User login
Obstructive sleep apnea (OSA), the repetitive collapse of posterior oropharynx during sleep resulting in hypoxia and/or arousals from sleep, is the most common form of sleep disordered breathing and a common chronic respiratory disorders among middle-aged adults. OSA can lead to significant health problems, such as worsened cardiometabolic disease and cognitive impairment, which can increase morbidity and mortality.1
The gold standard for OSA diagnosis is polysomnography (PSG), although home sleep studies can be performed for select patients. OSA diagnoses are based on the number of times per hour of sleep a patient’s airway narrows or collapses, reducing or stopping airflow, scored as hypopnea or apnea events, respectively. An Apnea-Hypopnea Index (AHI) score of 5 to 14 events/hour is considered mild OSA, 15 to 30 events/hour moderate OSA, and ≥ 30 events/hour severe OSA.2
Treatment commonly includes positive airway pressure (PAP) but more than one-half of patients are not adherent to continuous PAP (CPAP) treatment after about 90 days.3 Efficacy of treatments vary as a function of disease severity and etiology, which—in addition to the classic presentation of obesity with large neck/narrowupper airway—includes craniofacial abnormalities, altered muscle function in the upper airway, pharyngeal neuropathy, and fluid shifts to the neck.
Background
The American Academy of Sleep Medicine (AASM) estimates that 10% to 17% of adults in the United States have OSA.4 Compared with civilians, the military population generally is younger and healthier. Service members have access to regular health care with yearly physical examinations, exercise scheduled into the workday, and mandatory height/weight and fitness standards. Because obesity is a major risk factor for OSA, and the incidence of obesity is relatively low in the military population (estimated at 18.8% in 2021 vs 39.8% among all US adults aged 20 to 39 years), it might be expected that incidence of OSA would be correspondingly low.5,6 However, there is evidence of a rapidly increasing incidence of OSA in military populations. A 2021 study revealed that OSA incidence rates increased from 11 to 333 per 10,000 between 2005 and 2019 across all military branches and demographics, with the highest rate among Army personnel.7 An earlier study revealed a 600% increase in OSA incidence among Army personnel between 2003 and 2011.8
Several factors likely contributed to this increase, including expanding obesity and greater physician awareness and availability of sleep study centers. Rogers and colleagues found that 40% to 50% of incident OSA diagnoses among military personnel occur within 12 months of separation, suggesting that the secondary gains associated with military disability benefits might motivate OSA evaluation.9 It is possible that secondary gain is a factor because an OSA diagnosis can range from a 0% to 100% disability rating, depending on the severity.10 This disability claim is based on evidence that untreated OSA can negatively affect long-term health and mission readiness.8 For example, untreated OSA can lead to hypertension, which contributes to a long list of adverse health and wellness consequences. Most importantly for the military, OSA has been shown to increase daytime sleepiness and reduce cognitive performance.10
The current first-line treatment for OSA is CPAP, which improves symptoms of daytime sleepiness, hypertension management, and daytime alertness.11 Despite its efficacy, nonadherence rates range from 29% to 83%.12-15 Nonadherence factors include lifestyle changes, adverse effects (eg, nasal congestion), and lack of education on proper use.11 Lifestyle changes needed to increase the likelihood of successful therapy, such as regular sleep schedules and proper CPAP cleaning and maintenance, are difficult for military personnel because of the nature of continuous or sustained operations that might require shift work and/or around-the-clock (ie, 24-hour, 7 days a week) task performance. Traveling with CPAP is an added burden for service members deployed to combat operations (ie, added luggage, weight, maintenance). Although alternate treatments such as oral appliances (ie, custom dental devices) are available, they generally are less effective than CPAP.2 Oral appliances could be a reasonable alternative treatment for some patients who cannot manage their OSA with behavioral modifications and are intolerant or unable to effectively use CPAP. This could include patients in the military who are deployed to austere environments.
Surgically implanted hypoglossal nerve stimulator (HGNS) treatment may provide long-term health benefits to service members. After the device is implanted near the hypoglossal nerve, electrical stimulation causes the tongue to move forward, which opens the airway in the anteroposterior dimension. The most important consideration is the mechanism of airway collapse. HGNS is not effective for patients whose OSA events are caused by circumferential collapse of other airway muscles. The cause of airway collapse is ascertained before surgery with drug-induced sleep endoscopy, a procedure that allows visualization of conformational changes in the upper airway during OSA events.
The US Food and Drug Administration (FDA) approved HGNS in 2014. However, it is not considered a first-line treatment for OSA by the AASM. Original candidate criteria for HGNS included an AHI score of 15 to 65 events/hour, age ≥ 18 years, failed CPAP use, body mass index (BMI) < 32, absence of palatal complete concentric collapse, and central apneas comprising < 25% of total events.16 In June 2023, the FDA expanded approval to increase the upper limit of AHI to 100 events/hour and the BMI to < 40.17
HGNS has been reported to be effective in appropriately selected patients with OSA at tertiary care centers with established multidisciplinary sleep surgical programs. These benefits have not been confirmed in larger, community-based settings, where most of these surgeries occur. In community practice, there is significant confusion among patients and clinicians about the optimal pathway for patient selection and clinical follow-up. Many patients view HGNS as a viable alternative to CPAP, but initially do not understand that it requires surgery. Surgical treatments for OSA, such as HGNS, are appealing because they suggest a 1-time intervention that permanently treats the condition, without need for follow-up or equipment resupply. HGNS might be an appealing treatment option because it is less obtrusive than CPAP and requires fewer resources for set-up and maintenance. Also, it does not cause skin irritation (a possible adverse effect of nightly use of a CPAP mask), allows the individual to sleep in a variety of positions, has less impact on social and sex life, and does not require an electric outlet. In the long term, HGNS might be more cost effective because there is no yearly physician follow-up or equipment resupply and/or maintenance.
The military population has specific demands that impact delivery and effectiveness of health care. Among service members with OSA, CPAP treatment can be challenging because of low adherence, required annual follow-up despite frequent moving cycles that pose a challenge for care continuity, and duty limitations for affected service members (ie, the requirement for a waiver to deploy and potential medical separation if symptoms are not adequately controlled). As the incidence of OSA continues to increase among service members, so does the need for OSA treatment options that are efficacious as CPAP but better tolerated and more suitable for use during military operations. The aim of this review is to assess the effectiveness of HGNS and its potential use by the military OSA patient population.
METHODS
To identify eligible studies, we employed PICOS: Population (patients aged ≥ 18 years with a history of OSA), Intervention (HGNS), Comparator (standard of care PAP therapy), Outcome (AHI or Epworth Sleepiness Scale [ESS], and Study (randomized control trial [RCT] or clinical trial). Studies were excluded if they were not written in English or included pediatric populations. The ESS is a subjective rating scale used to determine and quantify a patient’s level of daytime sleepiness, using a 4-point scale for the likelihood of falling asleep totaled across 8 different situations.18 Daytime sleepiness is considered lower normal(0-5 points), higher normal (6-10 points), mild or moderate excessive (11-15 points), and severe excessive (16-24 points).
Literature Search
We conducted a review of PubMed and Scopus for RCTs and controlled trials published from 2013 to 2023 that included the keywords and phrases: obstructive sleep apnea and either hypoglossal nerve stimulation or upper airway stimulation. The final literature search was performed December 8, 2023.
Two authors independently assessed the titles and abstracts of studies identified in the literature search based on the predefined inclusion criteria. If it was not clear whether an article met inclusion criteria based on its title and/or abstract, the 2 review authors assessed the full text of study and resolved any disagreement through consensus. If consensus was not obtained, a third author was consulted. No duplicates were identified. The PRISMA study selection process is presented in the Figure.
Data extraction was performed by 1 independent reviewer. A second author reviewed the extracted data. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third author was consulted. Study data included methods (study design and study objective), participants mean age, inclusion criteria, exclusion criteria, interventions and comparators, and primary study outcomes.
The quality of evidence was assessed using a rating of 1 to 5 based on a modified version of the Oxford Centre for Evidence-based Medicine Levels of Evidence and Grades of Recommendation.19 A rating of 1 indicated a properly powered and conducted RCT, 2 demonstrated a well-designed controlled trial without randomization or prospective comparative cohort trial, 3 designated a case-control study or retrospective cohort study, 4 signified a case series with or without intervention or a cross-sectional study, and 5 denoted an opinion of respected authorities or case reports. Two reviewers independently evaluated the quality of evidence. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third review author was consulted.
RESULTS
We identified 30 studies; 19 articles did not meet inclusion criteria. The remaining 11 articles were divided into 4 cohorts. Five articles were based on data from the STAR trial, a multicenter study that included adults with moderate-to-severe OSA and inadequate adherence to CPAP.20-24 Four articles used the same patient selection criteria as the STAR trial for a long-term German postmarket study of upper airway stimulation efficacy with OSA.25-28 The third and fourth cohorts each consist of 31 patients with moderate-to-severe OSA with CPAP nonadherence or failure.29,30 The STAR trial included follow-up at 5 years, and the German-postmarket had a follow-up at3 years. The remaining 2 cohorts have 1-year follow-ups.
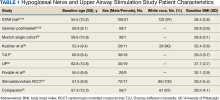
The Scopus review identified 304 studies; 299 did not meet inclusion criteria and 1 was part of the STAR trial.31 The remaining 4 articles were classified as distinct cohorts. Huntley and colleagues included patients from Thomas Jefferson University (TJU) and University of Pittsburgh (UP) academic medical centers.32 The Pordzik and colleagues cohort received implantation at a tertiary medical center, an RCCT, and a 1:1 comparator trial (Table 1).33-35
STAR Trial
This multicenter, prospective, single-group cohort study was conducted in the US, Germany, Belgium, Netherlands, and France. The STAR trial included 126 patients who were not CPAP therapy adherent. Patients were excluded if they had AHI < 20 or > 50, central sleep apnea > 25% of total AHI, anatomical abnormalities that prevent effective assessment of upper-airway stimulation, complete concentric collapse of the retropalatal airway during drug-induced sleep, neuromuscular disease, hypoglossal-nerve palsy, severe restrictive or obstructive pulmonary disease, moderate-to-severe pulmonary arterial hypertension, severe valvular heart disease, New York Heart Association class III or IV heart failure, recent myocardial infarction or severe cardiac arrhythmias (within the past 6 months), persistent uncontrolled hypertension despite medication use, active psychiatric illness, or coexisting nonrespiratory sleep disorders that would confound functional sleep assessment. Primary outcome measures included the AHI and oxygen desaturation index (ODI) with secondary outcomes using the ESS, the Functional Outcomes of Sleep Questionnaire (FOSQ), and the percentage of sleep time with oxygen saturation < 90%. Of 126 patients who received implantation, 71 underwent an overnight PSG evaluation at 5-year follow-up. Mean (SD) AHI at baseline was reduced with HGNS treatment to from 32.0 (11.8) to 12.4 (16.3). Mean (SD) ESS for 92 participants with 2 measurements declined from 11.6 (5.0) at baseline to 6.9 (4.7) at 5-year follow-up.
