User login
Do PFAs Cause Kidney Cancer? VA to Investigate
The US Department of Veterans Affairs (VA) will conduct a scientific assessment to find out in whether kidney cancer should be considered a presumptive service-connected condition for veterans exposed to per- and polyfluoroalkyl substances (PFAs). This assessment is the first step in the VA presumptive condition investigative process, which could allow exposed veterans who were exposed to PFAs during their service to access more VA services.
A class of more than 12,000 chemicals, PFAs have been used in the military since the early 1970s in many items, including military-grade firefighting foam. Studies have already suggested links between the so-called forever chemicals and cancer, particularly kidney cancer.
The US Department of Defense (DoD) is assessing contamination at hundreds of sites, while the National Defense Authorization Act in Fiscal Year 2020 mandated that DoD stop using those foams starting in October and remove all stocks from active and former installations and equipment. That may not happen until next year, though, because the DoD has requested a waiver through October 2025 and may extend it through 2026.
When a condition is considered presumptive, eligible veterans do not need to prove their service caused their disease to receive benefits. As part of the Biden Administration’s efforts to expand benefits and services for toxin-exposed veterans and their families, the VA expedited health care and benefits eligibility under the PACT Act by several years—including extending presumptions for head cancer, neck cancer, gastrointestinal cancer, reproductive cancer, lymphoma, pancreatic cancer, kidney cancer, melanoma, and hypertension for Vietnam era veterans. The VA has also extended presumptions for > 300 new conditions, most recently for male breast cancer, urethral cancer, and cancer of the paraurethral glands.
Whether a condition is an established presumptive condition or not, the VA will consider claims on a case-by-case basis and can grant disability compensation benefits if sufficient evidence of service connection is found. “[M]ake no mistake: Veterans should not wait for the outcome of this review to apply for the benefits and care they deserve,” VA Secretary Denis McDonough said in a release. “If you’re a veteran and believe your military service has negatively impacted your health, we encourage you to apply for VA care and benefits today.”
The public has 30 days to comment on the proposed scientific assessment between PFAs exposure and kidney cancer via the Federal Register. The VA is set to host a listening session on Nov. 19, 2024, to allow individuals to share research and input. Interested individuals may register to participate. The public may also comment via either forum on other conditions that would benefit from review for potential service-connection.
The US Department of Veterans Affairs (VA) will conduct a scientific assessment to find out in whether kidney cancer should be considered a presumptive service-connected condition for veterans exposed to per- and polyfluoroalkyl substances (PFAs). This assessment is the first step in the VA presumptive condition investigative process, which could allow exposed veterans who were exposed to PFAs during their service to access more VA services.
A class of more than 12,000 chemicals, PFAs have been used in the military since the early 1970s in many items, including military-grade firefighting foam. Studies have already suggested links between the so-called forever chemicals and cancer, particularly kidney cancer.
The US Department of Defense (DoD) is assessing contamination at hundreds of sites, while the National Defense Authorization Act in Fiscal Year 2020 mandated that DoD stop using those foams starting in October and remove all stocks from active and former installations and equipment. That may not happen until next year, though, because the DoD has requested a waiver through October 2025 and may extend it through 2026.
When a condition is considered presumptive, eligible veterans do not need to prove their service caused their disease to receive benefits. As part of the Biden Administration’s efforts to expand benefits and services for toxin-exposed veterans and their families, the VA expedited health care and benefits eligibility under the PACT Act by several years—including extending presumptions for head cancer, neck cancer, gastrointestinal cancer, reproductive cancer, lymphoma, pancreatic cancer, kidney cancer, melanoma, and hypertension for Vietnam era veterans. The VA has also extended presumptions for > 300 new conditions, most recently for male breast cancer, urethral cancer, and cancer of the paraurethral glands.
Whether a condition is an established presumptive condition or not, the VA will consider claims on a case-by-case basis and can grant disability compensation benefits if sufficient evidence of service connection is found. “[M]ake no mistake: Veterans should not wait for the outcome of this review to apply for the benefits and care they deserve,” VA Secretary Denis McDonough said in a release. “If you’re a veteran and believe your military service has negatively impacted your health, we encourage you to apply for VA care and benefits today.”
The public has 30 days to comment on the proposed scientific assessment between PFAs exposure and kidney cancer via the Federal Register. The VA is set to host a listening session on Nov. 19, 2024, to allow individuals to share research and input. Interested individuals may register to participate. The public may also comment via either forum on other conditions that would benefit from review for potential service-connection.
The US Department of Veterans Affairs (VA) will conduct a scientific assessment to find out in whether kidney cancer should be considered a presumptive service-connected condition for veterans exposed to per- and polyfluoroalkyl substances (PFAs). This assessment is the first step in the VA presumptive condition investigative process, which could allow exposed veterans who were exposed to PFAs during their service to access more VA services.
A class of more than 12,000 chemicals, PFAs have been used in the military since the early 1970s in many items, including military-grade firefighting foam. Studies have already suggested links between the so-called forever chemicals and cancer, particularly kidney cancer.
The US Department of Defense (DoD) is assessing contamination at hundreds of sites, while the National Defense Authorization Act in Fiscal Year 2020 mandated that DoD stop using those foams starting in October and remove all stocks from active and former installations and equipment. That may not happen until next year, though, because the DoD has requested a waiver through October 2025 and may extend it through 2026.
When a condition is considered presumptive, eligible veterans do not need to prove their service caused their disease to receive benefits. As part of the Biden Administration’s efforts to expand benefits and services for toxin-exposed veterans and their families, the VA expedited health care and benefits eligibility under the PACT Act by several years—including extending presumptions for head cancer, neck cancer, gastrointestinal cancer, reproductive cancer, lymphoma, pancreatic cancer, kidney cancer, melanoma, and hypertension for Vietnam era veterans. The VA has also extended presumptions for > 300 new conditions, most recently for male breast cancer, urethral cancer, and cancer of the paraurethral glands.
Whether a condition is an established presumptive condition or not, the VA will consider claims on a case-by-case basis and can grant disability compensation benefits if sufficient evidence of service connection is found. “[M]ake no mistake: Veterans should not wait for the outcome of this review to apply for the benefits and care they deserve,” VA Secretary Denis McDonough said in a release. “If you’re a veteran and believe your military service has negatively impacted your health, we encourage you to apply for VA care and benefits today.”
The public has 30 days to comment on the proposed scientific assessment between PFAs exposure and kidney cancer via the Federal Register. The VA is set to host a listening session on Nov. 19, 2024, to allow individuals to share research and input. Interested individuals may register to participate. The public may also comment via either forum on other conditions that would benefit from review for potential service-connection.
Vancomycin AUC-Dosing Initiative at a Regional Antibiotic Stewardship Collaborative
Antimicrobial resistance is a global threat and burden to health care, with > 2.8 million antibiotic-resistant infections occurring annually in the United States.1 To combat this issue and improve patient care, the US Department of Veterans Affairs (VA) has implemented antimicrobial stewardship programs (ASPs) across its health care systems. ASPs are multidisciplinary teams that promote evidence-based use of antimicrobials through activities supporting appropriate selection, dosing, route, and duration of antimicrobial therapy. ASP best practices are also included in the Joint Commission and Centers for Medicare and Medicaid Services accreditation standards.2
The foundational charge for VA facilities to develop and maintain ASPs was outlined in 2014 and updated in 2023 in the Veterans Health Administration (VHA) Directive 1031 on antimicrobial stewardship programs.2 This directive outlines specific requirements for all VA ASPs, including personnel, staffing levels, and the roles and responsibilities of all team members. VHA now requires that Veterans Integrated Services Networks (VISNs) establish robust ASP collaboratives. A VISN ASP collaborative consists of stewardship champions from each VA medical center in the VISN and is designed to support, develop, and enhance ASP programs across all facilities within that VISN.2 Some VISNs may lack an ASP collaborative altogether, and others with existing groups may seek ways to expand their collaboratives in line with the updated directive. Prior to VHA Directive 1031, the VA Sunshine Healthcare Network (VISN 8) established an ASP collaborative. This article describes the structure and activities of the VISN 8 ASP collaborative and highlights a recent VISN 8 quality assurance initiative related to vancomycin area under the curve (AUC) dosing that illustrates how ASP collaboratives can enhance stewardship and clinical care across broad geographic areas.
VISN 8 ASP
The VHA, the largest integrated US health care system, is divided into 18 VISNs that provide regional systems of care to enhance access and meet the local health care needs of veterans.3 VISN 8 serves > 1.5 million veterans across 165,759 km2 in Florida, South Georgia, Puerto Rico, and the US Virgin Islands.4 The network is composed of 7 health systems with 8 medical centers and > 60 outpatient clinics. These facilities provide comprehensive acute, primary, and specialty care, as well as mental health and extended care services in inpatient, outpatient, nursing home, and home care settings.4
The 2023 VHA Directive 1031 update recognizes the importance of VISN-level coordination of ASP activities to enhance the standardization of care and build partnerships in stewardship across all levels of care. The VISN 8 ASP collaborative workgroup (ASPWG) was established in 2015. Consistent with Directive 1031, the ASPWG is guided by clinician and pharmacist VISN leads. These leads serve as subject matter experts, facilitate access to resources, establish VISN-level consensus, and enhance communication among local ASP champions at medical centers within the VISN. All 7 health systems include = 1 ASP champion (clinician or pharmacist) in the ASPWG. Ad hoc members, whose routine duties are not solely focused on antimicrobial stewardship, contribute to specific stewardship projects as needed. For example, the ASPWG has included internal medicine, emergency department, community living center pharmacists, representatives from pharmacy administration, and trainees (pharmacy students and residents, and infectious diseases fellows) in antimicrobial stewardship initiatives. The inclusion of non-ASP champions is not discussed in VHA Directive 1031. However, these members have made valuable contributions to the ASPWG.
The ASPWG meets monthly. Agendas and priorities are developed by the VISN pharmacist and health care practitioner (HCP) leads. Monthly discussions may include but are not limited to a review of national formulary decisions, VISN goals and metrics, infectious diseases hot topics, pharmacoeconomic initiatives, strong practice presentations, regulatory and accreditation preparation, preparation of tracking reports, as well as the development of both patient-level and HCPlevel tools, resources, and education materials. This forum facilitates collaborative learning: members process and synthesize information, share and reframe ideas, and listen to other viewpoints to gain a complete understanding as a group.5 For example, ASPWG members have leaned on each other to prepare for Joint Commission accreditation surveys and strengthen the VISN 8 COVID-19 program through the rollout of vaccines and treatments. Other collaborative projects completed over the past few years included a penicillin allergy testing initiative and anti-methicillin-resistant Staphylococcus aureus (MRSA) and pseudomonal medication use evaluations. This team-centric problem-solving approach is highly effective while also fostering professional and social relationships. However, collaboratives could be perceived to have drawbacks. There may be opportunity costs if ASP time is allocated for issues that have already been addressed locally or concerns that standardization might hinder rapid adoption of practices at individual sites. Therefore, participation in each distinct group initiative is optional. This allows sites to choose projects related to their high priority areas and maintain bandwidth to implement practices not yet adopted by the larger group.
The ASPWG tracks metrics related to antimicrobial use with quarterly data presented by the VISN pharmacist lead. Both inpatient and outpatient metrics are evaluated, such as days of therapy per 1000 days and outpatient antibiotic prescriptions per 1000 unique patients. Facilities are benchmarked against their own historical data and other VISN sites, as well as other VISNs across the country. When outliers are identified, facilities are encouraged to conduct local projects to identify reasons for different antimicrobial use patterns and subsequent initiatives to optimize antimicrobial use. Benchmarking against VISN facilities can be useful since VISN facilities may be more similar than facilities in different geographic regions. Each year, the ASPWG reviews the current metrics, makes adjustments to address VISN priorities, and votes for approval of the metrics that will be tracked in the coming year.
Participation in an ASP collaborative streamlines the rollout of ASP and quality improvement initiatives across multiple sites, allowing ASPs to impact a greater number of veterans and evaluate initiatives on a larger scale. In 2019, with the anticipation of revised vancomycin dosing and monitoring guidelines, our ASPWG began to strategize the transition to AUC-based vancomycin monitoring.6 This multisite initiative showcases the strengths of implementing and evaluating practice changes as part of an ASP collaborative.
Vancomycin Dosing
The antibiotic vancomycin is used primarily for the treatment of MRSA infections.6 The 2020 consensus guidelines for vancomycin therapeutic monitoring recommend using the AUC to minimum inhibitory concentration (MIC) ratio as the pharmacodynamic target for serious MRSA infections, with an AUC/MIC goal of 400 to 600 mcg*h/mL.6 Prior guidelines recommended using vancomycin trough concentrations of 15 to 20 mcg/mL as a surrogate for this AUC target. However, subsequent studies have shown that trough-based dosing is associated with higher vancomycin exposures, supratherapeutic AUCs, and increased risk of vancomycin-associated acute kidney injury (AKI).7,8 Therefore, more direct AUC estimation is now recommended.6 The preferred approach for AUC calculations is through Bayesian modeling. Due to limited resources and software availability, many facilities use an alternative method involving 2 postdistributive serum vancomycin concentrations and first-order pharmacokinetic equations. This approach can optimize vancomycin dosing but is more mathematically and logistically challenging. Transitioning from troughto AUC-based vancomycin monitoring requires careful planning and comprehensive staff education.
In 2019, the VISN 8 ASPWG created a comprehensive vancomycin AUC toolkit to facilitate implementation. Components included a pharmacokinetic management policy and procedure, a vancomycin dosing guide, a progress note template, educational materials specific to pharmacy, nursing, laboratory, and medical services, a pharmacist competency examination, and a vancomycin AUC calculator (eAppendix). Each component was developed by a subgroup with the understanding that sites could incorporate variations based on local practices and needs.

The vancomycin AUC calculator was developed to be user-friendly and included safety validation protocols to prevent the entry of erroneous data (eg, unrealistic patient weight or laboratory values). The calculator allowed users to copy data into the electronic health record to avoid manual transcription errors and improve operational efficiency. It offered suggested volume of distribution estimates and 2 methods to estimate elimination constant (Ke ) depending on the patient’s weight.9,10 Creatinine clearance could be estimated using serum creatinine or cystatin C and considered amputation history. The default AUC goal in the calculator was 400 to 550 mcg*h/mL. This range was chosen based on consensus guidelines, data suggesting increased risk of AKI with AUCs > 515 mcg*h/mL, and the preference for conservative empiric dosing in the generally older VA population.11 The calculator suggested loading doses of about 25 mg/kg with a 2500 mg limit. VHA facilities could make limited modifications to the calculator based on local policies and procedures (eg, adjusting default infusion times or a dosing intervals).
The VISN 8 Pharmacy Pharmacokinetic Dosing Manual was developed as a comprehensive document to guide pharmacy staff with dosing vancomycin across diverse patient populations. This document included recommendations for renal function assessment, patient-specific considerations when choosing an empiric vancomycin dose, methods of ordering vancomycin peak, trough, and surveillance levels, dose determination based on 2 levels, and other clinical insights or frequently asked questions.
ASPWG members presented an accredited continuing education webinar for pharmacists, which reviewed the rationale for AUC-targeted dosing, changes to the current pharmacokinetic dosing program, case-based scenarios across various patient populations, and potential challenges associated with vancomycin AUC-based dosing. A recording of the live training was also made available. A vancomycin AUC dosing competency test was developed with 11 basic pharmacokinetic and case-based questions and comprehensive explanations provided for each answer.
VHA facilities implemented AUC dosing in a staggered manner, allowing for lessons learned at earlier adopters to be addressed proactively at later sites. The dosing calculator and education documents were updated iteratively as opportunities for improvement were discovered. ASPWG members held local office hours to address questions or concerns from staff at their facilities. Sharing standardized materials across the VISN reduced individual site workload and complications in rolling out this complex new process.
VISN-WIDE QUALITY ASSURANCE
At the time of project conception, 4 of 7 VISN 8 health systems had transitioned to AUC-based dosing. A quality assurance protocol to compare patient outcomes before and after changing to AUC dosing was developed. Each site followed local protocols for project approval and data were deidentified, collected, and aggregated for analysis.
The primary objectives were to compare the incidence of AKI and persistent bacteremia and assess rates of AUC target attainment (400-600 mcg*h/mL) in the AUC-based and trough-based dosing groups.6 Data for both groups included anthropomorphic measurements, serum creatinine, amputation status, vancomycin dosing, and infection characteristics. The X2 test was used for categorical data and the t test was used for continuous data. A 2-tailed α of 0.05 was used to determine significance. Each site sequentially reviewed all patients receiving ≥ 48 hours of intravenous vancomycin over a 3-month period and contributed up to 50 patients for each group. Due to staggered implementation, the study periods for sites spanned 2018 to 2023. A minimum 6-month washout period was observed between the trough and AUC groups at each site. Patients were excluded if pregnant, receiving renal replacement therapy, or presenting with AKI at the time of vancomycin initiation.
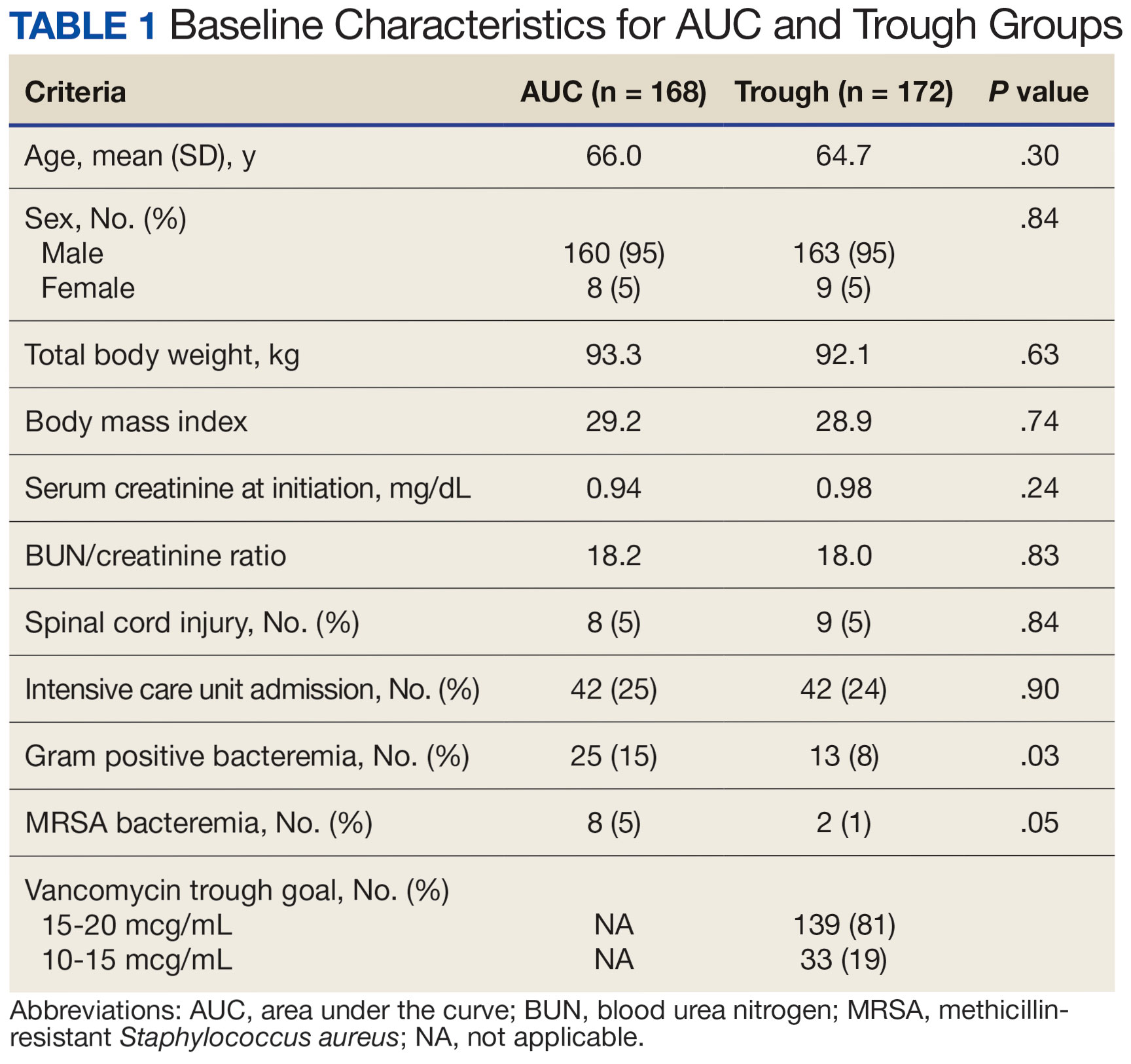
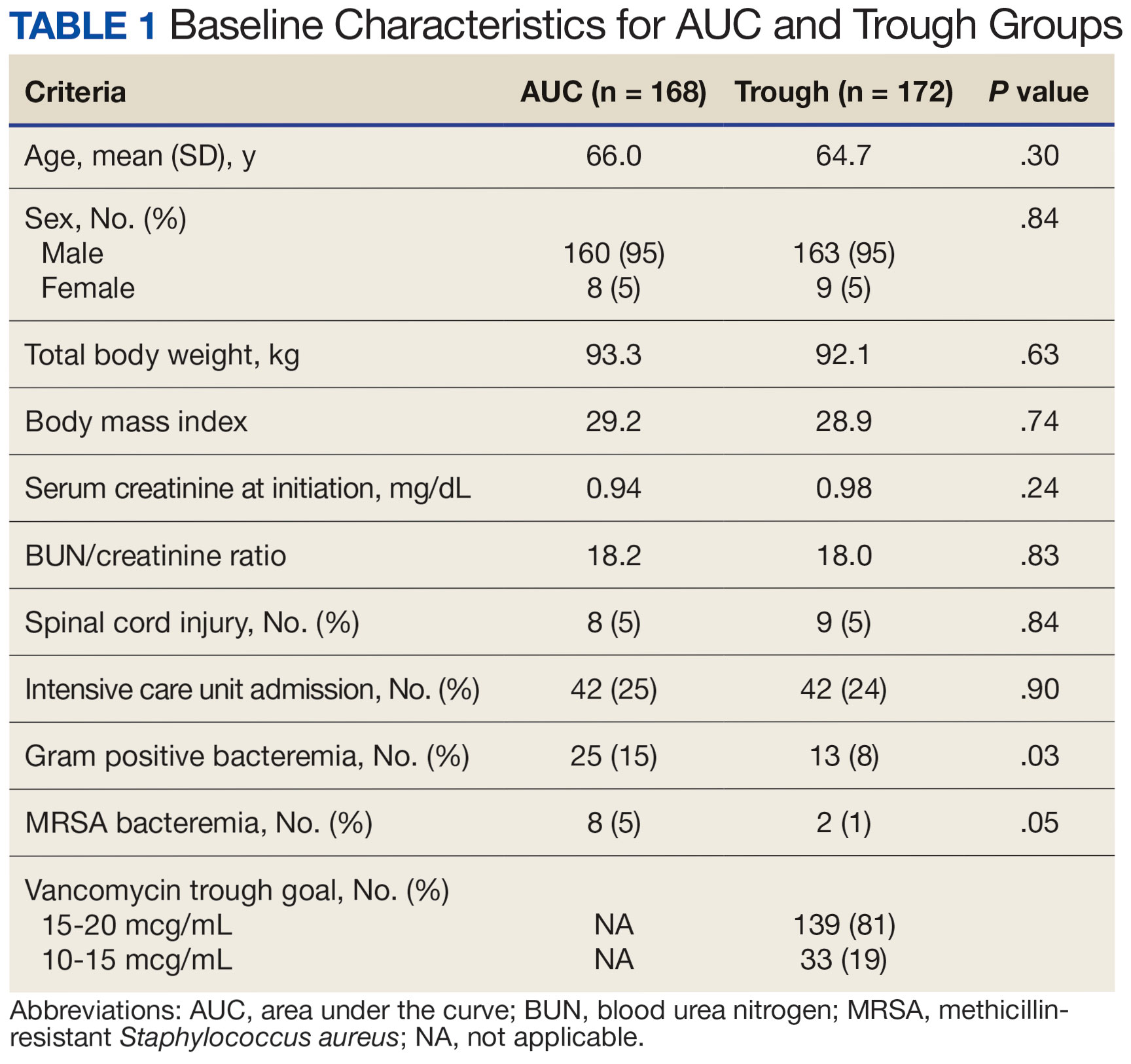
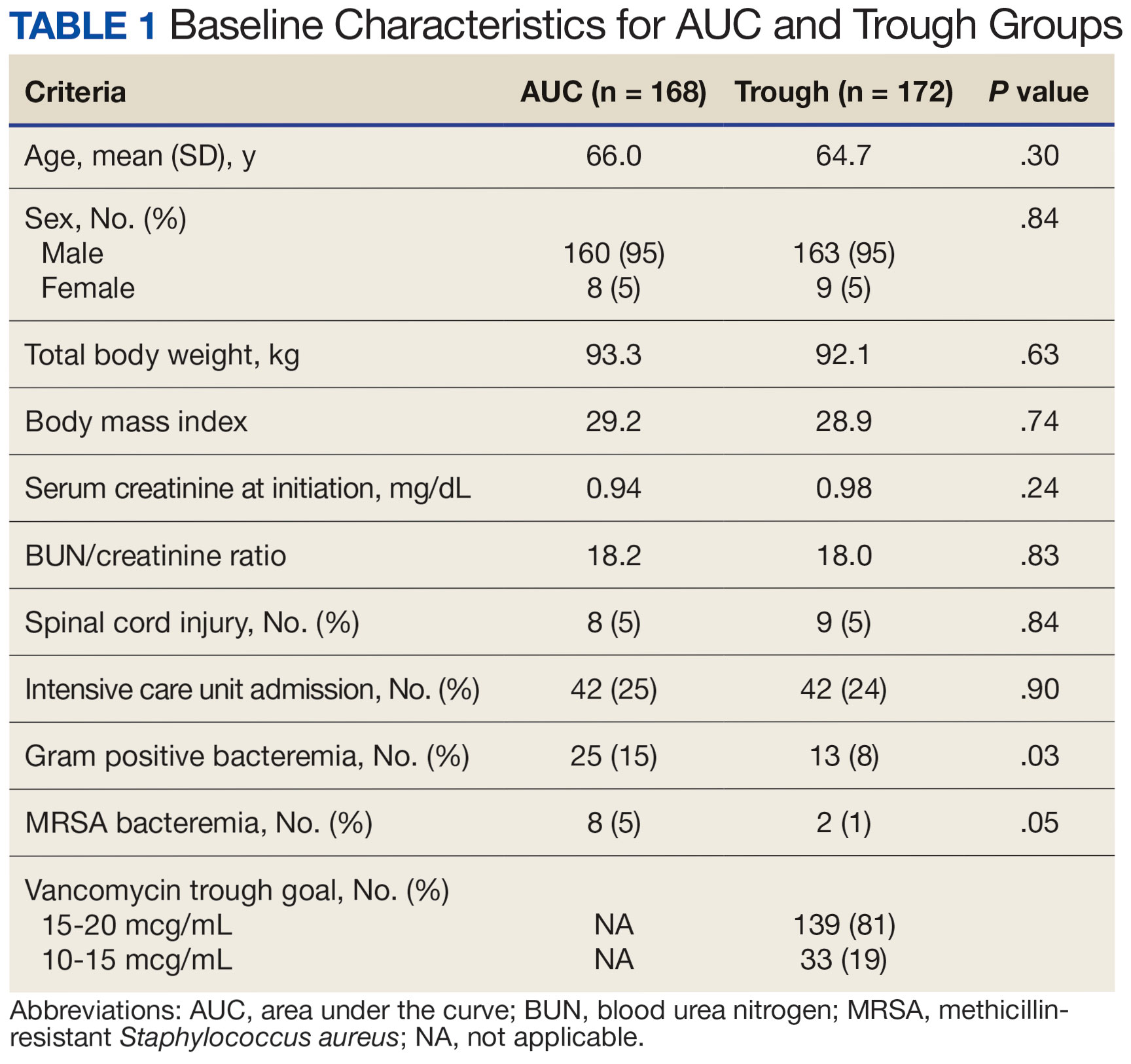
There were 168 patients in the AUC group and 172 patients in the trough group (Table 1). The rate of AUC target attainment with the initial dosing regimen varied across sites from 18% to 69% (mean, 48%). Total daily vancomycin exposure was lower in the AUC group compared with the trough group (2402 mg vs 2605 mg, respectively), with AUC-dosed patients being less likely to experience troughs level ≥ 15 or 20 mcg/mL (Table 2). There was a statistically significant lower rate of AKI in the AUC group: 2.4% in the AUC group (range, 2%-3%) vs 10.4% (range 7%-12%) in the trough group (P = .002). Rates of AKI were comparable to those observed in previous interventions.6 There was no statistical difference in length of stay, time to blood culture clearance, or rate of persistent bacteremia in the 2 groups, but these assessments were limited by sample size.

We did not anticipate such variability in initial target attainment across sites. The multisite quality assurance design allowed for qualitative evaluation of variability in dosing practices, which likely arose from sites and individual pharmacists having some flexibility in adjusting dosing tool parameters. Further analysis revealed that the facility with low initial target attainment was not routinely utilizing vancomycin loading doses. Sites routinely use robust loading doses achieved earlier and more consistent target attainment. Some sites used a narrower AUC target range in certain clinical scenarios (eg, > 500 mcg*h/mL for septic patients and < 500 mcg*h/mL for patients with less severe infections) rather than the 400 to 550 mcg*h/mL range for all patients. Sites targeting broader AUC ranges for all patients had higher rates of target attainment. Reviewing differences among sites allowed the ASPWG to identify best practices to optimize future care.
CONCLUSIONS
VHA ASPs must meet the standards outlined in VHA Directive 1031, including the new requirement for each VISN to develop an ASP collaborative. The VISN 8 ASPWG demonstrates how ASP champions can collaborate to solve common issues, complete tasks, explore new infectious diseases concepts, and impact large veteran populations. Furthermore, ASP collaboratives can harness their collective size to complete robust quality assurance evaluations that might otherwise be underpowered if completed at a single center. A limitation of the collaborative model is that a site with a robust ASP may already have specific practices in place. Expanding the ASP collaborative model further highlights the VHA role as a nationwide leader in ASP best practices.
- Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2019. Updated December 2019. Accessed September 10, 2024. https:// www.cdc.gov/antimicrobial-resistance/media/pdfs/2019-ar-threats-report-508.pdf
- US Department of Veterans Affairs. Antimicrobial stewardship programs. Updated September 22, 2023. Accessed September 13, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=11458
- US Department of Veterans Affairs, Veteran Health Administration. Veterans Integrated Service Networks (VISNs). Accessed September 13, 2024. https://www.va.gov/HEALTH/visns.asp
- US Department of Veterans Affairs. Veterans Health Administration, Veterans Integrated Service Networks, VISN 08. Updated September 10, 2024. Accessed September 13, 2024. https://department.va.gov/integrated-service-networks/visn-08/
- Andreev I. What is collaborative learning? Theory, examples of activities. Valamis. Updated July 10, 2024. Accessed September 10, 2024. https://www.valamis.com/hub/collaborative-learning
- Rybak MJ, Le J, Lodise TP, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2020;77(11):835-864. doi:10.1093/ajhp/zxaa036
- Finch NA, Zasowski EJ, Murray KP, et al. A quasi-experiment to study the impact of vancomycin area under the concentration-time curve-guided dosing on vancomycinassociated nephrotoxicity. Antimicrob Agents Chemother. 2017;61(12):e01293-17. doi:10.1128/AAC.01293-17
- Zasowski EJ, Murray KP, Trinh TD, et al. Identification of vancomycin exposure-toxicity thresholds in hospitalized patients receiving intravenous vancomycin. Antimicrob Agents Chemother. 2017;62(1):e01684-17. doi:10.1128/AAC.01684-17
- Matzke GR, Kovarik JM, Rybak MJ, Boike SC. Evaluation of the vancomycin-clearance: creatinine-clearance relationship for predicting vancomycin dosage. Clin Pharm. 1985;4(3):311-315.
- Crass RL, Dunn R, Hong J, Krop LC, Pai MP. Dosing vancomycin in the super obese: less is more. J Antimicrob Chemother. 2018;73(11):3081-3086. doi:10.1093/jac/dky310
- Lodise TP, Rosenkranz SL, Finnemeyer M, et al. The emperor’s new clothes: prospective observational evaluation of the association between initial vancomycIn exposure and failure rates among adult hospitalized patients with methicillin-resistant staphylococcus aureus bloodstream infections (PROVIDE). Clin Infect Dis. 2020;70(8):1536-1545. doi:10.1093/cid/ciz460
Antimicrobial resistance is a global threat and burden to health care, with > 2.8 million antibiotic-resistant infections occurring annually in the United States.1 To combat this issue and improve patient care, the US Department of Veterans Affairs (VA) has implemented antimicrobial stewardship programs (ASPs) across its health care systems. ASPs are multidisciplinary teams that promote evidence-based use of antimicrobials through activities supporting appropriate selection, dosing, route, and duration of antimicrobial therapy. ASP best practices are also included in the Joint Commission and Centers for Medicare and Medicaid Services accreditation standards.2
The foundational charge for VA facilities to develop and maintain ASPs was outlined in 2014 and updated in 2023 in the Veterans Health Administration (VHA) Directive 1031 on antimicrobial stewardship programs.2 This directive outlines specific requirements for all VA ASPs, including personnel, staffing levels, and the roles and responsibilities of all team members. VHA now requires that Veterans Integrated Services Networks (VISNs) establish robust ASP collaboratives. A VISN ASP collaborative consists of stewardship champions from each VA medical center in the VISN and is designed to support, develop, and enhance ASP programs across all facilities within that VISN.2 Some VISNs may lack an ASP collaborative altogether, and others with existing groups may seek ways to expand their collaboratives in line with the updated directive. Prior to VHA Directive 1031, the VA Sunshine Healthcare Network (VISN 8) established an ASP collaborative. This article describes the structure and activities of the VISN 8 ASP collaborative and highlights a recent VISN 8 quality assurance initiative related to vancomycin area under the curve (AUC) dosing that illustrates how ASP collaboratives can enhance stewardship and clinical care across broad geographic areas.
VISN 8 ASP
The VHA, the largest integrated US health care system, is divided into 18 VISNs that provide regional systems of care to enhance access and meet the local health care needs of veterans.3 VISN 8 serves > 1.5 million veterans across 165,759 km2 in Florida, South Georgia, Puerto Rico, and the US Virgin Islands.4 The network is composed of 7 health systems with 8 medical centers and > 60 outpatient clinics. These facilities provide comprehensive acute, primary, and specialty care, as well as mental health and extended care services in inpatient, outpatient, nursing home, and home care settings.4
The 2023 VHA Directive 1031 update recognizes the importance of VISN-level coordination of ASP activities to enhance the standardization of care and build partnerships in stewardship across all levels of care. The VISN 8 ASP collaborative workgroup (ASPWG) was established in 2015. Consistent with Directive 1031, the ASPWG is guided by clinician and pharmacist VISN leads. These leads serve as subject matter experts, facilitate access to resources, establish VISN-level consensus, and enhance communication among local ASP champions at medical centers within the VISN. All 7 health systems include = 1 ASP champion (clinician or pharmacist) in the ASPWG. Ad hoc members, whose routine duties are not solely focused on antimicrobial stewardship, contribute to specific stewardship projects as needed. For example, the ASPWG has included internal medicine, emergency department, community living center pharmacists, representatives from pharmacy administration, and trainees (pharmacy students and residents, and infectious diseases fellows) in antimicrobial stewardship initiatives. The inclusion of non-ASP champions is not discussed in VHA Directive 1031. However, these members have made valuable contributions to the ASPWG.
The ASPWG meets monthly. Agendas and priorities are developed by the VISN pharmacist and health care practitioner (HCP) leads. Monthly discussions may include but are not limited to a review of national formulary decisions, VISN goals and metrics, infectious diseases hot topics, pharmacoeconomic initiatives, strong practice presentations, regulatory and accreditation preparation, preparation of tracking reports, as well as the development of both patient-level and HCPlevel tools, resources, and education materials. This forum facilitates collaborative learning: members process and synthesize information, share and reframe ideas, and listen to other viewpoints to gain a complete understanding as a group.5 For example, ASPWG members have leaned on each other to prepare for Joint Commission accreditation surveys and strengthen the VISN 8 COVID-19 program through the rollout of vaccines and treatments. Other collaborative projects completed over the past few years included a penicillin allergy testing initiative and anti-methicillin-resistant Staphylococcus aureus (MRSA) and pseudomonal medication use evaluations. This team-centric problem-solving approach is highly effective while also fostering professional and social relationships. However, collaboratives could be perceived to have drawbacks. There may be opportunity costs if ASP time is allocated for issues that have already been addressed locally or concerns that standardization might hinder rapid adoption of practices at individual sites. Therefore, participation in each distinct group initiative is optional. This allows sites to choose projects related to their high priority areas and maintain bandwidth to implement practices not yet adopted by the larger group.
The ASPWG tracks metrics related to antimicrobial use with quarterly data presented by the VISN pharmacist lead. Both inpatient and outpatient metrics are evaluated, such as days of therapy per 1000 days and outpatient antibiotic prescriptions per 1000 unique patients. Facilities are benchmarked against their own historical data and other VISN sites, as well as other VISNs across the country. When outliers are identified, facilities are encouraged to conduct local projects to identify reasons for different antimicrobial use patterns and subsequent initiatives to optimize antimicrobial use. Benchmarking against VISN facilities can be useful since VISN facilities may be more similar than facilities in different geographic regions. Each year, the ASPWG reviews the current metrics, makes adjustments to address VISN priorities, and votes for approval of the metrics that will be tracked in the coming year.
Participation in an ASP collaborative streamlines the rollout of ASP and quality improvement initiatives across multiple sites, allowing ASPs to impact a greater number of veterans and evaluate initiatives on a larger scale. In 2019, with the anticipation of revised vancomycin dosing and monitoring guidelines, our ASPWG began to strategize the transition to AUC-based vancomycin monitoring.6 This multisite initiative showcases the strengths of implementing and evaluating practice changes as part of an ASP collaborative.
Vancomycin Dosing
The antibiotic vancomycin is used primarily for the treatment of MRSA infections.6 The 2020 consensus guidelines for vancomycin therapeutic monitoring recommend using the AUC to minimum inhibitory concentration (MIC) ratio as the pharmacodynamic target for serious MRSA infections, with an AUC/MIC goal of 400 to 600 mcg*h/mL.6 Prior guidelines recommended using vancomycin trough concentrations of 15 to 20 mcg/mL as a surrogate for this AUC target. However, subsequent studies have shown that trough-based dosing is associated with higher vancomycin exposures, supratherapeutic AUCs, and increased risk of vancomycin-associated acute kidney injury (AKI).7,8 Therefore, more direct AUC estimation is now recommended.6 The preferred approach for AUC calculations is through Bayesian modeling. Due to limited resources and software availability, many facilities use an alternative method involving 2 postdistributive serum vancomycin concentrations and first-order pharmacokinetic equations. This approach can optimize vancomycin dosing but is more mathematically and logistically challenging. Transitioning from troughto AUC-based vancomycin monitoring requires careful planning and comprehensive staff education.
In 2019, the VISN 8 ASPWG created a comprehensive vancomycin AUC toolkit to facilitate implementation. Components included a pharmacokinetic management policy and procedure, a vancomycin dosing guide, a progress note template, educational materials specific to pharmacy, nursing, laboratory, and medical services, a pharmacist competency examination, and a vancomycin AUC calculator (eAppendix). Each component was developed by a subgroup with the understanding that sites could incorporate variations based on local practices and needs.

The vancomycin AUC calculator was developed to be user-friendly and included safety validation protocols to prevent the entry of erroneous data (eg, unrealistic patient weight or laboratory values). The calculator allowed users to copy data into the electronic health record to avoid manual transcription errors and improve operational efficiency. It offered suggested volume of distribution estimates and 2 methods to estimate elimination constant (Ke ) depending on the patient’s weight.9,10 Creatinine clearance could be estimated using serum creatinine or cystatin C and considered amputation history. The default AUC goal in the calculator was 400 to 550 mcg*h/mL. This range was chosen based on consensus guidelines, data suggesting increased risk of AKI with AUCs > 515 mcg*h/mL, and the preference for conservative empiric dosing in the generally older VA population.11 The calculator suggested loading doses of about 25 mg/kg with a 2500 mg limit. VHA facilities could make limited modifications to the calculator based on local policies and procedures (eg, adjusting default infusion times or a dosing intervals).
The VISN 8 Pharmacy Pharmacokinetic Dosing Manual was developed as a comprehensive document to guide pharmacy staff with dosing vancomycin across diverse patient populations. This document included recommendations for renal function assessment, patient-specific considerations when choosing an empiric vancomycin dose, methods of ordering vancomycin peak, trough, and surveillance levels, dose determination based on 2 levels, and other clinical insights or frequently asked questions.
ASPWG members presented an accredited continuing education webinar for pharmacists, which reviewed the rationale for AUC-targeted dosing, changes to the current pharmacokinetic dosing program, case-based scenarios across various patient populations, and potential challenges associated with vancomycin AUC-based dosing. A recording of the live training was also made available. A vancomycin AUC dosing competency test was developed with 11 basic pharmacokinetic and case-based questions and comprehensive explanations provided for each answer.
VHA facilities implemented AUC dosing in a staggered manner, allowing for lessons learned at earlier adopters to be addressed proactively at later sites. The dosing calculator and education documents were updated iteratively as opportunities for improvement were discovered. ASPWG members held local office hours to address questions or concerns from staff at their facilities. Sharing standardized materials across the VISN reduced individual site workload and complications in rolling out this complex new process.
VISN-WIDE QUALITY ASSURANCE
At the time of project conception, 4 of 7 VISN 8 health systems had transitioned to AUC-based dosing. A quality assurance protocol to compare patient outcomes before and after changing to AUC dosing was developed. Each site followed local protocols for project approval and data were deidentified, collected, and aggregated for analysis.
The primary objectives were to compare the incidence of AKI and persistent bacteremia and assess rates of AUC target attainment (400-600 mcg*h/mL) in the AUC-based and trough-based dosing groups.6 Data for both groups included anthropomorphic measurements, serum creatinine, amputation status, vancomycin dosing, and infection characteristics. The X2 test was used for categorical data and the t test was used for continuous data. A 2-tailed α of 0.05 was used to determine significance. Each site sequentially reviewed all patients receiving ≥ 48 hours of intravenous vancomycin over a 3-month period and contributed up to 50 patients for each group. Due to staggered implementation, the study periods for sites spanned 2018 to 2023. A minimum 6-month washout period was observed between the trough and AUC groups at each site. Patients were excluded if pregnant, receiving renal replacement therapy, or presenting with AKI at the time of vancomycin initiation.
There were 168 patients in the AUC group and 172 patients in the trough group (Table 1). The rate of AUC target attainment with the initial dosing regimen varied across sites from 18% to 69% (mean, 48%). Total daily vancomycin exposure was lower in the AUC group compared with the trough group (2402 mg vs 2605 mg, respectively), with AUC-dosed patients being less likely to experience troughs level ≥ 15 or 20 mcg/mL (Table 2). There was a statistically significant lower rate of AKI in the AUC group: 2.4% in the AUC group (range, 2%-3%) vs 10.4% (range 7%-12%) in the trough group (P = .002). Rates of AKI were comparable to those observed in previous interventions.6 There was no statistical difference in length of stay, time to blood culture clearance, or rate of persistent bacteremia in the 2 groups, but these assessments were limited by sample size.

We did not anticipate such variability in initial target attainment across sites. The multisite quality assurance design allowed for qualitative evaluation of variability in dosing practices, which likely arose from sites and individual pharmacists having some flexibility in adjusting dosing tool parameters. Further analysis revealed that the facility with low initial target attainment was not routinely utilizing vancomycin loading doses. Sites routinely use robust loading doses achieved earlier and more consistent target attainment. Some sites used a narrower AUC target range in certain clinical scenarios (eg, > 500 mcg*h/mL for septic patients and < 500 mcg*h/mL for patients with less severe infections) rather than the 400 to 550 mcg*h/mL range for all patients. Sites targeting broader AUC ranges for all patients had higher rates of target attainment. Reviewing differences among sites allowed the ASPWG to identify best practices to optimize future care.
CONCLUSIONS
VHA ASPs must meet the standards outlined in VHA Directive 1031, including the new requirement for each VISN to develop an ASP collaborative. The VISN 8 ASPWG demonstrates how ASP champions can collaborate to solve common issues, complete tasks, explore new infectious diseases concepts, and impact large veteran populations. Furthermore, ASP collaboratives can harness their collective size to complete robust quality assurance evaluations that might otherwise be underpowered if completed at a single center. A limitation of the collaborative model is that a site with a robust ASP may already have specific practices in place. Expanding the ASP collaborative model further highlights the VHA role as a nationwide leader in ASP best practices.
Antimicrobial resistance is a global threat and burden to health care, with > 2.8 million antibiotic-resistant infections occurring annually in the United States.1 To combat this issue and improve patient care, the US Department of Veterans Affairs (VA) has implemented antimicrobial stewardship programs (ASPs) across its health care systems. ASPs are multidisciplinary teams that promote evidence-based use of antimicrobials through activities supporting appropriate selection, dosing, route, and duration of antimicrobial therapy. ASP best practices are also included in the Joint Commission and Centers for Medicare and Medicaid Services accreditation standards.2
The foundational charge for VA facilities to develop and maintain ASPs was outlined in 2014 and updated in 2023 in the Veterans Health Administration (VHA) Directive 1031 on antimicrobial stewardship programs.2 This directive outlines specific requirements for all VA ASPs, including personnel, staffing levels, and the roles and responsibilities of all team members. VHA now requires that Veterans Integrated Services Networks (VISNs) establish robust ASP collaboratives. A VISN ASP collaborative consists of stewardship champions from each VA medical center in the VISN and is designed to support, develop, and enhance ASP programs across all facilities within that VISN.2 Some VISNs may lack an ASP collaborative altogether, and others with existing groups may seek ways to expand their collaboratives in line with the updated directive. Prior to VHA Directive 1031, the VA Sunshine Healthcare Network (VISN 8) established an ASP collaborative. This article describes the structure and activities of the VISN 8 ASP collaborative and highlights a recent VISN 8 quality assurance initiative related to vancomycin area under the curve (AUC) dosing that illustrates how ASP collaboratives can enhance stewardship and clinical care across broad geographic areas.
VISN 8 ASP
The VHA, the largest integrated US health care system, is divided into 18 VISNs that provide regional systems of care to enhance access and meet the local health care needs of veterans.3 VISN 8 serves > 1.5 million veterans across 165,759 km2 in Florida, South Georgia, Puerto Rico, and the US Virgin Islands.4 The network is composed of 7 health systems with 8 medical centers and > 60 outpatient clinics. These facilities provide comprehensive acute, primary, and specialty care, as well as mental health and extended care services in inpatient, outpatient, nursing home, and home care settings.4
The 2023 VHA Directive 1031 update recognizes the importance of VISN-level coordination of ASP activities to enhance the standardization of care and build partnerships in stewardship across all levels of care. The VISN 8 ASP collaborative workgroup (ASPWG) was established in 2015. Consistent with Directive 1031, the ASPWG is guided by clinician and pharmacist VISN leads. These leads serve as subject matter experts, facilitate access to resources, establish VISN-level consensus, and enhance communication among local ASP champions at medical centers within the VISN. All 7 health systems include = 1 ASP champion (clinician or pharmacist) in the ASPWG. Ad hoc members, whose routine duties are not solely focused on antimicrobial stewardship, contribute to specific stewardship projects as needed. For example, the ASPWG has included internal medicine, emergency department, community living center pharmacists, representatives from pharmacy administration, and trainees (pharmacy students and residents, and infectious diseases fellows) in antimicrobial stewardship initiatives. The inclusion of non-ASP champions is not discussed in VHA Directive 1031. However, these members have made valuable contributions to the ASPWG.
The ASPWG meets monthly. Agendas and priorities are developed by the VISN pharmacist and health care practitioner (HCP) leads. Monthly discussions may include but are not limited to a review of national formulary decisions, VISN goals and metrics, infectious diseases hot topics, pharmacoeconomic initiatives, strong practice presentations, regulatory and accreditation preparation, preparation of tracking reports, as well as the development of both patient-level and HCPlevel tools, resources, and education materials. This forum facilitates collaborative learning: members process and synthesize information, share and reframe ideas, and listen to other viewpoints to gain a complete understanding as a group.5 For example, ASPWG members have leaned on each other to prepare for Joint Commission accreditation surveys and strengthen the VISN 8 COVID-19 program through the rollout of vaccines and treatments. Other collaborative projects completed over the past few years included a penicillin allergy testing initiative and anti-methicillin-resistant Staphylococcus aureus (MRSA) and pseudomonal medication use evaluations. This team-centric problem-solving approach is highly effective while also fostering professional and social relationships. However, collaboratives could be perceived to have drawbacks. There may be opportunity costs if ASP time is allocated for issues that have already been addressed locally or concerns that standardization might hinder rapid adoption of practices at individual sites. Therefore, participation in each distinct group initiative is optional. This allows sites to choose projects related to their high priority areas and maintain bandwidth to implement practices not yet adopted by the larger group.
The ASPWG tracks metrics related to antimicrobial use with quarterly data presented by the VISN pharmacist lead. Both inpatient and outpatient metrics are evaluated, such as days of therapy per 1000 days and outpatient antibiotic prescriptions per 1000 unique patients. Facilities are benchmarked against their own historical data and other VISN sites, as well as other VISNs across the country. When outliers are identified, facilities are encouraged to conduct local projects to identify reasons for different antimicrobial use patterns and subsequent initiatives to optimize antimicrobial use. Benchmarking against VISN facilities can be useful since VISN facilities may be more similar than facilities in different geographic regions. Each year, the ASPWG reviews the current metrics, makes adjustments to address VISN priorities, and votes for approval of the metrics that will be tracked in the coming year.
Participation in an ASP collaborative streamlines the rollout of ASP and quality improvement initiatives across multiple sites, allowing ASPs to impact a greater number of veterans and evaluate initiatives on a larger scale. In 2019, with the anticipation of revised vancomycin dosing and monitoring guidelines, our ASPWG began to strategize the transition to AUC-based vancomycin monitoring.6 This multisite initiative showcases the strengths of implementing and evaluating practice changes as part of an ASP collaborative.
Vancomycin Dosing
The antibiotic vancomycin is used primarily for the treatment of MRSA infections.6 The 2020 consensus guidelines for vancomycin therapeutic monitoring recommend using the AUC to minimum inhibitory concentration (MIC) ratio as the pharmacodynamic target for serious MRSA infections, with an AUC/MIC goal of 400 to 600 mcg*h/mL.6 Prior guidelines recommended using vancomycin trough concentrations of 15 to 20 mcg/mL as a surrogate for this AUC target. However, subsequent studies have shown that trough-based dosing is associated with higher vancomycin exposures, supratherapeutic AUCs, and increased risk of vancomycin-associated acute kidney injury (AKI).7,8 Therefore, more direct AUC estimation is now recommended.6 The preferred approach for AUC calculations is through Bayesian modeling. Due to limited resources and software availability, many facilities use an alternative method involving 2 postdistributive serum vancomycin concentrations and first-order pharmacokinetic equations. This approach can optimize vancomycin dosing but is more mathematically and logistically challenging. Transitioning from troughto AUC-based vancomycin monitoring requires careful planning and comprehensive staff education.
In 2019, the VISN 8 ASPWG created a comprehensive vancomycin AUC toolkit to facilitate implementation. Components included a pharmacokinetic management policy and procedure, a vancomycin dosing guide, a progress note template, educational materials specific to pharmacy, nursing, laboratory, and medical services, a pharmacist competency examination, and a vancomycin AUC calculator (eAppendix). Each component was developed by a subgroup with the understanding that sites could incorporate variations based on local practices and needs.

The vancomycin AUC calculator was developed to be user-friendly and included safety validation protocols to prevent the entry of erroneous data (eg, unrealistic patient weight or laboratory values). The calculator allowed users to copy data into the electronic health record to avoid manual transcription errors and improve operational efficiency. It offered suggested volume of distribution estimates and 2 methods to estimate elimination constant (Ke ) depending on the patient’s weight.9,10 Creatinine clearance could be estimated using serum creatinine or cystatin C and considered amputation history. The default AUC goal in the calculator was 400 to 550 mcg*h/mL. This range was chosen based on consensus guidelines, data suggesting increased risk of AKI with AUCs > 515 mcg*h/mL, and the preference for conservative empiric dosing in the generally older VA population.11 The calculator suggested loading doses of about 25 mg/kg with a 2500 mg limit. VHA facilities could make limited modifications to the calculator based on local policies and procedures (eg, adjusting default infusion times or a dosing intervals).
The VISN 8 Pharmacy Pharmacokinetic Dosing Manual was developed as a comprehensive document to guide pharmacy staff with dosing vancomycin across diverse patient populations. This document included recommendations for renal function assessment, patient-specific considerations when choosing an empiric vancomycin dose, methods of ordering vancomycin peak, trough, and surveillance levels, dose determination based on 2 levels, and other clinical insights or frequently asked questions.
ASPWG members presented an accredited continuing education webinar for pharmacists, which reviewed the rationale for AUC-targeted dosing, changes to the current pharmacokinetic dosing program, case-based scenarios across various patient populations, and potential challenges associated with vancomycin AUC-based dosing. A recording of the live training was also made available. A vancomycin AUC dosing competency test was developed with 11 basic pharmacokinetic and case-based questions and comprehensive explanations provided for each answer.
VHA facilities implemented AUC dosing in a staggered manner, allowing for lessons learned at earlier adopters to be addressed proactively at later sites. The dosing calculator and education documents were updated iteratively as opportunities for improvement were discovered. ASPWG members held local office hours to address questions or concerns from staff at their facilities. Sharing standardized materials across the VISN reduced individual site workload and complications in rolling out this complex new process.
VISN-WIDE QUALITY ASSURANCE
At the time of project conception, 4 of 7 VISN 8 health systems had transitioned to AUC-based dosing. A quality assurance protocol to compare patient outcomes before and after changing to AUC dosing was developed. Each site followed local protocols for project approval and data were deidentified, collected, and aggregated for analysis.
The primary objectives were to compare the incidence of AKI and persistent bacteremia and assess rates of AUC target attainment (400-600 mcg*h/mL) in the AUC-based and trough-based dosing groups.6 Data for both groups included anthropomorphic measurements, serum creatinine, amputation status, vancomycin dosing, and infection characteristics. The X2 test was used for categorical data and the t test was used for continuous data. A 2-tailed α of 0.05 was used to determine significance. Each site sequentially reviewed all patients receiving ≥ 48 hours of intravenous vancomycin over a 3-month period and contributed up to 50 patients for each group. Due to staggered implementation, the study periods for sites spanned 2018 to 2023. A minimum 6-month washout period was observed between the trough and AUC groups at each site. Patients were excluded if pregnant, receiving renal replacement therapy, or presenting with AKI at the time of vancomycin initiation.
There were 168 patients in the AUC group and 172 patients in the trough group (Table 1). The rate of AUC target attainment with the initial dosing regimen varied across sites from 18% to 69% (mean, 48%). Total daily vancomycin exposure was lower in the AUC group compared with the trough group (2402 mg vs 2605 mg, respectively), with AUC-dosed patients being less likely to experience troughs level ≥ 15 or 20 mcg/mL (Table 2). There was a statistically significant lower rate of AKI in the AUC group: 2.4% in the AUC group (range, 2%-3%) vs 10.4% (range 7%-12%) in the trough group (P = .002). Rates of AKI were comparable to those observed in previous interventions.6 There was no statistical difference in length of stay, time to blood culture clearance, or rate of persistent bacteremia in the 2 groups, but these assessments were limited by sample size.

We did not anticipate such variability in initial target attainment across sites. The multisite quality assurance design allowed for qualitative evaluation of variability in dosing practices, which likely arose from sites and individual pharmacists having some flexibility in adjusting dosing tool parameters. Further analysis revealed that the facility with low initial target attainment was not routinely utilizing vancomycin loading doses. Sites routinely use robust loading doses achieved earlier and more consistent target attainment. Some sites used a narrower AUC target range in certain clinical scenarios (eg, > 500 mcg*h/mL for septic patients and < 500 mcg*h/mL for patients with less severe infections) rather than the 400 to 550 mcg*h/mL range for all patients. Sites targeting broader AUC ranges for all patients had higher rates of target attainment. Reviewing differences among sites allowed the ASPWG to identify best practices to optimize future care.
CONCLUSIONS
VHA ASPs must meet the standards outlined in VHA Directive 1031, including the new requirement for each VISN to develop an ASP collaborative. The VISN 8 ASPWG demonstrates how ASP champions can collaborate to solve common issues, complete tasks, explore new infectious diseases concepts, and impact large veteran populations. Furthermore, ASP collaboratives can harness their collective size to complete robust quality assurance evaluations that might otherwise be underpowered if completed at a single center. A limitation of the collaborative model is that a site with a robust ASP may already have specific practices in place. Expanding the ASP collaborative model further highlights the VHA role as a nationwide leader in ASP best practices.
- Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2019. Updated December 2019. Accessed September 10, 2024. https:// www.cdc.gov/antimicrobial-resistance/media/pdfs/2019-ar-threats-report-508.pdf
- US Department of Veterans Affairs. Antimicrobial stewardship programs. Updated September 22, 2023. Accessed September 13, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=11458
- US Department of Veterans Affairs, Veteran Health Administration. Veterans Integrated Service Networks (VISNs). Accessed September 13, 2024. https://www.va.gov/HEALTH/visns.asp
- US Department of Veterans Affairs. Veterans Health Administration, Veterans Integrated Service Networks, VISN 08. Updated September 10, 2024. Accessed September 13, 2024. https://department.va.gov/integrated-service-networks/visn-08/
- Andreev I. What is collaborative learning? Theory, examples of activities. Valamis. Updated July 10, 2024. Accessed September 10, 2024. https://www.valamis.com/hub/collaborative-learning
- Rybak MJ, Le J, Lodise TP, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2020;77(11):835-864. doi:10.1093/ajhp/zxaa036
- Finch NA, Zasowski EJ, Murray KP, et al. A quasi-experiment to study the impact of vancomycin area under the concentration-time curve-guided dosing on vancomycinassociated nephrotoxicity. Antimicrob Agents Chemother. 2017;61(12):e01293-17. doi:10.1128/AAC.01293-17
- Zasowski EJ, Murray KP, Trinh TD, et al. Identification of vancomycin exposure-toxicity thresholds in hospitalized patients receiving intravenous vancomycin. Antimicrob Agents Chemother. 2017;62(1):e01684-17. doi:10.1128/AAC.01684-17
- Matzke GR, Kovarik JM, Rybak MJ, Boike SC. Evaluation of the vancomycin-clearance: creatinine-clearance relationship for predicting vancomycin dosage. Clin Pharm. 1985;4(3):311-315.
- Crass RL, Dunn R, Hong J, Krop LC, Pai MP. Dosing vancomycin in the super obese: less is more. J Antimicrob Chemother. 2018;73(11):3081-3086. doi:10.1093/jac/dky310
- Lodise TP, Rosenkranz SL, Finnemeyer M, et al. The emperor’s new clothes: prospective observational evaluation of the association between initial vancomycIn exposure and failure rates among adult hospitalized patients with methicillin-resistant staphylococcus aureus bloodstream infections (PROVIDE). Clin Infect Dis. 2020;70(8):1536-1545. doi:10.1093/cid/ciz460
- Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2019. Updated December 2019. Accessed September 10, 2024. https:// www.cdc.gov/antimicrobial-resistance/media/pdfs/2019-ar-threats-report-508.pdf
- US Department of Veterans Affairs. Antimicrobial stewardship programs. Updated September 22, 2023. Accessed September 13, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=11458
- US Department of Veterans Affairs, Veteran Health Administration. Veterans Integrated Service Networks (VISNs). Accessed September 13, 2024. https://www.va.gov/HEALTH/visns.asp
- US Department of Veterans Affairs. Veterans Health Administration, Veterans Integrated Service Networks, VISN 08. Updated September 10, 2024. Accessed September 13, 2024. https://department.va.gov/integrated-service-networks/visn-08/
- Andreev I. What is collaborative learning? Theory, examples of activities. Valamis. Updated July 10, 2024. Accessed September 10, 2024. https://www.valamis.com/hub/collaborative-learning
- Rybak MJ, Le J, Lodise TP, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm. 2020;77(11):835-864. doi:10.1093/ajhp/zxaa036
- Finch NA, Zasowski EJ, Murray KP, et al. A quasi-experiment to study the impact of vancomycin area under the concentration-time curve-guided dosing on vancomycinassociated nephrotoxicity. Antimicrob Agents Chemother. 2017;61(12):e01293-17. doi:10.1128/AAC.01293-17
- Zasowski EJ, Murray KP, Trinh TD, et al. Identification of vancomycin exposure-toxicity thresholds in hospitalized patients receiving intravenous vancomycin. Antimicrob Agents Chemother. 2017;62(1):e01684-17. doi:10.1128/AAC.01684-17
- Matzke GR, Kovarik JM, Rybak MJ, Boike SC. Evaluation of the vancomycin-clearance: creatinine-clearance relationship for predicting vancomycin dosage. Clin Pharm. 1985;4(3):311-315.
- Crass RL, Dunn R, Hong J, Krop LC, Pai MP. Dosing vancomycin in the super obese: less is more. J Antimicrob Chemother. 2018;73(11):3081-3086. doi:10.1093/jac/dky310
- Lodise TP, Rosenkranz SL, Finnemeyer M, et al. The emperor’s new clothes: prospective observational evaluation of the association between initial vancomycIn exposure and failure rates among adult hospitalized patients with methicillin-resistant staphylococcus aureus bloodstream infections (PROVIDE). Clin Infect Dis. 2020;70(8):1536-1545. doi:10.1093/cid/ciz460
Age-Friendly Health Systems Transformation: A Whole Person Approach to Support the Well-Being of Older Adults
The COVID-19 pandemic established a new normal for health care delivery, with leaders rethinking core practices to survive and thrive in a changing environment and improve the health and well-being of patients. The Veterans Health Administration (VHA) is embracing a shift in focus from “what is the matter” to “what really matters” to address pre- and postpandemic challenges through a whole health approach.1 Initially conceptualized by the VHA in 2011, whole health “is an approach to health care that empowers and equips people to take charge of their health and well-being so that they can live their life to the fullest.”1 Whole health integrates evidence-based complementary and integrative health (CIH) therapies to manage pain; this includes acupuncture, meditation, tai chi, yoga, massage therapy, guided imagery, biofeedback, and clinical hypnosis.1 The VHA now recognizes well-being as a core value, helping clinicians respond to emerging challenges related to the social determinants of health (eg, access to health care, physical activity, and healthy foods) and guiding health care decision making.1,2
Well-being through empowerment—elements of whole health and Age-Friendly Health Systems (AFHS)—encourages health care institutions to work with employees, patients, and other stakeholders to address global challenges, clinician burnout, and social issues faced by their communities. This approach focuses on life’s purpose and meaning for individuals and inspires leaders to engage with patients, staff, and communities in new, impactful ways by focusing on wellbeing and wholeness rather than illness and disease. Having a higher sense of purpose is associated with lower all-cause mortality, reduced risk of specific diseases, better health behaviors, greater use of preventive services, and fewer hospital days of care.3
This article describes how AFHS supports the well-being of older adults and aligns with the whole health model of care. It also outlines the VHA investment to transform health care to be more person-centered by documenting what matters in the electronic health record (EHR).
AGE-FRIENDLY CARE
Given that nearly half of veterans enrolled in the VHA are aged ≥ 65 years, there is an increased need to identify models of care to support this aging population.4 This is especially critical because older veterans often have multiple chronic conditions and complex care needs that benefit from a whole person approach. The AFHS movement aims to provide evidence-based care aligned with what matters to older adults and provides a mechanism for transforming care to meet the needs of older veterans. This includes addressing age-related health concerns while promoting optimal health outcomes and quality of life. AFHS follows the 4Ms framework: what matters, medication, mentation, and mobility.5 The 4Ms serve as a guide for the health care of older adults in any setting, where each “M” is assessed and acted on to support what matters.5 Since 2020, > 390 teams have developed a plan to implement the 4Ms at 156 VHA facilities, demonstrating the VHA commitment to transforming health care for veterans.6
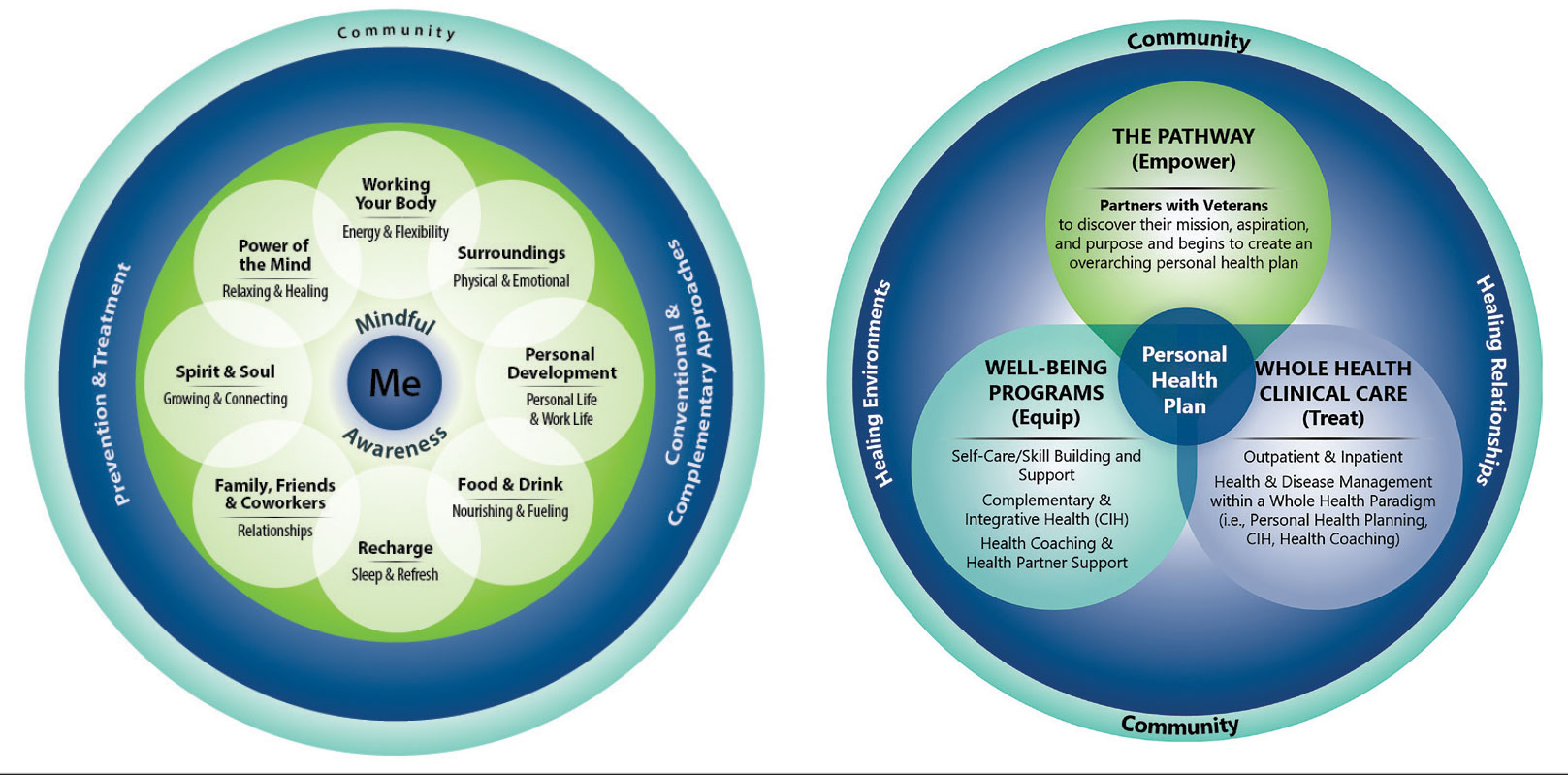
When VHA teams join the AFHS movement, they may also engage older veterans in a whole health system (WHS) (Figure). While AFHS is designed to improve care for patients aged ≥ 65 years, it also complements whole health, a person-centered approach available to all veterans enrolled in the VHA. Through the WHS and AFHS, veterans are empowered and equipped to take charge of their health and well-being through conversations about their unique goals, preferences, and health priorities.4 Clinicians are challenged to assess what matters by asking questions like, “What brings you joy?” and, “How can we help you meet your health goals?”1,5 These questions shift the conversation from disease-based treatment and enable clinicians to better understand the veteran as a person.1,5
For whole health and AFHS, conversations about what matters are anchored in the veteran’s goals and preferences, especially those facing a significant health change (ie, a new diagnosis or treatment decision).5,7 Together, the veteran’s goals and priorities serve as the foundation for developing person-centered care plans that often go beyond conventional medical treatments to address the physical, mental, emotional, and social aspects of health.
SYSTEM-WIDE DIRECTIVE
The WHS enhances AFHS discussions about what matters to veterans by adding a system-level lens for conceptualizing health care delivery by leveraging the 3 components of WHS: the “pathway,” well-being programs, and whole health clinical care.
The Pathway
Discovering what matters, or the veteran’s “mission, aspiration, and purpose,” begins with the WHS pathway. When stepping into the pathway, veterans begin completing a personal health inventory, or “walking the circle of health,” which encourages self-reflection that focuses on components of their life that can influence health and well-being.1,8 The circle of health offers a visual representation of the 4 most important aspects of health and well-being: First, “Me” at the center as an individual who is the expert on their life, values, goals, and priorities. Only the individual can know what really matters through mindful awareness and what works for their life. Second, self-care consists of 8 areas that impact health and wellbeing: working your body; surroundings; personal development; food and drink; recharge; family, friends, and coworkers; spirit and soul; and power of the mind. Third, professional care consists of prevention, conventional care, and complementary care. Finally, the community that supports the individual.
Well-Being Programs
VHA provides WHS programs that support veterans in building self-care skills and improving their quality of life, often through integrative care clinics that offer coaching and CIH therapies. For example, a veteran who prioritizes mobility when seeking care at an integrative care clinic will not only receive conventional medical treatment for their physical symptoms but may also be offered CIH therapies depending on their goals. The veteran may set a daily mobility goal with their care team that supports what matters, incorporating CIH approaches, such as yoga and tai chi into the care plan.5 These holistic approaches for moving the body can help alleviate physical symptoms, reduce stress, improve mindful awareness, and provide opportunities for self-discovery and growth, thus promote overall well-being
Whole Health Clinical Care
AFHS and the 4Ms embody the clinical care component of the WHS. Because what matters is the driver of the 4Ms, every action taken by the care team supports wellbeing and quality of life by promoting independence, connection, and support, and addressing external factors, such as social determinants of health. At a minimum, well-being includes “functioning well: the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships.”9 From a system perspective, the VHA has begun to normalize focusing on what matters to veterans, using an interprofessional approach, one of the first steps to implementing AFHS.
As the programs expand, AFHS teams can learn from whole health well-being programs and increase the capacity for self-care in older veterans. Learning about the key elements included in the circle of health helps clinicians understand each veteran’s perceived strengths and weaknesses to support their self-care. From there, teams can act on the 4Ms and connect older veterans with the most appropriate programs and services at their facility, ensuring continuum of care.
DOCUMENTATION
The VHA leverages several tools and evidence-based practices to assess and act on what matters for veterans of all ages (Table).5,10-16 The VHA EHR and associated dashboards contain a wealth of information about whole health and AFHS implementation, scale up, and spread. A national AFHS 4Ms note template contains standardized data elements called health factors, which provide a mechanism for monitoring 4Ms care via its related dashboard. This template was developed by an interprofessional workgroup of VHA staff and underwent a thorough human factors engineering review and testing process prior to its release. Although teams continue to personalize care based on what matters to the veteran, data from the standardized 4Ms note template and dashboard provide a way to establish consistent, equitable care across multiple care settings.17
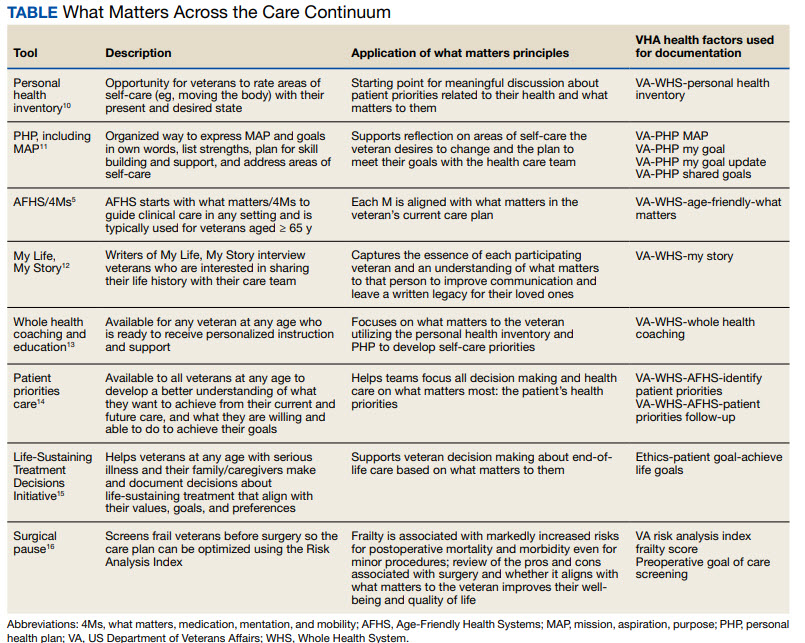
Between January 2022 and December 2023, > 612,000 participants aged ≥ 65 years identified what matters to them through 1.35 million assessments. During that period, > 36,000 veterans aged ≥ 65 years participated in AFHS and had what matters conversations documented. A personalized health plan was completed by 585,270 veterans for a total of 1.1 million assessments.11 Whole health coaching has been documented for > 57,000 veterans with > 200,000 assessments completed.13 In fiscal year 2023, a total of 1,802,131 veterans participated in whole health.
When teams share information about what matters to the veteran in a clinicianfacing format in the EHR, this helps ensure that the VHA honors veteran preferences throughout transitions of care and across all phases of health care. Although the EHR captures data on what matters, measurement of the overall impact on veteran and health system outcomes is essential. Further evaluation and ongoing education are needed to ensure clinicians are accurately and efficiently capturing the care provided by completing the appropriate EHR. Additional challenges include identifying ways to balance the documentation burden, while ensuring notes include valuable patient-centered information to guide care. EHR tools and templates have helped to unlock important insights on health care delivery in the VHA; however, health systems must consider how these clinical practices support the overall well-being of patients. How leaders empower frontline clinicians in any care setting to use these data to drive meaningful change is also important.
TRANSFORMING VHA CARE DELIVERY
In Achieving Whole Health: A New Approach for Veterans and the Nation, the National Academy of Science proposes a framework for the transformation of health care institutions to provide better whole health to veterans.3 Transformation requires change in entire systems and leaders who mobilize people “for participation in the process of change, encouraging a sense of collective identity and collective efficacy, which in turn brings stronger feelings of self-worth and self-efficacy,” and an enhanced sense of meaningfulness in their work and lives.18
Shifting health care approaches to equipping and empowering veterans and employees with whole health and AFHS resources is transformational and requires radically different assumptions and approaches that cannot be realized through traditional approaches. This change requires robust and multifaceted cultural transformation spanning all levels of the organization. Whole health and AFHS are facilitating this transformation by supporting documentation and data needs, tracking outcomes across settings, and accelerating spread to new facilities and care settings nationwide to support older veterans in improving their health and well-being.
Whole health and AFHS are complementary approaches to care that can work to empower veterans (as well as caregivers and clinicians) to align services with what matters most to veterans. Lessons such as standardizing person-centered assessments of what matters, creating supportive structures to better align care with veterans’ priorities, and identifying meaningful veteran and system-level outcomes to help sustain transformational change can be applied from whole health to AFHS. Together these programs have the potential to enhance overall health outcomes and quality of life for veterans.
- Kligler B, Hyde J, Gantt C, Bokhour B. The Whole Health transformation at the Veterans Health Administration: moving from “what’s the matter with you?” to “what matters to you?” Med Care. 2022;60(5):387-391. doi:10.1097/MLR.0000000000001706
- Centers for Disease Control and Prevention. Social determinants of health (SDOH) at CDC. January 17, 2024. Accessed September 12, 2024. https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html
- National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. The National Academies Press; 2023. Accessed September 9, 2024. doi:10.17226/26854
- Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58 Suppl 1(Suppl 1):5-8. doi:10.1111/1475-6773.14110
- Laderman M, Jackson C, Little K, Duong T, Pelton L. “What Matters” to older adults? A toolkit for health systems to design better care with older adults. Institute for Healthcare Improvement; 2019. Accessed September 9, 2024. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Age_Friendly_What_Matters_to_Older_Adults_Toolkit.pdf
- U.S. Department of Veterans Affairs. Age-Friendly Health Systems. Updated September 4, 2024. Accessed September 9, 2024. https://marketplace.va.gov/innovations/age-friendly-health-systems
- Brown TT, Hurley VB, Rodriguez HP, et al. Shared dec i s i o n - m a k i n g l o w e r s m e d i c a l e x p e n d i t u re s a n d the effect is amplified in racially-ethnically concordant relationships. Med Care. 2023;61(8):528-535. doi:10.1097/MLR.0000000000001881
- Kligler B. Whole Health in the Veterans Health Administration. Glob Adv Health Med. 2022;11:2164957X221077214.
- Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y
- U.S. Department of Veterans Affairs. Personal Health Inventory. Updated May 2022. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/docs/PHI-long-May22-fillable-508.pdf doi:10.1177/2164957X221077214
- Veterans Health Administration. Personal Health Plan. Updated March 2019. Accessed September 9, 2024. https:// www.va.gov/WHOLEHEALTH/docs/PersonalHealthPlan_508_03-2019.pdf
- Veterans Health Administration. Whole Health: My Life, My Story. Updated March 20, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/mylifemystory/index.asp
- U.S. Department of Veterans Affairs. Whole Health Library: Whole Health for Skill Building. Updated April 17, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- U.S. Department of Veterans Affairs. Making Decisions: Current Care Planning. Updated May 21, 2024. Accessed September 9, 2024. https://www.va.gov/geriatrics/pages/making_decisions.asp
- U.S. Department of Veterans Affairs. Life-Sustaining Treatment Decisions Initiative (LSTDI). Updated March 2024. Accessed September 12, 2024. https://marketplace.va.gov/innovations/life-sustaining-treatment-decisions-initiative
- U.S. Department of Veterans Affairs. Center for Health Equity Research and Promotion: Surgical Pause Saving Veterans Lives. Updated September 22, 2021. Accessed September 9, 2024. https://www.cherp.research.va.gov/features/Surgical_Pause_Saving_Veterans_Lives.asp
- Munro S, Church K, Berner C, et al. Implementation of an agefriendly template in the Veterans Health Administration electronic health record. J Inform Nurs. 2023;8(3):6-11.
- Burns JM. Transforming Leadership: A New Pursuit of Happiness. Grove Press; 2003.
- US Department of Veterans Affairs, Veterans Health Administration. Whole Health: Circle of Health Overview. Updated May 20, 2024. Accessed September 12, 2024. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
The COVID-19 pandemic established a new normal for health care delivery, with leaders rethinking core practices to survive and thrive in a changing environment and improve the health and well-being of patients. The Veterans Health Administration (VHA) is embracing a shift in focus from “what is the matter” to “what really matters” to address pre- and postpandemic challenges through a whole health approach.1 Initially conceptualized by the VHA in 2011, whole health “is an approach to health care that empowers and equips people to take charge of their health and well-being so that they can live their life to the fullest.”1 Whole health integrates evidence-based complementary and integrative health (CIH) therapies to manage pain; this includes acupuncture, meditation, tai chi, yoga, massage therapy, guided imagery, biofeedback, and clinical hypnosis.1 The VHA now recognizes well-being as a core value, helping clinicians respond to emerging challenges related to the social determinants of health (eg, access to health care, physical activity, and healthy foods) and guiding health care decision making.1,2
Well-being through empowerment—elements of whole health and Age-Friendly Health Systems (AFHS)—encourages health care institutions to work with employees, patients, and other stakeholders to address global challenges, clinician burnout, and social issues faced by their communities. This approach focuses on life’s purpose and meaning for individuals and inspires leaders to engage with patients, staff, and communities in new, impactful ways by focusing on wellbeing and wholeness rather than illness and disease. Having a higher sense of purpose is associated with lower all-cause mortality, reduced risk of specific diseases, better health behaviors, greater use of preventive services, and fewer hospital days of care.3
This article describes how AFHS supports the well-being of older adults and aligns with the whole health model of care. It also outlines the VHA investment to transform health care to be more person-centered by documenting what matters in the electronic health record (EHR).
AGE-FRIENDLY CARE
Given that nearly half of veterans enrolled in the VHA are aged ≥ 65 years, there is an increased need to identify models of care to support this aging population.4 This is especially critical because older veterans often have multiple chronic conditions and complex care needs that benefit from a whole person approach. The AFHS movement aims to provide evidence-based care aligned with what matters to older adults and provides a mechanism for transforming care to meet the needs of older veterans. This includes addressing age-related health concerns while promoting optimal health outcomes and quality of life. AFHS follows the 4Ms framework: what matters, medication, mentation, and mobility.5 The 4Ms serve as a guide for the health care of older adults in any setting, where each “M” is assessed and acted on to support what matters.5 Since 2020, > 390 teams have developed a plan to implement the 4Ms at 156 VHA facilities, demonstrating the VHA commitment to transforming health care for veterans.6
When VHA teams join the AFHS movement, they may also engage older veterans in a whole health system (WHS) (Figure). While AFHS is designed to improve care for patients aged ≥ 65 years, it also complements whole health, a person-centered approach available to all veterans enrolled in the VHA. Through the WHS and AFHS, veterans are empowered and equipped to take charge of their health and well-being through conversations about their unique goals, preferences, and health priorities.4 Clinicians are challenged to assess what matters by asking questions like, “What brings you joy?” and, “How can we help you meet your health goals?”1,5 These questions shift the conversation from disease-based treatment and enable clinicians to better understand the veteran as a person.1,5
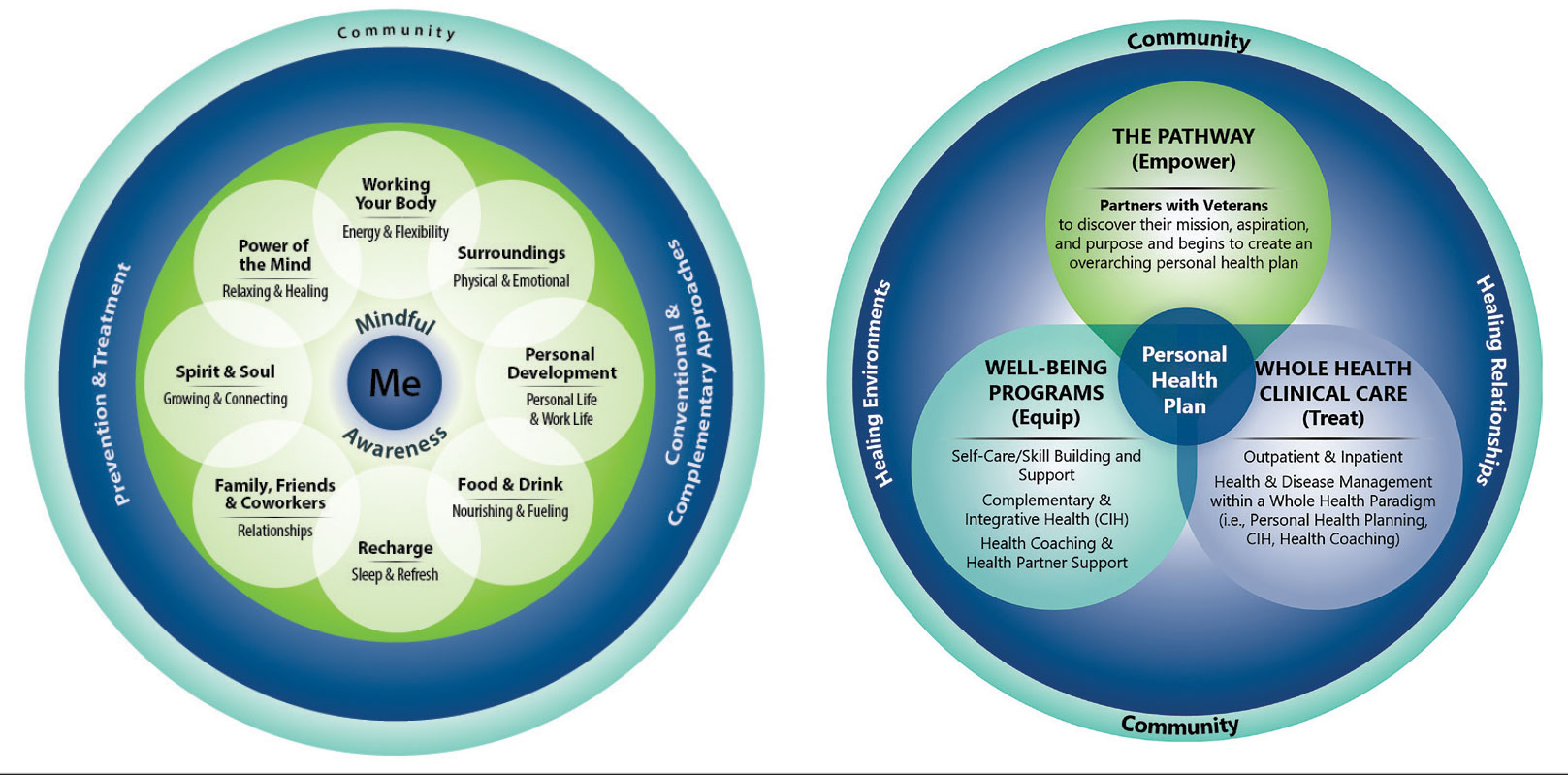
For whole health and AFHS, conversations about what matters are anchored in the veteran’s goals and preferences, especially those facing a significant health change (ie, a new diagnosis or treatment decision).5,7 Together, the veteran’s goals and priorities serve as the foundation for developing person-centered care plans that often go beyond conventional medical treatments to address the physical, mental, emotional, and social aspects of health.
SYSTEM-WIDE DIRECTIVE
The WHS enhances AFHS discussions about what matters to veterans by adding a system-level lens for conceptualizing health care delivery by leveraging the 3 components of WHS: the “pathway,” well-being programs, and whole health clinical care.
The Pathway
Discovering what matters, or the veteran’s “mission, aspiration, and purpose,” begins with the WHS pathway. When stepping into the pathway, veterans begin completing a personal health inventory, or “walking the circle of health,” which encourages self-reflection that focuses on components of their life that can influence health and well-being.1,8 The circle of health offers a visual representation of the 4 most important aspects of health and well-being: First, “Me” at the center as an individual who is the expert on their life, values, goals, and priorities. Only the individual can know what really matters through mindful awareness and what works for their life. Second, self-care consists of 8 areas that impact health and wellbeing: working your body; surroundings; personal development; food and drink; recharge; family, friends, and coworkers; spirit and soul; and power of the mind. Third, professional care consists of prevention, conventional care, and complementary care. Finally, the community that supports the individual.
Well-Being Programs
VHA provides WHS programs that support veterans in building self-care skills and improving their quality of life, often through integrative care clinics that offer coaching and CIH therapies. For example, a veteran who prioritizes mobility when seeking care at an integrative care clinic will not only receive conventional medical treatment for their physical symptoms but may also be offered CIH therapies depending on their goals. The veteran may set a daily mobility goal with their care team that supports what matters, incorporating CIH approaches, such as yoga and tai chi into the care plan.5 These holistic approaches for moving the body can help alleviate physical symptoms, reduce stress, improve mindful awareness, and provide opportunities for self-discovery and growth, thus promote overall well-being
Whole Health Clinical Care
AFHS and the 4Ms embody the clinical care component of the WHS. Because what matters is the driver of the 4Ms, every action taken by the care team supports wellbeing and quality of life by promoting independence, connection, and support, and addressing external factors, such as social determinants of health. At a minimum, well-being includes “functioning well: the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships.”9 From a system perspective, the VHA has begun to normalize focusing on what matters to veterans, using an interprofessional approach, one of the first steps to implementing AFHS.
As the programs expand, AFHS teams can learn from whole health well-being programs and increase the capacity for self-care in older veterans. Learning about the key elements included in the circle of health helps clinicians understand each veteran’s perceived strengths and weaknesses to support their self-care. From there, teams can act on the 4Ms and connect older veterans with the most appropriate programs and services at their facility, ensuring continuum of care.
DOCUMENTATION
The VHA leverages several tools and evidence-based practices to assess and act on what matters for veterans of all ages (Table).5,10-16 The VHA EHR and associated dashboards contain a wealth of information about whole health and AFHS implementation, scale up, and spread. A national AFHS 4Ms note template contains standardized data elements called health factors, which provide a mechanism for monitoring 4Ms care via its related dashboard. This template was developed by an interprofessional workgroup of VHA staff and underwent a thorough human factors engineering review and testing process prior to its release. Although teams continue to personalize care based on what matters to the veteran, data from the standardized 4Ms note template and dashboard provide a way to establish consistent, equitable care across multiple care settings.17
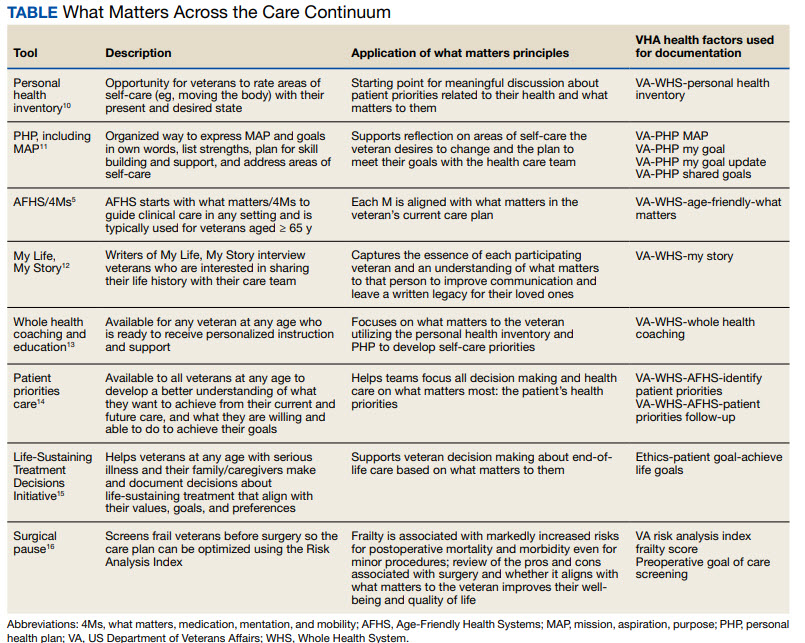
Between January 2022 and December 2023, > 612,000 participants aged ≥ 65 years identified what matters to them through 1.35 million assessments. During that period, > 36,000 veterans aged ≥ 65 years participated in AFHS and had what matters conversations documented. A personalized health plan was completed by 585,270 veterans for a total of 1.1 million assessments.11 Whole health coaching has been documented for > 57,000 veterans with > 200,000 assessments completed.13 In fiscal year 2023, a total of 1,802,131 veterans participated in whole health.
When teams share information about what matters to the veteran in a clinicianfacing format in the EHR, this helps ensure that the VHA honors veteran preferences throughout transitions of care and across all phases of health care. Although the EHR captures data on what matters, measurement of the overall impact on veteran and health system outcomes is essential. Further evaluation and ongoing education are needed to ensure clinicians are accurately and efficiently capturing the care provided by completing the appropriate EHR. Additional challenges include identifying ways to balance the documentation burden, while ensuring notes include valuable patient-centered information to guide care. EHR tools and templates have helped to unlock important insights on health care delivery in the VHA; however, health systems must consider how these clinical practices support the overall well-being of patients. How leaders empower frontline clinicians in any care setting to use these data to drive meaningful change is also important.
TRANSFORMING VHA CARE DELIVERY
In Achieving Whole Health: A New Approach for Veterans and the Nation, the National Academy of Science proposes a framework for the transformation of health care institutions to provide better whole health to veterans.3 Transformation requires change in entire systems and leaders who mobilize people “for participation in the process of change, encouraging a sense of collective identity and collective efficacy, which in turn brings stronger feelings of self-worth and self-efficacy,” and an enhanced sense of meaningfulness in their work and lives.18
Shifting health care approaches to equipping and empowering veterans and employees with whole health and AFHS resources is transformational and requires radically different assumptions and approaches that cannot be realized through traditional approaches. This change requires robust and multifaceted cultural transformation spanning all levels of the organization. Whole health and AFHS are facilitating this transformation by supporting documentation and data needs, tracking outcomes across settings, and accelerating spread to new facilities and care settings nationwide to support older veterans in improving their health and well-being.
Whole health and AFHS are complementary approaches to care that can work to empower veterans (as well as caregivers and clinicians) to align services with what matters most to veterans. Lessons such as standardizing person-centered assessments of what matters, creating supportive structures to better align care with veterans’ priorities, and identifying meaningful veteran and system-level outcomes to help sustain transformational change can be applied from whole health to AFHS. Together these programs have the potential to enhance overall health outcomes and quality of life for veterans.
The COVID-19 pandemic established a new normal for health care delivery, with leaders rethinking core practices to survive and thrive in a changing environment and improve the health and well-being of patients. The Veterans Health Administration (VHA) is embracing a shift in focus from “what is the matter” to “what really matters” to address pre- and postpandemic challenges through a whole health approach.1 Initially conceptualized by the VHA in 2011, whole health “is an approach to health care that empowers and equips people to take charge of their health and well-being so that they can live their life to the fullest.”1 Whole health integrates evidence-based complementary and integrative health (CIH) therapies to manage pain; this includes acupuncture, meditation, tai chi, yoga, massage therapy, guided imagery, biofeedback, and clinical hypnosis.1 The VHA now recognizes well-being as a core value, helping clinicians respond to emerging challenges related to the social determinants of health (eg, access to health care, physical activity, and healthy foods) and guiding health care decision making.1,2
Well-being through empowerment—elements of whole health and Age-Friendly Health Systems (AFHS)—encourages health care institutions to work with employees, patients, and other stakeholders to address global challenges, clinician burnout, and social issues faced by their communities. This approach focuses on life’s purpose and meaning for individuals and inspires leaders to engage with patients, staff, and communities in new, impactful ways by focusing on wellbeing and wholeness rather than illness and disease. Having a higher sense of purpose is associated with lower all-cause mortality, reduced risk of specific diseases, better health behaviors, greater use of preventive services, and fewer hospital days of care.3
This article describes how AFHS supports the well-being of older adults and aligns with the whole health model of care. It also outlines the VHA investment to transform health care to be more person-centered by documenting what matters in the electronic health record (EHR).
AGE-FRIENDLY CARE
Given that nearly half of veterans enrolled in the VHA are aged ≥ 65 years, there is an increased need to identify models of care to support this aging population.4 This is especially critical because older veterans often have multiple chronic conditions and complex care needs that benefit from a whole person approach. The AFHS movement aims to provide evidence-based care aligned with what matters to older adults and provides a mechanism for transforming care to meet the needs of older veterans. This includes addressing age-related health concerns while promoting optimal health outcomes and quality of life. AFHS follows the 4Ms framework: what matters, medication, mentation, and mobility.5 The 4Ms serve as a guide for the health care of older adults in any setting, where each “M” is assessed and acted on to support what matters.5 Since 2020, > 390 teams have developed a plan to implement the 4Ms at 156 VHA facilities, demonstrating the VHA commitment to transforming health care for veterans.6
When VHA teams join the AFHS movement, they may also engage older veterans in a whole health system (WHS) (Figure). While AFHS is designed to improve care for patients aged ≥ 65 years, it also complements whole health, a person-centered approach available to all veterans enrolled in the VHA. Through the WHS and AFHS, veterans are empowered and equipped to take charge of their health and well-being through conversations about their unique goals, preferences, and health priorities.4 Clinicians are challenged to assess what matters by asking questions like, “What brings you joy?” and, “How can we help you meet your health goals?”1,5 These questions shift the conversation from disease-based treatment and enable clinicians to better understand the veteran as a person.1,5
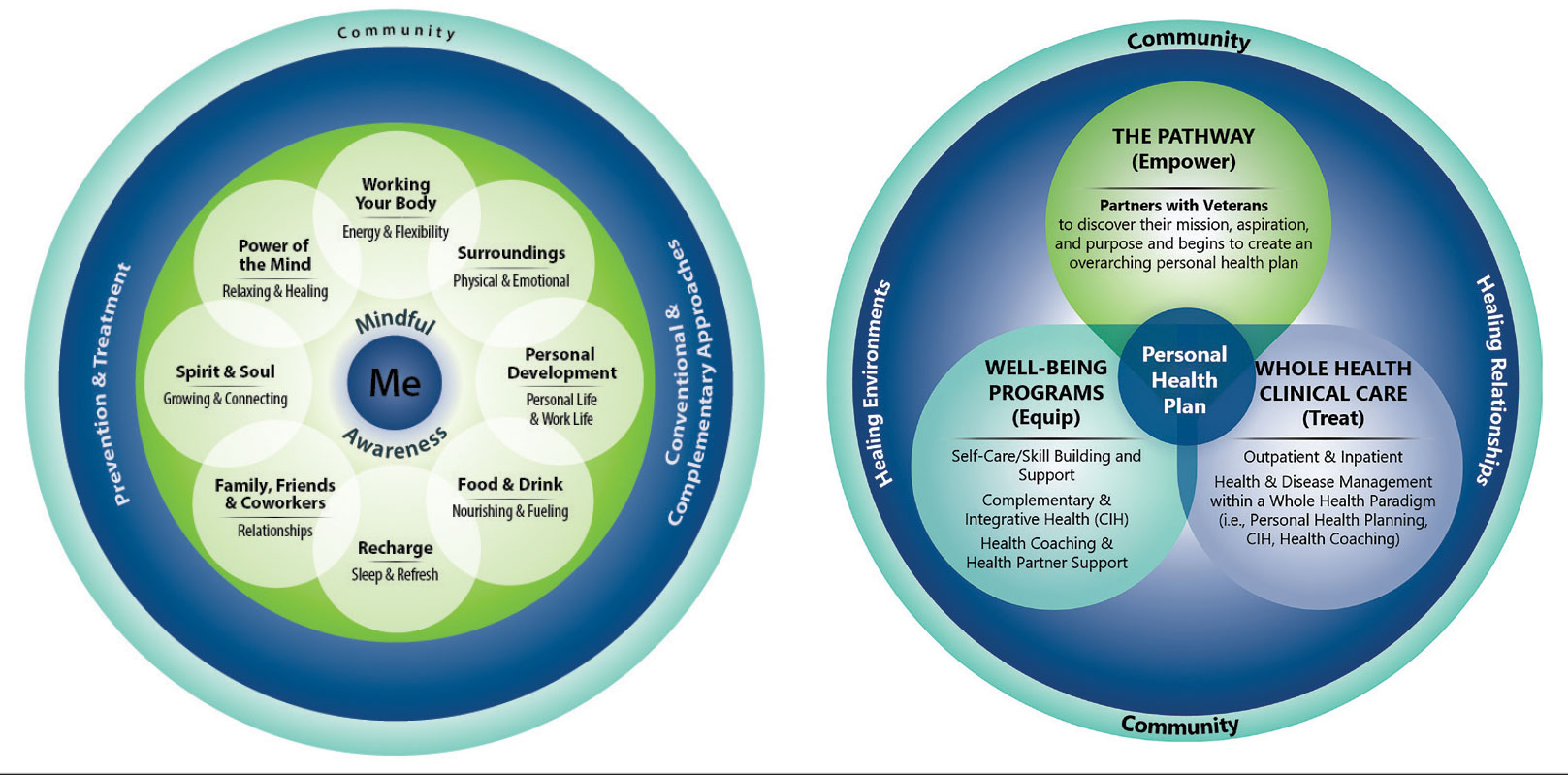
For whole health and AFHS, conversations about what matters are anchored in the veteran’s goals and preferences, especially those facing a significant health change (ie, a new diagnosis or treatment decision).5,7 Together, the veteran’s goals and priorities serve as the foundation for developing person-centered care plans that often go beyond conventional medical treatments to address the physical, mental, emotional, and social aspects of health.
SYSTEM-WIDE DIRECTIVE
The WHS enhances AFHS discussions about what matters to veterans by adding a system-level lens for conceptualizing health care delivery by leveraging the 3 components of WHS: the “pathway,” well-being programs, and whole health clinical care.
The Pathway
Discovering what matters, or the veteran’s “mission, aspiration, and purpose,” begins with the WHS pathway. When stepping into the pathway, veterans begin completing a personal health inventory, or “walking the circle of health,” which encourages self-reflection that focuses on components of their life that can influence health and well-being.1,8 The circle of health offers a visual representation of the 4 most important aspects of health and well-being: First, “Me” at the center as an individual who is the expert on their life, values, goals, and priorities. Only the individual can know what really matters through mindful awareness and what works for their life. Second, self-care consists of 8 areas that impact health and wellbeing: working your body; surroundings; personal development; food and drink; recharge; family, friends, and coworkers; spirit and soul; and power of the mind. Third, professional care consists of prevention, conventional care, and complementary care. Finally, the community that supports the individual.
Well-Being Programs
VHA provides WHS programs that support veterans in building self-care skills and improving their quality of life, often through integrative care clinics that offer coaching and CIH therapies. For example, a veteran who prioritizes mobility when seeking care at an integrative care clinic will not only receive conventional medical treatment for their physical symptoms but may also be offered CIH therapies depending on their goals. The veteran may set a daily mobility goal with their care team that supports what matters, incorporating CIH approaches, such as yoga and tai chi into the care plan.5 These holistic approaches for moving the body can help alleviate physical symptoms, reduce stress, improve mindful awareness, and provide opportunities for self-discovery and growth, thus promote overall well-being
Whole Health Clinical Care
AFHS and the 4Ms embody the clinical care component of the WHS. Because what matters is the driver of the 4Ms, every action taken by the care team supports wellbeing and quality of life by promoting independence, connection, and support, and addressing external factors, such as social determinants of health. At a minimum, well-being includes “functioning well: the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships.”9 From a system perspective, the VHA has begun to normalize focusing on what matters to veterans, using an interprofessional approach, one of the first steps to implementing AFHS.
As the programs expand, AFHS teams can learn from whole health well-being programs and increase the capacity for self-care in older veterans. Learning about the key elements included in the circle of health helps clinicians understand each veteran’s perceived strengths and weaknesses to support their self-care. From there, teams can act on the 4Ms and connect older veterans with the most appropriate programs and services at their facility, ensuring continuum of care.
DOCUMENTATION
The VHA leverages several tools and evidence-based practices to assess and act on what matters for veterans of all ages (Table).5,10-16 The VHA EHR and associated dashboards contain a wealth of information about whole health and AFHS implementation, scale up, and spread. A national AFHS 4Ms note template contains standardized data elements called health factors, which provide a mechanism for monitoring 4Ms care via its related dashboard. This template was developed by an interprofessional workgroup of VHA staff and underwent a thorough human factors engineering review and testing process prior to its release. Although teams continue to personalize care based on what matters to the veteran, data from the standardized 4Ms note template and dashboard provide a way to establish consistent, equitable care across multiple care settings.17
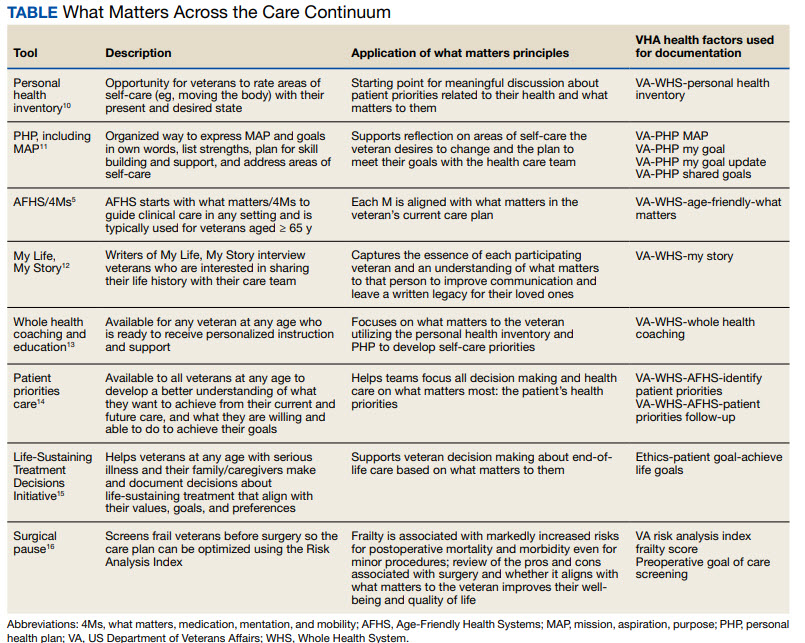
Between January 2022 and December 2023, > 612,000 participants aged ≥ 65 years identified what matters to them through 1.35 million assessments. During that period, > 36,000 veterans aged ≥ 65 years participated in AFHS and had what matters conversations documented. A personalized health plan was completed by 585,270 veterans for a total of 1.1 million assessments.11 Whole health coaching has been documented for > 57,000 veterans with > 200,000 assessments completed.13 In fiscal year 2023, a total of 1,802,131 veterans participated in whole health.
When teams share information about what matters to the veteran in a clinicianfacing format in the EHR, this helps ensure that the VHA honors veteran preferences throughout transitions of care and across all phases of health care. Although the EHR captures data on what matters, measurement of the overall impact on veteran and health system outcomes is essential. Further evaluation and ongoing education are needed to ensure clinicians are accurately and efficiently capturing the care provided by completing the appropriate EHR. Additional challenges include identifying ways to balance the documentation burden, while ensuring notes include valuable patient-centered information to guide care. EHR tools and templates have helped to unlock important insights on health care delivery in the VHA; however, health systems must consider how these clinical practices support the overall well-being of patients. How leaders empower frontline clinicians in any care setting to use these data to drive meaningful change is also important.
TRANSFORMING VHA CARE DELIVERY
In Achieving Whole Health: A New Approach for Veterans and the Nation, the National Academy of Science proposes a framework for the transformation of health care institutions to provide better whole health to veterans.3 Transformation requires change in entire systems and leaders who mobilize people “for participation in the process of change, encouraging a sense of collective identity and collective efficacy, which in turn brings stronger feelings of self-worth and self-efficacy,” and an enhanced sense of meaningfulness in their work and lives.18
Shifting health care approaches to equipping and empowering veterans and employees with whole health and AFHS resources is transformational and requires radically different assumptions and approaches that cannot be realized through traditional approaches. This change requires robust and multifaceted cultural transformation spanning all levels of the organization. Whole health and AFHS are facilitating this transformation by supporting documentation and data needs, tracking outcomes across settings, and accelerating spread to new facilities and care settings nationwide to support older veterans in improving their health and well-being.
Whole health and AFHS are complementary approaches to care that can work to empower veterans (as well as caregivers and clinicians) to align services with what matters most to veterans. Lessons such as standardizing person-centered assessments of what matters, creating supportive structures to better align care with veterans’ priorities, and identifying meaningful veteran and system-level outcomes to help sustain transformational change can be applied from whole health to AFHS. Together these programs have the potential to enhance overall health outcomes and quality of life for veterans.
- Kligler B, Hyde J, Gantt C, Bokhour B. The Whole Health transformation at the Veterans Health Administration: moving from “what’s the matter with you?” to “what matters to you?” Med Care. 2022;60(5):387-391. doi:10.1097/MLR.0000000000001706
- Centers for Disease Control and Prevention. Social determinants of health (SDOH) at CDC. January 17, 2024. Accessed September 12, 2024. https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html
- National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. The National Academies Press; 2023. Accessed September 9, 2024. doi:10.17226/26854
- Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58 Suppl 1(Suppl 1):5-8. doi:10.1111/1475-6773.14110
- Laderman M, Jackson C, Little K, Duong T, Pelton L. “What Matters” to older adults? A toolkit for health systems to design better care with older adults. Institute for Healthcare Improvement; 2019. Accessed September 9, 2024. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Age_Friendly_What_Matters_to_Older_Adults_Toolkit.pdf
- U.S. Department of Veterans Affairs. Age-Friendly Health Systems. Updated September 4, 2024. Accessed September 9, 2024. https://marketplace.va.gov/innovations/age-friendly-health-systems
- Brown TT, Hurley VB, Rodriguez HP, et al. Shared dec i s i o n - m a k i n g l o w e r s m e d i c a l e x p e n d i t u re s a n d the effect is amplified in racially-ethnically concordant relationships. Med Care. 2023;61(8):528-535. doi:10.1097/MLR.0000000000001881
- Kligler B. Whole Health in the Veterans Health Administration. Glob Adv Health Med. 2022;11:2164957X221077214.
- Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y
- U.S. Department of Veterans Affairs. Personal Health Inventory. Updated May 2022. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/docs/PHI-long-May22-fillable-508.pdf doi:10.1177/2164957X221077214
- Veterans Health Administration. Personal Health Plan. Updated March 2019. Accessed September 9, 2024. https:// www.va.gov/WHOLEHEALTH/docs/PersonalHealthPlan_508_03-2019.pdf
- Veterans Health Administration. Whole Health: My Life, My Story. Updated March 20, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/mylifemystory/index.asp
- U.S. Department of Veterans Affairs. Whole Health Library: Whole Health for Skill Building. Updated April 17, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- U.S. Department of Veterans Affairs. Making Decisions: Current Care Planning. Updated May 21, 2024. Accessed September 9, 2024. https://www.va.gov/geriatrics/pages/making_decisions.asp
- U.S. Department of Veterans Affairs. Life-Sustaining Treatment Decisions Initiative (LSTDI). Updated March 2024. Accessed September 12, 2024. https://marketplace.va.gov/innovations/life-sustaining-treatment-decisions-initiative
- U.S. Department of Veterans Affairs. Center for Health Equity Research and Promotion: Surgical Pause Saving Veterans Lives. Updated September 22, 2021. Accessed September 9, 2024. https://www.cherp.research.va.gov/features/Surgical_Pause_Saving_Veterans_Lives.asp
- Munro S, Church K, Berner C, et al. Implementation of an agefriendly template in the Veterans Health Administration electronic health record. J Inform Nurs. 2023;8(3):6-11.
- Burns JM. Transforming Leadership: A New Pursuit of Happiness. Grove Press; 2003.
- US Department of Veterans Affairs, Veterans Health Administration. Whole Health: Circle of Health Overview. Updated May 20, 2024. Accessed September 12, 2024. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
- Kligler B, Hyde J, Gantt C, Bokhour B. The Whole Health transformation at the Veterans Health Administration: moving from “what’s the matter with you?” to “what matters to you?” Med Care. 2022;60(5):387-391. doi:10.1097/MLR.0000000000001706
- Centers for Disease Control and Prevention. Social determinants of health (SDOH) at CDC. January 17, 2024. Accessed September 12, 2024. https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html
- National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. The National Academies Press; 2023. Accessed September 9, 2024. doi:10.17226/26854
- Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58 Suppl 1(Suppl 1):5-8. doi:10.1111/1475-6773.14110
- Laderman M, Jackson C, Little K, Duong T, Pelton L. “What Matters” to older adults? A toolkit for health systems to design better care with older adults. Institute for Healthcare Improvement; 2019. Accessed September 9, 2024. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Age_Friendly_What_Matters_to_Older_Adults_Toolkit.pdf
- U.S. Department of Veterans Affairs. Age-Friendly Health Systems. Updated September 4, 2024. Accessed September 9, 2024. https://marketplace.va.gov/innovations/age-friendly-health-systems
- Brown TT, Hurley VB, Rodriguez HP, et al. Shared dec i s i o n - m a k i n g l o w e r s m e d i c a l e x p e n d i t u re s a n d the effect is amplified in racially-ethnically concordant relationships. Med Care. 2023;61(8):528-535. doi:10.1097/MLR.0000000000001881
- Kligler B. Whole Health in the Veterans Health Administration. Glob Adv Health Med. 2022;11:2164957X221077214.
- Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y
- U.S. Department of Veterans Affairs. Personal Health Inventory. Updated May 2022. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/docs/PHI-long-May22-fillable-508.pdf doi:10.1177/2164957X221077214
- Veterans Health Administration. Personal Health Plan. Updated March 2019. Accessed September 9, 2024. https:// www.va.gov/WHOLEHEALTH/docs/PersonalHealthPlan_508_03-2019.pdf
- Veterans Health Administration. Whole Health: My Life, My Story. Updated March 20, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/mylifemystory/index.asp
- U.S. Department of Veterans Affairs. Whole Health Library: Whole Health for Skill Building. Updated April 17, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- U.S. Department of Veterans Affairs. Making Decisions: Current Care Planning. Updated May 21, 2024. Accessed September 9, 2024. https://www.va.gov/geriatrics/pages/making_decisions.asp
- U.S. Department of Veterans Affairs. Life-Sustaining Treatment Decisions Initiative (LSTDI). Updated March 2024. Accessed September 12, 2024. https://marketplace.va.gov/innovations/life-sustaining-treatment-decisions-initiative
- U.S. Department of Veterans Affairs. Center for Health Equity Research and Promotion: Surgical Pause Saving Veterans Lives. Updated September 22, 2021. Accessed September 9, 2024. https://www.cherp.research.va.gov/features/Surgical_Pause_Saving_Veterans_Lives.asp
- Munro S, Church K, Berner C, et al. Implementation of an agefriendly template in the Veterans Health Administration electronic health record. J Inform Nurs. 2023;8(3):6-11.
