User login
Aseptic abscesses syndrome
The clinical presentation with cervical feverish lymphadenopathy in a patient who underwent anti–tumor necrosis factor-alpha therapy was worrisome and suggestive of tuberculosis lymphadenitis. However, the ineffective antituberculosis treatment and the negative exploration for an etiology instead suggested another pathologic process. After antituberculosis treatment and because repeated negative results came from extensive searches for an infectious cause, a corticoid treatment was subsequently initiated. The clinical response was quick, with apyrexia, diminution of C-reactive protein at 10 mg/L, disappearance of the swelling, and complete healing of the fistula in 3 weeks (Figures E, F). This response to steroid treatment suggested an autoinflammatory pathologic process. Histology with epithelioid cell granuloma could evoke metastatic Crohn’s disease. However, this hypothesis was unlikely in this case because inside the granuloma was spotted noncaseous necrosis, and because symptoms occurred under infliximab treatment while the disease was well-controlled throughout the period in question. Furthermore, metastatic Crohn’s disease is usually localized in skin creases, such as the submammary fold, inguinal areas, and abdominal skinfold creases.1 In addition, we are not aware of any lymph node involvement described in literature.
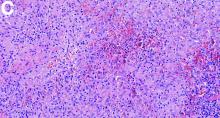
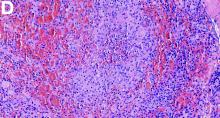
Aseptic abscesses syndrome is a rare condition associated with Crohn’s disease first described in 1995 by André et al.2 Aseptic abscesses syndrome is an autoinflammatory disease involving neutrophils that is characterized by disseminated sterile purulent collections. An inflammatory bowel disease is associated in 70% of the cases.3 Aseptic abscesses are generally located in the spleen (90% of cases) and abdominal lymph nodes, but can also affect the liver, lung, pancreas, and superficial lymph nodes.3 Repeated bacteriologic tests are always negative. Fever is the most frequent clinical feature (90%) and persists despite antibiotic therapy, whereas symptoms can vary depending on the aseptic abscesses localization. Biochemical tests show an increased CRP and leukocyte count. Histologically, aseptic abscesses are well-limited nodular lesions measuring from a few millimeters to 7 cm and containing white pus. These abscesses are surrounded by epithelioid cell granulomatous reaction, inside of which can be found a noncaseous necrosis, unlike tuberculosis. Specific colorations are negative as well (Ziehl, periodic acid-Schiff, Grocott, and Whartin-Starry).
In subcutaneous node involvement, the main differential diagnosis is pyoderma gangrenosum, but abscesses are not surrounded by granulomatosis reaction in pyoderma gangrenosum. Limited forms can be treated by colchicine, thalidomide, or dapsone, but steroid therapy is almost always necessary, with a consistently favorable evolution. However, relapses occur in two-thirds of cases.
In conclusion, aseptic abscesses syndrome is a diagnosis of exclusion, which is rare and should be considered in a patient known for inflammatory bowel disease who develops fever and deep abscesses with negative results on repeated searches for infectious causes.3
References
1. Guest G.D. Fink R.L.W. Metastatic Crohn’s disease: case report of an unusual variant and review of the literature. Dis Colon Rectum. 2000;43:1764–6.
2. André M., Aumaitre O., Marcheix J.C. et al. Unexplained sterile systemic abscesses in Crohn’s disease: aseptic abscesses as a new entity. Am J Gastroenterol. 1995;90:1183–4.
3. André M.F.J., Piette J.-C., Kémény J.-L. et al. Aseptic abscesses: a study of 30 patients with or without inflammatory bowel disease and review of the literature. Medicine (Baltimore). 2007;86:145–61.
