User login
Purpose Despite numerous studies on adherence, there is little research on the first-fill rate of antihypertensive prescriptions. Our study took advantage of the recent increase in electronic prescribing (e-prescribing) and used data from e-prescribing physicians to determine the first-fill failure rate of antihypertensive prescriptions and to assess which factors predict first-fill failure.
Methods This retrospective study reviewed claims from a Mid-Atlantic managed care organization (MCO). We included adult members with continuous medical and pharmacy coverage who were prescribed an antihypertensive in 2008 by an e-prescribing physician. First-fill failure occurred when the patient did not obtain the antihypertensive medication due to either a denial by the MCO or reversal by the dispensing pharmacist. (Pharmacists reverse claims when a patient fails to pick up a medication.) Multivariate regression analysis determined the clinical and demographic factors associated with failure to fill.
Results The cohort consisted of 14,693 antihypertensive prescriptions, prescribed by 164 e-prescribing physicians for 7061 unique members. There were 2289 out of 14,693 prescriptions (15.6%) that went unfilled, affecting 24.3% of patients. Of the prescriptions not obtained, 1466 (64%) were denied by the MCO and 823 (36%) were reversed. Significant factors associated with first-fill failure were new diagnosis of hypertension, new antihypertensive agent, higher co-payment, and enrollment in a health maintenance organization or preferred provider organization.
Conclusions Patients newly diagnosed with hypertension and those prescribed a new antihypertensive were at particularly high risk for not obtaining their medication. Because nearly a quarter of patients did not obtain their initial fill of an antihypertensive prescription, future research should determine efficient and cost-effective systems to address first-fill failure in primary care.
Poor patient adherence to medical directives—the main cause of unsuccessful efforts to control hypertension1—is often difficult to assess in daily practice and in research. A common example of nonadherence is the failure to fill new prescriptions or to refill existing ones. In measuring adherence to first-fill and refilled prescriptions, investigators have often relied on patient self-report.2,3 However, this means of evaluation may be biased. One study found that patients markedly overstated their adherence to antihypertensive regimens, when compared with adherence measured by prescriptions actually filled.4
Objectively determining the rate of first-fill failure (not obtaining the initial fill of a prescription) has typically been cumbersome, requiring time-consuming chart reviews, which is unrealistic for studying large populations. A more efficient way to collect these data is through electronic prescribing (e-prescribing)—the electronic transmission of prescription or prescription-related information between a prescriber, a dispenser, and a pharmacy benefit manager or health plan, either directly or through an intermediary service.5
Our study sought to extend previous knowledge of adherence by determining the rate of first-fill failure for antihypertensive agents prescribed by electronic means, as well as identifying the clinical and demographic factors most closely associated with that failure. We believe e-prescribing may offer a way to improve antihypertensive medication adherence, especially for particular subgroups of patients, by providing information on the patient’s formulary and fill status notification.
Methods
This retrospective study used administrative, medical, and pharmacy data from a Mid-Atlantic managed care organization (MCO) serving 3.3 million medical and 1.2 million pharmacy members. To be eligible for inclusion, a member had to have an antihypertensive agent prescribed by a physician using e-prescribing. Our assumption in reviewing only prescriptions written by e-prescribing physicians was that each prescription would have a corresponding claim. To recruit a minimum of 100 electronic prescribers, we began by surveying physicians who had prescribed the highest volume of antihypertensive medication during the first half of 2008. We faxed a survey to these physicians, and if we received no response, we followed up by phone. Our final sample of physicians comprised those who were e-prescribing at least 75% of the time before January 1, 2008.6
A pharmacy claims query identified all antihypertensive prescriptions from January 1, 2008 through December 31, 2008 that were coded as new (a new prescription for either a new agent or the same agent the patient had been taking) and were prescribed by our group of electronic prescribers. We excluded members (and their prescription claims) who were younger than 18 years on the date of their first prescription and those who were not continuously enrolled in the same medical and pharmacy benefit plan from July 1, 2006 through December 31, 2008.
For each prescription, 3 claim options were possible: paid, denied, or reversed.
A paid claim meant that the prescription was approved by the MCO for coverage and that the member obtained the medication.
A denied claim occurred when coverage for the prescribed product was refused by the MCO.
A reversed claim meant that the prescription had been approved by the MCO for coverage, but the approved claim was later reversed by the pharmacist when a patient failed to pick up the prescription within 14 days.
A denied or reversed claim meant that the patient did not receive the medication, and this occurrence was labeled as failure to fill.
For members in the cohort, a medical claims query identified hypertension using specific International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes in the 401 category from July 1, 2006 through December 31, 2008. We deemed patients as newly diagnosed with hypertension if their first ICD-9-CM code for hypertension was within the preceding 6 months of the first antihypertensive prescription.
Outcome measures
The primary outcome measure was the percentage of new antihypertensive prescriptions that patients failed to obtain. To calculate this number, we designated the numerator as the number of denied or reversed claims for antihypertensive prescriptions, and the denominator as the overall number of antihypertensive prescriptions in the cohort.
The secondary outcome measure was the set of clinical and demographic factors related to failure to obtain the first fill. We evaluated the possible association of first-fill failure with age, sex, prior antihypertensive use, hypertension diagnosis, formulary status, co-payment, monotherapy vs combination product, pharmacologic category, type of health plan, and number of antihypertensive prescriptions.
All data collection conformed to patient privacy standards set by the Health Insurance Portability and Accountability Act (HIPAA), and the dataset was delivered to the researchers with de-identified patient information. The University of Maryland, Baltimore (UMB) Institutional Review Board (IRB) fully approved the research protocol.
Statistical analysis
Statistical analysis included descriptive statistics such as percentages for discrete variables (eg, sex) and calculations of means and standard deviations (SD) for continuous variables (eg, age). Univariate analyses examined the correlation between clinical/demographic characteristics and first-fill rates. We used binomial logistic regression to assess predictors of first-fill failure. We set statistical significance at an accepted alpha (P<.05).
Results
E-prescribing physicians
There were 1313 e-prescribing physicians ranked according to antihypertensive prescription volume. We contacted 457 physicians who prescribed the highest volume of medications and selected a final group of 164.
Patient/prescription cohort
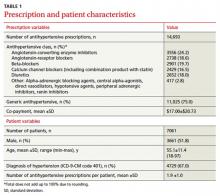
The cohort consisted of 14,693 antihypertensive prescriptions prescribed by the 164 e-prescribing physicians. There were 7061 unique members with a mean age of 55.1±11.4 years (TABLE 1). Half were men (51.8%), and each member had a mean of 1.9 antihypertensive prescriptions. About two-thirds had a diagnosis of hypertension, as represented by ICD-9-CM codes.
Three-fourths of the prescriptions were for generic antihypertensives. ACE inhibitors were the most commonly prescribed class of drug, at 24.2%, followed by beta-blockers, angiotensin-receptor blockers, diuretics, and calcium channel blockers. Agents not fitting into the above classes were prescribed the least, at 2.8% of prescription volume. The mean co-payment per antihypertensive prescription was $17.00±$20.73.
