User login
Case
A 68-year-old man with hypertension, diabetes, and recent hip fracture with poor functional status presents from a nursing home with a productive cough, shortness of breath, and chills of two-day duration. He finished a five-day course of cephalexin for a urinary tract infection one week ago. His vital signs reveal a blood pressure of 162/80 mm/Hg, temperature of 101.9°F, respirations of 26 breaths per minute, and oxygen saturation of 88% on room air. Coarse breath sounds are noted in the right lung field and his chest X-ray reveals a right-middle-lobe infiltrate.
He is admitted to the hospital with a diagnosis of healthcare-associated pneumonia. What is the best empiric antibiotic coverage for this patient?
Overview
Modern medicine exists over a continuum of care that is delivered in a manifold of different settings. Patients routinely receive complex medical care at home, including wound care and infusion of intravenous antibiotics. Additionally, many patients are interfacing with the healthcare system on a regular basis via hemodialysis centers or sub-acute rehabilitation centers. As a result of these interactions, patients are exposed to—and colonized by—different bacterial pathogens that can result in a variety of infections.1
While patients with healthcare-associated pneumonia (HCAP) can present similarly to those with community-acquired pneumonia (CAP)—patients with CAP normally present with a lower-respiratory-tract infection—the differences in the likely etiological pathogens dictate that these patients be considered for broader-spectrum empiric antibiotics. Hospitalists will continue to be responsible for choosing the initial antibiotic regimen for these patients, and they need to be able to recognize this disease process in order to treat it appropriately.
The joint American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) guidelines released in 2005 emphasize that certain clinical HCAP risk factors center on increased interactions and encounters with healthcare facilities.2 These risk factors are evolving over time to include a patient’s functional status, recent antibiotic use, and clinical severity.
Review of the Data
Differences between HCAP and CAP
HCAP represents a diagnostic category of pneumonia created to differentiate patients with infections caused by a different microbiological subset of bacteria, including possible multi-drug-resistant (MDR) organisms, from patients with CAP. Thus far, culture data support this dichotomy.3,4
Kollef and colleagues performed a multicenter, retrospective cohort study of 4,543 patients with bacterial respiratory culture-positive pneumonia between 2002 and 2003. The study examined the bacteriological differences between CAP and HCAP. In this study, HCAP patients were defined as having: transfer from another healthcare facility; long-term hemodialysis; or prior hospitalization within 30 days in which they had non-ventilator-associated pneumonia (VAP). CAP patients were defined as having non-VAP and non-HCAP.
The study showed that the frequency of Pseudomonas aeurginosa (25% HCAP vs. 17% CAP) and Staphylococcus aureus (46% vs. 25%), which included methicillin-resistant Staphylococcus aureus (MRSA) (18% vs. 6%), was significantly higher in patients with HCAP than those with CAP. Additionally, frequency of Streptococcus pneumoniae (5% vs. 16%) and Haemophilus influenza (5% vs. 16%) infections were noted as significantly lower.3
A single-center, retrospective cohort analysis of 639 patients done by Micek et al yielded similar culture differences between CAP and HCAP patients. In this study, criteria for HCAP were defined as hospitalization in the past year, immunosuppression, nursing-home resident, or hemodialysis. The study authors found that a significantly higher percentage of HCAP patients were infected with MRSA (30% vs. 12%), Pseudomonas aeurginosa (25% vs. 4%), and other non-fermenting gram-negative rods (GNR) (10% vs. 2%). HCAP patients again were noted as having significantly fewer infections with S. pneumoniae (10% vs. 40%) and Haemophilus influenza (4% vs. 17%).