- Burns JM. Transforming Leadership: A New Pursuit of Happiness. Grove Press; 2003.
- US Department of Veterans Affairs, Veterans Health Administration. Whole Health: Circle of Health Overview. Updated May 20, 2024. Accessed September 12, 2024. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
Establishing a Just Culture: Implications for the Veterans Health Administration Journey to High Reliability
Medical errors are a persistent problem and leading cause of preventable death in the United States. There is considerable momentum behind the idea that implementation of a just culture is foundational to detecting and learning from errors in pursuit of zero patient harm.1-6 Just culture is a framework that fosters an environment of trust within health care organizations, aiming to achieve fair outcomes for those involved in incidents or near misses. It emphasizes openness, accountability, and learning, prioritizing the repair of harm and systemic improvement over assigning blame.7
A just culture mindset reflects a significant shift in thinking that moves from the tendency to blame and punish others toward a focus on organizational learning and continued process improvement.8,9 This systemic shift in fundamental thinking transforms how leaders approach staff errors and how they are addressed.10 In essence, just culture reflects an ethos centered on openness, a deep appreciation of human fallibility, and shared accountability at both the individual and organizational levels.
Organizational learning and innovation are stifled in the absence of a just culture, and there is a tendency for employees to avoid disclosing their own errors as well as those of their colleagues.11 The transformation to a just culture is often slowed or disrupted by personal, systemic, and cultural barriers.12 It is imperative that all executive, service line, and frontline managers recognize and execute their distinct responsibilities while adjudicating the appropriate course of action in the aftermath of adverse events or near misses. This requires a nuanced understanding of the factors that contribute to errors at the individual and organizational levels to ensure an appropriate response.
The Veterans Health Administration (VHA) is orchestrating an enterprise transformation to develop into a high reliability organization (HRO). This began with a single-site test in 2016, which demonstrated successful results in patient safety culture, patient safety event reporting, and patient safety outcomes.13 In 2019, the VHA formally launched its enterprise-wide HRO journey in 18 hospital facilities, followed by successive waves of 67 and 54 facilities in 2021 and 2022, respectively. The VHA journey to transform into an HRO aligns with 3 pillars, 5 principles, and 7 values. The VHA has emphasized the importance of just culture as a foundational element of the HRO framework, specifically under the pillar of leadership. To promote leadership engagement, the VHA has employed an array of approaches that include education, leader coaching, and change management strategies. Given the diversity among VHA facilities, each with local cultures and histories, some sites have more readily implemented a just culture than others.14 A deeper exploration into potential obstacles, particularly concerning leadership engagement, could be instrumental for formulating strategies that further establish a just culture across the VHA.15
There is a paucity of empirical research regarding factors that facilitate and/or impede the implementation of a just culture in health care settings.16,17 Likert scale surveys, such as the Patient Safety Culture Module for the VHA All Employee Survey and its predecessor, the Patient Safety Culture Survey, have been used to assess culture and climate.18 However, qualitative evaluations directly assessing the lived experiences of those trying to implement a just culture provide additional depth and context that can help identify specific factors that support or impede becoming an HRO. The purpose of this study was to increase understanding of factors that influence the establishment and sustainment of a just culture and to identify specific methods for improving the implementation of just culture principles and practices aligned with HRO.
METHODS
This qualitative study explored facilitators and barriers to establishing and sustaining a just culture as experienced across a subset of VHA facilities by HRO leads or staff assigned with the primary responsibilities of supporting facility-level HRO transformation. HRO leads are assigned responsibility for supporting executive leadership in planning, coordinating, implementing, and monitoring activities to ensure effective high reliability efforts, including focused efforts to establish a robust patient safety program, a culture of safety, and a culture of continuous process improvement.
Virtual focus group discussions held via Microsoft Teams generated in-depth, diverse perspectives from participants across 16 VHA facilities. Qualitative research and evaluation methods provide an enhanced depth of understanding and allow the emergence of detailed data.19 A qualitative grounded theory approach elicits complex, multifaceted phenomena that cannot be appreciated solely by numeric data.20 Grounded theory was selected to limit preconceived notions and provide a more systematic analysis, including open, axial, and thematic coding. Such methods afford opportunities to adapt to unplanned follow-up questions and thus provide a flexible approach to generate new ideas and concepts.21 Additionally, qualitative methods help overcome the tendencies of respondents to agree rather than disagree when presented with Likert-style scales, which tend to skew responses toward the positive.22
Participants must have been assigned as an HRO lead for ≥ 6 months at the same facility. Potential participants were identified through purposive sampling, considering their leadership roles in HRO and experience with just culture implementation, the size and complexity of their facility, and geographic distribution. Invitations explaining the study and encouraging voluntary participation to participate were emailed. Of 37 HRO leads invited to participate in the study, 16 agreed to participate and attended 1 of 3 hour-long focus group sessions. One session was rescheduled due to limited attendance. Participants represented a mix of VHA sites in terms of geography, facility size, and complexity.
Focus Group Procedures
Demographic data were collected prior to sessions via an online form to better understand the participant population, including facility complexity level, length of time in HRO lead role, clinical background, and facility level just culture training. Each session was led by an experienced focus group facilitator (CV) who was not directly involved with the overall HRO implementation to establish a neutral perspective. Each session was attended by 4 to 7 participants and 2 observers who took notes. The sessions were recorded and included automated transcriptions, which were edited for accuracy.
Focus group sessions began with a brief introduction and an opportunity for participants to ask questions. Participants were then asked a series of open-ended questions to elicit responses regardingfacilitators, barriers, and leadership support needed for implementing just culture. The questions were part of a facilitator guide that included an introductory script and discussion prompts to ensure consistency across focus groups.
Facilitators were defined as factors that increase the likelihood of establishing or sustaining a just culture. Barriers were defined as factors that decrease or inhibit the likelihood of establishing or sustaining just culture. The focus group facilitator encouraged all participants to share their views and provided clarification if needed, as well as prompts and examples where appropriate, but primarily sought to elicit responses to the questions.
Institutional review board review and approval were not required for this quality improvement initiative. The project adhered to ethical standards of research, including asking participants for verbal consent and preserving their confidentiality. Participation was voluntary, and prior to the focus group sessions, participants were provided information explaining the study’s purpose, procedures, and their rights. Participant identities were kept confidential, and all data were anonymized during the analysis phase. Pseudonyms or identifiers were used during data transcription to protect participant identity. All data, including recordings and transcriptions, were stored on password-protected devices accessible only to the research team. Any identifiable information was removed during data analysis to ensure confidentiality.
Analysis
Focus group recordings were transcribed verbatim, capturing all verbal interactions and nonverbal cues that may contribute to understanding the participants' perspectives. Thematic analysis was used to analyze the qualitative data from the focus group discussions.23 The transcribed data were organized, coded, and analyzed using ATLAS.ti 23 qualitative data software to identify key themes and patterns.
Results
The themes identified include the 5 facilitators, barriers, and recommendations most frequently mentioned by HRO leads across focus group sessions. The nature of each theme is described, along with commonly mentioned examples and direct quotes from participants that illustrate our understanding of their perspectives.
Facilitators
Training and coaching (26 responses). The availability of training around the Just Culture Decision Support Tool (DST) was cited as a practical aid in guiding leaders through complex just culture decisions to ensure consistency and fairness. Additionally, an executive leadership team that served as champions for just culture principles played a vital role in promoting and sustaining the approach: “Training them on the roll-out of the decision support tool with supervisors at all levels, and education for just culture and making it part of our safety forum has helped for the last 4 months.” “Having some regular training and share-out cadences embedded within the schedule as well as dynamic directors and well-trained executive leadership team (ELT) for support has been a facilitator.”
Increased transparency (16 responses). Participants consistently highlighted the importance of leadership transparency as a key facilitator for implementing just culture. Open and honest communication from top-level executives fostered an environment of trust and accountability. Approachable and physically present leadership was seen as essential for creating a culture where employees felt comfortable reporting errors and concerns without fear of retaliation: “They’re surprisingly honest with themselves about what we can do, what we cannot do, and they set the expectations exactly at that.”
Approachable leadership (15 responses). Participants frequently mentioned the importance of having dynamic leadership spearheading the implementation of just culture and leading by example. Having a leadership team that accepts accountability and reinforces consistency in the manner that near misses or mistakes are addressed is paramount to promoting the principles of just culture and increasing psychological safety: “We do have very approachable leadership, which I know is hard if you’re trying to implement that nationwide, it’s hard to implement approachability. But I do think that people raise their concerns, and they’ll stop them in the hallway and ask them questions. So, in terms of comfort level with the executive leadership, I do think that’s high, which would promote psychological safety.”
Feedback loops and follow through (13 responses). Participants emphasized the importance of taking concrete actions to address concerns and improve processes. Regular check-ins with supervisors to discuss matters related to just culture provided a structured opportunity for addressing issues and reinforcing the importance of the approach: “One thing that we’ve really focused on is not only identifying mistakes, but [taking] ownership. We continue to track it until … it’s completed and then a process of how to communicate that back and really using closed loop communication with the staff and letting them know.”
Forums and town halls (10 responses). These platforms created feedback loops that were seen as invaluable tools for sharing near misses, celebrating successes, and promoting open dialogue. Forums and town halls cultivated a culture of continuous improvement and trust: “We’ll celebrate catches, a safety story is inside that catch. So, if we celebrate the change, people feel safer to speak up.” “Truthfully, we’ve had a great relationship since establishing our safety forums and just value open lines of communication.”
Barriers
Inadequate training (30 responses). Insufficient engagement during training—limited bandwidth and availability to attend and actively participate in training—was perceived as detrimental to creating awareness and buy-in from staff, supervisors, and leadership, thereby hindering successful integration of just culture principles. Participants also identified too many conflicting priorities from VHA leadership, which contributes to training and information fatigue among staff and supervisors. “Our biggest barrier is just so many different competing priorities going on. We have so much that we’re asking people to do.” “One hundred percent training is feeling more like a ticked box than actually yielding results, I have a very hard time getting staff engaged.”
Inconsistency between executive leaders and middle managers (28 responses). A lack of consistency in the commitment to and enactment of just culture principles among leaders poses a challenge. Participants gave several examples of inconsistencies in messaging and reinforcement of just culture principles, leading to confusion among staff and hindering adoption. Likewise, the absence of standardized procedures for implementing just culture created variability: “The director coming in and trying to change things, it put a lot of resistance, we struggle with getting the other ELT members on board … some of the messages that come out at times can feel more punitive.”
Middle management resistance (22 responses). In some instances, participants reported middle managers exhibiting attitudes and behaviors that undermined the application of just culture principles and effectiveness. Such attitudes and behaviors were attributed to a lack of adequate training, coaching, and awareness. Other perceived contributions included fear of failure and a desire to distance oneself from staff who have made mistakes: “As soon as someone makes an error, they go straight to suspend them, and that’s the disconnect right there.” “There’s almost a level of working in the opposite direction in some of the mid-management.”
Cultural misalignment (18 responses). The existing culture of distancing oneself from mistakes presented a significant barrier to the adoption of just culture because it clashed with the principles of open reporting and accountability. Staff underreported errors or framed them in a way that minimized personal responsibility, thereby making it more essential to put in the necessary and difficult work to learn from mistakes: “One, you’re going to get in trouble. There’s going to be more work added to you or something of that nature."
Lack of accountability for opposition(17 responses). Participants noted a clear lack of accountability for those who opposed or showed resistance to just culture, which allowed resistance to persist without consequences. In many instances, leaders were described as having overlooked repeated instances of unjust attitudes and behaviors (eg, inappropriate blame or punishment), which allowed those practices to continue. “Executive leadership is standing on the hill and saying we’re a just culture and we do everything correctly, and staff has the expectation that they’re going to be treated with just culture and then the middle management is setting that on fire, then we show them that that’s not just culture, and they continue to have those poor behaviors, but there’s a lack of accountability.”
Limited bandwidth and lack of coordination (14 responses). HRO leads often faced role-specific constraints in having adequate time and authority to coordinate efforts to implement or sustain just culture. This includes challenges with coordination across organizational levels (eg, between the hospital and regional Veterans Integrated Service Network [VISN] management levels) and across departments within the hospital (eg, between human resources and service lines or units). “Our VISN human resources is completely detached. They’ll not cooperate with these efforts, which is hard.” “There’s not enough bandwidth to actually support, I’m just 1 person.” “[There’s] all these mandated trainings of 8 hours when we’re already fatigued, short-staffed, taking 3 other HRO classes.”
Recommendations
Training improvements (24 responses). HRO leads recommended that comprehensive training programs be developed and implemented for staff, supervisors, and leadership to increase awareness and understanding of just culture principles. These training initiatives should focus on fostering a shared understanding of the core tenets of just culture, the importance of error reporting, and the processes involved in fair and consistent decision making (eg, training simulations on use of the Just Culture DST). “We’ve really never had any formal training on the decision support tool. I hope that what’s coming out for next year. We’ll have some more formal training for the tool because I think it would be great to really have our leadership and our supervisors and our managers use that tool.” “We can give a more directed and intentional training to leadership on the 4 foundational practices and what it means to implement those and what it means to utilize that behavioral component of HRO.”
Clear and consistent procedures toincrease accountability (22 responses). To promote a culture of accountability and consistency in the application of just culture principles, organizations should establish clear mechanisms for reporting, investigating, and addressing incidents. Standardized procedures and DSTs can aid in ensuring that responses to errors are equitable and align with just culture principles: “I recommend accountability; if it’s clearly evidenced that you’re not toeing the just culture line, then we need to be able to do something about it and not just finger wag.” “[We need to have] a templated way to approach just culture implementation. The decision support tool is great, I absolutely love having the resources and being able to find a lot of clinical examples and discussion tools like that. But when it comes down to it, not having that kind of official thing to fall back on it can be a little bit rough.”
Additional coaching and consultationsupport (15 responses). To support supervisors in effectively implementing just culture within their teams, participants recommended that organizations provide ongoing coaching and mentorship opportunities. Additionally, third-party consultants with expertise in just culture were described as offering valuable guidance, particularly in cases where internal staff resources or HRO lead bandwidth may be limited. “There are so many consulting agencies with HRO that have been contracted to do different projects, but maybe that can help with an educational program.” “I want to see my executive leadership coach the supervisors up right and then allow them to do one-on-ones and facilitate and empower the frontline staff, and it’s just a good way of transparency and communication.”
Improved leadership sponsorship (15 responses). Participants noted that leadership buy-in is crucial for the successful implementation of just culture. Facilities should actively engage and educate leadership teams on the benefits of just culture and how it aligns with broader patient safety and organizational goals. Leaders should be visible and active champions of its principles, supporting change in their daily engagements with staff. “ELT support is absolutely necessary. Why? Because they will make it important to those in their service lines. They will make it important to those supervisors and managers. If it’s not important to that ELT member, then it’s not going to be important to that manager or that supervisor.”
Improved collaboration with patient safety and human resources (6 responses). Collaborative efforts with patient safety and human resources departments were seen as instrumental in supporting just culture, emphasizing its importance, and effectively addressing issues. Coordinating with these departments specifically contributes to consistent reinforcement and expands the bandwidth of HRO leads. These departments play integral roles in supporting just culture through effective policies, procedures, and communication. “I think it would be really helpful to have common language between what human resources teaches and what is in our decision support tool.”
DISCUSSION
This study sought to collect and synthesize the experiences of leaders across a large, integrated health care system in establishing and sustaining a just culture as part of an enterprise journey to become an HRO.24 The VHA has provided enterprise-wide support (eg, training, leader coaching, and communications) for the implementation of HRO principles and practices with the goal of creating a culture of safety, which includes just culture elements. This support includes enterprise program offices, VISNs, and hospital facilities, though notably, there is variability in how HRO is implemented at the local level. The facilitators, barriers, and recommendations presented in this article are representative of the designated HRO leads at VHA hospital facilities who have direct experience with implementing and sustaining just culture. The themes presented offer specific opportunities for intervention and actionable strategies to enhance just culture initiatives, foster psychological safety and accountability, and ultimately improve the quality of care and patient outcomes.3,25
Frequently identified facilitators such as providing training and coaching, having leaders who are available and approachable, demonstrating follow-through to address identified issues, and creating venues where errors and successes can be openly discussed.26 These facilitators are aligned with enterprise HRO support strategies orchestrated by the VHA at the enterprise VISN and facility levels to support a culture of safety, continuous process improvement, and leadership commitment.
Frequently identified barriers included inadequate training, inconsistent application of just culture by middle managers vs senior leaders, a lack of accountability or corrective action when unjust corrective actions took place, time and resource constraints, and inadequate coordination across departments (eg, operational departments and human resources) and organizational levels. These factors were identified through focus groups with a limited set of HRO leads. They may reflect challenges to changing culture that may be deeply engrained in individual histories, organizational norms, and systemic practices. Improving upon these just culture initiatives requires multifaceted approaches and working through resistance to change.
VHA HRO leads identified several actionable recommendations that may be used in pursuit of a just culture. First, improvements in training involving how to apply just culture principles and, specifically, the use of the Just Culture DST were identified as an opportunity for improvement. The VHA National Center for Patient Safety developed the DST as an aid for leaders to effectively address errors in line with just culture principles, balancing individual and system accountability.27 The DST specifically addresses human error as well as risky and reckless behavior, and it clarifies the delineation between individual and organizational accountability (Table).3
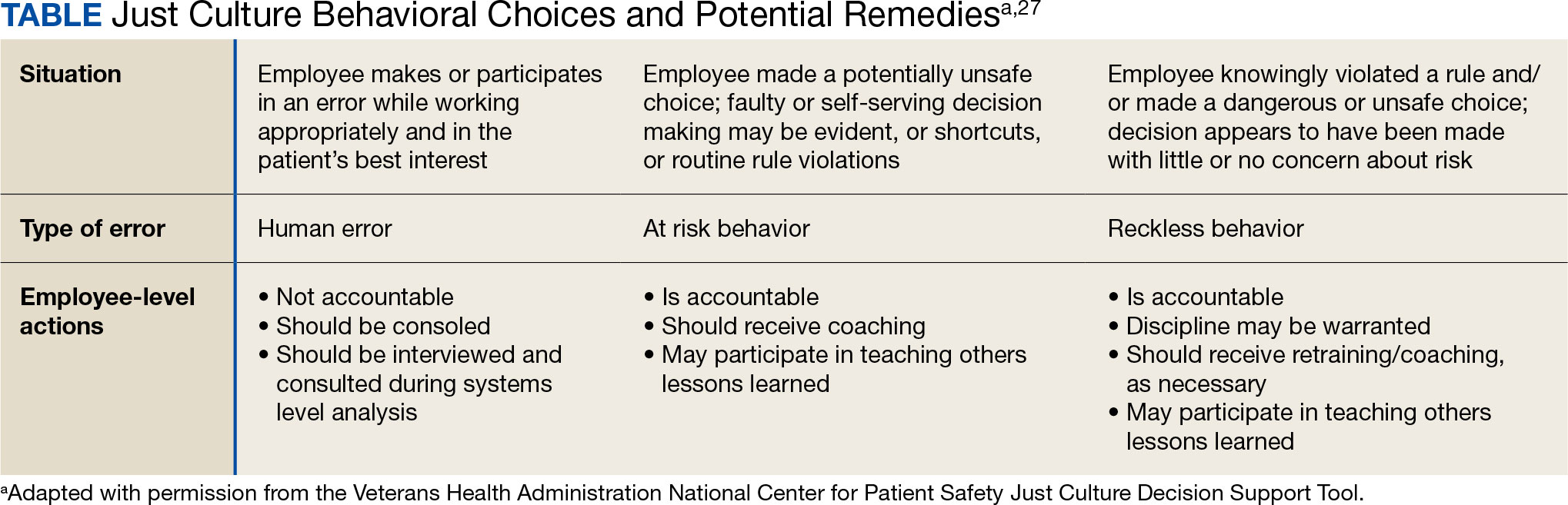
Scenario-based interactive training and simulations may prove especially useful for middle managers and frontline supervisors who are closest to errors. Clear and repeatable procedures for determining courses of action for accountability in response are needed, and support for their application must be coordinated across multiple departments (eg, patient safety and human resources) to ensure consistency and fairness. Coaching and consultation are also viewed as beneficial in supporting applications. Coaching is provided to senior leaders across most facilities, but the availability of specific, role-based coaching and training is more limited for middle managers and frontline supervisors who may benefit most from hands-on support.
Lastly, sponsorship from leaders was viewed as critical to success, but follow through to ensure support flows down from the executive suite to the frontline is variable across facilities and requires consistent effort over time. This is especially challenging given the frequent turnover in leadership roles evident in the VHA and other health care systems.
Limitations
This study employed qualitative methods and sampled a relatively small subset of experienced leaders with specific roles in implementing HRO in the VHA. Thus, it should not be considered representative of the perspectives of all leaders within the VHA or other health care systems. Future studies should assess facilitators and barriers beyond the facility level, including a focus incorporating both the VISN and VHA. More broadly, qualitative methods such as those employed in this study offer great depth and nuance but have limited ability to identify system-wide trends and differences. As such, it may be beneficial to specifically look at sites that are high- or low-performing on measures of patient safety culture to identify differences that may inform implementation strategies based on organizational maturity and readiness for change.
Conclusions
Successful implementation of these recommendations will require ongoing commitment, collaboration, and a sustained effort from all stakeholders involved at multiple levels of the health care system. Monitoring and evaluating progress should be conducted regularly to ensure that recommendations lead to improvements in implementing just culture principles. This quality improvement study adds to the knowledge base on factors that impact the just culture and broader efforts to realize HRO principles and practices in health care systems. The approach of this study may serve as a model for identifying opportunities to improve HRO implementation within the VHA and other settings, especially when paired with ongoing quantitative evaluation of organizational safety culture, just culture behaviors, and patient outcomes.
- Aljabari S, Kadhim Z. Common barriers to reporting medical errors. ScientificWorldJournal. 2021;2021:6494889. doi:10.1155/2021/6494889
- Arnal-Velasco D, Heras-Hernando V. Learning from errors and resilience. Curr Opin Anaesthesiol. 2023;36(3):376-381. doi:10.1097/ACO.0000000000001257
- Murray JS, Clifford J, Larson S, Lee JK, Sculli GL. Implementing just culture to improve patient safety. Mil Med. doi:10.1093/milmed/usac115
- Murray JS, Kelly S, Hanover C. Promoting psychological safety in healthcare organizations. Mil Med. 2022;187(7-8):808-810. doi:10.1093/milmed/usac041
- van Baarle E, Hartman L, Rooijakkers S, et al. Fostering a just culture in healthcare organizations: experiences in practice. BMC Health Serv Res. 2022;22(1):1035. doi:10.1186/s12913-022-08418-z
- Weenink JW, Wallenburg I, Hartman L, et al. Role of the regulator in enabling a just culture: a qualitative study in mental health and hospital care. BMJ Open. 2022;12(7):e061321. doi:10.1136/bmjopen-2022-061321
- White RM, Delacroix R. Second victim phenomenon: is ‘just culture’ a reality? An integrative review. Appl Nurs Res. 2020;56:151319. doi:10.1016/j.apnr.2020.151319
- Cribb A, O’Hara JK, Waring J. Improving responses to safety incidents: we need to talk about justice. BMJ Qual Saf. 2022;31(4):327-330. doi:10.1136/bmjqs-2021-014333
- Rocco C, Rodríguez AM, Noya B. Elimination of punitive outcomes and criminalization of medical errors. Curr Opin Anaesthesiol. 2022;35(6):728-732. doi:10.1097/ACO.0000000000001197
- Dekker S, Rafferty J, Oates A. Restorative Just Culture in Practice: Implementation and Evaluation. Routledge; 2022.
- Brattebø G, Flaatten HK. Errors in medicine: punishment versus learning medical adverse events revisited - expanding the frame. Curr Opin Anaesthesiol. 2023;36(2):240-245. doi:10.1097/ACO.0000000000001235
- Shabel W, Dennis JL. Missouri’s just culture collaborative. J Healthc Risk Manag. 2012;32(2):38-43. doi:10.1002/jhrm.21093
- Sculli GL, Pendley-Louis R, Neily J, et al. A high-reliability organization framework for health care: a multiyear implementation strategy and associated outcomes. J Patient Saf. 2022;18(1):64-70. doi:10.1097/PTS.0000000000000788
- Martin G, Chew S, McCarthy I, Dawson J, Dixon-Woods M. Encouraging openness in health care: policy and practice implications of a mixed-methods study in the English National Health Service. J Health Serv Res Policy. 2023;28(1):14-24. doi:10.1177/13558196221109053
- Siewert B, Brook OR, Swedeen S, Eisenberg RL, Hochman M. Overcoming human barriers to safety event reporting in radiology. Radiographics. 2019;39(1):251-263. doi:10.1148/rg.2019180135
- Barkell NP, Snyder SS. Just culture in healthcare: an integrative review. Nurs Forum. 2021;56(1):103-111. doi:10.1111/nuf.12525
- Murray JS, Lee J, Larson S, Range A, Scott D, Clifford J. Requirements for implementing a ‘just culture’ within healthcare organisations: an integrative review. BMJ Open Qual. 2023;12(2)e002237. doi:10.1136/bmjoq-2022-002237
- Mohr DC, Chen C, Sullivan J, Gunnar W, Damschroder L. Development and validation of the Veterans Health Administration patient safety culture survey. J Patient Saf. 2022;18(6):539-545. doi:10.1097/PTS.0000000000001027
- Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. SAGE Publications, Inc.; 2014.
- Patton MQ. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. 4th ed. SAGE Publications, Inc.; 2015.
- Maxwell JA. Qualitative Research Design: An Interactive Approach. 3rd ed. SAGE Publications, Inc.; 2013.
- Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025-2047. doi:10.1007/s11135-011-9640-9
- Braun V, Clarke V. Thematic Analysis: A Practical Guide. SAGE Publications, Inc; 2021.
- Cox GR, Starr LM. VHA’s movement for change: implementing high-reliability principles and practices. J Healthc Manag. 2023;68(3):151-157. doi:10.1097/JDM-D-23-00056
- Dietl JE, Derksen C, Keller FM, Lippke S. Interdisciplinary and interprofessional communication intervention: how psychological safety fosters communication and increases patient safety. Front Psychol. 2023;14:1164288. doi:10.3389/fpsyg.2023.1164288
- Eng DM, Schweikart SJ. Why accountability sharing in health care organizational cultures means patients are probably safer. AMA J Ethics. 2020;22(9):E779-E783. doi:10.1001/amajethics.2020.779
- Veterans Health Administration National Center for Patient Safety. Just Culture Decision Support Tool. Revised May 2021. Accessed August 5, 2024.https://www.patientsafety.va.gov/docs/Just-Culture-Decision-Support-Tool-2022.pdf
Medical errors are a persistent problem and leading cause of preventable death in the United States. There is considerable momentum behind the idea that implementation of a just culture is foundational to detecting and learning from errors in pursuit of zero patient harm.1-6 Just culture is a framework that fosters an environment of trust within health care organizations, aiming to achieve fair outcomes for those involved in incidents or near misses. It emphasizes openness, accountability, and learning, prioritizing the repair of harm and systemic improvement over assigning blame.7
A just culture mindset reflects a significant shift in thinking that moves from the tendency to blame and punish others toward a focus on organizational learning and continued process improvement.8,9 This systemic shift in fundamental thinking transforms how leaders approach staff errors and how they are addressed.10 In essence, just culture reflects an ethos centered on openness, a deep appreciation of human fallibility, and shared accountability at both the individual and organizational levels.
Organizational learning and innovation are stifled in the absence of a just culture, and there is a tendency for employees to avoid disclosing their own errors as well as those of their colleagues.11 The transformation to a just culture is often slowed or disrupted by personal, systemic, and cultural barriers.12 It is imperative that all executive, service line, and frontline managers recognize and execute their distinct responsibilities while adjudicating the appropriate course of action in the aftermath of adverse events or near misses. This requires a nuanced understanding of the factors that contribute to errors at the individual and organizational levels to ensure an appropriate response.
The Veterans Health Administration (VHA) is orchestrating an enterprise transformation to develop into a high reliability organization (HRO). This began with a single-site test in 2016, which demonstrated successful results in patient safety culture, patient safety event reporting, and patient safety outcomes.13 In 2019, the VHA formally launched its enterprise-wide HRO journey in 18 hospital facilities, followed by successive waves of 67 and 54 facilities in 2021 and 2022, respectively. The VHA journey to transform into an HRO aligns with 3 pillars, 5 principles, and 7 values. The VHA has emphasized the importance of just culture as a foundational element of the HRO framework, specifically under the pillar of leadership. To promote leadership engagement, the VHA has employed an array of approaches that include education, leader coaching, and change management strategies. Given the diversity among VHA facilities, each with local cultures and histories, some sites have more readily implemented a just culture than others.14 A deeper exploration into potential obstacles, particularly concerning leadership engagement, could be instrumental for formulating strategies that further establish a just culture across the VHA.15
There is a paucity of empirical research regarding factors that facilitate and/or impede the implementation of a just culture in health care settings.16,17 Likert scale surveys, such as the Patient Safety Culture Module for the VHA All Employee Survey and its predecessor, the Patient Safety Culture Survey, have been used to assess culture and climate.18 However, qualitative evaluations directly assessing the lived experiences of those trying to implement a just culture provide additional depth and context that can help identify specific factors that support or impede becoming an HRO. The purpose of this study was to increase understanding of factors that influence the establishment and sustainment of a just culture and to identify specific methods for improving the implementation of just culture principles and practices aligned with HRO.
METHODS
This qualitative study explored facilitators and barriers to establishing and sustaining a just culture as experienced across a subset of VHA facilities by HRO leads or staff assigned with the primary responsibilities of supporting facility-level HRO transformation. HRO leads are assigned responsibility for supporting executive leadership in planning, coordinating, implementing, and monitoring activities to ensure effective high reliability efforts, including focused efforts to establish a robust patient safety program, a culture of safety, and a culture of continuous process improvement.
Virtual focus group discussions held via Microsoft Teams generated in-depth, diverse perspectives from participants across 16 VHA facilities. Qualitative research and evaluation methods provide an enhanced depth of understanding and allow the emergence of detailed data.19 A qualitative grounded theory approach elicits complex, multifaceted phenomena that cannot be appreciated solely by numeric data.20 Grounded theory was selected to limit preconceived notions and provide a more systematic analysis, including open, axial, and thematic coding. Such methods afford opportunities to adapt to unplanned follow-up questions and thus provide a flexible approach to generate new ideas and concepts.21 Additionally, qualitative methods help overcome the tendencies of respondents to agree rather than disagree when presented with Likert-style scales, which tend to skew responses toward the positive.22
Participants must have been assigned as an HRO lead for ≥ 6 months at the same facility. Potential participants were identified through purposive sampling, considering their leadership roles in HRO and experience with just culture implementation, the size and complexity of their facility, and geographic distribution. Invitations explaining the study and encouraging voluntary participation to participate were emailed. Of 37 HRO leads invited to participate in the study, 16 agreed to participate and attended 1 of 3 hour-long focus group sessions. One session was rescheduled due to limited attendance. Participants represented a mix of VHA sites in terms of geography, facility size, and complexity.
Focus Group Procedures
Demographic data were collected prior to sessions via an online form to better understand the participant population, including facility complexity level, length of time in HRO lead role, clinical background, and facility level just culture training. Each session was led by an experienced focus group facilitator (CV) who was not directly involved with the overall HRO implementation to establish a neutral perspective. Each session was attended by 4 to 7 participants and 2 observers who took notes. The sessions were recorded and included automated transcriptions, which were edited for accuracy.
Focus group sessions began with a brief introduction and an opportunity for participants to ask questions. Participants were then asked a series of open-ended questions to elicit responses regardingfacilitators, barriers, and leadership support needed for implementing just culture. The questions were part of a facilitator guide that included an introductory script and discussion prompts to ensure consistency across focus groups.
Facilitators were defined as factors that increase the likelihood of establishing or sustaining a just culture. Barriers were defined as factors that decrease or inhibit the likelihood of establishing or sustaining just culture. The focus group facilitator encouraged all participants to share their views and provided clarification if needed, as well as prompts and examples where appropriate, but primarily sought to elicit responses to the questions.
Institutional review board review and approval were not required for this quality improvement initiative. The project adhered to ethical standards of research, including asking participants for verbal consent and preserving their confidentiality. Participation was voluntary, and prior to the focus group sessions, participants were provided information explaining the study’s purpose, procedures, and their rights. Participant identities were kept confidential, and all data were anonymized during the analysis phase. Pseudonyms or identifiers were used during data transcription to protect participant identity. All data, including recordings and transcriptions, were stored on password-protected devices accessible only to the research team. Any identifiable information was removed during data analysis to ensure confidentiality.
Analysis
Focus group recordings were transcribed verbatim, capturing all verbal interactions and nonverbal cues that may contribute to understanding the participants' perspectives. Thematic analysis was used to analyze the qualitative data from the focus group discussions.23 The transcribed data were organized, coded, and analyzed using ATLAS.ti 23 qualitative data software to identify key themes and patterns.
Results
The themes identified include the 5 facilitators, barriers, and recommendations most frequently mentioned by HRO leads across focus group sessions. The nature of each theme is described, along with commonly mentioned examples and direct quotes from participants that illustrate our understanding of their perspectives.
Facilitators
Training and coaching (26 responses). The availability of training around the Just Culture Decision Support Tool (DST) was cited as a practical aid in guiding leaders through complex just culture decisions to ensure consistency and fairness. Additionally, an executive leadership team that served as champions for just culture principles played a vital role in promoting and sustaining the approach: “Training them on the roll-out of the decision support tool with supervisors at all levels, and education for just culture and making it part of our safety forum has helped for the last 4 months.” “Having some regular training and share-out cadences embedded within the schedule as well as dynamic directors and well-trained executive leadership team (ELT) for support has been a facilitator.”
Increased transparency (16 responses). Participants consistently highlighted the importance of leadership transparency as a key facilitator for implementing just culture. Open and honest communication from top-level executives fostered an environment of trust and accountability. Approachable and physically present leadership was seen as essential for creating a culture where employees felt comfortable reporting errors and concerns without fear of retaliation: “They’re surprisingly honest with themselves about what we can do, what we cannot do, and they set the expectations exactly at that.”
Approachable leadership (15 responses). Participants frequently mentioned the importance of having dynamic leadership spearheading the implementation of just culture and leading by example. Having a leadership team that accepts accountability and reinforces consistency in the manner that near misses or mistakes are addressed is paramount to promoting the principles of just culture and increasing psychological safety: “We do have very approachable leadership, which I know is hard if you’re trying to implement that nationwide, it’s hard to implement approachability. But I do think that people raise their concerns, and they’ll stop them in the hallway and ask them questions. So, in terms of comfort level with the executive leadership, I do think that’s high, which would promote psychological safety.”
Feedback loops and follow through (13 responses). Participants emphasized the importance of taking concrete actions to address concerns and improve processes. Regular check-ins with supervisors to discuss matters related to just culture provided a structured opportunity for addressing issues and reinforcing the importance of the approach: “One thing that we’ve really focused on is not only identifying mistakes, but [taking] ownership. We continue to track it until … it’s completed and then a process of how to communicate that back and really using closed loop communication with the staff and letting them know.”
Forums and town halls (10 responses). These platforms created feedback loops that were seen as invaluable tools for sharing near misses, celebrating successes, and promoting open dialogue. Forums and town halls cultivated a culture of continuous improvement and trust: “We’ll celebrate catches, a safety story is inside that catch. So, if we celebrate the change, people feel safer to speak up.” “Truthfully, we’ve had a great relationship since establishing our safety forums and just value open lines of communication.”
Barriers
Inadequate training (30 responses). Insufficient engagement during training—limited bandwidth and availability to attend and actively participate in training—was perceived as detrimental to creating awareness and buy-in from staff, supervisors, and leadership, thereby hindering successful integration of just culture principles. Participants also identified too many conflicting priorities from VHA leadership, which contributes to training and information fatigue among staff and supervisors. “Our biggest barrier is just so many different competing priorities going on. We have so much that we’re asking people to do.” “One hundred percent training is feeling more like a ticked box than actually yielding results, I have a very hard time getting staff engaged.”
Inconsistency between executive leaders and middle managers (28 responses). A lack of consistency in the commitment to and enactment of just culture principles among leaders poses a challenge. Participants gave several examples of inconsistencies in messaging and reinforcement of just culture principles, leading to confusion among staff and hindering adoption. Likewise, the absence of standardized procedures for implementing just culture created variability: “The director coming in and trying to change things, it put a lot of resistance, we struggle with getting the other ELT members on board … some of the messages that come out at times can feel more punitive.”
Middle management resistance (22 responses). In some instances, participants reported middle managers exhibiting attitudes and behaviors that undermined the application of just culture principles and effectiveness. Such attitudes and behaviors were attributed to a lack of adequate training, coaching, and awareness. Other perceived contributions included fear of failure and a desire to distance oneself from staff who have made mistakes: “As soon as someone makes an error, they go straight to suspend them, and that’s the disconnect right there.” “There’s almost a level of working in the opposite direction in some of the mid-management.”
Cultural misalignment (18 responses). The existing culture of distancing oneself from mistakes presented a significant barrier to the adoption of just culture because it clashed with the principles of open reporting and accountability. Staff underreported errors or framed them in a way that minimized personal responsibility, thereby making it more essential to put in the necessary and difficult work to learn from mistakes: “One, you’re going to get in trouble. There’s going to be more work added to you or something of that nature."
Lack of accountability for opposition(17 responses). Participants noted a clear lack of accountability for those who opposed or showed resistance to just culture, which allowed resistance to persist without consequences. In many instances, leaders were described as having overlooked repeated instances of unjust attitudes and behaviors (eg, inappropriate blame or punishment), which allowed those practices to continue. “Executive leadership is standing on the hill and saying we’re a just culture and we do everything correctly, and staff has the expectation that they’re going to be treated with just culture and then the middle management is setting that on fire, then we show them that that’s not just culture, and they continue to have those poor behaviors, but there’s a lack of accountability.”
Limited bandwidth and lack of coordination (14 responses). HRO leads often faced role-specific constraints in having adequate time and authority to coordinate efforts to implement or sustain just culture. This includes challenges with coordination across organizational levels (eg, between the hospital and regional Veterans Integrated Service Network [VISN] management levels) and across departments within the hospital (eg, between human resources and service lines or units). “Our VISN human resources is completely detached. They’ll not cooperate with these efforts, which is hard.” “There’s not enough bandwidth to actually support, I’m just 1 person.” “[There’s] all these mandated trainings of 8 hours when we’re already fatigued, short-staffed, taking 3 other HRO classes.”
Recommendations
Training improvements (24 responses). HRO leads recommended that comprehensive training programs be developed and implemented for staff, supervisors, and leadership to increase awareness and understanding of just culture principles. These training initiatives should focus on fostering a shared understanding of the core tenets of just culture, the importance of error reporting, and the processes involved in fair and consistent decision making (eg, training simulations on use of the Just Culture DST). “We’ve really never had any formal training on the decision support tool. I hope that what’s coming out for next year. We’ll have some more formal training for the tool because I think it would be great to really have our leadership and our supervisors and our managers use that tool.” “We can give a more directed and intentional training to leadership on the 4 foundational practices and what it means to implement those and what it means to utilize that behavioral component of HRO.”
Clear and consistent procedures toincrease accountability (22 responses). To promote a culture of accountability and consistency in the application of just culture principles, organizations should establish clear mechanisms for reporting, investigating, and addressing incidents. Standardized procedures and DSTs can aid in ensuring that responses to errors are equitable and align with just culture principles: “I recommend accountability; if it’s clearly evidenced that you’re not toeing the just culture line, then we need to be able to do something about it and not just finger wag.” “[We need to have] a templated way to approach just culture implementation. The decision support tool is great, I absolutely love having the resources and being able to find a lot of clinical examples and discussion tools like that. But when it comes down to it, not having that kind of official thing to fall back on it can be a little bit rough.”
Additional coaching and consultationsupport (15 responses). To support supervisors in effectively implementing just culture within their teams, participants recommended that organizations provide ongoing coaching and mentorship opportunities. Additionally, third-party consultants with expertise in just culture were described as offering valuable guidance, particularly in cases where internal staff resources or HRO lead bandwidth may be limited. “There are so many consulting agencies with HRO that have been contracted to do different projects, but maybe that can help with an educational program.” “I want to see my executive leadership coach the supervisors up right and then allow them to do one-on-ones and facilitate and empower the frontline staff, and it’s just a good way of transparency and communication.”
Improved leadership sponsorship (15 responses). Participants noted that leadership buy-in is crucial for the successful implementation of just culture. Facilities should actively engage and educate leadership teams on the benefits of just culture and how it aligns with broader patient safety and organizational goals. Leaders should be visible and active champions of its principles, supporting change in their daily engagements with staff. “ELT support is absolutely necessary. Why? Because they will make it important to those in their service lines. They will make it important to those supervisors and managers. If it’s not important to that ELT member, then it’s not going to be important to that manager or that supervisor.”
Improved collaboration with patient safety and human resources (6 responses). Collaborative efforts with patient safety and human resources departments were seen as instrumental in supporting just culture, emphasizing its importance, and effectively addressing issues. Coordinating with these departments specifically contributes to consistent reinforcement and expands the bandwidth of HRO leads. These departments play integral roles in supporting just culture through effective policies, procedures, and communication. “I think it would be really helpful to have common language between what human resources teaches and what is in our decision support tool.”
DISCUSSION
This study sought to collect and synthesize the experiences of leaders across a large, integrated health care system in establishing and sustaining a just culture as part of an enterprise journey to become an HRO.24 The VHA has provided enterprise-wide support (eg, training, leader coaching, and communications) for the implementation of HRO principles and practices with the goal of creating a culture of safety, which includes just culture elements. This support includes enterprise program offices, VISNs, and hospital facilities, though notably, there is variability in how HRO is implemented at the local level. The facilitators, barriers, and recommendations presented in this article are representative of the designated HRO leads at VHA hospital facilities who have direct experience with implementing and sustaining just culture. The themes presented offer specific opportunities for intervention and actionable strategies to enhance just culture initiatives, foster psychological safety and accountability, and ultimately improve the quality of care and patient outcomes.3,25
Frequently identified facilitators such as providing training and coaching, having leaders who are available and approachable, demonstrating follow-through to address identified issues, and creating venues where errors and successes can be openly discussed.26 These facilitators are aligned with enterprise HRO support strategies orchestrated by the VHA at the enterprise VISN and facility levels to support a culture of safety, continuous process improvement, and leadership commitment.
Frequently identified barriers included inadequate training, inconsistent application of just culture by middle managers vs senior leaders, a lack of accountability or corrective action when unjust corrective actions took place, time and resource constraints, and inadequate coordination across departments (eg, operational departments and human resources) and organizational levels. These factors were identified through focus groups with a limited set of HRO leads. They may reflect challenges to changing culture that may be deeply engrained in individual histories, organizational norms, and systemic practices. Improving upon these just culture initiatives requires multifaceted approaches and working through resistance to change.
VHA HRO leads identified several actionable recommendations that may be used in pursuit of a just culture. First, improvements in training involving how to apply just culture principles and, specifically, the use of the Just Culture DST were identified as an opportunity for improvement. The VHA National Center for Patient Safety developed the DST as an aid for leaders to effectively address errors in line with just culture principles, balancing individual and system accountability.27 The DST specifically addresses human error as well as risky and reckless behavior, and it clarifies the delineation between individual and organizational accountability (Table).3
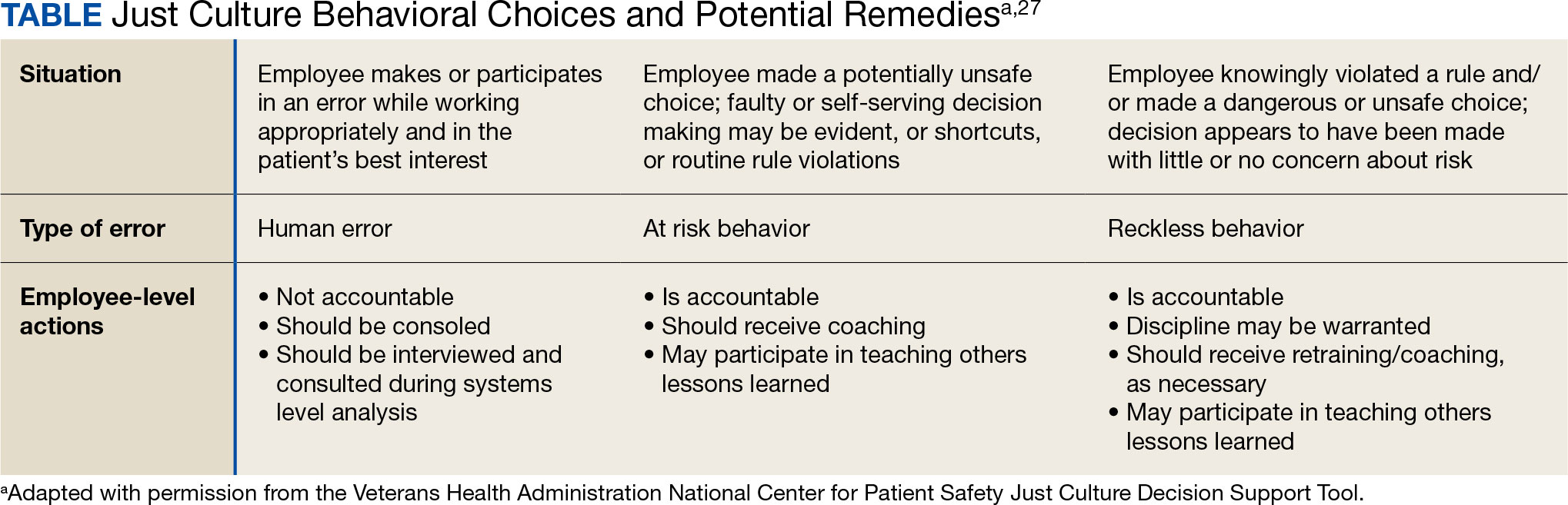
Scenario-based interactive training and simulations may prove especially useful for middle managers and frontline supervisors who are closest to errors. Clear and repeatable procedures for determining courses of action for accountability in response are needed, and support for their application must be coordinated across multiple departments (eg, patient safety and human resources) to ensure consistency and fairness. Coaching and consultation are also viewed as beneficial in supporting applications. Coaching is provided to senior leaders across most facilities, but the availability of specific, role-based coaching and training is more limited for middle managers and frontline supervisors who may benefit most from hands-on support.
Lastly, sponsorship from leaders was viewed as critical to success, but follow through to ensure support flows down from the executive suite to the frontline is variable across facilities and requires consistent effort over time. This is especially challenging given the frequent turnover in leadership roles evident in the VHA and other health care systems.
Limitations
This study employed qualitative methods and sampled a relatively small subset of experienced leaders with specific roles in implementing HRO in the VHA. Thus, it should not be considered representative of the perspectives of all leaders within the VHA or other health care systems. Future studies should assess facilitators and barriers beyond the facility level, including a focus incorporating both the VISN and VHA. More broadly, qualitative methods such as those employed in this study offer great depth and nuance but have limited ability to identify system-wide trends and differences. As such, it may be beneficial to specifically look at sites that are high- or low-performing on measures of patient safety culture to identify differences that may inform implementation strategies based on organizational maturity and readiness for change.
Conclusions
Successful implementation of these recommendations will require ongoing commitment, collaboration, and a sustained effort from all stakeholders involved at multiple levels of the health care system. Monitoring and evaluating progress should be conducted regularly to ensure that recommendations lead to improvements in implementing just culture principles. This quality improvement study adds to the knowledge base on factors that impact the just culture and broader efforts to realize HRO principles and practices in health care systems. The approach of this study may serve as a model for identifying opportunities to improve HRO implementation within the VHA and other settings, especially when paired with ongoing quantitative evaluation of organizational safety culture, just culture behaviors, and patient outcomes.
Medical errors are a persistent problem and leading cause of preventable death in the United States. There is considerable momentum behind the idea that implementation of a just culture is foundational to detecting and learning from errors in pursuit of zero patient harm.1-6 Just culture is a framework that fosters an environment of trust within health care organizations, aiming to achieve fair outcomes for those involved in incidents or near misses. It emphasizes openness, accountability, and learning, prioritizing the repair of harm and systemic improvement over assigning blame.7
A just culture mindset reflects a significant shift in thinking that moves from the tendency to blame and punish others toward a focus on organizational learning and continued process improvement.8,9 This systemic shift in fundamental thinking transforms how leaders approach staff errors and how they are addressed.10 In essence, just culture reflects an ethos centered on openness, a deep appreciation of human fallibility, and shared accountability at both the individual and organizational levels.
Organizational learning and innovation are stifled in the absence of a just culture, and there is a tendency for employees to avoid disclosing their own errors as well as those of their colleagues.11 The transformation to a just culture is often slowed or disrupted by personal, systemic, and cultural barriers.12 It is imperative that all executive, service line, and frontline managers recognize and execute their distinct responsibilities while adjudicating the appropriate course of action in the aftermath of adverse events or near misses. This requires a nuanced understanding of the factors that contribute to errors at the individual and organizational levels to ensure an appropriate response.
The Veterans Health Administration (VHA) is orchestrating an enterprise transformation to develop into a high reliability organization (HRO). This began with a single-site test in 2016, which demonstrated successful results in patient safety culture, patient safety event reporting, and patient safety outcomes.13 In 2019, the VHA formally launched its enterprise-wide HRO journey in 18 hospital facilities, followed by successive waves of 67 and 54 facilities in 2021 and 2022, respectively. The VHA journey to transform into an HRO aligns with 3 pillars, 5 principles, and 7 values. The VHA has emphasized the importance of just culture as a foundational element of the HRO framework, specifically under the pillar of leadership. To promote leadership engagement, the VHA has employed an array of approaches that include education, leader coaching, and change management strategies. Given the diversity among VHA facilities, each with local cultures and histories, some sites have more readily implemented a just culture than others.14 A deeper exploration into potential obstacles, particularly concerning leadership engagement, could be instrumental for formulating strategies that further establish a just culture across the VHA.15
There is a paucity of empirical research regarding factors that facilitate and/or impede the implementation of a just culture in health care settings.16,17 Likert scale surveys, such as the Patient Safety Culture Module for the VHA All Employee Survey and its predecessor, the Patient Safety Culture Survey, have been used to assess culture and climate.18 However, qualitative evaluations directly assessing the lived experiences of those trying to implement a just culture provide additional depth and context that can help identify specific factors that support or impede becoming an HRO. The purpose of this study was to increase understanding of factors that influence the establishment and sustainment of a just culture and to identify specific methods for improving the implementation of just culture principles and practices aligned with HRO.
METHODS
This qualitative study explored facilitators and barriers to establishing and sustaining a just culture as experienced across a subset of VHA facilities by HRO leads or staff assigned with the primary responsibilities of supporting facility-level HRO transformation. HRO leads are assigned responsibility for supporting executive leadership in planning, coordinating, implementing, and monitoring activities to ensure effective high reliability efforts, including focused efforts to establish a robust patient safety program, a culture of safety, and a culture of continuous process improvement.
Virtual focus group discussions held via Microsoft Teams generated in-depth, diverse perspectives from participants across 16 VHA facilities. Qualitative research and evaluation methods provide an enhanced depth of understanding and allow the emergence of detailed data.19 A qualitative grounded theory approach elicits complex, multifaceted phenomena that cannot be appreciated solely by numeric data.20 Grounded theory was selected to limit preconceived notions and provide a more systematic analysis, including open, axial, and thematic coding. Such methods afford opportunities to adapt to unplanned follow-up questions and thus provide a flexible approach to generate new ideas and concepts.21 Additionally, qualitative methods help overcome the tendencies of respondents to agree rather than disagree when presented with Likert-style scales, which tend to skew responses toward the positive.22
Participants must have been assigned as an HRO lead for ≥ 6 months at the same facility. Potential participants were identified through purposive sampling, considering their leadership roles in HRO and experience with just culture implementation, the size and complexity of their facility, and geographic distribution. Invitations explaining the study and encouraging voluntary participation to participate were emailed. Of 37 HRO leads invited to participate in the study, 16 agreed to participate and attended 1 of 3 hour-long focus group sessions. One session was rescheduled due to limited attendance. Participants represented a mix of VHA sites in terms of geography, facility size, and complexity.
Focus Group Procedures
Demographic data were collected prior to sessions via an online form to better understand the participant population, including facility complexity level, length of time in HRO lead role, clinical background, and facility level just culture training. Each session was led by an experienced focus group facilitator (CV) who was not directly involved with the overall HRO implementation to establish a neutral perspective. Each session was attended by 4 to 7 participants and 2 observers who took notes. The sessions were recorded and included automated transcriptions, which were edited for accuracy.
Focus group sessions began with a brief introduction and an opportunity for participants to ask questions. Participants were then asked a series of open-ended questions to elicit responses regardingfacilitators, barriers, and leadership support needed for implementing just culture. The questions were part of a facilitator guide that included an introductory script and discussion prompts to ensure consistency across focus groups.
Facilitators were defined as factors that increase the likelihood of establishing or sustaining a just culture. Barriers were defined as factors that decrease or inhibit the likelihood of establishing or sustaining just culture. The focus group facilitator encouraged all participants to share their views and provided clarification if needed, as well as prompts and examples where appropriate, but primarily sought to elicit responses to the questions.
Institutional review board review and approval were not required for this quality improvement initiative. The project adhered to ethical standards of research, including asking participants for verbal consent and preserving their confidentiality. Participation was voluntary, and prior to the focus group sessions, participants were provided information explaining the study’s purpose, procedures, and their rights. Participant identities were kept confidential, and all data were anonymized during the analysis phase. Pseudonyms or identifiers were used during data transcription to protect participant identity. All data, including recordings and transcriptions, were stored on password-protected devices accessible only to the research team. Any identifiable information was removed during data analysis to ensure confidentiality.
Analysis
Focus group recordings were transcribed verbatim, capturing all verbal interactions and nonverbal cues that may contribute to understanding the participants' perspectives. Thematic analysis was used to analyze the qualitative data from the focus group discussions.23 The transcribed data were organized, coded, and analyzed using ATLAS.ti 23 qualitative data software to identify key themes and patterns.
Results
The themes identified include the 5 facilitators, barriers, and recommendations most frequently mentioned by HRO leads across focus group sessions. The nature of each theme is described, along with commonly mentioned examples and direct quotes from participants that illustrate our understanding of their perspectives.
Facilitators
Training and coaching (26 responses). The availability of training around the Just Culture Decision Support Tool (DST) was cited as a practical aid in guiding leaders through complex just culture decisions to ensure consistency and fairness. Additionally, an executive leadership team that served as champions for just culture principles played a vital role in promoting and sustaining the approach: “Training them on the roll-out of the decision support tool with supervisors at all levels, and education for just culture and making it part of our safety forum has helped for the last 4 months.” “Having some regular training and share-out cadences embedded within the schedule as well as dynamic directors and well-trained executive leadership team (ELT) for support has been a facilitator.”
Increased transparency (16 responses). Participants consistently highlighted the importance of leadership transparency as a key facilitator for implementing just culture. Open and honest communication from top-level executives fostered an environment of trust and accountability. Approachable and physically present leadership was seen as essential for creating a culture where employees felt comfortable reporting errors and concerns without fear of retaliation: “They’re surprisingly honest with themselves about what we can do, what we cannot do, and they set the expectations exactly at that.”
Approachable leadership (15 responses). Participants frequently mentioned the importance of having dynamic leadership spearheading the implementation of just culture and leading by example. Having a leadership team that accepts accountability and reinforces consistency in the manner that near misses or mistakes are addressed is paramount to promoting the principles of just culture and increasing psychological safety: “We do have very approachable leadership, which I know is hard if you’re trying to implement that nationwide, it’s hard to implement approachability. But I do think that people raise their concerns, and they’ll stop them in the hallway and ask them questions. So, in terms of comfort level with the executive leadership, I do think that’s high, which would promote psychological safety.”
Feedback loops and follow through (13 responses). Participants emphasized the importance of taking concrete actions to address concerns and improve processes. Regular check-ins with supervisors to discuss matters related to just culture provided a structured opportunity for addressing issues and reinforcing the importance of the approach: “One thing that we’ve really focused on is not only identifying mistakes, but [taking] ownership. We continue to track it until … it’s completed and then a process of how to communicate that back and really using closed loop communication with the staff and letting them know.”
Forums and town halls (10 responses). These platforms created feedback loops that were seen as invaluable tools for sharing near misses, celebrating successes, and promoting open dialogue. Forums and town halls cultivated a culture of continuous improvement and trust: “We’ll celebrate catches, a safety story is inside that catch. So, if we celebrate the change, people feel safer to speak up.” “Truthfully, we’ve had a great relationship since establishing our safety forums and just value open lines of communication.”
