User login
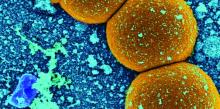
The U.S. Department of Veterans Affairs MRSA Prevention Initiative, implemented in October 2007, has shown progress at limiting health care–associated infections of methicillin-resistant Staphylococcus aureus through 2011 and 2012.
A new report published in the January 2017 issue of the American Journal of Infection Control tracks continued declines in infection through September 2015.
Monthly rates of health care–associated infections fell significantly in all settings from October 2007 to September 2015: an 87% decrease in ICUs, 80.1% in non-ICUs, 80.9% in spinal cord injury units, and 49.4% in long-term care facilities (P for all less than .0001).
“The VA data suggest that active surveillance followed by contact precautions (with or without decolonization) may be most useful when MRSA [health care–associated infection] rates are unacceptably high (as they were in VA facilities during 2007) or to decrease infections in high-risk units such as ICUs,” Dr. Evans and his colleagues concluded.
Details about the implementation of the initiative were previously published in the New England Journal of Medicine in 2011, including the initiative’s goal to promote “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” (N Engl J Med. 2011;364:1419-30).
Dr. Evans and his colleagues had no relevant financial disclosures.
The U.S. Department of Veterans Affairs MRSA Prevention Initiative, implemented in October 2007, has shown progress at limiting health care–associated infections of methicillin-resistant Staphylococcus aureus through 2011 and 2012.
A new report published in the January 2017 issue of the American Journal of Infection Control tracks continued declines in infection through September 2015.
Monthly rates of health care–associated infections fell significantly in all settings from October 2007 to September 2015: an 87% decrease in ICUs, 80.1% in non-ICUs, 80.9% in spinal cord injury units, and 49.4% in long-term care facilities (P for all less than .0001).
“The VA data suggest that active surveillance followed by contact precautions (with or without decolonization) may be most useful when MRSA [health care–associated infection] rates are unacceptably high (as they were in VA facilities during 2007) or to decrease infections in high-risk units such as ICUs,” Dr. Evans and his colleagues concluded.
Details about the implementation of the initiative were previously published in the New England Journal of Medicine in 2011, including the initiative’s goal to promote “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” (N Engl J Med. 2011;364:1419-30).
Dr. Evans and his colleagues had no relevant financial disclosures.
The U.S. Department of Veterans Affairs MRSA Prevention Initiative, implemented in October 2007, has shown progress at limiting health care–associated infections of methicillin-resistant Staphylococcus aureus through 2011 and 2012.
A new report published in the January 2017 issue of the American Journal of Infection Control tracks continued declines in infection through September 2015.
Monthly rates of health care–associated infections fell significantly in all settings from October 2007 to September 2015: an 87% decrease in ICUs, 80.1% in non-ICUs, 80.9% in spinal cord injury units, and 49.4% in long-term care facilities (P for all less than .0001).
“The VA data suggest that active surveillance followed by contact precautions (with or without decolonization) may be most useful when MRSA [health care–associated infection] rates are unacceptably high (as they were in VA facilities during 2007) or to decrease infections in high-risk units such as ICUs,” Dr. Evans and his colleagues concluded.
Details about the implementation of the initiative were previously published in the New England Journal of Medicine in 2011, including the initiative’s goal to promote “a change in the institutional culture whereby infection control would become the responsibility of everyone who had contact with patients” (N Engl J Med. 2011;364:1419-30).
Dr. Evans and his colleagues had no relevant financial disclosures.
FROM THE AMERICAN JOURNAL OF INFECTION CONTROL