In addition to showing a difference in the bacteriology of CAP and HCAP, the Kollef study also evaluated mortality rates, length of stay, and hospital charges. Mortality rates for HCAP (19.8%) were similar to those of hospital-acquired pneumonia (HAP) (18.8%), and both of these were significantly higher than CAP (10%). Length of stay and hospital cost increased across the spectrum, from CAP to HCAP to HAP, with significant differences between each.3
ATS/IDSA Guidelines
In 2005, a joint committee of the ATS and ISDA updated its initial 1996 nosocomial pneumonia guidelines. The guideline update included the new HCAP category.2 The No. 1 goal of these guidelines was to emphasize early and appropriate antibiotics, followed by tailoring of the treatment regimen based upon culture and clinical data. To this end, HCAP risk factors were developed via extrapolation from observational data generated from HAP and VAP patients.5,6,7
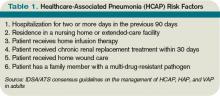
The risk factors are summarized in Table 1 (see p. 19).2 Guidelines dictated that the identification of any of these risk factors in pneumonia patients at the time of admission indicates increased risk for infection with an MDR organism. These high-risk patients require placement into the diagnostic category of HCAP.
Once a patient has been diagnosed with HCAP, the guidelines recommended obtaining lower-respiratory-tract cultures and initiating broad-spectrum antibiotic therapy. Appropriate empiric antibiotic therapy was suggested to be the same as for HAP. This regimen requires coverage with two anti-pseudomonal agents, as well as an agent with activity against MRSA.
The rationale behind initial coverage with two anti-pseudomonal agents stems from the finding that pseudomonas has a high rate of resistance to many antibiotics, and that if two agents are empirically started, chances of appropriate coverage increase from the outset. This is important, as timely administration of appropriate antibiotics has been shown to decrease mortality in infections.8
Additional considerations for empiric antibiotic treatment include sensitivities of local microbiologic data, as well as any recent antibiotic regimens given to the patient. Following this broad primary antibiotic coverage, de-escalation was recommended based on results of lower respiratory cultures and clinical improvement.2
Evolution of Diagnostic Criteria and Empiric Antibiotic Coverage
Since the publication of the 2005 ATS/IDSA guidelines, the aforementioned risk factors for HCAP have been brought into question, as they have yet to be validated by prospective trials. There is a growing concern that these criteria may not be adequately specific and, therefore, might call for too many patients to be treated with a broader spectrum of antibiotic coverage, thereby increasing the likelihood of developing MDR bacteria.
In order to further analyze HCAP criteria, Poch and Ost wrote a review earlier this year examining the data behind each of the risk factors cited in the ATS/IDSA guidelines; they found considerable heterogeneity in magnitude of MDR infection risk for these criteria.9 The authors also reviewed studies looking at other risk factors for MDR infections in patients living in nursing homes or afflicted with CAP. They proposed that such additional factors as patient specific risks (including functional status and previous antibiotic exposure) and contextual risks (including nurse-to-patient ratio) be evaluated and possibly incorporated into criteria.
Of all the patients with HCAP criteria, residents in nursing homes have been studied the best. Loeb et al, while looking for a way to decrease hospitalizations for nursing-home residents, showed that patients who get pneumonia (by guideline definition HCAP) can be effectively treated as outpatients with a single antibiotic agent.10 This randomized controlled trial of 680 patients, all with HCAP, were treated with oral levofloxacin at the nursing home or admitted to the hospital. There were no significant differences between mortality (8% vs. 9%) and quality-of-life measures between the two groups. Furthermore, analysis of data from the 1980s showed that nursing-home-acquired pneumonia could be treated effectively with single agents.11,12
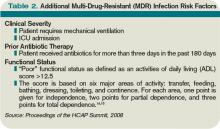
To address some of the questions regarding HCAP, national infectious-disease leaders were brought together to respond to a number of HCAP questions.13 One of the questions centered on the recommended empiric coverage for HCAP. Given the above noted studies in nursing-home patients, disagreement emerged about the need to empirically treat all HCAP patients with broad-spectrum antibiotics. Therefore, another assessment of risk factors for MDR infections was proposed (see Table 2, p. 20) and a consensus was reached, resulting in the current recommendations. The current guidelines state that once a patient has met HCAP criteria, if they have additional MDR risk factors, then broad antibiotic coverage is recommended; however, if no additional MDR risk is found, then more conservative, narrower coverage could be given (see Table 3, p. 31).13
Additional considerations
More studies are needed to refine and validate the specific diagnostic criteria for HCAP, as well as the MDR infectious risk factors. Moreover, current recommendations are for lower respiratory cultures to be obtained on all patients with pneumonia and antibiotic coverage to be titrated according to these results. This practice, however, appears to be uncommon. More data are needed to further guide treatment following initiation of empiric antibiotic coverage without the guidance of culture data, with reliance upon clinical parameters instead.