The STAR trial included a randomized controlled withdrawal study for 46 patients who had a positive response to therapy to evaluate efficacy and durability of upper airway stimulation. Patients were randomly assigned to therapy maintenance or therapy withdrawal groups for ≥ 1 week. The short-term withdrawal effect was assessed using the original trial outcome measures and indicated that both the withdrawal and maintenance groups showed improvements at 12 months compared with the baseline. However, after the randomized withdrawal, the withdrawal group’s outcome measures deteriorated to baseline levels while the maintenance group showed no change. At 18 months of therapy, outcome measures for both groups were similar to those observed with therapy at 12 months.24 The STAR trial included self-reported outcomes at baseline, 12 months, and 24 months that used ESS to measure daytime sleepiness. These results included subsequent STAR trial reports.20-24,31
The German Postmarket Cohort
This multicenter, prospective, single-arm study used selection criteria that were based on those used in the STAR trial and included patients with moderate-to-severe OSA and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, AHI < 15 or > 65; central apnea index > 25% of total AHI; or complete concentric collapse at the velopharynx during drug-induced sleep. Measured outcomes included AHI, ODI, FOSQ, and ESS. Among the 60 participants, 38 received implantation and a 3-year follow-up. Mean (SD) AHI decreased from 31.2 (13.2) at baseline to 13.1 (14.1) at follow-up, while mean (SD) ESS decreased from 12.8 (5.3) at baseline to 6.0 (3.2) at follow-up.25-28
Munich Cohort
This single-center, prospective clinical trial included patients with AHI > 15 and < 65, central apnea index < 25% of total AHI, and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, anatomical abnormalities that would prevent effective assessment of upper-airway stimulation; all other exclusion criteria matched those used in the STAR trial. Among 31 patients who received implants and completed a 1-year follow-up, mean (SD) AHI decreased from 32.9 (11.2) at baseline to 7.1 (5.9) at follow-up and mean (SD) ESS decreased from 12.6 (5.6) at baseline to 5.9 (5.2) at follow-up.29
Kezirian and Colleagues Cohort
This prospective, single-arm, open-label study was conducted at 4 Australian and 4 US sites. Selection criteria included moderate-to-severe OSA with failure of CPAP, AHI of 20 to 100 with ≥ 15 events/hour occurring in sleep that was non-REM (rapid eye movement) sleep, BMI ≤ 40 (Australia) or ≤ 37 (US), and a predominance of hypopneas (≥ 80% of disordered breathing events during sleep). Patients were excluded if they had earlier upper airway surgery, markedly enlarged tonsils, uncontrolled nasal obstruction, severe retrognathia, > 5% central or mixed apneic events, incompletely treated sleep disorders other than OSA, or a major disorder of the pulmonary, cardiac, renal, or nervous systems. Data were reported for 31 patients whose mean (SD) AHI declined from 45.4 (17.5) at baseline to 25.3 (20.6) at 1-year follow-up and mean (SD) ESS score declined from 12.1 (4.6) at baseline to 7.9 (3.8) 1 year later.30
TJU and UP Cohorts
The TJU and UP cohorts are composed of patients who underwent implantation between May 2014 and August 2016 at 2 academic centers.31,32 Selection criteria was consistent with that used in the STAR trial, and patients completed postoperative titration PSG and outpatient follow-up (48 patients at TJU and 49 at UP). Primary outcomes included AHI, ESS, and O2 nadir. Secondary outcomes consisted of surgical success and percentage of patients tolerating optimal titration setting at follow-up. Postoperative outcomes were assessed during the titration PSG. Time from initial ESS to postoperative PSG at TJU was 1.7 years and at UP was 1.9 years. Time from initial AHI to postoperative PSG at TJU was 90.4 days and 85.2 days at UP. At TJU, mean (SD) AHI and ESS dropped from 35.9 (20.8) and 11.1 (3.8), respectively at baseline to 6.3 (11.5) and 5.8 (3.4), respectively at follow-up. At UP, mean (SD) AHI and ESS fell from 35.3 (15.3) and 10.9 (4.9), respectively at baseline to 6.3 (6.1) and 6.6 (4.5), respectively at follow-up. There were no site-related differences in rates of AHI, ESS, or surgical success.31
Pordzik and Colleagues Cohort
This cohort of 29 patients underwent implantation between February 2020 and June 2022 at a tertiary university medical center with both pre- and postoperative PSG. Selection criteria was consistent with that of the German postmarket cohort. Postoperative PSG was completed a mean (SD) 96.3 (27.0) days after device activation. Mean (SD) AHI dropped from 38.6 (12.7) preoperatively to 24.4 (13.3) postoperatively. Notably, this cohort showed a much lower decrease of postoperative AHI than reported by the STAR trial and UP/TJU cohort.33
Stimulation vs Sham Trial
This multicenter, double-blinded, randomized, crossover trial assessed the effect of HGNS (stim) vs sham stimulation (sham) in 86 patients that completed both phases of the trial. Primary outcomes included AHI and ESS. Secondary outcomes included FOSQ. No carryover effect was found during the crossover phase. The difference between the phases was−15.5 (95% CI, −18.3 to −12.8) for AHI and −3.3 (95% CI, −4.4 to −2.2) for ESS.34
Comparator
The comparator study used propensity score matching to compare outcomes of HGNS and PAP therapy. Primary outcomes included sleepiness, AHI, and effectiveness with outcome measures of AHI and ESS collected at baseline and 12 months postimplantation. The article reported that 126 of 227 patients were matched 1:1. Both groups showed improvement in AHI and ESS. Mean (SD) AHI for the HGNS group at baseline started at 33.9 (15.1) and decreased to 8.1 (6.3). Mean (SD) ESS for the HGNS group at baseline was 15.4 (3.5) and decreased to 7.5 (4.7). In the PAP comparator group, mean (SD) baseline AHI was 36.8 (21.6) and at follow-up was 6.6 (8.0) and mean (SD) ESS was 14.6 (3.9) at baseline and 10.8 (5.6) at follow-up.35
DISCUSSION
The current clinical data on HGNS suggest that this treatment is effective in adults with moderate-to-severe OSA and effects are sustained at long-term follow-up, as measured by AHI reduction and improvements in sleep related symptoms and quality of life (Table 2). These results have been consistent across several sites.
The STAR trial included a randomized control withdrawal group, for whom HGNS treatment was withdrawn after the 12-month follow-up, and then restored at 18 months.21 This revealed that withdrawal of HGNS treatment resulted in deterioration of both objective and subjective measures of OSA and sleepiness. The beneficial effects of HGNS were restored when treatment was resumed.24 Additionally, the RCCT revealed that therapeutic stimulation via HGNS significantly reduced subjective and objective measures of OSA.34 These studies provide definitive evidence of HGNS efficacy.
Currently, a diagnosis of OSA on PAP is classified as a 50% military disability rating. This rating is based primarily on epidemiologic evidence that untreated OSA is a costly disease that leads to other chronic illnesses that increases health care utilization.9 HGNS requires an initially invasive procedure and higher upfront costs, but it could result in reduced health care use and long-term costs because of improved adherence to treatment—compared with CPAP—that results in better outcomes.
Limitations to OSA Studies
The reviewed studies have several limitations that warrant caution when determining the possible benefits of HGNS treatment. The primary limitation is the lack of active control groups, therefore precluding a direct comparison of the short- and long-term effectiveness of HGNS vs other treatments (eg, CPAP). This is especially problematic because in the reviewed studies HGNS treatment efficacy is reported as a function of the mean—and SD—percent reduction in the AHI, whereas the efficacy of CPAP treatment usually is defined in terms of “adequacy of titration” as suggested by the AASM.36 It has been reported that with CPAP treatment, 50% to 60% of OSA patients achieve AASM-defined optimal improvement of respiratory disturbance index of < 5/hour during a polysomnographic sleep recording of ≥ 15 minutes duration that includes REM sleep in the supine position.37 In most of the reviewed studies, treatment success was more liberally defined as a decrease of AHI by ≥ 50%, regardless of the resulting AHI. It is notable that among the reviewed HGNS studies, the TJU and UP cohorts achieved the best outcome in short-term follow-up of 2 months with a mean (SD) AHI of 6.3 (11.5) and 6.4 (6.1), respectively. Among those cohortsassessed at a 12-month follow-up, the Munich cohort achieved the best outcome with a mean (SD) AHI of 7.1 (5.9).
Although the metrics reported in the reviewed studies are not directly comparable, the reported findings strongly suggest that HGNS generally is less effective than CPAP. How important are these differences? With findings that HGNS “reliably produces clinically meaningful (positive) effects on daytime sleepiness, daytime functioning, and sleep quality,” does it really matter if the outcome metrics for HGNS are a little less positive than those produced by CPAP?38 For individual military OSA patients the answer is yes. This is because in military operational environments—especially during deployment—sleep restriction is nearly ubiquitous, therefore any mild residual deficits in sleep quality and daytime alertness resulting from nominally adequate, but suboptimal OSA treatment, could be exacerbated by sleep restriction, therefore placing the service member and the mission at increased risk.39
Another limitation is the narrow inclusion criteria these studies employed, which limits the generalizability of the findings. Participants in the reviewed clinical trials were selected from a patient population that was mostly middle-aged, White, and obese or overweight. In a Medical Surveillance Monthly Report study, OSA was found to be highest among service members aged > 40 years, male, obese, and Black/non-Hispanic (although it should be noted that more than one-half of enlisted service members aged ≤ 25 years).40,41 Obesity has been noted as a growing concern for the military as the military population is beginning to mirror the civilian population in terms of being overweight or obese despite height and weight standards. HGNS might not be as successful in military populations with different demographics. Moreover, HGNS has been shown to have greater AHI reduction among those with higher BMI.30 Although obese service members have a 6-fold higher 12-year incidence rate of OSA than service members without obesity, this nevertheless suggests that general level of HGNS efficacy might be lower among the military patient population, because obesity is less prevalent in the military than the general population.9
Ethnicity has been found to be a relevant factor, with the highest incidence rate of OSA among non-Hispanic Black males, a demographic that was underrepresented in cohorts included in this review. Further studies will be needed to determine the extent to which findings from HGNS treatment studies are generalizable to the broader OSA patient population.
HGNS Implementation Challenges
Current impediments to widespread use of HGNS as an OSA treatment include no standardized guidance for titration and follow-on care, which varies based on the resources available. Titrating a new device for HGNS requires experienced sleep technicians who have close relationships with device representatives and can troubleshoot problems. Technical expertise, which currently is rare, is required if there are complications after placement or if adjustments to voltage settings are needed over time. In addition, patients may require multiple specialists making it easy to get lost to follow-up after implantation. This is particularly challenging in a transient community, such as the military, because there is no guarantee that a service member will have access to the same specialty care at the next duty station.
Although some evidence suggests that HGNS is a viable alternative treatment for some patients with OSA, the generalizability of these findings to the military patient population is unclear. Specialized facilities and expertise are needed for the surgical procedure and follow-up requirements, which currently constitute significant logistical constraints. As with any implantable device, there is a risk of complications including infection that could result in medical evacuation from a theater of operations. If the device malfunctions or loses effectiveness in a deployed environment, the service member might not have immediate access to medical support, potentially leading to undertreatment of OSA. In future battlefield scenarios in multidomain operations, prolonged, far-forward field care will become the new normal because the military is not expected to have air superiority or the ability to quickly evacuate service members to a higher level of medical care.42
In deployed environments, the potential limitations of HGNS become increasingly risky for the service member and the overall mission. Considering these factors, it will be important to evaluate the practicality of HGNS as a treatment option in military populations. Military-specific challenges associated with HGNS that require further study, include guidance for patient selection outside academic centers, guidance on long-term postsurgical care and device maintenance, duty limitation and military retention considerations, and limitations in training and combat environments. The military medical community needs to conduct its own studies in appropriately selected service members to guide clinical practice.