Primary outcome
Patients failed to obtain the antihypertensive medication for 2289/14,693 (15.6%) prescriptions. Of the prescriptions not obtained, 1466 (64%) were denied and 823 (36%) were reversed. Failure to obtain the 2289 prescriptions affected 24.3% (1713/7061) of patients.
Secondary outcome
We compared clinical and demographic characteristics between the 2 outcome groups (TABLE 2). Univariate analyses revealed statistically significant differences for age, history of antihypertensive use and hypertension diagnosis, formulary status, medication characteristics, and type of health plan. Patients prescribed a new antihypertensive product or receiving a new diagnosis of hypertension were significantly less likely to fill their prescriptions (P<.001). Prescriptions for brand and combination products were, respectively, 2.2 percentage points (P=.025) and 3 percentage points (P=.002) higher in the failure-to-obtain category than in the obtained category. The difference in mean co-payment was $2.56 higher in the failure-to-obtain group (P<.001). There were differences between the obtained and failure-to-obtain groups based on the member’s type of health plan (P<.001).
Statistically significant factors from univariate analyses were included in the logistic regression model (data not shown). Factors associated with failure to obtain an antihypertensive prescription fell into 3 categories: history of hypertension (new vs existing diagnosis), formulary status of antihypertensive agent, and type of health plan. Prescriptions for new antihypertensive products were 49.44 times more likely to go unfilled (P<.001). Prescriptions were 1.73 times more likely to remain unfilled for members with a new diagnosis for hypertension (P<.001). In addition, the formulary status of the prescription showed that prescriptions were less likely to be filled for brand products (P=.030) or for those requiring higher co-payments (P<.001). Compared with indemnity health plans, health maintenance organizations and preferred provider organizations were more likely to be associated with unfilled prescriptions (P<.001 and P=.044, respectively).
TABLE 2
Prescription characteristics associated with different claims outcomes (N=14,693)*
| Variable | Obtained antihyper-tensive (n=12,404) | Failed to obtain antihypertensive (n=2289) | P value |
|---|---|---|---|
| Age | |||
| Mean ±SD, y | 56.2 ±11.4 | 55.4 ±11.9 | .002 |
| Sex | |||
| Male | 6581 (53.1) | 1182 (51.6) | .212 |
| Female | 5823 (46.9) | 1107 (48.4) | |
| Prior antihypertensive prescriptions | |||
| New antihypertensive product (no pharmacy claims for this agent within prior 6 months) | 41 (0.3) | 383 (16.7) | <.001 |
| Hypertension diagnosis | |||
| New diagnosis (at least 1 medical claim for HTN <6 months prior and no medical claims for HTN >6 months prior to antihypertensive prescription) | 626 (5.0) | 367 (16.0) | <.001 |
| Monotherapy/combination product | |||
| Monotherapy | 9482 (76.4) | 1681 (73.4) | .002 |
| Combination | 2922 (23.6) | 608 (26.6) | |
| Brand or generic status of product | |||
| Generic | 9350 (75.4) | 1675 (73.2) | .025 |
| Brand | 3054 (24.6) | 614 (26.8) | |
| Tier status | |||
| Tier 1 | 9350 (75.4) | 1675 (73.2) | .074 |
| Tier 2 | 1282 (10.3) | 252 (11.0) | |
| Tier 3 | 1772 (14.3) | 362 (15.8) | |
| Co-payment | |||
| Mean ±SD | $16.60±$20.17 | $19.16±$23.43 | <.001 |
| Type of health plan | |||
| Health maintenance organization | 5574 (44.9) | 1188 (51.9) | <.001 |
| Preferred provider organization | 2372 (19.1) | 426 (18.6) | |
| Consumer directed | 1847 (14.9) | 278 (12.1) | |
| Indemnity | 2611 (21.0) | 397 (17.3) | |
| Number of antihypertensive prescriptions | |||
| Mean ±SD | 1.9 ±1.0 | 1.8 ±1.0 | .001 |
| Therapeutic class | |||
| Angiotensin-converting enzyme inhibitors | 3008 (24.3) | 548 (23.9) | .939 |
| Angiotensin-receptor blockers | 2296 (18.5) | 442 (19.3) | |
| Beta-blockers | 2461 (19.8) | 440 (19.2) | |
| Calcium channel blockers (including combination product with statin) | 2047 (16.5) | 382 (16.7) | |
| Diuretics | 2242 (18.1) | 410 (17.9) | |
| Other: Alpha-adrenergic blocking agents, central alpha-agonists, direct vasodilators, hypotensive agents, peripheral adrenergic inhibitors, renin inhibitors | 350 (2.8) | 67 (2.9) | |
| HTN, hypertension. *Data are presented as n(%) unless otherwise noted. | |||
Discussion
This study used e-prescribing to evaluate nonadherence to the first-fill of an antihypertensive prescription. Our findings that 24.3% of patients did not obtain the first-fill of a medication and that 15.6% of prescriptions remained unclaimed are comparable to those of other research using electronically obtained prescription data.7,8
In a cross-sectional study of 327 African American adults enrolled in a Medicaid managed care plan, the authors reported that 24.9% (433/1742) of antihypertensive prescriptions were unfilled.7 In a study of therapeutically naïve patients, the first-fill failure rate was 17%.8 These patients were less likely to fill their antihypertensive prescriptions if they were prescribed loop diuretics or had a higher prescription co-payment. The median co-payment was $2 higher for prescriptions not obtained, compared with those that were obtained (P<.001). This finding was similar to the $2.56 difference we found for mean co-payment.
Higher co-payment was a strong predictor of decreased adherence in other antihypertensive adherence studies.9,10 In a survey of Medicare patients, the most common reason cited for failing to fill any prescription was that “it would cost too much.”2 Prescribing a less costly agent based on an insurer’s formulary may reduce the first-fill failure rate.
Although educating patients about their disease, involving family, and increasing patient participation through self-monitoring of blood pressure all have a positive impact on adherence rates and blood pressure control, physicians are hard pressed for time during an office visit to address such interventions.11-19 E-prescribing potentially offers a more efficient way to improve antihypertensive medication adherence. A recent ruling by the Centers for Medicare & Medicaid Services (CMS) requires e-prescribing systems to have the capability of providing formulary and benefit transaction, medication history transaction, and fill status notification to prescribers.20 Prescribers can readily access patients’ insurance coverage information. Formulary decision support, as part of an e-prescribing system, has been shown to increase use of formulary products.21 Fill status notification allows two-way communication between the prescriber and pharmacy so that prescribers can be made aware if patients fail to fill prescriptions.