Back to the Case
This patient met initial criteria for HCAP because he was a nursing home resident, and was found to have additional MDR risk factors (poor functional status and a recent course of antibiotics). Therefore, lower respiratory cultures were obtained, supplemental oxygen was started, and piperacillin/tazobactam plus levofloxacin and vancomycin (with consideration made for local resistance patterns) was administered. He clinically improved over the next two days. His sputum cultures grew Pseudomonas aeuroginosa, which was sensitive to piperacillin/tazobactam but resistant to levofloxacin.
The vancomycin and levofloxacin were discontinued, and he was treated with a seven-day course of piperacillin/tazobactam.
Bottom Line
For adults who present with pneumonia from the community, special attention must be paid to certain parts of the patient’s history to determine if they have HCAP.
Patients who have HCAP can benefit from broad-spectrum empiric antibiotic coverage, which current expert consensus believes is dependent upon further MDR infection risk factors. TH
Dr. Rohde is medicine faculty hospitalist at the University of Michigan in Ann Arbor.
References
- Jernigan JA, Pullen AL, Flowers L, Bell M, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus at the time of hospital admission. Infect Control Hosp Epidemiol. 2003;24(6):409-414.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
- Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(5):3854-3862.
- Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568-3573.
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
- Celis R, Torres A, Gatell JM, Almela M, Rodríguez-Roisin R, Augustí-Vidal A. Nosocomial pneumonia: a multivariate analysis of risk and prognosis. Chest. 1988;93(2):318-324.
- Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J. 2001;18(2):362-368.
- Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31 Supple 4:S131-S138.
- Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30(1):26-35.
- Loeb M, Carusone SC, Goeree R, et al. Effect of clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503-2510.
- Peterson PK, Stein D, Guay DR, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med. 1988;85(2):164-171.
- Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med. 1989(5A);87:116S-118S.
- Kollef MH, Morrow LE, Baughman RP, et al. Healthcare-associated pneumonia (HCAP): a critical appraisal to improve identification, management and outcomes—proceedings of the HCAP summit. Clin Infect Dis. 2008;46 Suppl 4:S296-S334.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919.
- El Solh AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39(4):474-480.
If you are interested in joining our reader-involvement program, e-mail Editor Jason Carris at [email protected].
Case
A 68-year-old man with hypertension, diabetes, and recent hip fracture with poor functional status presents from a nursing home with a productive cough, shortness of breath, and chills of two-day duration. He finished a five-day course of cephalexin for a urinary tract infection one week ago. His vital signs reveal a blood pressure of 162/80 mm/Hg, temperature of 101.9°F, respirations of 26 breaths per minute, and oxygen saturation of 88% on room air. Coarse breath sounds are noted in the right lung field and his chest X-ray reveals a right-middle-lobe infiltrate.
He is admitted to the hospital with a diagnosis of healthcare-associated pneumonia. What is the best empiric antibiotic coverage for this patient?
Overview
Modern medicine exists over a continuum of care that is delivered in a manifold of different settings. Patients routinely receive complex medical care at home, including wound care and infusion of intravenous antibiotics. Additionally, many patients are interfacing with the healthcare system on a regular basis via hemodialysis centers or sub-acute rehabilitation centers. As a result of these interactions, patients are exposed to—and colonized by—different bacterial pathogens that can result in a variety of infections.1
While patients with healthcare-associated pneumonia (HCAP) can present similarly to those with community-acquired pneumonia (CAP)—patients with CAP normally present with a lower-respiratory-tract infection—the differences in the likely etiological pathogens dictate that these patients be considered for broader-spectrum empiric antibiotics. Hospitalists will continue to be responsible for choosing the initial antibiotic regimen for these patients, and they need to be able to recognize this disease process in order to treat it appropriately.