CONCLUSIONS
HGNS treatment results in improvement of both AHI and ESS scores and could be a deployable treatment option for military patients with OSA. However, HGNS has not been found to be as effective as CPAP, although the current literature is limited by small sample sizes, homogeneous populations that do not reflect the demographics of the military, and mostly short follow-up periods. Future studies should be focused on collecting data on HGNS from demographic groups that are more representative of the military OSA patient population and identifying the subpopulation of patients who derive the greatest benefit from HGNS, so that this treatment can be better individually targeted. Until data on existing military patients is published, it is not possible to fully weigh risks and benefits in this population and generalize civilian guidance to the military.
1. Cumpston E, Chen P. Sleep Apnea Syndrome. PubMed. Updated September 4, 2023. Published January 2024. https://www.ncbi.nlm.nih.gov/books/NBK564431/
2. American Academy of Sleep Medicine. Obstructive sleep apnea. Accessed November 27, 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf
3. Cowen J, Harrison S, Thom L, et al. Use of historical remote monitoring data to determine predictors of CPAP non-compliance in patients with Osa. Sleep Breath. 2023;27(5):1899-1908. doi:10.1007/s11325-023-02806-3
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi:10.1093/aje/kws342
5. Stiegmann RA, Payne CB, Kiel MA, Stahlman SL. Increased Prevalence of Overweight and Obesity and Incidence of Prediabetes and Type 2 Diabetes During the COVID-19 Pandemic, Active Component Service Members, U.S. Armed Forces, 2018 to 2021. MSMR. 2023;30(1):11-18. Published 2023 Jan 20.
6. Adult obesity facts. Centers for Disease Control and Prevention. Updated May 17, 2022. Accessed November 27, 2023. https://www.cdc.gov/obesity/data/adult.html
7. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
8. Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. doi:10.1093/sleep/zsz112
9. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
10. Veterans Affairs 38 C.F.R. § 4.97-13, Code 6847.
11. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323-335. doi:10.1007/s11325-010-0391-y
12. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178. doi:10.1513/pats.200708-119mg
13. Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435. doi:10.1378/chest.121.2.430
14. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Obstruction nasale et compliance à la ventilation nasale à pression positive [Nasal obstruction and compliance to nasal positive airway pressure]. Ann Otolaryngol Chir Cervicofac. 2003;120(3):161-166.
15. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13-18.
16. Suurna MV, Jacobowitz O, Chang J, et al. Improving outcomes of hypoglossal nerve stimulation therapy: current practice, future directions, and research gaps. Proceedings of the 2019 International Sleep Surgery Society Research Forum. J Clin Sleep Med. 2021;17(12):2477-2487. doi:10.5664/jcsm.9542
17. Inspire Medical Systems, Inc. Announces FDA approval for apnea hypopnea index indication expansion and increased body mass index labeling. Inspire Medical Systems, Inc. Accessed July 14, 2023. https://investors.inspiresleep.com/investors/press-releases/press-release-details/2023/Inspire-Medical-Systems-Inc.-Announces-FDA-Approval-for-Apnea-Hypopnea-Index-Indication-Expansion-and-Increased-Body-Mass-Index-Labeling/default.aspx
18. Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: Validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(08):1293-1301. Published 2018 Aug 15. doi:10.5664/jcsm.7258
19. The Centre for Evidence-Based Medicine. November 25, 2020. http://www.cebm.net/index.aspx?o=5653
20. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
21. Strollo PJ Jr, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38(10):1593-1598. Published 2015 Oct 1. doi:10.5665/sleep.5054
22. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181-188. doi:10.1177/0194599815616618
23. Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194-202. doi:10.1177/0194599818762383
24. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg. 2014;151(5):880-887. doi:10.1177/0194599814544445
25. Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg. 2017;156(2):378-384. doi:10.1177/0194599816683378
26. Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509-515. doi:10.1002/lary.26688
27. Steffen A, Sommer UJ, Maurer JT, Abrams N, Hofauer B, Heiser C. Long-term follow-up of the German post-market study for upper airway stimulation for obstructive sleep apnea. Sleep Breath. 2020;24(3):979-984. doi:10.1007/s11325-019-01933-028.
28. Hasselbacher K, Hofauer B, Maurer JT, Heiser C, Steffen A, Sommer JU. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol. 2018;275(7):1913-1919. doi:10.1007/s00405-018-5017-129.
29. Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727-1734. doi:10.1007/s00405-016-4297-6
30. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res. 2014;23(1):77-83. doi:10.1111/jsr.12079
31. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med. 2016;12(1):43-48. doi:10.5664/jcsm.5390
32. Huntley C, Kaffenberger T, Doghramji K, Soose R, Boon M. Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med. 2017;13(9):1075-1079. Published 2017 Sep 15. doi:10.5664/jcsm.6726

33. Pordzik J, Seifen C, Ludwig K, et al. Short-term outcome of unilateral inspiration-coupled hypoglossal nerve stimulation in patients with obstructive sleep apnea. Int J Environ Res Public Health. 2022;19(24):16443. Published 2022 Dec 8. doi:10.3390/ijerph192416443
34. Heiser C, Steffen A, Hofauer B, et al. Effect of upper airway stimulation in patients with obstructive sleep apnea (EFFECT): a randomized controlled crossover trial. J Clin Med. 2021;10(13):2880. Published 2021 Jun 29. doi:10.3390/jcm1013288035.
35. Heiser C, Steffen A, Strollo PJ Jr, Giaie-Miniet C, Vanderveken OM, Hofauer B. Hypoglossal nerve stimulation versus positive airway pressure therapy for obstructive sleep apnea. Sleep Breath. 2023;27(2):693-701. doi:10.1007/s11325-022-02663-6
36. Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157-171.
37. Freedman N, Johnson K. Positive airway pressure treatment for obstructive sleep apnea. In: Kryger MH, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. Elsevier; 2022:1260-1283.
38. Braun M, Stoerzel M, Wollny M, Schoebel C, Ulrich Sommer J, Heiser C. Patient-reported outcomes with hypoglossal nerve stimulation for treatment of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280(10):4627-4639. doi:10.1007/s00405-023-08062-1
39. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. doi:10.5665/SLEEP.1236
40. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
41. Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2017 Demographics: Profile of the Military Community. US Dept of Defense;2017. Accessed April 4, 2024. http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf
42. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2S Suppl 1): S180-S184. doi:10.1097/TA.0000000000004063
Obstructive sleep apnea (OSA), the repetitive collapse of posterior oropharynx during sleep resulting in hypoxia and/or arousals from sleep, is the most common form of sleep disordered breathing and a common chronic respiratory disorders among middle-aged adults. OSA can lead to significant health problems, such as worsened cardiometabolic disease and cognitive impairment, which can increase morbidity and mortality.1
The gold standard for OSA diagnosis is polysomnography (PSG), although home sleep studies can be performed for select patients. OSA diagnoses are based on the number of times per hour of sleep a patient’s airway narrows or collapses, reducing or stopping airflow, scored as hypopnea or apnea events, respectively. An Apnea-Hypopnea Index (AHI) score of 5 to 14 events/hour is considered mild OSA, 15 to 30 events/hour moderate OSA, and ≥ 30 events/hour severe OSA.2
Treatment commonly includes positive airway pressure (PAP) but more than one-half of patients are not adherent to continuous PAP (CPAP) treatment after about 90 days.3 Efficacy of treatments vary as a function of disease severity and etiology, which—in addition to the classic presentation of obesity with large neck/narrowupper airway—includes craniofacial abnormalities, altered muscle function in the upper airway, pharyngeal neuropathy, and fluid shifts to the neck.
Background
The American Academy of Sleep Medicine (AASM) estimates that 10% to 17% of adults in the United States have OSA.4 Compared with civilians, the military population generally is younger and healthier. Service members have access to regular health care with yearly physical examinations, exercise scheduled into the workday, and mandatory height/weight and fitness standards. Because obesity is a major risk factor for OSA, and the incidence of obesity is relatively low in the military population (estimated at 18.8% in 2021 vs 39.8% among all US adults aged 20 to 39 years), it might be expected that incidence of OSA would be correspondingly low.5,6 However, there is evidence of a rapidly increasing incidence of OSA in military populations. A 2021 study revealed that OSA incidence rates increased from 11 to 333 per 10,000 between 2005 and 2019 across all military branches and demographics, with the highest rate among Army personnel.7 An earlier study revealed a 600% increase in OSA incidence among Army personnel between 2003 and 2011.8
Several factors likely contributed to this increase, including expanding obesity and greater physician awareness and availability of sleep study centers. Rogers and colleagues found that 40% to 50% of incident OSA diagnoses among military personnel occur within 12 months of separation, suggesting that the secondary gains associated with military disability benefits might motivate OSA evaluation.9 It is possible that secondary gain is a factor because an OSA diagnosis can range from a 0% to 100% disability rating, depending on the severity.10 This disability claim is based on evidence that untreated OSA can negatively affect long-term health and mission readiness.8 For example, untreated OSA can lead to hypertension, which contributes to a long list of adverse health and wellness consequences. Most importantly for the military, OSA has been shown to increase daytime sleepiness and reduce cognitive performance.10
The current first-line treatment for OSA is CPAP, which improves symptoms of daytime sleepiness, hypertension management, and daytime alertness.11 Despite its efficacy, nonadherence rates range from 29% to 83%.12-15 Nonadherence factors include lifestyle changes, adverse effects (eg, nasal congestion), and lack of education on proper use.11 Lifestyle changes needed to increase the likelihood of successful therapy, such as regular sleep schedules and proper CPAP cleaning and maintenance, are difficult for military personnel because of the nature of continuous or sustained operations that might require shift work and/or around-the-clock (ie, 24-hour, 7 days a week) task performance. Traveling with CPAP is an added burden for service members deployed to combat operations (ie, added luggage, weight, maintenance). Although alternate treatments such as oral appliances (ie, custom dental devices) are available, they generally are less effective than CPAP.2 Oral appliances could be a reasonable alternative treatment for some patients who cannot manage their OSA with behavioral modifications and are intolerant or unable to effectively use CPAP. This could include patients in the military who are deployed to austere environments.
Surgically implanted hypoglossal nerve stimulator (HGNS) treatment may provide long-term health benefits to service members. After the device is implanted near the hypoglossal nerve, electrical stimulation causes the tongue to move forward, which opens the airway in the anteroposterior dimension. The most important consideration is the mechanism of airway collapse. HGNS is not effective for patients whose OSA events are caused by circumferential collapse of other airway muscles. The cause of airway collapse is ascertained before surgery with drug-induced sleep endoscopy, a procedure that allows visualization of conformational changes in the upper airway during OSA events.