Unfortunately, e-prescribing is not yet widely used. Approximately 26% of office-based US physicians use e-prescribing, and only 30% of them take advantage of formulary information.22 E-prescribing authorities believe practices not using the fill status notification probably lack resources needed to manage patients who are nonadherent.22 While it may not be necessary to check whether all patients have obtained their prescription, it may be useful for subgroups of patients, such as those who have received a new diagnosis, whose disease is poorly controlled, who are prescribed new antihypertensive agents, or who are otherwise thought to be nonadherent.
Study limitations. First, claims data serve as a proxy for medication adherence. Even though a patient obtained an antihypertensive prescription according to claims data, this does not guarantee that the patient used the medication.
Second, not all patients had a diagnosis of hypertension designated by specific ICD-9-CM codes. Patients may have been prescribed antihypertensive medications for other indications, such as heart failure, migraine, anxiety, etc. Our results apply to all patients prescribed antihypertensive agents, and although most had hypertension, there may be differences in first-fill rates for those with and without hypertension.
Third, patients were required to fill their prescriptions through insurance. In community pharmacy settings, some prescriptions may be paid for with cash due to the availability of several inexpensive generic antihypertensive medications (eg, a 30-day supply for $4, or 90-day supply for $10).23 Patients taking advantage of these promotions would result in an overestimation of first-fill failure rate.
Fourth, patients may have received samples from their physician and subsequently failed to obtain their antihypertensive prescription at the pharmacy because the medication sample was ineffective or not tolerated.
Fifth, claims data from physicians who were e-prescribing were used to proxy electronic prescriptions. However, some physicians may have handed patients their prescriptions, which, if never taken to the pharmacy, would result in an underestimation of first-fill failure rate.
CORRESPONDENCE
Catherine E. Cooke, President, PosiHealth, Inc., 5106 Bonnie Branch Road, Ellicott City, MD 21043; [email protected]
1. Sabate E. ed. Adherence to long-term therapies: evidence for action. Geneva, Switzerland. World Health Organization, 20030. Available at: http://www.who.int/chp/knowledge/publications/adherence_report/en. Accessed May 20, 2011.
2. Kennedy J, Tuleu I, Mackay K. Unfilled prescriptions of Medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm. 2008;14:553-560.
3. Esposito D, Schone E, Williams T, et al. Prevalence of unclaimed prescriptions at military pharmacies. J Manag Care Pharm. 2008;14:541-552.
4. Wang PS, Benner JS, Glynn RJ, et al. How well do patients report noncompliance with antihypertensive medications? a comparison of self-report versus filled prescriptions. Pharmacoepidemiol Drug Saf. 2004;13:11-19.
5. eHealth Initiative and The Center for Improving Medication Management. A clinician’s guide to electronic prescribing. White paper from the eHealth Initiative and The Center for Improving Medication Management, 2008. Available at: http://www.ehealthinitiative.org/sites/default/files/e-Prescribing_Clinicians_Guide_Final(1).pdf. Accessed March 21, 2010.
6. Solberg LI, Asche SE, Pawlson LG, et al. Practice systems are associated with high-quality care for diabetes. Am J Manag Care. 2008;14:85-92.
7. Lagu T, Weiner MG, Eachus S, et al. Effect of patient comorbidities on filling of antihypertensive prescriptions Am J Manag Care. 2009;15:24-30.
8. Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens. 2009;22:392-396.
9. Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298:61-69.
10. Kamal-Bahl S, Briesacher B. How do incentive-based formularies influence drug selection and spending for hypertension? Health Aff. 2004;23:227-236.
11. Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72:115-121.
12. Boulware LE, Daumit GL, Frick KD, et al. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001;21:221-232.
13. Feldman R, Bacher M, Campbell N, et al. Adherence to pharmacologic management of hypertension. Can J Public Health. 1998;89:I16-I18.
14. Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15-minute visit. Arch Intern Med. 2008;168:1843-1852.
15. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028-3035.
16. Morisky DE, Levine DM, Green LW, et al. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983;73:153-162.
17. Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657-665.
18. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care visits. Health Serv Res. 2007;42:1871-1894.
19. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
20. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; standards for e-prescribing under Medicare Part D and identification of backward compatible version of adopted standard for e-prescribing and the Medicare prescription drug program (version 8.1). Final rule. Fed Regist. 2008;73:18917-18942.
21. Fischer MA, Vogeli C, Stedman M, et al. Effect of electronic prescribing with formulary decision support on medication use and cost. Arch Intern Med. 2008;168:2433-2439.
22. SureScripts 2009 Progress Report on E-Prescribing. Available at: http://www.surescripts.com/downloads/NPR/national-progress-report.pdf. Accessed March 21, 2010.
23. Walmart. Retail prescription program drug list. Available at: http://i.walmartimages.com/i/if/hmp/fusion/customer_list.pdf. Accessed March 21, 2010.
Purpose Despite numerous studies on adherence, there is little research on the first-fill rate of antihypertensive prescriptions. Our study took advantage of the recent increase in electronic prescribing (e-prescribing) and used data from e-prescribing physicians to determine the first-fill failure rate of antihypertensive prescriptions and to assess which factors predict first-fill failure.
Methods This retrospective study reviewed claims from a Mid-Atlantic managed care organization (MCO). We included adult members with continuous medical and pharmacy coverage who were prescribed an antihypertensive in 2008 by an e-prescribing physician. First-fill failure occurred when the patient did not obtain the antihypertensive medication due to either a denial by the MCO or reversal by the dispensing pharmacist. (Pharmacists reverse claims when a patient fails to pick up a medication.) Multivariate regression analysis determined the clinical and demographic factors associated with failure to fill.
Results The cohort consisted of 14,693 antihypertensive prescriptions, prescribed by 164 e-prescribing physicians for 7061 unique members. There were 2289 out of 14,693 prescriptions (15.6%) that went unfilled, affecting 24.3% of patients. Of the prescriptions not obtained, 1466 (64%) were denied by the MCO and 823 (36%) were reversed. Significant factors associated with first-fill failure were new diagnosis of hypertension, new antihypertensive agent, higher co-payment, and enrollment in a health maintenance organization or preferred provider organization.
Conclusions Patients newly diagnosed with hypertension and those prescribed a new antihypertensive were at particularly high risk for not obtaining their medication. Because nearly a quarter of patients did not obtain their initial fill of an antihypertensive prescription, future research should determine efficient and cost-effective systems to address first-fill failure in primary care.
Poor patient adherence to medical directives—the main cause of unsuccessful efforts to control hypertension1—is often difficult to assess in daily practice and in research. A common example of nonadherence is the failure to fill new prescriptions or to refill existing ones. In measuring adherence to first-fill and refilled prescriptions, investigators have often relied on patient self-report.2,3 However, this means of evaluation may be biased. One study found that patients markedly overstated their adherence to antihypertensive regimens, when compared with adherence measured by prescriptions actually filled.4
Objectively determining the rate of first-fill failure (not obtaining the initial fill of a prescription) has typically been cumbersome, requiring time-consuming chart reviews, which is unrealistic for studying large populations. A more efficient way to collect these data is through electronic prescribing (e-prescribing)—the electronic transmission of prescription or prescription-related information between a prescriber, a dispenser, and a pharmacy benefit manager or health plan, either directly or through an intermediary service.5
Our study sought to extend previous knowledge of adherence by determining the rate of first-fill failure for antihypertensive agents prescribed by electronic means, as well as identifying the clinical and demographic factors most closely associated with that failure. We believe e-prescribing may offer a way to improve antihypertensive medication adherence, especially for particular subgroups of patients, by providing information on the patient’s formulary and fill status notification.