The joint American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) guidelines released in 2005 emphasize that certain clinical HCAP risk factors center on increased interactions and encounters with healthcare facilities.2 These risk factors are evolving over time to include a patient’s functional status, recent antibiotic use, and clinical severity.
Review of the Data
Differences between HCAP and CAP
HCAP represents a diagnostic category of pneumonia created to differentiate patients with infections caused by a different microbiological subset of bacteria, including possible multi-drug-resistant (MDR) organisms, from patients with CAP. Thus far, culture data support this dichotomy.3,4
Kollef and colleagues performed a multicenter, retrospective cohort study of 4,543 patients with bacterial respiratory culture-positive pneumonia between 2002 and 2003. The study examined the bacteriological differences between CAP and HCAP. In this study, HCAP patients were defined as having: transfer from another healthcare facility; long-term hemodialysis; or prior hospitalization within 30 days in which they had non-ventilator-associated pneumonia (VAP). CAP patients were defined as having non-VAP and non-HCAP.
The study showed that the frequency of Pseudomonas aeurginosa (25% HCAP vs. 17% CAP) and Staphylococcus aureus (46% vs. 25%), which included methicillin-resistant Staphylococcus aureus (MRSA) (18% vs. 6%), was significantly higher in patients with HCAP than those with CAP. Additionally, frequency of Streptococcus pneumoniae (5% vs. 16%) and Haemophilus influenza (5% vs. 16%) infections were noted as significantly lower.3
A single-center, retrospective cohort analysis of 639 patients done by Micek et al yielded similar culture differences between CAP and HCAP patients. In this study, criteria for HCAP were defined as hospitalization in the past year, immunosuppression, nursing-home resident, or hemodialysis. The study authors found that a significantly higher percentage of HCAP patients were infected with MRSA (30% vs. 12%), Pseudomonas aeurginosa (25% vs. 4%), and other non-fermenting gram-negative rods (GNR) (10% vs. 2%). HCAP patients again were noted as having significantly fewer infections with S. pneumoniae (10% vs. 40%) and Haemophilus influenza (4% vs. 17%).
In addition to showing a difference in the bacteriology of CAP and HCAP, the Kollef study also evaluated mortality rates, length of stay, and hospital charges. Mortality rates for HCAP (19.8%) were similar to those of hospital-acquired pneumonia (HAP) (18.8%), and both of these were significantly higher than CAP (10%). Length of stay and hospital cost increased across the spectrum, from CAP to HCAP to HAP, with significant differences between each.3
ATS/IDSA Guidelines
In 2005, a joint committee of the ATS and ISDA updated its initial 1996 nosocomial pneumonia guidelines. The guideline update included the new HCAP category.2 The No. 1 goal of these guidelines was to emphasize early and appropriate antibiotics, followed by tailoring of the treatment regimen based upon culture and clinical data. To this end, HCAP risk factors were developed via extrapolation from observational data generated from HAP and VAP patients.5,6,7
The risk factors are summarized in Table 1 (see p. 19).2 Guidelines dictated that the identification of any of these risk factors in pneumonia patients at the time of admission indicates increased risk for infection with an MDR organism. These high-risk patients require placement into the diagnostic category of HCAP.
Once a patient has been diagnosed with HCAP, the guidelines recommended obtaining lower-respiratory-tract cultures and initiating broad-spectrum antibiotic therapy. Appropriate empiric antibiotic therapy was suggested to be the same as for HAP. This regimen requires coverage with two anti-pseudomonal agents, as well as an agent with activity against MRSA.
The rationale behind initial coverage with two anti-pseudomonal agents stems from the finding that pseudomonas has a high rate of resistance to many antibiotics, and that if two agents are empirically started, chances of appropriate coverage increase from the outset. This is important, as timely administration of appropriate antibiotics has been shown to decrease mortality in infections.8
Additional considerations for empiric antibiotic treatment include sensitivities of local microbiologic data, as well as any recent antibiotic regimens given to the patient. Following this broad primary antibiotic coverage, de-escalation was recommended based on results of lower respiratory cultures and clinical improvement.2
Evolution of Diagnostic Criteria and Empiric Antibiotic Coverage
Since the publication of the 2005 ATS/IDSA guidelines, the aforementioned risk factors for HCAP have been brought into question, as they have yet to be validated by prospective trials. There is a growing concern that these criteria may not be adequately specific and, therefore, might call for too many patients to be treated with a broader spectrum of antibiotic coverage, thereby increasing the likelihood of developing MDR bacteria.
