User login
EVIDENCE-BASED ANSWER:
For adults with chronic rhinosinusitis (CRS), intranasal steroid (INS) therapy is more likely than placebo to improve symptoms (50% vs 32%; strength of recommendation [SOR]: A, systematic reviews).
Nasal saline irrigation (SI) alleviates symptoms better than no therapy (SOR: A, systematic reviews), but it’s probably not as effective as INS treatment (SOR: B, randomized controlled trial [RCT] with wide confidence interval).
Long-term (12 weeks) macrolide therapy doesn’t alter patient-oriented quality-of-life measures (SOR: A, systematic reviews).
Endoscopic sinus surgery improves CRS symptoms—nasal obstruction, discharge, and facial pain—over baseline (SOR: A, systematic reviews). Surgery and medical therapy appear about equivalent in terms of symptom improvement and quality-of-life measures (SOR: B, systematic reviews of low-quality RCTs).
EVIDENCE SUMMARY
The TABLE1-4 shows the major results of the meta-analyses for the various medical therapy trials.
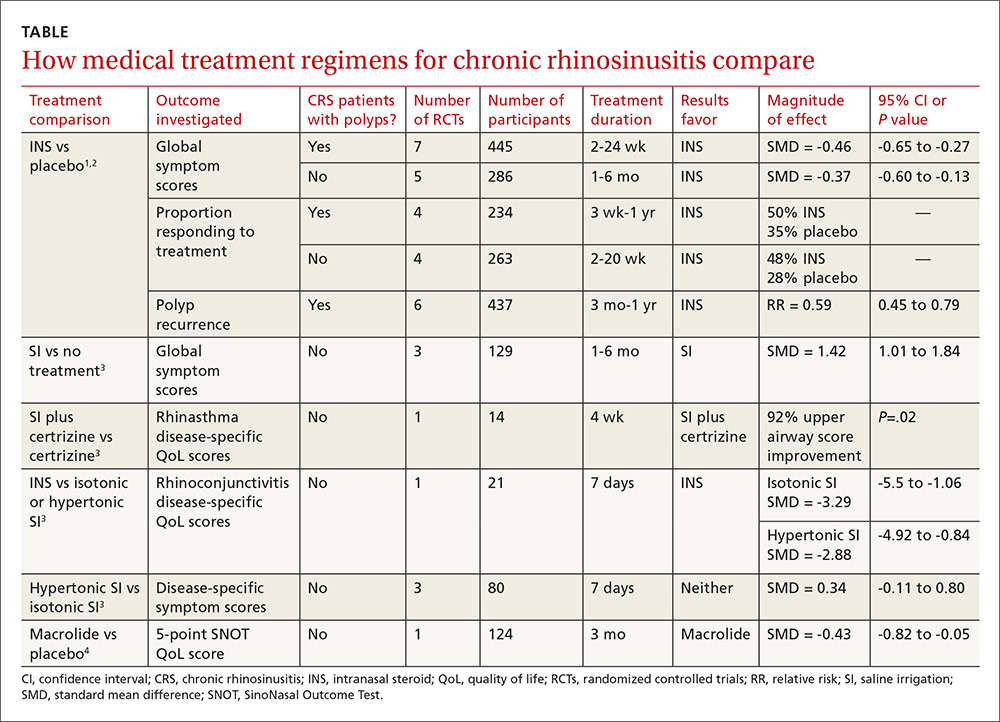
Two systematic reviews with meta-analyses evaluated treatment with INS for CRS with nasal polyps (40 RCTs; 3624 patients, mean age 48 years, 64% male) and without polyps (10 RCTs; 590 patients, mean age 39 years, 51% male).1,2 Trials reported sinonasal symptom outcomes differently and couldn’t be combined. In addition to reducing rate of polyp occurrence, for both CRS with and without polyps, key findings were:
- Global symptom scores were better for INS than placebo.
- Proportion of patients responding was greater for INS than with placebo.
There was no significant difference between adverse event rates with INS and placebo.
A systematic review and meta-analysis (8 RCTs, 389 patients) compared different SI regimens for CRS.3 The standardized mean difference was used to combine trials using various symptom outcomes. Key findings included the following:
- SI was better than no treatment.
- SI adjunctive therapy (with an antihistamine) improved disease-specific quality-of-life scores.
- SI was less effective than INS therapy for symptom improvement.
Hypertonic and isotonic saline yielded similar symptom scores. No adverse effects were reported.
