User login
Vitamin D is the new wonder cure and preventive for all kinds of ailments and chronic diseases. Or so it would seem from the popular press and Internet.1
But what do we actually know about the health benefits of vitamin D? Should we be screening patients for vitamin D deficiency? How much vitamin D should our patients consume daily? This Practice Alert answers these questions.
Vitamin D basics
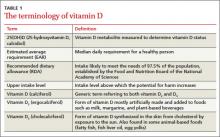
Vitamin D is synthesized in the skin from cholesterol through sun exposure (vitamin D3) and consumed in food fortified with vitamin D2, such as milk, yogurt, and orange juice, or food that contains vitamin D3 (fatty fish and eggs). Both forms of vitamin D are inactive until metabolized in the liver to 25(OH)D (TABLE 1), which is further metabolized in the kidney to the biologically active calcitriol. The 25(OH)D circulates in the blood with a vitamin D–binding protein and is the basis of measurement of serum vitamin D levels.
The terminology of vitamin D
The metabolic actions of calcitriol include regulation of calcium and phosphate levels and maintenance of bone health. It also has a role in regulating cell proliferation and immune system functions. These last 2 activities are not well understood; still, they have led to the hypothesis that vitamin D may help prevent cancer, autoimmune conditions, and cardiovascular disease. Promotion of calcitriol for these purposes has yet to be supported by well-controlled clinical trials.
One more source…Vitamin D can also be found in multivitamin preparations at various dosages and is sold as a single vitamin supplement—sometimes in megadoses of up to 50,000 international units (IU).
How much vitamin D is enough?
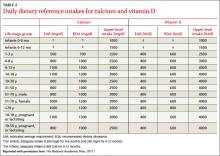
There is universal agreement that vitamin D and calcium are important for bone health. The Institute of Medicine (IOM) recently revised the recommended dietary allowance (RDA) of vitamin D, by age (TABLE 2).2 The IOM calculated the newer RDAs under the assumption that, in the United States and Canada, little or no vitamin D is obtained from sun exposure, particularly given anticancer campaigns that stress sun avoidance. The IOM committee also expressed concern, however, about high levels of vitamin D intake that have not been linked to any proven benefits but have been linked to harms.2 Excess vitamin D from oral intake (not from sun exposure, which is subject to autoregulatory mechanisms) can cause vitamin D intoxication, hypercalcemia, and kidney stones.
Daily dietary reference intakes for calcium and vitamin D
Recent systematic reviews and recommendations
The IOM reviewed the medical literature on the effects of vitamin D to prevent or treat cancer, cardiovascular disease, hypertension, diabetes, metabolic syndrome, falls, and preeclampsia; and to boost immune response, neuropsychological function, physical performance, and reproductive outcomes. The panel found that the evidence for all of these effects is mixed and inconclusive, even though the media often report a beneficial effect.2
Several Cochrane systematic reviews have yielded similar results. One looked at overall mortality in adults and found that vitamin D3 seems to decrease mortality, but mostly in elderly women in institutions and dependent-care settings. Vitamin D2 had no effect on mortality. Vitamin D3 and calcium significantly increased the incidence of kidney stones.3Another review examined the effect of vitamin D on chronic pain and concluded that there were only low-quality observational studies insufficient for drawing conclusions.4
The United States Preventive Services Task Force (USPSTF) recently released 2 recommendations related to vitamin D supplementation.5,6 It first recommends exercise or physical therapy and vitamin D supplementation (800 IU daily) to prevent falls in community-dwelling adults ≥65 years at increased risk for falls (described in a previous Practice Alert7). The second recommendation pertains to primary prevention of fractures and advises against daily supplementation with vitamin D and calcium at doses ≤400 IU and 1000 mg, respectively, for noninstitutionalized postmenopausal women. At these doses, supplementation with vitamin D and calcium does not prevent fractures but does cause kidney stones, with a number needed to harm of 273 over 7 years.6 The USPSTF concluded that the evidence is insufficient to assess the value of either vitamin D or calcium in men and premenopausal women at any dose, or daily supplementation with >400 IU of vitamin D3 and >1000 mg of calcium for the primary prevention of fractures in noninstitutionalized postmenopausal women.