In order to further analyze HCAP criteria, Poch and Ost wrote a review earlier this year examining the data behind each of the risk factors cited in the ATS/IDSA guidelines; they found considerable heterogeneity in magnitude of MDR infection risk for these criteria.9 The authors also reviewed studies looking at other risk factors for MDR infections in patients living in nursing homes or afflicted with CAP. They proposed that such additional factors as patient specific risks (including functional status and previous antibiotic exposure) and contextual risks (including nurse-to-patient ratio) be evaluated and possibly incorporated into criteria.
Of all the patients with HCAP criteria, residents in nursing homes have been studied the best. Loeb et al, while looking for a way to decrease hospitalizations for nursing-home residents, showed that patients who get pneumonia (by guideline definition HCAP) can be effectively treated as outpatients with a single antibiotic agent.10 This randomized controlled trial of 680 patients, all with HCAP, were treated with oral levofloxacin at the nursing home or admitted to the hospital. There were no significant differences between mortality (8% vs. 9%) and quality-of-life measures between the two groups. Furthermore, analysis of data from the 1980s showed that nursing-home-acquired pneumonia could be treated effectively with single agents.11,12
To address some of the questions regarding HCAP, national infectious-disease leaders were brought together to respond to a number of HCAP questions.13 One of the questions centered on the recommended empiric coverage for HCAP. Given the above noted studies in nursing-home patients, disagreement emerged about the need to empirically treat all HCAP patients with broad-spectrum antibiotics. Therefore, another assessment of risk factors for MDR infections was proposed (see Table 2, p. 20) and a consensus was reached, resulting in the current recommendations. The current guidelines state that once a patient has met HCAP criteria, if they have additional MDR risk factors, then broad antibiotic coverage is recommended; however, if no additional MDR risk is found, then more conservative, narrower coverage could be given (see Table 3, p. 31).13
Additional considerations
More studies are needed to refine and validate the specific diagnostic criteria for HCAP, as well as the MDR infectious risk factors. Moreover, current recommendations are for lower respiratory cultures to be obtained on all patients with pneumonia and antibiotic coverage to be titrated according to these results. This practice, however, appears to be uncommon. More data are needed to further guide treatment following initiation of empiric antibiotic coverage without the guidance of culture data, with reliance upon clinical parameters instead.
Back to the Case
This patient met initial criteria for HCAP because he was a nursing home resident, and was found to have additional MDR risk factors (poor functional status and a recent course of antibiotics). Therefore, lower respiratory cultures were obtained, supplemental oxygen was started, and piperacillin/tazobactam plus levofloxacin and vancomycin (with consideration made for local resistance patterns) was administered. He clinically improved over the next two days. His sputum cultures grew Pseudomonas aeuroginosa, which was sensitive to piperacillin/tazobactam but resistant to levofloxacin.
The vancomycin and levofloxacin were discontinued, and he was treated with a seven-day course of piperacillin/tazobactam.
Bottom Line
For adults who present with pneumonia from the community, special attention must be paid to certain parts of the patient’s history to determine if they have HCAP.
Patients who have HCAP can benefit from broad-spectrum empiric antibiotic coverage, which current expert consensus believes is dependent upon further MDR infection risk factors. TH
Dr. Rohde is medicine faculty hospitalist at the University of Michigan in Ann Arbor.
References
- Jernigan JA, Pullen AL, Flowers L, Bell M, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus at the time of hospital admission. Infect Control Hosp Epidemiol. 2003;24(6):409-414.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
- Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(5):3854-3862.
- Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568-3573.