Methods
This retrospective study used administrative, medical, and pharmacy data from a Mid-Atlantic managed care organization (MCO) serving 3.3 million medical and 1.2 million pharmacy members. To be eligible for inclusion, a member had to have an antihypertensive agent prescribed by a physician using e-prescribing. Our assumption in reviewing only prescriptions written by e-prescribing physicians was that each prescription would have a corresponding claim. To recruit a minimum of 100 electronic prescribers, we began by surveying physicians who had prescribed the highest volume of antihypertensive medication during the first half of 2008. We faxed a survey to these physicians, and if we received no response, we followed up by phone. Our final sample of physicians comprised those who were e-prescribing at least 75% of the time before January 1, 2008.6
A pharmacy claims query identified all antihypertensive prescriptions from January 1, 2008 through December 31, 2008 that were coded as new (a new prescription for either a new agent or the same agent the patient had been taking) and were prescribed by our group of electronic prescribers. We excluded members (and their prescription claims) who were younger than 18 years on the date of their first prescription and those who were not continuously enrolled in the same medical and pharmacy benefit plan from July 1, 2006 through December 31, 2008.
For each prescription, 3 claim options were possible: paid, denied, or reversed.
A paid claim meant that the prescription was approved by the MCO for coverage and that the member obtained the medication.
A denied claim occurred when coverage for the prescribed product was refused by the MCO.
A reversed claim meant that the prescription had been approved by the MCO for coverage, but the approved claim was later reversed by the pharmacist when a patient failed to pick up the prescription within 14 days.
A denied or reversed claim meant that the patient did not receive the medication, and this occurrence was labeled as failure to fill.
For members in the cohort, a medical claims query identified hypertension using specific International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes in the 401 category from July 1, 2006 through December 31, 2008. We deemed patients as newly diagnosed with hypertension if their first ICD-9-CM code for hypertension was within the preceding 6 months of the first antihypertensive prescription.
Outcome measures
The primary outcome measure was the percentage of new antihypertensive prescriptions that patients failed to obtain. To calculate this number, we designated the numerator as the number of denied or reversed claims for antihypertensive prescriptions, and the denominator as the overall number of antihypertensive prescriptions in the cohort.
The secondary outcome measure was the set of clinical and demographic factors related to failure to obtain the first fill. We evaluated the possible association of first-fill failure with age, sex, prior antihypertensive use, hypertension diagnosis, formulary status, co-payment, monotherapy vs combination product, pharmacologic category, type of health plan, and number of antihypertensive prescriptions.
All data collection conformed to patient privacy standards set by the Health Insurance Portability and Accountability Act (HIPAA), and the dataset was delivered to the researchers with de-identified patient information. The University of Maryland, Baltimore (UMB) Institutional Review Board (IRB) fully approved the research protocol.
Statistical analysis
Statistical analysis included descriptive statistics such as percentages for discrete variables (eg, sex) and calculations of means and standard deviations (SD) for continuous variables (eg, age). Univariate analyses examined the correlation between clinical/demographic characteristics and first-fill rates. We used binomial logistic regression to assess predictors of first-fill failure. We set statistical significance at an accepted alpha (P<.05).
Results
E-prescribing physicians
There were 1313 e-prescribing physicians ranked according to antihypertensive prescription volume. We contacted 457 physicians who prescribed the highest volume of medications and selected a final group of 164.
Patient/prescription cohort
The cohort consisted of 14,693 antihypertensive prescriptions prescribed by the 164 e-prescribing physicians. There were 7061 unique members with a mean age of 55.1±11.4 years (TABLE 1). Half were men (51.8%), and each member had a mean of 1.9 antihypertensive prescriptions. About two-thirds had a diagnosis of hypertension, as represented by ICD-9-CM codes.
Three-fourths of the prescriptions were for generic antihypertensives. ACE inhibitors were the most commonly prescribed class of drug, at 24.2%, followed by beta-blockers, angiotensin-receptor blockers, diuretics, and calcium channel blockers. Agents not fitting into the above classes were prescribed the least, at 2.8% of prescription volume. The mean co-payment per antihypertensive prescription was $17.00±$20.73.
Primary outcome
Patients failed to obtain the antihypertensive medication for 2289/14,693 (15.6%) prescriptions. Of the prescriptions not obtained, 1466 (64%) were denied and 823 (36%) were reversed. Failure to obtain the 2289 prescriptions affected 24.3% (1713/7061) of patients.
Secondary outcome
We compared clinical and demographic characteristics between the 2 outcome groups (TABLE 2). Univariate analyses revealed statistically significant differences for age, history of antihypertensive use and hypertension diagnosis, formulary status, medication characteristics, and type of health plan. Patients prescribed a new antihypertensive product or receiving a new diagnosis of hypertension were significantly less likely to fill their prescriptions (P<.001). Prescriptions for brand and combination products were, respectively, 2.2 percentage points (P=.025) and 3 percentage points (P=.002) higher in the failure-to-obtain category than in the obtained category. The difference in mean co-payment was $2.56 higher in the failure-to-obtain group (P<.001). There were differences between the obtained and failure-to-obtain groups based on the member’s type of health plan (P<.001).
Statistically significant factors from univariate analyses were included in the logistic regression model (data not shown). Factors associated with failure to obtain an antihypertensive prescription fell into 3 categories: history of hypertension (new vs existing diagnosis), formulary status of antihypertensive agent, and type of health plan. Prescriptions for new antihypertensive products were 49.44 times more likely to go unfilled (P<.001). Prescriptions were 1.73 times more likely to remain unfilled for members with a new diagnosis for hypertension (P<.001). In addition, the formulary status of the prescription showed that prescriptions were less likely to be filled for brand products (P=.030) or for those requiring higher co-payments (P<.001). Compared with indemnity health plans, health maintenance organizations and preferred provider organizations were more likely to be associated with unfilled prescriptions (P<.001 and P=.044, respectively).
