User login
An ankle-brachial index is best for evaluating patients with symptoms of claudication (strength of recommendation [SOR]: B, multiple cohort studies). That said, duplex ultrasonography or magnetic resonance angiography may be a preferable first step if immediate revascularization appears necessary (SOR: C, expert consensus and case reports). In addition, a toe-brachial index may be superior to an ankle-brachial index for evaluating elderly and diabetic patients (SOR: C, expert consensus and case reports).
After considering the accuracy, cost, and risk of available tests, an appropriate stepwise approach begins with a complete history and targeted physical examination (palpation of pulses) (SOR: B, consistent cohort studies); then obtain an ankle-brachial index to confirm the diagnosis.
Ankle-brachial index: An underused test
Vincent Lo, MD
San Joaquin Family Medicine Residency, French Camp, Calif
In my experience, the ankle-brachial index is often underused because of a lack of time, equipment, and proper training. Nonetheless, as the evidence makes clear, this test is the best approach for patients with symptoms of claudication.
Another option you may want to consider is the Edinburgh Claudication Questionnaire (FIGURE). This tool has a strong positive predictive value and positive likelihood ratio and may allow for a presumptive diagnosis, especially among patients with significant risk factors such as diabetes, hypertension, hyperlipidemia, coronary artery disease, and tobacco use. It has limitations, though, which are detailed in this Clinical Inquiry.
For initial management of peripheral vascular disease (PVD), you can recommend lifestyle modification, antiplatelet agents, and aggressive control of blood glucose, blood pressure, and lipids without further testing. Reserve Doppler ultrasound and magnetic resonance angiography for patients who require revascularization or don’t respond to medical therapy.
Evidence summary
PVD is a progressive atherosclerotic narrowing of arteries in the extremities. The prevalence increases with age—it is less than 1% in people between 40 and 49 years of age and 15% in people 70 years and older.1,2 Risk factors are the same as for coronary artery disease.1
Weighing your options
Methods for evaluating patients for PVD include medical history, physical examination (inspection of the extremities and palpation of peripheral pulses), and ancillary testing (ankle-brachial index, duplex ultrasound, and magnetic resonance imaging with contrast, and angiography). The toe-brachial index may be useful in the elderly and patients with advanced diabetes because noncompressible vasculature in these patients may render the ankle-brachial index unreliable.3
1. Do you get a pain or discomfort in your leg(s) when you walk?
□ Yes □ No □ I am unable to walk
If you answered “Yes” to question (1), please answer the following questions. Otherwise, you need not continue.
2. Does this pain ever begin when you are standing still or sitting?
□ Yes □ No
3. Do you get it if you walk uphill or hurry?
□ Yes □ No
4. Do you get it when you walk at an ordinary pace on the level?
□ Yes □ No
5. What happens to it if you stand still?
□ Usually continues more than 10 minutes.
□ Usually disappears in 10 minutes or less.
6. Where do you get this pain or discomfort?
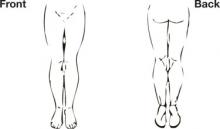
Mark the place(s) with an “x” on the diagram below.
Definition of positive classification requires all of the following responses: “Yes” to (1), “No” to (2), “Yes” to (3), and “usually disappears in 10 minutes or less” to (5); grade 1=“No” to (4) and grade 2=“Yes” to (4). If these criteria are fulfilled, a definite claudicant is one who indicates pain in the calf, regardless of whether pain is also marked in other sites; a diagnosis of atypical claudication is made if pain is indicated in the thigh or buttock, in the absence of any calf pain. Patients should not be considered to have claudication if pain is indicated in the hamstrings, feet, shins, joints, or appears to radiate, in the absence of any pain in the calf.
Source: Leng GC, Fowkes FG.4 Adapted with permission.
The TABLE lists the sensitivities, specificities, positive predictive values, and likelihood ratios for commonly used tests.3-8 The calculations assume peripheral vascular disease to have a prevalence of 14% among people older than 60 years, based on pooled results from several epidemiologic studies.1
A questionnaire-based history of claudication (the Edinburgh Claudication Questionnaire) has been shown to have a high positive predictive value and likelihood ratio for PVD; physical examination techniques appear to be less predictive.4-7 However, the gold standard in the questionnaire study was “clinician determination,” which carries a risk of subjectivity and lack of testing independence that may make the test appear more accurate than it is in typical application.