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
- Celis R, Torres A, Gatell JM, Almela M, Rodríguez-Roisin R, Augustí-Vidal A. Nosocomial pneumonia: a multivariate analysis of risk and prognosis. Chest. 1988;93(2):318-324.
- Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J. 2001;18(2):362-368.
- Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31 Supple 4:S131-S138.
- Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30(1):26-35.
- Loeb M, Carusone SC, Goeree R, et al. Effect of clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503-2510.
- Peterson PK, Stein D, Guay DR, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med. 1988;85(2):164-171.
- Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med. 1989(5A);87:116S-118S.
- Kollef MH, Morrow LE, Baughman RP, et al. Healthcare-associated pneumonia (HCAP): a critical appraisal to improve identification, management and outcomes—proceedings of the HCAP summit. Clin Infect Dis. 2008;46 Suppl 4:S296-S334.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919.
- El Solh AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39(4):474-480.
If you are interested in joining our reader-involvement program, e-mail Editor Jason Carris at [email protected].
Case
A 68-year-old man with hypertension, diabetes, and recent hip fracture with poor functional status presents from a nursing home with a productive cough, shortness of breath, and chills of two-day duration. He finished a five-day course of cephalexin for a urinary tract infection one week ago. His vital signs reveal a blood pressure of 162/80 mm/Hg, temperature of 101.9°F, respirations of 26 breaths per minute, and oxygen saturation of 88% on room air. Coarse breath sounds are noted in the right lung field and his chest X-ray reveals a right-middle-lobe infiltrate.
He is admitted to the hospital with a diagnosis of healthcare-associated pneumonia. What is the best empiric antibiotic coverage for this patient?
Overview
Modern medicine exists over a continuum of care that is delivered in a manifold of different settings. Patients routinely receive complex medical care at home, including wound care and infusion of intravenous antibiotics. Additionally, many patients are interfacing with the healthcare system on a regular basis via hemodialysis centers or sub-acute rehabilitation centers. As a result of these interactions, patients are exposed to—and colonized by—different bacterial pathogens that can result in a variety of infections.1
While patients with healthcare-associated pneumonia (HCAP) can present similarly to those with community-acquired pneumonia (CAP)—patients with CAP normally present with a lower-respiratory-tract infection—the differences in the likely etiological pathogens dictate that these patients be considered for broader-spectrum empiric antibiotics. Hospitalists will continue to be responsible for choosing the initial antibiotic regimen for these patients, and they need to be able to recognize this disease process in order to treat it appropriately.
The joint American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) guidelines released in 2005 emphasize that certain clinical HCAP risk factors center on increased interactions and encounters with healthcare facilities.2 These risk factors are evolving over time to include a patient’s functional status, recent antibiotic use, and clinical severity.
Review of the Data
Differences between HCAP and CAP
HCAP represents a diagnostic category of pneumonia created to differentiate patients with infections caused by a different microbiological subset of bacteria, including possible multi-drug-resistant (MDR) organisms, from patients with CAP. Thus far, culture data support this dichotomy.3,4
Kollef and colleagues performed a multicenter, retrospective cohort study of 4,543 patients with bacterial respiratory culture-positive pneumonia between 2002 and 2003. The study examined the bacteriological differences between CAP and HCAP. In this study, HCAP patients were defined as having: transfer from another healthcare facility; long-term hemodialysis; or prior hospitalization within 30 days in which they had non-ventilator-associated pneumonia (VAP). CAP patients were defined as having non-VAP and non-HCAP.
The study showed that the frequency of Pseudomonas aeurginosa (25% HCAP vs. 17% CAP) and Staphylococcus aureus (46% vs. 25%), which included methicillin-resistant Staphylococcus aureus (MRSA) (18% vs. 6%), was significantly higher in patients with HCAP than those with CAP. Additionally, frequency of Streptococcus pneumoniae (5% vs. 16%) and Haemophilus influenza (5% vs. 16%) infections were noted as significantly lower.3
A single-center, retrospective cohort analysis of 639 patients done by Micek et al yielded similar culture differences between CAP and HCAP patients. In this study, criteria for HCAP were defined as hospitalization in the past year, immunosuppression, nursing-home resident, or hemodialysis. The study authors found that a significantly higher percentage of HCAP patients were infected with MRSA (30% vs. 12%), Pseudomonas aeurginosa (25% vs. 4%), and other non-fermenting gram-negative rods (GNR) (10% vs. 2%). HCAP patients again were noted as having significantly fewer infections with S. pneumoniae (10% vs. 40%) and Haemophilus influenza (4% vs. 17%).