What about screening for vitamin D deficiency?
The Endocrine Society recommends screening for vitamin D deficiency in individuals at risk FAST TRACK. The USPSTF recommends vitamin D supplementation at 800 IU/d to prevent falls in community-dwelling adults >65 years at increased risk for falls. for deficiency—ie, those who have darkly pigmented skin, live in northern latitudes, or receive little exposure to sun. It does not recommend population screening for vitamin D deficiency in individuals not at risk. It defines vitamin D deficiency as a 25(OH)D level <20 ng/mL (50 nmol/L) and vitamin D insufficiency as a 25(OH)D level of 21 to 29 ng/mL (52.5-72.5 nmol/L).8
The IOM expresses concern about testing for vitamin D levels because there is no validated cutoff, and some labs report cutoffs above what the IOM considers a deficient level, leading to inflated numbers of those labeled as deficient.2 The USPSTF is about to weigh in on this issue. It has posted a draft research plan that will guide its evidence report and recommendation considerations.9
Take-home message
Information on the health benefits of vitamin D is difficult to sort out. Evidence for anything other than bone health and fall prevention is problematic. Consider vitamin D supplements along with calcium for the frail elderly at risk for falls10and for those who have osteoporosis. Screening for vitamin D deficiency is of questionable value and the USPSTF will be producing an evidence-based report on this topic, which should be available in about a year. The IOM RDA tables are available to guide dietary advice.
1. Vitamin D Council. Available at: http://www.vitamindcouncil.org/health-conditions. Accessed May 7, 2013.
2. Institute of Medicine of the National Academies. Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press; 2011. Available at: http://www.nap.edu/catalog.php?record_id=13050. Accessed June 3, 2013.
3. Bjelakovic G, Gluud LL, Whitfield K, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev. 2011;(7):CD007470.
4. Straube S, Derry S, Moore RA, et al. Vitamin D for the treatment of chronic painful conditions in adults. Cochrane Database Syst Rev. 2010;(1):CD007771.
5. USPSTF. Prevention of falls in community-dwelling older adults. Available at: http://www.uspreventiveservicestaskforce.org/
uspstf/uspsfalls.htm. Accessed May 7, 2013.
6. USPSTF. Vitamin D and calcium supplementation to prevent fractures in adults. Available at: http://www.uspreventive
servicestaskforce.org/uspstf/uspsvitd.htm. Accessed May 7, 2013.
7. Campos-Outcalt D. The latest recommendations from the
USPSTF. J Fam Pract. 2013;62:249-252.
8. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency. J Clin Endocrinol Metab. 2011;96:1911-1930.
9. USPSTF. Draft research plan. Screening for vitamin D deficiency. Available at: http://www.uspreventiveservicestaskforce.org/
uspstf13/vitddefic/vitddeficdraftresplan.htm. Accessed May 7, 2013.
10. Avenell A, Gillespie WJ, Gillespie LD, et al. Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev. 2009;(2):CD000227.
Vitamin D is the new wonder cure and preventive for all kinds of ailments and chronic diseases. Or so it would seem from the popular press and Internet.1
But what do we actually know about the health benefits of vitamin D? Should we be screening patients for vitamin D deficiency? How much vitamin D should our patients consume daily? This Practice Alert answers these questions.
Vitamin D basics
Vitamin D is synthesized in the skin from cholesterol through sun exposure (vitamin D3) and consumed in food fortified with vitamin D2, such as milk, yogurt, and orange juice, or food that contains vitamin D3 (fatty fish and eggs). Both forms of vitamin D are inactive until metabolized in the liver to 25(OH)D (TABLE 1), which is further metabolized in the kidney to the biologically active calcitriol. The 25(OH)D circulates in the blood with a vitamin D–binding protein and is the basis of measurement of serum vitamin D levels.
The terminology of vitamin D
The metabolic actions of calcitriol include regulation of calcium and phosphate levels and maintenance of bone health. It also has a role in regulating cell proliferation and immune system functions. These last 2 activities are not well understood; still, they have led to the hypothesis that vitamin D may help prevent cancer, autoimmune conditions, and cardiovascular disease. Promotion of calcitriol for these purposes has yet to be supported by well-controlled clinical trials.