A stepwise approach
After balancing the accuracy, cost, and risk of available tests, an appropriate stepwise approach to evaluation for PVD is:
First, do a complete history and targeted physical examination (palpation of pulses).
Next, obtain an ankle-brachial index to confirm the diagnosis.
Then, proceed directly to either duplex ultrasonography or magnetic resonance angiography when revascularization is clearly needed.9
TABLE
Commonly used tests for peripheral vascular disease
| TEST | COMPARISON/STANDARD | SENSITIVITY % (95% CI, IF REPORTED) | SENSITIVITY % (95% CI, IF REPORTED) | SPECIFICITY % (95% CI, IF REPORTED) | PPV* | LR- | LR+ | REIMBURSEMENT ESTIMATE† |
|---|---|---|---|---|---|---|---|---|
| MEDICAL HISTORY | CPT CODE | ESTIMATED COST | ||||||
| Edinburgh Claudication Questionnaire4 | Claudication by clinician assessment | 91.0 (88.1-94.5) | 99.0 (98.9-100.0) | 0.955 | 0.09 | 91.0 | 99203 | $87.29 |
| PHYSICAL EXAMINATION | ||||||||
| Color abnormality of extremity skin (pale, red, or blue)5 | ABI<0.9 | 35.0 | 87.0 | 0.305 | 0.75 | 2.7 | 99203 | $87.29 |
| Cool skin unilaterally5 | ABI<0.9 | 10.0 | 98.0 | 0.449 | 0.92 | 5.0 | 99203 | $87.29 |
| Any abnormal pulse by palpation6 | Multiple criteria‡ | 76.9 | 86.4 | 0.479 | 0.27 | 5.7 | 99203 | $87.29 |
| Presence of femoral bruit6 | Multiple criteria‡ | 20.0 | 95.7 | 0.431 | 0.84 | 4.7 | 99203 | $87.29 |
| Absent pedal pulses (dorsalis pedis and posterior tibial)7 | ABI<0.9 | 63.0 | 99.0 | 0.912 | 0.37 | 63.9 | 99203 | $87.29 |
| LABORATORY INVESTIGATIONS | ||||||||
| ABI <0.93 | Conventional angiography | 79.0 | 96.0 | 0.763 | 0.22 | 19.8 | 93923 | $165.18 |
| Duplex ultrasound8 | Conventional angiography | 87.6 (84.4-90.8) | 94.7 (93.2-96.2) | 0.729 | 0.13 | 16.5 | 93923 | $165.18 |
| Gadolinium-enhanced magnetic resonance angiography8 | Conventional angiographyy | 97.5 (95.7-99.3) | 96.2 (94.4-97.9) | 0.807 | 0.03 | 25.7 | 73725 | $504.00 |
| ABI, ankle-brachial index; CI, confidence interval; LR, likelihood ratio; PPV, positive predictive value. | ||||||||
| *Based on a prevalence of peripheral vascular disease of 14% (Pasternak RC et al1). | ||||||||
| † Based on estimated Medicare-approved CPT reimbursement rates, https://catalog.ama-assn.org/Catalog/cpt/cpt_search.jsp. Accessed December 2, 2007. History and physical items based on a new-patient visit of moderate complexity, CPT Code 99203. Cost estimate for conventional invasive angiography (angiography, extremity, unilateral, radiological supervision and interpretation, CPT Code 75710) $426.14 (Downstate Illinois estimates). | ||||||||
| ‡ Multiple criteria = segmental blood pressure, flow velocity by Doppler, postocclusive reactive hyperemia, pulse reappearance half-time, small or large vessel peripheral arterial disease, and surgery. | ||||||||
The major advantages of the ankle-brachial index include low cost and non-invasiveness (low potential for harm). However, it doesn’t detect proximal aneurysms or PVD distal to the ankle, and it may be difficult to perform on patients with noncompressible distal vasculature. Adequately evaluating such patients may require invasive testing.
Recommendations
The US Preventive Services Task Force recommends against (D recommendation) any screening tests for PVD in patients without symptoms.10 The American College of Cardiology gives a class I recommendation (tests for which there is evidence or general agreement that a procedure is useful, beneficial, or effective) to the ankle-brachial index as the baseline diagnostic tool for establishing peripheral vascular disease, except in elderly patients or those with advanced diabetes, for whom the test is unreliable.11
1. Pasternak RC, Criqui MH, Benjamin EJ, et al. Atherosclerotic Vascular Disease Conference: Writing Group I: Epidemiology. Circulation. 2004;109:2605-2612.
2. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110:738-743.
3. American College of Cardiology, American Heart Association. ACC/AHA 2005 Practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report. Circulation. 2006;113:e463-654.
4. Leng GC, Fowkes FG. The Edinburgh Claudication Questionnaire: an improved version of the WHO/Rose Questionnaire for use in epidemiological surveys. J Clin Epidemiol. 1992;45:1101-1109.
5. Stoffers HE, Kester AD, Kaiser V, et al. Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach. Med Decis Making. 1997;17:61-70.
6. Criqui MH, Fronek A, Klauber MR, et al. The sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from noninvasive testing in a defined population. Circulation 1985;71:516-522.
7. McGee SR, Boyko EJ. Physical examination and chronic lower-extremity ischemia: a critical review. Arch Intern Med. 1998;158:1357-1364.
8. Visser K, Myriam Hunink MG. Peripheral arterial disease: gadolinium-enhanced MR angiography versus color-guided duplex US-A meta-analysis. Radiology. 2000;216:67-77.
9. Sondtheimer DL. Peripheral vascular disease: diagnosis and treatment. Am Fam Physician. 2006;73:1971-1976.
10. US Preventive Services Task Force. Screening for Peripheral Vascular Disease: Recommendation Statement. Rockville, MD: Agency for Healthcare Research and Quality; August, 2005.
11. American College of Cardiology, American Heart Association. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic). Circulation. 2006;113:1474-1547.
An ankle-brachial index is best for evaluating patients with symptoms of claudication (strength of recommendation [SOR]: B, multiple cohort studies). That said, duplex ultrasonography or magnetic resonance angiography may be a preferable first step if immediate revascularization appears necessary (SOR: C, expert consensus and case reports). In addition, a toe-brachial index may be superior to an ankle-brachial index for evaluating elderly and diabetic patients (SOR: C, expert consensus and case reports).
After considering the accuracy, cost, and risk of available tests, an appropriate stepwise approach begins with a complete history and targeted physical examination (palpation of pulses) (SOR: B, consistent cohort studies); then obtain an ankle-brachial index to confirm the diagnosis.
Ankle-brachial index: An underused test
Vincent Lo, MD
San Joaquin Family Medicine Residency, French Camp, Calif
In my experience, the ankle-brachial index is often underused because of a lack of time, equipment, and proper training. Nonetheless, as the evidence makes clear, this test is the best approach for patients with symptoms of claudication.
Another option you may want to consider is the Edinburgh Claudication Questionnaire (FIGURE). This tool has a strong positive predictive value and positive likelihood ratio and may allow for a presumptive diagnosis, especially among patients with significant risk factors such as diabetes, hypertension, hyperlipidemia, coronary artery disease, and tobacco use. It has limitations, though, which are detailed in this Clinical Inquiry.
For initial management of peripheral vascular disease (PVD), you can recommend lifestyle modification, antiplatelet agents, and aggressive control of blood glucose, blood pressure, and lipids without further testing. Reserve Doppler ultrasound and magnetic resonance angiography for patients who require revascularization or don’t respond to medical therapy.
Evidence summary
PVD is a progressive atherosclerotic narrowing of arteries in the extremities. The prevalence increases with age—it is less than 1% in people between 40 and 49 years of age and 15% in people 70 years and older.1,2 Risk factors are the same as for coronary artery disease.1
Weighing your options
Methods for evaluating patients for PVD include medical history, physical examination (inspection of the extremities and palpation of peripheral pulses), and ancillary testing (ankle-brachial index, duplex ultrasound, and magnetic resonance imaging with contrast, and angiography). The toe-brachial index may be useful in the elderly and patients with advanced diabetes because noncompressible vasculature in these patients may render the ankle-brachial index unreliable.3
1. Do you get a pain or discomfort in your leg(s) when you walk?
□ Yes □ No □ I am unable to walk
If you answered “Yes” to question (1), please answer the following questions. Otherwise, you need not continue.
2. Does this pain ever begin when you are standing still or sitting?
□ Yes □ No
3. Do you get it if you walk uphill or hurry?
□ Yes □ No
4. Do you get it when you walk at an ordinary pace on the level?
□ Yes □ No
5. What happens to it if you stand still?
□ Usually continues more than 10 minutes.
□ Usually disappears in 10 minutes or less.
6. Where do you get this pain or discomfort?
Mark the place(s) with an “x” on the diagram below.