One meta-analysis evaluated patient-reported outcomes with 12 weeks of macrolide therapy compared to placebo using the results of the SinoNasal Outcome Test (SNOT). The SNOT is a quality-of-life questionnaire that lists symptoms and the social-emotional consequences of CRS; a negative change in the SNOT score, on a 0 to 5 scale, indicates improvement. Overall the SNOT score improved 8% with macrolide therapy—statistically significant, but of uncertain clinical importance.4
Surgery improves nasal obstruction, pain, and postnasal discharge
A systematic review of 21 studies (prospective RCTs, prospective controlled clinical trials, cohort studies, case series, and retrospective record reviews) with a total of 2070 patients analyzed the effectiveness of endoscopic sinus surgery alone for improving CRS symptoms.5 Mean duration of post-operative follow-up was 14 months. Meta-analysis was performed separately for each symptom and the standard mean difference of the symptom severity score before and after surgery was reported as the effect size (ES) for the outcome measure (an ES of 0.2 is considered small; 0.6, moderate; 1.2, large; and 2, very large).
All symptoms improved compared to their preoperative severity scores. Nasal obstruction improved the most (ES=1.73; 95% CI, 1.45-2.02). Large symptom improvement was also observed for facial pain (ES=1.13; 95% CI, 0.96-1.31) and postnasal discharge (ES=1.19; 95% CI, 0.96-1.43).
Surgery and medical therapy may provide comparable symptom relief
A recent Cochrane review of 4 low-quality RCTs including 378 patients compared surgical with medical interventions for CRS with nasal polyps. Study heterogeneity and selective outcome reporting prevented meta-analysis.
The 3 comparison groups were endoscopic sinus surgery vs systemic steroids + INS; polypectomy vs systemic steroid + INS; and endoscopic surgery + INS vs antibiotic + “high-dose” INS. Overall, neither surgery nor medical therapy was superior in terms of patient-reported symptom scores or quality-of-life measures.6
1. Kalish L, Snidvongs K, Sivasubramaniam R, et al. Topical steroids for nasal polyps. Cochrane Database Syst Rev. 2012;(12):CD006549.
2. Snidvongs K, Kalish L, Sacks R, et al. Topical steroids for chronic rhinosinusitis without polyps. Cochrane Database Syst Rev. 2011;(8):CD009274.
3. Harvey R, Hannan SA, Badia L, et al. Nasal saline irrigation for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
4. Pynnonen MA, Venkatraman G, Davis GE. Macrolide therapy for chronic rhinosinusitis: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148:366-373.
5. Chester AC, Antisdel JL, Sindwani R. Symptom-specific outcomes of endoscopic sinus surgery: a systematic review. Otolaryngol Head Neck Surg. 2009;140:633-639.
6. Rimmer J, Fokkens W, Chong LY, et al. Surgical versus medical interventions for chronic rhinosinusitis with nasal polyps. Cochrane Database Syst Rev. 2014;(12):CD0069991.
EVIDENCE-BASED ANSWER:
For adults with chronic rhinosinusitis (CRS), intranasal steroid (INS) therapy is more likely than placebo to improve symptoms (50% vs 32%; strength of recommendation [SOR]: A, systematic reviews).
Nasal saline irrigation (SI) alleviates symptoms better than no therapy (SOR: A, systematic reviews), but it’s probably not as effective as INS treatment (SOR: B, randomized controlled trial [RCT] with wide confidence interval).
Long-term (12 weeks) macrolide therapy doesn’t alter patient-oriented quality-of-life measures (SOR: A, systematic reviews).
Endoscopic sinus surgery improves CRS symptoms—nasal obstruction, discharge, and facial pain—over baseline (SOR: A, systematic reviews). Surgery and medical therapy appear about equivalent in terms of symptom improvement and quality-of-life measures (SOR: B, systematic reviews of low-quality RCTs).
EVIDENCE SUMMARY
The TABLE1-4 shows the major results of the meta-analyses for the various medical therapy trials.