One more source…Vitamin D can also be found in multivitamin preparations at various dosages and is sold as a single vitamin supplement—sometimes in megadoses of up to 50,000 international units (IU).
How much vitamin D is enough?
There is universal agreement that vitamin D and calcium are important for bone health. The Institute of Medicine (IOM) recently revised the recommended dietary allowance (RDA) of vitamin D, by age (TABLE 2).2 The IOM calculated the newer RDAs under the assumption that, in the United States and Canada, little or no vitamin D is obtained from sun exposure, particularly given anticancer campaigns that stress sun avoidance. The IOM committee also expressed concern, however, about high levels of vitamin D intake that have not been linked to any proven benefits but have been linked to harms.2 Excess vitamin D from oral intake (not from sun exposure, which is subject to autoregulatory mechanisms) can cause vitamin D intoxication, hypercalcemia, and kidney stones.
Daily dietary reference intakes for calcium and vitamin D
Recent systematic reviews and recommendations
The IOM reviewed the medical literature on the effects of vitamin D to prevent or treat cancer, cardiovascular disease, hypertension, diabetes, metabolic syndrome, falls, and preeclampsia; and to boost immune response, neuropsychological function, physical performance, and reproductive outcomes. The panel found that the evidence for all of these effects is mixed and inconclusive, even though the media often report a beneficial effect.2
Several Cochrane systematic reviews have yielded similar results. One looked at overall mortality in adults and found that vitamin D3 seems to decrease mortality, but mostly in elderly women in institutions and dependent-care settings. Vitamin D2 had no effect on mortality. Vitamin D3 and calcium significantly increased the incidence of kidney stones.3Another review examined the effect of vitamin D on chronic pain and concluded that there were only low-quality observational studies insufficient for drawing conclusions.4
The United States Preventive Services Task Force (USPSTF) recently released 2 recommendations related to vitamin D supplementation.5,6 It first recommends exercise or physical therapy and vitamin D supplementation (800 IU daily) to prevent falls in community-dwelling adults ≥65 years at increased risk for falls (described in a previous Practice Alert7). The second recommendation pertains to primary prevention of fractures and advises against daily supplementation with vitamin D and calcium at doses ≤400 IU and 1000 mg, respectively, for noninstitutionalized postmenopausal women. At these doses, supplementation with vitamin D and calcium does not prevent fractures but does cause kidney stones, with a number needed to harm of 273 over 7 years.6 The USPSTF concluded that the evidence is insufficient to assess the value of either vitamin D or calcium in men and premenopausal women at any dose, or daily supplementation with >400 IU of vitamin D3 and >1000 mg of calcium for the primary prevention of fractures in noninstitutionalized postmenopausal women.
What about screening for vitamin D deficiency?
The Endocrine Society recommends screening for vitamin D deficiency in individuals at risk FAST TRACK. The USPSTF recommends vitamin D supplementation at 800 IU/d to prevent falls in community-dwelling adults >65 years at increased risk for falls. for deficiency—ie, those who have darkly pigmented skin, live in northern latitudes, or receive little exposure to sun. It does not recommend population screening for vitamin D deficiency in individuals not at risk. It defines vitamin D deficiency as a 25(OH)D level <20 ng/mL (50 nmol/L) and vitamin D insufficiency as a 25(OH)D level of 21 to 29 ng/mL (52.5-72.5 nmol/L).8
The IOM expresses concern about testing for vitamin D levels because there is no validated cutoff, and some labs report cutoffs above what the IOM considers a deficient level, leading to inflated numbers of those labeled as deficient.2 The USPSTF is about to weigh in on this issue. It has posted a draft research plan that will guide its evidence report and recommendation considerations.9
Take-home message
Information on the health benefits of vitamin D is difficult to sort out. Evidence for anything other than bone health and fall prevention is problematic. Consider vitamin D supplements along with calcium for the frail elderly at risk for falls10and for those who have osteoporosis. Screening for vitamin D deficiency is of questionable value and the USPSTF will be producing an evidence-based report on this topic, which should be available in about a year. The IOM RDA tables are available to guide dietary advice.