TABLE 2
Prescription characteristics associated with different claims outcomes (N=14,693)*
| Variable | Obtained antihyper-tensive (n=12,404) | Failed to obtain antihypertensive (n=2289) | P value |
|---|---|---|---|
| Age | |||
| Mean ±SD, y | 56.2 ±11.4 | 55.4 ±11.9 | .002 |
| Sex | |||
| Male | 6581 (53.1) | 1182 (51.6) | .212 |
| Female | 5823 (46.9) | 1107 (48.4) | |
| Prior antihypertensive prescriptions | |||
| New antihypertensive product (no pharmacy claims for this agent within prior 6 months) | 41 (0.3) | 383 (16.7) | <.001 |
| Hypertension diagnosis | |||
| New diagnosis (at least 1 medical claim for HTN <6 months prior and no medical claims for HTN >6 months prior to antihypertensive prescription) | 626 (5.0) | 367 (16.0) | <.001 |
| Monotherapy/combination product | |||
| Monotherapy | 9482 (76.4) | 1681 (73.4) | .002 |
| Combination | 2922 (23.6) | 608 (26.6) | |
| Brand or generic status of product | |||
| Generic | 9350 (75.4) | 1675 (73.2) | .025 |
| Brand | 3054 (24.6) | 614 (26.8) | |
| Tier status | |||
| Tier 1 | 9350 (75.4) | 1675 (73.2) | .074 |
| Tier 2 | 1282 (10.3) | 252 (11.0) | |
| Tier 3 | 1772 (14.3) | 362 (15.8) | |
| Co-payment | |||
| Mean ±SD | $16.60±$20.17 | $19.16±$23.43 | <.001 |
| Type of health plan | |||
| Health maintenance organization | 5574 (44.9) | 1188 (51.9) | <.001 |
| Preferred provider organization | 2372 (19.1) | 426 (18.6) | |
| Consumer directed | 1847 (14.9) | 278 (12.1) | |
| Indemnity | 2611 (21.0) | 397 (17.3) | |
| Number of antihypertensive prescriptions | |||
| Mean ±SD | 1.9 ±1.0 | 1.8 ±1.0 | .001 |
| Therapeutic class | |||
| Angiotensin-converting enzyme inhibitors | 3008 (24.3) | 548 (23.9) | .939 |
| Angiotensin-receptor blockers | 2296 (18.5) | 442 (19.3) | |
| Beta-blockers | 2461 (19.8) | 440 (19.2) | |
| Calcium channel blockers (including combination product with statin) | 2047 (16.5) | 382 (16.7) | |
| Diuretics | 2242 (18.1) | 410 (17.9) | |
| Other: Alpha-adrenergic blocking agents, central alpha-agonists, direct vasodilators, hypotensive agents, peripheral adrenergic inhibitors, renin inhibitors | 350 (2.8) | 67 (2.9) | |
| HTN, hypertension. *Data are presented as n(%) unless otherwise noted. | |||
Discussion
This study used e-prescribing to evaluate nonadherence to the first-fill of an antihypertensive prescription. Our findings that 24.3% of patients did not obtain the first-fill of a medication and that 15.6% of prescriptions remained unclaimed are comparable to those of other research using electronically obtained prescription data.7,8
In a cross-sectional study of 327 African American adults enrolled in a Medicaid managed care plan, the authors reported that 24.9% (433/1742) of antihypertensive prescriptions were unfilled.7 In a study of therapeutically naïve patients, the first-fill failure rate was 17%.8 These patients were less likely to fill their antihypertensive prescriptions if they were prescribed loop diuretics or had a higher prescription co-payment. The median co-payment was $2 higher for prescriptions not obtained, compared with those that were obtained (P<.001). This finding was similar to the $2.56 difference we found for mean co-payment.
Higher co-payment was a strong predictor of decreased adherence in other antihypertensive adherence studies.9,10 In a survey of Medicare patients, the most common reason cited for failing to fill any prescription was that “it would cost too much.”2 Prescribing a less costly agent based on an insurer’s formulary may reduce the first-fill failure rate.
Although educating patients about their disease, involving family, and increasing patient participation through self-monitoring of blood pressure all have a positive impact on adherence rates and blood pressure control, physicians are hard pressed for time during an office visit to address such interventions.11-19 E-prescribing potentially offers a more efficient way to improve antihypertensive medication adherence. A recent ruling by the Centers for Medicare & Medicaid Services (CMS) requires e-prescribing systems to have the capability of providing formulary and benefit transaction, medication history transaction, and fill status notification to prescribers.20 Prescribers can readily access patients’ insurance coverage information. Formulary decision support, as part of an e-prescribing system, has been shown to increase use of formulary products.21 Fill status notification allows two-way communication between the prescriber and pharmacy so that prescribers can be made aware if patients fail to fill prescriptions.
Unfortunately, e-prescribing is not yet widely used. Approximately 26% of office-based US physicians use e-prescribing, and only 30% of them take advantage of formulary information.22 E-prescribing authorities believe practices not using the fill status notification probably lack resources needed to manage patients who are nonadherent.22 While it may not be necessary to check whether all patients have obtained their prescription, it may be useful for subgroups of patients, such as those who have received a new diagnosis, whose disease is poorly controlled, who are prescribed new antihypertensive agents, or who are otherwise thought to be nonadherent.
Study limitations. First, claims data serve as a proxy for medication adherence. Even though a patient obtained an antihypertensive prescription according to claims data, this does not guarantee that the patient used the medication.
Second, not all patients had a diagnosis of hypertension designated by specific ICD-9-CM codes. Patients may have been prescribed antihypertensive medications for other indications, such as heart failure, migraine, anxiety, etc. Our results apply to all patients prescribed antihypertensive agents, and although most had hypertension, there may be differences in first-fill rates for those with and without hypertension.
Third, patients were required to fill their prescriptions through insurance. In community pharmacy settings, some prescriptions may be paid for with cash due to the availability of several inexpensive generic antihypertensive medications (eg, a 30-day supply for $4, or 90-day supply for $10).23 Patients taking advantage of these promotions would result in an overestimation of first-fill failure rate.
Fourth, patients may have received samples from their physician and subsequently failed to obtain their antihypertensive prescription at the pharmacy because the medication sample was ineffective or not tolerated.
Fifth, claims data from physicians who were e-prescribing were used to proxy electronic prescriptions. However, some physicians may have handed patients their prescriptions, which, if never taken to the pharmacy, would result in an underestimation of first-fill failure rate.
CORRESPONDENCE
Catherine E. Cooke, President, PosiHealth, Inc., 5106 Bonnie Branch Road, Ellicott City, MD 21043; [email protected]
Purpose Despite numerous studies on adherence, there is little research on the first-fill rate of antihypertensive prescriptions. Our study took advantage of the recent increase in electronic prescribing (e-prescribing) and used data from e-prescribing physicians to determine the first-fill failure rate of antihypertensive prescriptions and to assess which factors predict first-fill failure.
Methods This retrospective study reviewed claims from a Mid-Atlantic managed care organization (MCO). We included adult members with continuous medical and pharmacy coverage who were prescribed an antihypertensive in 2008 by an e-prescribing physician. First-fill failure occurred when the patient did not obtain the antihypertensive medication due to either a denial by the MCO or reversal by the dispensing pharmacist. (Pharmacists reverse claims when a patient fails to pick up a medication.) Multivariate regression analysis determined the clinical and demographic factors associated with failure to fill.