Definition of positive classification requires all of the following responses: “Yes” to (1), “No” to (2), “Yes” to (3), and “usually disappears in 10 minutes or less” to (5); grade 1=“No” to (4) and grade 2=“Yes” to (4). If these criteria are fulfilled, a definite claudicant is one who indicates pain in the calf, regardless of whether pain is also marked in other sites; a diagnosis of atypical claudication is made if pain is indicated in the thigh or buttock, in the absence of any calf pain. Patients should not be considered to have claudication if pain is indicated in the hamstrings, feet, shins, joints, or appears to radiate, in the absence of any pain in the calf.
Source: Leng GC, Fowkes FG.4 Adapted with permission.
The TABLE lists the sensitivities, specificities, positive predictive values, and likelihood ratios for commonly used tests.3-8 The calculations assume peripheral vascular disease to have a prevalence of 14% among people older than 60 years, based on pooled results from several epidemiologic studies.1
A questionnaire-based history of claudication (the Edinburgh Claudication Questionnaire) has been shown to have a high positive predictive value and likelihood ratio for PVD; physical examination techniques appear to be less predictive.4-7 However, the gold standard in the questionnaire study was “clinician determination,” which carries a risk of subjectivity and lack of testing independence that may make the test appear more accurate than it is in typical application.
A stepwise approach
After balancing the accuracy, cost, and risk of available tests, an appropriate stepwise approach to evaluation for PVD is:
First, do a complete history and targeted physical examination (palpation of pulses).
Next, obtain an ankle-brachial index to confirm the diagnosis.
Then, proceed directly to either duplex ultrasonography or magnetic resonance angiography when revascularization is clearly needed.9
TABLE
Commonly used tests for peripheral vascular disease
| TEST | COMPARISON/STANDARD | SENSITIVITY % (95% CI, IF REPORTED) | SENSITIVITY % (95% CI, IF REPORTED) | SPECIFICITY % (95% CI, IF REPORTED) | PPV* | LR- | LR+ | REIMBURSEMENT ESTIMATE† |
|---|---|---|---|---|---|---|---|---|
| MEDICAL HISTORY | CPT CODE | ESTIMATED COST | ||||||
| Edinburgh Claudication Questionnaire4 | Claudication by clinician assessment | 91.0 (88.1-94.5) | 99.0 (98.9-100.0) | 0.955 | 0.09 | 91.0 | 99203 | $87.29 |
| PHYSICAL EXAMINATION | ||||||||
| Color abnormality of extremity skin (pale, red, or blue)5 | ABI<0.9 | 35.0 | 87.0 | 0.305 | 0.75 | 2.7 | 99203 | $87.29 |
| Cool skin unilaterally5 | ABI<0.9 | 10.0 | 98.0 | 0.449 | 0.92 | 5.0 | 99203 | $87.29 |
| Any abnormal pulse by palpation6 | Multiple criteria‡ | 76.9 | 86.4 | 0.479 | 0.27 | 5.7 | 99203 | $87.29 |
| Presence of femoral bruit6 | Multiple criteria‡ | 20.0 | 95.7 | 0.431 | 0.84 | 4.7 | 99203 | $87.29 |
| Absent pedal pulses (dorsalis pedis and posterior tibial)7 | ABI<0.9 | 63.0 | 99.0 | 0.912 | 0.37 | 63.9 | 99203 | $87.29 |
| LABORATORY INVESTIGATIONS | ||||||||
| ABI <0.93 | Conventional angiography | 79.0 | 96.0 | 0.763 | 0.22 | 19.8 | 93923 | $165.18 |
| Duplex ultrasound8 | Conventional angiography | 87.6 (84.4-90.8) | 94.7 (93.2-96.2) | 0.729 | 0.13 | 16.5 | 93923 | $165.18 |
| Gadolinium-enhanced magnetic resonance angiography8 | Conventional angiographyy | 97.5 (95.7-99.3) | 96.2 (94.4-97.9) | 0.807 | 0.03 | 25.7 | 73725 | $504.00 |
| ABI, ankle-brachial index; CI, confidence interval; LR, likelihood ratio; PPV, positive predictive value. | ||||||||
| *Based on a prevalence of peripheral vascular disease of 14% (Pasternak RC et al1). | ||||||||
| † Based on estimated Medicare-approved CPT reimbursement rates, https://catalog.ama-assn.org/Catalog/cpt/cpt_search.jsp. Accessed December 2, 2007. History and physical items based on a new-patient visit of moderate complexity, CPT Code 99203. Cost estimate for conventional invasive angiography (angiography, extremity, unilateral, radiological supervision and interpretation, CPT Code 75710) $426.14 (Downstate Illinois estimates). | ||||||||
| ‡ Multiple criteria = segmental blood pressure, flow velocity by Doppler, postocclusive reactive hyperemia, pulse reappearance half-time, small or large vessel peripheral arterial disease, and surgery. | ||||||||
The major advantages of the ankle-brachial index include low cost and non-invasiveness (low potential for harm). However, it doesn’t detect proximal aneurysms or PVD distal to the ankle, and it may be difficult to perform on patients with noncompressible distal vasculature. Adequately evaluating such patients may require invasive testing.