Aseptic abscesses syndrome
The clinical presentation with cervical feverish lymphadenopathy in a patient who underwent anti–tumor necrosis factor-alpha therapy was worrisome and suggestive of tuberculosis lymphadenitis. However, the ineffective antituberculosis treatment and the negative exploration for an etiology instead suggested another pathologic process. After antituberculosis treatment and because repeated negative results came from extensive searches for an infectious cause, a corticoid treatment was subsequently initiated. The clinical response was quick, with apyrexia, diminution of C-reactive protein at 10 mg/L, disappearance of the swelling, and complete healing of the fistula in 3 weeks (Figures E, F). This response to steroid treatment suggested an autoinflammatory pathologic process. Histology with epithelioid cell granuloma could evoke metastatic Crohn’s disease. However, this hypothesis was unlikely in this case because inside the granuloma was spotted noncaseous necrosis, and because symptoms occurred under infliximab treatment while the disease was well-controlled throughout the period in question. Furthermore, metastatic Crohn’s disease is usually localized in skin creases, such as the submammary fold, inguinal areas, and abdominal skinfold creases.1 In addition, we are not aware of any lymph node involvement described in literature.
Aseptic abscesses syndrome is a rare condition associated with Crohn’s disease first described in 1995 by André et al.2 Aseptic abscesses syndrome is an autoinflammatory disease involving neutrophils that is characterized by disseminated sterile purulent collections. An inflammatory bowel disease is associated in 70% of the cases.3 Aseptic abscesses are generally located in the spleen (90% of cases) and abdominal lymph nodes, but can also affect the liver, lung, pancreas, and superficial lymph nodes.3 Repeated bacteriologic tests are always negative. Fever is the most frequent clinical feature (90%) and persists despite antibiotic therapy, whereas symptoms can vary depending on the aseptic abscesses localization. Biochemical tests show an increased CRP and leukocyte count. Histologically, aseptic abscesses are well-limited nodular lesions measuring from a few millimeters to 7 cm and containing white pus. These abscesses are surrounded by epithelioid cell granulomatous reaction, inside of which can be found a noncaseous necrosis, unlike tuberculosis. Specific colorations are negative as well (Ziehl, periodic acid-Schiff, Grocott, and Whartin-Starry).
In subcutaneous node involvement, the main differential diagnosis is pyoderma gangrenosum, but abscesses are not surrounded by granulomatosis reaction in pyoderma gangrenosum. Limited forms can be treated by colchicine, thalidomide, or dapsone, but steroid therapy is almost always necessary, with a consistently favorable evolution. However, relapses occur in two-thirds of cases.
In conclusion, aseptic abscesses syndrome is a diagnosis of exclusion, which is rare and should be considered in a patient known for inflammatory bowel disease who develops fever and deep abscesses with negative results on repeated searches for infectious causes.3
References
1. Guest G.D. Fink R.L.W. Metastatic Crohn’s disease: case report of an unusual variant and review of the literature. Dis Colon Rectum. 2000;43:1764–6.
2. André M., Aumaitre O., Marcheix J.C. et al. Unexplained sterile systemic abscesses in Crohn’s disease: aseptic abscesses as a new entity. Am J Gastroenterol. 1995;90:1183–4.
3. André M.F.J., Piette J.-C., Kémény J.-L. et al. Aseptic abscesses: a study of 30 patients with or without inflammatory bowel disease and review of the literature. Medicine (Baltimore). 2007;86:145–61.
Aseptic abscesses syndrome
The clinical presentation with cervical feverish lymphadenopathy in a patient who underwent anti–tumor necrosis factor-alpha therapy was worrisome and suggestive of tuberculosis lymphadenitis. However, the ineffective antituberculosis treatment and the negative exploration for an etiology instead suggested another pathologic process. After antituberculosis treatment and because repeated negative results came from extensive searches for an infectious cause, a corticoid treatment was subsequently initiated. The clinical response was quick, with apyrexia, diminution of C-reactive protein at 10 mg/L, disappearance of the swelling, and complete healing of the fistula in 3 weeks (Figures E, F). This response to steroid treatment suggested an autoinflammatory pathologic process. Histology with epithelioid cell granuloma could evoke metastatic Crohn’s disease. However, this hypothesis was unlikely in this case because inside the granuloma was spotted noncaseous necrosis, and because symptoms occurred under infliximab treatment while the disease was well-controlled throughout the period in question. Furthermore, metastatic Crohn’s disease is usually localized in skin creases, such as the submammary fold, inguinal areas, and abdominal skinfold creases.1 In addition, we are not aware of any lymph node involvement described in literature.