Results The cohort consisted of 14,693 antihypertensive prescriptions, prescribed by 164 e-prescribing physicians for 7061 unique members. There were 2289 out of 14,693 prescriptions (15.6%) that went unfilled, affecting 24.3% of patients. Of the prescriptions not obtained, 1466 (64%) were denied by the MCO and 823 (36%) were reversed. Significant factors associated with first-fill failure were new diagnosis of hypertension, new antihypertensive agent, higher co-payment, and enrollment in a health maintenance organization or preferred provider organization.
Conclusions Patients newly diagnosed with hypertension and those prescribed a new antihypertensive were at particularly high risk for not obtaining their medication. Because nearly a quarter of patients did not obtain their initial fill of an antihypertensive prescription, future research should determine efficient and cost-effective systems to address first-fill failure in primary care.
Poor patient adherence to medical directives—the main cause of unsuccessful efforts to control hypertension1—is often difficult to assess in daily practice and in research. A common example of nonadherence is the failure to fill new prescriptions or to refill existing ones. In measuring adherence to first-fill and refilled prescriptions, investigators have often relied on patient self-report.2,3 However, this means of evaluation may be biased. One study found that patients markedly overstated their adherence to antihypertensive regimens, when compared with adherence measured by prescriptions actually filled.4
Objectively determining the rate of first-fill failure (not obtaining the initial fill of a prescription) has typically been cumbersome, requiring time-consuming chart reviews, which is unrealistic for studying large populations. A more efficient way to collect these data is through electronic prescribing (e-prescribing)—the electronic transmission of prescription or prescription-related information between a prescriber, a dispenser, and a pharmacy benefit manager or health plan, either directly or through an intermediary service.5
Our study sought to extend previous knowledge of adherence by determining the rate of first-fill failure for antihypertensive agents prescribed by electronic means, as well as identifying the clinical and demographic factors most closely associated with that failure. We believe e-prescribing may offer a way to improve antihypertensive medication adherence, especially for particular subgroups of patients, by providing information on the patient’s formulary and fill status notification.
Methods
This retrospective study used administrative, medical, and pharmacy data from a Mid-Atlantic managed care organization (MCO) serving 3.3 million medical and 1.2 million pharmacy members. To be eligible for inclusion, a member had to have an antihypertensive agent prescribed by a physician using e-prescribing. Our assumption in reviewing only prescriptions written by e-prescribing physicians was that each prescription would have a corresponding claim. To recruit a minimum of 100 electronic prescribers, we began by surveying physicians who had prescribed the highest volume of antihypertensive medication during the first half of 2008. We faxed a survey to these physicians, and if we received no response, we followed up by phone. Our final sample of physicians comprised those who were e-prescribing at least 75% of the time before January 1, 2008.6
A pharmacy claims query identified all antihypertensive prescriptions from January 1, 2008 through December 31, 2008 that were coded as new (a new prescription for either a new agent or the same agent the patient had been taking) and were prescribed by our group of electronic prescribers. We excluded members (and their prescription claims) who were younger than 18 years on the date of their first prescription and those who were not continuously enrolled in the same medical and pharmacy benefit plan from July 1, 2006 through December 31, 2008.
For each prescription, 3 claim options were possible: paid, denied, or reversed.
A paid claim meant that the prescription was approved by the MCO for coverage and that the member obtained the medication.
A denied claim occurred when coverage for the prescribed product was refused by the MCO.
A reversed claim meant that the prescription had been approved by the MCO for coverage, but the approved claim was later reversed by the pharmacist when a patient failed to pick up the prescription within 14 days.
A denied or reversed claim meant that the patient did not receive the medication, and this occurrence was labeled as failure to fill.
For members in the cohort, a medical claims query identified hypertension using specific International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes in the 401 category from July 1, 2006 through December 31, 2008. We deemed patients as newly diagnosed with hypertension if their first ICD-9-CM code for hypertension was within the preceding 6 months of the first antihypertensive prescription.
Outcome measures
The primary outcome measure was the percentage of new antihypertensive prescriptions that patients failed to obtain. To calculate this number, we designated the numerator as the number of denied or reversed claims for antihypertensive prescriptions, and the denominator as the overall number of antihypertensive prescriptions in the cohort.
The secondary outcome measure was the set of clinical and demographic factors related to failure to obtain the first fill. We evaluated the possible association of first-fill failure with age, sex, prior antihypertensive use, hypertension diagnosis, formulary status, co-payment, monotherapy vs combination product, pharmacologic category, type of health plan, and number of antihypertensive prescriptions.
All data collection conformed to patient privacy standards set by the Health Insurance Portability and Accountability Act (HIPAA), and the dataset was delivered to the researchers with de-identified patient information. The University of Maryland, Baltimore (UMB) Institutional Review Board (IRB) fully approved the research protocol.
Statistical analysis
Statistical analysis included descriptive statistics such as percentages for discrete variables (eg, sex) and calculations of means and standard deviations (SD) for continuous variables (eg, age). Univariate analyses examined the correlation between clinical/demographic characteristics and first-fill rates. We used binomial logistic regression to assess predictors of first-fill failure. We set statistical significance at an accepted alpha (P<.05).
Results
E-prescribing physicians
There were 1313 e-prescribing physicians ranked according to antihypertensive prescription volume. We contacted 457 physicians who prescribed the highest volume of medications and selected a final group of 164.
Patient/prescription cohort
The cohort consisted of 14,693 antihypertensive prescriptions prescribed by the 164 e-prescribing physicians. There were 7061 unique members with a mean age of 55.1±11.4 years (TABLE 1). Half were men (51.8%), and each member had a mean of 1.9 antihypertensive prescriptions. About two-thirds had a diagnosis of hypertension, as represented by ICD-9-CM codes.
Three-fourths of the prescriptions were for generic antihypertensives. ACE inhibitors were the most commonly prescribed class of drug, at 24.2%, followed by beta-blockers, angiotensin-receptor blockers, diuretics, and calcium channel blockers. Agents not fitting into the above classes were prescribed the least, at 2.8% of prescription volume. The mean co-payment per antihypertensive prescription was $17.00±$20.73.
Primary outcome
Patients failed to obtain the antihypertensive medication for 2289/14,693 (15.6%) prescriptions. Of the prescriptions not obtained, 1466 (64%) were denied and 823 (36%) were reversed. Failure to obtain the 2289 prescriptions affected 24.3% (1713/7061) of patients.
Secondary outcome
We compared clinical and demographic characteristics between the 2 outcome groups (TABLE 2). Univariate analyses revealed statistically significant differences for age, history of antihypertensive use and hypertension diagnosis, formulary status, medication characteristics, and type of health plan. Patients prescribed a new antihypertensive product or receiving a new diagnosis of hypertension were significantly less likely to fill their prescriptions (P<.001). Prescriptions for brand and combination products were, respectively, 2.2 percentage points (P=.025) and 3 percentage points (P=.002) higher in the failure-to-obtain category than in the obtained category. The difference in mean co-payment was $2.56 higher in the failure-to-obtain group (P<.001). There were differences between the obtained and failure-to-obtain groups based on the member’s type of health plan (P<.001).