Vitamin D is the new wonder cure and preventive for all kinds of ailments and chronic diseases. Or so it would seem from the popular press and Internet.1
But what do we actually know about the health benefits of vitamin D? Should we be screening patients for vitamin D deficiency? How much vitamin D should our patients consume daily? This Practice Alert answers these questions.
Vitamin D basics
Vitamin D is synthesized in the skin from cholesterol through sun exposure (vitamin D3) and consumed in food fortified with vitamin D2, such as milk, yogurt, and orange juice, or food that contains vitamin D3 (fatty fish and eggs). Both forms of vitamin D are inactive until metabolized in the liver to 25(OH)D (TABLE 1), which is further metabolized in the kidney to the biologically active calcitriol. The 25(OH)D circulates in the blood with a vitamin D–binding protein and is the basis of measurement of serum vitamin D levels.
The terminology of vitamin D
The metabolic actions of calcitriol include regulation of calcium and phosphate levels and maintenance of bone health. It also has a role in regulating cell proliferation and immune system functions. These last 2 activities are not well understood; still, they have led to the hypothesis that vitamin D may help prevent cancer, autoimmune conditions, and cardiovascular disease. Promotion of calcitriol for these purposes has yet to be supported by well-controlled clinical trials.
One more source…Vitamin D can also be found in multivitamin preparations at various dosages and is sold as a single vitamin supplement—sometimes in megadoses of up to 50,000 international units (IU).
How much vitamin D is enough?
There is universal agreement that vitamin D and calcium are important for bone health. The Institute of Medicine (IOM) recently revised the recommended dietary allowance (RDA) of vitamin D, by age (TABLE 2).2 The IOM calculated the newer RDAs under the assumption that, in the United States and Canada, little or no vitamin D is obtained from sun exposure, particularly given anticancer campaigns that stress sun avoidance. The IOM committee also expressed concern, however, about high levels of vitamin D intake that have not been linked to any proven benefits but have been linked to harms.2 Excess vitamin D from oral intake (not from sun exposure, which is subject to autoregulatory mechanisms) can cause vitamin D intoxication, hypercalcemia, and kidney stones.
Daily dietary reference intakes for calcium and vitamin D
Recent systematic reviews and recommendations
The IOM reviewed the medical literature on the effects of vitamin D to prevent or treat cancer, cardiovascular disease, hypertension, diabetes, metabolic syndrome, falls, and preeclampsia; and to boost immune response, neuropsychological function, physical performance, and reproductive outcomes. The panel found that the evidence for all of these effects is mixed and inconclusive, even though the media often report a beneficial effect.2
Several Cochrane systematic reviews have yielded similar results. One looked at overall mortality in adults and found that vitamin D3 seems to decrease mortality, but mostly in elderly women in institutions and dependent-care settings. Vitamin D2 had no effect on mortality. Vitamin D3 and calcium significantly increased the incidence of kidney stones.3Another review examined the effect of vitamin D on chronic pain and concluded that there were only low-quality observational studies insufficient for drawing conclusions.4
The United States Preventive Services Task Force (USPSTF) recently released 2 recommendations related to vitamin D supplementation.5,6 It first recommends exercise or physical therapy and vitamin D supplementation (800 IU daily) to prevent falls in community-dwelling adults ≥65 years at increased risk for falls (described in a previous Practice Alert7). The second recommendation pertains to primary prevention of fractures and advises against daily supplementation with vitamin D and calcium at doses ≤400 IU and 1000 mg, respectively, for noninstitutionalized postmenopausal women. At these doses, supplementation with vitamin D and calcium does not prevent fractures but does cause kidney stones, with a number needed to harm of 273 over 7 years.6 The USPSTF concluded that the evidence is insufficient to assess the value of either vitamin D or calcium in men and premenopausal women at any dose, or daily supplementation with >400 IU of vitamin D3 and >1000 mg of calcium for the primary prevention of fractures in noninstitutionalized postmenopausal women.
What about screening for vitamin D deficiency?