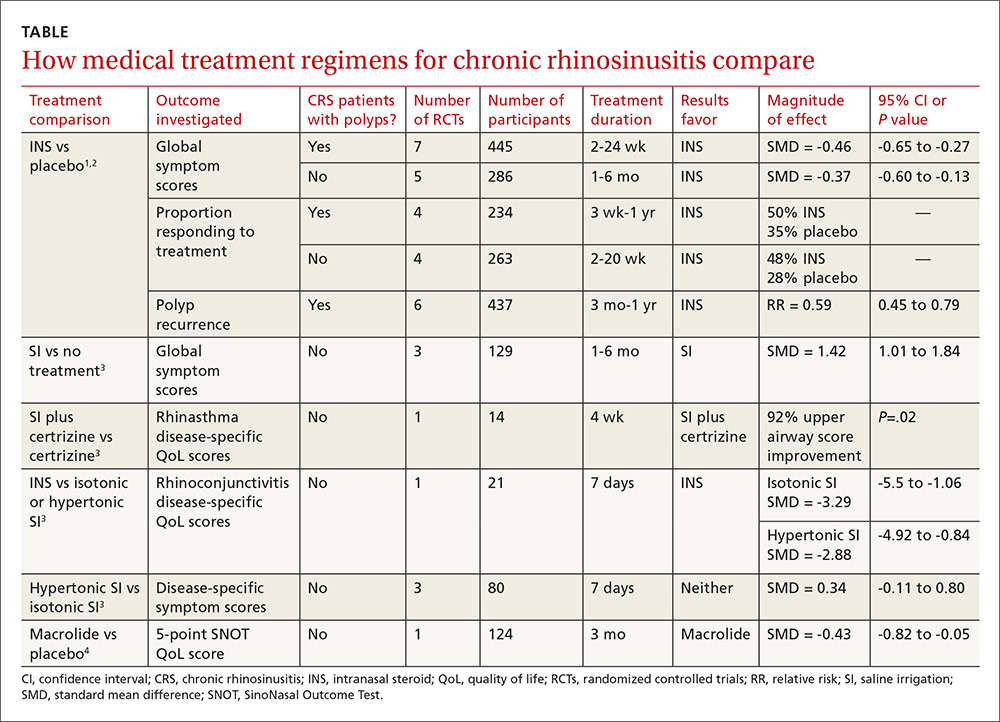
Two systematic reviews with meta-analyses evaluated treatment with INS for CRS with nasal polyps (40 RCTs; 3624 patients, mean age 48 years, 64% male) and without polyps (10 RCTs; 590 patients, mean age 39 years, 51% male).1,2 Trials reported sinonasal symptom outcomes differently and couldn’t be combined. In addition to reducing rate of polyp occurrence, for both CRS with and without polyps, key findings were:
- Global symptom scores were better for INS than placebo.
- Proportion of patients responding was greater for INS than with placebo.
There was no significant difference between adverse event rates with INS and placebo.
A systematic review and meta-analysis (8 RCTs, 389 patients) compared different SI regimens for CRS.3 The standardized mean difference was used to combine trials using various symptom outcomes. Key findings included the following:
- SI was better than no treatment.
- SI adjunctive therapy (with an antihistamine) improved disease-specific quality-of-life scores.
- SI was less effective than INS therapy for symptom improvement.
Hypertonic and isotonic saline yielded similar symptom scores. No adverse effects were reported.
One meta-analysis evaluated patient-reported outcomes with 12 weeks of macrolide therapy compared to placebo using the results of the SinoNasal Outcome Test (SNOT). The SNOT is a quality-of-life questionnaire that lists symptoms and the social-emotional consequences of CRS; a negative change in the SNOT score, on a 0 to 5 scale, indicates improvement. Overall the SNOT score improved 8% with macrolide therapy—statistically significant, but of uncertain clinical importance.4
Surgery improves nasal obstruction, pain, and postnasal discharge
A systematic review of 21 studies (prospective RCTs, prospective controlled clinical trials, cohort studies, case series, and retrospective record reviews) with a total of 2070 patients analyzed the effectiveness of endoscopic sinus surgery alone for improving CRS symptoms.5 Mean duration of post-operative follow-up was 14 months. Meta-analysis was performed separately for each symptom and the standard mean difference of the symptom severity score before and after surgery was reported as the effect size (ES) for the outcome measure (an ES of 0.2 is considered small; 0.6, moderate; 1.2, large; and 2, very large).
All symptoms improved compared to their preoperative severity scores. Nasal obstruction improved the most (ES=1.73; 95% CI, 1.45-2.02). Large symptom improvement was also observed for facial pain (ES=1.13; 95% CI, 0.96-1.31) and postnasal discharge (ES=1.19; 95% CI, 0.96-1.43).
Surgery and medical therapy may provide comparable symptom relief
A recent Cochrane review of 4 low-quality RCTs including 378 patients compared surgical with medical interventions for CRS with nasal polyps. Study heterogeneity and selective outcome reporting prevented meta-analysis.