The US Food and Drug Administration (FDA) approved HGNS in 2014. However, it is not considered a first-line treatment for OSA by the AASM. Original candidate criteria for HGNS included an AHI score of 15 to 65 events/hour, age ≥ 18 years, failed CPAP use, body mass index (BMI) < 32, absence of palatal complete concentric collapse, and central apneas comprising < 25% of total events.16 In June 2023, the FDA expanded approval to increase the upper limit of AHI to 100 events/hour and the BMI to < 40.17
HGNS has been reported to be effective in appropriately selected patients with OSA at tertiary care centers with established multidisciplinary sleep surgical programs. These benefits have not been confirmed in larger, community-based settings, where most of these surgeries occur. In community practice, there is significant confusion among patients and clinicians about the optimal pathway for patient selection and clinical follow-up. Many patients view HGNS as a viable alternative to CPAP, but initially do not understand that it requires surgery. Surgical treatments for OSA, such as HGNS, are appealing because they suggest a 1-time intervention that permanently treats the condition, without need for follow-up or equipment resupply. HGNS might be an appealing treatment option because it is less obtrusive than CPAP and requires fewer resources for set-up and maintenance. Also, it does not cause skin irritation (a possible adverse effect of nightly use of a CPAP mask), allows the individual to sleep in a variety of positions, has less impact on social and sex life, and does not require an electric outlet. In the long term, HGNS might be more cost effective because there is no yearly physician follow-up or equipment resupply and/or maintenance.
The military population has specific demands that impact delivery and effectiveness of health care. Among service members with OSA, CPAP treatment can be challenging because of low adherence, required annual follow-up despite frequent moving cycles that pose a challenge for care continuity, and duty limitations for affected service members (ie, the requirement for a waiver to deploy and potential medical separation if symptoms are not adequately controlled). As the incidence of OSA continues to increase among service members, so does the need for OSA treatment options that are efficacious as CPAP but better tolerated and more suitable for use during military operations. The aim of this review is to assess the effectiveness of HGNS and its potential use by the military OSA patient population.
METHODS
To identify eligible studies, we employed PICOS: Population (patients aged ≥ 18 years with a history of OSA), Intervention (HGNS), Comparator (standard of care PAP therapy), Outcome (AHI or Epworth Sleepiness Scale [ESS], and Study (randomized control trial [RCT] or clinical trial). Studies were excluded if they were not written in English or included pediatric populations. The ESS is a subjective rating scale used to determine and quantify a patient’s level of daytime sleepiness, using a 4-point scale for the likelihood of falling asleep totaled across 8 different situations.18 Daytime sleepiness is considered lower normal(0-5 points), higher normal (6-10 points), mild or moderate excessive (11-15 points), and severe excessive (16-24 points).
Literature Search
We conducted a review of PubMed and Scopus for RCTs and controlled trials published from 2013 to 2023 that included the keywords and phrases: obstructive sleep apnea and either hypoglossal nerve stimulation or upper airway stimulation. The final literature search was performed December 8, 2023.
Two authors independently assessed the titles and abstracts of studies identified in the literature search based on the predefined inclusion criteria. If it was not clear whether an article met inclusion criteria based on its title and/or abstract, the 2 review authors assessed the full text of study and resolved any disagreement through consensus. If consensus was not obtained, a third author was consulted. No duplicates were identified. The PRISMA study selection process is presented in the Figure.
Data extraction was performed by 1 independent reviewer. A second author reviewed the extracted data. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third author was consulted. Study data included methods (study design and study objective), participants mean age, inclusion criteria, exclusion criteria, interventions and comparators, and primary study outcomes.
The quality of evidence was assessed using a rating of 1 to 5 based on a modified version of the Oxford Centre for Evidence-based Medicine Levels of Evidence and Grades of Recommendation.19 A rating of 1 indicated a properly powered and conducted RCT, 2 demonstrated a well-designed controlled trial without randomization or prospective comparative cohort trial, 3 designated a case-control study or retrospective cohort study, 4 signified a case series with or without intervention or a cross-sectional study, and 5 denoted an opinion of respected authorities or case reports. Two reviewers independently evaluated the quality of evidence. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third review author was consulted.
RESULTS
We identified 30 studies; 19 articles did not meet inclusion criteria. The remaining 11 articles were divided into 4 cohorts. Five articles were based on data from the STAR trial, a multicenter study that included adults with moderate-to-severe OSA and inadequate adherence to CPAP.20-24 Four articles used the same patient selection criteria as the STAR trial for a long-term German postmarket study of upper airway stimulation efficacy with OSA.25-28 The third and fourth cohorts each consist of 31 patients with moderate-to-severe OSA with CPAP nonadherence or failure.29,30 The STAR trial included follow-up at 5 years, and the German-postmarket had a follow-up at3 years. The remaining 2 cohorts have 1-year follow-ups.
The Scopus review identified 304 studies; 299 did not meet inclusion criteria and 1 was part of the STAR trial.31 The remaining 4 articles were classified as distinct cohorts. Huntley and colleagues included patients from Thomas Jefferson University (TJU) and University of Pittsburgh (UP) academic medical centers.32 The Pordzik and colleagues cohort received implantation at a tertiary medical center, an RCCT, and a 1:1 comparator trial (Table 1).33-35
STAR Trial
This multicenter, prospective, single-group cohort study was conducted in the US, Germany, Belgium, Netherlands, and France. The STAR trial included 126 patients who were not CPAP therapy adherent. Patients were excluded if they had AHI < 20 or > 50, central sleep apnea > 25% of total AHI, anatomical abnormalities that prevent effective assessment of upper-airway stimulation, complete concentric collapse of the retropalatal airway during drug-induced sleep, neuromuscular disease, hypoglossal-nerve palsy, severe restrictive or obstructive pulmonary disease, moderate-to-severe pulmonary arterial hypertension, severe valvular heart disease, New York Heart Association class III or IV heart failure, recent myocardial infarction or severe cardiac arrhythmias (within the past 6 months), persistent uncontrolled hypertension despite medication use, active psychiatric illness, or coexisting nonrespiratory sleep disorders that would confound functional sleep assessment. Primary outcome measures included the AHI and oxygen desaturation index (ODI) with secondary outcomes using the ESS, the Functional Outcomes of Sleep Questionnaire (FOSQ), and the percentage of sleep time with oxygen saturation < 90%. Of 126 patients who received implantation, 71 underwent an overnight PSG evaluation at 5-year follow-up. Mean (SD) AHI at baseline was reduced with HGNS treatment to from 32.0 (11.8) to 12.4 (16.3). Mean (SD) ESS for 92 participants with 2 measurements declined from 11.6 (5.0) at baseline to 6.9 (4.7) at 5-year follow-up.
The STAR trial included a randomized controlled withdrawal study for 46 patients who had a positive response to therapy to evaluate efficacy and durability of upper airway stimulation. Patients were randomly assigned to therapy maintenance or therapy withdrawal groups for ≥ 1 week. The short-term withdrawal effect was assessed using the original trial outcome measures and indicated that both the withdrawal and maintenance groups showed improvements at 12 months compared with the baseline. However, after the randomized withdrawal, the withdrawal group’s outcome measures deteriorated to baseline levels while the maintenance group showed no change. At 18 months of therapy, outcome measures for both groups were similar to those observed with therapy at 12 months.24 The STAR trial included self-reported outcomes at baseline, 12 months, and 24 months that used ESS to measure daytime sleepiness. These results included subsequent STAR trial reports.20-24,31
The German Postmarket Cohort
This multicenter, prospective, single-arm study used selection criteria that were based on those used in the STAR trial and included patients with moderate-to-severe OSA and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, AHI < 15 or > 65; central apnea index > 25% of total AHI; or complete concentric collapse at the velopharynx during drug-induced sleep. Measured outcomes included AHI, ODI, FOSQ, and ESS. Among the 60 participants, 38 received implantation and a 3-year follow-up. Mean (SD) AHI decreased from 31.2 (13.2) at baseline to 13.1 (14.1) at follow-up, while mean (SD) ESS decreased from 12.8 (5.3) at baseline to 6.0 (3.2) at follow-up.25-28
Munich Cohort
This single-center, prospective clinical trial included patients with AHI > 15 and < 65, central apnea index < 25% of total AHI, and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, anatomical abnormalities that would prevent effective assessment of upper-airway stimulation; all other exclusion criteria matched those used in the STAR trial. Among 31 patients who received implants and completed a 1-year follow-up, mean (SD) AHI decreased from 32.9 (11.2) at baseline to 7.1 (5.9) at follow-up and mean (SD) ESS decreased from 12.6 (5.6) at baseline to 5.9 (5.2) at follow-up.29
Kezirian and Colleagues Cohort
This prospective, single-arm, open-label study was conducted at 4 Australian and 4 US sites. Selection criteria included moderate-to-severe OSA with failure of CPAP, AHI of 20 to 100 with ≥ 15 events/hour occurring in sleep that was non-REM (rapid eye movement) sleep, BMI ≤ 40 (Australia) or ≤ 37 (US), and a predominance of hypopneas (≥ 80% of disordered breathing events during sleep). Patients were excluded if they had earlier upper airway surgery, markedly enlarged tonsils, uncontrolled nasal obstruction, severe retrognathia, > 5% central or mixed apneic events, incompletely treated sleep disorders other than OSA, or a major disorder of the pulmonary, cardiac, renal, or nervous systems. Data were reported for 31 patients whose mean (SD) AHI declined from 45.4 (17.5) at baseline to 25.3 (20.6) at 1-year follow-up and mean (SD) ESS score declined from 12.1 (4.6) at baseline to 7.9 (3.8) 1 year later.30
TJU and UP Cohorts
The TJU and UP cohorts are composed of patients who underwent implantation between May 2014 and August 2016 at 2 academic centers.31,32 Selection criteria was consistent with that used in the STAR trial, and patients completed postoperative titration PSG and outpatient follow-up (48 patients at TJU and 49 at UP). Primary outcomes included AHI, ESS, and O2 nadir. Secondary outcomes consisted of surgical success and percentage of patients tolerating optimal titration setting at follow-up. Postoperative outcomes were assessed during the titration PSG. Time from initial ESS to postoperative PSG at TJU was 1.7 years and at UP was 1.9 years. Time from initial AHI to postoperative PSG at TJU was 90.4 days and 85.2 days at UP. At TJU, mean (SD) AHI and ESS dropped from 35.9 (20.8) and 11.1 (3.8), respectively at baseline to 6.3 (11.5) and 5.8 (3.4), respectively at follow-up. At UP, mean (SD) AHI and ESS fell from 35.3 (15.3) and 10.9 (4.9), respectively at baseline to 6.3 (6.1) and 6.6 (4.5), respectively at follow-up. There were no site-related differences in rates of AHI, ESS, or surgical success.31
Pordzik and Colleagues Cohort
This cohort of 29 patients underwent implantation between February 2020 and June 2022 at a tertiary university medical center with both pre- and postoperative PSG. Selection criteria was consistent with that of the German postmarket cohort. Postoperative PSG was completed a mean (SD) 96.3 (27.0) days after device activation. Mean (SD) AHI dropped from 38.6 (12.7) preoperatively to 24.4 (13.3) postoperatively. Notably, this cohort showed a much lower decrease of postoperative AHI than reported by the STAR trial and UP/TJU cohort.33
Stimulation vs Sham Trial
This multicenter, double-blinded, randomized, crossover trial assessed the effect of HGNS (stim) vs sham stimulation (sham) in 86 patients that completed both phases of the trial. Primary outcomes included AHI and ESS. Secondary outcomes included FOSQ. No carryover effect was found during the crossover phase. The difference between the phases was−15.5 (95% CI, −18.3 to −12.8) for AHI and −3.3 (95% CI, −4.4 to −2.2) for ESS.34
Comparator
The comparator study used propensity score matching to compare outcomes of HGNS and PAP therapy. Primary outcomes included sleepiness, AHI, and effectiveness with outcome measures of AHI and ESS collected at baseline and 12 months postimplantation. The article reported that 126 of 227 patients were matched 1:1. Both groups showed improvement in AHI and ESS. Mean (SD) AHI for the HGNS group at baseline started at 33.9 (15.1) and decreased to 8.1 (6.3). Mean (SD) ESS for the HGNS group at baseline was 15.4 (3.5) and decreased to 7.5 (4.7). In the PAP comparator group, mean (SD) baseline AHI was 36.8 (21.6) and at follow-up was 6.6 (8.0) and mean (SD) ESS was 14.6 (3.9) at baseline and 10.8 (5.6) at follow-up.35
DISCUSSION
The current clinical data on HGNS suggest that this treatment is effective in adults with moderate-to-severe OSA and effects are sustained at long-term follow-up, as measured by AHI reduction and improvements in sleep related symptoms and quality of life (Table 2). These results have been consistent across several sites.