Statistically significant factors from univariate analyses were included in the logistic regression model (data not shown). Factors associated with failure to obtain an antihypertensive prescription fell into 3 categories: history of hypertension (new vs existing diagnosis), formulary status of antihypertensive agent, and type of health plan. Prescriptions for new antihypertensive products were 49.44 times more likely to go unfilled (P<.001). Prescriptions were 1.73 times more likely to remain unfilled for members with a new diagnosis for hypertension (P<.001). In addition, the formulary status of the prescription showed that prescriptions were less likely to be filled for brand products (P=.030) or for those requiring higher co-payments (P<.001). Compared with indemnity health plans, health maintenance organizations and preferred provider organizations were more likely to be associated with unfilled prescriptions (P<.001 and P=.044, respectively).
TABLE 2
Prescription characteristics associated with different claims outcomes (N=14,693)*
| Variable | Obtained antihyper-tensive (n=12,404) | Failed to obtain antihypertensive (n=2289) | P value |
|---|---|---|---|
| Age | |||
| Mean ±SD, y | 56.2 ±11.4 | 55.4 ±11.9 | .002 |
| Sex | |||
| Male | 6581 (53.1) | 1182 (51.6) | .212 |
| Female | 5823 (46.9) | 1107 (48.4) | |
| Prior antihypertensive prescriptions | |||
| New antihypertensive product (no pharmacy claims for this agent within prior 6 months) | 41 (0.3) | 383 (16.7) | <.001 |
| Hypertension diagnosis | |||
| New diagnosis (at least 1 medical claim for HTN <6 months prior and no medical claims for HTN >6 months prior to antihypertensive prescription) | 626 (5.0) | 367 (16.0) | <.001 |
| Monotherapy/combination product | |||
| Monotherapy | 9482 (76.4) | 1681 (73.4) | .002 |
| Combination | 2922 (23.6) | 608 (26.6) | |
| Brand or generic status of product | |||
| Generic | 9350 (75.4) | 1675 (73.2) | .025 |
| Brand | 3054 (24.6) | 614 (26.8) | |
| Tier status | |||
| Tier 1 | 9350 (75.4) | 1675 (73.2) | .074 |
| Tier 2 | 1282 (10.3) | 252 (11.0) | |
| Tier 3 | 1772 (14.3) | 362 (15.8) | |
| Co-payment | |||
| Mean ±SD | $16.60±$20.17 | $19.16±$23.43 | <.001 |
| Type of health plan | |||
| Health maintenance organization | 5574 (44.9) | 1188 (51.9) | <.001 |
| Preferred provider organization | 2372 (19.1) | 426 (18.6) | |
| Consumer directed | 1847 (14.9) | 278 (12.1) | |
| Indemnity | 2611 (21.0) | 397 (17.3) | |
| Number of antihypertensive prescriptions | |||
| Mean ±SD | 1.9 ±1.0 | 1.8 ±1.0 | .001 |
| Therapeutic class | |||
| Angiotensin-converting enzyme inhibitors | 3008 (24.3) | 548 (23.9) | .939 |
| Angiotensin-receptor blockers | 2296 (18.5) | 442 (19.3) | |
| Beta-blockers | 2461 (19.8) | 440 (19.2) | |
| Calcium channel blockers (including combination product with statin) | 2047 (16.5) | 382 (16.7) | |
| Diuretics | 2242 (18.1) | 410 (17.9) | |
| Other: Alpha-adrenergic blocking agents, central alpha-agonists, direct vasodilators, hypotensive agents, peripheral adrenergic inhibitors, renin inhibitors | 350 (2.8) | 67 (2.9) | |
| HTN, hypertension. *Data are presented as n(%) unless otherwise noted. | |||
Discussion
This study used e-prescribing to evaluate nonadherence to the first-fill of an antihypertensive prescription. Our findings that 24.3% of patients did not obtain the first-fill of a medication and that 15.6% of prescriptions remained unclaimed are comparable to those of other research using electronically obtained prescription data.7,8
In a cross-sectional study of 327 African American adults enrolled in a Medicaid managed care plan, the authors reported that 24.9% (433/1742) of antihypertensive prescriptions were unfilled.7 In a study of therapeutically naïve patients, the first-fill failure rate was 17%.8 These patients were less likely to fill their antihypertensive prescriptions if they were prescribed loop diuretics or had a higher prescription co-payment. The median co-payment was $2 higher for prescriptions not obtained, compared with those that were obtained (P<.001). This finding was similar to the $2.56 difference we found for mean co-payment.
Higher co-payment was a strong predictor of decreased adherence in other antihypertensive adherence studies.9,10 In a survey of Medicare patients, the most common reason cited for failing to fill any prescription was that “it would cost too much.”2 Prescribing a less costly agent based on an insurer’s formulary may reduce the first-fill failure rate.
Although educating patients about their disease, involving family, and increasing patient participation through self-monitoring of blood pressure all have a positive impact on adherence rates and blood pressure control, physicians are hard pressed for time during an office visit to address such interventions.11-19 E-prescribing potentially offers a more efficient way to improve antihypertensive medication adherence. A recent ruling by the Centers for Medicare & Medicaid Services (CMS) requires e-prescribing systems to have the capability of providing formulary and benefit transaction, medication history transaction, and fill status notification to prescribers.20 Prescribers can readily access patients’ insurance coverage information. Formulary decision support, as part of an e-prescribing system, has been shown to increase use of formulary products.21 Fill status notification allows two-way communication between the prescriber and pharmacy so that prescribers can be made aware if patients fail to fill prescriptions.
Unfortunately, e-prescribing is not yet widely used. Approximately 26% of office-based US physicians use e-prescribing, and only 30% of them take advantage of formulary information.22 E-prescribing authorities believe practices not using the fill status notification probably lack resources needed to manage patients who are nonadherent.22 While it may not be necessary to check whether all patients have obtained their prescription, it may be useful for subgroups of patients, such as those who have received a new diagnosis, whose disease is poorly controlled, who are prescribed new antihypertensive agents, or who are otherwise thought to be nonadherent.
Study limitations. First, claims data serve as a proxy for medication adherence. Even though a patient obtained an antihypertensive prescription according to claims data, this does not guarantee that the patient used the medication.
Second, not all patients had a diagnosis of hypertension designated by specific ICD-9-CM codes. Patients may have been prescribed antihypertensive medications for other indications, such as heart failure, migraine, anxiety, etc. Our results apply to all patients prescribed antihypertensive agents, and although most had hypertension, there may be differences in first-fill rates for those with and without hypertension.
Third, patients were required to fill their prescriptions through insurance. In community pharmacy settings, some prescriptions may be paid for with cash due to the availability of several inexpensive generic antihypertensive medications (eg, a 30-day supply for $4, or 90-day supply for $10).23 Patients taking advantage of these promotions would result in an overestimation of first-fill failure rate.