In addition to showing a difference in the bacteriology of CAP and HCAP, the Kollef study also evaluated mortality rates, length of stay, and hospital charges. Mortality rates for HCAP (19.8%) were similar to those of hospital-acquired pneumonia (HAP) (18.8%), and both of these were significantly higher than CAP (10%). Length of stay and hospital cost increased across the spectrum, from CAP to HCAP to HAP, with significant differences between each.3
ATS/IDSA Guidelines
In 2005, a joint committee of the ATS and ISDA updated its initial 1996 nosocomial pneumonia guidelines. The guideline update included the new HCAP category.2 The No. 1 goal of these guidelines was to emphasize early and appropriate antibiotics, followed by tailoring of the treatment regimen based upon culture and clinical data. To this end, HCAP risk factors were developed via extrapolation from observational data generated from HAP and VAP patients.5,6,7
The risk factors are summarized in Table 1 (see p. 19).2 Guidelines dictated that the identification of any of these risk factors in pneumonia patients at the time of admission indicates increased risk for infection with an MDR organism. These high-risk patients require placement into the diagnostic category of HCAP.
Once a patient has been diagnosed with HCAP, the guidelines recommended obtaining lower-respiratory-tract cultures and initiating broad-spectrum antibiotic therapy. Appropriate empiric antibiotic therapy was suggested to be the same as for HAP. This regimen requires coverage with two anti-pseudomonal agents, as well as an agent with activity against MRSA.
The rationale behind initial coverage with two anti-pseudomonal agents stems from the finding that pseudomonas has a high rate of resistance to many antibiotics, and that if two agents are empirically started, chances of appropriate coverage increase from the outset. This is important, as timely administration of appropriate antibiotics has been shown to decrease mortality in infections.8
Additional considerations for empiric antibiotic treatment include sensitivities of local microbiologic data, as well as any recent antibiotic regimens given to the patient. Following this broad primary antibiotic coverage, de-escalation was recommended based on results of lower respiratory cultures and clinical improvement.2
Evolution of Diagnostic Criteria and Empiric Antibiotic Coverage
Since the publication of the 2005 ATS/IDSA guidelines, the aforementioned risk factors for HCAP have been brought into question, as they have yet to be validated by prospective trials. There is a growing concern that these criteria may not be adequately specific and, therefore, might call for too many patients to be treated with a broader spectrum of antibiotic coverage, thereby increasing the likelihood of developing MDR bacteria.
In order to further analyze HCAP criteria, Poch and Ost wrote a review earlier this year examining the data behind each of the risk factors cited in the ATS/IDSA guidelines; they found considerable heterogeneity in magnitude of MDR infection risk for these criteria.9 The authors also reviewed studies looking at other risk factors for MDR infections in patients living in nursing homes or afflicted with CAP. They proposed that such additional factors as patient specific risks (including functional status and previous antibiotic exposure) and contextual risks (including nurse-to-patient ratio) be evaluated and possibly incorporated into criteria.