The STAR trial included a randomized control withdrawal group, for whom HGNS treatment was withdrawn after the 12-month follow-up, and then restored at 18 months.21 This revealed that withdrawal of HGNS treatment resulted in deterioration of both objective and subjective measures of OSA and sleepiness. The beneficial effects of HGNS were restored when treatment was resumed.24 Additionally, the RCCT revealed that therapeutic stimulation via HGNS significantly reduced subjective and objective measures of OSA.34 These studies provide definitive evidence of HGNS efficacy.
Currently, a diagnosis of OSA on PAP is classified as a 50% military disability rating. This rating is based primarily on epidemiologic evidence that untreated OSA is a costly disease that leads to other chronic illnesses that increases health care utilization.9 HGNS requires an initially invasive procedure and higher upfront costs, but it could result in reduced health care use and long-term costs because of improved adherence to treatment—compared with CPAP—that results in better outcomes.
Limitations to OSA Studies
The reviewed studies have several limitations that warrant caution when determining the possible benefits of HGNS treatment. The primary limitation is the lack of active control groups, therefore precluding a direct comparison of the short- and long-term effectiveness of HGNS vs other treatments (eg, CPAP). This is especially problematic because in the reviewed studies HGNS treatment efficacy is reported as a function of the mean—and SD—percent reduction in the AHI, whereas the efficacy of CPAP treatment usually is defined in terms of “adequacy of titration” as suggested by the AASM.36 It has been reported that with CPAP treatment, 50% to 60% of OSA patients achieve AASM-defined optimal improvement of respiratory disturbance index of < 5/hour during a polysomnographic sleep recording of ≥ 15 minutes duration that includes REM sleep in the supine position.37 In most of the reviewed studies, treatment success was more liberally defined as a decrease of AHI by ≥ 50%, regardless of the resulting AHI. It is notable that among the reviewed HGNS studies, the TJU and UP cohorts achieved the best outcome in short-term follow-up of 2 months with a mean (SD) AHI of 6.3 (11.5) and 6.4 (6.1), respectively. Among those cohortsassessed at a 12-month follow-up, the Munich cohort achieved the best outcome with a mean (SD) AHI of 7.1 (5.9).
Although the metrics reported in the reviewed studies are not directly comparable, the reported findings strongly suggest that HGNS generally is less effective than CPAP. How important are these differences? With findings that HGNS “reliably produces clinically meaningful (positive) effects on daytime sleepiness, daytime functioning, and sleep quality,” does it really matter if the outcome metrics for HGNS are a little less positive than those produced by CPAP?38 For individual military OSA patients the answer is yes. This is because in military operational environments—especially during deployment—sleep restriction is nearly ubiquitous, therefore any mild residual deficits in sleep quality and daytime alertness resulting from nominally adequate, but suboptimal OSA treatment, could be exacerbated by sleep restriction, therefore placing the service member and the mission at increased risk.39
Another limitation is the narrow inclusion criteria these studies employed, which limits the generalizability of the findings. Participants in the reviewed clinical trials were selected from a patient population that was mostly middle-aged, White, and obese or overweight. In a Medical Surveillance Monthly Report study, OSA was found to be highest among service members aged > 40 years, male, obese, and Black/non-Hispanic (although it should be noted that more than one-half of enlisted service members aged ≤ 25 years).40,41 Obesity has been noted as a growing concern for the military as the military population is beginning to mirror the civilian population in terms of being overweight or obese despite height and weight standards. HGNS might not be as successful in military populations with different demographics. Moreover, HGNS has been shown to have greater AHI reduction among those with higher BMI.30 Although obese service members have a 6-fold higher 12-year incidence rate of OSA than service members without obesity, this nevertheless suggests that general level of HGNS efficacy might be lower among the military patient population, because obesity is less prevalent in the military than the general population.9
Ethnicity has been found to be a relevant factor, with the highest incidence rate of OSA among non-Hispanic Black males, a demographic that was underrepresented in cohorts included in this review. Further studies will be needed to determine the extent to which findings from HGNS treatment studies are generalizable to the broader OSA patient population.
HGNS Implementation Challenges
Current impediments to widespread use of HGNS as an OSA treatment include no standardized guidance for titration and follow-on care, which varies based on the resources available. Titrating a new device for HGNS requires experienced sleep technicians who have close relationships with device representatives and can troubleshoot problems. Technical expertise, which currently is rare, is required if there are complications after placement or if adjustments to voltage settings are needed over time. In addition, patients may require multiple specialists making it easy to get lost to follow-up after implantation. This is particularly challenging in a transient community, such as the military, because there is no guarantee that a service member will have access to the same specialty care at the next duty station.
Although some evidence suggests that HGNS is a viable alternative treatment for some patients with OSA, the generalizability of these findings to the military patient population is unclear. Specialized facilities and expertise are needed for the surgical procedure and follow-up requirements, which currently constitute significant logistical constraints. As with any implantable device, there is a risk of complications including infection that could result in medical evacuation from a theater of operations. If the device malfunctions or loses effectiveness in a deployed environment, the service member might not have immediate access to medical support, potentially leading to undertreatment of OSA. In future battlefield scenarios in multidomain operations, prolonged, far-forward field care will become the new normal because the military is not expected to have air superiority or the ability to quickly evacuate service members to a higher level of medical care.42
In deployed environments, the potential limitations of HGNS become increasingly risky for the service member and the overall mission. Considering these factors, it will be important to evaluate the practicality of HGNS as a treatment option in military populations. Military-specific challenges associated with HGNS that require further study, include guidance for patient selection outside academic centers, guidance on long-term postsurgical care and device maintenance, duty limitation and military retention considerations, and limitations in training and combat environments. The military medical community needs to conduct its own studies in appropriately selected service members to guide clinical practice.
CONCLUSIONS
HGNS treatment results in improvement of both AHI and ESS scores and could be a deployable treatment option for military patients with OSA. However, HGNS has not been found to be as effective as CPAP, although the current literature is limited by small sample sizes, homogeneous populations that do not reflect the demographics of the military, and mostly short follow-up periods. Future studies should be focused on collecting data on HGNS from demographic groups that are more representative of the military OSA patient population and identifying the subpopulation of patients who derive the greatest benefit from HGNS, so that this treatment can be better individually targeted. Until data on existing military patients is published, it is not possible to fully weigh risks and benefits in this population and generalize civilian guidance to the military.
Obstructive sleep apnea (OSA), the repetitive collapse of posterior oropharynx during sleep resulting in hypoxia and/or arousals from sleep, is the most common form of sleep disordered breathing and a common chronic respiratory disorders among middle-aged adults. OSA can lead to significant health problems, such as worsened cardiometabolic disease and cognitive impairment, which can increase morbidity and mortality.1
The gold standard for OSA diagnosis is polysomnography (PSG), although home sleep studies can be performed for select patients. OSA diagnoses are based on the number of times per hour of sleep a patient’s airway narrows or collapses, reducing or stopping airflow, scored as hypopnea or apnea events, respectively. An Apnea-Hypopnea Index (AHI) score of 5 to 14 events/hour is considered mild OSA, 15 to 30 events/hour moderate OSA, and ≥ 30 events/hour severe OSA.2
Treatment commonly includes positive airway pressure (PAP) but more than one-half of patients are not adherent to continuous PAP (CPAP) treatment after about 90 days.3 Efficacy of treatments vary as a function of disease severity and etiology, which—in addition to the classic presentation of obesity with large neck/narrowupper airway—includes craniofacial abnormalities, altered muscle function in the upper airway, pharyngeal neuropathy, and fluid shifts to the neck.
Background
The American Academy of Sleep Medicine (AASM) estimates that 10% to 17% of adults in the United States have OSA.4 Compared with civilians, the military population generally is younger and healthier. Service members have access to regular health care with yearly physical examinations, exercise scheduled into the workday, and mandatory height/weight and fitness standards. Because obesity is a major risk factor for OSA, and the incidence of obesity is relatively low in the military population (estimated at 18.8% in 2021 vs 39.8% among all US adults aged 20 to 39 years), it might be expected that incidence of OSA would be correspondingly low.5,6 However, there is evidence of a rapidly increasing incidence of OSA in military populations. A 2021 study revealed that OSA incidence rates increased from 11 to 333 per 10,000 between 2005 and 2019 across all military branches and demographics, with the highest rate among Army personnel.7 An earlier study revealed a 600% increase in OSA incidence among Army personnel between 2003 and 2011.8
Several factors likely contributed to this increase, including expanding obesity and greater physician awareness and availability of sleep study centers. Rogers and colleagues found that 40% to 50% of incident OSA diagnoses among military personnel occur within 12 months of separation, suggesting that the secondary gains associated with military disability benefits might motivate OSA evaluation.9 It is possible that secondary gain is a factor because an OSA diagnosis can range from a 0% to 100% disability rating, depending on the severity.10 This disability claim is based on evidence that untreated OSA can negatively affect long-term health and mission readiness.8 For example, untreated OSA can lead to hypertension, which contributes to a long list of adverse health and wellness consequences. Most importantly for the military, OSA has been shown to increase daytime sleepiness and reduce cognitive performance.10
The current first-line treatment for OSA is CPAP, which improves symptoms of daytime sleepiness, hypertension management, and daytime alertness.11 Despite its efficacy, nonadherence rates range from 29% to 83%.12-15 Nonadherence factors include lifestyle changes, adverse effects (eg, nasal congestion), and lack of education on proper use.11 Lifestyle changes needed to increase the likelihood of successful therapy, such as regular sleep schedules and proper CPAP cleaning and maintenance, are difficult for military personnel because of the nature of continuous or sustained operations that might require shift work and/or around-the-clock (ie, 24-hour, 7 days a week) task performance. Traveling with CPAP is an added burden for service members deployed to combat operations (ie, added luggage, weight, maintenance). Although alternate treatments such as oral appliances (ie, custom dental devices) are available, they generally are less effective than CPAP.2 Oral appliances could be a reasonable alternative treatment for some patients who cannot manage their OSA with behavioral modifications and are intolerant or unable to effectively use CPAP. This could include patients in the military who are deployed to austere environments.