Recommendations
The US Preventive Services Task Force recommends against (D recommendation) any screening tests for PVD in patients without symptoms.10 The American College of Cardiology gives a class I recommendation (tests for which there is evidence or general agreement that a procedure is useful, beneficial, or effective) to the ankle-brachial index as the baseline diagnostic tool for establishing peripheral vascular disease, except in elderly patients or those with advanced diabetes, for whom the test is unreliable.11
An ankle-brachial index is best for evaluating patients with symptoms of claudication (strength of recommendation [SOR]: B, multiple cohort studies). That said, duplex ultrasonography or magnetic resonance angiography may be a preferable first step if immediate revascularization appears necessary (SOR: C, expert consensus and case reports). In addition, a toe-brachial index may be superior to an ankle-brachial index for evaluating elderly and diabetic patients (SOR: C, expert consensus and case reports).
After considering the accuracy, cost, and risk of available tests, an appropriate stepwise approach begins with a complete history and targeted physical examination (palpation of pulses) (SOR: B, consistent cohort studies); then obtain an ankle-brachial index to confirm the diagnosis.
Ankle-brachial index: An underused test
Vincent Lo, MD
San Joaquin Family Medicine Residency, French Camp, Calif
In my experience, the ankle-brachial index is often underused because of a lack of time, equipment, and proper training. Nonetheless, as the evidence makes clear, this test is the best approach for patients with symptoms of claudication.
Another option you may want to consider is the Edinburgh Claudication Questionnaire (FIGURE). This tool has a strong positive predictive value and positive likelihood ratio and may allow for a presumptive diagnosis, especially among patients with significant risk factors such as diabetes, hypertension, hyperlipidemia, coronary artery disease, and tobacco use. It has limitations, though, which are detailed in this Clinical Inquiry.
For initial management of peripheral vascular disease (PVD), you can recommend lifestyle modification, antiplatelet agents, and aggressive control of blood glucose, blood pressure, and lipids without further testing. Reserve Doppler ultrasound and magnetic resonance angiography for patients who require revascularization or don’t respond to medical therapy.
Evidence summary
PVD is a progressive atherosclerotic narrowing of arteries in the extremities. The prevalence increases with age—it is less than 1% in people between 40 and 49 years of age and 15% in people 70 years and older.1,2 Risk factors are the same as for coronary artery disease.1
Weighing your options
Methods for evaluating patients for PVD include medical history, physical examination (inspection of the extremities and palpation of peripheral pulses), and ancillary testing (ankle-brachial index, duplex ultrasound, and magnetic resonance imaging with contrast, and angiography). The toe-brachial index may be useful in the elderly and patients with advanced diabetes because noncompressible vasculature in these patients may render the ankle-brachial index unreliable.3
1. Do you get a pain or discomfort in your leg(s) when you walk?
□ Yes □ No □ I am unable to walk
If you answered “Yes” to question (1), please answer the following questions. Otherwise, you need not continue.
2. Does this pain ever begin when you are standing still or sitting?
□ Yes □ No
3. Do you get it if you walk uphill or hurry?
□ Yes □ No
4. Do you get it when you walk at an ordinary pace on the level?
□ Yes □ No
5. What happens to it if you stand still?
□ Usually continues more than 10 minutes.
□ Usually disappears in 10 minutes or less.
6. Where do you get this pain or discomfort?
Mark the place(s) with an “x” on the diagram below.
