot variation in stool antigen tests.22 The most likely explanation is that the polyclonal serum used for the capture antibody is obtained from rabbits and thus difficult to standardize.23 Stool antigen testing has also proven to be less reliable when used soon after the end of therapy, and it is now generally recommended that one must wait 6 or 8 weeks after therapy when using the stool antigen test to confirm eradication. For example, a recent study had a false negative rate of 12.5% (95% confidence interval, 1.5–33).24Recent recommendations are that the UBT is preferred where available.4
The US Food and Drug Administration recently cleared the UBiT-IR300 instrument for use with the commercial 13C-UBT. The costs of the UBT are but a fraction of those of endoscopy, not including indirect patient costs. Office-based testing has a separate reimbursement for testing, and overall the costs appear less than those of the stool antigen test. Economic impact studies comparing the tests are planned. Office-based infrared analysis for 13C makes near-patient or point-of-care UBT and analysis practical and should make accurate diagnosis of active H pylori infection readily available.
Acknowledgments
The authors thank the clinical study coordinators, including Ms Rebecca Garza, Ms Flora Godard, and Mr Zachary Patton for their conscientious efforts.
1. Levine TS, Price AB. Helicobacter pylori: enough to give anyone an ulcer. Br J Clin Pract 1993;47:328-32.
2. Staat MA, Kruszon-Moran D, McQuillan GM, Kaslow RA. A population-based survey of Helicobacter pylori infection in children and adolescents in the United States. J Infect Dis 1996;174:1120-3.
3. Opekun AR, Gilger MA, Denyes SM, et al. Helicobacter pylori infection in children of Texas. J Pediatr Gastroenterol Nutr 2000;31:405-10.
4. Malfertheiner P, Megraud F, O’Morain C, et al. Current concepts in the management of Helicobacter pylori infection—the Maastricht 2-2000 Consensus Report. Aliment Pharmacol Ther 2002;16:167-80.
5. Shiotani A, Nurgalieva ZZ, Yamaoka Y, Graham DY. Helicobacter pylori Med Clin North Am 2000;84:1125-36.
6. Meuer LN. Treatment of peptic ulcer disease and nonulcer dyspepsia. J Fam Pract 2001;50:614-9.
7. Greenberg PD, Koch J, Cello JP. Clinical utility of cost effectiveness of Helicobacter pylori testing for patients with duodenal and gastric ulcers. Am J Gastroenterol 1996;91:228-32.
8. Meurer LN, Bower DJ. Management of Helicobacter pylori infection. Am Fam Phys 2002;65:1327-36.
9. Megraud F. Diagnosis of Helicobacter pylori. Scand J Gastroenterol 1996;31(suppl):214-46.
10. Graham DY, Klein PD, Evans DJ, et al. Campylobacter pylori detected noninvasively by the 13C-urea breath test. Lancet 1987;1:1174-7.
11. Klein PD, Malaty HM, Martin RF, Graham KS, Genta RM, Graham DY. Noninvasive detection of Helicobacter pylori infection in clinical practice: the 13C urea breath test. Am J Gastroenterol 1996;91:690-4.
12. Graham DY, Klein PD. Accurate diagnosis of Helicobacter pylori: 13C-urea breath test. Gastroenterol Clin North Am 2000;29:885-93.
13. Graham DY, Runke D, Anderson-SY, Malaty HM, Klein PD. Citric acid as the test meal for the 13C-urea breath test. Am J Gastroenterol 1999;94:1214-7.
14. Braden B, Haisch M, Duan LP, Lembcke B, Caspary WF, Hering P. Clinically feasible stable isotope techniques at a reasonable price: analysis of 13CO2/12CO2-abundance in breath samples with a new isotope selective non-dispersive infrared spectrometer. Z Gastroenterol 1994;32:675-8.
15. Mion F, Ecochard R, Guitton J, Ponchon T. 13CO(2) breath tests: comparison of isotope-ratio mass spectrometry and non-dispersive infrared spectrometry results. Gastroenterol Clin Bio 2001;25:345-9.
16. Sheu BS, Lee SC, Yang HB, et al. Lower-dose 13C-urea breath test to detect Helicobacter pylori infection-comparison between infrared spectrometer and mass spectrometer. Aliment Pharmacol Ther 2000;10:1359-63.
17. Mansfield CD, Rutt HN. The application of infrared spectrometry to breath CO2 isotope-ratio measurements and the risk of spurious results. Phys Med Biol 1998;43:1225-39.
18. Ohara S, Kato M, Asaka M, Toyota T. The UbiT-100 13CO2 infrared analyzer: comparison between infrared spectrometric analysis and mass spectrometric analysis. Helicobacter 1998;3:49-53.
19. Savarino V, Mela GS, Zentilin P, et al. Comparison of isotope-ratio mass spectrometry and non-dispersive isotope-selective infrared spectroscopy for 13C-urea breath test. Am J Gastroenterol 1999;94:1203-8.
20. Goddard AF, Logan RPH. Review article: urea breath tests for detecting Helicobacter pylori. Aliment Pharmacol Ther 1997;11:641-9.
21. Goodwin CS, Mendall MM, Northfield TC. Helicobacter pylori infection. Lancet 1997;349:265-9.
22. Vaira D, Vakil N, Menegatti, et al. The stool antigen test for detection of Helicobacter pylori after eradication therapy. Ann Intern Med 2002;136:280-7.