Barriers
Inadequate training (30 responses). Insufficient engagement during training—limited bandwidth and availability to attend and actively participate in training—was perceived as detrimental to creating awareness and buy-in from staff, supervisors, and leadership, thereby hindering successful integration of just culture principles. Participants also identified too many conflicting priorities from VHA leadership, which contributes to training and information fatigue among staff and supervisors. “Our biggest barrier is just so many different competing priorities going on. We have so much that we’re asking people to do.” “One hundred percent training is feeling more like a ticked box than actually yielding results, I have a very hard time getting staff engaged.”
Inconsistency between executive leaders and middle managers (28 responses). A lack of consistency in the commitment to and enactment of just culture principles among leaders poses a challenge. Participants gave several examples of inconsistencies in messaging and reinforcement of just culture principles, leading to confusion among staff and hindering adoption. Likewise, the absence of standardized procedures for implementing just culture created variability: “The director coming in and trying to change things, it put a lot of resistance, we struggle with getting the other ELT members on board … some of the messages that come out at times can feel more punitive.”
Middle management resistance (22 responses). In some instances, participants reported middle managers exhibiting attitudes and behaviors that undermined the application of just culture principles and effectiveness. Such attitudes and behaviors were attributed to a lack of adequate training, coaching, and awareness. Other perceived contributions included fear of failure and a desire to distance oneself from staff who have made mistakes: “As soon as someone makes an error, they go straight to suspend them, and that’s the disconnect right there.” “There’s almost a level of working in the opposite direction in some of the mid-management.”
Cultural misalignment (18 responses). The existing culture of distancing oneself from mistakes presented a significant barrier to the adoption of just culture because it clashed with the principles of open reporting and accountability. Staff underreported errors or framed them in a way that minimized personal responsibility, thereby making it more essential to put in the necessary and difficult work to learn from mistakes: “One, you’re going to get in trouble. There’s going to be more work added to you or something of that nature."
Lack of accountability for opposition(17 responses). Participants noted a clear lack of accountability for those who opposed or showed resistance to just culture, which allowed resistance to persist without consequences. In many instances, leaders were described as having overlooked repeated instances of unjust attitudes and behaviors (eg, inappropriate blame or punishment), which allowed those practices to continue. “Executive leadership is standing on the hill and saying we’re a just culture and we do everything correctly, and staff has the expectation that they’re going to be treated with just culture and then the middle management is setting that on fire, then we show them that that’s not just culture, and they continue to have those poor behaviors, but there’s a lack of accountability.”
Limited bandwidth and lack of coordination (14 responses). HRO leads often faced role-specific constraints in having adequate time and authority to coordinate efforts to implement or sustain just culture. This includes challenges with coordination across organizational levels (eg, between the hospital and regional Veterans Integrated Service Network [VISN] management levels) and across departments within the hospital (eg, between human resources and service lines or units). “Our VISN human resources is completely detached. They’ll not cooperate with these efforts, which is hard.” “There’s not enough bandwidth to actually support, I’m just 1 person.” “[There’s] all these mandated trainings of 8 hours when we’re already fatigued, short-staffed, taking 3 other HRO classes.”
Recommendations
Training improvements (24 responses). HRO leads recommended that comprehensive training programs be developed and implemented for staff, supervisors, and leadership to increase awareness and understanding of just culture principles. These training initiatives should focus on fostering a shared understanding of the core tenets of just culture, the importance of error reporting, and the processes involved in fair and consistent decision making (eg, training simulations on use of the Just Culture DST). “We’ve really never had any formal training on the decision support tool. I hope that what’s coming out for next year. We’ll have some more formal training for the tool because I think it would be great to really have our leadership and our supervisors and our managers use that tool.” “We can give a more directed and intentional training to leadership on the 4 foundational practices and what it means to implement those and what it means to utilize that behavioral component of HRO.”
Clear and consistent procedures toincrease accountability (22 responses). To promote a culture of accountability and consistency in the application of just culture principles, organizations should establish clear mechanisms for reporting, investigating, and addressing incidents. Standardized procedures and DSTs can aid in ensuring that responses to errors are equitable and align with just culture principles: “I recommend accountability; if it’s clearly evidenced that you’re not toeing the just culture line, then we need to be able to do something about it and not just finger wag.” “[We need to have] a templated way to approach just culture implementation. The decision support tool is great, I absolutely love having the resources and being able to find a lot of clinical examples and discussion tools like that. But when it comes down to it, not having that kind of official thing to fall back on it can be a little bit rough.”
Additional coaching and consultationsupport (15 responses). To support supervisors in effectively implementing just culture within their teams, participants recommended that organizations provide ongoing coaching and mentorship opportunities. Additionally, third-party consultants with expertise in just culture were described as offering valuable guidance, particularly in cases where internal staff resources or HRO lead bandwidth may be limited. “There are so many consulting agencies with HRO that have been contracted to do different projects, but maybe that can help with an educational program.” “I want to see my executive leadership coach the supervisors up right and then allow them to do one-on-ones and facilitate and empower the frontline staff, and it’s just a good way of transparency and communication.”
Improved leadership sponsorship (15 responses). Participants noted that leadership buy-in is crucial for the successful implementation of just culture. Facilities should actively engage and educate leadership teams on the benefits of just culture and how it aligns with broader patient safety and organizational goals. Leaders should be visible and active champions of its principles, supporting change in their daily engagements with staff. “ELT support is absolutely necessary. Why? Because they will make it important to those in their service lines. They will make it important to those supervisors and managers. If it’s not important to that ELT member, then it’s not going to be important to that manager or that supervisor.”
Improved collaboration with patient safety and human resources (6 responses). Collaborative efforts with patient safety and human resources departments were seen as instrumental in supporting just culture, emphasizing its importance, and effectively addressing issues. Coordinating with these departments specifically contributes to consistent reinforcement and expands the bandwidth of HRO leads. These departments play integral roles in supporting just culture through effective policies, procedures, and communication. “I think it would be really helpful to have common language between what human resources teaches and what is in our decision support tool.”
DISCUSSION
This study sought to collect and synthesize the experiences of leaders across a large, integrated health care system in establishing and sustaining a just culture as part of an enterprise journey to become an HRO.24 The VHA has provided enterprise-wide support (eg, training, leader coaching, and communications) for the implementation of HRO principles and practices with the goal of creating a culture of safety, which includes just culture elements. This support includes enterprise program offices, VISNs, and hospital facilities, though notably, there is variability in how HRO is implemented at the local level. The facilitators, barriers, and recommendations presented in this article are representative of the designated HRO leads at VHA hospital facilities who have direct experience with implementing and sustaining just culture. The themes presented offer specific opportunities for intervention and actionable strategies to enhance just culture initiatives, foster psychological safety and accountability, and ultimately improve the quality of care and patient outcomes.3,25
Frequently identified facilitators such as providing training and coaching, having leaders who are available and approachable, demonstrating follow-through to address identified issues, and creating venues where errors and successes can be openly discussed.26 These facilitators are aligned with enterprise HRO support strategies orchestrated by the VHA at the enterprise VISN and facility levels to support a culture of safety, continuous process improvement, and leadership commitment.
Frequently identified barriers included inadequate training, inconsistent application of just culture by middle managers vs senior leaders, a lack of accountability or corrective action when unjust corrective actions took place, time and resource constraints, and inadequate coordination across departments (eg, operational departments and human resources) and organizational levels. These factors were identified through focus groups with a limited set of HRO leads. They may reflect challenges to changing culture that may be deeply engrained in individual histories, organizational norms, and systemic practices. Improving upon these just culture initiatives requires multifaceted approaches and working through resistance to change.
VHA HRO leads identified several actionable recommendations that may be used in pursuit of a just culture. First, improvements in training involving how to apply just culture principles and, specifically, the use of the Just Culture DST were identified as an opportunity for improvement. The VHA National Center for Patient Safety developed the DST as an aid for leaders to effectively address errors in line with just culture principles, balancing individual and system accountability.27 The DST specifically addresses human error as well as risky and reckless behavior, and it clarifies the delineation between individual and organizational accountability (Table).3
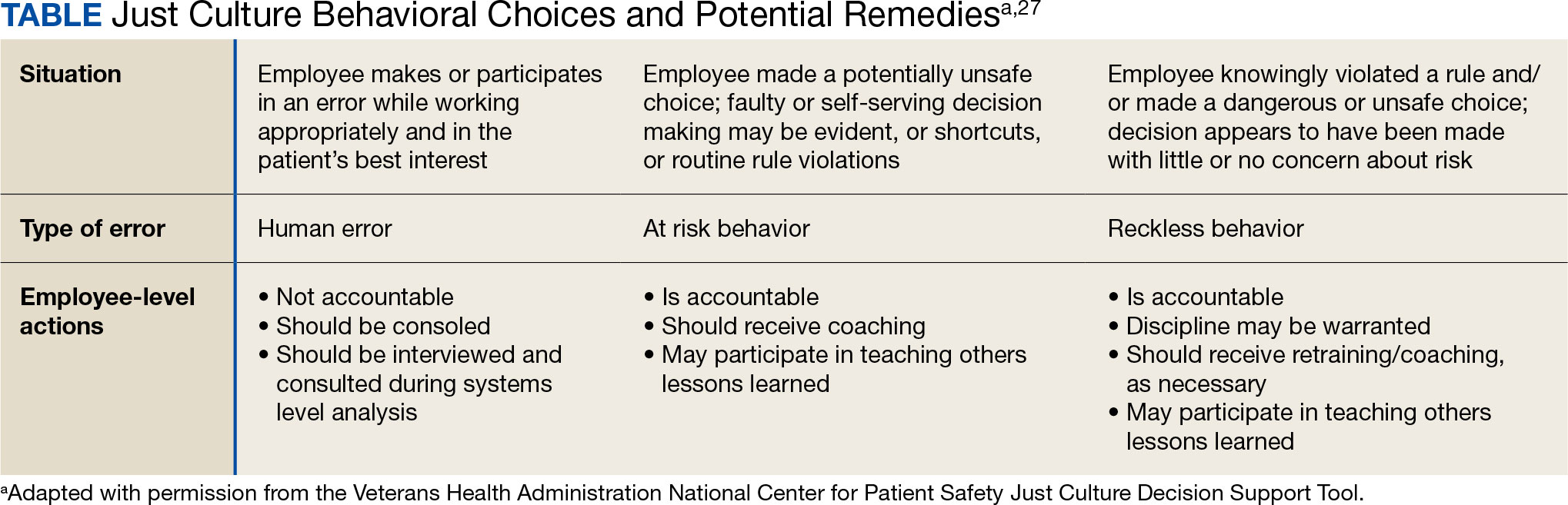
Scenario-based interactive training and simulations may prove especially useful for middle managers and frontline supervisors who are closest to errors. Clear and repeatable procedures for determining courses of action for accountability in response are needed, and support for their application must be coordinated across multiple departments (eg, patient safety and human resources) to ensure consistency and fairness. Coaching and consultation are also viewed as beneficial in supporting applications. Coaching is provided to senior leaders across most facilities, but the availability of specific, role-based coaching and training is more limited for middle managers and frontline supervisors who may benefit most from hands-on support.
Lastly, sponsorship from leaders was viewed as critical to success, but follow through to ensure support flows down from the executive suite to the frontline is variable across facilities and requires consistent effort over time. This is especially challenging given the frequent turnover in leadership roles evident in the VHA and other health care systems.
Limitations
This study employed qualitative methods and sampled a relatively small subset of experienced leaders with specific roles in implementing HRO in the VHA. Thus, it should not be considered representative of the perspectives of all leaders within the VHA or other health care systems. Future studies should assess facilitators and barriers beyond the facility level, including a focus incorporating both the VISN and VHA. More broadly, qualitative methods such as those employed in this study offer great depth and nuance but have limited ability to identify system-wide trends and differences. As such, it may be beneficial to specifically look at sites that are high- or low-performing on measures of patient safety culture to identify differences that may inform implementation strategies based on organizational maturity and readiness for change.
Conclusions
Successful implementation of these recommendations will require ongoing commitment, collaboration, and a sustained effort from all stakeholders involved at multiple levels of the health care system. Monitoring and evaluating progress should be conducted regularly to ensure that recommendations lead to improvements in implementing just culture principles. This quality improvement study adds to the knowledge base on factors that impact the just culture and broader efforts to realize HRO principles and practices in health care systems. The approach of this study may serve as a model for identifying opportunities to improve HRO implementation within the VHA and other settings, especially when paired with ongoing quantitative evaluation of organizational safety culture, just culture behaviors, and patient outcomes.
- Aljabari S, Kadhim Z. Common barriers to reporting medical errors. ScientificWorldJournal. 2021;2021:6494889. doi:10.1155/2021/6494889
- Arnal-Velasco D, Heras-Hernando V. Learning from errors and resilience. Curr Opin Anaesthesiol. 2023;36(3):376-381. doi:10.1097/ACO.0000000000001257
- Murray JS, Clifford J, Larson S, Lee JK, Sculli GL. Implementing just culture to improve patient safety. Mil Med. doi:10.1093/milmed/usac115
- Murray JS, Kelly S, Hanover C. Promoting psychological safety in healthcare organizations. Mil Med. 2022;187(7-8):808-810. doi:10.1093/milmed/usac041
- van Baarle E, Hartman L, Rooijakkers S, et al. Fostering a just culture in healthcare organizations: experiences in practice. BMC Health Serv Res. 2022;22(1):1035. doi:10.1186/s12913-022-08418-z
- Weenink JW, Wallenburg I, Hartman L, et al. Role of the regulator in enabling a just culture: a qualitative study in mental health and hospital care. BMJ Open. 2022;12(7):e061321. doi:10.1136/bmjopen-2022-061321
- White RM, Delacroix R. Second victim phenomenon: is ‘just culture’ a reality? An integrative review. Appl Nurs Res. 2020;56:151319. doi:10.1016/j.apnr.2020.151319
- Cribb A, O’Hara JK, Waring J. Improving responses to safety incidents: we need to talk about justice. BMJ Qual Saf. 2022;31(4):327-330. doi:10.1136/bmjqs-2021-014333
- Rocco C, Rodríguez AM, Noya B. Elimination of punitive outcomes and criminalization of medical errors. Curr Opin Anaesthesiol. 2022;35(6):728-732. doi:10.1097/ACO.0000000000001197
- Dekker S, Rafferty J, Oates A. Restorative Just Culture in Practice: Implementation and Evaluation. Routledge; 2022.
- Brattebø G, Flaatten HK. Errors in medicine: punishment versus learning medical adverse events revisited - expanding the frame. Curr Opin Anaesthesiol. 2023;36(2):240-245. doi:10.1097/ACO.0000000000001235
- Shabel W, Dennis JL. Missouri’s just culture collaborative. J Healthc Risk Manag. 2012;32(2):38-43. doi:10.1002/jhrm.21093
- Sculli GL, Pendley-Louis R, Neily J, et al. A high-reliability organization framework for health care: a multiyear implementation strategy and associated outcomes. J Patient Saf. 2022;18(1):64-70. doi:10.1097/PTS.0000000000000788
- Martin G, Chew S, McCarthy I, Dawson J, Dixon-Woods M. Encouraging openness in health care: policy and practice implications of a mixed-methods study in the English National Health Service. J Health Serv Res Policy. 2023;28(1):14-24. doi:10.1177/13558196221109053
- Siewert B, Brook OR, Swedeen S, Eisenberg RL, Hochman M. Overcoming human barriers to safety event reporting in radiology. Radiographics. 2019;39(1):251-263. doi:10.1148/rg.2019180135
- Barkell NP, Snyder SS. Just culture in healthcare: an integrative review. Nurs Forum. 2021;56(1):103-111. doi:10.1111/nuf.12525
- Murray JS, Lee J, Larson S, Range A, Scott D, Clifford J. Requirements for implementing a ‘just culture’ within healthcare organisations: an integrative review. BMJ Open Qual. 2023;12(2)e002237. doi:10.1136/bmjoq-2022-002237
- Mohr DC, Chen C, Sullivan J, Gunnar W, Damschroder L. Development and validation of the Veterans Health Administration patient safety culture survey. J Patient Saf. 2022;18(6):539-545. doi:10.1097/PTS.0000000000001027
- Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. SAGE Publications, Inc.; 2014.
- Patton MQ. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. 4th ed. SAGE Publications, Inc.; 2015.
- Maxwell JA. Qualitative Research Design: An Interactive Approach. 3rd ed. SAGE Publications, Inc.; 2013.
- Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025-2047. doi:10.1007/s11135-011-9640-9
- Braun V, Clarke V. Thematic Analysis: A Practical Guide. SAGE Publications, Inc; 2021.
- Cox GR, Starr LM. VHA’s movement for change: implementing high-reliability principles and practices. J Healthc Manag. 2023;68(3):151-157. doi:10.1097/JDM-D-23-00056
- Dietl JE, Derksen C, Keller FM, Lippke S. Interdisciplinary and interprofessional communication intervention: how psychological safety fosters communication and increases patient safety. Front Psychol. 2023;14:1164288. doi:10.3389/fpsyg.2023.1164288
- Eng DM, Schweikart SJ. Why accountability sharing in health care organizational cultures means patients are probably safer. AMA J Ethics. 2020;22(9):E779-E783. doi:10.1001/amajethics.2020.779
- Veterans Health Administration National Center for Patient Safety. Just Culture Decision Support Tool. Revised May 2021. Accessed August 5, 2024.https://www.patientsafety.va.gov/docs/Just-Culture-Decision-Support-Tool-2022.pdf
- Aljabari S, Kadhim Z. Common barriers to reporting medical errors. ScientificWorldJournal. 2021;2021:6494889. doi:10.1155/2021/6494889
- Arnal-Velasco D, Heras-Hernando V. Learning from errors and resilience. Curr Opin Anaesthesiol. 2023;36(3):376-381. doi:10.1097/ACO.0000000000001257
- Murray JS, Clifford J, Larson S, Lee JK, Sculli GL. Implementing just culture to improve patient safety. Mil Med. doi:10.1093/milmed/usac115
- Murray JS, Kelly S, Hanover C. Promoting psychological safety in healthcare organizations. Mil Med. 2022;187(7-8):808-810. doi:10.1093/milmed/usac041
- van Baarle E, Hartman L, Rooijakkers S, et al. Fostering a just culture in healthcare organizations: experiences in practice. BMC Health Serv Res. 2022;22(1):1035. doi:10.1186/s12913-022-08418-z
- Weenink JW, Wallenburg I, Hartman L, et al. Role of the regulator in enabling a just culture: a qualitative study in mental health and hospital care. BMJ Open. 2022;12(7):e061321. doi:10.1136/bmjopen-2022-061321
- White RM, Delacroix R. Second victim phenomenon: is ‘just culture’ a reality? An integrative review. Appl Nurs Res. 2020;56:151319. doi:10.1016/j.apnr.2020.151319
- Cribb A, O’Hara JK, Waring J. Improving responses to safety incidents: we need to talk about justice. BMJ Qual Saf. 2022;31(4):327-330. doi:10.1136/bmjqs-2021-014333
- Rocco C, Rodríguez AM, Noya B. Elimination of punitive outcomes and criminalization of medical errors. Curr Opin Anaesthesiol. 2022;35(6):728-732. doi:10.1097/ACO.0000000000001197
- Dekker S, Rafferty J, Oates A. Restorative Just Culture in Practice: Implementation and Evaluation. Routledge; 2022.
- Brattebø G, Flaatten HK. Errors in medicine: punishment versus learning medical adverse events revisited - expanding the frame. Curr Opin Anaesthesiol. 2023;36(2):240-245. doi:10.1097/ACO.0000000000001235
- Shabel W, Dennis JL. Missouri’s just culture collaborative. J Healthc Risk Manag. 2012;32(2):38-43. doi:10.1002/jhrm.21093
- Sculli GL, Pendley-Louis R, Neily J, et al. A high-reliability organization framework for health care: a multiyear implementation strategy and associated outcomes. J Patient Saf. 2022;18(1):64-70. doi:10.1097/PTS.0000000000000788
- Martin G, Chew S, McCarthy I, Dawson J, Dixon-Woods M. Encouraging openness in health care: policy and practice implications of a mixed-methods study in the English National Health Service. J Health Serv Res Policy. 2023;28(1):14-24. doi:10.1177/13558196221109053
- Siewert B, Brook OR, Swedeen S, Eisenberg RL, Hochman M. Overcoming human barriers to safety event reporting in radiology. Radiographics. 2019;39(1):251-263. doi:10.1148/rg.2019180135
- Barkell NP, Snyder SS. Just culture in healthcare: an integrative review. Nurs Forum. 2021;56(1):103-111. doi:10.1111/nuf.12525
- Murray JS, Lee J, Larson S, Range A, Scott D, Clifford J. Requirements for implementing a ‘just culture’ within healthcare organisations: an integrative review. BMJ Open Qual. 2023;12(2)e002237. doi:10.1136/bmjoq-2022-002237
- Mohr DC, Chen C, Sullivan J, Gunnar W, Damschroder L. Development and validation of the Veterans Health Administration patient safety culture survey. J Patient Saf. 2022;18(6):539-545. doi:10.1097/PTS.0000000000001027
- Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed. SAGE Publications, Inc.; 2014.
- Patton MQ. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. 4th ed. SAGE Publications, Inc.; 2015.
- Maxwell JA. Qualitative Research Design: An Interactive Approach. 3rd ed. SAGE Publications, Inc.; 2013.
- Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025-2047. doi:10.1007/s11135-011-9640-9
- Braun V, Clarke V. Thematic Analysis: A Practical Guide. SAGE Publications, Inc; 2021.
- Cox GR, Starr LM. VHA’s movement for change: implementing high-reliability principles and practices. J Healthc Manag. 2023;68(3):151-157. doi:10.1097/JDM-D-23-00056
- Dietl JE, Derksen C, Keller FM, Lippke S. Interdisciplinary and interprofessional communication intervention: how psychological safety fosters communication and increases patient safety. Front Psychol. 2023;14:1164288. doi:10.3389/fpsyg.2023.1164288
- Eng DM, Schweikart SJ. Why accountability sharing in health care organizational cultures means patients are probably safer. AMA J Ethics. 2020;22(9):E779-E783. doi:10.1001/amajethics.2020.779
- Veterans Health Administration National Center for Patient Safety. Just Culture Decision Support Tool. Revised May 2021. Accessed August 5, 2024.https://www.patientsafety.va.gov/docs/Just-Culture-Decision-Support-Tool-2022.pdf
Impact of Expanded Eligibility for Veterans With Other Than Honorable Discharges on Treatment Courts and VA Mental Health Care
In April 2022, the US Department of Veterans Affairs (VA) revised its behavioral health care eligibility policies to provide comprehensive mental and behavioral health care to former service members who received an Other Than Honorable (OTH) discharge characterization upon separation from military service.1 This policy shift represents a marked expansion in eligibility practices (Table 1 includes amended eligibility criteria).
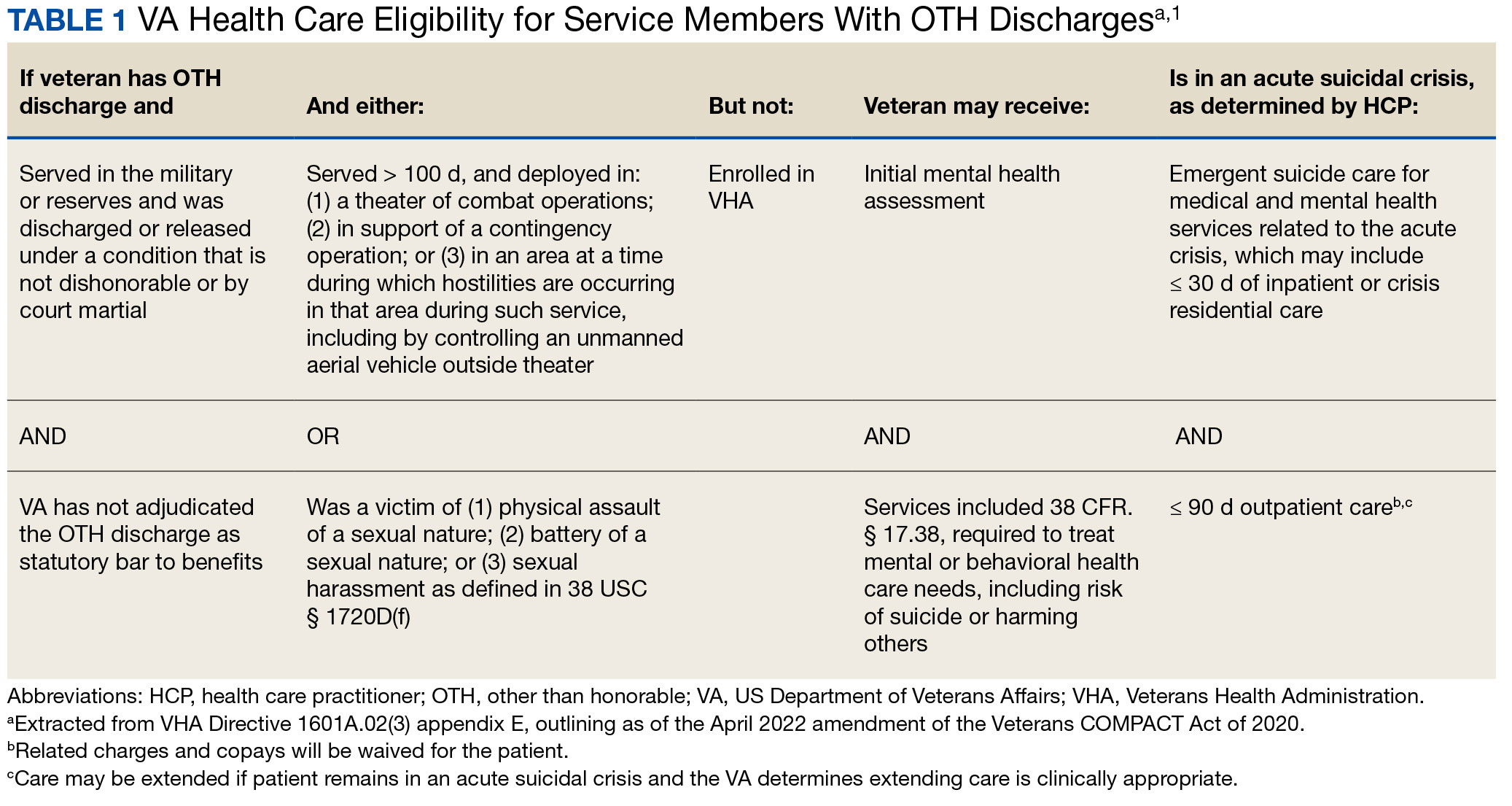
Since June 2017, eligibility policies allowed veterans with OTH discharges to receive “emergent mental health services” needed to stabilize acute mental health crises related to military service (eg, acute escalations in suicide risk).2,3 Previously, veterans with OTH discharges were largely ineligible for VA-based health care; these individuals were only able to access Veterans Health Administration (VHA) mental and behavioral health care through limited channels of eligibility (eg, for treatment of military sexual trauma or psychosis or other mental illness within 2 years of discharge).4,5 The impetus for expansions in eligibility stemmed from VA efforts to reduce the suicide rate among veterans.6-8 Implications of such expansion extend beyond suicide prevention efforts, with notable promised effects on the care of veterans with criminal-legal involvement. This article highlights potential effects of recent eligibility expansions on veterans with criminal-legal involvement and makes specific recommendations for agencies and organizations serving these veterans.
OTHER THAN HONORABLE DISCHARGE
The US Department of Defense delineates 6 discharge characterizations provided to service members upon separation from military service: honorable, general under honorable conditions, OTH, bad conduct, dishonorable, and uncharacterized. Honorable discharge characterizations are considered to reflect general concordance between service member behavior and military standards; general discharge characterizations reflect some disparity between the service member’s behavior and military standards; OTH, bad conduct, and dishonorable discharge characterizations reflect serious disparities between the service member’s behavior and military standards; and uncharacterized discharge characterizations are given when other discharge characterizations are deemed inappropriate.9,10 OTH discharge characterizations are typically issued under instances of misconduct, fraudulent entry, security reasons, or in lieu of trial by court martial.9,10
Recent research suggests that about 85% of service members receive an honorable discharge characterization upon separation from military service, 8% receive general, 6% receive OTH, and 1% receive bad conduct or dishonorable discharges.11 In 2017, the VA estimated there were > 500,000 prior service members with OTH discharge characterizations, which has grown over time (1.9% during the Korean Conflict, 2.5% during the Vietnam War Era, 3.9% during the Cold War, 4.8% in the Persian Gulf War, and 5.8% in the post-9/11 era).7,11
The OTH discharge characterization is 1 of 3 less than honorable discharges informally referred to as bad papers (ie, OTH, bad conduct, or dishonorable). Former service members receiving these discharge characterizations face significant social stigma and structural discrimination upon military discharge, including significant hurdles to employment and educational pursuits as well as notable social alienation.12 Due to their discharge characterization, some are viewed as less deserving of the veteran title, and until recently, many did not qualify for the complex legal definition of veteran as established by the Congress.11,13 Veterans with OTH discharge characterizations have also historically been excluded from services (eg, VHA care),3 benefits (eg, disability compensation),14 and protections (eg, Uniformed Services Employment and Reemployment Rights Act)15 offered to veterans with honorable or general discharge characterizations. However, eligibility policies have gradually expanded, providing veterans with OTH discharges with access to VHA-based mental and behavioral health services and VA supportive housing assistance.1,3,16
Perhaps due to their historical exclusion from VA services, there is limited research available on the behavioral health and associated needs of veterans with OTH discharges. Some scholars argue that historical exclusions have exacerbated underlying difficulties faced by this population, thereby contributing to stark health and social disparities across discharge types.14,15,17 Studies with large veteran samples, for example, reflect notable demographic and behavioral health differences across discharge types. Compared to routinely discharged veterans, veterans with OTH discharges are significantly more likely to be younger, have lower income, use substances, have a history of criminal-legal involvement, and have mental and physical health difficulties.18,19
Substantial evidence also suggests a historical racial bias, with service members of color being disproportionately more likely to receive an OTH discharge.12 Similarly, across all branches of military service, Black service members are significantly more likely to face general or special court martial in military justice proceedings when compared with White service members.20 Service members from gender and sexual minorities are also disproportionately impacted by the OTH designation. Historically, many have been discharged with bad papers due to discriminatory policies, such as Don’t Ask Don’t Tell, which discriminated on the basis of sexual orientation between December 1993 and September 2011, and Directive-type Memorandum-19-004, which banned transgender persons from military service between April 2019 and January 2021.21,22
There is also significant mental health bias in the provision of OTH discharges, such that OTH characterizations are disproportionately represented among individuals with mental health disorders.18-20 Veterans discharged from military service due to behavioral misconduct are significantly more likely to meet diagnostic criteria for various behavioral health conditions and to experience homelessness, criminal-legal involvement, and suicidal ideation and behavior compared with routinely-discharged veterans.23-28
Consistent with their comparatively higher rates of criminal-legal involvement relative to routinely discharged veterans, veterans with OTH discharges are disproportionately represented in criminal justice settings. While veterans with OTH discharges represent only 6% of discharging service members and 2.5% of community-based veterans, they represent 10% of incarcerated veterans.11,18,23,29 Preliminary research suggests veterans with OTH discharges may be at higher risk for lifetime incarceration, though the association between OTH discharge and frequency of lifetime arrests remains unclear.18,30
VETERANS TREATMENT COURTS
Given the overrepresentation of veterans with OTH discharges in criminal-legal settings, consideration for this subset of the veteran population and its unique needs is commonplace among problem-solving courts that service veterans. First conceptualized in 2004, Veterans Treatment Courts (VTCs) are specialized problem-solving courts that divert veterans away from traditional judicial court and penal systems and into community-based supervision and treatment (most commonly behavioral health services).31-34 Although each VTC program is unique in structure, policies, and procedures, most VTCs can be characterized by certain key elements, including voluntary participation, plea requirements, delayed sentencing (often including reduced or dismissed charges), integration of military culture into court proceedings, a rehabilitative vs adversarial approach to decreasing risk of future criminal behavior, mandated treatment and supervision during participation, and use of veteran mentors to provide peer support.32-35 Eligibility requirements vary; however, many restrict participation to veterans with honorable discharge types and charges for nonviolent offenses.32,33,35-37
VTCs connect veterans within the criminal-legal system to needed behavioral health, community, and social services.31-33,37 VTC participants are commonly connected to case management, behavioral health care, therapeutic journaling programs, and vocational rehabilitation.38,39 Accordingly, the most common difficulties faced by veterans participating in these courts include substance use, mental health, family issues, anger management and/or aggressive behavior, and homelessness.36,39 There is limited research on the effectiveness of VTCs. Evidence on their overall effectiveness is largely mixed, though some studies suggest VTC graduates tend to have lower recidivism rates than offenders more broadly or persons who terminate VTC programs prior to completion.40,41 Other studies suggest that VTC participants are more likely to have jail sanctions, new arrests, and new incarcerations relative to nontreatment court participants.42 Notably, experimental designs (considered the gold standard in assessing effectiveness) to date have not been applied to evaluate the effectiveness of VTCs; as such, the effectiveness of these programs remains an area in need of continued empirical investigation.
Like all problem-solving courts, VTCs occasionally struggle to connect participating defendants with appropriate care, particularly when encountering structural barriers (eg, insurance, transportation) and/or complex behavioral health needs (eg, personality disorders).34,43 As suicide rates among veterans experiencing criminal-legal involvement surge (about 150 per 100,000 in 2021, a 10% increase from 2020 to 2021 compared to about 40 per 100,000 and a 1.8% increase among other veterans), efficiency of adequate care coordination is vital.44 Many VTCs rely on VTC-VA partnerships and collaborations to navigate these difficulties and facilitate connection of participating veterans to needed services.32-34,45 For example, within the VHA, Veterans Justice Outreach (VJO) and Health Care for Re-Entry Veterans (HCRV) specialists assist and bridge the gap between the criminal-legal system (including, but not limited to VTCs) and VA services by engaging veterans involved in the criminal-legal system and connecting them to needed VA-based services (Table 2). Generally, VJO specialists support veterans involved with the front end of the criminallegal system (eg, arrest, pretrial incarceration, or participation in VTCs), while HCRV specialists tend to support veterans transitioning back into the community after a period of incarceration.46,47 Specific to VTCs, VJO specialists typically serve as liaisons between the courts and VA, coordinating VA services for defendants to fulfill their terms of VTC participation.46
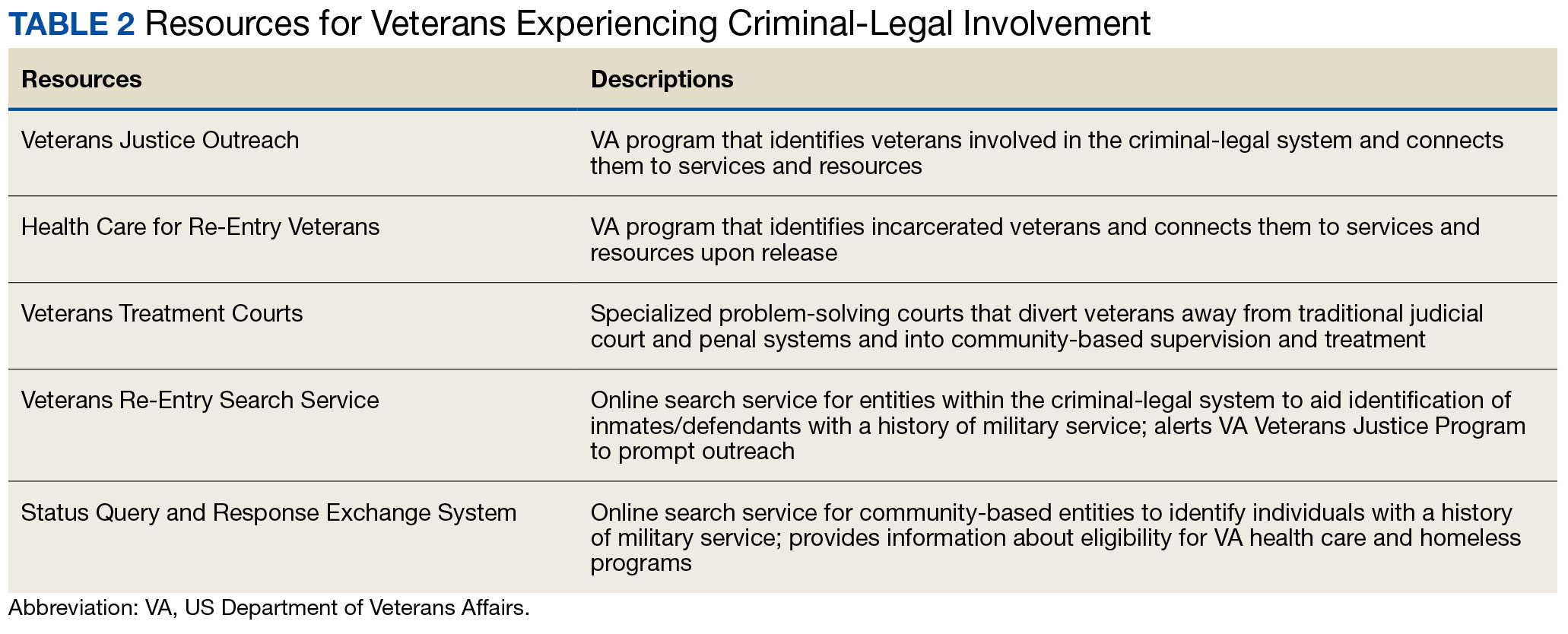
The historical exclusion of veterans with OTH discharge characterizations from VA-based services has restricted many from accessing VTC programs.32 Of 17 VTC programs active in Pennsylvania in 2014, only 5 accepted veterans with OTstayH discharges, and 3 required application to and eligibility for VA benefits.33 Similarly, in national surveys of VTC programs, about 1 in 3 report excluding veterans deemed ineligible for VA services.35,36 When veterans with OTH discharges have accessed VTC programs, they have historically relied on non-VA, community-based programming to fulfill treatment mandates, which may be less suited to addressing the unique needs of veterans.48
Veterans who utilize VTCs receive several benefits, namely peer support and mentorship, acceptance into a veteran-centric space, and connection with specially trained staff capable of supporting the veteran through applications for a range of VA benefits (eg, service connection, housing support).31-33,37 Given the disparate prevalence of OTH discharge characterizations among service members from racial, sexual, and gender minorities and among service members with mental health disorders, exclusion of veterans with OTH discharges from VTCs solely based on the type of discharge likely contributes to structural inequities among these already underserved groups by restricting access to these potential benefits. Such structural inequity stands in direct conflict with VTC best practice standards, which admonish programs to adjust eligibility requirements to facilitate access to treatment court programs for historically marginalized groups.49
ELIGIBILITY EXPANSIONS
Given the overrepresentation of veterans with OTH discharge characterizations within the criminal-legal system and historical barriers of these veterans to access needed mental and behavioral health care, expansions in VA eligibility policies could have immense implications for VTCs. First, these expansions could mitigate common barriers to connecting VTC-participating veterans with OTH discharges with needed behavioral health care by allowing these veterans to access established, VA-based services and programming. Expansion may also allow VTCs to serve as a key intercept point for identifying and engaging veterans with OTH discharges who may be unaware of their eligibility for VA-based behavioral health care.
Access to VA health care services is a major resource for VTC participants and a common requirement.32 Eligibility expansion should ease access barriers veterans with OTH discharges commonly face. By providing a potential source of treatment, expansions may also support OTH eligibility practices within VTCs, particularly practices that require participants to be eligible for VA health care.33,35,36 Some VTCs may continue to determine eligibility on the basis of discharge status and remain inaccessible to veterans with OTH discharge characterizations without program-level policy changes.32,36,37
Communicating changes in eligibility policies relevant to veterans with OTH discharges may be a challenge, because many of these individuals have no established channels of communication with the VA. Because veterans with OTH discharges are at increased risk for legal system involvement, VTCs may serve as a unique point of contact to help facilitate communication.18 For example, upon referral to a VTC, veterans with OTH discharges can be identified, VA health care eligibility can be verified, and veterans can connect to VA staff to facilitate enrollment in VA services and care.
VJO specialists are in a favorable position to serve a critical role in utilizing VTCs as a potential intercept point for engaging veterans with OTH discharge characterizations. As outlined in the STRONG Veterans Act of 2022, VJOs are mandated to “spread awareness and understanding of veteran eligibility for the [VJO] Program, including the eligibility of veterans who were discharged from service in the Armed Forces under conditions other than honorable.”50 The Act further requires VJOs to be annually trained in communicating eligibility changes as they arise. Accordingly, VJOs receive ongoing training in a wide variety of critical outreach topics, including changes in eligibility; while VJOs cannot make eligibility determinations, they are tasked with enrolling all veterans involved in the criminal-legal system with whom they interact into VHA services, whether through typical or special eligibility criteria (M. Stimmel, PhD, National Training Director for Veteran Justice Programming, oral communication, July 14, 2023). VJOs therefore routinely serve in this capacity of facilitating VA enrollment of veterans with OTH discharge characterizations.
Recommendations to Veteran-Servicing Judicial Programs
Considering these potential implications, professionals routinely interacting with veterans involved in the criminal-legal system should become familiarized with recent changes in VA eligibility policies. Such familiarization would support the identification of veterans previously considered ineligible for care; provision of education to these veterans regarding their new eligibility; and referral to appropriate VA-based behavioral health care options. Although conceptually simple, executing such an educational campaign may prove logistically difficult. Given their historical exclusion from VA services, veterans with OTH discharge characterizations are unlikely to seek VA-based services in times of need, instead relying on a broad swath of civilian community-based organizations and resources. Usual approaches to advertising VHA health care policy changes (eg, by notifying VA employees and/or departments providing corresponding services or by circulating information to veteran-focused mailing lists and organizations) likely would prove insufficient. Educational campaigns to disseminate information about recent OTH eligibility changes should instead consider partnering with traditionally civilian, communitybased organizations and institutions, such as state bar associations, legal aid networks, case management services, nonveteran treatment court programs (eg, drug courts, or domestic violence courts), or probation/ parole programs. Because national surveys suggest generally low military cultural competence among civilian populations, providing concurrent support in developing foundational veteran cultural competencies (eg, how to phrase questions about military service history, or understanding discharge characterizations) may be necessary to ensure effective identification and engagement of veteran clients.48
Programs that serve veterans with criminal-legal involvement should also consider potential relevance of recent OTH eligibility changes to program operations. VTC program staff and key partners (eg, judges, case managers, district attorneys, or defense attorneys), should revisit policies and procedures surrounding the engagement of veterans with OTH discharges within VTC programs and strategies for connecting these veterans with needed services. VTC programs that have historically excluded veterans with OTH discharges due to associated difficulties in locating and connecting with needed services should consider expanding eligibility policies considering recent shifts in VA behavioral health care eligibility.33,35,36 Within the VHA, VJO specialists can play a critical role in supporting these VTC eligibility and cultural shifts. Some evidence suggests a large proportion of VTC referrals are facilitated by VJO specialists and that many such referrals are identified when veterans involved with the criminal-legal system seek VA support and/or services.33 Given the historical exclusion of veterans with OTH discharges from VA care, strategies used by VJO specialists to identify, connect, and engage veterans with OTH discharges with VTCs and other services may be beneficial.
Even with knowledge of VA eligibility changes and considerations of these changes on local operations, many forensic settings and programs struggle to identify veterans. These difficulties are likely amplified among veterans with OTH discharge characterizations, who may be hesitant to self-disclose their military service history due to fear of stigma and/or views of OTH discharge characterizations as undeserving of the veteran title.12 The VA offers 2 tools to aid in identification of veterans for these settings: the Veterans Re-Entry Search Service (VRSS) and Status Query and Response Exchange System (SQUARES). For VRSS, correctional facilities, courts, and other criminal justice entities upload a simple spreadsheet that contains basic identifying information of inmates or defendants in their system. VRSS returns information about which inmates or defendants have a history of military service and alerts VA Veterans Justice Programs staff so they can conduct outreach. A pilot study conducted by the California Department of Corrections and Rehabilitation found that 2.7% of its inmate population self-identified as veterans, while VRSS identified 7.7% of inmates with a history of military service. This difference represented about 5000 previously unidentified veterans.51 Similarly, community entities that partner with the VA, such as law enforcement or homeless service programs, can be approved to become a SQUARES user and submit identifying information of individuals with whom they interact directly into the SQUARES search engine. SQUARES then directly returns information about the individual’s veteran status and eligibility for VA health care and homeless programs.
Other Eligibility Limitations
VTCs and other professionals looking to refer veterans with OTH discharge characterizations to VA-based behavioral health care should be aware of potential limitations in eligibility and access. Specifically, although veterans with OTH discharges are now broadly eligible for VA-based behavioral health care and homeless programs, they remain ineligible for other forms of health care, including primary care and nonbehavioral specialty care.1 Research has found a strong comorbidity between behavioral and nonbehavioral health concerns, particularly within historically marginalized demographic groups.52-55 Because these historically marginalized groups are often overrepresented among persons with criminal-legal involvement, veterans with OTH discharges, and VTC participants, such comorbidities require consideration by services or programming designed to support veterans with criminal-legal involvement.12,56-58 Connection with VA-based health care will therefore continue to fall short of addressing all health care needs of veterans with OTH discharges and effective case management will require considerable treatment coordination between VA behavioral health care practitioners (HCPs) and community-based HCPs (eg, primary care professionals or nonbehavioral HCPs).
Implications for VA Mental Health Care
Recent eligibility expansions will also have inevitable consequences for VA mental health care systems. For many years, these systems have been overburdened by high caseloads and clinician burnout.59,60 Given the generally elevated rates of mental health and substance use concerns among veterans with OTH discharge characterizations, expansions hold the potential to further burden caseloads with clinically complex, high-risk, high-need clients. Nevertheless, these expansions are also structured in a way that forces existing systems to absorb the responsibilities of providing necessary care to these veterans. To mitigate detrimental effects of eligibility expansions on the broader VA mental health system, clinicians should be explicitly trained in identifying veterans with OTH discharge characterizations and the implications of discharge status on broader health care eligibility. Treatment of veterans with OTH discharges may also benefit from close coordination between mental health professionals and behavioral health care coordinators to ensure appropriate coordination of care between VA- and non–VA-based HCPs.
CONCLUSIONS
Recent changes to VA eligibility policies now allow comprehensive mental and behavioral health care services to be provided to veterans with OTH discharges.1 Compared to routinely discharged veterans, veterans with OTH discharges are more likely to be persons of color, sexual or gender minorities, and experiencing mental health-related difficulties. Given the disproportionate mental health burden often faced by veterans with OTH discharges and relative overrepresentation of these veterans in judicial and correctional systems, these changes have considerable implications for programs and services designed to support veterans with criminallegal involvement. Professionals within these systems, particularly VTC programs, are therefore encouraged to familiarize themselves with recent changes in VA eligibility policies and to revisit strategies, policies, and procedures surrounding the engagement and enrollment of veterans with OTH discharge characterizations. Doing so may ensure veterans with OTH discharges are effectively connected to needed behavioral health care services.
- US Department of Veterans, Veterans Health Administration. VHA Directive 1601A.02(6): Eligibility Determination. Updated March 6, 2024. Accessed August 8, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8908
- Mental and behavioral health care for certain former members of the Armed Forces. 38 USC §1720I (2018). Accessed August 5, 2024. https://uscode.house.gov/view.xhtml?req=(title:38%20section:1720I%20edition:prelim
- US Department of Veterans, Veterans Health Administration. VHA Directive 1601A.02, Eligibility Determination. June 7, 2017.
- US Department of Veterans, Veterans Health Administration. VHA Directive 1115(1), Military Sexual Trauma (MST) Program. May 8, 2018. Accessed August 5, 2024. https:// www.va.gov/vhapublications/viewpublication.asp?pub_ID=6402
- US Department of Veterans Affairs. Tentative Eligibility Determinations; Presumptive Eligibility for Psychosis and Other Mental Illness. 38 CFR §17.109. May 14, 2013. Accessed August 5, 2024. https://www.federalregister.gov/documents/2013/05/14/2013-11410/tentative-eligibility-determinations-presumptive-eligibility-for-psychosis-and-other-mental-illness
- US Department of Veterans Affairs, VA Office of Mental Health and Suicide Prevention. National strategy for preventing veteran suicide 2018-2028. Published September 2018. Accessed August 5, 2024. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf
- US Department of Veterans Affairs. VA secretary announces intention to expand mental health care to former service members with other-than-honorable discharges and in crisis. Press Release. March 8, 2017. Accessed August 5, 2024. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=2867
- Smith C. Dramatic increase in mental health services to other-than-honorable discharge veterans. VA News. February 23, 2022. Accessed August 5, 2024. https://news.va.gov/100460/dramatic-increase-in-mental-health-services-to-other-than-honorable-discharge-veterans/
- US Department of Defense. DoD Instruction 1332.14. Enlisted administrative separations. Updated August 1, 2024. Accessed August 5, 2024. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133214p.pdf
- US Department of Defense. DoD Instruction 1332.30. Commissioned officer administrative separations. Updated September 9, 2021. Accessed August 5, 2024. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133230p.pdf
- OUTVETS, Legal Services Center of Harvard Law School, Veterans Legal Services. Turned away: how the VA unlawfully denies healthcare to veterans with bad paper discharges. 2020. Accessed August 5, 2024. https://legalservicescenter.org/wp-content/uploads/Turn-Away-Report.pdf
- McClean H. Discharged and discarded: the collateral consequences of a less-than-honorable military discharge. Columbia Law Rev. 2021;121(7):2203-2268.
- Veterans Benefits, General Provisions, Definitions. 38 USC §101(2) (1958). Accessed August 5, 2024. https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title38-section101&num=0&edition=prelim
- Bedford JR. Other than honorable discharges: unfair and unjust life sentences of decreased earning capacity. U Penn J Law Pub Affairs. 2021;6(4):687.
- Karin ML. Other than honorable discrimination. Case Western Reserve Law Rev. 2016;67(1):135-191. https://scholarlycommons.law.case.edu/caselrev/vol67/iss1/9
- Veteran HOUSE Act of 2020, HR 2398, 116th Cong, (2020). Accessed August 5, 2024. https://www.congress.gov/bill/116th-congress/house-bill/2398
- Scapardine D. Leaving other than honorable soldiers behind: how the Departments of Defense and Veterans Affairs inadvertently created a health and social crisis. Md Law Rev. 2017;76(4):1133-1165.
- Elbogen EB, Wagner HR, Brancu M, et al. Psychosocial risk factors and other than honorable military discharge: providing healthcare to previously ineligible veterans. Mil Med. 2018;183(9-10):e532-e538. doi:10.1093/milmed/usx128
- Tsai J, Rosenheck RA. Characteristics and health needs of veterans with other-than-honorable discharges: expanding eligibility in the Veterans Health Administration. Mil Med. 2018;183(5-6):e153-e157. doi:10.1093/milmed/usx110
- Christensen DM, Tsilker Y. Racial disparities in military justice: findings of substantial and persistent racial disparities within the United States military justice system. Accessed August 5, 2024. https://www.protectourdefenders.com/wp-content/uploads/2017/05/Report_20.pdf
- Don’t Ask Don’t Tell, 10 USC §654 (1993) (Repealed 2010). Accessed August 5, 2024. http://www.gpo.gov/fdsys/pkg/USCODE-2010-title10/pdf/USCODE-2010-title10-subtitleA-partII-chap37-sec654.pdf
- Palm Center. The making of a ban: how DTM-19-004 works to push transgender people out of military service. 2019. March 20, 2019. Accessed August 5, 2024. https://www.palmcenter.org/wp-content/uploads/2019/04/The-Making-of-a-Ban.pdf
- Edwards ER, Greene AL, Epshteyn G, Gromatsky M, Kinney AR, Holliday R. Mental health of incarcerated veterans and civilians: latent class analysis of the 2016 Survey of Prison Inmates. Crim Justice Behav. 2022;49(12):1800- 1821. doi:10.1177/00938548221121142
- Brignone E, Fargo JD, Blais RK, Carter ME, Samore MH, Gundlapalli AV. Non-routine discharge from military service: mental illness, substance use disorders, and suicidality. Am J Prev Med. 2017;52(5):557-565. doi:10.1016/j.amepre.2016.11.015
- Gamache G, Rosenheck R, Tessler R. Military discharge status of homeless veterans with mental illness. Mil Med. 2000;165(11):803-808. doi:10.1093/milmed/165.11.803
- Gundlapalli AV, Fargo JD, Metraux S, et al. Military Misconduct and Homelessness Among US Veterans Separated From Active Duty, 2001-2012. JAMA. 2015;314(8):832-834. doi:10.1001/jama.2015.8207
- Brooks Holliday S, Pedersen ER. The association between discharge status, mental health, and substance misuse among young adult veterans. Psychiatry Res. 2017;256:428-434. doi:10.1016/j.psychres.2017.07.011
- Williamson RB. DOD Health: Actions Needed to Ensure Post-Traumatic Stress Disorder and Traumatic Brain Injury are Considered in Misconduct Separations. US Government Accountability Office; 2017. Accessed August 5, 2024. https://apps.dtic.mil/sti/pdfs/AD1168610.pdf
- Maruschak LM, Bronson J, Alper M. Indicators of mental health problems reported by prisoners: survey of prison inmates. US Department of Justice Bureau of Justice Statistics. June 2021. Accessed August 5, 2024. https://bjs.ojp.gov/sites/g/files/xyckuh236/files/media/document/imhprpspi16st.pdf
- Brooke E, Gau J. Military service and lifetime arrests: examining the effects of the total military experience on arrests in a sample of prison inmates. Crim Justice Policy Rev. 2018;29(1):24-44. doi:10.1177/0887403415619007
- Russell RT. Veterans treatment court: a proactive approach. N Engl J Crim Civ Confin. 2009;35:357-372.
- Cartwright T. To care for him who shall have borne the battle: the recent development of Veterans Treatment Courts in America. Stanford Law Pol Rev. 2011;22:295-316.
- Douds AS, Ahlin EM, Howard D, Stigerwalt S. Varieties of veterans’ courts: a statewide assessment of veterans’ treatment court components. Crim Justice Policy Rev. 2017;28:740-769. doi:10.1177/0887403415620633
- Rowen J. Worthy of justice: a veterans treatment court in practice. Law Policy. 2020;42(1):78-100. doi:10.1111/lapo.12142
- Timko C, Flatley B, Tjemsland A, et al. A longitudinal examination of veterans treatment courts’ characteristics and eligibility criteria. Justice Res Policy. 2016;17(2):123-136.
- Baldwin JM. Executive summary: national survey of veterans treatment courts. SSRN. Preprint posted online June 5, 2013. Accessed August 5, 2024. doi:10.2139/ssrn.2274138
- Renz T. Veterans treatment court: a hand up rather than lock up. Richmond Public Interest Law Rev. 2013;17(3):697-705. https://scholarship.richmond.edu/pilr/vol17/iss3/6
- Knudsen KJ, Wingenfeld S. A specialized treatment court for veterans with trauma exposure: implications for the field. Community Ment Health J. 2016;52(2):127-135. doi:10.1007/s10597-015-9845-9
- McCall JD, Tsai J, Gordon AJ. Veterans treatment court research: participant characteristics, outcomes, and gaps in the literature. J Offender Rehabil. 2018;57:384-401. doi:10.1080/10509674.2018.1510864
- Smith JS. The Anchorage, Alaska veterans court and recidivism: July 6, 2004 – December 31, 2010. Alsk Law Rev. 2012;29(1):93-111.
- Hartley RD, Baldwin JM. Waging war on recidivism among justice-involved veterans: an impact evaluation of a large urban veterans treatment court. Crim Justice Policy Rev. 2019;30(1):52-78. doi:10.1177/0887403416650490
- Tsai J, Flatley B, Kasprow WJ, Clark S, Finlay A. Diversion of veterans with criminal justice involvement to treatment courts: participant characteristics and outcomes. Psychiatr Serv. 2017;68(4):375-383. doi:10.1176/appi.ps.201600233
- Edwards ER, Sissoko DR, Abrams D, Samost D, La Gamma S, Geraci J. Connecting mental health court participants with services: process, challenges, and recommendations. Psychol Public Policy Law. 2020;26(4):463-475. doi:10.1037/law0000236
- US Department of Veterans Affairs, VA Office of Mental Health and Suicide Prevention. 2023 National Veteran Suicide Prevention Annual Report. US Department of Veterans Affairs; November 2023. Accessed August 5, 2024. https://www.mentalhealth.va.gov/docs/data-sheets/2023/2023-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-508.pdf
- Finlay AK, Clark S, Blue-Howells J, et al. Logic model of the Department of Veterans Affairs’ role in veterans treatment courts. Drug Court Rev. 2019;2:45-62.