The 3 comparison groups were endoscopic sinus surgery vs systemic steroids + INS; polypectomy vs systemic steroid + INS; and endoscopic surgery + INS vs antibiotic + “high-dose” INS. Overall, neither surgery nor medical therapy was superior in terms of patient-reported symptom scores or quality-of-life measures.6
EVIDENCE-BASED ANSWER:
For adults with chronic rhinosinusitis (CRS), intranasal steroid (INS) therapy is more likely than placebo to improve symptoms (50% vs 32%; strength of recommendation [SOR]: A, systematic reviews).
Nasal saline irrigation (SI) alleviates symptoms better than no therapy (SOR: A, systematic reviews), but it’s probably not as effective as INS treatment (SOR: B, randomized controlled trial [RCT] with wide confidence interval).
Long-term (12 weeks) macrolide therapy doesn’t alter patient-oriented quality-of-life measures (SOR: A, systematic reviews).
Endoscopic sinus surgery improves CRS symptoms—nasal obstruction, discharge, and facial pain—over baseline (SOR: A, systematic reviews). Surgery and medical therapy appear about equivalent in terms of symptom improvement and quality-of-life measures (SOR: B, systematic reviews of low-quality RCTs).
EVIDENCE SUMMARY
The TABLE1-4 shows the major results of the meta-analyses for the various medical therapy trials.
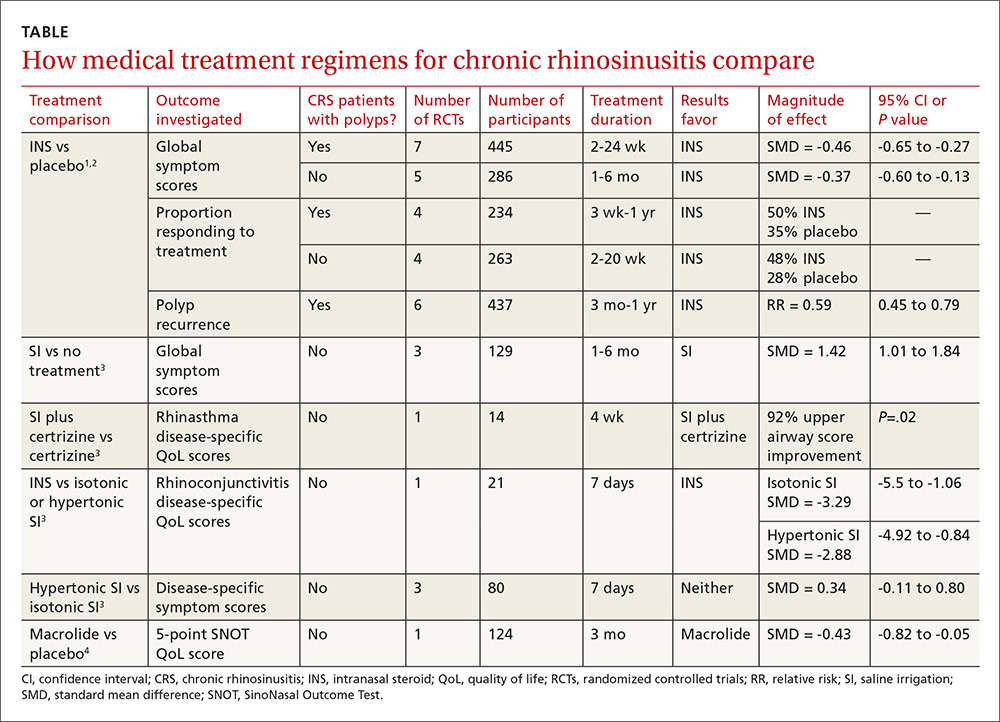
Two systematic reviews with meta-analyses evaluated treatment with INS for CRS with nasal polyps (40 RCTs; 3624 patients, mean age 48 years, 64% male) and without polyps (10 RCTs; 590 patients, mean age 39 years, 51% male).1,2 Trials reported sinonasal symptom outcomes differently and couldn’t be combined. In addition to reducing rate of polyp occurrence, for both CRS with and without polyps, key findings were:
- Global symptom scores were better for INS than placebo.
- Proportion of patients responding was greater for INS than with placebo.
There was no significant difference between adverse event rates with INS and placebo.