Of all the patients with HCAP criteria, residents in nursing homes have been studied the best. Loeb et al, while looking for a way to decrease hospitalizations for nursing-home residents, showed that patients who get pneumonia (by guideline definition HCAP) can be effectively treated as outpatients with a single antibiotic agent.10 This randomized controlled trial of 680 patients, all with HCAP, were treated with oral levofloxacin at the nursing home or admitted to the hospital. There were no significant differences between mortality (8% vs. 9%) and quality-of-life measures between the two groups. Furthermore, analysis of data from the 1980s showed that nursing-home-acquired pneumonia could be treated effectively with single agents.11,12
To address some of the questions regarding HCAP, national infectious-disease leaders were brought together to respond to a number of HCAP questions.13 One of the questions centered on the recommended empiric coverage for HCAP. Given the above noted studies in nursing-home patients, disagreement emerged about the need to empirically treat all HCAP patients with broad-spectrum antibiotics. Therefore, another assessment of risk factors for MDR infections was proposed (see Table 2, p. 20) and a consensus was reached, resulting in the current recommendations. The current guidelines state that once a patient has met HCAP criteria, if they have additional MDR risk factors, then broad antibiotic coverage is recommended; however, if no additional MDR risk is found, then more conservative, narrower coverage could be given (see Table 3, p. 31).13
Additional considerations
More studies are needed to refine and validate the specific diagnostic criteria for HCAP, as well as the MDR infectious risk factors. Moreover, current recommendations are for lower respiratory cultures to be obtained on all patients with pneumonia and antibiotic coverage to be titrated according to these results. This practice, however, appears to be uncommon. More data are needed to further guide treatment following initiation of empiric antibiotic coverage without the guidance of culture data, with reliance upon clinical parameters instead.
Back to the Case
This patient met initial criteria for HCAP because he was a nursing home resident, and was found to have additional MDR risk factors (poor functional status and a recent course of antibiotics). Therefore, lower respiratory cultures were obtained, supplemental oxygen was started, and piperacillin/tazobactam plus levofloxacin and vancomycin (with consideration made for local resistance patterns) was administered. He clinically improved over the next two days. His sputum cultures grew Pseudomonas aeuroginosa, which was sensitive to piperacillin/tazobactam but resistant to levofloxacin.
The vancomycin and levofloxacin were discontinued, and he was treated with a seven-day course of piperacillin/tazobactam.
Bottom Line
For adults who present with pneumonia from the community, special attention must be paid to certain parts of the patient’s history to determine if they have HCAP.
Patients who have HCAP can benefit from broad-spectrum empiric antibiotic coverage, which current expert consensus believes is dependent upon further MDR infection risk factors. TH
Dr. Rohde is medicine faculty hospitalist at the University of Michigan in Ann Arbor.
References
- Jernigan JA, Pullen AL, Flowers L, Bell M, Jarvis WR. Prevalence of and risk factors for colonization with methicillin-resistant Staphylococcus aureus at the time of hospital admission. Infect Control Hosp Epidemiol. 2003;24(6):409-414.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
- Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest. 2005;128(5):3854-3862.
- Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51(10):3568-3573.
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
- Celis R, Torres A, Gatell JM, Almela M, Rodríguez-Roisin R, Augustí-Vidal A. Nosocomial pneumonia: a multivariate analysis of risk and prognosis. Chest. 1988;93(2):318-324.
- Lim WS, Macfarlane JT. A prospective comparison of nursing home acquired pneumonia with community acquired pneumonia. Eur Respir J. 2001;18(2):362-368.
- Kollef MH. Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients. Clin Infect Dis. 2000;31 Supple 4:S131-S138.
- Poch DS, Ost DE. What are the important risk factors for healthcare-associated pneumonia? Semin Respir Crit Care Med. 2009;30(1):26-35.
- Loeb M, Carusone SC, Goeree R, et al. Effect of clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006;295(21):2503-2510.
- Peterson PK, Stein D, Guay DR, et al. Prospective study of lower respiratory tract infections in an extended-care nursing home program: potential role of oral ciprofloxacin. Am J Med. 1988;85(2):164-171.
- Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med. 1989(5A);87:116S-118S.
- Kollef MH, Morrow LE, Baughman RP, et al. Healthcare-associated pneumonia (HCAP): a critical appraisal to improve identification, management and outcomes—proceedings of the HCAP summit. Clin Infect Dis. 2008;46 Suppl 4:S296-S334.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914-919.
- El Solh AA, Pietrantoni C, Bhat A, Bhora M, Berbary E. Indicators of potentially drug-resistant bacteria in severe nursing home-acquired pneumonia. Clin Infect Dis. 2004;39(4):474-480.
If you are interested in joining our reader-involvement program, e-mail Editor Jason Carris at [email protected].