- Finlay AK, Smelson D, Sawh L, et al. U.S. Department of Veterans Affairs veterans justice outreach program: connecting justice-involved veterans with mental health and substance use disorder treatment. Crim Justice Policy Rev. 2016;27(2):10.1177/0887403414562601. doi:10.1177/0887403414562601
- Finlay AK, Stimmel M, Blue-Howells J, et al. Use of Veterans Health Administration mental health and substance use disorder treatment after exiting prison: the health care for reentry veterans program. Adm Policy Ment Health. 2017;44(2):177-187. doi:10.1007/s10488-015-0708-z
- Meyer EG, Writer BW, Brim W. The Importance of Military Cultural Competence. Curr Psychiatry Rep. 2016;18(3):26. doi:10.1007/s11920-016-0662-9
- National Association of Drug Court Professionals. Adult Drug Court Best Practice Standards Volume I. National Association of Drug Court Professionals; 2013. Accessed August 5, 2024. https://allrise.org/publications/standards/
- STRONG Veterans Act of 2022, HR 6411, 117th Cong (2022). https://www.congress.gov/bill/117th-congress/house-bill/6411/text
- Pelletier D, Clark S, Davis L. Veterans reentry search service (VRSS) and the SQUARES application. Presented at: National Association of Drug Court Professionals Conference; August 15-18, 2021; National Harbor, Maryland.
- Scott KM, Lim C, Al-Hamzawi A, et al. Association of Mental Disorders With Subsequent Chronic Physical Conditions: World Mental Health Surveys From 17 Countries. JAMA Psychiatry. 2016;73(2):150-158. doi:10.1001/jamapsychiatry.2015.2688
- Ahmed N, Conway CA. Medical and mental health comorbidities among minority racial/ethnic groups in the United States. J Soc Beh Health Sci. 2020;14(1):153-168. doi:10.5590/JSBHS.2020.14.1.11
- Hanna B, Desai R, Parekh T, Guirguis E, Kumar G, Sachdeva R. Psychiatric disorders in the U.S. transgender population. Ann Epidemiol. 2019;39:1-7.e1. doi:10.1016/j.annepidem.2019.09.009
- Watkins DC, Assari S, Johnson-Lawrence V. Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder, and chronic medical conditions. J Racial Ethn Health Disparities. 2015;2(3):385- 394. doi:10.1007/s40615-015-0085-z
- Baldwin J. Whom do they serve? National examination of veterans treatment court participants and their challenges. Crim Justice Policy Rev. 2017;28(6):515-554. doi:10.1177/0887403415606184
- Beatty LG, Snell TL. Profile of prison inmates, 2016. US Department of Justice Bureau of Justice Statistics. December 2021. Accessed August 5, 2024. https://bjs.ojp.gov/content/pub/pdf/ppi16.pdf
- Al-Rousan T, Rubenstein L, Sieleni B, Deol H, Wallace RB. Inside the nation’s largest mental health institution: a prevalence study in a state prison system. BMC Public Health. 2017;17(1):342. doi:10.1186/s12889-017-4257-0
- Rosen CS, Kaplan AN, Nelson DB, et al. Implementation context and burnout among Department of Veterans Affairs psychotherapists prior to and during the COVID-19 pandemic. J Affect Disord. 2023;320:517-524. doi:10.1016/j.jad.2022.09.141
- Tsai J, Jones N, Klee A, Deegan D. Job burnout among mental health staff at a veterans affairs psychosocial rehabilitation center. Community Ment Health J. 2020;56(2):294- 297. doi:10.1007/s10597-019-00487-5
In April 2022, the US Department of Veterans Affairs (VA) revised its behavioral health care eligibility policies to provide comprehensive mental and behavioral health care to former service members who received an Other Than Honorable (OTH) discharge characterization upon separation from military service.1 This policy shift represents a marked expansion in eligibility practices (Table 1 includes amended eligibility criteria).
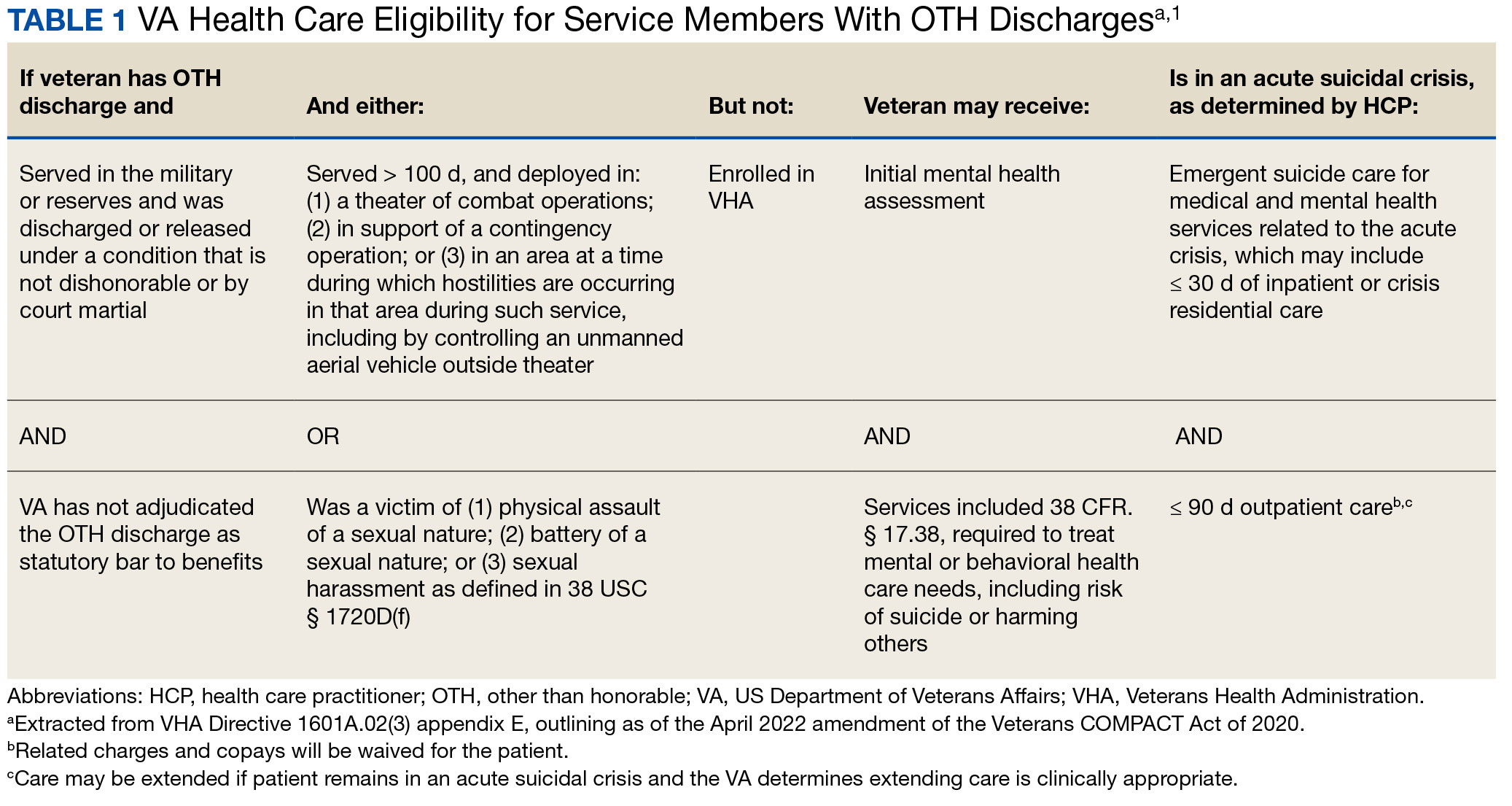
Since June 2017, eligibility policies allowed veterans with OTH discharges to receive “emergent mental health services” needed to stabilize acute mental health crises related to military service (eg, acute escalations in suicide risk).2,3 Previously, veterans with OTH discharges were largely ineligible for VA-based health care; these individuals were only able to access Veterans Health Administration (VHA) mental and behavioral health care through limited channels of eligibility (eg, for treatment of military sexual trauma or psychosis or other mental illness within 2 years of discharge).4,5 The impetus for expansions in eligibility stemmed from VA efforts to reduce the suicide rate among veterans.6-8 Implications of such expansion extend beyond suicide prevention efforts, with notable promised effects on the care of veterans with criminal-legal involvement. This article highlights potential effects of recent eligibility expansions on veterans with criminal-legal involvement and makes specific recommendations for agencies and organizations serving these veterans.
OTHER THAN HONORABLE DISCHARGE
The US Department of Defense delineates 6 discharge characterizations provided to service members upon separation from military service: honorable, general under honorable conditions, OTH, bad conduct, dishonorable, and uncharacterized. Honorable discharge characterizations are considered to reflect general concordance between service member behavior and military standards; general discharge characterizations reflect some disparity between the service member’s behavior and military standards; OTH, bad conduct, and dishonorable discharge characterizations reflect serious disparities between the service member’s behavior and military standards; and uncharacterized discharge characterizations are given when other discharge characterizations are deemed inappropriate.9,10 OTH discharge characterizations are typically issued under instances of misconduct, fraudulent entry, security reasons, or in lieu of trial by court martial.9,10
Recent research suggests that about 85% of service members receive an honorable discharge characterization upon separation from military service, 8% receive general, 6% receive OTH, and 1% receive bad conduct or dishonorable discharges.11 In 2017, the VA estimated there were > 500,000 prior service members with OTH discharge characterizations, which has grown over time (1.9% during the Korean Conflict, 2.5% during the Vietnam War Era, 3.9% during the Cold War, 4.8% in the Persian Gulf War, and 5.8% in the post-9/11 era).7,11
The OTH discharge characterization is 1 of 3 less than honorable discharges informally referred to as bad papers (ie, OTH, bad conduct, or dishonorable). Former service members receiving these discharge characterizations face significant social stigma and structural discrimination upon military discharge, including significant hurdles to employment and educational pursuits as well as notable social alienation.12 Due to their discharge characterization, some are viewed as less deserving of the veteran title, and until recently, many did not qualify for the complex legal definition of veteran as established by the Congress.11,13 Veterans with OTH discharge characterizations have also historically been excluded from services (eg, VHA care),3 benefits (eg, disability compensation),14 and protections (eg, Uniformed Services Employment and Reemployment Rights Act)15 offered to veterans with honorable or general discharge characterizations. However, eligibility policies have gradually expanded, providing veterans with OTH discharges with access to VHA-based mental and behavioral health services and VA supportive housing assistance.1,3,16
Perhaps due to their historical exclusion from VA services, there is limited research available on the behavioral health and associated needs of veterans with OTH discharges. Some scholars argue that historical exclusions have exacerbated underlying difficulties faced by this population, thereby contributing to stark health and social disparities across discharge types.14,15,17 Studies with large veteran samples, for example, reflect notable demographic and behavioral health differences across discharge types. Compared to routinely discharged veterans, veterans with OTH discharges are significantly more likely to be younger, have lower income, use substances, have a history of criminal-legal involvement, and have mental and physical health difficulties.18,19
Substantial evidence also suggests a historical racial bias, with service members of color being disproportionately more likely to receive an OTH discharge.12 Similarly, across all branches of military service, Black service members are significantly more likely to face general or special court martial in military justice proceedings when compared with White service members.20 Service members from gender and sexual minorities are also disproportionately impacted by the OTH designation. Historically, many have been discharged with bad papers due to discriminatory policies, such as Don’t Ask Don’t Tell, which discriminated on the basis of sexual orientation between December 1993 and September 2011, and Directive-type Memorandum-19-004, which banned transgender persons from military service between April 2019 and January 2021.21,22
There is also significant mental health bias in the provision of OTH discharges, such that OTH characterizations are disproportionately represented among individuals with mental health disorders.18-20 Veterans discharged from military service due to behavioral misconduct are significantly more likely to meet diagnostic criteria for various behavioral health conditions and to experience homelessness, criminal-legal involvement, and suicidal ideation and behavior compared with routinely-discharged veterans.23-28
Consistent with their comparatively higher rates of criminal-legal involvement relative to routinely discharged veterans, veterans with OTH discharges are disproportionately represented in criminal justice settings. While veterans with OTH discharges represent only 6% of discharging service members and 2.5% of community-based veterans, they represent 10% of incarcerated veterans.11,18,23,29 Preliminary research suggests veterans with OTH discharges may be at higher risk for lifetime incarceration, though the association between OTH discharge and frequency of lifetime arrests remains unclear.18,30
VETERANS TREATMENT COURTS
Given the overrepresentation of veterans with OTH discharges in criminal-legal settings, consideration for this subset of the veteran population and its unique needs is commonplace among problem-solving courts that service veterans. First conceptualized in 2004, Veterans Treatment Courts (VTCs) are specialized problem-solving courts that divert veterans away from traditional judicial court and penal systems and into community-based supervision and treatment (most commonly behavioral health services).31-34 Although each VTC program is unique in structure, policies, and procedures, most VTCs can be characterized by certain key elements, including voluntary participation, plea requirements, delayed sentencing (often including reduced or dismissed charges), integration of military culture into court proceedings, a rehabilitative vs adversarial approach to decreasing risk of future criminal behavior, mandated treatment and supervision during participation, and use of veteran mentors to provide peer support.32-35 Eligibility requirements vary; however, many restrict participation to veterans with honorable discharge types and charges for nonviolent offenses.32,33,35-37
VTCs connect veterans within the criminal-legal system to needed behavioral health, community, and social services.31-33,37 VTC participants are commonly connected to case management, behavioral health care, therapeutic journaling programs, and vocational rehabilitation.38,39 Accordingly, the most common difficulties faced by veterans participating in these courts include substance use, mental health, family issues, anger management and/or aggressive behavior, and homelessness.36,39 There is limited research on the effectiveness of VTCs. Evidence on their overall effectiveness is largely mixed, though some studies suggest VTC graduates tend to have lower recidivism rates than offenders more broadly or persons who terminate VTC programs prior to completion.40,41 Other studies suggest that VTC participants are more likely to have jail sanctions, new arrests, and new incarcerations relative to nontreatment court participants.42 Notably, experimental designs (considered the gold standard in assessing effectiveness) to date have not been applied to evaluate the effectiveness of VTCs; as such, the effectiveness of these programs remains an area in need of continued empirical investigation.
Like all problem-solving courts, VTCs occasionally struggle to connect participating defendants with appropriate care, particularly when encountering structural barriers (eg, insurance, transportation) and/or complex behavioral health needs (eg, personality disorders).34,43 As suicide rates among veterans experiencing criminal-legal involvement surge (about 150 per 100,000 in 2021, a 10% increase from 2020 to 2021 compared to about 40 per 100,000 and a 1.8% increase among other veterans), efficiency of adequate care coordination is vital.44 Many VTCs rely on VTC-VA partnerships and collaborations to navigate these difficulties and facilitate connection of participating veterans to needed services.32-34,45 For example, within the VHA, Veterans Justice Outreach (VJO) and Health Care for Re-Entry Veterans (HCRV) specialists assist and bridge the gap between the criminal-legal system (including, but not limited to VTCs) and VA services by engaging veterans involved in the criminal-legal system and connecting them to needed VA-based services (Table 2). Generally, VJO specialists support veterans involved with the front end of the criminallegal system (eg, arrest, pretrial incarceration, or participation in VTCs), while HCRV specialists tend to support veterans transitioning back into the community after a period of incarceration.46,47 Specific to VTCs, VJO specialists typically serve as liaisons between the courts and VA, coordinating VA services for defendants to fulfill their terms of VTC participation.46
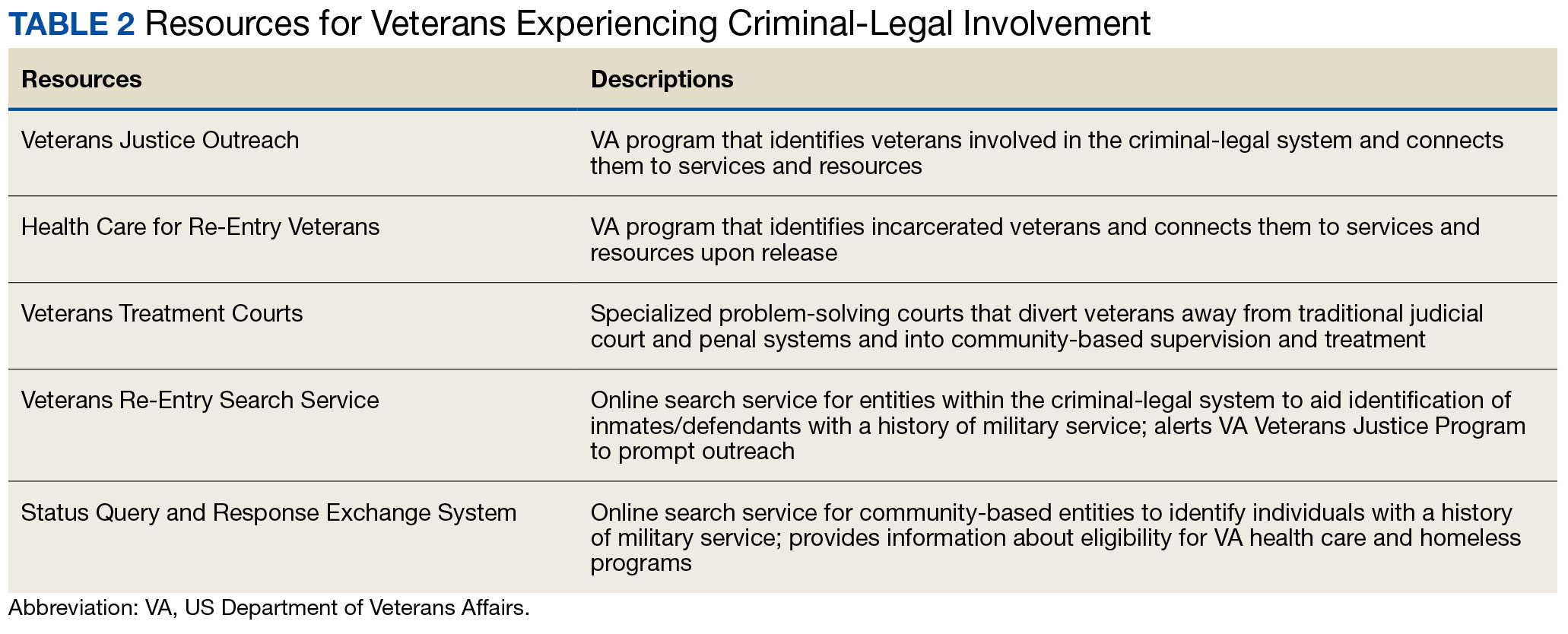
The historical exclusion of veterans with OTH discharge characterizations from VA-based services has restricted many from accessing VTC programs.32 Of 17 VTC programs active in Pennsylvania in 2014, only 5 accepted veterans with OTstayH discharges, and 3 required application to and eligibility for VA benefits.33 Similarly, in national surveys of VTC programs, about 1 in 3 report excluding veterans deemed ineligible for VA services.35,36 When veterans with OTH discharges have accessed VTC programs, they have historically relied on non-VA, community-based programming to fulfill treatment mandates, which may be less suited to addressing the unique needs of veterans.48
Veterans who utilize VTCs receive several benefits, namely peer support and mentorship, acceptance into a veteran-centric space, and connection with specially trained staff capable of supporting the veteran through applications for a range of VA benefits (eg, service connection, housing support).31-33,37 Given the disparate prevalence of OTH discharge characterizations among service members from racial, sexual, and gender minorities and among service members with mental health disorders, exclusion of veterans with OTH discharges from VTCs solely based on the type of discharge likely contributes to structural inequities among these already underserved groups by restricting access to these potential benefits. Such structural inequity stands in direct conflict with VTC best practice standards, which admonish programs to adjust eligibility requirements to facilitate access to treatment court programs for historically marginalized groups.49
ELIGIBILITY EXPANSIONS
Given the overrepresentation of veterans with OTH discharge characterizations within the criminal-legal system and historical barriers of these veterans to access needed mental and behavioral health care, expansions in VA eligibility policies could have immense implications for VTCs. First, these expansions could mitigate common barriers to connecting VTC-participating veterans with OTH discharges with needed behavioral health care by allowing these veterans to access established, VA-based services and programming. Expansion may also allow VTCs to serve as a key intercept point for identifying and engaging veterans with OTH discharges who may be unaware of their eligibility for VA-based behavioral health care.
Access to VA health care services is a major resource for VTC participants and a common requirement.32 Eligibility expansion should ease access barriers veterans with OTH discharges commonly face. By providing a potential source of treatment, expansions may also support OTH eligibility practices within VTCs, particularly practices that require participants to be eligible for VA health care.33,35,36 Some VTCs may continue to determine eligibility on the basis of discharge status and remain inaccessible to veterans with OTH discharge characterizations without program-level policy changes.32,36,37
Communicating changes in eligibility policies relevant to veterans with OTH discharges may be a challenge, because many of these individuals have no established channels of communication with the VA. Because veterans with OTH discharges are at increased risk for legal system involvement, VTCs may serve as a unique point of contact to help facilitate communication.18 For example, upon referral to a VTC, veterans with OTH discharges can be identified, VA health care eligibility can be verified, and veterans can connect to VA staff to facilitate enrollment in VA services and care.
VJO specialists are in a favorable position to serve a critical role in utilizing VTCs as a potential intercept point for engaging veterans with OTH discharge characterizations. As outlined in the STRONG Veterans Act of 2022, VJOs are mandated to “spread awareness and understanding of veteran eligibility for the [VJO] Program, including the eligibility of veterans who were discharged from service in the Armed Forces under conditions other than honorable.”50 The Act further requires VJOs to be annually trained in communicating eligibility changes as they arise. Accordingly, VJOs receive ongoing training in a wide variety of critical outreach topics, including changes in eligibility; while VJOs cannot make eligibility determinations, they are tasked with enrolling all veterans involved in the criminal-legal system with whom they interact into VHA services, whether through typical or special eligibility criteria (M. Stimmel, PhD, National Training Director for Veteran Justice Programming, oral communication, July 14, 2023). VJOs therefore routinely serve in this capacity of facilitating VA enrollment of veterans with OTH discharge characterizations.
Recommendations to Veteran-Servicing Judicial Programs
Considering these potential implications, professionals routinely interacting with veterans involved in the criminal-legal system should become familiarized with recent changes in VA eligibility policies. Such familiarization would support the identification of veterans previously considered ineligible for care; provision of education to these veterans regarding their new eligibility; and referral to appropriate VA-based behavioral health care options. Although conceptually simple, executing such an educational campaign may prove logistically difficult. Given their historical exclusion from VA services, veterans with OTH discharge characterizations are unlikely to seek VA-based services in times of need, instead relying on a broad swath of civilian community-based organizations and resources. Usual approaches to advertising VHA health care policy changes (eg, by notifying VA employees and/or departments providing corresponding services or by circulating information to veteran-focused mailing lists and organizations) likely would prove insufficient. Educational campaigns to disseminate information about recent OTH eligibility changes should instead consider partnering with traditionally civilian, communitybased organizations and institutions, such as state bar associations, legal aid networks, case management services, nonveteran treatment court programs (eg, drug courts, or domestic violence courts), or probation/ parole programs. Because national surveys suggest generally low military cultural competence among civilian populations, providing concurrent support in developing foundational veteran cultural competencies (eg, how to phrase questions about military service history, or understanding discharge characterizations) may be necessary to ensure effective identification and engagement of veteran clients.48
Programs that serve veterans with criminal-legal involvement should also consider potential relevance of recent OTH eligibility changes to program operations. VTC program staff and key partners (eg, judges, case managers, district attorneys, or defense attorneys), should revisit policies and procedures surrounding the engagement of veterans with OTH discharges within VTC programs and strategies for connecting these veterans with needed services. VTC programs that have historically excluded veterans with OTH discharges due to associated difficulties in locating and connecting with needed services should consider expanding eligibility policies considering recent shifts in VA behavioral health care eligibility.33,35,36 Within the VHA, VJO specialists can play a critical role in supporting these VTC eligibility and cultural shifts. Some evidence suggests a large proportion of VTC referrals are facilitated by VJO specialists and that many such referrals are identified when veterans involved with the criminal-legal system seek VA support and/or services.33 Given the historical exclusion of veterans with OTH discharges from VA care, strategies used by VJO specialists to identify, connect, and engage veterans with OTH discharges with VTCs and other services may be beneficial.
Even with knowledge of VA eligibility changes and considerations of these changes on local operations, many forensic settings and programs struggle to identify veterans. These difficulties are likely amplified among veterans with OTH discharge characterizations, who may be hesitant to self-disclose their military service history due to fear of stigma and/or views of OTH discharge characterizations as undeserving of the veteran title.12 The VA offers 2 tools to aid in identification of veterans for these settings: the Veterans Re-Entry Search Service (VRSS) and Status Query and Response Exchange System (SQUARES). For VRSS, correctional facilities, courts, and other criminal justice entities upload a simple spreadsheet that contains basic identifying information of inmates or defendants in their system. VRSS returns information about which inmates or defendants have a history of military service and alerts VA Veterans Justice Programs staff so they can conduct outreach. A pilot study conducted by the California Department of Corrections and Rehabilitation found that 2.7% of its inmate population self-identified as veterans, while VRSS identified 7.7% of inmates with a history of military service. This difference represented about 5000 previously unidentified veterans.51 Similarly, community entities that partner with the VA, such as law enforcement or homeless service programs, can be approved to become a SQUARES user and submit identifying information of individuals with whom they interact directly into the SQUARES search engine. SQUARES then directly returns information about the individual’s veteran status and eligibility for VA health care and homeless programs.
Other Eligibility Limitations
VTCs and other professionals looking to refer veterans with OTH discharge characterizations to VA-based behavioral health care should be aware of potential limitations in eligibility and access. Specifically, although veterans with OTH discharges are now broadly eligible for VA-based behavioral health care and homeless programs, they remain ineligible for other forms of health care, including primary care and nonbehavioral specialty care.1 Research has found a strong comorbidity between behavioral and nonbehavioral health concerns, particularly within historically marginalized demographic groups.52-55 Because these historically marginalized groups are often overrepresented among persons with criminal-legal involvement, veterans with OTH discharges, and VTC participants, such comorbidities require consideration by services or programming designed to support veterans with criminal-legal involvement.12,56-58 Connection with VA-based health care will therefore continue to fall short of addressing all health care needs of veterans with OTH discharges and effective case management will require considerable treatment coordination between VA behavioral health care practitioners (HCPs) and community-based HCPs (eg, primary care professionals or nonbehavioral HCPs).
Implications for VA Mental Health Care
Recent eligibility expansions will also have inevitable consequences for VA mental health care systems. For many years, these systems have been overburdened by high caseloads and clinician burnout.59,60 Given the generally elevated rates of mental health and substance use concerns among veterans with OTH discharge characterizations, expansions hold the potential to further burden caseloads with clinically complex, high-risk, high-need clients. Nevertheless, these expansions are also structured in a way that forces existing systems to absorb the responsibilities of providing necessary care to these veterans. To mitigate detrimental effects of eligibility expansions on the broader VA mental health system, clinicians should be explicitly trained in identifying veterans with OTH discharge characterizations and the implications of discharge status on broader health care eligibility. Treatment of veterans with OTH discharges may also benefit from close coordination between mental health professionals and behavioral health care coordinators to ensure appropriate coordination of care between VA- and non–VA-based HCPs.
CONCLUSIONS
Recent changes to VA eligibility policies now allow comprehensive mental and behavioral health care services to be provided to veterans with OTH discharges.1 Compared to routinely discharged veterans, veterans with OTH discharges are more likely to be persons of color, sexual or gender minorities, and experiencing mental health-related difficulties. Given the disproportionate mental health burden often faced by veterans with OTH discharges and relative overrepresentation of these veterans in judicial and correctional systems, these changes have considerable implications for programs and services designed to support veterans with criminallegal involvement. Professionals within these systems, particularly VTC programs, are therefore encouraged to familiarize themselves with recent changes in VA eligibility policies and to revisit strategies, policies, and procedures surrounding the engagement and enrollment of veterans with OTH discharge characterizations. Doing so may ensure veterans with OTH discharges are effectively connected to needed behavioral health care services.
In April 2022, the US Department of Veterans Affairs (VA) revised its behavioral health care eligibility policies to provide comprehensive mental and behavioral health care to former service members who received an Other Than Honorable (OTH) discharge characterization upon separation from military service.1 This policy shift represents a marked expansion in eligibility practices (Table 1 includes amended eligibility criteria).
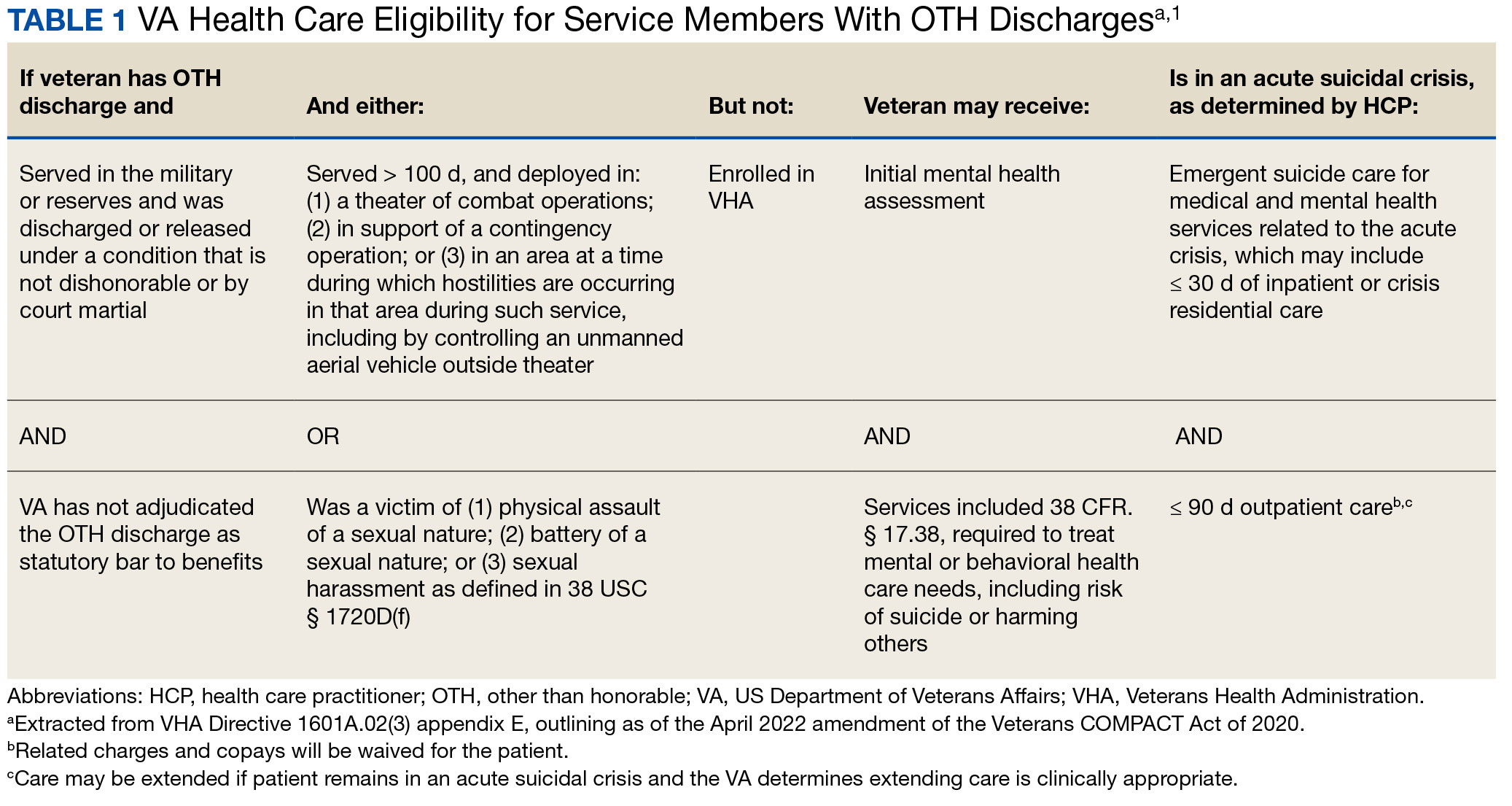
Since June 2017, eligibility policies allowed veterans with OTH discharges to receive “emergent mental health services” needed to stabilize acute mental health crises related to military service (eg, acute escalations in suicide risk).2,3 Previously, veterans with OTH discharges were largely ineligible for VA-based health care; these individuals were only able to access Veterans Health Administration (VHA) mental and behavioral health care through limited channels of eligibility (eg, for treatment of military sexual trauma or psychosis or other mental illness within 2 years of discharge).4,5 The impetus for expansions in eligibility stemmed from VA efforts to reduce the suicide rate among veterans.6-8 Implications of such expansion extend beyond suicide prevention efforts, with notable promised effects on the care of veterans with criminal-legal involvement. This article highlights potential effects of recent eligibility expansions on veterans with criminal-legal involvement and makes specific recommendations for agencies and organizations serving these veterans.
OTHER THAN HONORABLE DISCHARGE
The US Department of Defense delineates 6 discharge characterizations provided to service members upon separation from military service: honorable, general under honorable conditions, OTH, bad conduct, dishonorable, and uncharacterized. Honorable discharge characterizations are considered to reflect general concordance between service member behavior and military standards; general discharge characterizations reflect some disparity between the service member’s behavior and military standards; OTH, bad conduct, and dishonorable discharge characterizations reflect serious disparities between the service member’s behavior and military standards; and uncharacterized discharge characterizations are given when other discharge characterizations are deemed inappropriate.9,10 OTH discharge characterizations are typically issued under instances of misconduct, fraudulent entry, security reasons, or in lieu of trial by court martial.9,10
Recent research suggests that about 85% of service members receive an honorable discharge characterization upon separation from military service, 8% receive general, 6% receive OTH, and 1% receive bad conduct or dishonorable discharges.11 In 2017, the VA estimated there were > 500,000 prior service members with OTH discharge characterizations, which has grown over time (1.9% during the Korean Conflict, 2.5% during the Vietnam War Era, 3.9% during the Cold War, 4.8% in the Persian Gulf War, and 5.8% in the post-9/11 era).7,11
The OTH discharge characterization is 1 of 3 less than honorable discharges informally referred to as bad papers (ie, OTH, bad conduct, or dishonorable). Former service members receiving these discharge characterizations face significant social stigma and structural discrimination upon military discharge, including significant hurdles to employment and educational pursuits as well as notable social alienation.12 Due to their discharge characterization, some are viewed as less deserving of the veteran title, and until recently, many did not qualify for the complex legal definition of veteran as established by the Congress.11,13 Veterans with OTH discharge characterizations have also historically been excluded from services (eg, VHA care),3 benefits (eg, disability compensation),14 and protections (eg, Uniformed Services Employment and Reemployment Rights Act)15 offered to veterans with honorable or general discharge characterizations. However, eligibility policies have gradually expanded, providing veterans with OTH discharges with access to VHA-based mental and behavioral health services and VA supportive housing assistance.1,3,16
Perhaps due to their historical exclusion from VA services, there is limited research available on the behavioral health and associated needs of veterans with OTH discharges. Some scholars argue that historical exclusions have exacerbated underlying difficulties faced by this population, thereby contributing to stark health and social disparities across discharge types.14,15,17 Studies with large veteran samples, for example, reflect notable demographic and behavioral health differences across discharge types. Compared to routinely discharged veterans, veterans with OTH discharges are significantly more likely to be younger, have lower income, use substances, have a history of criminal-legal involvement, and have mental and physical health difficulties.18,19
Substantial evidence also suggests a historical racial bias, with service members of color being disproportionately more likely to receive an OTH discharge.12 Similarly, across all branches of military service, Black service members are significantly more likely to face general or special court martial in military justice proceedings when compared with White service members.20 Service members from gender and sexual minorities are also disproportionately impacted by the OTH designation. Historically, many have been discharged with bad papers due to discriminatory policies, such as Don’t Ask Don’t Tell, which discriminated on the basis of sexual orientation between December 1993 and September 2011, and Directive-type Memorandum-19-004, which banned transgender persons from military service between April 2019 and January 2021.21,22
There is also significant mental health bias in the provision of OTH discharges, such that OTH characterizations are disproportionately represented among individuals with mental health disorders.18-20 Veterans discharged from military service due to behavioral misconduct are significantly more likely to meet diagnostic criteria for various behavioral health conditions and to experience homelessness, criminal-legal involvement, and suicidal ideation and behavior compared with routinely-discharged veterans.23-28
Consistent with their comparatively higher rates of criminal-legal involvement relative to routinely discharged veterans, veterans with OTH discharges are disproportionately represented in criminal justice settings. While veterans with OTH discharges represent only 6% of discharging service members and 2.5% of community-based veterans, they represent 10% of incarcerated veterans.11,18,23,29 Preliminary research suggests veterans with OTH discharges may be at higher risk for lifetime incarceration, though the association between OTH discharge and frequency of lifetime arrests remains unclear.18,30
VETERANS TREATMENT COURTS
Given the overrepresentation of veterans with OTH discharges in criminal-legal settings, consideration for this subset of the veteran population and its unique needs is commonplace among problem-solving courts that service veterans. First conceptualized in 2004, Veterans Treatment Courts (VTCs) are specialized problem-solving courts that divert veterans away from traditional judicial court and penal systems and into community-based supervision and treatment (most commonly behavioral health services).31-34 Although each VTC program is unique in structure, policies, and procedures, most VTCs can be characterized by certain key elements, including voluntary participation, plea requirements, delayed sentencing (often including reduced or dismissed charges), integration of military culture into court proceedings, a rehabilitative vs adversarial approach to decreasing risk of future criminal behavior, mandated treatment and supervision during participation, and use of veteran mentors to provide peer support.32-35 Eligibility requirements vary; however, many restrict participation to veterans with honorable discharge types and charges for nonviolent offenses.32,33,35-37
VTCs connect veterans within the criminal-legal system to needed behavioral health, community, and social services.31-33,37 VTC participants are commonly connected to case management, behavioral health care, therapeutic journaling programs, and vocational rehabilitation.38,39 Accordingly, the most common difficulties faced by veterans participating in these courts include substance use, mental health, family issues, anger management and/or aggressive behavior, and homelessness.36,39 There is limited research on the effectiveness of VTCs. Evidence on their overall effectiveness is largely mixed, though some studies suggest VTC graduates tend to have lower recidivism rates than offenders more broadly or persons who terminate VTC programs prior to completion.40,41 Other studies suggest that VTC participants are more likely to have jail sanctions, new arrests, and new incarcerations relative to nontreatment court participants.42 Notably, experimental designs (considered the gold standard in assessing effectiveness) to date have not been applied to evaluate the effectiveness of VTCs; as such, the effectiveness of these programs remains an area in need of continued empirical investigation.
Like all problem-solving courts, VTCs occasionally struggle to connect participating defendants with appropriate care, particularly when encountering structural barriers (eg, insurance, transportation) and/or complex behavioral health needs (eg, personality disorders).34,43 As suicide rates among veterans experiencing criminal-legal involvement surge (about 150 per 100,000 in 2021, a 10% increase from 2020 to 2021 compared to about 40 per 100,000 and a 1.8% increase among other veterans), efficiency of adequate care coordination is vital.44 Many VTCs rely on VTC-VA partnerships and collaborations to navigate these difficulties and facilitate connection of participating veterans to needed services.32-34,45 For example, within the VHA, Veterans Justice Outreach (VJO) and Health Care for Re-Entry Veterans (HCRV) specialists assist and bridge the gap between the criminal-legal system (including, but not limited to VTCs) and VA services by engaging veterans involved in the criminal-legal system and connecting them to needed VA-based services (Table 2). Generally, VJO specialists support veterans involved with the front end of the criminallegal system (eg, arrest, pretrial incarceration, or participation in VTCs), while HCRV specialists tend to support veterans transitioning back into the community after a period of incarceration.46,47 Specific to VTCs, VJO specialists typically serve as liaisons between the courts and VA, coordinating VA services for defendants to fulfill their terms of VTC participation.46
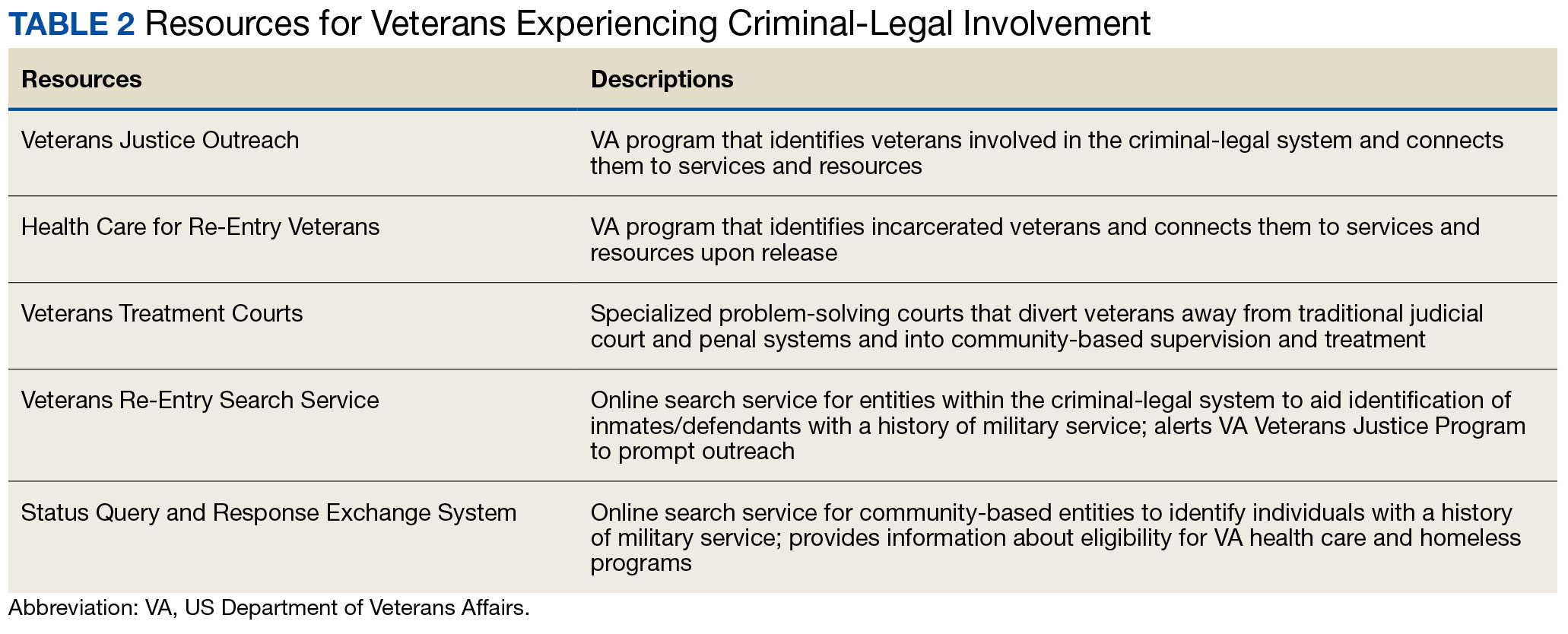
The historical exclusion of veterans with OTH discharge characterizations from VA-based services has restricted many from accessing VTC programs.32 Of 17 VTC programs active in Pennsylvania in 2014, only 5 accepted veterans with OTstayH discharges, and 3 required application to and eligibility for VA benefits.33 Similarly, in national surveys of VTC programs, about 1 in 3 report excluding veterans deemed ineligible for VA services.35,36 When veterans with OTH discharges have accessed VTC programs, they have historically relied on non-VA, community-based programming to fulfill treatment mandates, which may be less suited to addressing the unique needs of veterans.48
Veterans who utilize VTCs receive several benefits, namely peer support and mentorship, acceptance into a veteran-centric space, and connection with specially trained staff capable of supporting the veteran through applications for a range of VA benefits (eg, service connection, housing support).31-33,37 Given the disparate prevalence of OTH discharge characterizations among service members from racial, sexual, and gender minorities and among service members with mental health disorders, exclusion of veterans with OTH discharges from VTCs solely based on the type of discharge likely contributes to structural inequities among these already underserved groups by restricting access to these potential benefits. Such structural inequity stands in direct conflict with VTC best practice standards, which admonish programs to adjust eligibility requirements to facilitate access to treatment court programs for historically marginalized groups.49
ELIGIBILITY EXPANSIONS
Given the overrepresentation of veterans with OTH discharge characterizations within the criminal-legal system and historical barriers of these veterans to access needed mental and behavioral health care, expansions in VA eligibility policies could have immense implications for VTCs. First, these expansions could mitigate common barriers to connecting VTC-participating veterans with OTH discharges with needed behavioral health care by allowing these veterans to access established, VA-based services and programming. Expansion may also allow VTCs to serve as a key intercept point for identifying and engaging veterans with OTH discharges who may be unaware of their eligibility for VA-based behavioral health care.
Access to VA health care services is a major resource for VTC participants and a common requirement.32 Eligibility expansion should ease access barriers veterans with OTH discharges commonly face. By providing a potential source of treatment, expansions may also support OTH eligibility practices within VTCs, particularly practices that require participants to be eligible for VA health care.33,35,36 Some VTCs may continue to determine eligibility on the basis of discharge status and remain inaccessible to veterans with OTH discharge characterizations without program-level policy changes.32,36,37
Communicating changes in eligibility policies relevant to veterans with OTH discharges may be a challenge, because many of these individuals have no established channels of communication with the VA. Because veterans with OTH discharges are at increased risk for legal system involvement, VTCs may serve as a unique point of contact to help facilitate communication.18 For example, upon referral to a VTC, veterans with OTH discharges can be identified, VA health care eligibility can be verified, and veterans can connect to VA staff to facilitate enrollment in VA services and care.
VJO specialists are in a favorable position to serve a critical role in utilizing VTCs as a potential intercept point for engaging veterans with OTH discharge characterizations. As outlined in the STRONG Veterans Act of 2022, VJOs are mandated to “spread awareness and understanding of veteran eligibility for the [VJO] Program, including the eligibility of veterans who were discharged from service in the Armed Forces under conditions other than honorable.”50 The Act further requires VJOs to be annually trained in communicating eligibility changes as they arise. Accordingly, VJOs receive ongoing training in a wide variety of critical outreach topics, including changes in eligibility; while VJOs cannot make eligibility determinations, they are tasked with enrolling all veterans involved in the criminal-legal system with whom they interact into VHA services, whether through typical or special eligibility criteria (M. Stimmel, PhD, National Training Director for Veteran Justice Programming, oral communication, July 14, 2023). VJOs therefore routinely serve in this capacity of facilitating VA enrollment of veterans with OTH discharge characterizations.
Recommendations to Veteran-Servicing Judicial Programs
Considering these potential implications, professionals routinely interacting with veterans involved in the criminal-legal system should become familiarized with recent changes in VA eligibility policies. Such familiarization would support the identification of veterans previously considered ineligible for care; provision of education to these veterans regarding their new eligibility; and referral to appropriate VA-based behavioral health care options. Although conceptually simple, executing such an educational campaign may prove logistically difficult. Given their historical exclusion from VA services, veterans with OTH discharge characterizations are unlikely to seek VA-based services in times of need, instead relying on a broad swath of civilian community-based organizations and resources. Usual approaches to advertising VHA health care policy changes (eg, by notifying VA employees and/or departments providing corresponding services or by circulating information to veteran-focused mailing lists and organizations) likely would prove insufficient. Educational campaigns to disseminate information about recent OTH eligibility changes should instead consider partnering with traditionally civilian, communitybased organizations and institutions, such as state bar associations, legal aid networks, case management services, nonveteran treatment court programs (eg, drug courts, or domestic violence courts), or probation/ parole programs. Because national surveys suggest generally low military cultural competence among civilian populations, providing concurrent support in developing foundational veteran cultural competencies (eg, how to phrase questions about military service history, or understanding discharge characterizations) may be necessary to ensure effective identification and engagement of veteran clients.48
Programs that serve veterans with criminal-legal involvement should also consider potential relevance of recent OTH eligibility changes to program operations. VTC program staff and key partners (eg, judges, case managers, district attorneys, or defense attorneys), should revisit policies and procedures surrounding the engagement of veterans with OTH discharges within VTC programs and strategies for connecting these veterans with needed services. VTC programs that have historically excluded veterans with OTH discharges due to associated difficulties in locating and connecting with needed services should consider expanding eligibility policies considering recent shifts in VA behavioral health care eligibility.33,35,36 Within the VHA, VJO specialists can play a critical role in supporting these VTC eligibility and cultural shifts. Some evidence suggests a large proportion of VTC referrals are facilitated by VJO specialists and that many such referrals are identified when veterans involved with the criminal-legal system seek VA support and/or services.33 Given the historical exclusion of veterans with OTH discharges from VA care, strategies used by VJO specialists to identify, connect, and engage veterans with OTH discharges with VTCs and other services may be beneficial.
Even with knowledge of VA eligibility changes and considerations of these changes on local operations, many forensic settings and programs struggle to identify veterans. These difficulties are likely amplified among veterans with OTH discharge characterizations, who may be hesitant to self-disclose their military service history due to fear of stigma and/or views of OTH discharge characterizations as undeserving of the veteran title.12 The VA offers 2 tools to aid in identification of veterans for these settings: the Veterans Re-Entry Search Service (VRSS) and Status Query and Response Exchange System (SQUARES). For VRSS, correctional facilities, courts, and other criminal justice entities upload a simple spreadsheet that contains basic identifying information of inmates or defendants in their system. VRSS returns information about which inmates or defendants have a history of military service and alerts VA Veterans Justice Programs staff so they can conduct outreach. A pilot study conducted by the California Department of Corrections and Rehabilitation found that 2.7% of its inmate population self-identified as veterans, while VRSS identified 7.7% of inmates with a history of military service. This difference represented about 5000 previously unidentified veterans.51 Similarly, community entities that partner with the VA, such as law enforcement or homeless service programs, can be approved to become a SQUARES user and submit identifying information of individuals with whom they interact directly into the SQUARES search engine. SQUARES then directly returns information about the individual’s veteran status and eligibility for VA health care and homeless programs.
Other Eligibility Limitations
VTCs and other professionals looking to refer veterans with OTH discharge characterizations to VA-based behavioral health care should be aware of potential limitations in eligibility and access. Specifically, although veterans with OTH discharges are now broadly eligible for VA-based behavioral health care and homeless programs, they remain ineligible for other forms of health care, including primary care and nonbehavioral specialty care.1 Research has found a strong comorbidity between behavioral and nonbehavioral health concerns, particularly within historically marginalized demographic groups.52-55 Because these historically marginalized groups are often overrepresented among persons with criminal-legal involvement, veterans with OTH discharges, and VTC participants, such comorbidities require consideration by services or programming designed to support veterans with criminal-legal involvement.12,56-58 Connection with VA-based health care will therefore continue to fall short of addressing all health care needs of veterans with OTH discharges and effective case management will require considerable treatment coordination between VA behavioral health care practitioners (HCPs) and community-based HCPs (eg, primary care professionals or nonbehavioral HCPs).
Implications for VA Mental Health Care
Recent eligibility expansions will also have inevitable consequences for VA mental health care systems. For many years, these systems have been overburdened by high caseloads and clinician burnout.59,60 Given the generally elevated rates of mental health and substance use concerns among veterans with OTH discharge characterizations, expansions hold the potential to further burden caseloads with clinically complex, high-risk, high-need clients. Nevertheless, these expansions are also structured in a way that forces existing systems to absorb the responsibilities of providing necessary care to these veterans. To mitigate detrimental effects of eligibility expansions on the broader VA mental health system, clinicians should be explicitly trained in identifying veterans with OTH discharge characterizations and the implications of discharge status on broader health care eligibility. Treatment of veterans with OTH discharges may also benefit from close coordination between mental health professionals and behavioral health care coordinators to ensure appropriate coordination of care between VA- and non–VA-based HCPs.
CONCLUSIONS
Recent changes to VA eligibility policies now allow comprehensive mental and behavioral health care services to be provided to veterans with OTH discharges.1 Compared to routinely discharged veterans, veterans with OTH discharges are more likely to be persons of color, sexual or gender minorities, and experiencing mental health-related difficulties. Given the disproportionate mental health burden often faced by veterans with OTH discharges and relative overrepresentation of these veterans in judicial and correctional systems, these changes have considerable implications for programs and services designed to support veterans with criminallegal involvement. Professionals within these systems, particularly VTC programs, are therefore encouraged to familiarize themselves with recent changes in VA eligibility policies and to revisit strategies, policies, and procedures surrounding the engagement and enrollment of veterans with OTH discharge characterizations. Doing so may ensure veterans with OTH discharges are effectively connected to needed behavioral health care services.
- US Department of Veterans, Veterans Health Administration. VHA Directive 1601A.02(6): Eligibility Determination. Updated March 6, 2024. Accessed August 8, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8908
- Mental and behavioral health care for certain former members of the Armed Forces. 38 USC §1720I (2018). Accessed August 5, 2024. https://uscode.house.gov/view.xhtml?req=(title:38%20section:1720I%20edition:prelim
- US Department of Veterans, Veterans Health Administration. VHA Directive 1601A.02, Eligibility Determination. June 7, 2017.
- US Department of Veterans, Veterans Health Administration. VHA Directive 1115(1), Military Sexual Trauma (MST) Program. May 8, 2018. Accessed August 5, 2024. https:// www.va.gov/vhapublications/viewpublication.asp?pub_ID=6402
- US Department of Veterans Affairs. Tentative Eligibility Determinations; Presumptive Eligibility for Psychosis and Other Mental Illness. 38 CFR §17.109. May 14, 2013. Accessed August 5, 2024. https://www.federalregister.gov/documents/2013/05/14/2013-11410/tentative-eligibility-determinations-presumptive-eligibility-for-psychosis-and-other-mental-illness
- US Department of Veterans Affairs, VA Office of Mental Health and Suicide Prevention. National strategy for preventing veteran suicide 2018-2028. Published September 2018. Accessed August 5, 2024. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf
- US Department of Veterans Affairs. VA secretary announces intention to expand mental health care to former service members with other-than-honorable discharges and in crisis. Press Release. March 8, 2017. Accessed August 5, 2024. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=2867
- Smith C. Dramatic increase in mental health services to other-than-honorable discharge veterans. VA News. February 23, 2022. Accessed August 5, 2024. https://news.va.gov/100460/dramatic-increase-in-mental-health-services-to-other-than-honorable-discharge-veterans/
- US Department of Defense. DoD Instruction 1332.14. Enlisted administrative separations. Updated August 1, 2024. Accessed August 5, 2024. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133214p.pdf
- US Department of Defense. DoD Instruction 1332.30. Commissioned officer administrative separations. Updated September 9, 2021. Accessed August 5, 2024. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133230p.pdf
- OUTVETS, Legal Services Center of Harvard Law School, Veterans Legal Services. Turned away: how the VA unlawfully denies healthcare to veterans with bad paper discharges. 2020. Accessed August 5, 2024. https://legalservicescenter.org/wp-content/uploads/Turn-Away-Report.pdf
- McClean H. Discharged and discarded: the collateral consequences of a less-than-honorable military discharge. Columbia Law Rev. 2021;121(7):2203-2268.
- Veterans Benefits, General Provisions, Definitions. 38 USC §101(2) (1958). Accessed August 5, 2024. https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title38-section101&num=0&edition=prelim
- Bedford JR. Other than honorable discharges: unfair and unjust life sentences of decreased earning capacity. U Penn J Law Pub Affairs. 2021;6(4):687.
- Karin ML. Other than honorable discrimination. Case Western Reserve Law Rev. 2016;67(1):135-191. https://scholarlycommons.law.case.edu/caselrev/vol67/iss1/9
- Veteran HOUSE Act of 2020, HR 2398, 116th Cong, (2020). Accessed August 5, 2024. https://www.congress.gov/bill/116th-congress/house-bill/2398
- Scapardine D. Leaving other than honorable soldiers behind: how the Departments of Defense and Veterans Affairs inadvertently created a health and social crisis. Md Law Rev. 2017;76(4):1133-1165.