Surgically implanted hypoglossal nerve stimulator (HGNS) treatment may provide long-term health benefits to service members. After the device is implanted near the hypoglossal nerve, electrical stimulation causes the tongue to move forward, which opens the airway in the anteroposterior dimension. The most important consideration is the mechanism of airway collapse. HGNS is not effective for patients whose OSA events are caused by circumferential collapse of other airway muscles. The cause of airway collapse is ascertained before surgery with drug-induced sleep endoscopy, a procedure that allows visualization of conformational changes in the upper airway during OSA events.
The US Food and Drug Administration (FDA) approved HGNS in 2014. However, it is not considered a first-line treatment for OSA by the AASM. Original candidate criteria for HGNS included an AHI score of 15 to 65 events/hour, age ≥ 18 years, failed CPAP use, body mass index (BMI) < 32, absence of palatal complete concentric collapse, and central apneas comprising < 25% of total events.16 In June 2023, the FDA expanded approval to increase the upper limit of AHI to 100 events/hour and the BMI to < 40.17
HGNS has been reported to be effective in appropriately selected patients with OSA at tertiary care centers with established multidisciplinary sleep surgical programs. These benefits have not been confirmed in larger, community-based settings, where most of these surgeries occur. In community practice, there is significant confusion among patients and clinicians about the optimal pathway for patient selection and clinical follow-up. Many patients view HGNS as a viable alternative to CPAP, but initially do not understand that it requires surgery. Surgical treatments for OSA, such as HGNS, are appealing because they suggest a 1-time intervention that permanently treats the condition, without need for follow-up or equipment resupply. HGNS might be an appealing treatment option because it is less obtrusive than CPAP and requires fewer resources for set-up and maintenance. Also, it does not cause skin irritation (a possible adverse effect of nightly use of a CPAP mask), allows the individual to sleep in a variety of positions, has less impact on social and sex life, and does not require an electric outlet. In the long term, HGNS might be more cost effective because there is no yearly physician follow-up or equipment resupply and/or maintenance.
The military population has specific demands that impact delivery and effectiveness of health care. Among service members with OSA, CPAP treatment can be challenging because of low adherence, required annual follow-up despite frequent moving cycles that pose a challenge for care continuity, and duty limitations for affected service members (ie, the requirement for a waiver to deploy and potential medical separation if symptoms are not adequately controlled). As the incidence of OSA continues to increase among service members, so does the need for OSA treatment options that are efficacious as CPAP but better tolerated and more suitable for use during military operations. The aim of this review is to assess the effectiveness of HGNS and its potential use by the military OSA patient population.
METHODS
To identify eligible studies, we employed PICOS: Population (patients aged ≥ 18 years with a history of OSA), Intervention (HGNS), Comparator (standard of care PAP therapy), Outcome (AHI or Epworth Sleepiness Scale [ESS], and Study (randomized control trial [RCT] or clinical trial). Studies were excluded if they were not written in English or included pediatric populations. The ESS is a subjective rating scale used to determine and quantify a patient’s level of daytime sleepiness, using a 4-point scale for the likelihood of falling asleep totaled across 8 different situations.18 Daytime sleepiness is considered lower normal(0-5 points), higher normal (6-10 points), mild or moderate excessive (11-15 points), and severe excessive (16-24 points).
Literature Search
We conducted a review of PubMed and Scopus for RCTs and controlled trials published from 2013 to 2023 that included the keywords and phrases: obstructive sleep apnea and either hypoglossal nerve stimulation or upper airway stimulation. The final literature search was performed December 8, 2023.
Two authors independently assessed the titles and abstracts of studies identified in the literature search based on the predefined inclusion criteria. If it was not clear whether an article met inclusion criteria based on its title and/or abstract, the 2 review authors assessed the full text of study and resolved any disagreement through consensus. If consensus was not obtained, a third author was consulted. No duplicates were identified. The PRISMA study selection process is presented in the Figure.
Data extraction was performed by 1 independent reviewer. A second author reviewed the extracted data. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third author was consulted. Study data included methods (study design and study objective), participants mean age, inclusion criteria, exclusion criteria, interventions and comparators, and primary study outcomes.
The quality of evidence was assessed using a rating of 1 to 5 based on a modified version of the Oxford Centre for Evidence-based Medicine Levels of Evidence and Grades of Recommendation.19 A rating of 1 indicated a properly powered and conducted RCT, 2 demonstrated a well-designed controlled trial without randomization or prospective comparative cohort trial, 3 designated a case-control study or retrospective cohort study, 4 signified a case series with or without intervention or a cross-sectional study, and 5 denoted an opinion of respected authorities or case reports. Two reviewers independently evaluated the quality of evidence. Any identified discrepancies were resolved through discussion and consensus. If consensus was not obtained, a third review author was consulted.
RESULTS
We identified 30 studies; 19 articles did not meet inclusion criteria. The remaining 11 articles were divided into 4 cohorts. Five articles were based on data from the STAR trial, a multicenter study that included adults with moderate-to-severe OSA and inadequate adherence to CPAP.20-24 Four articles used the same patient selection criteria as the STAR trial for a long-term German postmarket study of upper airway stimulation efficacy with OSA.25-28 The third and fourth cohorts each consist of 31 patients with moderate-to-severe OSA with CPAP nonadherence or failure.29,30 The STAR trial included follow-up at 5 years, and the German-postmarket had a follow-up at3 years. The remaining 2 cohorts have 1-year follow-ups.
The Scopus review identified 304 studies; 299 did not meet inclusion criteria and 1 was part of the STAR trial.31 The remaining 4 articles were classified as distinct cohorts. Huntley and colleagues included patients from Thomas Jefferson University (TJU) and University of Pittsburgh (UP) academic medical centers.32 The Pordzik and colleagues cohort received implantation at a tertiary medical center, an RCCT, and a 1:1 comparator trial (Table 1).33-35
STAR Trial
This multicenter, prospective, single-group cohort study was conducted in the US, Germany, Belgium, Netherlands, and France. The STAR trial included 126 patients who were not CPAP therapy adherent. Patients were excluded if they had AHI < 20 or > 50, central sleep apnea > 25% of total AHI, anatomical abnormalities that prevent effective assessment of upper-airway stimulation, complete concentric collapse of the retropalatal airway during drug-induced sleep, neuromuscular disease, hypoglossal-nerve palsy, severe restrictive or obstructive pulmonary disease, moderate-to-severe pulmonary arterial hypertension, severe valvular heart disease, New York Heart Association class III or IV heart failure, recent myocardial infarction or severe cardiac arrhythmias (within the past 6 months), persistent uncontrolled hypertension despite medication use, active psychiatric illness, or coexisting nonrespiratory sleep disorders that would confound functional sleep assessment. Primary outcome measures included the AHI and oxygen desaturation index (ODI) with secondary outcomes using the ESS, the Functional Outcomes of Sleep Questionnaire (FOSQ), and the percentage of sleep time with oxygen saturation < 90%. Of 126 patients who received implantation, 71 underwent an overnight PSG evaluation at 5-year follow-up. Mean (SD) AHI at baseline was reduced with HGNS treatment to from 32.0 (11.8) to 12.4 (16.3). Mean (SD) ESS for 92 participants with 2 measurements declined from 11.6 (5.0) at baseline to 6.9 (4.7) at 5-year follow-up.
The STAR trial included a randomized controlled withdrawal study for 46 patients who had a positive response to therapy to evaluate efficacy and durability of upper airway stimulation. Patients were randomly assigned to therapy maintenance or therapy withdrawal groups for ≥ 1 week. The short-term withdrawal effect was assessed using the original trial outcome measures and indicated that both the withdrawal and maintenance groups showed improvements at 12 months compared with the baseline. However, after the randomized withdrawal, the withdrawal group’s outcome measures deteriorated to baseline levels while the maintenance group showed no change. At 18 months of therapy, outcome measures for both groups were similar to those observed with therapy at 12 months.24 The STAR trial included self-reported outcomes at baseline, 12 months, and 24 months that used ESS to measure daytime sleepiness. These results included subsequent STAR trial reports.20-24,31
The German Postmarket Cohort
This multicenter, prospective, single-arm study used selection criteria that were based on those used in the STAR trial and included patients with moderate-to-severe OSA and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, AHI < 15 or > 65; central apnea index > 25% of total AHI; or complete concentric collapse at the velopharynx during drug-induced sleep. Measured outcomes included AHI, ODI, FOSQ, and ESS. Among the 60 participants, 38 received implantation and a 3-year follow-up. Mean (SD) AHI decreased from 31.2 (13.2) at baseline to 13.1 (14.1) at follow-up, while mean (SD) ESS decreased from 12.8 (5.3) at baseline to 6.0 (3.2) at follow-up.25-28
Munich Cohort
This single-center, prospective clinical trial included patients with AHI > 15 and < 65, central apnea index < 25% of total AHI, and nonadherence to CPAP. Patients were excluded if they had a BMI > 35, anatomical abnormalities that would prevent effective assessment of upper-airway stimulation; all other exclusion criteria matched those used in the STAR trial. Among 31 patients who received implants and completed a 1-year follow-up, mean (SD) AHI decreased from 32.9 (11.2) at baseline to 7.1 (5.9) at follow-up and mean (SD) ESS decreased from 12.6 (5.6) at baseline to 5.9 (5.2) at follow-up.29
Kezirian and Colleagues Cohort
This prospective, single-arm, open-label study was conducted at 4 Australian and 4 US sites. Selection criteria included moderate-to-severe OSA with failure of CPAP, AHI of 20 to 100 with ≥ 15 events/hour occurring in sleep that was non-REM (rapid eye movement) sleep, BMI ≤ 40 (Australia) or ≤ 37 (US), and a predominance of hypopneas (≥ 80% of disordered breathing events during sleep). Patients were excluded if they had earlier upper airway surgery, markedly enlarged tonsils, uncontrolled nasal obstruction, severe retrognathia, > 5% central or mixed apneic events, incompletely treated sleep disorders other than OSA, or a major disorder of the pulmonary, cardiac, renal, or nervous systems. Data were reported for 31 patients whose mean (SD) AHI declined from 45.4 (17.5) at baseline to 25.3 (20.6) at 1-year follow-up and mean (SD) ESS score declined from 12.1 (4.6) at baseline to 7.9 (3.8) 1 year later.30
TJU and UP Cohorts
The TJU and UP cohorts are composed of patients who underwent implantation between May 2014 and August 2016 at 2 academic centers.31,32 Selection criteria was consistent with that used in the STAR trial, and patients completed postoperative titration PSG and outpatient follow-up (48 patients at TJU and 49 at UP). Primary outcomes included AHI, ESS, and O2 nadir. Secondary outcomes consisted of surgical success and percentage of patients tolerating optimal titration setting at follow-up. Postoperative outcomes were assessed during the titration PSG. Time from initial ESS to postoperative PSG at TJU was 1.7 years and at UP was 1.9 years. Time from initial AHI to postoperative PSG at TJU was 90.4 days and 85.2 days at UP. At TJU, mean (SD) AHI and ESS dropped from 35.9 (20.8) and 11.1 (3.8), respectively at baseline to 6.3 (11.5) and 5.8 (3.4), respectively at follow-up. At UP, mean (SD) AHI and ESS fell from 35.3 (15.3) and 10.9 (4.9), respectively at baseline to 6.3 (6.1) and 6.6 (4.5), respectively at follow-up. There were no site-related differences in rates of AHI, ESS, or surgical success.31
Pordzik and Colleagues Cohort
This cohort of 29 patients underwent implantation between February 2020 and June 2022 at a tertiary university medical center with both pre- and postoperative PSG. Selection criteria was consistent with that of the German postmarket cohort. Postoperative PSG was completed a mean (SD) 96.3 (27.0) days after device activation. Mean (SD) AHI dropped from 38.6 (12.7) preoperatively to 24.4 (13.3) postoperatively. Notably, this cohort showed a much lower decrease of postoperative AHI than reported by the STAR trial and UP/TJU cohort.33
Stimulation vs Sham Trial
This multicenter, double-blinded, randomized, crossover trial assessed the effect of HGNS (stim) vs sham stimulation (sham) in 86 patients that completed both phases of the trial. Primary outcomes included AHI and ESS. Secondary outcomes included FOSQ. No carryover effect was found during the crossover phase. The difference between the phases was−15.5 (95% CI, −18.3 to −12.8) for AHI and −3.3 (95% CI, −4.4 to −2.2) for ESS.34
Comparator
The comparator study used propensity score matching to compare outcomes of HGNS and PAP therapy. Primary outcomes included sleepiness, AHI, and effectiveness with outcome measures of AHI and ESS collected at baseline and 12 months postimplantation. The article reported that 126 of 227 patients were matched 1:1. Both groups showed improvement in AHI and ESS. Mean (SD) AHI for the HGNS group at baseline started at 33.9 (15.1) and decreased to 8.1 (6.3). Mean (SD) ESS for the HGNS group at baseline was 15.4 (3.5) and decreased to 7.5 (4.7). In the PAP comparator group, mean (SD) baseline AHI was 36.8 (21.6) and at follow-up was 6.6 (8.0) and mean (SD) ESS was 14.6 (3.9) at baseline and 10.8 (5.6) at follow-up.35
DISCUSSION
The current clinical data on HGNS suggest that this treatment is effective in adults with moderate-to-severe OSA and effects are sustained at long-term follow-up, as measured by AHI reduction and improvements in sleep related symptoms and quality of life (Table 2). These results have been consistent across several sites.