Definition of positive classification requires all of the following responses: “Yes” to (1), “No” to (2), “Yes” to (3), and “usually disappears in 10 minutes or less” to (5); grade 1=“No” to (4) and grade 2=“Yes” to (4). If these criteria are fulfilled, a definite claudicant is one who indicates pain in the calf, regardless of whether pain is also marked in other sites; a diagnosis of atypical claudication is made if pain is indicated in the thigh or buttock, in the absence of any calf pain. Patients should not be considered to have claudication if pain is indicated in the hamstrings, feet, shins, joints, or appears to radiate, in the absence of any pain in the calf.
Source: Leng GC, Fowkes FG.4 Adapted with permission.
The TABLE lists the sensitivities, specificities, positive predictive values, and likelihood ratios for commonly used tests.3-8 The calculations assume peripheral vascular disease to have a prevalence of 14% among people older than 60 years, based on pooled results from several epidemiologic studies.1
A questionnaire-based history of claudication (the Edinburgh Claudication Questionnaire) has been shown to have a high positive predictive value and likelihood ratio for PVD; physical examination techniques appear to be less predictive.4-7 However, the gold standard in the questionnaire study was “clinician determination,” which carries a risk of subjectivity and lack of testing independence that may make the test appear more accurate than it is in typical application.
A stepwise approach
After balancing the accuracy, cost, and risk of available tests, an appropriate stepwise approach to evaluation for PVD is:
First, do a complete history and targeted physical examination (palpation of pulses).
Next, obtain an ankle-brachial index to confirm the diagnosis.
Then, proceed directly to either duplex ultrasonography or magnetic resonance angiography when revascularization is clearly needed.9
TABLE
Commonly used tests for peripheral vascular disease
| TEST | COMPARISON/STANDARD | SENSITIVITY % (95% CI, IF REPORTED) | SENSITIVITY % (95% CI, IF REPORTED) | SPECIFICITY % (95% CI, IF REPORTED) | PPV* | LR- | LR+ | REIMBURSEMENT ESTIMATE† |
|---|---|---|---|---|---|---|---|---|
| MEDICAL HISTORY | CPT CODE | ESTIMATED COST | ||||||
| Edinburgh Claudication Questionnaire4 | Claudication by clinician assessment | 91.0 (88.1-94.5) | 99.0 (98.9-100.0) | 0.955 | 0.09 | 91.0 | 99203 | $87.29 |
| PHYSICAL EXAMINATION | ||||||||
| Color abnormality of extremity skin (pale, red, or blue)5 | ABI<0.9 | 35.0 | 87.0 | 0.305 | 0.75 | 2.7 | 99203 | $87.29 |
| Cool skin unilaterally5 | ABI<0.9 | 10.0 | 98.0 | 0.449 | 0.92 | 5.0 | 99203 | $87.29 |
| Any abnormal pulse by palpation6 | Multiple criteria‡ | 76.9 | 86.4 | 0.479 | 0.27 | 5.7 | 99203 | $87.29 |
| Presence of femoral bruit6 | Multiple criteria‡ | 20.0 | 95.7 | 0.431 | 0.84 | 4.7 | 99203 | $87.29 |
| Absent pedal pulses (dorsalis pedis and posterior tibial)7 | ABI<0.9 | 63.0 | 99.0 | 0.912 | 0.37 | 63.9 | 99203 | $87.29 |
| LABORATORY INVESTIGATIONS | ||||||||
| ABI <0.93 | Conventional angiography | 79.0 | 96.0 | 0.763 | 0.22 | 19.8 | 93923 | $165.18 |
| Duplex ultrasound8 | Conventional angiography | 87.6 (84.4-90.8) | 94.7 (93.2-96.2) | 0.729 | 0.13 | 16.5 | 93923 | $165.18 |
| Gadolinium-enhanced magnetic resonance angiography8 | Conventional angiographyy | 97.5 (95.7-99.3) | 96.2 (94.4-97.9) | 0.807 | 0.03 | 25.7 | 73725 | $504.00 |
| ABI, ankle-brachial index; CI, confidence interval; LR, likelihood ratio; PPV, positive predictive value. | ||||||||
| *Based on a prevalence of peripheral vascular disease of 14% (Pasternak RC et al1). | ||||||||
| † Based on estimated Medicare-approved CPT reimbursement rates, https://catalog.ama-assn.org/Catalog/cpt/cpt_search.jsp. Accessed December 2, 2007. History and physical items based on a new-patient visit of moderate complexity, CPT Code 99203. Cost estimate for conventional invasive angiography (angiography, extremity, unilateral, radiological supervision and interpretation, CPT Code 75710) $426.14 (Downstate Illinois estimates). | ||||||||
| ‡ Multiple criteria = segmental blood pressure, flow velocity by Doppler, postocclusive reactive hyperemia, pulse reappearance half-time, small or large vessel peripheral arterial disease, and surgery. | ||||||||
The major advantages of the ankle-brachial index include low cost and non-invasiveness (low potential for harm). However, it doesn’t detect proximal aneurysms or PVD distal to the ankle, and it may be difficult to perform on patients with noncompressible distal vasculature. Adequately evaluating such patients may require invasive testing.