- Elbogen EB, Wagner HR, Brancu M, et al. Psychosocial risk factors and other than honorable military discharge: providing healthcare to previously ineligible veterans. Mil Med. 2018;183(9-10):e532-e538. doi:10.1093/milmed/usx128
- Tsai J, Rosenheck RA. Characteristics and health needs of veterans with other-than-honorable discharges: expanding eligibility in the Veterans Health Administration. Mil Med. 2018;183(5-6):e153-e157. doi:10.1093/milmed/usx110
- Christensen DM, Tsilker Y. Racial disparities in military justice: findings of substantial and persistent racial disparities within the United States military justice system. Accessed August 5, 2024. https://www.protectourdefenders.com/wp-content/uploads/2017/05/Report_20.pdf
- Don’t Ask Don’t Tell, 10 USC §654 (1993) (Repealed 2010). Accessed August 5, 2024. http://www.gpo.gov/fdsys/pkg/USCODE-2010-title10/pdf/USCODE-2010-title10-subtitleA-partII-chap37-sec654.pdf
- Palm Center. The making of a ban: how DTM-19-004 works to push transgender people out of military service. 2019. March 20, 2019. Accessed August 5, 2024. https://www.palmcenter.org/wp-content/uploads/2019/04/The-Making-of-a-Ban.pdf
- Edwards ER, Greene AL, Epshteyn G, Gromatsky M, Kinney AR, Holliday R. Mental health of incarcerated veterans and civilians: latent class analysis of the 2016 Survey of Prison Inmates. Crim Justice Behav. 2022;49(12):1800- 1821. doi:10.1177/00938548221121142
- Brignone E, Fargo JD, Blais RK, Carter ME, Samore MH, Gundlapalli AV. Non-routine discharge from military service: mental illness, substance use disorders, and suicidality. Am J Prev Med. 2017;52(5):557-565. doi:10.1016/j.amepre.2016.11.015
- Gamache G, Rosenheck R, Tessler R. Military discharge status of homeless veterans with mental illness. Mil Med. 2000;165(11):803-808. doi:10.1093/milmed/165.11.803
- Gundlapalli AV, Fargo JD, Metraux S, et al. Military Misconduct and Homelessness Among US Veterans Separated From Active Duty, 2001-2012. JAMA. 2015;314(8):832-834. doi:10.1001/jama.2015.8207
- Brooks Holliday S, Pedersen ER. The association between discharge status, mental health, and substance misuse among young adult veterans. Psychiatry Res. 2017;256:428-434. doi:10.1016/j.psychres.2017.07.011
- Williamson RB. DOD Health: Actions Needed to Ensure Post-Traumatic Stress Disorder and Traumatic Brain Injury are Considered in Misconduct Separations. US Government Accountability Office; 2017. Accessed August 5, 2024. https://apps.dtic.mil/sti/pdfs/AD1168610.pdf
- Maruschak LM, Bronson J, Alper M. Indicators of mental health problems reported by prisoners: survey of prison inmates. US Department of Justice Bureau of Justice Statistics. June 2021. Accessed August 5, 2024. https://bjs.ojp.gov/sites/g/files/xyckuh236/files/media/document/imhprpspi16st.pdf
- Brooke E, Gau J. Military service and lifetime arrests: examining the effects of the total military experience on arrests in a sample of prison inmates. Crim Justice Policy Rev. 2018;29(1):24-44. doi:10.1177/0887403415619007
- Russell RT. Veterans treatment court: a proactive approach. N Engl J Crim Civ Confin. 2009;35:357-372.
- Cartwright T. To care for him who shall have borne the battle: the recent development of Veterans Treatment Courts in America. Stanford Law Pol Rev. 2011;22:295-316.
- Douds AS, Ahlin EM, Howard D, Stigerwalt S. Varieties of veterans’ courts: a statewide assessment of veterans’ treatment court components. Crim Justice Policy Rev. 2017;28:740-769. doi:10.1177/0887403415620633
- Rowen J. Worthy of justice: a veterans treatment court in practice. Law Policy. 2020;42(1):78-100. doi:10.1111/lapo.12142
- Timko C, Flatley B, Tjemsland A, et al. A longitudinal examination of veterans treatment courts’ characteristics and eligibility criteria. Justice Res Policy. 2016;17(2):123-136.
- Baldwin JM. Executive summary: national survey of veterans treatment courts. SSRN. Preprint posted online June 5, 2013. Accessed August 5, 2024. doi:10.2139/ssrn.2274138
- Renz T. Veterans treatment court: a hand up rather than lock up. Richmond Public Interest Law Rev. 2013;17(3):697-705. https://scholarship.richmond.edu/pilr/vol17/iss3/6
- Knudsen KJ, Wingenfeld S. A specialized treatment court for veterans with trauma exposure: implications for the field. Community Ment Health J. 2016;52(2):127-135. doi:10.1007/s10597-015-9845-9
- McCall JD, Tsai J, Gordon AJ. Veterans treatment court research: participant characteristics, outcomes, and gaps in the literature. J Offender Rehabil. 2018;57:384-401. doi:10.1080/10509674.2018.1510864
- Smith JS. The Anchorage, Alaska veterans court and recidivism: July 6, 2004 – December 31, 2010. Alsk Law Rev. 2012;29(1):93-111.
- Hartley RD, Baldwin JM. Waging war on recidivism among justice-involved veterans: an impact evaluation of a large urban veterans treatment court. Crim Justice Policy Rev. 2019;30(1):52-78. doi:10.1177/0887403416650490
- Tsai J, Flatley B, Kasprow WJ, Clark S, Finlay A. Diversion of veterans with criminal justice involvement to treatment courts: participant characteristics and outcomes. Psychiatr Serv. 2017;68(4):375-383. doi:10.1176/appi.ps.201600233
- Edwards ER, Sissoko DR, Abrams D, Samost D, La Gamma S, Geraci J. Connecting mental health court participants with services: process, challenges, and recommendations. Psychol Public Policy Law. 2020;26(4):463-475. doi:10.1037/law0000236
- US Department of Veterans Affairs, VA Office of Mental Health and Suicide Prevention. 2023 National Veteran Suicide Prevention Annual Report. US Department of Veterans Affairs; November 2023. Accessed August 5, 2024. https://www.mentalhealth.va.gov/docs/data-sheets/2023/2023-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-508.pdf
- Finlay AK, Clark S, Blue-Howells J, et al. Logic model of the Department of Veterans Affairs’ role in veterans treatment courts. Drug Court Rev. 2019;2:45-62.
- Finlay AK, Smelson D, Sawh L, et al. U.S. Department of Veterans Affairs veterans justice outreach program: connecting justice-involved veterans with mental health and substance use disorder treatment. Crim Justice Policy Rev. 2016;27(2):10.1177/0887403414562601. doi:10.1177/0887403414562601
- Finlay AK, Stimmel M, Blue-Howells J, et al. Use of Veterans Health Administration mental health and substance use disorder treatment after exiting prison: the health care for reentry veterans program. Adm Policy Ment Health. 2017;44(2):177-187. doi:10.1007/s10488-015-0708-z
- Meyer EG, Writer BW, Brim W. The Importance of Military Cultural Competence. Curr Psychiatry Rep. 2016;18(3):26. doi:10.1007/s11920-016-0662-9
- National Association of Drug Court Professionals. Adult Drug Court Best Practice Standards Volume I. National Association of Drug Court Professionals; 2013. Accessed August 5, 2024. https://allrise.org/publications/standards/
- STRONG Veterans Act of 2022, HR 6411, 117th Cong (2022). https://www.congress.gov/bill/117th-congress/house-bill/6411/text
- Pelletier D, Clark S, Davis L. Veterans reentry search service (VRSS) and the SQUARES application. Presented at: National Association of Drug Court Professionals Conference; August 15-18, 2021; National Harbor, Maryland.
- Scott KM, Lim C, Al-Hamzawi A, et al. Association of Mental Disorders With Subsequent Chronic Physical Conditions: World Mental Health Surveys From 17 Countries. JAMA Psychiatry. 2016;73(2):150-158. doi:10.1001/jamapsychiatry.2015.2688
- Ahmed N, Conway CA. Medical and mental health comorbidities among minority racial/ethnic groups in the United States. J Soc Beh Health Sci. 2020;14(1):153-168. doi:10.5590/JSBHS.2020.14.1.11
- Hanna B, Desai R, Parekh T, Guirguis E, Kumar G, Sachdeva R. Psychiatric disorders in the U.S. transgender population. Ann Epidemiol. 2019;39:1-7.e1. doi:10.1016/j.annepidem.2019.09.009
- Watkins DC, Assari S, Johnson-Lawrence V. Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder, and chronic medical conditions. J Racial Ethn Health Disparities. 2015;2(3):385- 394. doi:10.1007/s40615-015-0085-z
- Baldwin J. Whom do they serve? National examination of veterans treatment court participants and their challenges. Crim Justice Policy Rev. 2017;28(6):515-554. doi:10.1177/0887403415606184
- Beatty LG, Snell TL. Profile of prison inmates, 2016. US Department of Justice Bureau of Justice Statistics. December 2021. Accessed August 5, 2024. https://bjs.ojp.gov/content/pub/pdf/ppi16.pdf
- Al-Rousan T, Rubenstein L, Sieleni B, Deol H, Wallace RB. Inside the nation’s largest mental health institution: a prevalence study in a state prison system. BMC Public Health. 2017;17(1):342. doi:10.1186/s12889-017-4257-0
- Rosen CS, Kaplan AN, Nelson DB, et al. Implementation context and burnout among Department of Veterans Affairs psychotherapists prior to and during the COVID-19 pandemic. J Affect Disord. 2023;320:517-524. doi:10.1016/j.jad.2022.09.141
- Tsai J, Jones N, Klee A, Deegan D. Job burnout among mental health staff at a veterans affairs psychosocial rehabilitation center. Community Ment Health J. 2020;56(2):294- 297. doi:10.1007/s10597-019-00487-5
- US Department of Veterans, Veterans Health Administration. VHA Directive 1601A.02(6): Eligibility Determination. Updated March 6, 2024. Accessed August 8, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=8908
- Mental and behavioral health care for certain former members of the Armed Forces. 38 USC §1720I (2018). Accessed August 5, 2024. https://uscode.house.gov/view.xhtml?req=(title:38%20section:1720I%20edition:prelim
- US Department of Veterans, Veterans Health Administration. VHA Directive 1601A.02, Eligibility Determination. June 7, 2017.
- US Department of Veterans, Veterans Health Administration. VHA Directive 1115(1), Military Sexual Trauma (MST) Program. May 8, 2018. Accessed August 5, 2024. https:// www.va.gov/vhapublications/viewpublication.asp?pub_ID=6402
- US Department of Veterans Affairs. Tentative Eligibility Determinations; Presumptive Eligibility for Psychosis and Other Mental Illness. 38 CFR §17.109. May 14, 2013. Accessed August 5, 2024. https://www.federalregister.gov/documents/2013/05/14/2013-11410/tentative-eligibility-determinations-presumptive-eligibility-for-psychosis-and-other-mental-illness
- US Department of Veterans Affairs, VA Office of Mental Health and Suicide Prevention. National strategy for preventing veteran suicide 2018-2028. Published September 2018. Accessed August 5, 2024. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf
- US Department of Veterans Affairs. VA secretary announces intention to expand mental health care to former service members with other-than-honorable discharges and in crisis. Press Release. March 8, 2017. Accessed August 5, 2024. https://www.va.gov/opa/pressrel/pressrelease.cfm?id=2867
- Smith C. Dramatic increase in mental health services to other-than-honorable discharge veterans. VA News. February 23, 2022. Accessed August 5, 2024. https://news.va.gov/100460/dramatic-increase-in-mental-health-services-to-other-than-honorable-discharge-veterans/
- US Department of Defense. DoD Instruction 1332.14. Enlisted administrative separations. Updated August 1, 2024. Accessed August 5, 2024. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133214p.pdf
- US Department of Defense. DoD Instruction 1332.30. Commissioned officer administrative separations. Updated September 9, 2021. Accessed August 5, 2024. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133230p.pdf
- OUTVETS, Legal Services Center of Harvard Law School, Veterans Legal Services. Turned away: how the VA unlawfully denies healthcare to veterans with bad paper discharges. 2020. Accessed August 5, 2024. https://legalservicescenter.org/wp-content/uploads/Turn-Away-Report.pdf
- McClean H. Discharged and discarded: the collateral consequences of a less-than-honorable military discharge. Columbia Law Rev. 2021;121(7):2203-2268.
- Veterans Benefits, General Provisions, Definitions. 38 USC §101(2) (1958). Accessed August 5, 2024. https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title38-section101&num=0&edition=prelim
- Bedford JR. Other than honorable discharges: unfair and unjust life sentences of decreased earning capacity. U Penn J Law Pub Affairs. 2021;6(4):687.
- Karin ML. Other than honorable discrimination. Case Western Reserve Law Rev. 2016;67(1):135-191. https://scholarlycommons.law.case.edu/caselrev/vol67/iss1/9
- Veteran HOUSE Act of 2020, HR 2398, 116th Cong, (2020). Accessed August 5, 2024. https://www.congress.gov/bill/116th-congress/house-bill/2398
- Scapardine D. Leaving other than honorable soldiers behind: how the Departments of Defense and Veterans Affairs inadvertently created a health and social crisis. Md Law Rev. 2017;76(4):1133-1165.
- Elbogen EB, Wagner HR, Brancu M, et al. Psychosocial risk factors and other than honorable military discharge: providing healthcare to previously ineligible veterans. Mil Med. 2018;183(9-10):e532-e538. doi:10.1093/milmed/usx128
- Tsai J, Rosenheck RA. Characteristics and health needs of veterans with other-than-honorable discharges: expanding eligibility in the Veterans Health Administration. Mil Med. 2018;183(5-6):e153-e157. doi:10.1093/milmed/usx110
- Christensen DM, Tsilker Y. Racial disparities in military justice: findings of substantial and persistent racial disparities within the United States military justice system. Accessed August 5, 2024. https://www.protectourdefenders.com/wp-content/uploads/2017/05/Report_20.pdf
- Don’t Ask Don’t Tell, 10 USC §654 (1993) (Repealed 2010). Accessed August 5, 2024. http://www.gpo.gov/fdsys/pkg/USCODE-2010-title10/pdf/USCODE-2010-title10-subtitleA-partII-chap37-sec654.pdf
- Palm Center. The making of a ban: how DTM-19-004 works to push transgender people out of military service. 2019. March 20, 2019. Accessed August 5, 2024. https://www.palmcenter.org/wp-content/uploads/2019/04/The-Making-of-a-Ban.pdf
- Edwards ER, Greene AL, Epshteyn G, Gromatsky M, Kinney AR, Holliday R. Mental health of incarcerated veterans and civilians: latent class analysis of the 2016 Survey of Prison Inmates. Crim Justice Behav. 2022;49(12):1800- 1821. doi:10.1177/00938548221121142
- Brignone E, Fargo JD, Blais RK, Carter ME, Samore MH, Gundlapalli AV. Non-routine discharge from military service: mental illness, substance use disorders, and suicidality. Am J Prev Med. 2017;52(5):557-565. doi:10.1016/j.amepre.2016.11.015
- Gamache G, Rosenheck R, Tessler R. Military discharge status of homeless veterans with mental illness. Mil Med. 2000;165(11):803-808. doi:10.1093/milmed/165.11.803
- Gundlapalli AV, Fargo JD, Metraux S, et al. Military Misconduct and Homelessness Among US Veterans Separated From Active Duty, 2001-2012. JAMA. 2015;314(8):832-834. doi:10.1001/jama.2015.8207
- Brooks Holliday S, Pedersen ER. The association between discharge status, mental health, and substance misuse among young adult veterans. Psychiatry Res. 2017;256:428-434. doi:10.1016/j.psychres.2017.07.011
- Williamson RB. DOD Health: Actions Needed to Ensure Post-Traumatic Stress Disorder and Traumatic Brain Injury are Considered in Misconduct Separations. US Government Accountability Office; 2017. Accessed August 5, 2024. https://apps.dtic.mil/sti/pdfs/AD1168610.pdf
- Maruschak LM, Bronson J, Alper M. Indicators of mental health problems reported by prisoners: survey of prison inmates. US Department of Justice Bureau of Justice Statistics. June 2021. Accessed August 5, 2024. https://bjs.ojp.gov/sites/g/files/xyckuh236/files/media/document/imhprpspi16st.pdf
- Brooke E, Gau J. Military service and lifetime arrests: examining the effects of the total military experience on arrests in a sample of prison inmates. Crim Justice Policy Rev. 2018;29(1):24-44. doi:10.1177/0887403415619007
- Russell RT. Veterans treatment court: a proactive approach. N Engl J Crim Civ Confin. 2009;35:357-372.
- Cartwright T. To care for him who shall have borne the battle: the recent development of Veterans Treatment Courts in America. Stanford Law Pol Rev. 2011;22:295-316.
- Douds AS, Ahlin EM, Howard D, Stigerwalt S. Varieties of veterans’ courts: a statewide assessment of veterans’ treatment court components. Crim Justice Policy Rev. 2017;28:740-769. doi:10.1177/0887403415620633
- Rowen J. Worthy of justice: a veterans treatment court in practice. Law Policy. 2020;42(1):78-100. doi:10.1111/lapo.12142
- Timko C, Flatley B, Tjemsland A, et al. A longitudinal examination of veterans treatment courts’ characteristics and eligibility criteria. Justice Res Policy. 2016;17(2):123-136.
- Baldwin JM. Executive summary: national survey of veterans treatment courts. SSRN. Preprint posted online June 5, 2013. Accessed August 5, 2024. doi:10.2139/ssrn.2274138
- Renz T. Veterans treatment court: a hand up rather than lock up. Richmond Public Interest Law Rev. 2013;17(3):697-705. https://scholarship.richmond.edu/pilr/vol17/iss3/6
- Knudsen KJ, Wingenfeld S. A specialized treatment court for veterans with trauma exposure: implications for the field. Community Ment Health J. 2016;52(2):127-135. doi:10.1007/s10597-015-9845-9
- McCall JD, Tsai J, Gordon AJ. Veterans treatment court research: participant characteristics, outcomes, and gaps in the literature. J Offender Rehabil. 2018;57:384-401. doi:10.1080/10509674.2018.1510864
- Smith JS. The Anchorage, Alaska veterans court and recidivism: July 6, 2004 – December 31, 2010. Alsk Law Rev. 2012;29(1):93-111.
- Hartley RD, Baldwin JM. Waging war on recidivism among justice-involved veterans: an impact evaluation of a large urban veterans treatment court. Crim Justice Policy Rev. 2019;30(1):52-78. doi:10.1177/0887403416650490
- Tsai J, Flatley B, Kasprow WJ, Clark S, Finlay A. Diversion of veterans with criminal justice involvement to treatment courts: participant characteristics and outcomes. Psychiatr Serv. 2017;68(4):375-383. doi:10.1176/appi.ps.201600233
- Edwards ER, Sissoko DR, Abrams D, Samost D, La Gamma S, Geraci J. Connecting mental health court participants with services: process, challenges, and recommendations. Psychol Public Policy Law. 2020;26(4):463-475. doi:10.1037/law0000236
- US Department of Veterans Affairs, VA Office of Mental Health and Suicide Prevention. 2023 National Veteran Suicide Prevention Annual Report. US Department of Veterans Affairs; November 2023. Accessed August 5, 2024. https://www.mentalhealth.va.gov/docs/data-sheets/2023/2023-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-508.pdf
- Finlay AK, Clark S, Blue-Howells J, et al. Logic model of the Department of Veterans Affairs’ role in veterans treatment courts. Drug Court Rev. 2019;2:45-62.
- Finlay AK, Smelson D, Sawh L, et al. U.S. Department of Veterans Affairs veterans justice outreach program: connecting justice-involved veterans with mental health and substance use disorder treatment. Crim Justice Policy Rev. 2016;27(2):10.1177/0887403414562601. doi:10.1177/0887403414562601
- Finlay AK, Stimmel M, Blue-Howells J, et al. Use of Veterans Health Administration mental health and substance use disorder treatment after exiting prison: the health care for reentry veterans program. Adm Policy Ment Health. 2017;44(2):177-187. doi:10.1007/s10488-015-0708-z
- Meyer EG, Writer BW, Brim W. The Importance of Military Cultural Competence. Curr Psychiatry Rep. 2016;18(3):26. doi:10.1007/s11920-016-0662-9
- National Association of Drug Court Professionals. Adult Drug Court Best Practice Standards Volume I. National Association of Drug Court Professionals; 2013. Accessed August 5, 2024. https://allrise.org/publications/standards/
- STRONG Veterans Act of 2022, HR 6411, 117th Cong (2022). https://www.congress.gov/bill/117th-congress/house-bill/6411/text
- Pelletier D, Clark S, Davis L. Veterans reentry search service (VRSS) and the SQUARES application. Presented at: National Association of Drug Court Professionals Conference; August 15-18, 2021; National Harbor, Maryland.
- Scott KM, Lim C, Al-Hamzawi A, et al. Association of Mental Disorders With Subsequent Chronic Physical Conditions: World Mental Health Surveys From 17 Countries. JAMA Psychiatry. 2016;73(2):150-158. doi:10.1001/jamapsychiatry.2015.2688
- Ahmed N, Conway CA. Medical and mental health comorbidities among minority racial/ethnic groups in the United States. J Soc Beh Health Sci. 2020;14(1):153-168. doi:10.5590/JSBHS.2020.14.1.11
- Hanna B, Desai R, Parekh T, Guirguis E, Kumar G, Sachdeva R. Psychiatric disorders in the U.S. transgender population. Ann Epidemiol. 2019;39:1-7.e1. doi:10.1016/j.annepidem.2019.09.009
- Watkins DC, Assari S, Johnson-Lawrence V. Race and ethnic group differences in comorbid major depressive disorder, generalized anxiety disorder, and chronic medical conditions. J Racial Ethn Health Disparities. 2015;2(3):385- 394. doi:10.1007/s40615-015-0085-z
- Baldwin J. Whom do they serve? National examination of veterans treatment court participants and their challenges. Crim Justice Policy Rev. 2017;28(6):515-554. doi:10.1177/0887403415606184
- Beatty LG, Snell TL. Profile of prison inmates, 2016. US Department of Justice Bureau of Justice Statistics. December 2021. Accessed August 5, 2024. https://bjs.ojp.gov/content/pub/pdf/ppi16.pdf
- Al-Rousan T, Rubenstein L, Sieleni B, Deol H, Wallace RB. Inside the nation’s largest mental health institution: a prevalence study in a state prison system. BMC Public Health. 2017;17(1):342. doi:10.1186/s12889-017-4257-0
- Rosen CS, Kaplan AN, Nelson DB, et al. Implementation context and burnout among Department of Veterans Affairs psychotherapists prior to and during the COVID-19 pandemic. J Affect Disord. 2023;320:517-524. doi:10.1016/j.jad.2022.09.141
- Tsai J, Jones N, Klee A, Deegan D. Job burnout among mental health staff at a veterans affairs psychosocial rehabilitation center. Community Ment Health J. 2020;56(2):294- 297. doi:10.1007/s10597-019-00487-5
The Rebuilding of Military Medicine
It is the neglect of timely repair that makes rebuilding necessary.
Richard Whately, economist and theologian (1787-1863)
US Congressional inquiry and media attention are so frequently directed at the trials and tribulations of the US Department of Veterans Affairs (VA) that we forget the US Department of Defense (DoD) medical system also shares the federal practitioner space. The focus of the government and press recently has shifted to examine the weaknesses and woes of military medicine. This editorial reviews what that examination discovered about the decline of the DoD house of medicine, why it is in disrepair, proposals for its rebuilding, and reflects on what this trajectory can tell us about maintaining the structure of federal practice.
My father never tired of telling me that he and his medical colleagues returned from the Second World War with knowledge and skills gained in combat theaters that, in many respects, surpassed those of the civilian sector. Though he was biased as a career military physician and combat veteran, there is strong evidence backing the assertion that from World War I to Operations Enduring Freedom and Iraqi Freedom, American military medicine has been the glory of the world.1
A November 2023 report from the DoD Office of the Inspector General (OIG) warned that military medicine was in trouble. The report’s emphasis on access and staffing problems that endanger the availability and quality of health care services will likely strike a chord with VA clinicians. The document is based on data from OIG reports, hotline calls, and audits from the last several years; however, the OIG acknowledges that it did not conduct on-the-ground investigations to confirm the findings.2
When we hear the term military medicine, many immediately think of active duty service members. However, the patient population of DoD is far larger and more diverse. The Military Health System (MHS) provides care to > 9.5 million beneficiaries, including dependents and retirees, veterans, civilian DoD employees, and even contractors. Those who most heavily rely on the MHS are individuals in uniform and their families are experiencing the greatest difficulty with accessing care.3 This includes crucial mental health treatment at a time when rates of military suicide continue to climb.4
The lack of access and dearth of health care practitioners (HCPs) spans both military facilities and the civilian clinics and hospitals where current and former service members and their dependents use the TRICARE beneficiary insurance. Reminiscent of recent challenges at the VA, DoD members are encountering long wait times and the frustrating bureaucracy of inefficient and, at times, inept referral networks. Additionally, many institutions and HCPs will not accept TRICARE because it pays less and has more paperwork than other insurance plans. What is worse, there is currently no governmental leverage to compel them to participate.
The lack of access and dearth of health care practitioners (HCPs) spans both military facilities and the civilian clinics and hospitals where current and former service members and their dependents use the TRICARE beneficiary insurance. Reminiscent of recent challenges at the VA, DoD members are encountering long wait times and the frustrating bureaucracy of inefficient and, at times, inept referral networks. Additionally, many institutions and HCPs will not accept TRICARE because it pays less and has more paperwork than other insurance plans. What is worse, there is currently no governmental leverage to compel them to participate.
As with both the VA and civilian health care spheres, rural areas are the most impacted. Resource shortfalls adversely affect all aspects of care, especially the highly paid specialties like gastroenterology and urology, as well as primary care practitioners essential to ensure the health of military families. The deficits are widespread—all branches report similar obstacles to providing responsive, appropriate care. As if this was not enough to complete the mirror image of the VA’s struggles, there is a rising tide of complaints about the military’s electronic health record system.5 How did the preeminent MHS so rapidly decay? Experts in and out of uniform offer several explanations.
As with most forms of managed care, the need to cut costs drove the Pentagon to send military members and dependents to civilian health care systems to have their medical needs addressed. However, this outsourcing strategy was based on a false assumption that the community had enough capacity to deliver services to the many beneficiaries needing them. Nearly every sector of contemporary American medicine is experiencing a drastic shortage of HCPs. Though the resource allocation problems began before the pandemic, COVID-19 only exacerbated and accelerated them.6
This downsizing of military hospitals and clinics led to another predictable and seemingly unheeded consequence. A decrease in complex cases (particularly surgical cases) led to a reduction in the skills of military HCPs and a further flight of highly trained specialists who require a reasonable volume of complicated cases to retain and sharpen their expertise. The losses of those experienced clinicians further drain the pool of specialists the military can muster to sustain the readiness of troops for war and the health of their families in peace.7
The OIG recommended that the Defense Health Agency address MHS staffing and access deficiencies noted in its report, including identifying poorly performing TRICARE specialty networks and requiring them to meet their access obligation.2 As is customary, the OIG asked for DoD comment. It is unclear whether the DoD responded to that formal request; however, it is more certain it heard the message the OIG and beneficiaries conveyed. In December 2023, the Deputy Secretary of the DoD published a memorandum ordering the stabilization of the MHS. It instructs the MHS to address each of the 3 problem areas outlined in this article: (1) to reclaim patients and beneficiaries who had been outsourced or whose resources were constrained to seek care in the community; (2) to improve access to and staffing for military hospitals and clinics for active duty members and families; and (3) to restore and maintain the military readiness of the clinical forces.8 Several other documents have been issued that emphasize the crucial need to recruit and retain qualified HCPs and support staff if these aims are to be actualized, including the 2024 to 2029 MHS strategic plan.9 As the VA and US Public Health Service know, the current health care environment may be a near impossible mission.10 Although what we know from the history of military medicine is that they have a track record of achieving the impossible.
- Barr J, Podolsky SH. A national medical response to crisis - the legacy of World War II. N Engl J Med. 2020;383(7):613-615. doi:10.1056/NEJMp2008512
- US Department of Defense, Office of the Inspector General. Management advisory: concerns with access to care and staffing shortages in the Military Health System. November 29, 2023. Accessed August 26, 2024. https://www.dodig.mil/reports.html/Article/3602650/management-advisory-concerns-with-access-to-care-and-staffing-shortages-in-the/
- Management advisory: concerns with access to care and staffing shortages in the Military Health System. News release. US Department of Defense, Office of the Inspector General. November 29, 2023. Accessed August 26, 2024. https://www.dodig.mil/In-the-Spotlight/Article/3602662/press-release-management-advisory-concerns-with-access-to-care-and-staffing-sho
- US Department of Defense. Annual report on suicide in the military: calendar year 2022. Accessed August 26, 2024. https://www.dspo.mil/Portals/113/Documents/ARSM_CY22.pdf
- American Hospital Association. Strengthening the Health Care Work Force. November 2021. Accessed August 26, 2024. https://www.aha.org/system/files/media/file/2021/05/fact-sheet-workforce-infrastructure-0521.pdf
- Ziezulewicz G. DOD watchdog report warns of issues across military health system. Military Times. December 6, 2023. Accessed August 26, 2024. https://www.militarytimes.com/news/your-military/2023/12/07/dod-watchdog-report-warns-of-issues-across-military-health-care-system/
- Lawrence Q. It’s time to stop downsizing health care, the Pentagon says. This couple can’t wait. National Public Radio. April 3, 2024. Accessed August 26, 2024. https://www.npr.org/transcripts/1240724195
- Mincher R. Military Health System stabilization: rebuilding health care access is critical to patient’s well-being. January 22, 2024. Accessed August 26, 2024. https://www.defense.gov/News/News-Stories/Article/article/3652092/military-health-system-stabilization-rebuilding-health-care-access-is-critical/
- US Department of Defense, Defense Health Agency. Military Health System strategy fiscal years 2024-2029. Accessed August 26, 2024. https://www.health.mil/Reference-Center/Publications/2023/12/15/MHS_Strategic_Plan_FY24_29
- Jowers K. Pentagon plans to fix ‘chronically understaffed’ medical facilities. Military Times. January 25, 2024. Accessed August 26, 2024. https://www.militarytimes.com/news/your-military/2024/01/25/pentagon-plans-to-fix-chronically-understaffed-medical-facilities/
It is the neglect of timely repair that makes rebuilding necessary.
Richard Whately, economist and theologian (1787-1863)
US Congressional inquiry and media attention are so frequently directed at the trials and tribulations of the US Department of Veterans Affairs (VA) that we forget the US Department of Defense (DoD) medical system also shares the federal practitioner space. The focus of the government and press recently has shifted to examine the weaknesses and woes of military medicine. This editorial reviews what that examination discovered about the decline of the DoD house of medicine, why it is in disrepair, proposals for its rebuilding, and reflects on what this trajectory can tell us about maintaining the structure of federal practice.
My father never tired of telling me that he and his medical colleagues returned from the Second World War with knowledge and skills gained in combat theaters that, in many respects, surpassed those of the civilian sector. Though he was biased as a career military physician and combat veteran, there is strong evidence backing the assertion that from World War I to Operations Enduring Freedom and Iraqi Freedom, American military medicine has been the glory of the world.1
A November 2023 report from the DoD Office of the Inspector General (OIG) warned that military medicine was in trouble. The report’s emphasis on access and staffing problems that endanger the availability and quality of health care services will likely strike a chord with VA clinicians. The document is based on data from OIG reports, hotline calls, and audits from the last several years; however, the OIG acknowledges that it did not conduct on-the-ground investigations to confirm the findings.2
When we hear the term military medicine, many immediately think of active duty service members. However, the patient population of DoD is far larger and more diverse. The Military Health System (MHS) provides care to > 9.5 million beneficiaries, including dependents and retirees, veterans, civilian DoD employees, and even contractors. Those who most heavily rely on the MHS are individuals in uniform and their families are experiencing the greatest difficulty with accessing care.3 This includes crucial mental health treatment at a time when rates of military suicide continue to climb.4
The lack of access and dearth of health care practitioners (HCPs) spans both military facilities and the civilian clinics and hospitals where current and former service members and their dependents use the TRICARE beneficiary insurance. Reminiscent of recent challenges at the VA, DoD members are encountering long wait times and the frustrating bureaucracy of inefficient and, at times, inept referral networks. Additionally, many institutions and HCPs will not accept TRICARE because it pays less and has more paperwork than other insurance plans. What is worse, there is currently no governmental leverage to compel them to participate.
The lack of access and dearth of health care practitioners (HCPs) spans both military facilities and the civilian clinics and hospitals where current and former service members and their dependents use the TRICARE beneficiary insurance. Reminiscent of recent challenges at the VA, DoD members are encountering long wait times and the frustrating bureaucracy of inefficient and, at times, inept referral networks. Additionally, many institutions and HCPs will not accept TRICARE because it pays less and has more paperwork than other insurance plans. What is worse, there is currently no governmental leverage to compel them to participate.
As with both the VA and civilian health care spheres, rural areas are the most impacted. Resource shortfalls adversely affect all aspects of care, especially the highly paid specialties like gastroenterology and urology, as well as primary care practitioners essential to ensure the health of military families. The deficits are widespread—all branches report similar obstacles to providing responsive, appropriate care. As if this was not enough to complete the mirror image of the VA’s struggles, there is a rising tide of complaints about the military’s electronic health record system.5 How did the preeminent MHS so rapidly decay? Experts in and out of uniform offer several explanations.
As with most forms of managed care, the need to cut costs drove the Pentagon to send military members and dependents to civilian health care systems to have their medical needs addressed. However, this outsourcing strategy was based on a false assumption that the community had enough capacity to deliver services to the many beneficiaries needing them. Nearly every sector of contemporary American medicine is experiencing a drastic shortage of HCPs. Though the resource allocation problems began before the pandemic, COVID-19 only exacerbated and accelerated them.6
This downsizing of military hospitals and clinics led to another predictable and seemingly unheeded consequence. A decrease in complex cases (particularly surgical cases) led to a reduction in the skills of military HCPs and a further flight of highly trained specialists who require a reasonable volume of complicated cases to retain and sharpen their expertise. The losses of those experienced clinicians further drain the pool of specialists the military can muster to sustain the readiness of troops for war and the health of their families in peace.7
The OIG recommended that the Defense Health Agency address MHS staffing and access deficiencies noted in its report, including identifying poorly performing TRICARE specialty networks and requiring them to meet their access obligation.2 As is customary, the OIG asked for DoD comment. It is unclear whether the DoD responded to that formal request; however, it is more certain it heard the message the OIG and beneficiaries conveyed. In December 2023, the Deputy Secretary of the DoD published a memorandum ordering the stabilization of the MHS. It instructs the MHS to address each of the 3 problem areas outlined in this article: (1) to reclaim patients and beneficiaries who had been outsourced or whose resources were constrained to seek care in the community; (2) to improve access to and staffing for military hospitals and clinics for active duty members and families; and (3) to restore and maintain the military readiness of the clinical forces.8 Several other documents have been issued that emphasize the crucial need to recruit and retain qualified HCPs and support staff if these aims are to be actualized, including the 2024 to 2029 MHS strategic plan.9 As the VA and US Public Health Service know, the current health care environment may be a near impossible mission.10 Although what we know from the history of military medicine is that they have a track record of achieving the impossible.
It is the neglect of timely repair that makes rebuilding necessary.
Richard Whately, economist and theologian (1787-1863)
US Congressional inquiry and media attention are so frequently directed at the trials and tribulations of the US Department of Veterans Affairs (VA) that we forget the US Department of Defense (DoD) medical system also shares the federal practitioner space. The focus of the government and press recently has shifted to examine the weaknesses and woes of military medicine. This editorial reviews what that examination discovered about the decline of the DoD house of medicine, why it is in disrepair, proposals for its rebuilding, and reflects on what this trajectory can tell us about maintaining the structure of federal practice.
My father never tired of telling me that he and his medical colleagues returned from the Second World War with knowledge and skills gained in combat theaters that, in many respects, surpassed those of the civilian sector. Though he was biased as a career military physician and combat veteran, there is strong evidence backing the assertion that from World War I to Operations Enduring Freedom and Iraqi Freedom, American military medicine has been the glory of the world.1
A November 2023 report from the DoD Office of the Inspector General (OIG) warned that military medicine was in trouble. The report’s emphasis on access and staffing problems that endanger the availability and quality of health care services will likely strike a chord with VA clinicians. The document is based on data from OIG reports, hotline calls, and audits from the last several years; however, the OIG acknowledges that it did not conduct on-the-ground investigations to confirm the findings.2
When we hear the term military medicine, many immediately think of active duty service members. However, the patient population of DoD is far larger and more diverse. The Military Health System (MHS) provides care to > 9.5 million beneficiaries, including dependents and retirees, veterans, civilian DoD employees, and even contractors. Those who most heavily rely on the MHS are individuals in uniform and their families are experiencing the greatest difficulty with accessing care.3 This includes crucial mental health treatment at a time when rates of military suicide continue to climb.4
The lack of access and dearth of health care practitioners (HCPs) spans both military facilities and the civilian clinics and hospitals where current and former service members and their dependents use the TRICARE beneficiary insurance. Reminiscent of recent challenges at the VA, DoD members are encountering long wait times and the frustrating bureaucracy of inefficient and, at times, inept referral networks. Additionally, many institutions and HCPs will not accept TRICARE because it pays less and has more paperwork than other insurance plans. What is worse, there is currently no governmental leverage to compel them to participate.
The lack of access and dearth of health care practitioners (HCPs) spans both military facilities and the civilian clinics and hospitals where current and former service members and their dependents use the TRICARE beneficiary insurance. Reminiscent of recent challenges at the VA, DoD members are encountering long wait times and the frustrating bureaucracy of inefficient and, at times, inept referral networks. Additionally, many institutions and HCPs will not accept TRICARE because it pays less and has more paperwork than other insurance plans. What is worse, there is currently no governmental leverage to compel them to participate.
As with both the VA and civilian health care spheres, rural areas are the most impacted. Resource shortfalls adversely affect all aspects of care, especially the highly paid specialties like gastroenterology and urology, as well as primary care practitioners essential to ensure the health of military families. The deficits are widespread—all branches report similar obstacles to providing responsive, appropriate care. As if this was not enough to complete the mirror image of the VA’s struggles, there is a rising tide of complaints about the military’s electronic health record system.5 How did the preeminent MHS so rapidly decay? Experts in and out of uniform offer several explanations.
As with most forms of managed care, the need to cut costs drove the Pentagon to send military members and dependents to civilian health care systems to have their medical needs addressed. However, this outsourcing strategy was based on a false assumption that the community had enough capacity to deliver services to the many beneficiaries needing them. Nearly every sector of contemporary American medicine is experiencing a drastic shortage of HCPs. Though the resource allocation problems began before the pandemic, COVID-19 only exacerbated and accelerated them.6
This downsizing of military hospitals and clinics led to another predictable and seemingly unheeded consequence. A decrease in complex cases (particularly surgical cases) led to a reduction in the skills of military HCPs and a further flight of highly trained specialists who require a reasonable volume of complicated cases to retain and sharpen their expertise. The losses of those experienced clinicians further drain the pool of specialists the military can muster to sustain the readiness of troops for war and the health of their families in peace.7
The OIG recommended that the Defense Health Agency address MHS staffing and access deficiencies noted in its report, including identifying poorly performing TRICARE specialty networks and requiring them to meet their access obligation.2 As is customary, the OIG asked for DoD comment. It is unclear whether the DoD responded to that formal request; however, it is more certain it heard the message the OIG and beneficiaries conveyed. In December 2023, the Deputy Secretary of the DoD published a memorandum ordering the stabilization of the MHS. It instructs the MHS to address each of the 3 problem areas outlined in this article: (1) to reclaim patients and beneficiaries who had been outsourced or whose resources were constrained to seek care in the community; (2) to improve access to and staffing for military hospitals and clinics for active duty members and families; and (3) to restore and maintain the military readiness of the clinical forces.8 Several other documents have been issued that emphasize the crucial need to recruit and retain qualified HCPs and support staff if these aims are to be actualized, including the 2024 to 2029 MHS strategic plan.9 As the VA and US Public Health Service know, the current health care environment may be a near impossible mission.10 Although what we know from the history of military medicine is that they have a track record of achieving the impossible.
- Barr J, Podolsky SH. A national medical response to crisis - the legacy of World War II. N Engl J Med. 2020;383(7):613-615. doi:10.1056/NEJMp2008512
- US Department of Defense, Office of the Inspector General. Management advisory: concerns with access to care and staffing shortages in the Military Health System. November 29, 2023. Accessed August 26, 2024. https://www.dodig.mil/reports.html/Article/3602650/management-advisory-concerns-with-access-to-care-and-staffing-shortages-in-the/
- Management advisory: concerns with access to care and staffing shortages in the Military Health System. News release. US Department of Defense, Office of the Inspector General. November 29, 2023. Accessed August 26, 2024. https://www.dodig.mil/In-the-Spotlight/Article/3602662/press-release-management-advisory-concerns-with-access-to-care-and-staffing-sho
- US Department of Defense. Annual report on suicide in the military: calendar year 2022. Accessed August 26, 2024. https://www.dspo.mil/Portals/113/Documents/ARSM_CY22.pdf
- American Hospital Association. Strengthening the Health Care Work Force. November 2021. Accessed August 26, 2024. https://www.aha.org/system/files/media/file/2021/05/fact-sheet-workforce-infrastructure-0521.pdf
- Ziezulewicz G. DOD watchdog report warns of issues across military health system. Military Times. December 6, 2023. Accessed August 26, 2024. https://www.militarytimes.com/news/your-military/2023/12/07/dod-watchdog-report-warns-of-issues-across-military-health-care-system/
- Lawrence Q. It’s time to stop downsizing health care, the Pentagon says. This couple can’t wait. National Public Radio. April 3, 2024. Accessed August 26, 2024. https://www.npr.org/transcripts/1240724195
- Mincher R. Military Health System stabilization: rebuilding health care access is critical to patient’s well-being. January 22, 2024. Accessed August 26, 2024. https://www.defense.gov/News/News-Stories/Article/article/3652092/military-health-system-stabilization-rebuilding-health-care-access-is-critical/
- US Department of Defense, Defense Health Agency. Military Health System strategy fiscal years 2024-2029. Accessed August 26, 2024. https://www.health.mil/Reference-Center/Publications/2023/12/15/MHS_Strategic_Plan_FY24_29
- Jowers K. Pentagon plans to fix ‘chronically understaffed’ medical facilities. Military Times. January 25, 2024. Accessed August 26, 2024. https://www.militarytimes.com/news/your-military/2024/01/25/pentagon-plans-to-fix-chronically-understaffed-medical-facilities/
- Barr J, Podolsky SH. A national medical response to crisis - the legacy of World War II. N Engl J Med. 2020;383(7):613-615. doi:10.1056/NEJMp2008512
- US Department of Defense, Office of the Inspector General. Management advisory: concerns with access to care and staffing shortages in the Military Health System. November 29, 2023. Accessed August 26, 2024. https://www.dodig.mil/reports.html/Article/3602650/management-advisory-concerns-with-access-to-care-and-staffing-shortages-in-the/
- Management advisory: concerns with access to care and staffing shortages in the Military Health System. News release. US Department of Defense, Office of the Inspector General. November 29, 2023. Accessed August 26, 2024. https://www.dodig.mil/In-the-Spotlight/Article/3602662/press-release-management-advisory-concerns-with-access-to-care-and-staffing-sho
- US Department of Defense. Annual report on suicide in the military: calendar year 2022. Accessed August 26, 2024. https://www.dspo.mil/Portals/113/Documents/ARSM_CY22.pdf
- American Hospital Association. Strengthening the Health Care Work Force. November 2021. Accessed August 26, 2024. https://www.aha.org/system/files/media/file/2021/05/fact-sheet-workforce-infrastructure-0521.pdf
- Ziezulewicz G. DOD watchdog report warns of issues across military health system. Military Times. December 6, 2023. Accessed August 26, 2024. https://www.militarytimes.com/news/your-military/2023/12/07/dod-watchdog-report-warns-of-issues-across-military-health-care-system/
- Lawrence Q. It’s time to stop downsizing health care, the Pentagon says. This couple can’t wait. National Public Radio. April 3, 2024. Accessed August 26, 2024. https://www.npr.org/transcripts/1240724195
- Mincher R. Military Health System stabilization: rebuilding health care access is critical to patient’s well-being. January 22, 2024. Accessed August 26, 2024. https://www.defense.gov/News/News-Stories/Article/article/3652092/military-health-system-stabilization-rebuilding-health-care-access-is-critical/
- US Department of Defense, Defense Health Agency. Military Health System strategy fiscal years 2024-2029. Accessed August 26, 2024. https://www.health.mil/Reference-Center/Publications/2023/12/15/MHS_Strategic_Plan_FY24_29
- Jowers K. Pentagon plans to fix ‘chronically understaffed’ medical facilities. Military Times. January 25, 2024. Accessed August 26, 2024. https://www.militarytimes.com/news/your-military/2024/01/25/pentagon-plans-to-fix-chronically-understaffed-medical-facilities/
Has the VA Fulfilled its Commitment to Trust and Healing?
Trust is built step by step, commitment by commitment, on every level.
Robert C. Solomon1
The US Department of Veterans Affairs (VA) was created in response to criticism of its predecessors. Since its establishment in 1930, the VA has never been short of critics who denounced its corruption, called for its dismantling in favor of privatization, and derided its incompetence.2 Despite multiple scandals that have handed more ammunition to those who object to its continued existence, the VA has not only survived, but thrived. This editorial is written in the form of a debate between exemplar opponents and defenders of the VA on whether it is currently fulfilling its commitment to veterans.
In May 2024, the Veterans Signals survey found that 80.4% of respondents reported trust in the VA, the highest level ever recorded.3 At its 2016 launch, the survey found that only 55% of veterans expressed trust in the VA. The survey was conducted 2 years after the scandal over access to care for veterans in Phoenix. Scores would surely have been even lower than 55% during that period when the critique of the VA—even from those who believe in its mission—was most trenchant.4 Administered quarterly, the survey samples > 38,000 of the 9 million enrolled veterans. Veterans surveyed were using services from all 3 branches of the VA: Veterans Health Administration, Veterans Benefits Administration, and National Cemetery Administration. Participants are asked whether they trust the VA to fulfill the country’s commitment to veterans and specifically how they rate the VA in 3 specific criteria: effectiveness, emotional resonance, and overall ease. In the latest survey, 80.5% of veterans rated the VA positively for effectiveness, 78.4% for emotional resonance, and 75.9% for overall ease. Even more impressive is the 91.8% of participants who reported they trust the VA for outpatient health care, capping a 7-year upward trend.3
The paradigmatic VA antagonist will rightly point out the well-known methodological limitations of this type of survey, including self-selection, sampling bias, and especially low response rates. However, VA researchers will counter that the 18% response rate for the latest Veterans Signals survey is higher than the industry average.5
VA critics might say that it would not matter if the response rate were 4 times higher; what matters is not what veterans say on a survey but what decisions they make about their care. The VA defender would be constrained to concede that even the most statistically sophisticated survey remains an indirect measure of veteran trust. They could, though, marshal far stronger evidence. Two direct demonstrations published in the literature suggest that veterans do as they say and are acting on their trust in the agency. First, the VA delivered more services, health care, and benefits to veterans during the 2023 fiscal year than ever before. Importantly for Federal Practitioner readers, the 16 million documented health care visits were 3 million more than previous records.6 Second, and in some ways even more encouraging for the future of the VA as a health care system, is that due in large part to the passage of the PACT Act, there has been a surge in VA enrollment by veterans. The VA recently announced that in the last year, > 400,000 veterans signed up for its health care and services. Enrollments are 30% more than the previous year and represented the highest figure in the past 5 years, a remarkable 50% increase over 2020 pandemic levels.7
VA critics could legitimately rebut this data by asking, “So more veterans are signing up for VA, and you are delivering more care, but what about the quality of that care? Has it improved?” The VA proponent’s rejoinder from multiple converging empirical studies would be a resounding yes. We have space to cite only a few examples of that rigorous recent research. What stands out ethically about these studies is that the VA has a broad program of research into the quality of the care it delivers and then transparently publishes those findings. The VA quality improvement research mission is truly unique and provides a shared open set of data for both critics and defenders to objectively examine VA successes and failures.
Among the most persuasive analysis was a systematic review of 37 studies contrasting VA with non-VA care from 2015 to 2023. The authors examined clinical quality, safety, patient access, experience, cost-efficiency, and equity of outcome. “VA care is consistently as good as or better than non-VA care in terms of clinical quality and safety,” the systematic review authors stated while qualifying that “Access, cost/efficiency, and patient experience between the 2 systems are not well studied.”8
A second systematic review looked specifically at similar key areas of quality, safety, access, patient experience, and comparative cost-efficiency for surgical treatment delivered in the VA and the community from 2015 to 2021. Only 18 studies met the inclusion criteria, but as the authors argued:
Based on limited data, these findings suggest that expanding eligibility for veterans to get care in the community may not provide benefits in terms of increasing access to surgical procedures, will not result in better quality, and may result in worse quality of care, but may reduce inpatient length of stay and perhaps cost less.9
At this juncture, the faultfinder may become frustrated and resort to a new tactic, challenging the very assumption that is the subject of the debate and demanding proof that there is any connection between veterans’ trust in the VA and their health and well-being. “Fair enough,” the VA side would reply, “here is some research that bolsters that connection.” Kopacz and colleagues examined the relationship between trust and healing at 6 sites and included 427 veterans and active-duty service members with combat posttraumatic stress disorder (PTSD) symptoms. The researchers found that trust and lack thereof are related to several significant mental, social, and physical health outcomes. The authors indicate the need for more research to better understand the importance and impact of trust and healing, but they show it is significant.10 Finally, veterans recognize the crucial link between trust in the unique expertise of VA practitioners in the treatment of PTSD. In a 2019 study, a majority expressed a preference to receive their PTSD treatment at the VA compared to a smaller group choosing care in the community.11
You be the judge of who won the debate, but knowing the dedication of my fellow federal practitioners, many of you will endorse my sentiment that we all need to stop talking and get back to doing our best to enhance veteran trust and healing; doing our essential part to keep fulfilling our commitment.
1. Solomon RC, Fernando F. Building Trust: In Business, Politics, Relationships, and Life. Oxford University Press; 2003:49.
2. Seiken J. 1921: Veterans Bureau is born - precursor to Department of Veterans Affairs. November 12, 2021. Updated September 4, 2023. Accessed July 22, 2024. https://department.va.gov/history/featured-stories/veterans-bureau/
3. US Department of Veterans Affairs. Serving America’s veterans, January 1 - March 31, 2024. Accessed July 22, 2024. https://department.va.gov/veterans-experience/wp-content/uploads/sites/2/2024/05/veteran-trust-report-fiscal-year-2024-quarter-2.pdf
4. Kizer KW, Jha AK. Restoring trust in VA health care. N Engl J Med. 2014;371(4):295-297. doi:10.1056/NEJMp1406852
5. Veteran trust in VA has increased 25% since 2016, reached an all-time high. News release. US Department of Veterans Affairs. May 28, 2024. Accessed July 22, 2024. https://news.va.gov/press-room/veteran-trust-va-increased-25-since-2016-high
6. VA sets all-time records for care and benefits delivered to Veterans in fiscal year 2023. News release. US Department of Veterans Affairs. November 6, 2023. Accessed July 23, 2024. https://news.va.gov/press-room/va-all-time-record-care-benefits-veterans-fy-2023/
7. 400,000+ Veterans enrolled in VA health care over the past 365 days, a 30% increase over last year. News release. US Department of Veterans Affairs. March 29, 2024. Accessed July 23, 2024. https://news.va.gov/press-room/va-enrolled-401006-veterans-healthcare-365/
8. Apaydin EA, Paige NM, Begashaw MM, Larkin J, Miake-Lye IM, Shekelle PG. Veterans Health Administration (VA) vs. non-VA healthcare quality: a systematic review. J Gen Intern Med. 2023;38(9):2179-2188. doi:10.1007/s11606-023-08207-2
9. Blegen M, Ko J, Salzman G, et al. Comparing quality of surgical care between the US Department of Veterans Affairs and non-veterans affairs settings: a systematic review. J Am Coll Surg. 2023;237(2):352-361. doi:10.1097/XCS.0000000000000720
10. Kopacz MS, Ames D, Koenig HG. Association between trust and mental, social, and physical health outcomes in veterans and active duty service members with combat-related PTSD symptomatology. Front Psychiatry. 2018;9:408. doi:10.3389/fpsyt.2018.00408
11. Haro E, Mader M, Noël PH, et al. The impact of trust, satisfaction, and perceived quality on preference for setting of future care among veterans with PTSD. Mil Med. 2019;184(11-12):e708-e714. doi:10.1093/milmed/usz078
Trust is built step by step, commitment by commitment, on every level.
Robert C. Solomon1
The US Department of Veterans Affairs (VA) was created in response to criticism of its predecessors. Since its establishment in 1930, the VA has never been short of critics who denounced its corruption, called for its dismantling in favor of privatization, and derided its incompetence.2 Despite multiple scandals that have handed more ammunition to those who object to its continued existence, the VA has not only survived, but thrived. This editorial is written in the form of a debate between exemplar opponents and defenders of the VA on whether it is currently fulfilling its commitment to veterans.
In May 2024, the Veterans Signals survey found that 80.4% of respondents reported trust in the VA, the highest level ever recorded.3 At its 2016 launch, the survey found that only 55% of veterans expressed trust in the VA. The survey was conducted 2 years after the scandal over access to care for veterans in Phoenix. Scores would surely have been even lower than 55% during that period when the critique of the VA—even from those who believe in its mission—was most trenchant.4 Administered quarterly, the survey samples > 38,000 of the 9 million enrolled veterans. Veterans surveyed were using services from all 3 branches of the VA: Veterans Health Administration, Veterans Benefits Administration, and National Cemetery Administration. Participants are asked whether they trust the VA to fulfill the country’s commitment to veterans and specifically how they rate the VA in 3 specific criteria: effectiveness, emotional resonance, and overall ease. In the latest survey, 80.5% of veterans rated the VA positively for effectiveness, 78.4% for emotional resonance, and 75.9% for overall ease. Even more impressive is the 91.8% of participants who reported they trust the VA for outpatient health care, capping a 7-year upward trend.3
The paradigmatic VA antagonist will rightly point out the well-known methodological limitations of this type of survey, including self-selection, sampling bias, and especially low response rates. However, VA researchers will counter that the 18% response rate for the latest Veterans Signals survey is higher than the industry average.5
VA critics might say that it would not matter if the response rate were 4 times higher; what matters is not what veterans say on a survey but what decisions they make about their care. The VA defender would be constrained to concede that even the most statistically sophisticated survey remains an indirect measure of veteran trust. They could, though, marshal far stronger evidence. Two direct demonstrations published in the literature suggest that veterans do as they say and are acting on their trust in the agency. First, the VA delivered more services, health care, and benefits to veterans during the 2023 fiscal year than ever before. Importantly for Federal Practitioner readers, the 16 million documented health care visits were 3 million more than previous records.6 Second, and in some ways even more encouraging for the future of the VA as a health care system, is that due in large part to the passage of the PACT Act, there has been a surge in VA enrollment by veterans. The VA recently announced that in the last year, > 400,000 veterans signed up for its health care and services. Enrollments are 30% more than the previous year and represented the highest figure in the past 5 years, a remarkable 50% increase over 2020 pandemic levels.7
VA critics could legitimately rebut this data by asking, “So more veterans are signing up for VA, and you are delivering more care, but what about the quality of that care? Has it improved?” The VA proponent’s rejoinder from multiple converging empirical studies would be a resounding yes. We have space to cite only a few examples of that rigorous recent research. What stands out ethically about these studies is that the VA has a broad program of research into the quality of the care it delivers and then transparently publishes those findings. The VA quality improvement research mission is truly unique and provides a shared open set of data for both critics and defenders to objectively examine VA successes and failures.
Among the most persuasive analysis was a systematic review of 37 studies contrasting VA with non-VA care from 2015 to 2023. The authors examined clinical quality, safety, patient access, experience, cost-efficiency, and equity of outcome. “VA care is consistently as good as or better than non-VA care in terms of clinical quality and safety,” the systematic review authors stated while qualifying that “Access, cost/efficiency, and patient experience between the 2 systems are not well studied.”8
A second systematic review looked specifically at similar key areas of quality, safety, access, patient experience, and comparative cost-efficiency for surgical treatment delivered in the VA and the community from 2015 to 2021. Only 18 studies met the inclusion criteria, but as the authors argued:
Based on limited data, these findings suggest that expanding eligibility for veterans to get care in the community may not provide benefits in terms of increasing access to surgical procedures, will not result in better quality, and may result in worse quality of care, but may reduce inpatient length of stay and perhaps cost less.9
At this juncture, the faultfinder may become frustrated and resort to a new tactic, challenging the very assumption that is the subject of the debate and demanding proof that there is any connection between veterans’ trust in the VA and their health and well-being. “Fair enough,” the VA side would reply, “here is some research that bolsters that connection.” Kopacz and colleagues examined the relationship between trust and healing at 6 sites and included 427 veterans and active-duty service members with combat posttraumatic stress disorder (PTSD) symptoms. The researchers found that trust and lack thereof are related to several significant mental, social, and physical health outcomes. The authors indicate the need for more research to better understand the importance and impact of trust and healing, but they show it is significant.10 Finally, veterans recognize the crucial link between trust in the unique expertise of VA practitioners in the treatment of PTSD. In a 2019 study, a majority expressed a preference to receive their PTSD treatment at the VA compared to a smaller group choosing care in the community.11
You be the judge of who won the debate, but knowing the dedication of my fellow federal practitioners, many of you will endorse my sentiment that we all need to stop talking and get back to doing our best to enhance veteran trust and healing; doing our essential part to keep fulfilling our commitment.
Trust is built step by step, commitment by commitment, on every level.