The STAR trial included a randomized control withdrawal group, for whom HGNS treatment was withdrawn after the 12-month follow-up, and then restored at 18 months.21 This revealed that withdrawal of HGNS treatment resulted in deterioration of both objective and subjective measures of OSA and sleepiness. The beneficial effects of HGNS were restored when treatment was resumed.24 Additionally, the RCCT revealed that therapeutic stimulation via HGNS significantly reduced subjective and objective measures of OSA.34 These studies provide definitive evidence of HGNS efficacy.
Currently, a diagnosis of OSA on PAP is classified as a 50% military disability rating. This rating is based primarily on epidemiologic evidence that untreated OSA is a costly disease that leads to other chronic illnesses that increases health care utilization.9 HGNS requires an initially invasive procedure and higher upfront costs, but it could result in reduced health care use and long-term costs because of improved adherence to treatment—compared with CPAP—that results in better outcomes.
Limitations to OSA Studies
The reviewed studies have several limitations that warrant caution when determining the possible benefits of HGNS treatment. The primary limitation is the lack of active control groups, therefore precluding a direct comparison of the short- and long-term effectiveness of HGNS vs other treatments (eg, CPAP). This is especially problematic because in the reviewed studies HGNS treatment efficacy is reported as a function of the mean—and SD—percent reduction in the AHI, whereas the efficacy of CPAP treatment usually is defined in terms of “adequacy of titration” as suggested by the AASM.36 It has been reported that with CPAP treatment, 50% to 60% of OSA patients achieve AASM-defined optimal improvement of respiratory disturbance index of < 5/hour during a polysomnographic sleep recording of ≥ 15 minutes duration that includes REM sleep in the supine position.37 In most of the reviewed studies, treatment success was more liberally defined as a decrease of AHI by ≥ 50%, regardless of the resulting AHI. It is notable that among the reviewed HGNS studies, the TJU and UP cohorts achieved the best outcome in short-term follow-up of 2 months with a mean (SD) AHI of 6.3 (11.5) and 6.4 (6.1), respectively. Among those cohortsassessed at a 12-month follow-up, the Munich cohort achieved the best outcome with a mean (SD) AHI of 7.1 (5.9).
Although the metrics reported in the reviewed studies are not directly comparable, the reported findings strongly suggest that HGNS generally is less effective than CPAP. How important are these differences? With findings that HGNS “reliably produces clinically meaningful (positive) effects on daytime sleepiness, daytime functioning, and sleep quality,” does it really matter if the outcome metrics for HGNS are a little less positive than those produced by CPAP?38 For individual military OSA patients the answer is yes. This is because in military operational environments—especially during deployment—sleep restriction is nearly ubiquitous, therefore any mild residual deficits in sleep quality and daytime alertness resulting from nominally adequate, but suboptimal OSA treatment, could be exacerbated by sleep restriction, therefore placing the service member and the mission at increased risk.39
Another limitation is the narrow inclusion criteria these studies employed, which limits the generalizability of the findings. Participants in the reviewed clinical trials were selected from a patient population that was mostly middle-aged, White, and obese or overweight. In a Medical Surveillance Monthly Report study, OSA was found to be highest among service members aged > 40 years, male, obese, and Black/non-Hispanic (although it should be noted that more than one-half of enlisted service members aged ≤ 25 years).40,41 Obesity has been noted as a growing concern for the military as the military population is beginning to mirror the civilian population in terms of being overweight or obese despite height and weight standards. HGNS might not be as successful in military populations with different demographics. Moreover, HGNS has been shown to have greater AHI reduction among those with higher BMI.30 Although obese service members have a 6-fold higher 12-year incidence rate of OSA than service members without obesity, this nevertheless suggests that general level of HGNS efficacy might be lower among the military patient population, because obesity is less prevalent in the military than the general population.9
Ethnicity has been found to be a relevant factor, with the highest incidence rate of OSA among non-Hispanic Black males, a demographic that was underrepresented in cohorts included in this review. Further studies will be needed to determine the extent to which findings from HGNS treatment studies are generalizable to the broader OSA patient population.
HGNS Implementation Challenges
Current impediments to widespread use of HGNS as an OSA treatment include no standardized guidance for titration and follow-on care, which varies based on the resources available. Titrating a new device for HGNS requires experienced sleep technicians who have close relationships with device representatives and can troubleshoot problems. Technical expertise, which currently is rare, is required if there are complications after placement or if adjustments to voltage settings are needed over time. In addition, patients may require multiple specialists making it easy to get lost to follow-up after implantation. This is particularly challenging in a transient community, such as the military, because there is no guarantee that a service member will have access to the same specialty care at the next duty station.
Although some evidence suggests that HGNS is a viable alternative treatment for some patients with OSA, the generalizability of these findings to the military patient population is unclear. Specialized facilities and expertise are needed for the surgical procedure and follow-up requirements, which currently constitute significant logistical constraints. As with any implantable device, there is a risk of complications including infection that could result in medical evacuation from a theater of operations. If the device malfunctions or loses effectiveness in a deployed environment, the service member might not have immediate access to medical support, potentially leading to undertreatment of OSA. In future battlefield scenarios in multidomain operations, prolonged, far-forward field care will become the new normal because the military is not expected to have air superiority or the ability to quickly evacuate service members to a higher level of medical care.42
In deployed environments, the potential limitations of HGNS become increasingly risky for the service member and the overall mission. Considering these factors, it will be important to evaluate the practicality of HGNS as a treatment option in military populations. Military-specific challenges associated with HGNS that require further study, include guidance for patient selection outside academic centers, guidance on long-term postsurgical care and device maintenance, duty limitation and military retention considerations, and limitations in training and combat environments. The military medical community needs to conduct its own studies in appropriately selected service members to guide clinical practice.
CONCLUSIONS
HGNS treatment results in improvement of both AHI and ESS scores and could be a deployable treatment option for military patients with OSA. However, HGNS has not been found to be as effective as CPAP, although the current literature is limited by small sample sizes, homogeneous populations that do not reflect the demographics of the military, and mostly short follow-up periods. Future studies should be focused on collecting data on HGNS from demographic groups that are more representative of the military OSA patient population and identifying the subpopulation of patients who derive the greatest benefit from HGNS, so that this treatment can be better individually targeted. Until data on existing military patients is published, it is not possible to fully weigh risks and benefits in this population and generalize civilian guidance to the military.
1. Cumpston E, Chen P. Sleep Apnea Syndrome. PubMed. Updated September 4, 2023. Published January 2024. https://www.ncbi.nlm.nih.gov/books/NBK564431/
2. American Academy of Sleep Medicine. Obstructive sleep apnea. Accessed November 27, 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf
3. Cowen J, Harrison S, Thom L, et al. Use of historical remote monitoring data to determine predictors of CPAP non-compliance in patients with Osa. Sleep Breath. 2023;27(5):1899-1908. doi:10.1007/s11325-023-02806-3
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi:10.1093/aje/kws342
5. Stiegmann RA, Payne CB, Kiel MA, Stahlman SL. Increased Prevalence of Overweight and Obesity and Incidence of Prediabetes and Type 2 Diabetes During the COVID-19 Pandemic, Active Component Service Members, U.S. Armed Forces, 2018 to 2021. MSMR. 2023;30(1):11-18. Published 2023 Jan 20.
6. Adult obesity facts. Centers for Disease Control and Prevention. Updated May 17, 2022. Accessed November 27, 2023. https://www.cdc.gov/obesity/data/adult.html
7. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
8. Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. doi:10.1093/sleep/zsz112
9. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
10. Veterans Affairs 38 C.F.R. § 4.97-13, Code 6847.
11. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323-335. doi:10.1007/s11325-010-0391-y
12. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178. doi:10.1513/pats.200708-119mg
13. Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435. doi:10.1378/chest.121.2.430
14. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Obstruction nasale et compliance à la ventilation nasale à pression positive [Nasal obstruction and compliance to nasal positive airway pressure]. Ann Otolaryngol Chir Cervicofac. 2003;120(3):161-166.
15. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13-18.