Recommendations
The US Preventive Services Task Force recommends against (D recommendation) any screening tests for PVD in patients without symptoms.10 The American College of Cardiology gives a class I recommendation (tests for which there is evidence or general agreement that a procedure is useful, beneficial, or effective) to the ankle-brachial index as the baseline diagnostic tool for establishing peripheral vascular disease, except in elderly patients or those with advanced diabetes, for whom the test is unreliable.11
1. Pasternak RC, Criqui MH, Benjamin EJ, et al. Atherosclerotic Vascular Disease Conference: Writing Group I: Epidemiology. Circulation. 2004;109:2605-2612.
2. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110:738-743.
3. American College of Cardiology, American Heart Association. ACC/AHA 2005 Practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report. Circulation. 2006;113:e463-654.
4. Leng GC, Fowkes FG. The Edinburgh Claudication Questionnaire: an improved version of the WHO/Rose Questionnaire for use in epidemiological surveys. J Clin Epidemiol. 1992;45:1101-1109.
5. Stoffers HE, Kester AD, Kaiser V, et al. Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach. Med Decis Making. 1997;17:61-70.
6. Criqui MH, Fronek A, Klauber MR, et al. The sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from noninvasive testing in a defined population. Circulation 1985;71:516-522.
7. McGee SR, Boyko EJ. Physical examination and chronic lower-extremity ischemia: a critical review. Arch Intern Med. 1998;158:1357-1364.
8. Visser K, Myriam Hunink MG. Peripheral arterial disease: gadolinium-enhanced MR angiography versus color-guided duplex US-A meta-analysis. Radiology. 2000;216:67-77.
9. Sondtheimer DL. Peripheral vascular disease: diagnosis and treatment. Am Fam Physician. 2006;73:1971-1976.
10. US Preventive Services Task Force. Screening for Peripheral Vascular Disease: Recommendation Statement. Rockville, MD: Agency for Healthcare Research and Quality; August, 2005.
11. American College of Cardiology, American Heart Association. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic). Circulation. 2006;113:1474-1547.
1. Pasternak RC, Criqui MH, Benjamin EJ, et al. Atherosclerotic Vascular Disease Conference: Writing Group I: Epidemiology. Circulation. 2004;109:2605-2612.
2. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110:738-743.
3. American College of Cardiology, American Heart Association. ACC/AHA 2005 Practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report. Circulation. 2006;113:e463-654.
4. Leng GC, Fowkes FG. The Edinburgh Claudication Questionnaire: an improved version of the WHO/Rose Questionnaire for use in epidemiological surveys. J Clin Epidemiol. 1992;45:1101-1109.
5. Stoffers HE, Kester AD, Kaiser V, et al. Diagnostic value of signs and symptoms associated with peripheral arterial occlusive disease seen in general practice: a multivariable approach. Med Decis Making. 1997;17:61-70.
6. Criqui MH, Fronek A, Klauber MR, et al. The sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from noninvasive testing in a defined population. Circulation 1985;71:516-522.
7. McGee SR, Boyko EJ. Physical examination and chronic lower-extremity ischemia: a critical review. Arch Intern Med. 1998;158:1357-1364.
8. Visser K, Myriam Hunink MG. Peripheral arterial disease: gadolinium-enhanced MR angiography versus color-guided duplex US-A meta-analysis. Radiology. 2000;216:67-77.
9. Sondtheimer DL. Peripheral vascular disease: diagnosis and treatment. Am Fam Physician. 2006;73:1971-1976.
10. US Preventive Services Task Force. Screening for Peripheral Vascular Disease: Recommendation Statement. Rockville, MD: Agency for Healthcare Research and Quality; August, 2005.
11. American College of Cardiology, American Heart Association. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic). Circulation. 2006;113:1474-1547.
Evidence-based answers from the Family Physicians Inquiries Network