Aseptic abscesses syndrome is a rare condition associated with Crohn’s disease first described in 1995 by André et al.2 Aseptic abscesses syndrome is an autoinflammatory disease involving neutrophils that is characterized by disseminated sterile purulent collections. An inflammatory bowel disease is associated in 70% of the cases.3 Aseptic abscesses are generally located in the spleen (90% of cases) and abdominal lymph nodes, but can also affect the liver, lung, pancreas, and superficial lymph nodes.3 Repeated bacteriologic tests are always negative. Fever is the most frequent clinical feature (90%) and persists despite antibiotic therapy, whereas symptoms can vary depending on the aseptic abscesses localization. Biochemical tests show an increased CRP and leukocyte count. Histologically, aseptic abscesses are well-limited nodular lesions measuring from a few millimeters to 7 cm and containing white pus. These abscesses are surrounded by epithelioid cell granulomatous reaction, inside of which can be found a noncaseous necrosis, unlike tuberculosis. Specific colorations are negative as well (Ziehl, periodic acid-Schiff, Grocott, and Whartin-Starry).
In subcutaneous node involvement, the main differential diagnosis is pyoderma gangrenosum, but abscesses are not surrounded by granulomatosis reaction in pyoderma gangrenosum. Limited forms can be treated by colchicine, thalidomide, or dapsone, but steroid therapy is almost always necessary, with a consistently favorable evolution. However, relapses occur in two-thirds of cases.
In conclusion, aseptic abscesses syndrome is a diagnosis of exclusion, which is rare and should be considered in a patient known for inflammatory bowel disease who develops fever and deep abscesses with negative results on repeated searches for infectious causes.3
References
1. Guest G.D. Fink R.L.W. Metastatic Crohn’s disease: case report of an unusual variant and review of the literature. Dis Colon Rectum. 2000;43:1764–6.
2. André M., Aumaitre O., Marcheix J.C. et al. Unexplained sterile systemic abscesses in Crohn’s disease: aseptic abscesses as a new entity. Am J Gastroenterol. 1995;90:1183–4.
3. André M.F.J., Piette J.-C., Kémény J.-L. et al. Aseptic abscesses: a study of 30 patients with or without inflammatory bowel disease and review of the literature. Medicine (Baltimore). 2007;86:145–61.
An 18-year-old man presented with feverish cervical swelling that had developed over a few weeks.
He had a prior history of severe Crohn's disease with perianal manifestation with spontaneous perforation and had required an ileocecal and jejunal resection 3 years before. Clinical remission was achieved after 1 year of combination therapy by infliximab and azathioprine, followed by infliximab alone.
Physical examination showed an elevated body temperature of 38.5°C, and cervical palpation identified 3 painful erythematous nodes (3 cm in the left level IIb; 1 cm in the right IIb; 1 cm right supraclavicular space; Figure A). The rest of the examination was normal, and he did not complain about his bowel movements. He stated that he had not been traveling recently, nor had he been in contact with any sick person.
Laboratory tests spotted elevated levels of C-reactive protein (95.5 mg/L). Interferon-gamma release assays QuantiFERON-TB Gold was normal. Fine-needle aspiration showed a purulent content with repeated bacteriologic culture and gram stain culture, both of which were negative. Specific culture and polymerase chain reaction for Mycobacterium tuberculosis were negative as well.
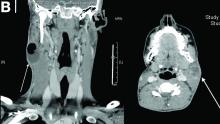
On computed tomography scan, the lymphadenitis showed liquid content with peripheral enhancement. One had an air-fluid level because of a spontaneous fistulization (Figure B). There were neither pulmonary abnormalities, mediastinal adenopathy, nor signs of Crohn's disease activity.
Histologic analysis of a lymph node excision showed epithelioid cell granuloma with noncaseous necrosis (Figure C, D).
Because the patient underwent anti-tumor necrosis factor-alpha therapy and despite the negative specific testing for tuberculosis, he was treated with probabilistic antituberculosis drugs for 6 months. Treatment proved ineffective and the patient's condition evolved with further fistulization and node size increase.
Considering the patient's medical history and evolution, what treatment should we consider, and what is the diagnosis?