Fourth, patients may have received samples from their physician and subsequently failed to obtain their antihypertensive prescription at the pharmacy because the medication sample was ineffective or not tolerated.
Fifth, claims data from physicians who were e-prescribing were used to proxy electronic prescriptions. However, some physicians may have handed patients their prescriptions, which, if never taken to the pharmacy, would result in an underestimation of first-fill failure rate.
CORRESPONDENCE
Catherine E. Cooke, President, PosiHealth, Inc., 5106 Bonnie Branch Road, Ellicott City, MD 21043; [email protected]
1. Sabate E. ed. Adherence to long-term therapies: evidence for action. Geneva, Switzerland. World Health Organization, 20030. Available at: http://www.who.int/chp/knowledge/publications/adherence_report/en. Accessed May 20, 2011.
2. Kennedy J, Tuleu I, Mackay K. Unfilled prescriptions of Medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm. 2008;14:553-560.
3. Esposito D, Schone E, Williams T, et al. Prevalence of unclaimed prescriptions at military pharmacies. J Manag Care Pharm. 2008;14:541-552.
4. Wang PS, Benner JS, Glynn RJ, et al. How well do patients report noncompliance with antihypertensive medications? a comparison of self-report versus filled prescriptions. Pharmacoepidemiol Drug Saf. 2004;13:11-19.
5. eHealth Initiative and The Center for Improving Medication Management. A clinician’s guide to electronic prescribing. White paper from the eHealth Initiative and The Center for Improving Medication Management, 2008. Available at: http://www.ehealthinitiative.org/sites/default/files/e-Prescribing_Clinicians_Guide_Final(1).pdf. Accessed March 21, 2010.
6. Solberg LI, Asche SE, Pawlson LG, et al. Practice systems are associated with high-quality care for diabetes. Am J Manag Care. 2008;14:85-92.
7. Lagu T, Weiner MG, Eachus S, et al. Effect of patient comorbidities on filling of antihypertensive prescriptions Am J Manag Care. 2009;15:24-30.
8. Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens. 2009;22:392-396.
9. Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298:61-69.
10. Kamal-Bahl S, Briesacher B. How do incentive-based formularies influence drug selection and spending for hypertension? Health Aff. 2004;23:227-236.
11. Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72:115-121.
12. Boulware LE, Daumit GL, Frick KD, et al. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001;21:221-232.
13. Feldman R, Bacher M, Campbell N, et al. Adherence to pharmacologic management of hypertension. Can J Public Health. 1998;89:I16-I18.
14. Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15-minute visit. Arch Intern Med. 2008;168:1843-1852.
15. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028-3035.
16. Morisky DE, Levine DM, Green LW, et al. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983;73:153-162.
17. Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657-665.
18. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care visits. Health Serv Res. 2007;42:1871-1894.
19. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
20. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; standards for e-prescribing under Medicare Part D and identification of backward compatible version of adopted standard for e-prescribing and the Medicare prescription drug program (version 8.1). Final rule. Fed Regist. 2008;73:18917-18942.
21. Fischer MA, Vogeli C, Stedman M, et al. Effect of electronic prescribing with formulary decision support on medication use and cost. Arch Intern Med. 2008;168:2433-2439.
22. SureScripts 2009 Progress Report on E-Prescribing. Available at: http://www.surescripts.com/downloads/NPR/national-progress-report.pdf. Accessed March 21, 2010.
23. Walmart. Retail prescription program drug list. Available at: http://i.walmartimages.com/i/if/hmp/fusion/customer_list.pdf. Accessed March 21, 2010.
1. Sabate E. ed. Adherence to long-term therapies: evidence for action. Geneva, Switzerland. World Health Organization, 20030. Available at: http://www.who.int/chp/knowledge/publications/adherence_report/en. Accessed May 20, 2011.
2. Kennedy J, Tuleu I, Mackay K. Unfilled prescriptions of Medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm. 2008;14:553-560.
3. Esposito D, Schone E, Williams T, et al. Prevalence of unclaimed prescriptions at military pharmacies. J Manag Care Pharm. 2008;14:541-552.
4. Wang PS, Benner JS, Glynn RJ, et al. How well do patients report noncompliance with antihypertensive medications? a comparison of self-report versus filled prescriptions. Pharmacoepidemiol Drug Saf. 2004;13:11-19.
5. eHealth Initiative and The Center for Improving Medication Management. A clinician’s guide to electronic prescribing. White paper from the eHealth Initiative and The Center for Improving Medication Management, 2008. Available at: http://www.ehealthinitiative.org/sites/default/files/e-Prescribing_Clinicians_Guide_Final(1).pdf. Accessed March 21, 2010.
6. Solberg LI, Asche SE, Pawlson LG, et al. Practice systems are associated with high-quality care for diabetes. Am J Manag Care. 2008;14:85-92.
7. Lagu T, Weiner MG, Eachus S, et al. Effect of patient comorbidities on filling of antihypertensive prescriptions Am J Manag Care. 2009;15:24-30.
8. Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens. 2009;22:392-396.
9. Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298:61-69.
10. Kamal-Bahl S, Briesacher B. How do incentive-based formularies influence drug selection and spending for hypertension? Health Aff. 2004;23:227-236.
11. Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72:115-121.
12. Boulware LE, Daumit GL, Frick KD, et al. An evidence-based review of patient-centered behavioral interventions for hypertension. Am J Prev Med. 2001;21:221-232.
13. Feldman R, Bacher M, Campbell N, et al. Adherence to pharmacologic management of hypertension. Can J Public Health. 1998;89:I16-I18.
14. Fiscella K, Epstein RM. So much to do, so little time: care for the socially disadvantaged and the 15-minute visit. Arch Intern Med. 2008;168:1843-1852.
15. Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028-3035.
16. Morisky DE, Levine DM, Green LW, et al. Five-year blood pressure control and mortality following health education for hypertensive patients. Am J Public Health. 1983;73:153-162.
17. Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657-665.
18. Tai-Seale M, McGuire TG, Zhang W. Time allocation in primary care visits. Health Serv Res. 2007;42:1871-1894.
19. Yarnall KS, Pollak KI, Østbye T, et al. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635-641.
20. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; standards for e-prescribing under Medicare Part D and identification of backward compatible version of adopted standard for e-prescribing and the Medicare prescription drug program (version 8.1). Final rule. Fed Regist. 2008;73:18917-18942.
21. Fischer MA, Vogeli C, Stedman M, et al. Effect of electronic prescribing with formulary decision support on medication use and cost. Arch Intern Med. 2008;168:2433-2439.
22. SureScripts 2009 Progress Report on E-Prescribing. Available at: http://www.surescripts.com/downloads/NPR/national-progress-report.pdf. Accessed March 21, 2010.
23. Walmart. Retail prescription program drug list. Available at: http://i.walmartimages.com/i/if/hmp/fusion/customer_list.pdf. Accessed March 21, 2010.