16. Suurna MV, Jacobowitz O, Chang J, et al. Improving outcomes of hypoglossal nerve stimulation therapy: current practice, future directions, and research gaps. Proceedings of the 2019 International Sleep Surgery Society Research Forum. J Clin Sleep Med. 2021;17(12):2477-2487. doi:10.5664/jcsm.9542
17. Inspire Medical Systems, Inc. Announces FDA approval for apnea hypopnea index indication expansion and increased body mass index labeling. Inspire Medical Systems, Inc. Accessed July 14, 2023. https://investors.inspiresleep.com/investors/press-releases/press-release-details/2023/Inspire-Medical-Systems-Inc.-Announces-FDA-Approval-for-Apnea-Hypopnea-Index-Indication-Expansion-and-Increased-Body-Mass-Index-Labeling/default.aspx
18. Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: Validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(08):1293-1301. Published 2018 Aug 15. doi:10.5664/jcsm.7258
19. The Centre for Evidence-Based Medicine. November 25, 2020. http://www.cebm.net/index.aspx?o=5653
20. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
21. Strollo PJ Jr, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38(10):1593-1598. Published 2015 Oct 1. doi:10.5665/sleep.5054
22. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181-188. doi:10.1177/0194599815616618
23. Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194-202. doi:10.1177/0194599818762383
24. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg. 2014;151(5):880-887. doi:10.1177/0194599814544445
25. Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg. 2017;156(2):378-384. doi:10.1177/0194599816683378
26. Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509-515. doi:10.1002/lary.26688
27. Steffen A, Sommer UJ, Maurer JT, Abrams N, Hofauer B, Heiser C. Long-term follow-up of the German post-market study for upper airway stimulation for obstructive sleep apnea. Sleep Breath. 2020;24(3):979-984. doi:10.1007/s11325-019-01933-028.
28. Hasselbacher K, Hofauer B, Maurer JT, Heiser C, Steffen A, Sommer JU. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol. 2018;275(7):1913-1919. doi:10.1007/s00405-018-5017-129.
29. Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727-1734. doi:10.1007/s00405-016-4297-6
30. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res. 2014;23(1):77-83. doi:10.1111/jsr.12079
31. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med. 2016;12(1):43-48. doi:10.5664/jcsm.5390
32. Huntley C, Kaffenberger T, Doghramji K, Soose R, Boon M. Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med. 2017;13(9):1075-1079. Published 2017 Sep 15. doi:10.5664/jcsm.6726

33. Pordzik J, Seifen C, Ludwig K, et al. Short-term outcome of unilateral inspiration-coupled hypoglossal nerve stimulation in patients with obstructive sleep apnea. Int J Environ Res Public Health. 2022;19(24):16443. Published 2022 Dec 8. doi:10.3390/ijerph192416443
34. Heiser C, Steffen A, Hofauer B, et al. Effect of upper airway stimulation in patients with obstructive sleep apnea (EFFECT): a randomized controlled crossover trial. J Clin Med. 2021;10(13):2880. Published 2021 Jun 29. doi:10.3390/jcm1013288035.
35. Heiser C, Steffen A, Strollo PJ Jr, Giaie-Miniet C, Vanderveken OM, Hofauer B. Hypoglossal nerve stimulation versus positive airway pressure therapy for obstructive sleep apnea. Sleep Breath. 2023;27(2):693-701. doi:10.1007/s11325-022-02663-6
36. Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157-171.
37. Freedman N, Johnson K. Positive airway pressure treatment for obstructive sleep apnea. In: Kryger MH, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. Elsevier; 2022:1260-1283.
38. Braun M, Stoerzel M, Wollny M, Schoebel C, Ulrich Sommer J, Heiser C. Patient-reported outcomes with hypoglossal nerve stimulation for treatment of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280(10):4627-4639. doi:10.1007/s00405-023-08062-1
39. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. doi:10.5665/SLEEP.1236
40. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
41. Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2017 Demographics: Profile of the Military Community. US Dept of Defense;2017. Accessed April 4, 2024. http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf
42. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2S Suppl 1): S180-S184. doi:10.1097/TA.0000000000004063
1. Cumpston E, Chen P. Sleep Apnea Syndrome. PubMed. Updated September 4, 2023. Published January 2024. https://www.ncbi.nlm.nih.gov/books/NBK564431/
2. American Academy of Sleep Medicine. Obstructive sleep apnea. Accessed November 27, 2023. https://aasm.org/resources/factsheets/sleepapnea.pdf
3. Cowen J, Harrison S, Thom L, et al. Use of historical remote monitoring data to determine predictors of CPAP non-compliance in patients with Osa. Sleep Breath. 2023;27(5):1899-1908. doi:10.1007/s11325-023-02806-3
4. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006-1014. doi:10.1093/aje/kws342
5. Stiegmann RA, Payne CB, Kiel MA, Stahlman SL. Increased Prevalence of Overweight and Obesity and Incidence of Prediabetes and Type 2 Diabetes During the COVID-19 Pandemic, Active Component Service Members, U.S. Armed Forces, 2018 to 2021. MSMR. 2023;30(1):11-18. Published 2023 Jan 20.
6. Adult obesity facts. Centers for Disease Control and Prevention. Updated May 17, 2022. Accessed November 27, 2023. https://www.cdc.gov/obesity/data/adult.html
7. Moore BA, Tison LM, Palacios JG, Peterson AL, Mysliwiec V. Incidence of insomnia and obstructive sleep apnea in active duty United States military service members. Sleep. 2021;44(7):zsab024. doi:10.1093/sleep/zsab024
8. Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: a retrospective cohort investigation. Sleep. 2019;42(8):zsz112. doi:10.1093/sleep/zsz112
9. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
10. Veterans Affairs 38 C.F.R. § 4.97-13, Code 6847.
11. Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath. 2010;14(4):323-335. doi:10.1007/s11325-010-0391-y
12. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173-178. doi:10.1513/pats.200708-119mg
13. Sin DD, Mayers I, Man GCW, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435. doi:10.1378/chest.121.2.430
14. Nowak C, Bourgin P, Portier F, Genty E, Escourrou P, Bobin S. Obstruction nasale et compliance à la ventilation nasale à pression positive [Nasal obstruction and compliance to nasal positive airway pressure]. Ann Otolaryngol Chir Cervicofac. 2003;120(3):161-166.
15. Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7(1):13-18.
16. Suurna MV, Jacobowitz O, Chang J, et al. Improving outcomes of hypoglossal nerve stimulation therapy: current practice, future directions, and research gaps. Proceedings of the 2019 International Sleep Surgery Society Research Forum. J Clin Sleep Med. 2021;17(12):2477-2487. doi:10.5664/jcsm.9542
17. Inspire Medical Systems, Inc. Announces FDA approval for apnea hypopnea index indication expansion and increased body mass index labeling. Inspire Medical Systems, Inc. Accessed July 14, 2023. https://investors.inspiresleep.com/investors/press-releases/press-release-details/2023/Inspire-Medical-Systems-Inc.-Announces-FDA-Approval-for-Apnea-Hypopnea-Index-Indication-Expansion-and-Increased-Body-Mass-Index-Labeling/default.aspx
18. Lapin BR, Bena JF, Walia HK, Moul DE. The Epworth Sleepiness Scale: Validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med. 2018;14(08):1293-1301. Published 2018 Aug 15. doi:10.5664/jcsm.7258
19. The Centre for Evidence-Based Medicine. November 25, 2020. http://www.cebm.net/index.aspx?o=5653
20. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
21. Strollo PJ Jr, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep. 2015;38(10):1593-1598. Published 2015 Oct 1. doi:10.5665/sleep.5054
22. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg. 2016;154(1):181-188. doi:10.1177/0194599815616618
23. Woodson BT, Strohl KP, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: 5-year outcomes. Otolaryngol Head Neck Surg. 2018;159(1):194-202. doi:10.1177/0194599818762383
24. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg. 2014;151(5):880-887. doi:10.1177/0194599814544445
25. Heiser C, Maurer JT, Hofauer B, Sommer JU, Seitz A, Steffen A. Outcomes of upper airway stimulation for obstructive sleep apnea in a multicenter German postmarket study. Otolaryngol Head Neck Surg. 2017;156(2):378-384. doi:10.1177/0194599816683378
26. Steffen A, Sommer JU, Hofauer B, Maurer JT, Hasselbacher K, Heiser C. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope. 2018;128(2):509-515. doi:10.1002/lary.26688
27. Steffen A, Sommer UJ, Maurer JT, Abrams N, Hofauer B, Heiser C. Long-term follow-up of the German post-market study for upper airway stimulation for obstructive sleep apnea. Sleep Breath. 2020;24(3):979-984. doi:10.1007/s11325-019-01933-028.
28. Hasselbacher K, Hofauer B, Maurer JT, Heiser C, Steffen A, Sommer JU. Patient-reported outcome: results of the multicenter German post-market study. Eur Arch Otorhinolaryngol. 2018;275(7):1913-1919. doi:10.1007/s00405-018-5017-129.
29. Heiser C, Knopf A, Bas M, Gahleitner C, Hofauer B. Selective upper airway stimulation for obstructive sleep apnea: a single center clinical experience. Eur Arch Otorhinolaryngol. 2017;274(3):1727-1734. doi:10.1007/s00405-016-4297-6
30. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res. 2014;23(1):77-83. doi:10.1111/jsr.12079
31. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med. 2016;12(1):43-48. doi:10.5664/jcsm.5390
32. Huntley C, Kaffenberger T, Doghramji K, Soose R, Boon M. Upper airway stimulation for treatment of obstructive sleep apnea: an evaluation and comparison of outcomes at two academic centers. J Clin Sleep Med. 2017;13(9):1075-1079. Published 2017 Sep 15. doi:10.5664/jcsm.6726

33. Pordzik J, Seifen C, Ludwig K, et al. Short-term outcome of unilateral inspiration-coupled hypoglossal nerve stimulation in patients with obstructive sleep apnea. Int J Environ Res Public Health. 2022;19(24):16443. Published 2022 Dec 8. doi:10.3390/ijerph192416443
34. Heiser C, Steffen A, Hofauer B, et al. Effect of upper airway stimulation in patients with obstructive sleep apnea (EFFECT): a randomized controlled crossover trial. J Clin Med. 2021;10(13):2880. Published 2021 Jun 29. doi:10.3390/jcm1013288035.
35. Heiser C, Steffen A, Strollo PJ Jr, Giaie-Miniet C, Vanderveken OM, Hofauer B. Hypoglossal nerve stimulation versus positive airway pressure therapy for obstructive sleep apnea. Sleep Breath. 2023;27(2):693-701. doi:10.1007/s11325-022-02663-6
36. Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157-171.
37. Freedman N, Johnson K. Positive airway pressure treatment for obstructive sleep apnea. In: Kryger MH, Roth T, Goldstein CA, Dement WC, eds. Principles and Practice of Sleep Medicine. Elsevier; 2022:1260-1283.
38. Braun M, Stoerzel M, Wollny M, Schoebel C, Ulrich Sommer J, Heiser C. Patient-reported outcomes with hypoglossal nerve stimulation for treatment of obstructive sleep apnea: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2023;280(10):4627-4639. doi:10.1007/s00405-023-08062-1
39. Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. doi:10.5665/SLEEP.1236
40. Rogers AE, Stahlman S, Hunt DJ, Oh GT, Clark LL. Obstructive sleep apnea and associated attrition, active component, U.S. Armed Forces, January 2004-May 2016. MSMR. 2016;23(10):2-11.
41. Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. 2017 Demographics: Profile of the Military Community. US Dept of Defense;2017. Accessed April 4, 2024. http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf
42. Remondelli MH, Remick KN, Shackelford SA, et al. Casualty care implications of large-scale combat operations. J Trauma Acute Care Surg. 2023;95(2S Suppl 1): S180-S184. doi:10.1097/TA.0000000000004063