The Endocrine Society recommends screening for vitamin D deficiency in individuals at risk FAST TRACK. The USPSTF recommends vitamin D supplementation at 800 IU/d to prevent falls in community-dwelling adults >65 years at increased risk for falls. for deficiency—ie, those who have darkly pigmented skin, live in northern latitudes, or receive little exposure to sun. It does not recommend population screening for vitamin D deficiency in individuals not at risk. It defines vitamin D deficiency as a 25(OH)D level <20 ng/mL (50 nmol/L) and vitamin D insufficiency as a 25(OH)D level of 21 to 29 ng/mL (52.5-72.5 nmol/L).8
The IOM expresses concern about testing for vitamin D levels because there is no validated cutoff, and some labs report cutoffs above what the IOM considers a deficient level, leading to inflated numbers of those labeled as deficient.2 The USPSTF is about to weigh in on this issue. It has posted a draft research plan that will guide its evidence report and recommendation considerations.9
Take-home message
Information on the health benefits of vitamin D is difficult to sort out. Evidence for anything other than bone health and fall prevention is problematic. Consider vitamin D supplements along with calcium for the frail elderly at risk for falls10and for those who have osteoporosis. Screening for vitamin D deficiency is of questionable value and the USPSTF will be producing an evidence-based report on this topic, which should be available in about a year. The IOM RDA tables are available to guide dietary advice.
1. Vitamin D Council. Available at: http://www.vitamindcouncil.org/health-conditions. Accessed May 7, 2013.
2. Institute of Medicine of the National Academies. Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press; 2011. Available at: http://www.nap.edu/catalog.php?record_id=13050. Accessed June 3, 2013.
3. Bjelakovic G, Gluud LL, Whitfield K, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev. 2011;(7):CD007470.
4. Straube S, Derry S, Moore RA, et al. Vitamin D for the treatment of chronic painful conditions in adults. Cochrane Database Syst Rev. 2010;(1):CD007771.
5. USPSTF. Prevention of falls in community-dwelling older adults. Available at: http://www.uspreventiveservicestaskforce.org/
uspstf/uspsfalls.htm. Accessed May 7, 2013.
6. USPSTF. Vitamin D and calcium supplementation to prevent fractures in adults. Available at: http://www.uspreventive
servicestaskforce.org/uspstf/uspsvitd.htm. Accessed May 7, 2013.
7. Campos-Outcalt D. The latest recommendations from the
USPSTF. J Fam Pract. 2013;62:249-252.
8. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency. J Clin Endocrinol Metab. 2011;96:1911-1930.
9. USPSTF. Draft research plan. Screening for vitamin D deficiency. Available at: http://www.uspreventiveservicestaskforce.org/
uspstf13/vitddefic/vitddeficdraftresplan.htm. Accessed May 7, 2013.
10. Avenell A, Gillespie WJ, Gillespie LD, et al. Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev. 2009;(2):CD000227.
1. Vitamin D Council. Available at: http://www.vitamindcouncil.org/health-conditions. Accessed May 7, 2013.
2. Institute of Medicine of the National Academies. Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press; 2011. Available at: http://www.nap.edu/catalog.php?record_id=13050. Accessed June 3, 2013.
3. Bjelakovic G, Gluud LL, Whitfield K, et al. Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev. 2011;(7):CD007470.
4. Straube S, Derry S, Moore RA, et al. Vitamin D for the treatment of chronic painful conditions in adults. Cochrane Database Syst Rev. 2010;(1):CD007771.
5. USPSTF. Prevention of falls in community-dwelling older adults. Available at: http://www.uspreventiveservicestaskforce.org/
uspstf/uspsfalls.htm. Accessed May 7, 2013.
6. USPSTF. Vitamin D and calcium supplementation to prevent fractures in adults. Available at: http://www.uspreventive
servicestaskforce.org/uspstf/uspsvitd.htm. Accessed May 7, 2013.
7. Campos-Outcalt D. The latest recommendations from the
USPSTF. J Fam Pract. 2013;62:249-252.
8. Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency. J Clin Endocrinol Metab. 2011;96:1911-1930.
9. USPSTF. Draft research plan. Screening for vitamin D deficiency. Available at: http://www.uspreventiveservicestaskforce.org/
uspstf13/vitddefic/vitddeficdraftresplan.htm. Accessed May 7, 2013.
10. Avenell A, Gillespie WJ, Gillespie LD, et al. Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev. 2009;(2):CD000227.