A systematic review and meta-analysis (8 RCTs, 389 patients) compared different SI regimens for CRS.3 The standardized mean difference was used to combine trials using various symptom outcomes. Key findings included the following:
- SI was better than no treatment.
- SI adjunctive therapy (with an antihistamine) improved disease-specific quality-of-life scores.
- SI was less effective than INS therapy for symptom improvement.
Hypertonic and isotonic saline yielded similar symptom scores. No adverse effects were reported.
One meta-analysis evaluated patient-reported outcomes with 12 weeks of macrolide therapy compared to placebo using the results of the SinoNasal Outcome Test (SNOT). The SNOT is a quality-of-life questionnaire that lists symptoms and the social-emotional consequences of CRS; a negative change in the SNOT score, on a 0 to 5 scale, indicates improvement. Overall the SNOT score improved 8% with macrolide therapy—statistically significant, but of uncertain clinical importance.4
Surgery improves nasal obstruction, pain, and postnasal discharge
A systematic review of 21 studies (prospective RCTs, prospective controlled clinical trials, cohort studies, case series, and retrospective record reviews) with a total of 2070 patients analyzed the effectiveness of endoscopic sinus surgery alone for improving CRS symptoms.5 Mean duration of post-operative follow-up was 14 months. Meta-analysis was performed separately for each symptom and the standard mean difference of the symptom severity score before and after surgery was reported as the effect size (ES) for the outcome measure (an ES of 0.2 is considered small; 0.6, moderate; 1.2, large; and 2, very large).
All symptoms improved compared to their preoperative severity scores. Nasal obstruction improved the most (ES=1.73; 95% CI, 1.45-2.02). Large symptom improvement was also observed for facial pain (ES=1.13; 95% CI, 0.96-1.31) and postnasal discharge (ES=1.19; 95% CI, 0.96-1.43).
Surgery and medical therapy may provide comparable symptom relief
A recent Cochrane review of 4 low-quality RCTs including 378 patients compared surgical with medical interventions for CRS with nasal polyps. Study heterogeneity and selective outcome reporting prevented meta-analysis.
The 3 comparison groups were endoscopic sinus surgery vs systemic steroids + INS; polypectomy vs systemic steroid + INS; and endoscopic surgery + INS vs antibiotic + “high-dose” INS. Overall, neither surgery nor medical therapy was superior in terms of patient-reported symptom scores or quality-of-life measures.6
1. Kalish L, Snidvongs K, Sivasubramaniam R, et al. Topical steroids for nasal polyps. Cochrane Database Syst Rev. 2012;(12):CD006549.
2. Snidvongs K, Kalish L, Sacks R, et al. Topical steroids for chronic rhinosinusitis without polyps. Cochrane Database Syst Rev. 2011;(8):CD009274.
3. Harvey R, Hannan SA, Badia L, et al. Nasal saline irrigation for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
4. Pynnonen MA, Venkatraman G, Davis GE. Macrolide therapy for chronic rhinosinusitis: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148:366-373.
5. Chester AC, Antisdel JL, Sindwani R. Symptom-specific outcomes of endoscopic sinus surgery: a systematic review. Otolaryngol Head Neck Surg. 2009;140:633-639.
6. Rimmer J, Fokkens W, Chong LY, et al. Surgical versus medical interventions for chronic rhinosinusitis with nasal polyps. Cochrane Database Syst Rev. 2014;(12):CD0069991.
1. Kalish L, Snidvongs K, Sivasubramaniam R, et al. Topical steroids for nasal polyps. Cochrane Database Syst Rev. 2012;(12):CD006549.
2. Snidvongs K, Kalish L, Sacks R, et al. Topical steroids for chronic rhinosinusitis without polyps. Cochrane Database Syst Rev. 2011;(8):CD009274.
3. Harvey R, Hannan SA, Badia L, et al. Nasal saline irrigation for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
4. Pynnonen MA, Venkatraman G, Davis GE. Macrolide therapy for chronic rhinosinusitis: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148:366-373.
5. Chester AC, Antisdel JL, Sindwani R. Symptom-specific outcomes of endoscopic sinus surgery: a systematic review. Otolaryngol Head Neck Surg. 2009;140:633-639.
6. Rimmer J, Fokkens W, Chong LY, et al. Surgical versus medical interventions for chronic rhinosinusitis with nasal polyps. Cochrane Database Syst Rev. 2014;(12):CD0069991.
Evidence-based answers from the Family Physicians Inquiries Network