Robert C. Solomon1
The US Department of Veterans Affairs (VA) was created in response to criticism of its predecessors. Since its establishment in 1930, the VA has never been short of critics who denounced its corruption, called for its dismantling in favor of privatization, and derided its incompetence.2 Despite multiple scandals that have handed more ammunition to those who object to its continued existence, the VA has not only survived, but thrived. This editorial is written in the form of a debate between exemplar opponents and defenders of the VA on whether it is currently fulfilling its commitment to veterans.
In May 2024, the Veterans Signals survey found that 80.4% of respondents reported trust in the VA, the highest level ever recorded.3 At its 2016 launch, the survey found that only 55% of veterans expressed trust in the VA. The survey was conducted 2 years after the scandal over access to care for veterans in Phoenix. Scores would surely have been even lower than 55% during that period when the critique of the VA—even from those who believe in its mission—was most trenchant.4 Administered quarterly, the survey samples > 38,000 of the 9 million enrolled veterans. Veterans surveyed were using services from all 3 branches of the VA: Veterans Health Administration, Veterans Benefits Administration, and National Cemetery Administration. Participants are asked whether they trust the VA to fulfill the country’s commitment to veterans and specifically how they rate the VA in 3 specific criteria: effectiveness, emotional resonance, and overall ease. In the latest survey, 80.5% of veterans rated the VA positively for effectiveness, 78.4% for emotional resonance, and 75.9% for overall ease. Even more impressive is the 91.8% of participants who reported they trust the VA for outpatient health care, capping a 7-year upward trend.3
The paradigmatic VA antagonist will rightly point out the well-known methodological limitations of this type of survey, including self-selection, sampling bias, and especially low response rates. However, VA researchers will counter that the 18% response rate for the latest Veterans Signals survey is higher than the industry average.5
VA critics might say that it would not matter if the response rate were 4 times higher; what matters is not what veterans say on a survey but what decisions they make about their care. The VA defender would be constrained to concede that even the most statistically sophisticated survey remains an indirect measure of veteran trust. They could, though, marshal far stronger evidence. Two direct demonstrations published in the literature suggest that veterans do as they say and are acting on their trust in the agency. First, the VA delivered more services, health care, and benefits to veterans during the 2023 fiscal year than ever before. Importantly for Federal Practitioner readers, the 16 million documented health care visits were 3 million more than previous records.6 Second, and in some ways even more encouraging for the future of the VA as a health care system, is that due in large part to the passage of the PACT Act, there has been a surge in VA enrollment by veterans. The VA recently announced that in the last year, > 400,000 veterans signed up for its health care and services. Enrollments are 30% more than the previous year and represented the highest figure in the past 5 years, a remarkable 50% increase over 2020 pandemic levels.7
VA critics could legitimately rebut this data by asking, “So more veterans are signing up for VA, and you are delivering more care, but what about the quality of that care? Has it improved?” The VA proponent’s rejoinder from multiple converging empirical studies would be a resounding yes. We have space to cite only a few examples of that rigorous recent research. What stands out ethically about these studies is that the VA has a broad program of research into the quality of the care it delivers and then transparently publishes those findings. The VA quality improvement research mission is truly unique and provides a shared open set of data for both critics and defenders to objectively examine VA successes and failures.
Among the most persuasive analysis was a systematic review of 37 studies contrasting VA with non-VA care from 2015 to 2023. The authors examined clinical quality, safety, patient access, experience, cost-efficiency, and equity of outcome. “VA care is consistently as good as or better than non-VA care in terms of clinical quality and safety,” the systematic review authors stated while qualifying that “Access, cost/efficiency, and patient experience between the 2 systems are not well studied.”8
A second systematic review looked specifically at similar key areas of quality, safety, access, patient experience, and comparative cost-efficiency for surgical treatment delivered in the VA and the community from 2015 to 2021. Only 18 studies met the inclusion criteria, but as the authors argued:
Based on limited data, these findings suggest that expanding eligibility for veterans to get care in the community may not provide benefits in terms of increasing access to surgical procedures, will not result in better quality, and may result in worse quality of care, but may reduce inpatient length of stay and perhaps cost less.9
At this juncture, the faultfinder may become frustrated and resort to a new tactic, challenging the very assumption that is the subject of the debate and demanding proof that there is any connection between veterans’ trust in the VA and their health and well-being. “Fair enough,” the VA side would reply, “here is some research that bolsters that connection.” Kopacz and colleagues examined the relationship between trust and healing at 6 sites and included 427 veterans and active-duty service members with combat posttraumatic stress disorder (PTSD) symptoms. The researchers found that trust and lack thereof are related to several significant mental, social, and physical health outcomes. The authors indicate the need for more research to better understand the importance and impact of trust and healing, but they show it is significant.10 Finally, veterans recognize the crucial link between trust in the unique expertise of VA practitioners in the treatment of PTSD. In a 2019 study, a majority expressed a preference to receive their PTSD treatment at the VA compared to a smaller group choosing care in the community.11
You be the judge of who won the debate, but knowing the dedication of my fellow federal practitioners, many of you will endorse my sentiment that we all need to stop talking and get back to doing our best to enhance veteran trust and healing; doing our essential part to keep fulfilling our commitment.
1. Solomon RC, Fernando F. Building Trust: In Business, Politics, Relationships, and Life. Oxford University Press; 2003:49.
2. Seiken J. 1921: Veterans Bureau is born - precursor to Department of Veterans Affairs. November 12, 2021. Updated September 4, 2023. Accessed July 22, 2024. https://department.va.gov/history/featured-stories/veterans-bureau/
3. US Department of Veterans Affairs. Serving America’s veterans, January 1 - March 31, 2024. Accessed July 22, 2024. https://department.va.gov/veterans-experience/wp-content/uploads/sites/2/2024/05/veteran-trust-report-fiscal-year-2024-quarter-2.pdf
4. Kizer KW, Jha AK. Restoring trust in VA health care. N Engl J Med. 2014;371(4):295-297. doi:10.1056/NEJMp1406852
5. Veteran trust in VA has increased 25% since 2016, reached an all-time high. News release. US Department of Veterans Affairs. May 28, 2024. Accessed July 22, 2024. https://news.va.gov/press-room/veteran-trust-va-increased-25-since-2016-high
6. VA sets all-time records for care and benefits delivered to Veterans in fiscal year 2023. News release. US Department of Veterans Affairs. November 6, 2023. Accessed July 23, 2024. https://news.va.gov/press-room/va-all-time-record-care-benefits-veterans-fy-2023/
7. 400,000+ Veterans enrolled in VA health care over the past 365 days, a 30% increase over last year. News release. US Department of Veterans Affairs. March 29, 2024. Accessed July 23, 2024. https://news.va.gov/press-room/va-enrolled-401006-veterans-healthcare-365/
8. Apaydin EA, Paige NM, Begashaw MM, Larkin J, Miake-Lye IM, Shekelle PG. Veterans Health Administration (VA) vs. non-VA healthcare quality: a systematic review. J Gen Intern Med. 2023;38(9):2179-2188. doi:10.1007/s11606-023-08207-2
9. Blegen M, Ko J, Salzman G, et al. Comparing quality of surgical care between the US Department of Veterans Affairs and non-veterans affairs settings: a systematic review. J Am Coll Surg. 2023;237(2):352-361. doi:10.1097/XCS.0000000000000720
10. Kopacz MS, Ames D, Koenig HG. Association between trust and mental, social, and physical health outcomes in veterans and active duty service members with combat-related PTSD symptomatology. Front Psychiatry. 2018;9:408. doi:10.3389/fpsyt.2018.00408
11. Haro E, Mader M, Noël PH, et al. The impact of trust, satisfaction, and perceived quality on preference for setting of future care among veterans with PTSD. Mil Med. 2019;184(11-12):e708-e714. doi:10.1093/milmed/usz078
1. Solomon RC, Fernando F. Building Trust: In Business, Politics, Relationships, and Life. Oxford University Press; 2003:49.
2. Seiken J. 1921: Veterans Bureau is born - precursor to Department of Veterans Affairs. November 12, 2021. Updated September 4, 2023. Accessed July 22, 2024. https://department.va.gov/history/featured-stories/veterans-bureau/
3. US Department of Veterans Affairs. Serving America’s veterans, January 1 - March 31, 2024. Accessed July 22, 2024. https://department.va.gov/veterans-experience/wp-content/uploads/sites/2/2024/05/veteran-trust-report-fiscal-year-2024-quarter-2.pdf
4. Kizer KW, Jha AK. Restoring trust in VA health care. N Engl J Med. 2014;371(4):295-297. doi:10.1056/NEJMp1406852
5. Veteran trust in VA has increased 25% since 2016, reached an all-time high. News release. US Department of Veterans Affairs. May 28, 2024. Accessed July 22, 2024. https://news.va.gov/press-room/veteran-trust-va-increased-25-since-2016-high
6. VA sets all-time records for care and benefits delivered to Veterans in fiscal year 2023. News release. US Department of Veterans Affairs. November 6, 2023. Accessed July 23, 2024. https://news.va.gov/press-room/va-all-time-record-care-benefits-veterans-fy-2023/
7. 400,000+ Veterans enrolled in VA health care over the past 365 days, a 30% increase over last year. News release. US Department of Veterans Affairs. March 29, 2024. Accessed July 23, 2024. https://news.va.gov/press-room/va-enrolled-401006-veterans-healthcare-365/
8. Apaydin EA, Paige NM, Begashaw MM, Larkin J, Miake-Lye IM, Shekelle PG. Veterans Health Administration (VA) vs. non-VA healthcare quality: a systematic review. J Gen Intern Med. 2023;38(9):2179-2188. doi:10.1007/s11606-023-08207-2
9. Blegen M, Ko J, Salzman G, et al. Comparing quality of surgical care between the US Department of Veterans Affairs and non-veterans affairs settings: a systematic review. J Am Coll Surg. 2023;237(2):352-361. doi:10.1097/XCS.0000000000000720
10. Kopacz MS, Ames D, Koenig HG. Association between trust and mental, social, and physical health outcomes in veterans and active duty service members with combat-related PTSD symptomatology. Front Psychiatry. 2018;9:408. doi:10.3389/fpsyt.2018.00408
11. Haro E, Mader M, Noël PH, et al. The impact of trust, satisfaction, and perceived quality on preference for setting of future care among veterans with PTSD. Mil Med. 2019;184(11-12):e708-e714. doi:10.1093/milmed/usz078
The Role of High Reliability Organization Foundational Practices in Building a Culture of Safety
Increasing complexities within health care systems are significant impediments to the consistent delivery of safe and effective patient care. These impediments include an increase in specialization of care, staff shortages, burnout, poor coordination of services and access to care, as well as rising costs.1 High reliability organizations (HROs) provide safe, high-quality, and effective care in highly complex and risk-prone environments without causing harm or experiencing catastrophic events.2
Within the US Department of Veterans Affairs (VA), the Veterans Health Administration (VHA) operates the nation’s largest integrated health care system, providing care to > 9 million veterans. The VHA formally launched plans for an enterprise-wide HRO in February 2019. During the first year, 18 medical facilities comprised cohort1 of the journey to high reliability. Cohort 2 began in October 2020 and consisted of 54 facilities. Cohort 3 started in October 2021 with 67 facilities.3
Health care organizations seeking high reliability exercise a philosophy aimed at learning from errors and addressing system failures. High reliability is accomplished by implementing 5 principles: (1) sensitivity to operations (a heightened understanding of the current state of systems); (2) preoccupation with failure (striving to anticipate risks that might suggest a much larger system problem); (3) reluctance to simplify (avoiding making any assumptions regarding the causes of failures); (4) commitment to resilience (preparing for potential failures and bouncing back when they occur); and (5) deference to expertise (deferring to individuals with the skills and proficiency to make the best decisions).2 The VHA also recognized that a successful journey to high reliability—in addition to achieving a culture of safety—relies on the implementation of foundational HRO practices: leader rounding, visual management systems, safety forums, and safety huddles. This article describes an initiative for how these foundational practices were implemented in a large integrated health care system.
BACKGROUND
The VHA has focused on 4 foundational components as part of its enterprise activities and support structure to implement HRO principles and practices. These components were selected based on pilot activities that preceded the enterprise-wide effort, reviews of the literature, and expert consultation with both government and private sector health systems. To support the implementation of these practices, the VHA provided training, toolkits, HRO executive leader coaching, and peer-to-peer mentoring. As the VHA enters its fifth year seeking high reliability, we undertook an initiative to reflect on our own experiences and refine our practices based on an updated literature review.
As part of this enterprise-wide initiative, we conducted a literature review from 2018 to March 2023 seeking recent evidence describing the value of implementing the 4 foundational HRO practices to advance high reliability and improve patient safety. A 5-year period was used to ensure recency and value of evidence.
Eligible literature was identified in PubMed, PsycINFO, the Cumulative Index to Nursing and Allied Health Literature, ScienceDirect, Scopus, the Cochrane Library, and ProQuest Dissertations & Theses Global. Inclusion and exclusion criteria were peer-reviewed interdisciplinary documents(eg, publications, dissertations, conference proceedings, and grey literature) written in English. Search terms included high reliability organizations, foundational practices, and patient safety. Boolean operators (AND, OR) were also used in the search. The search resulted in a dearth of evidence that addressed implementation of all 4 foundational practices across a health care system. Retrieved evidence focused on the implementation of only 1 particular foundational practice in a specific health care setting. In addition to describing the formal processes for the implementation of each foundational HRO practice, a brief description of representative examples of strong practices within the VHA is provided.
To support the implementation of HROs, the VHA paired HRO executive leader coaches with select medical center directors and their leadership teams. Executive leader coaches also support an organization’s HRO Lead and HRO Champion. The HRO Lead coordinates and facilitates the implementation of HRO principles and practices in pursuit of no harm across an organization. The HRO Champion supports the same as the HRO Lead, but typically has a different specialty background. For example, if the HRO Lead has an administrative background, the HRO Champion would have a clinical background.
Coaching focuses heavily on supporting site-specific implementation and sustainment of the 4 HRO foundational practices. The aim is to accelerate change, build enduring capacity, foster a safety culture, and accelerate HRO maturity. To measure change, HRO executive leader coaches track the progress of their aligned VA medical centers (VAMCs) using the Organizational Learning Tool (OLT). This tool was developed to provide information such as a facility summary and relationships between a medical center director, HRO Lead, HRO Champion, and the executive leader coach (Figure 1). The OLT also serves as a structured process to measure leader coaching performance against mutually agreed upon objectives that ultimately contribute to enterprise outcomes. It also collects data on the progress in implementing foundational practices, strong practices, needs and gaps, and more (Figure 2). Data collected from facilities supported by HRO executive leader coaches on whether foundational practices are in place are briefly described.
Leader Rounding
Leader rounding for high reliability ensures effective, bidirectional communication and collaboration among all disciplines to improve patient safety. It is an essential feature of a robust patient safety culture and an important method for demonstrating leadership engagement with high reliability.4,5 These rounds are conducted by organizational leadership (eg, executive teams, department/service chiefs, or unit managers) and frontline staff from different areas. They are specifically focused on high reliability, patient and staff safety, and improvement efforts. The aim is to learn about daily challenges that may contribute to patient harm.4
Leader rounding has been found to be highly effective at improving leadership visibility across the organization. It enhances interaction and open communication with frontline staff, fostering leader-staff collaboration and shared decision-making, as well as promoting leadership understanding of operational, clinical, nonclinical (eg, administrative, nutrition services, or facilities management), and patient/family experience issues.4 Collaboration among team members fosters the delivery of more effective and efficient care, increases staff satisfaction, and improves employee retention.6 Leader rounding for high reliability significantly contributes to the breakdown of power barriers by giving team members voice and agency, ultimately leading to deeper engagement.7
It is important that leader rounding for high reliability occurs as planned and when possible, scheduled in advance. This helps to avoid rounding at peak times when care activities are being performed.4,6 When scheduling conflicts arise, another leader should be sent to participate in rounds.4 Developing a list of questions in advance allows leadership to prepare messaging to share with staff as it relates to high reliability and patient safety (Table).4,6,8
Closing the loop improves bidirectional communication and is critical to leader rounding for high reliability. Closed-loop communication and following up on and/or closing out issues raised during rounding empowers the sharing of information, which is critical for advancing a culture of safety.4,8 Enhanced feedback is also associated with greater workforce engagement, staff feeling more connected to quality improvement activities, and lower rates of employee burnout.7 It is important to recognize that senior leaders are not responsible for resolving all issues. If a team or manager can resolve concerns that are raised, this should be encouraged and supported. Maintaining accountability at the lowest level of the organization promotes principles and practices of high reliability (Figure 3).4,8
The VA Bedford Healthcare System created and implemented a strong practice for leader rounding for high reliability. This phased implementation involved creating an evidence-based process, deciding on an appropriate cadence, developing a tracking tool, and measuring impact to determine the overall effectiveness of leader rounding for high reliability.4
Visual Management Systems
A visual management system (VMS) displays clinical and operational performance aligned with HRO goals and practices. It is used to view and guide discussions between interdisciplinary teams during tiered safety huddles, leader rounds for high reliability, and frontline staff on the current status and safety trends in a particular area.8,9 A VMS is highly effective in creating an environment where all staff members, especially frontline workers, feel empowered to voice their concerns related to safety or to identify improvement opportunities.8,10 Increased leader engagement in patient safety and heightened transparency of information associated with the use of a VMS improves staff morale and professional satisfaction.10
A VMS may be a dry-erase or whiteboard display, paper-based display, or electronic status board.8 VMSs are usually located in or near work settings (eg, nurses’ station, staff break room, or conference room).8 Although they can take different forms and display several types of information, a VMS should be easy to update and meet the specific needs of a work area. In the VHA, a VMS displays: (1) essential information for staff members to effectively perform their work; (2) improvement project ideas; (3) current work in progress; (4) tracking of implemented improvement activities; (5) strong practices that have been effective; and (6) staff recognition for those who have enhanced patient safety, including the reporting of close calls and near misses.
The VHA uses the MESS (methods, equipment, staffing, and supplies) VMS format. This format empowers staff to identify whether proper procedures and practices are in place, essential equipment and supplies are readily available in the quantity needed, and appropriate staffing is on hand to provide safe, high-quality patient care.8 Colored magnets are used as visual cues in a stoplight classification system to identify low or no safety risks (green), at risk (yellow), or high risk (red). Green coded issues are addressed locally by a manager or supervisor. Yellow coded concerns require increased staff and leadership vigilance. Red coded issues indicate that patient care would be impacted that day and therefore need to be immediately escalated and addressed with senior leaders to mitigate the threat.4,11 Dayton VAMC successfully implemented a VMS, using both physical and electronic visual management boards. The Dayton VAMC VMS boards are closely tied to tiered safety huddles and leader rounding for high reliability.
Safety Forums
Safety forums are another foundational practice of VHA health care organizations seeking high reliability. Recurring monthly, safety forums focus on reinforcing HRO principles and practices, safety programs, the importance and appreciation of reporting, and just culture. The emphasis on just culture reminds staff that adverse events in the organization are viewed as valuable learning opportunities to understand the factors leading to the situation as opposed to immediately assigning blame.12
Psychological safety is another important focus. When individuals feel psychologically safe, they are more likely to voice concerns and act without fear of reprisal, which supports a culture of safety.13 Safety forums are open to all members of the health care organization, including both clinical and nonclinical staff. Forums can be conducted by an HRO Lead, HRO Champion, Patient Safety Manager, or even executive leadership. Rotating the responsibility of leading these forums demonstrates that high reliability and safety are everyone’s responsibility.
Safety forums publicly review and discuss errors, adverse events, close calls, and near misses. Time is also spent discussing root cause analysis trends and highlighting continuous process improvement principles and current projects. During safety forums, leaders should recognize individuals for safety behaviors and reward reporting through a safety awards program.14 All forums should conclude with a question-and-answer session. Forums typically occur in virtual 30-minute sessions but can last up to 60 minutes when guest speakers attend and continuing education credit is offered.
The Jesse Brown VAMC in Chicago developed an interactive monthly safety forum appealing to a broad audience. Each forum is attended by about 200 staff members and includes leader engagement and panel discussions led by the chief medical officer, with topics on both patient and team safety connecting with HRO principles. A planning committee prepares guest speakers and offers continuing education credits.
Tiered Safety Huddles
Based on the processes of high reliability industries like aviation and nuclear power, tiered safety huddles have been increasingly adopted in health care. Huddles (health care, utilizing, deliberate, discussion,linking, and events) are department-level interdisciplinary meetings that last no more than 15 minutes.15 Their purpose is to improve communication by sharing day-to-day information across multiple disciplines, identify issues that may impact the delivery of care (eg, patient and staff safety concerns, staffing issues, or inadequate supplies) and resolve problems.
Tiered safety huddles are gaining popularity, especially in organizations seeking high reliability. They are more complex than traditional huddles because of the mechanics of elevating safety issues (eg, bedside to executive leadership teams), feedback loops, and sequencing, among other factors.15,16
Tiered safety huddles are focused, transparent forums with multidisciplinary staff, including frontline workers, along with senior leadership.15,16 When initially implemented, tiered safety huddles may take longer than the suggested 15 minutes; however, as teams become more experienced, huddles become more efficient.15 The goal of tiered safety huddles is to proactively identify, share, address, and resolve problems that have the potential to impact the delivery of safe and quality patient care. This may include addressing staffing shortfalls, inadequate allocation of supplies and equipment, operational issues, etc.8,15 Critical to theeffective utilization of tiered safety huddles is the appropriate escalation of issues between tiers. The most critical issues are elevated to higher tiers so they are addressed by the most qualified person in the organization.
Deciding on the number of tiers typically depends on the size and scope of services provided by the health care organization or integrated system. For example, tiered huddles in the VHA originate at the point of service (eg, critical care unit). Tier 1 includes staff members at the unit/team level along with immediate supervisors/managers. Tier 2 involves departments and service lines (eg, pharmacy, podiatry, or internal medicine) including their respective leadership. Tier 3 is the executive leadership team. This process allows for bidirectional communication instead of the traditional hierarchical communication pathway (Figure 4). Issues identified that cannot be addressed at a particular tier are elevated to the next tier. Elevated issues typically involve systems or processes requiring attention and resolution by senior leadership.15 Tier 4 huddles at the Veterans Integrated Services Network level and Tier 5 huddles at the VHA Central Office level are being initiated. These additional levels will more effectively identify system-level risks and issues that may impact multiple VHA facilities and may be addressed through centralized functions and resources.
Tiered safety huddles have been found to be instrumental to ensuring the flow of information across organizations, improving multidisciplinary and leadership engagement and collaboration, as well as increasing accountability for safety. Tiered safety huddles increase situational awareness, which improves an organization’s ability to appropriately respond to safety concerns. Furthermore, tiered safety huddles enhance teamwork and interprofessional collaboration, and have been found to significantly increase the reporting of patient safety events.15-19
The VA Connecticut Healthcare System tiered huddles followed a pilot testing implementation process. After receiving executive-level commitment, an evidence-based process was enacted, including staff education, selecting a VMS, determining tier interaction, and deciding on metrics to track.15
Implementing Foundational Practices
To examine the progress of the implementation of the 4 foundational HRO practices, quarterly metrics derived from the OLT are reviewed to determine whether each is being implemented and sustained. The OLT also tracks progress over time. For example, at the 27 cohort 2 and lead sites that initiated leader coaching in 2021 and continued through 2022, coaches observed a 27% increase in leader rounding for high reliability and a 46% increase in the use of VMSs. For the 66 cohort 3 sites that began leader coaching in 2022, coaches documented similar changes, ranging from a 40% increase in leader rounding for high reliability to a 66% increase in the use of safety forums. Additional data continue to be collected and analyzed to publish more comprehensive findings.
DISCUSSION
Incorporating leader rounding for high reliability, VMSs, safety forums, and tiered safety huddles into daily operations is critical to building and sustaining a robust culture of safety.8 The 4 foundational HRO practices are instrumental in providing psychologically safe forums for staff to share concerns and actively participate. These practices also promote continual, efficient bidirectional communication throughout organizational lines and across services. The increased visibility and transparency of leaders demonstrate the importance of fostering trust, enhancing closed-loop communication with issues that arise, and building momentum to achieve high reliability. The interconnectedness of the foundational HRO practices identified and implemented by the VHA helps foster teamwork and collaboration built on trust, respect, enthusiasm for improvement, and the delivery of exceptional patient care.
CONCLUSIONS
Incorporating the 4 foundational practices into daily operations is beneficial to the delivery of safe, high-quality health care. This effective and sustained application can strengthen a health care organization on its journey to high reliability and establishing a culture of safety. To be effective, these foundational practices should be personalized to support the unique circumstances of every health care environment. While the exact methodology by which organizations implement these practices may differ, they will help organizations approach patient safety in a more transparent and thoughtful manner.
Acknowledgments
The authors thank Aaron M. Sawyer, PhD, PMP, and Jessica Fankhauser, MA, for their unwavering administrative support, and Jeff Wright for exceptional graphic design support.
1. Figueroa CA, Harrison R, Chauhan A, Meyer L. Priorities and challenges for health leadership and workforce management globally: a rapid review. BMC Health Serv Res. 2019;19(1):239. Published 2019 Apr 24. doi:10.1186/s12913-019-4080-7
2. What is a high reliability organization (HRO) in healthcare? Vizient. Accessed May 22, 2024. https://www.vizientinc.com/our-solutions/care-delivery-excellence/reliable-care-delivery
3. US Department of Veterans Affairs, VHA National Center for Patient Safety. VHA’s HRO journey officially begins. March 29, 2019. Accessed May 22, 2024. https://www.patientsafety.va.gov/features/VHA_s_HRO_journey_officially_begins.asp
4. Murray JS, Clifford J, Scott D, Kelly S, Hanover C. Leader rounding for high reliability and improved patient safety. Fed Pract. 2024;41(1):16-21. doi:10.12788/fp.0444
5. Ryan L, Jackson D, Woods C, Usher K. Intentional rounding – an integrative literature review. J Adv Nurs. 2019;75(6):1151-1161. doi:10.1111/jan.13897
6. Hedenstrom M, Harrilson A, Heath M, Dyess S. “What’s old is new again”: innovative health care leader rounding—a strategy to foster connection. Nurse
7. Blake PG, Bacon CT. Structured rounding to improve staff nurse satisfaction with leadership. Nurse Lead. 2020;18(5):461-466. doi:10.1016/j.mnl.2020.04.009
8. US Department of Veterans Affairs, Veterans Health Administration. Leader’s guide to foundational high reliability organization (HRO) practices. https://dvagov.sharepoint.com/sites/OHT-PMO/high-reliability/Pages/default.aspx
9. Goyal A, Glanzman H, Quinn M, et al. Do bedside whiteboards enhance communication in hospitals? An exploratory multimethod study of patient and nurse perspectives. BMJ Qual Saf. 2020;29(10):1-2. doi:10.1136/bmjqs-2019-01020810. Williamsson A, Dellve L, Karltun A. Nurses’ use of visual management in hospitals-a longitudinal, quantitative study on its implications on systems performance and working conditions. J Adv Nurs. 2019;75(4):760-771. doi:10.1111/jan.13855
11. Prineas S, Culwick M, Endlich Y. A proposed system for standardization of colour-coding stages of escalating criticality in clinical incidents. Curr Opin Anaesthesiol. 2021;34(6):752-760. doi:10.1097/ACO.0000000000001071
12. Murray JS, Clifford J, Larson S, Lee JK, Sculli GL. Implementing just culture to improve patient safety. Mil Med. 2023;188(7-8):1596-1599. doi:10.1093/milmed/usac115
13. Murray JS, Kelly S, Hanover C. Promoting psychological safety in healthcare organizations. Mil Med. 2022;187(7-8):808-810. doi:10.1093/milmed/usac041
14. Merchant NB, O’Neal J, Murray JS. Development of a safety awards program at a veterans affairs health care system: a quality improvement initiative. J Clin Outcomes Manag. 2023;30(1):9-16. doi:10.12788/jcom.0120
15. Merchant NB, O’Neal J, Montoya A, Cox GR, Murray JS. Creating a process for the implementation of tiered huddles in a veterans affairs medical center. Mil Med. 2023;188(5-6):901-906. doi:10.1093/milmed/usac073
16. Mihaljevic T. Tiered daily huddles: the power of teamwork in managing large healthcare organisations. BMJ Qual Saf. 2020;29(12):1050-1052. doi:10.1136/bmjqs-2019-010575
17. Franklin BJ, Gandhi TK, Bates DW, et al. Impact of multidisciplinary team huddles on patient safety: a systematic review and proposed taxonomy. BMJ Qual Saf. 2020;29(10):1-2. doi:10.1136/bmjqs-2019-009911
18. Pimentel CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36(9):2772-2783. doi:10.1007/s11606-021-06632-9
19. Adapa K, Ivester T, Shea C, et al. The effect of a system-level tiered huddle system on reporting patient safety events: an interrupted time series analysis. Jt Comm J Qual Patient Saf. 2022;48(12):642-652. doi:10.1016/j.jcjq.2022.08.005
Increasing complexities within health care systems are significant impediments to the consistent delivery of safe and effective patient care. These impediments include an increase in specialization of care, staff shortages, burnout, poor coordination of services and access to care, as well as rising costs.1 High reliability organizations (HROs) provide safe, high-quality, and effective care in highly complex and risk-prone environments without causing harm or experiencing catastrophic events.2
Within the US Department of Veterans Affairs (VA), the Veterans Health Administration (VHA) operates the nation’s largest integrated health care system, providing care to > 9 million veterans. The VHA formally launched plans for an enterprise-wide HRO in February 2019. During the first year, 18 medical facilities comprised cohort1 of the journey to high reliability. Cohort 2 began in October 2020 and consisted of 54 facilities. Cohort 3 started in October 2021 with 67 facilities.3
Health care organizations seeking high reliability exercise a philosophy aimed at learning from errors and addressing system failures. High reliability is accomplished by implementing 5 principles: (1) sensitivity to operations (a heightened understanding of the current state of systems); (2) preoccupation with failure (striving to anticipate risks that might suggest a much larger system problem); (3) reluctance to simplify (avoiding making any assumptions regarding the causes of failures); (4) commitment to resilience (preparing for potential failures and bouncing back when they occur); and (5) deference to expertise (deferring to individuals with the skills and proficiency to make the best decisions).2 The VHA also recognized that a successful journey to high reliability—in addition to achieving a culture of safety—relies on the implementation of foundational HRO practices: leader rounding, visual management systems, safety forums, and safety huddles. This article describes an initiative for how these foundational practices were implemented in a large integrated health care system.
BACKGROUND
The VHA has focused on 4 foundational components as part of its enterprise activities and support structure to implement HRO principles and practices. These components were selected based on pilot activities that preceded the enterprise-wide effort, reviews of the literature, and expert consultation with both government and private sector health systems. To support the implementation of these practices, the VHA provided training, toolkits, HRO executive leader coaching, and peer-to-peer mentoring. As the VHA enters its fifth year seeking high reliability, we undertook an initiative to reflect on our own experiences and refine our practices based on an updated literature review.
As part of this enterprise-wide initiative, we conducted a literature review from 2018 to March 2023 seeking recent evidence describing the value of implementing the 4 foundational HRO practices to advance high reliability and improve patient safety. A 5-year period was used to ensure recency and value of evidence.
Eligible literature was identified in PubMed, PsycINFO, the Cumulative Index to Nursing and Allied Health Literature, ScienceDirect, Scopus, the Cochrane Library, and ProQuest Dissertations & Theses Global. Inclusion and exclusion criteria were peer-reviewed interdisciplinary documents(eg, publications, dissertations, conference proceedings, and grey literature) written in English. Search terms included high reliability organizations, foundational practices, and patient safety. Boolean operators (AND, OR) were also used in the search. The search resulted in a dearth of evidence that addressed implementation of all 4 foundational practices across a health care system. Retrieved evidence focused on the implementation of only 1 particular foundational practice in a specific health care setting. In addition to describing the formal processes for the implementation of each foundational HRO practice, a brief description of representative examples of strong practices within the VHA is provided.
To support the implementation of HROs, the VHA paired HRO executive leader coaches with select medical center directors and their leadership teams. Executive leader coaches also support an organization’s HRO Lead and HRO Champion. The HRO Lead coordinates and facilitates the implementation of HRO principles and practices in pursuit of no harm across an organization. The HRO Champion supports the same as the HRO Lead, but typically has a different specialty background. For example, if the HRO Lead has an administrative background, the HRO Champion would have a clinical background.
Coaching focuses heavily on supporting site-specific implementation and sustainment of the 4 HRO foundational practices. The aim is to accelerate change, build enduring capacity, foster a safety culture, and accelerate HRO maturity. To measure change, HRO executive leader coaches track the progress of their aligned VA medical centers (VAMCs) using the Organizational Learning Tool (OLT). This tool was developed to provide information such as a facility summary and relationships between a medical center director, HRO Lead, HRO Champion, and the executive leader coach (Figure 1). The OLT also serves as a structured process to measure leader coaching performance against mutually agreed upon objectives that ultimately contribute to enterprise outcomes. It also collects data on the progress in implementing foundational practices, strong practices, needs and gaps, and more (Figure 2). Data collected from facilities supported by HRO executive leader coaches on whether foundational practices are in place are briefly described.
Leader Rounding
Leader rounding for high reliability ensures effective, bidirectional communication and collaboration among all disciplines to improve patient safety. It is an essential feature of a robust patient safety culture and an important method for demonstrating leadership engagement with high reliability.4,5 These rounds are conducted by organizational leadership (eg, executive teams, department/service chiefs, or unit managers) and frontline staff from different areas. They are specifically focused on high reliability, patient and staff safety, and improvement efforts. The aim is to learn about daily challenges that may contribute to patient harm.4
Leader rounding has been found to be highly effective at improving leadership visibility across the organization. It enhances interaction and open communication with frontline staff, fostering leader-staff collaboration and shared decision-making, as well as promoting leadership understanding of operational, clinical, nonclinical (eg, administrative, nutrition services, or facilities management), and patient/family experience issues.4 Collaboration among team members fosters the delivery of more effective and efficient care, increases staff satisfaction, and improves employee retention.6 Leader rounding for high reliability significantly contributes to the breakdown of power barriers by giving team members voice and agency, ultimately leading to deeper engagement.7
It is important that leader rounding for high reliability occurs as planned and when possible, scheduled in advance. This helps to avoid rounding at peak times when care activities are being performed.4,6 When scheduling conflicts arise, another leader should be sent to participate in rounds.4 Developing a list of questions in advance allows leadership to prepare messaging to share with staff as it relates to high reliability and patient safety (Table).4,6,8
Closing the loop improves bidirectional communication and is critical to leader rounding for high reliability. Closed-loop communication and following up on and/or closing out issues raised during rounding empowers the sharing of information, which is critical for advancing a culture of safety.4,8 Enhanced feedback is also associated with greater workforce engagement, staff feeling more connected to quality improvement activities, and lower rates of employee burnout.7 It is important to recognize that senior leaders are not responsible for resolving all issues. If a team or manager can resolve concerns that are raised, this should be encouraged and supported. Maintaining accountability at the lowest level of the organization promotes principles and practices of high reliability (Figure 3).4,8
The VA Bedford Healthcare System created and implemented a strong practice for leader rounding for high reliability. This phased implementation involved creating an evidence-based process, deciding on an appropriate cadence, developing a tracking tool, and measuring impact to determine the overall effectiveness of leader rounding for high reliability.4
Visual Management Systems
A visual management system (VMS) displays clinical and operational performance aligned with HRO goals and practices. It is used to view and guide discussions between interdisciplinary teams during tiered safety huddles, leader rounds for high reliability, and frontline staff on the current status and safety trends in a particular area.8,9 A VMS is highly effective in creating an environment where all staff members, especially frontline workers, feel empowered to voice their concerns related to safety or to identify improvement opportunities.8,10 Increased leader engagement in patient safety and heightened transparency of information associated with the use of a VMS improves staff morale and professional satisfaction.10
A VMS may be a dry-erase or whiteboard display, paper-based display, or electronic status board.8 VMSs are usually located in or near work settings (eg, nurses’ station, staff break room, or conference room).8 Although they can take different forms and display several types of information, a VMS should be easy to update and meet the specific needs of a work area. In the VHA, a VMS displays: (1) essential information for staff members to effectively perform their work; (2) improvement project ideas; (3) current work in progress; (4) tracking of implemented improvement activities; (5) strong practices that have been effective; and (6) staff recognition for those who have enhanced patient safety, including the reporting of close calls and near misses.
The VHA uses the MESS (methods, equipment, staffing, and supplies) VMS format. This format empowers staff to identify whether proper procedures and practices are in place, essential equipment and supplies are readily available in the quantity needed, and appropriate staffing is on hand to provide safe, high-quality patient care.8 Colored magnets are used as visual cues in a stoplight classification system to identify low or no safety risks (green), at risk (yellow), or high risk (red). Green coded issues are addressed locally by a manager or supervisor. Yellow coded concerns require increased staff and leadership vigilance. Red coded issues indicate that patient care would be impacted that day and therefore need to be immediately escalated and addressed with senior leaders to mitigate the threat.4,11 Dayton VAMC successfully implemented a VMS, using both physical and electronic visual management boards. The Dayton VAMC VMS boards are closely tied to tiered safety huddles and leader rounding for high reliability.
Safety Forums
Safety forums are another foundational practice of VHA health care organizations seeking high reliability. Recurring monthly, safety forums focus on reinforcing HRO principles and practices, safety programs, the importance and appreciation of reporting, and just culture. The emphasis on just culture reminds staff that adverse events in the organization are viewed as valuable learning opportunities to understand the factors leading to the situation as opposed to immediately assigning blame.12
Psychological safety is another important focus. When individuals feel psychologically safe, they are more likely to voice concerns and act without fear of reprisal, which supports a culture of safety.13 Safety forums are open to all members of the health care organization, including both clinical and nonclinical staff. Forums can be conducted by an HRO Lead, HRO Champion, Patient Safety Manager, or even executive leadership. Rotating the responsibility of leading these forums demonstrates that high reliability and safety are everyone’s responsibility.
Safety forums publicly review and discuss errors, adverse events, close calls, and near misses. Time is also spent discussing root cause analysis trends and highlighting continuous process improvement principles and current projects. During safety forums, leaders should recognize individuals for safety behaviors and reward reporting through a safety awards program.14 All forums should conclude with a question-and-answer session. Forums typically occur in virtual 30-minute sessions but can last up to 60 minutes when guest speakers attend and continuing education credit is offered.
The Jesse Brown VAMC in Chicago developed an interactive monthly safety forum appealing to a broad audience. Each forum is attended by about 200 staff members and includes leader engagement and panel discussions led by the chief medical officer, with topics on both patient and team safety connecting with HRO principles. A planning committee prepares guest speakers and offers continuing education credits.
Tiered Safety Huddles
Based on the processes of high reliability industries like aviation and nuclear power, tiered safety huddles have been increasingly adopted in health care. Huddles (health care, utilizing, deliberate, discussion,linking, and events) are department-level interdisciplinary meetings that last no more than 15 minutes.15 Their purpose is to improve communication by sharing day-to-day information across multiple disciplines, identify issues that may impact the delivery of care (eg, patient and staff safety concerns, staffing issues, or inadequate supplies) and resolve problems.
Tiered safety huddles are gaining popularity, especially in organizations seeking high reliability. They are more complex than traditional huddles because of the mechanics of elevating safety issues (eg, bedside to executive leadership teams), feedback loops, and sequencing, among other factors.15,16
Tiered safety huddles are focused, transparent forums with multidisciplinary staff, including frontline workers, along with senior leadership.15,16 When initially implemented, tiered safety huddles may take longer than the suggested 15 minutes; however, as teams become more experienced, huddles become more efficient.15 The goal of tiered safety huddles is to proactively identify, share, address, and resolve problems that have the potential to impact the delivery of safe and quality patient care. This may include addressing staffing shortfalls, inadequate allocation of supplies and equipment, operational issues, etc.8,15 Critical to theeffective utilization of tiered safety huddles is the appropriate escalation of issues between tiers. The most critical issues are elevated to higher tiers so they are addressed by the most qualified person in the organization.
Deciding on the number of tiers typically depends on the size and scope of services provided by the health care organization or integrated system. For example, tiered huddles in the VHA originate at the point of service (eg, critical care unit). Tier 1 includes staff members at the unit/team level along with immediate supervisors/managers. Tier 2 involves departments and service lines (eg, pharmacy, podiatry, or internal medicine) including their respective leadership. Tier 3 is the executive leadership team. This process allows for bidirectional communication instead of the traditional hierarchical communication pathway (Figure 4). Issues identified that cannot be addressed at a particular tier are elevated to the next tier. Elevated issues typically involve systems or processes requiring attention and resolution by senior leadership.15 Tier 4 huddles at the Veterans Integrated Services Network level and Tier 5 huddles at the VHA Central Office level are being initiated. These additional levels will more effectively identify system-level risks and issues that may impact multiple VHA facilities and may be addressed through centralized functions and resources.
Tiered safety huddles have been found to be instrumental to ensuring the flow of information across organizations, improving multidisciplinary and leadership engagement and collaboration, as well as increasing accountability for safety. Tiered safety huddles increase situational awareness, which improves an organization’s ability to appropriately respond to safety concerns. Furthermore, tiered safety huddles enhance teamwork and interprofessional collaboration, and have been found to significantly increase the reporting of patient safety events.15-19
The VA Connecticut Healthcare System tiered huddles followed a pilot testing implementation process. After receiving executive-level commitment, an evidence-based process was enacted, including staff education, selecting a VMS, determining tier interaction, and deciding on metrics to track.15
Implementing Foundational Practices
To examine the progress of the implementation of the 4 foundational HRO practices, quarterly metrics derived from the OLT are reviewed to determine whether each is being implemented and sustained. The OLT also tracks progress over time. For example, at the 27 cohort 2 and lead sites that initiated leader coaching in 2021 and continued through 2022, coaches observed a 27% increase in leader rounding for high reliability and a 46% increase in the use of VMSs. For the 66 cohort 3 sites that began leader coaching in 2022, coaches documented similar changes, ranging from a 40% increase in leader rounding for high reliability to a 66% increase in the use of safety forums. Additional data continue to be collected and analyzed to publish more comprehensive findings.
DISCUSSION
Incorporating leader rounding for high reliability, VMSs, safety forums, and tiered safety huddles into daily operations is critical to building and sustaining a robust culture of safety.8 The 4 foundational HRO practices are instrumental in providing psychologically safe forums for staff to share concerns and actively participate. These practices also promote continual, efficient bidirectional communication throughout organizational lines and across services. The increased visibility and transparency of leaders demonstrate the importance of fostering trust, enhancing closed-loop communication with issues that arise, and building momentum to achieve high reliability. The interconnectedness of the foundational HRO practices identified and implemented by the VHA helps foster teamwork and collaboration built on trust, respect, enthusiasm for improvement, and the delivery of exceptional patient care.
CONCLUSIONS
Incorporating the 4 foundational practices into daily operations is beneficial to the delivery of safe, high-quality health care. This effective and sustained application can strengthen a health care organization on its journey to high reliability and establishing a culture of safety. To be effective, these foundational practices should be personalized to support the unique circumstances of every health care environment. While the exact methodology by which organizations implement these practices may differ, they will help organizations approach patient safety in a more transparent and thoughtful manner.
Acknowledgments
The authors thank Aaron M. Sawyer, PhD, PMP, and Jessica Fankhauser, MA, for their unwavering administrative support, and Jeff Wright for exceptional graphic design support.
Increasing complexities within health care systems are significant impediments to the consistent delivery of safe and effective patient care. These impediments include an increase in specialization of care, staff shortages, burnout, poor coordination of services and access to care, as well as rising costs.1 High reliability organizations (HROs) provide safe, high-quality, and effective care in highly complex and risk-prone environments without causing harm or experiencing catastrophic events.2
Within the US Department of Veterans Affairs (VA), the Veterans Health Administration (VHA) operates the nation’s largest integrated health care system, providing care to > 9 million veterans. The VHA formally launched plans for an enterprise-wide HRO in February 2019. During the first year, 18 medical facilities comprised cohort1 of the journey to high reliability. Cohort 2 began in October 2020 and consisted of 54 facilities. Cohort 3 started in October 2021 with 67 facilities.3
Health care organizations seeking high reliability exercise a philosophy aimed at learning from errors and addressing system failures. High reliability is accomplished by implementing 5 principles: (1) sensitivity to operations (a heightened understanding of the current state of systems); (2) preoccupation with failure (striving to anticipate risks that might suggest a much larger system problem); (3) reluctance to simplify (avoiding making any assumptions regarding the causes of failures); (4) commitment to resilience (preparing for potential failures and bouncing back when they occur); and (5) deference to expertise (deferring to individuals with the skills and proficiency to make the best decisions).2 The VHA also recognized that a successful journey to high reliability—in addition to achieving a culture of safety—relies on the implementation of foundational HRO practices: leader rounding, visual management systems, safety forums, and safety huddles. This article describes an initiative for how these foundational practices were implemented in a large integrated health care system.
BACKGROUND
The VHA has focused on 4 foundational components as part of its enterprise activities and support structure to implement HRO principles and practices. These components were selected based on pilot activities that preceded the enterprise-wide effort, reviews of the literature, and expert consultation with both government and private sector health systems. To support the implementation of these practices, the VHA provided training, toolkits, HRO executive leader coaching, and peer-to-peer mentoring. As the VHA enters its fifth year seeking high reliability, we undertook an initiative to reflect on our own experiences and refine our practices based on an updated literature review.
As part of this enterprise-wide initiative, we conducted a literature review from 2018 to March 2023 seeking recent evidence describing the value of implementing the 4 foundational HRO practices to advance high reliability and improve patient safety. A 5-year period was used to ensure recency and value of evidence.
Eligible literature was identified in PubMed, PsycINFO, the Cumulative Index to Nursing and Allied Health Literature, ScienceDirect, Scopus, the Cochrane Library, and ProQuest Dissertations & Theses Global. Inclusion and exclusion criteria were peer-reviewed interdisciplinary documents(eg, publications, dissertations, conference proceedings, and grey literature) written in English. Search terms included high reliability organizations, foundational practices, and patient safety. Boolean operators (AND, OR) were also used in the search. The search resulted in a dearth of evidence that addressed implementation of all 4 foundational practices across a health care system. Retrieved evidence focused on the implementation of only 1 particular foundational practice in a specific health care setting. In addition to describing the formal processes for the implementation of each foundational HRO practice, a brief description of representative examples of strong practices within the VHA is provided.
To support the implementation of HROs, the VHA paired HRO executive leader coaches with select medical center directors and their leadership teams. Executive leader coaches also support an organization’s HRO Lead and HRO Champion. The HRO Lead coordinates and facilitates the implementation of HRO principles and practices in pursuit of no harm across an organization. The HRO Champion supports the same as the HRO Lead, but typically has a different specialty background. For example, if the HRO Lead has an administrative background, the HRO Champion would have a clinical background.
Coaching focuses heavily on supporting site-specific implementation and sustainment of the 4 HRO foundational practices. The aim is to accelerate change, build enduring capacity, foster a safety culture, and accelerate HRO maturity. To measure change, HRO executive leader coaches track the progress of their aligned VA medical centers (VAMCs) using the Organizational Learning Tool (OLT). This tool was developed to provide information such as a facility summary and relationships between a medical center director, HRO Lead, HRO Champion, and the executive leader coach (Figure 1). The OLT also serves as a structured process to measure leader coaching performance against mutually agreed upon objectives that ultimately contribute to enterprise outcomes. It also collects data on the progress in implementing foundational practices, strong practices, needs and gaps, and more (Figure 2). Data collected from facilities supported by HRO executive leader coaches on whether foundational practices are in place are briefly described.
Leader Rounding
Leader rounding for high reliability ensures effective, bidirectional communication and collaboration among all disciplines to improve patient safety. It is an essential feature of a robust patient safety culture and an important method for demonstrating leadership engagement with high reliability.4,5 These rounds are conducted by organizational leadership (eg, executive teams, department/service chiefs, or unit managers) and frontline staff from different areas. They are specifically focused on high reliability, patient and staff safety, and improvement efforts. The aim is to learn about daily challenges that may contribute to patient harm.4
Leader rounding has been found to be highly effective at improving leadership visibility across the organization. It enhances interaction and open communication with frontline staff, fostering leader-staff collaboration and shared decision-making, as well as promoting leadership understanding of operational, clinical, nonclinical (eg, administrative, nutrition services, or facilities management), and patient/family experience issues.4 Collaboration among team members fosters the delivery of more effective and efficient care, increases staff satisfaction, and improves employee retention.6 Leader rounding for high reliability significantly contributes to the breakdown of power barriers by giving team members voice and agency, ultimately leading to deeper engagement.7
It is important that leader rounding for high reliability occurs as planned and when possible, scheduled in advance. This helps to avoid rounding at peak times when care activities are being performed.4,6 When scheduling conflicts arise, another leader should be sent to participate in rounds.4 Developing a list of questions in advance allows leadership to prepare messaging to share with staff as it relates to high reliability and patient safety (Table).4,6,8
Closing the loop improves bidirectional communication and is critical to leader rounding for high reliability. Closed-loop communication and following up on and/or closing out issues raised during rounding empowers the sharing of information, which is critical for advancing a culture of safety.4,8 Enhanced feedback is also associated with greater workforce engagement, staff feeling more connected to quality improvement activities, and lower rates of employee burnout.7 It is important to recognize that senior leaders are not responsible for resolving all issues. If a team or manager can resolve concerns that are raised, this should be encouraged and supported. Maintaining accountability at the lowest level of the organization promotes principles and practices of high reliability (Figure 3).4,8
The VA Bedford Healthcare System created and implemented a strong practice for leader rounding for high reliability. This phased implementation involved creating an evidence-based process, deciding on an appropriate cadence, developing a tracking tool, and measuring impact to determine the overall effectiveness of leader rounding for high reliability.4
Visual Management Systems
A visual management system (VMS) displays clinical and operational performance aligned with HRO goals and practices. It is used to view and guide discussions between interdisciplinary teams during tiered safety huddles, leader rounds for high reliability, and frontline staff on the current status and safety trends in a particular area.8,9 A VMS is highly effective in creating an environment where all staff members, especially frontline workers, feel empowered to voice their concerns related to safety or to identify improvement opportunities.8,10 Increased leader engagement in patient safety and heightened transparency of information associated with the use of a VMS improves staff morale and professional satisfaction.10
A VMS may be a dry-erase or whiteboard display, paper-based display, or electronic status board.8 VMSs are usually located in or near work settings (eg, nurses’ station, staff break room, or conference room).8 Although they can take different forms and display several types of information, a VMS should be easy to update and meet the specific needs of a work area. In the VHA, a VMS displays: (1) essential information for staff members to effectively perform their work; (2) improvement project ideas; (3) current work in progress; (4) tracking of implemented improvement activities; (5) strong practices that have been effective; and (6) staff recognition for those who have enhanced patient safety, including the reporting of close calls and near misses.
The VHA uses the MESS (methods, equipment, staffing, and supplies) VMS format. This format empowers staff to identify whether proper procedures and practices are in place, essential equipment and supplies are readily available in the quantity needed, and appropriate staffing is on hand to provide safe, high-quality patient care.8 Colored magnets are used as visual cues in a stoplight classification system to identify low or no safety risks (green), at risk (yellow), or high risk (red). Green coded issues are addressed locally by a manager or supervisor. Yellow coded concerns require increased staff and leadership vigilance. Red coded issues indicate that patient care would be impacted that day and therefore need to be immediately escalated and addressed with senior leaders to mitigate the threat.4,11 Dayton VAMC successfully implemented a VMS, using both physical and electronic visual management boards. The Dayton VAMC VMS boards are closely tied to tiered safety huddles and leader rounding for high reliability.
Safety Forums
Safety forums are another foundational practice of VHA health care organizations seeking high reliability. Recurring monthly, safety forums focus on reinforcing HRO principles and practices, safety programs, the importance and appreciation of reporting, and just culture. The emphasis on just culture reminds staff that adverse events in the organization are viewed as valuable learning opportunities to understand the factors leading to the situation as opposed to immediately assigning blame.12
Psychological safety is another important focus. When individuals feel psychologically safe, they are more likely to voice concerns and act without fear of reprisal, which supports a culture of safety.13 Safety forums are open to all members of the health care organization, including both clinical and nonclinical staff. Forums can be conducted by an HRO Lead, HRO Champion, Patient Safety Manager, or even executive leadership. Rotating the responsibility of leading these forums demonstrates that high reliability and safety are everyone’s responsibility.
Safety forums publicly review and discuss errors, adverse events, close calls, and near misses. Time is also spent discussing root cause analysis trends and highlighting continuous process improvement principles and current projects. During safety forums, leaders should recognize individuals for safety behaviors and reward reporting through a safety awards program.14 All forums should conclude with a question-and-answer session. Forums typically occur in virtual 30-minute sessions but can last up to 60 minutes when guest speakers attend and continuing education credit is offered.
The Jesse Brown VAMC in Chicago developed an interactive monthly safety forum appealing to a broad audience. Each forum is attended by about 200 staff members and includes leader engagement and panel discussions led by the chief medical officer, with topics on both patient and team safety connecting with HRO principles. A planning committee prepares guest speakers and offers continuing education credits.
Tiered Safety Huddles
Based on the processes of high reliability industries like aviation and nuclear power, tiered safety huddles have been increasingly adopted in health care. Huddles (health care, utilizing, deliberate, discussion,linking, and events) are department-level interdisciplinary meetings that last no more than 15 minutes.15 Their purpose is to improve communication by sharing day-to-day information across multiple disciplines, identify issues that may impact the delivery of care (eg, patient and staff safety concerns, staffing issues, or inadequate supplies) and resolve problems.
Tiered safety huddles are gaining popularity, especially in organizations seeking high reliability. They are more complex than traditional huddles because of the mechanics of elevating safety issues (eg, bedside to executive leadership teams), feedback loops, and sequencing, among other factors.15,16
Tiered safety huddles are focused, transparent forums with multidisciplinary staff, including frontline workers, along with senior leadership.15,16 When initially implemented, tiered safety huddles may take longer than the suggested 15 minutes; however, as teams become more experienced, huddles become more efficient.15 The goal of tiered safety huddles is to proactively identify, share, address, and resolve problems that have the potential to impact the delivery of safe and quality patient care. This may include addressing staffing shortfalls, inadequate allocation of supplies and equipment, operational issues, etc.8,15 Critical to theeffective utilization of tiered safety huddles is the appropriate escalation of issues between tiers. The most critical issues are elevated to higher tiers so they are addressed by the most qualified person in the organization.
Deciding on the number of tiers typically depends on the size and scope of services provided by the health care organization or integrated system. For example, tiered huddles in the VHA originate at the point of service (eg, critical care unit). Tier 1 includes staff members at the unit/team level along with immediate supervisors/managers. Tier 2 involves departments and service lines (eg, pharmacy, podiatry, or internal medicine) including their respective leadership. Tier 3 is the executive leadership team. This process allows for bidirectional communication instead of the traditional hierarchical communication pathway (Figure 4). Issues identified that cannot be addressed at a particular tier are elevated to the next tier. Elevated issues typically involve systems or processes requiring attention and resolution by senior leadership.15 Tier 4 huddles at the Veterans Integrated Services Network level and Tier 5 huddles at the VHA Central Office level are being initiated. These additional levels will more effectively identify system-level risks and issues that may impact multiple VHA facilities and may be addressed through centralized functions and resources.
Tiered safety huddles have been found to be instrumental to ensuring the flow of information across organizations, improving multidisciplinary and leadership engagement and collaboration, as well as increasing accountability for safety. Tiered safety huddles increase situational awareness, which improves an organization’s ability to appropriately respond to safety concerns. Furthermore, tiered safety huddles enhance teamwork and interprofessional collaboration, and have been found to significantly increase the reporting of patient safety events.15-19
The VA Connecticut Healthcare System tiered huddles followed a pilot testing implementation process. After receiving executive-level commitment, an evidence-based process was enacted, including staff education, selecting a VMS, determining tier interaction, and deciding on metrics to track.15
Implementing Foundational Practices
To examine the progress of the implementation of the 4 foundational HRO practices, quarterly metrics derived from the OLT are reviewed to determine whether each is being implemented and sustained. The OLT also tracks progress over time. For example, at the 27 cohort 2 and lead sites that initiated leader coaching in 2021 and continued through 2022, coaches observed a 27% increase in leader rounding for high reliability and a 46% increase in the use of VMSs. For the 66 cohort 3 sites that began leader coaching in 2022, coaches documented similar changes, ranging from a 40% increase in leader rounding for high reliability to a 66% increase in the use of safety forums. Additional data continue to be collected and analyzed to publish more comprehensive findings.
DISCUSSION
Incorporating leader rounding for high reliability, VMSs, safety forums, and tiered safety huddles into daily operations is critical to building and sustaining a robust culture of safety.8 The 4 foundational HRO practices are instrumental in providing psychologically safe forums for staff to share concerns and actively participate. These practices also promote continual, efficient bidirectional communication throughout organizational lines and across services. The increased visibility and transparency of leaders demonstrate the importance of fostering trust, enhancing closed-loop communication with issues that arise, and building momentum to achieve high reliability. The interconnectedness of the foundational HRO practices identified and implemented by the VHA helps foster teamwork and collaboration built on trust, respect, enthusiasm for improvement, and the delivery of exceptional patient care.