23. Graham DY, Qureshi WA. Markers of infection. In: Mobley HLT, Mendz GL, Hazell SL, eds. Helicobacter pylori: physiology and genetics. Washington, DC: ASM Press; 2001;499-510.
24. Lopez Penas D, Naranjo Rodriguez A, Munoz Molinero J, et al. Efficacy of fecal detection of Helicobacter pylori with the HpSA technique in patients with upper digestive hemorrhage. Gastroenterol Hepatol 2001;24:5-8.
1. Levine TS, Price AB. Helicobacter pylori: enough to give anyone an ulcer. Br J Clin Pract 1993;47:328-32.
2. Staat MA, Kruszon-Moran D, McQuillan GM, Kaslow RA. A population-based survey of Helicobacter pylori infection in children and adolescents in the United States. J Infect Dis 1996;174:1120-3.
3. Opekun AR, Gilger MA, Denyes SM, et al. Helicobacter pylori infection in children of Texas. J Pediatr Gastroenterol Nutr 2000;31:405-10.
4. Malfertheiner P, Megraud F, O’Morain C, et al. Current concepts in the management of Helicobacter pylori infection—the Maastricht 2-2000 Consensus Report. Aliment Pharmacol Ther 2002;16:167-80.
5. Shiotani A, Nurgalieva ZZ, Yamaoka Y, Graham DY. Helicobacter pylori Med Clin North Am 2000;84:1125-36.
6. Meuer LN. Treatment of peptic ulcer disease and nonulcer dyspepsia. J Fam Pract 2001;50:614-9.
7. Greenberg PD, Koch J, Cello JP. Clinical utility of cost effectiveness of Helicobacter pylori testing for patients with duodenal and gastric ulcers. Am J Gastroenterol 1996;91:228-32.
8. Meurer LN, Bower DJ. Management of Helicobacter pylori infection. Am Fam Phys 2002;65:1327-36.
9. Megraud F. Diagnosis of Helicobacter pylori. Scand J Gastroenterol 1996;31(suppl):214-46.
10. Graham DY, Klein PD, Evans DJ, et al. Campylobacter pylori detected noninvasively by the 13C-urea breath test. Lancet 1987;1:1174-7.
11. Klein PD, Malaty HM, Martin RF, Graham KS, Genta RM, Graham DY. Noninvasive detection of Helicobacter pylori infection in clinical practice: the 13C urea breath test. Am J Gastroenterol 1996;91:690-4.
12. Graham DY, Klein PD. Accurate diagnosis of Helicobacter pylori: 13C-urea breath test. Gastroenterol Clin North Am 2000;29:885-93.
13. Graham DY, Runke D, Anderson-SY, Malaty HM, Klein PD. Citric acid as the test meal for the 13C-urea breath test. Am J Gastroenterol 1999;94:1214-7.
14. Braden B, Haisch M, Duan LP, Lembcke B, Caspary WF, Hering P. Clinically feasible stable isotope techniques at a reasonable price: analysis of 13CO2/12CO2-abundance in breath samples with a new isotope selective non-dispersive infrared spectrometer. Z Gastroenterol 1994;32:675-8.
15. Mion F, Ecochard R, Guitton J, Ponchon T. 13CO(2) breath tests: comparison of isotope-ratio mass spectrometry and non-dispersive infrared spectrometry results. Gastroenterol Clin Bio 2001;25:345-9.
16. Sheu BS, Lee SC, Yang HB, et al. Lower-dose 13C-urea breath test to detect Helicobacter pylori infection-comparison between infrared spectrometer and mass spectrometer. Aliment Pharmacol Ther 2000;10:1359-63.
17. Mansfield CD, Rutt HN. The application of infrared spectrometry to breath CO2 isotope-ratio measurements and the risk of spurious results. Phys Med Biol 1998;43:1225-39.
18. Ohara S, Kato M, Asaka M, Toyota T. The UbiT-100 13CO2 infrared analyzer: comparison between infrared spectrometric analysis and mass spectrometric analysis. Helicobacter 1998;3:49-53.
19. Savarino V, Mela GS, Zentilin P, et al. Comparison of isotope-ratio mass spectrometry and non-dispersive isotope-selective infrared spectroscopy for 13C-urea breath test. Am J Gastroenterol 1999;94:1203-8.
20. Goddard AF, Logan RPH. Review article: urea breath tests for detecting Helicobacter pylori. Aliment Pharmacol Ther 1997;11:641-9.
21. Goodwin CS, Mendall MM, Northfield TC. Helicobacter pylori infection. Lancet 1997;349:265-9.
22. Vaira D, Vakil N, Menegatti, et al. The stool antigen test for detection of Helicobacter pylori after eradication therapy. Ann Intern Med 2002;136:280-7.
23. Graham DY, Qureshi WA. Markers of infection. In: Mobley HLT, Mendz GL, Hazell SL, eds. Helicobacter pylori: physiology and genetics. Washington, DC: ASM Press; 2001;499-510.
24. Lopez Penas D, Naranjo Rodriguez A, Munoz Molinero J, et al. Efficacy of fecal detection of Helicobacter pylori with the HpSA technique in patients with upper digestive hemorrhage. Gastroenterol Hepatol 2001;24:5-8.