CONCLUSIONS
Incorporating the 4 foundational practices into daily operations is beneficial to the delivery of safe, high-quality health care. This effective and sustained application can strengthen a health care organization on its journey to high reliability and establishing a culture of safety. To be effective, these foundational practices should be personalized to support the unique circumstances of every health care environment. While the exact methodology by which organizations implement these practices may differ, they will help organizations approach patient safety in a more transparent and thoughtful manner.
Acknowledgments
The authors thank Aaron M. Sawyer, PhD, PMP, and Jessica Fankhauser, MA, for their unwavering administrative support, and Jeff Wright for exceptional graphic design support.
1. Figueroa CA, Harrison R, Chauhan A, Meyer L. Priorities and challenges for health leadership and workforce management globally: a rapid review. BMC Health Serv Res. 2019;19(1):239. Published 2019 Apr 24. doi:10.1186/s12913-019-4080-7
2. What is a high reliability organization (HRO) in healthcare? Vizient. Accessed May 22, 2024. https://www.vizientinc.com/our-solutions/care-delivery-excellence/reliable-care-delivery
3. US Department of Veterans Affairs, VHA National Center for Patient Safety. VHA’s HRO journey officially begins. March 29, 2019. Accessed May 22, 2024. https://www.patientsafety.va.gov/features/VHA_s_HRO_journey_officially_begins.asp
4. Murray JS, Clifford J, Scott D, Kelly S, Hanover C. Leader rounding for high reliability and improved patient safety. Fed Pract. 2024;41(1):16-21. doi:10.12788/fp.0444
5. Ryan L, Jackson D, Woods C, Usher K. Intentional rounding – an integrative literature review. J Adv Nurs. 2019;75(6):1151-1161. doi:10.1111/jan.13897
6. Hedenstrom M, Harrilson A, Heath M, Dyess S. “What’s old is new again”: innovative health care leader rounding—a strategy to foster connection. Nurse
7. Blake PG, Bacon CT. Structured rounding to improve staff nurse satisfaction with leadership. Nurse Lead. 2020;18(5):461-466. doi:10.1016/j.mnl.2020.04.009
8. US Department of Veterans Affairs, Veterans Health Administration. Leader’s guide to foundational high reliability organization (HRO) practices. https://dvagov.sharepoint.com/sites/OHT-PMO/high-reliability/Pages/default.aspx
9. Goyal A, Glanzman H, Quinn M, et al. Do bedside whiteboards enhance communication in hospitals? An exploratory multimethod study of patient and nurse perspectives. BMJ Qual Saf. 2020;29(10):1-2. doi:10.1136/bmjqs-2019-01020810. Williamsson A, Dellve L, Karltun A. Nurses’ use of visual management in hospitals-a longitudinal, quantitative study on its implications on systems performance and working conditions. J Adv Nurs. 2019;75(4):760-771. doi:10.1111/jan.13855
11. Prineas S, Culwick M, Endlich Y. A proposed system for standardization of colour-coding stages of escalating criticality in clinical incidents. Curr Opin Anaesthesiol. 2021;34(6):752-760. doi:10.1097/ACO.0000000000001071
12. Murray JS, Clifford J, Larson S, Lee JK, Sculli GL. Implementing just culture to improve patient safety. Mil Med. 2023;188(7-8):1596-1599. doi:10.1093/milmed/usac115
13. Murray JS, Kelly S, Hanover C. Promoting psychological safety in healthcare organizations. Mil Med. 2022;187(7-8):808-810. doi:10.1093/milmed/usac041
14. Merchant NB, O’Neal J, Murray JS. Development of a safety awards program at a veterans affairs health care system: a quality improvement initiative. J Clin Outcomes Manag. 2023;30(1):9-16. doi:10.12788/jcom.0120
15. Merchant NB, O’Neal J, Montoya A, Cox GR, Murray JS. Creating a process for the implementation of tiered huddles in a veterans affairs medical center. Mil Med. 2023;188(5-6):901-906. doi:10.1093/milmed/usac073
16. Mihaljevic T. Tiered daily huddles: the power of teamwork in managing large healthcare organisations. BMJ Qual Saf. 2020;29(12):1050-1052. doi:10.1136/bmjqs-2019-010575
17. Franklin BJ, Gandhi TK, Bates DW, et al. Impact of multidisciplinary team huddles on patient safety: a systematic review and proposed taxonomy. BMJ Qual Saf. 2020;29(10):1-2. doi:10.1136/bmjqs-2019-009911
18. Pimentel CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36(9):2772-2783. doi:10.1007/s11606-021-06632-9
19. Adapa K, Ivester T, Shea C, et al. The effect of a system-level tiered huddle system on reporting patient safety events: an interrupted time series analysis. Jt Comm J Qual Patient Saf. 2022;48(12):642-652. doi:10.1016/j.jcjq.2022.08.005
1. Figueroa CA, Harrison R, Chauhan A, Meyer L. Priorities and challenges for health leadership and workforce management globally: a rapid review. BMC Health Serv Res. 2019;19(1):239. Published 2019 Apr 24. doi:10.1186/s12913-019-4080-7
2. What is a high reliability organization (HRO) in healthcare? Vizient. Accessed May 22, 2024. https://www.vizientinc.com/our-solutions/care-delivery-excellence/reliable-care-delivery
3. US Department of Veterans Affairs, VHA National Center for Patient Safety. VHA’s HRO journey officially begins. March 29, 2019. Accessed May 22, 2024. https://www.patientsafety.va.gov/features/VHA_s_HRO_journey_officially_begins.asp
4. Murray JS, Clifford J, Scott D, Kelly S, Hanover C. Leader rounding for high reliability and improved patient safety. Fed Pract. 2024;41(1):16-21. doi:10.12788/fp.0444
5. Ryan L, Jackson D, Woods C, Usher K. Intentional rounding – an integrative literature review. J Adv Nurs. 2019;75(6):1151-1161. doi:10.1111/jan.13897
6. Hedenstrom M, Harrilson A, Heath M, Dyess S. “What’s old is new again”: innovative health care leader rounding—a strategy to foster connection. Nurse
7. Blake PG, Bacon CT. Structured rounding to improve staff nurse satisfaction with leadership. Nurse Lead. 2020;18(5):461-466. doi:10.1016/j.mnl.2020.04.009
8. US Department of Veterans Affairs, Veterans Health Administration. Leader’s guide to foundational high reliability organization (HRO) practices. https://dvagov.sharepoint.com/sites/OHT-PMO/high-reliability/Pages/default.aspx
9. Goyal A, Glanzman H, Quinn M, et al. Do bedside whiteboards enhance communication in hospitals? An exploratory multimethod study of patient and nurse perspectives. BMJ Qual Saf. 2020;29(10):1-2. doi:10.1136/bmjqs-2019-01020810. Williamsson A, Dellve L, Karltun A. Nurses’ use of visual management in hospitals-a longitudinal, quantitative study on its implications on systems performance and working conditions. J Adv Nurs. 2019;75(4):760-771. doi:10.1111/jan.13855
11. Prineas S, Culwick M, Endlich Y. A proposed system for standardization of colour-coding stages of escalating criticality in clinical incidents. Curr Opin Anaesthesiol. 2021;34(6):752-760. doi:10.1097/ACO.0000000000001071
12. Murray JS, Clifford J, Larson S, Lee JK, Sculli GL. Implementing just culture to improve patient safety. Mil Med. 2023;188(7-8):1596-1599. doi:10.1093/milmed/usac115
13. Murray JS, Kelly S, Hanover C. Promoting psychological safety in healthcare organizations. Mil Med. 2022;187(7-8):808-810. doi:10.1093/milmed/usac041
14. Merchant NB, O’Neal J, Murray JS. Development of a safety awards program at a veterans affairs health care system: a quality improvement initiative. J Clin Outcomes Manag. 2023;30(1):9-16. doi:10.12788/jcom.0120
15. Merchant NB, O’Neal J, Montoya A, Cox GR, Murray JS. Creating a process for the implementation of tiered huddles in a veterans affairs medical center. Mil Med. 2023;188(5-6):901-906. doi:10.1093/milmed/usac073
16. Mihaljevic T. Tiered daily huddles: the power of teamwork in managing large healthcare organisations. BMJ Qual Saf. 2020;29(12):1050-1052. doi:10.1136/bmjqs-2019-010575
17. Franklin BJ, Gandhi TK, Bates DW, et al. Impact of multidisciplinary team huddles on patient safety: a systematic review and proposed taxonomy. BMJ Qual Saf. 2020;29(10):1-2. doi:10.1136/bmjqs-2019-009911
18. Pimentel CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36(9):2772-2783. doi:10.1007/s11606-021-06632-9
19. Adapa K, Ivester T, Shea C, et al. The effect of a system-level tiered huddle system on reporting patient safety events: an interrupted time series analysis. Jt Comm J Qual Patient Saf. 2022;48(12):642-652. doi:10.1016/j.jcjq.2022.08.005
Potential Impact of USPS Mail Delivery Delays on Colorectal Cancer Screening Programs
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States.1 In 2022, there were an estimated 151,030 new CRC cases and 52,580 deaths.1 Options for CRC screening of patients at average risk include stool tests (annual fecal immunochemical test [FIT], annual guaiac-based fecal occult blood test, or stool FIT-DNA test every 1 to 3 years), colonoscopies every 10 years, flexible sigmoidoscopies every 5 years (or every 10 years with annual FIT), and computed tomography (CT) colonography every 5 years.2 Many health care systems use annual FIT for patients at average risk. Compared with guaiac-based fecal occult blood testing, FIT does not require dietary or medication modifications and yields greater sensitivity and patient participation.3
The COVID-19 pandemic and staffing issues have caused a scheduling backlog for screening, diagnostic, and surveillance endoscopies at some medical centers. As a result, FIT has become the primary means of CRC screening at these institutions. FIT kits for home use are typically distributed to eligible patients at an office visit or by mail, and patients are then instructed to mail the kits back to the laboratory. For the test to be as sensitive as possible, FIT kit manufacturers advise laboratory analysis within 14 to 15 days of collection, if stored at ambient temperature, and to reject the sample if it does not meet testing criteria for stability. Delayed FIT sample analysis has been associated with higher false-negative rates because of hemoglobin degradation.4 FIT sample exposure to high ambient temperatures also has been linked to decreased sensitivity for detecting CRC.5
US Postal Service (USPS) mail delivery delays have plagued many areas of the country. A variety of factors, including the COVID-19 pandemic, understaffing, changes in USPS policies, closure of post offices, and changes in mail delivery standards, may also be contributory causes. According to the USPS website, delivery standard for first-class mail is 1 to 5 days, but this is not guaranteed.6
The Jesse Brown Veterans Affairs Medical Center (JBVAMC) laboratory in Chicago has reported receiving FIT kit envelopes in batches by the USPS, with some prepaid first-class business reply envelopes delivered up to 60 days after the time of sample collection. Polymedco, a company that assists US Department of Veterans Affairs (VA) medical centers with logistics of FIT programs for CRC screening, reports that USPS batching of FIT kits leading to delayed delivery has been a periodic problem for medical centers around the country. Polymedco staff remind USPS staff about 4 points when they encounter this issue: Mailers are first-class mail; mailers contain a human biologic specimen that has limited viability; the biological sample used for detecting cancer is time sensitive; and delays in delivery by holding/batching kits could impact morbidity and mortality. Reviewing these key points with local USPS staff usually helps, however, batching and delayed delivery of the FIT kits can sometimes recur with USPS staffing turnover.
Tracking and identifying when a patient receives the FIT kit is difficult. Patients are instructed to write the date of collection on the kit, so the receiving laboratory knows whether the sample can be reliably analyzed. When patients are notified about delayed delivery of their sample, a staff member asks if they postponed dropping the kit in the mail. Most patients report mailing the sample within 1 to 2 days of collection. Tracking and dating each step of FIT kit events is not feasible with a mass mailing campaign. In our experience, most patients write the date of collection on the kit. If a collection date is not provided, the laboratory will call the patient to confirm a date. Cheng and colleagues reviewed the causes for FIT specimen rejection in a laboratory analyzing specimens for VA patients and found that 14% of submitted samples were rejected because the specimen was received > 14 days after collection, and 6% because the patient did not record the collection date. With a series of interventions aimed at reminding patients and improving laboratory procedures, rates of rejection for these 2 causes were reduced to < 4%.7 USPS delays were not identified as a factor or tracked in this study.
It is unclear why the USPS sometimes holds FIT kits at their facilities and then delivers large bins of them at the same time. Because FIT kits should be analyzed within 14 to 15 days of sample collection to assure reliable results, mail delivery delays can result in increased sample rejection. Based on the JBVAMC experience, up to 30% of submitted samples might need to be discarded when batched delivery takes place. In these cases, patients need to be contacted, informed of the problem, and asked to submit new kits. Understandably, patients are reluctant to repeat this type of testing, and we are concerned this could lead to reduced rates of CRC screening in affected communities.
As an alternative to discarding delayed samples, laboratories could report the results of delayed FIT kits with an added comment that “negative test results may be less reliable due to delayed processing,” but this approach would raise quality and medicolegal concerns. Clinicians have reached out to local USPS supervisory personnel with mixed results. Sometimes batching and delayed deliveries stop for a few months, only to resume without warning. Dropping off the sample directly at the laboratory is not a realistic option for most patients. Some patients can be convinced to submit another sample, some elect to switch to other CRC screening strategies, while others, unfortunately, decline further screening efforts.
Laboratory staff can be overwhelmed with having to process hundreds of samples in a short time frame, especially because there is no way of knowing when USPS will make a batched delivery. Laboratory capacities can limit staff at some facilities to performing analysis of only 10 tests at a time. The FIT kits should be delivered on a rolling basis and without delay so that the samples can be reliably analyzed with a predictable workload for the laboratory personnel and without unexpected surges.
When health care facilities identify delayed mail delivery of FIT kits via USPS, laboratories should first ensure that the correct postage rates are used on the prepaid envelopes and that their USPS accounts are properly funded, so that insufficient funds are not contributing to delayed deliveries. Stakeholders should then reach out to local USPS supervisory staff and request that the practice of batching the delivery of FIT kits be stopped. Educating USPS supervisory staff about concerns related to decreased test reliability associated with delayed mail delivery can be a persuasive argument. Adding additional language to the preprinted envelopes, such as “time sensitive,” may also be helpful. Unfortunately, the JBVAMC experience has been that the problem initially gets better after contacting the USPS, only to unexpectedly resurface months later. This cycle has been repeated several times in the past 2 years at JBVAMC.
All clinicians involved in CRC screening and treatment at institutions that use FIT kits need to be aware of the impact that local USPS delays can have on the reliability of these results. Health care systems should be prepared to implement mitigation strategies if they encounter significant delays with mail delivery. If delays cannot be reliably resolved by working with the local USPS staff, consider involving national USPS oversight bodies. And if the problems persist despite an attempt to work with the USPS, some institutions might find it feasible to offer drop boxes at their clinics and instruct patients to drop off FIT kits immediately following collection, in lieu of mailing them. Switching to private carriers is not a cost-effective alternative for most health care systems, and some may exclude rural areas. Depending on the local availability and capacity of endoscopists, some clinicians might prioritize referring patients for screening colonoscopies or screening flexible sigmoidoscopies, and might deemphasize FIT kits as a preferred option for CRC screening. CT colonography is an alternative screening method that is not as widely offered, nor as widely accepted at this time.
Conclusions
CRC screening is an essential part of preventive medicine, and the percentage of eligible patients screened is a well-established quality metric in primary care settings. Health care systems, clinicians, and laboratories must be vigilant to ensure that USPS delays in delivering FIT kits do not negatively impact their CRC screening programs. Facilities should actively monitor for delays in the return of FIT kits.
Despite the widespread use of mail-order pharmacies and the use of mail to communicate notifications about test results and follow-up appointments, unreliable or delayed mail delivery traditionally has not been considered a social determinant of health.8 This article highlights the impact delayed mail delivery can have on health outcomes. Disadvantaged communities in inner cities and rural areas have been disproportionately affected by the worsening performance of the USPS over the past few years.9 This represents an underappreciated public health concern in need of a sustainable solution.
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
2. Centers for Disease Control and Prevention. Colorectal cancer screening tests. Updated February 23, 2023. Accessed March 14, 2024. https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
3. van Rossum LG, van Rijn AF, Laheij RJ, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135(1):82-90. doi:10.1053/j.gastro.2008.03.040
4. van Rossum LG, van Rijn AF, van Oijen MG, et al. False negative fecal occult blood tests due to delayed sample return in colorectal cancer screening. Int J Cancer. 2009;125(4):746-750. doi:10.1002/ijc.24458
5. Doubeni CA, Jensen CD, Fedewa SA, et al. Fecal immunochemical test (FIT) for colon cancer screening: variable performance with ambient temperature. J Am Board Fam Med. 2016;29(6):672-681. doi:10.3122/jabfm.2016.06.160060
6. United States Postal Service. Shipping and mailing with USPS. Accessed March 14, 2024. https://www.usps.com/ship
7. Cheng C, Ganz DA, Chang ET, Huynh A, De Peralta S. Reducing rejected fecal immunochemical tests received in the laboratory for colorectal cancer screening. J Healthc Qual. 2019;41(2):75-82.doi:10.1097/JHQ.0000000000000181
8. Hussaini SMQ, Alexander GC. The United States Postal Service: an essential public health agency? J Gen Intern Med. 2020;35(12):3699-3701. doi:10.1007/s11606-020-06275-2
9. Hampton DJ. Colorado mountain towns are plagued by post office delays as residents wait weeks for medication and retirement checks. NBC News. February 25, 2023. Accessed March 14, 2024. https://www.nbcnews.com/news/us-news/colo-mountain-towns-are-plagued-post-office-delays-residents-wait-week-rcna72085
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States.1 In 2022, there were an estimated 151,030 new CRC cases and 52,580 deaths.1 Options for CRC screening of patients at average risk include stool tests (annual fecal immunochemical test [FIT], annual guaiac-based fecal occult blood test, or stool FIT-DNA test every 1 to 3 years), colonoscopies every 10 years, flexible sigmoidoscopies every 5 years (or every 10 years with annual FIT), and computed tomography (CT) colonography every 5 years.2 Many health care systems use annual FIT for patients at average risk. Compared with guaiac-based fecal occult blood testing, FIT does not require dietary or medication modifications and yields greater sensitivity and patient participation.3
The COVID-19 pandemic and staffing issues have caused a scheduling backlog for screening, diagnostic, and surveillance endoscopies at some medical centers. As a result, FIT has become the primary means of CRC screening at these institutions. FIT kits for home use are typically distributed to eligible patients at an office visit or by mail, and patients are then instructed to mail the kits back to the laboratory. For the test to be as sensitive as possible, FIT kit manufacturers advise laboratory analysis within 14 to 15 days of collection, if stored at ambient temperature, and to reject the sample if it does not meet testing criteria for stability. Delayed FIT sample analysis has been associated with higher false-negative rates because of hemoglobin degradation.4 FIT sample exposure to high ambient temperatures also has been linked to decreased sensitivity for detecting CRC.5
US Postal Service (USPS) mail delivery delays have plagued many areas of the country. A variety of factors, including the COVID-19 pandemic, understaffing, changes in USPS policies, closure of post offices, and changes in mail delivery standards, may also be contributory causes. According to the USPS website, delivery standard for first-class mail is 1 to 5 days, but this is not guaranteed.6
The Jesse Brown Veterans Affairs Medical Center (JBVAMC) laboratory in Chicago has reported receiving FIT kit envelopes in batches by the USPS, with some prepaid first-class business reply envelopes delivered up to 60 days after the time of sample collection. Polymedco, a company that assists US Department of Veterans Affairs (VA) medical centers with logistics of FIT programs for CRC screening, reports that USPS batching of FIT kits leading to delayed delivery has been a periodic problem for medical centers around the country. Polymedco staff remind USPS staff about 4 points when they encounter this issue: Mailers are first-class mail; mailers contain a human biologic specimen that has limited viability; the biological sample used for detecting cancer is time sensitive; and delays in delivery by holding/batching kits could impact morbidity and mortality. Reviewing these key points with local USPS staff usually helps, however, batching and delayed delivery of the FIT kits can sometimes recur with USPS staffing turnover.
Tracking and identifying when a patient receives the FIT kit is difficult. Patients are instructed to write the date of collection on the kit, so the receiving laboratory knows whether the sample can be reliably analyzed. When patients are notified about delayed delivery of their sample, a staff member asks if they postponed dropping the kit in the mail. Most patients report mailing the sample within 1 to 2 days of collection. Tracking and dating each step of FIT kit events is not feasible with a mass mailing campaign. In our experience, most patients write the date of collection on the kit. If a collection date is not provided, the laboratory will call the patient to confirm a date. Cheng and colleagues reviewed the causes for FIT specimen rejection in a laboratory analyzing specimens for VA patients and found that 14% of submitted samples were rejected because the specimen was received > 14 days after collection, and 6% because the patient did not record the collection date. With a series of interventions aimed at reminding patients and improving laboratory procedures, rates of rejection for these 2 causes were reduced to < 4%.7 USPS delays were not identified as a factor or tracked in this study.
It is unclear why the USPS sometimes holds FIT kits at their facilities and then delivers large bins of them at the same time. Because FIT kits should be analyzed within 14 to 15 days of sample collection to assure reliable results, mail delivery delays can result in increased sample rejection. Based on the JBVAMC experience, up to 30% of submitted samples might need to be discarded when batched delivery takes place. In these cases, patients need to be contacted, informed of the problem, and asked to submit new kits. Understandably, patients are reluctant to repeat this type of testing, and we are concerned this could lead to reduced rates of CRC screening in affected communities.
As an alternative to discarding delayed samples, laboratories could report the results of delayed FIT kits with an added comment that “negative test results may be less reliable due to delayed processing,” but this approach would raise quality and medicolegal concerns. Clinicians have reached out to local USPS supervisory personnel with mixed results. Sometimes batching and delayed deliveries stop for a few months, only to resume without warning. Dropping off the sample directly at the laboratory is not a realistic option for most patients. Some patients can be convinced to submit another sample, some elect to switch to other CRC screening strategies, while others, unfortunately, decline further screening efforts.
Laboratory staff can be overwhelmed with having to process hundreds of samples in a short time frame, especially because there is no way of knowing when USPS will make a batched delivery. Laboratory capacities can limit staff at some facilities to performing analysis of only 10 tests at a time. The FIT kits should be delivered on a rolling basis and without delay so that the samples can be reliably analyzed with a predictable workload for the laboratory personnel and without unexpected surges.
When health care facilities identify delayed mail delivery of FIT kits via USPS, laboratories should first ensure that the correct postage rates are used on the prepaid envelopes and that their USPS accounts are properly funded, so that insufficient funds are not contributing to delayed deliveries. Stakeholders should then reach out to local USPS supervisory staff and request that the practice of batching the delivery of FIT kits be stopped. Educating USPS supervisory staff about concerns related to decreased test reliability associated with delayed mail delivery can be a persuasive argument. Adding additional language to the preprinted envelopes, such as “time sensitive,” may also be helpful. Unfortunately, the JBVAMC experience has been that the problem initially gets better after contacting the USPS, only to unexpectedly resurface months later. This cycle has been repeated several times in the past 2 years at JBVAMC.
All clinicians involved in CRC screening and treatment at institutions that use FIT kits need to be aware of the impact that local USPS delays can have on the reliability of these results. Health care systems should be prepared to implement mitigation strategies if they encounter significant delays with mail delivery. If delays cannot be reliably resolved by working with the local USPS staff, consider involving national USPS oversight bodies. And if the problems persist despite an attempt to work with the USPS, some institutions might find it feasible to offer drop boxes at their clinics and instruct patients to drop off FIT kits immediately following collection, in lieu of mailing them. Switching to private carriers is not a cost-effective alternative for most health care systems, and some may exclude rural areas. Depending on the local availability and capacity of endoscopists, some clinicians might prioritize referring patients for screening colonoscopies or screening flexible sigmoidoscopies, and might deemphasize FIT kits as a preferred option for CRC screening. CT colonography is an alternative screening method that is not as widely offered, nor as widely accepted at this time.
Conclusions
CRC screening is an essential part of preventive medicine, and the percentage of eligible patients screened is a well-established quality metric in primary care settings. Health care systems, clinicians, and laboratories must be vigilant to ensure that USPS delays in delivering FIT kits do not negatively impact their CRC screening programs. Facilities should actively monitor for delays in the return of FIT kits.
Despite the widespread use of mail-order pharmacies and the use of mail to communicate notifications about test results and follow-up appointments, unreliable or delayed mail delivery traditionally has not been considered a social determinant of health.8 This article highlights the impact delayed mail delivery can have on health outcomes. Disadvantaged communities in inner cities and rural areas have been disproportionately affected by the worsening performance of the USPS over the past few years.9 This represents an underappreciated public health concern in need of a sustainable solution.
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the United States.1 In 2022, there were an estimated 151,030 new CRC cases and 52,580 deaths.1 Options for CRC screening of patients at average risk include stool tests (annual fecal immunochemical test [FIT], annual guaiac-based fecal occult blood test, or stool FIT-DNA test every 1 to 3 years), colonoscopies every 10 years, flexible sigmoidoscopies every 5 years (or every 10 years with annual FIT), and computed tomography (CT) colonography every 5 years.2 Many health care systems use annual FIT for patients at average risk. Compared with guaiac-based fecal occult blood testing, FIT does not require dietary or medication modifications and yields greater sensitivity and patient participation.3
The COVID-19 pandemic and staffing issues have caused a scheduling backlog for screening, diagnostic, and surveillance endoscopies at some medical centers. As a result, FIT has become the primary means of CRC screening at these institutions. FIT kits for home use are typically distributed to eligible patients at an office visit or by mail, and patients are then instructed to mail the kits back to the laboratory. For the test to be as sensitive as possible, FIT kit manufacturers advise laboratory analysis within 14 to 15 days of collection, if stored at ambient temperature, and to reject the sample if it does not meet testing criteria for stability. Delayed FIT sample analysis has been associated with higher false-negative rates because of hemoglobin degradation.4 FIT sample exposure to high ambient temperatures also has been linked to decreased sensitivity for detecting CRC.5
US Postal Service (USPS) mail delivery delays have plagued many areas of the country. A variety of factors, including the COVID-19 pandemic, understaffing, changes in USPS policies, closure of post offices, and changes in mail delivery standards, may also be contributory causes. According to the USPS website, delivery standard for first-class mail is 1 to 5 days, but this is not guaranteed.6
The Jesse Brown Veterans Affairs Medical Center (JBVAMC) laboratory in Chicago has reported receiving FIT kit envelopes in batches by the USPS, with some prepaid first-class business reply envelopes delivered up to 60 days after the time of sample collection. Polymedco, a company that assists US Department of Veterans Affairs (VA) medical centers with logistics of FIT programs for CRC screening, reports that USPS batching of FIT kits leading to delayed delivery has been a periodic problem for medical centers around the country. Polymedco staff remind USPS staff about 4 points when they encounter this issue: Mailers are first-class mail; mailers contain a human biologic specimen that has limited viability; the biological sample used for detecting cancer is time sensitive; and delays in delivery by holding/batching kits could impact morbidity and mortality. Reviewing these key points with local USPS staff usually helps, however, batching and delayed delivery of the FIT kits can sometimes recur with USPS staffing turnover.
Tracking and identifying when a patient receives the FIT kit is difficult. Patients are instructed to write the date of collection on the kit, so the receiving laboratory knows whether the sample can be reliably analyzed. When patients are notified about delayed delivery of their sample, a staff member asks if they postponed dropping the kit in the mail. Most patients report mailing the sample within 1 to 2 days of collection. Tracking and dating each step of FIT kit events is not feasible with a mass mailing campaign. In our experience, most patients write the date of collection on the kit. If a collection date is not provided, the laboratory will call the patient to confirm a date. Cheng and colleagues reviewed the causes for FIT specimen rejection in a laboratory analyzing specimens for VA patients and found that 14% of submitted samples were rejected because the specimen was received > 14 days after collection, and 6% because the patient did not record the collection date. With a series of interventions aimed at reminding patients and improving laboratory procedures, rates of rejection for these 2 causes were reduced to < 4%.7 USPS delays were not identified as a factor or tracked in this study.
It is unclear why the USPS sometimes holds FIT kits at their facilities and then delivers large bins of them at the same time. Because FIT kits should be analyzed within 14 to 15 days of sample collection to assure reliable results, mail delivery delays can result in increased sample rejection. Based on the JBVAMC experience, up to 30% of submitted samples might need to be discarded when batched delivery takes place. In these cases, patients need to be contacted, informed of the problem, and asked to submit new kits. Understandably, patients are reluctant to repeat this type of testing, and we are concerned this could lead to reduced rates of CRC screening in affected communities.
As an alternative to discarding delayed samples, laboratories could report the results of delayed FIT kits with an added comment that “negative test results may be less reliable due to delayed processing,” but this approach would raise quality and medicolegal concerns. Clinicians have reached out to local USPS supervisory personnel with mixed results. Sometimes batching and delayed deliveries stop for a few months, only to resume without warning. Dropping off the sample directly at the laboratory is not a realistic option for most patients. Some patients can be convinced to submit another sample, some elect to switch to other CRC screening strategies, while others, unfortunately, decline further screening efforts.
Laboratory staff can be overwhelmed with having to process hundreds of samples in a short time frame, especially because there is no way of knowing when USPS will make a batched delivery. Laboratory capacities can limit staff at some facilities to performing analysis of only 10 tests at a time. The FIT kits should be delivered on a rolling basis and without delay so that the samples can be reliably analyzed with a predictable workload for the laboratory personnel and without unexpected surges.
When health care facilities identify delayed mail delivery of FIT kits via USPS, laboratories should first ensure that the correct postage rates are used on the prepaid envelopes and that their USPS accounts are properly funded, so that insufficient funds are not contributing to delayed deliveries. Stakeholders should then reach out to local USPS supervisory staff and request that the practice of batching the delivery of FIT kits be stopped. Educating USPS supervisory staff about concerns related to decreased test reliability associated with delayed mail delivery can be a persuasive argument. Adding additional language to the preprinted envelopes, such as “time sensitive,” may also be helpful. Unfortunately, the JBVAMC experience has been that the problem initially gets better after contacting the USPS, only to unexpectedly resurface months later. This cycle has been repeated several times in the past 2 years at JBVAMC.
All clinicians involved in CRC screening and treatment at institutions that use FIT kits need to be aware of the impact that local USPS delays can have on the reliability of these results. Health care systems should be prepared to implement mitigation strategies if they encounter significant delays with mail delivery. If delays cannot be reliably resolved by working with the local USPS staff, consider involving national USPS oversight bodies. And if the problems persist despite an attempt to work with the USPS, some institutions might find it feasible to offer drop boxes at their clinics and instruct patients to drop off FIT kits immediately following collection, in lieu of mailing them. Switching to private carriers is not a cost-effective alternative for most health care systems, and some may exclude rural areas. Depending on the local availability and capacity of endoscopists, some clinicians might prioritize referring patients for screening colonoscopies or screening flexible sigmoidoscopies, and might deemphasize FIT kits as a preferred option for CRC screening. CT colonography is an alternative screening method that is not as widely offered, nor as widely accepted at this time.
Conclusions
CRC screening is an essential part of preventive medicine, and the percentage of eligible patients screened is a well-established quality metric in primary care settings. Health care systems, clinicians, and laboratories must be vigilant to ensure that USPS delays in delivering FIT kits do not negatively impact their CRC screening programs. Facilities should actively monitor for delays in the return of FIT kits.
Despite the widespread use of mail-order pharmacies and the use of mail to communicate notifications about test results and follow-up appointments, unreliable or delayed mail delivery traditionally has not been considered a social determinant of health.8 This article highlights the impact delayed mail delivery can have on health outcomes. Disadvantaged communities in inner cities and rural areas have been disproportionately affected by the worsening performance of the USPS over the past few years.9 This represents an underappreciated public health concern in need of a sustainable solution.
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
2. Centers for Disease Control and Prevention. Colorectal cancer screening tests. Updated February 23, 2023. Accessed March 14, 2024. https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
3. van Rossum LG, van Rijn AF, Laheij RJ, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135(1):82-90. doi:10.1053/j.gastro.2008.03.040
4. van Rossum LG, van Rijn AF, van Oijen MG, et al. False negative fecal occult blood tests due to delayed sample return in colorectal cancer screening. Int J Cancer. 2009;125(4):746-750. doi:10.1002/ijc.24458
5. Doubeni CA, Jensen CD, Fedewa SA, et al. Fecal immunochemical test (FIT) for colon cancer screening: variable performance with ambient temperature. J Am Board Fam Med. 2016;29(6):672-681. doi:10.3122/jabfm.2016.06.160060
6. United States Postal Service. Shipping and mailing with USPS. Accessed March 14, 2024. https://www.usps.com/ship
7. Cheng C, Ganz DA, Chang ET, Huynh A, De Peralta S. Reducing rejected fecal immunochemical tests received in the laboratory for colorectal cancer screening. J Healthc Qual. 2019;41(2):75-82.doi:10.1097/JHQ.0000000000000181
8. Hussaini SMQ, Alexander GC. The United States Postal Service: an essential public health agency? J Gen Intern Med. 2020;35(12):3699-3701. doi:10.1007/s11606-020-06275-2
9. Hampton DJ. Colorado mountain towns are plagued by post office delays as residents wait weeks for medication and retirement checks. NBC News. February 25, 2023. Accessed March 14, 2024. https://www.nbcnews.com/news/us-news/colo-mountain-towns-are-plagued-post-office-delays-residents-wait-week-rcna72085
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi:10.3322/caac.21708
2. Centers for Disease Control and Prevention. Colorectal cancer screening tests. Updated February 23, 2023. Accessed March 14, 2024. https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
3. van Rossum LG, van Rijn AF, Laheij RJ, et al. Random comparison of guaiac and immunochemical fecal occult blood tests for colorectal cancer in a screening population. Gastroenterology. 2008;135(1):82-90. doi:10.1053/j.gastro.2008.03.040
4. van Rossum LG, van Rijn AF, van Oijen MG, et al. False negative fecal occult blood tests due to delayed sample return in colorectal cancer screening. Int J Cancer. 2009;125(4):746-750. doi:10.1002/ijc.24458
5. Doubeni CA, Jensen CD, Fedewa SA, et al. Fecal immunochemical test (FIT) for colon cancer screening: variable performance with ambient temperature. J Am Board Fam Med. 2016;29(6):672-681. doi:10.3122/jabfm.2016.06.160060
6. United States Postal Service. Shipping and mailing with USPS. Accessed March 14, 2024. https://www.usps.com/ship
7. Cheng C, Ganz DA, Chang ET, Huynh A, De Peralta S. Reducing rejected fecal immunochemical tests received in the laboratory for colorectal cancer screening. J Healthc Qual. 2019;41(2):75-82.doi:10.1097/JHQ.0000000000000181
8. Hussaini SMQ, Alexander GC. The United States Postal Service: an essential public health agency? J Gen Intern Med. 2020;35(12):3699-3701. doi:10.1007/s11606-020-06275-2
9. Hampton DJ. Colorado mountain towns are plagued by post office delays as residents wait weeks for medication and retirement checks. NBC News. February 25, 2023. Accessed March 14, 2024. https://www.nbcnews.com/news/us-news/colo-mountain-towns-are-plagued-post-office-delays-residents-wait-week-rcna72085
Moral Injury in Health Care: A Unified Definition and its Relationship to Burnout
Moral injury was identified by health care professionals (HCPs) as a driver of occupational distress prior to the COVID-19 pandemic, but the crisis expanded the appeal and investigation of the term.1 HCPs now consider moral injury an essential component of the framework to describe their distress, because using the term burnout alone fails to capture their full experience and has proven resistant to interventions.2 Moral injury goes beyond the transdiagnostic symptoms of exhaustion and cynicism and beyond operational, demand-resource mismatches that characterize burnout. It describes the frustration, anger, and helplessness associated with relational ruptures and the existential threats to a clinician’s professional identity as business interests erode their ability to put their patients’ needs ahead of corporate and health care system obligations.3
Proper characterization of moral injury in health care—separate from the military environments where it originated—is stymied by an ill-defined relationship between 2 definitions of the term and by an unclear relationship between moral injury and the long-standing body of scholarship in burnout. To clarify the concept, inform research agendas, and open avenues for more effective solutions to the crisis of HCP distress, we propose a unified conceptualization of moral injury and its association with burnout in health care.
CONTEXTUAL DISTINCTIONS
It is important to properly distinguish between the original use of moral injury in the military and its expanded use in civilian circumstances. Health care and the military are both professions whereupon donning the “uniform” of a physician—or soldier, sailor, airman, or marine—members must comport with strict expectations of behavior, including the refusal to engage in illegal actions or those contrary to professional ethics. Individuals in both professions acquire a highly specialized body of knowledge and enter an implied contract to provide critical services to society, specifically healing and protection, respectively. Members of both professions are trained to make complex judgments with integrity under conditions of technical and ethical uncertainty, upon which they take highly skilled action. Medical and military professionals must be free to act on their ethical principles, without confounding demands.4 However, the context of each profession’s commitment to society carries different moral implications.
The risk of moral injury is inherent in military service. The military promises protection with an implicit acknowledgment of the need to use lethal force to uphold the agreement. In contrast, HCPs promise healing and care. The military promises to protect our society, with an implicit acknowledgment of the need to use lethal force to uphold the agreement. Some military actions may inflict harm without the hope of benefitting an individual, and are therefore potentially morally injurious. The health care contract with society, promising healing and care, is devoid of inherent moral injury due to harm without potential individual benefit. Therefore, the presence of moral injury in health care settings are warning signs of a dysfunctional environment.
One complex example of the dysfunctional environments is illustrative. The military and health care are among the few industries where supply creates demand. For example, the more bad state actors there are, the more demand for the military. As we have seen since the 1950s, the more technology and therapeutics we create in health care, coupled with a larger share paid for by third parties, the greater the demand for and use of them.5 In a fee for service environment, corporate greed feeds on this reality. In most other environments, more technological and therapeutic options inevitably pit clinicians against multiple other factions: payers, who do not want to underwrite them; patients, who sometimes demand them without justification or later rail against spiraling health care costs; and administrators, especially in capitated systems, who watch their bottom lines erode. The moral injury risk in this instance demands a collective conversation among stakeholders regarding the structural determinants of health—how we choose to distribute limited resources. The intermediary of moral injury is a useful measure of the harm that results from ignoring or avoiding such challenges.
HARMONIZING DEFINITIONS
Moral injury is inherently nuanced. The 2 dominant definitions arise from work with combat veterans and create additional and perhaps unnecessary complexity. Unifying these 2 definitions eliminates inadvertent confusion, preventing the risk of unbridled interdisciplinary investigation which leads to a lack of precision in the meaning of moral injury and other related concepts, such as burnout.6
The first definition was developed by Jonathan Shay in 1994 and outlines 3 necessarycomponents, viewing the violator as a powerholder: (1) betrayal of what is right, (2) by someone who holds legitimate authority, (3) in a high stakes situation.7 Litz and colleagues describe moral injury another way: “Perpetrating, failing to prevent, bearing witness to, or learning about acts that transgress deeply held moral beliefs and expectations.”8 The violator is posited to be either the self or others.
Rather than representing “self” or “other” imposed moral injury, we propose the 2 definitions are related as exposure (ie, the perceived betrayal) and response (ie, the resulting transgression). An individual who experiences a betrayal by a legitimate authority has an opportunity to choose their response. They may acquiesce and transgress their moral beliefs (eg, their oath to provide ethical health care), or they could refuse, by speaking out, or in some way resisting the authority’s betrayal. The case of Ray Brovont is a useful illustration of reconciling the definitions (Box).9
Myriad factors—known as potentially morally injurious events—drive moral injury, such as resource-constrained decision making, witnessing the behaviors of colleagues that violate deeply held moral beliefs, questionable billing practices, and more. Each begins with a betrayal. Spotlighting the betrayal, refusing to perpetuate it, or taking actions toward change, may reduce the risk of experiencing moral injury.9 Conversely, acquiescing and transgressing one’s oath, the profession’s covenant with society, increases the risk of experiencing moral injury.8
Many HCPs believe they are not always free to resist betrayal, fearing retaliation, job loss, blacklisting, or worse. They feel constrained by debt accrued while receiving their education, being their household’s primary earner, community ties, practicing a niche specialty that requires working for a tertiary referral center, or perhaps believing the situation will be the same elsewhere. To not stand up or speak out is to choose complicity with corporate greed that uses HCPs to undermine their professional duties, which significantly increases the risk of experiencing moral injury.
MORAL INJURY AND BURNOUT
In addition to reconciling the definitions of moral injury, the relationship between moral injury and burnout are still being elucidated. We suggest that moral injury and burnout represent independent and potentially interrelated pathways to distress (Figure). Exposure to chronic, inconsonant, and transactional demands, which things like shorter work hours, better self-care, or improved health system operations might mitigate, manifests as burnout. In contrast, moral injury arises when a superior’s actions or a system’s policies and practices—such as justifiable but unnecessary testing, or referral restrictions to prevent revenue leakage—undermine one’s professional obligations to prioritize the patient’s best interest.
If concerns from HCPs about transactional demands are persistently dismissed, such inaction may be perceived as a betrayal, raising the risk of moral injury. Additionally, the resignation or helplessness of moral injury perceived as inescapable may present with emotional exhaustion, ineffectiveness, and depersonalization, all hallmarks of burnout. Both conditions can mediate and moderate the relationship between triggers for workplace distress and resulting psychological, physical, and existential harm.
CONCLUSIONS
Moral injury is increasingly recognized as a source of distress among HCPs, resulting from structural constraints on their ability to deliver optimal care and their own unwillingness to stand up for their patients, their oaths, and their professions.1 Unlike the military, where moral injury is inherent in the contract with society, moral injury in health care (and the relational rupture it connotes) is a signal of systemic dysfunction, fractured trust, and the need for relational repair.
Health care is at a crossroads, experiencing a workforce retention crisis while simultaneously predicting a significant increase in care needs by Baby Boomers over the next 3 decades.
Health care does not have the luxury of experimenting another 30 years with interventions that have limited impact. We must design a new generation of approaches, shaped by lessons learned from the pandemic while acknowledging that prepandemic standards were already failing the workforce. A unified definition of moral injury must be integrated to frame clinician distress alongside burnout, recentering ethical decision making, rather than profit, at the heart of health care. Harmonizing the definitions of moral injury and clarifying the relationship of moral injury with burnout reduces the need for further reinterpretations, allowing for more robust, easily comparable studies focused on identifying risk factors, as well as rapidly implementing effective mitigation strategies.
1. Griffin BJ, Weber MC, Hinkson KD, et al. Toward a dimensional contextual model of moral injury: a scoping review on healthcare workers. Curr Treat Options Psych. 2023;10:199-216. doi:10.1007/s40501-023-00296-4
2. National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. The National Academies Press; 2019. doi:10.17226/25521
3. Dean W, Talbot S, Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
4. Gardner HE, Schulman LS. The professions in America today: crucial but fragile. Daedalus. 2005;134(3):13-18. doi:10.1162/0011526054622132
5. Fuchs VR. Major trends in the U.S. health economy since 1950. N Engl J Med. 2012;366(11):973-977. doi:10.1056/NEJMp1200478
6. Molendijk T. Warnings against romanticising moral injury. Br J Psychiatry. 2022;220(1):1-3. doi:10.1192/bjp.2021.114
7. Shay J. Moral injury. Psychoanalytic Psychol. 2014;31(2):182-191. doi:10.1037/a0036090
8. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003
9. Brovont v KS-I Med. Servs., P.A., 622 SW3d 671 (Mo Ct App 2020).
Moral injury was identified by health care professionals (HCPs) as a driver of occupational distress prior to the COVID-19 pandemic, but the crisis expanded the appeal and investigation of the term.1 HCPs now consider moral injury an essential component of the framework to describe their distress, because using the term burnout alone fails to capture their full experience and has proven resistant to interventions.2 Moral injury goes beyond the transdiagnostic symptoms of exhaustion and cynicism and beyond operational, demand-resource mismatches that characterize burnout. It describes the frustration, anger, and helplessness associated with relational ruptures and the existential threats to a clinician’s professional identity as business interests erode their ability to put their patients’ needs ahead of corporate and health care system obligations.3
Proper characterization of moral injury in health care—separate from the military environments where it originated—is stymied by an ill-defined relationship between 2 definitions of the term and by an unclear relationship between moral injury and the long-standing body of scholarship in burnout. To clarify the concept, inform research agendas, and open avenues for more effective solutions to the crisis of HCP distress, we propose a unified conceptualization of moral injury and its association with burnout in health care.
CONTEXTUAL DISTINCTIONS
It is important to properly distinguish between the original use of moral injury in the military and its expanded use in civilian circumstances. Health care and the military are both professions whereupon donning the “uniform” of a physician—or soldier, sailor, airman, or marine—members must comport with strict expectations of behavior, including the refusal to engage in illegal actions or those contrary to professional ethics. Individuals in both professions acquire a highly specialized body of knowledge and enter an implied contract to provide critical services to society, specifically healing and protection, respectively. Members of both professions are trained to make complex judgments with integrity under conditions of technical and ethical uncertainty, upon which they take highly skilled action. Medical and military professionals must be free to act on their ethical principles, without confounding demands.4 However, the context of each profession’s commitment to society carries different moral implications.
The risk of moral injury is inherent in military service. The military promises protection with an implicit acknowledgment of the need to use lethal force to uphold the agreement. In contrast, HCPs promise healing and care. The military promises to protect our society, with an implicit acknowledgment of the need to use lethal force to uphold the agreement. Some military actions may inflict harm without the hope of benefitting an individual, and are therefore potentially morally injurious. The health care contract with society, promising healing and care, is devoid of inherent moral injury due to harm without potential individual benefit. Therefore, the presence of moral injury in health care settings are warning signs of a dysfunctional environment.
One complex example of the dysfunctional environments is illustrative. The military and health care are among the few industries where supply creates demand. For example, the more bad state actors there are, the more demand for the military. As we have seen since the 1950s, the more technology and therapeutics we create in health care, coupled with a larger share paid for by third parties, the greater the demand for and use of them.5 In a fee for service environment, corporate greed feeds on this reality. In most other environments, more technological and therapeutic options inevitably pit clinicians against multiple other factions: payers, who do not want to underwrite them; patients, who sometimes demand them without justification or later rail against spiraling health care costs; and administrators, especially in capitated systems, who watch their bottom lines erode. The moral injury risk in this instance demands a collective conversation among stakeholders regarding the structural determinants of health—how we choose to distribute limited resources. The intermediary of moral injury is a useful measure of the harm that results from ignoring or avoiding such challenges.
HARMONIZING DEFINITIONS
Moral injury is inherently nuanced. The 2 dominant definitions arise from work with combat veterans and create additional and perhaps unnecessary complexity. Unifying these 2 definitions eliminates inadvertent confusion, preventing the risk of unbridled interdisciplinary investigation which leads to a lack of precision in the meaning of moral injury and other related concepts, such as burnout.6
The first definition was developed by Jonathan Shay in 1994 and outlines 3 necessarycomponents, viewing the violator as a powerholder: (1) betrayal of what is right, (2) by someone who holds legitimate authority, (3) in a high stakes situation.7 Litz and colleagues describe moral injury another way: “Perpetrating, failing to prevent, bearing witness to, or learning about acts that transgress deeply held moral beliefs and expectations.”8 The violator is posited to be either the self or others.
Rather than representing “self” or “other” imposed moral injury, we propose the 2 definitions are related as exposure (ie, the perceived betrayal) and response (ie, the resulting transgression). An individual who experiences a betrayal by a legitimate authority has an opportunity to choose their response. They may acquiesce and transgress their moral beliefs (eg, their oath to provide ethical health care), or they could refuse, by speaking out, or in some way resisting the authority’s betrayal. The case of Ray Brovont is a useful illustration of reconciling the definitions (Box).9
Myriad factors—known as potentially morally injurious events—drive moral injury, such as resource-constrained decision making, witnessing the behaviors of colleagues that violate deeply held moral beliefs, questionable billing practices, and more. Each begins with a betrayal. Spotlighting the betrayal, refusing to perpetuate it, or taking actions toward change, may reduce the risk of experiencing moral injury.9 Conversely, acquiescing and transgressing one’s oath, the profession’s covenant with society, increases the risk of experiencing moral injury.8
Many HCPs believe they are not always free to resist betrayal, fearing retaliation, job loss, blacklisting, or worse. They feel constrained by debt accrued while receiving their education, being their household’s primary earner, community ties, practicing a niche specialty that requires working for a tertiary referral center, or perhaps believing the situation will be the same elsewhere. To not stand up or speak out is to choose complicity with corporate greed that uses HCPs to undermine their professional duties, which significantly increases the risk of experiencing moral injury.
MORAL INJURY AND BURNOUT
In addition to reconciling the definitions of moral injury, the relationship between moral injury and burnout are still being elucidated. We suggest that moral injury and burnout represent independent and potentially interrelated pathways to distress (Figure). Exposure to chronic, inconsonant, and transactional demands, which things like shorter work hours, better self-care, or improved health system operations might mitigate, manifests as burnout. In contrast, moral injury arises when a superior’s actions or a system’s policies and practices—such as justifiable but unnecessary testing, or referral restrictions to prevent revenue leakage—undermine one’s professional obligations to prioritize the patient’s best interest.
If concerns from HCPs about transactional demands are persistently dismissed, such inaction may be perceived as a betrayal, raising the risk of moral injury. Additionally, the resignation or helplessness of moral injury perceived as inescapable may present with emotional exhaustion, ineffectiveness, and depersonalization, all hallmarks of burnout. Both conditions can mediate and moderate the relationship between triggers for workplace distress and resulting psychological, physical, and existential harm.
CONCLUSIONS
Moral injury is increasingly recognized as a source of distress among HCPs, resulting from structural constraints on their ability to deliver optimal care and their own unwillingness to stand up for their patients, their oaths, and their professions.1 Unlike the military, where moral injury is inherent in the contract with society, moral injury in health care (and the relational rupture it connotes) is a signal of systemic dysfunction, fractured trust, and the need for relational repair.
Health care is at a crossroads, experiencing a workforce retention crisis while simultaneously predicting a significant increase in care needs by Baby Boomers over the next 3 decades.
Health care does not have the luxury of experimenting another 30 years with interventions that have limited impact. We must design a new generation of approaches, shaped by lessons learned from the pandemic while acknowledging that prepandemic standards were already failing the workforce. A unified definition of moral injury must be integrated to frame clinician distress alongside burnout, recentering ethical decision making, rather than profit, at the heart of health care. Harmonizing the definitions of moral injury and clarifying the relationship of moral injury with burnout reduces the need for further reinterpretations, allowing for more robust, easily comparable studies focused on identifying risk factors, as well as rapidly implementing effective mitigation strategies.
Moral injury was identified by health care professionals (HCPs) as a driver of occupational distress prior to the COVID-19 pandemic, but the crisis expanded the appeal and investigation of the term.1 HCPs now consider moral injury an essential component of the framework to describe their distress, because using the term burnout alone fails to capture their full experience and has proven resistant to interventions.2 Moral injury goes beyond the transdiagnostic symptoms of exhaustion and cynicism and beyond operational, demand-resource mismatches that characterize burnout. It describes the frustration, anger, and helplessness associated with relational ruptures and the existential threats to a clinician’s professional identity as business interests erode their ability to put their patients’ needs ahead of corporate and health care system obligations.3
Proper characterization of moral injury in health care—separate from the military environments where it originated—is stymied by an ill-defined relationship between 2 definitions of the term and by an unclear relationship between moral injury and the long-standing body of scholarship in burnout. To clarify the concept, inform research agendas, and open avenues for more effective solutions to the crisis of HCP distress, we propose a unified conceptualization of moral injury and its association with burnout in health care.
CONTEXTUAL DISTINCTIONS
It is important to properly distinguish between the original use of moral injury in the military and its expanded use in civilian circumstances. Health care and the military are both professions whereupon donning the “uniform” of a physician—or soldier, sailor, airman, or marine—members must comport with strict expectations of behavior, including the refusal to engage in illegal actions or those contrary to professional ethics. Individuals in both professions acquire a highly specialized body of knowledge and enter an implied contract to provide critical services to society, specifically healing and protection, respectively. Members of both professions are trained to make complex judgments with integrity under conditions of technical and ethical uncertainty, upon which they take highly skilled action. Medical and military professionals must be free to act on their ethical principles, without confounding demands.4 However, the context of each profession’s commitment to society carries different moral implications.
The risk of moral injury is inherent in military service. The military promises protection with an implicit acknowledgment of the need to use lethal force to uphold the agreement. In contrast, HCPs promise healing and care. The military promises to protect our society, with an implicit acknowledgment of the need to use lethal force to uphold the agreement. Some military actions may inflict harm without the hope of benefitting an individual, and are therefore potentially morally injurious. The health care contract with society, promising healing and care, is devoid of inherent moral injury due to harm without potential individual benefit. Therefore, the presence of moral injury in health care settings are warning signs of a dysfunctional environment.
One complex example of the dysfunctional environments is illustrative. The military and health care are among the few industries where supply creates demand. For example, the more bad state actors there are, the more demand for the military. As we have seen since the 1950s, the more technology and therapeutics we create in health care, coupled with a larger share paid for by third parties, the greater the demand for and use of them.5 In a fee for service environment, corporate greed feeds on this reality. In most other environments, more technological and therapeutic options inevitably pit clinicians against multiple other factions: payers, who do not want to underwrite them; patients, who sometimes demand them without justification or later rail against spiraling health care costs; and administrators, especially in capitated systems, who watch their bottom lines erode. The moral injury risk in this instance demands a collective conversation among stakeholders regarding the structural determinants of health—how we choose to distribute limited resources. The intermediary of moral injury is a useful measure of the harm that results from ignoring or avoiding such challenges.
HARMONIZING DEFINITIONS
Moral injury is inherently nuanced. The 2 dominant definitions arise from work with combat veterans and create additional and perhaps unnecessary complexity. Unifying these 2 definitions eliminates inadvertent confusion, preventing the risk of unbridled interdisciplinary investigation which leads to a lack of precision in the meaning of moral injury and other related concepts, such as burnout.6
The first definition was developed by Jonathan Shay in 1994 and outlines 3 necessarycomponents, viewing the violator as a powerholder: (1) betrayal of what is right, (2) by someone who holds legitimate authority, (3) in a high stakes situation.7 Litz and colleagues describe moral injury another way: “Perpetrating, failing to prevent, bearing witness to, or learning about acts that transgress deeply held moral beliefs and expectations.”8 The violator is posited to be either the self or others.
Rather than representing “self” or “other” imposed moral injury, we propose the 2 definitions are related as exposure (ie, the perceived betrayal) and response (ie, the resulting transgression). An individual who experiences a betrayal by a legitimate authority has an opportunity to choose their response. They may acquiesce and transgress their moral beliefs (eg, their oath to provide ethical health care), or they could refuse, by speaking out, or in some way resisting the authority’s betrayal. The case of Ray Brovont is a useful illustration of reconciling the definitions (Box).9
Myriad factors—known as potentially morally injurious events—drive moral injury, such as resource-constrained decision making, witnessing the behaviors of colleagues that violate deeply held moral beliefs, questionable billing practices, and more. Each begins with a betrayal. Spotlighting the betrayal, refusing to perpetuate it, or taking actions toward change, may reduce the risk of experiencing moral injury.9 Conversely, acquiescing and transgressing one’s oath, the profession’s covenant with society, increases the risk of experiencing moral injury.8
Many HCPs believe they are not always free to resist betrayal, fearing retaliation, job loss, blacklisting, or worse. They feel constrained by debt accrued while receiving their education, being their household’s primary earner, community ties, practicing a niche specialty that requires working for a tertiary referral center, or perhaps believing the situation will be the same elsewhere. To not stand up or speak out is to choose complicity with corporate greed that uses HCPs to undermine their professional duties, which significantly increases the risk of experiencing moral injury.
MORAL INJURY AND BURNOUT
In addition to reconciling the definitions of moral injury, the relationship between moral injury and burnout are still being elucidated. We suggest that moral injury and burnout represent independent and potentially interrelated pathways to distress (Figure). Exposure to chronic, inconsonant, and transactional demands, which things like shorter work hours, better self-care, or improved health system operations might mitigate, manifests as burnout. In contrast, moral injury arises when a superior’s actions or a system’s policies and practices—such as justifiable but unnecessary testing, or referral restrictions to prevent revenue leakage—undermine one’s professional obligations to prioritize the patient’s best interest.
If concerns from HCPs about transactional demands are persistently dismissed, such inaction may be perceived as a betrayal, raising the risk of moral injury. Additionally, the resignation or helplessness of moral injury perceived as inescapable may present with emotional exhaustion, ineffectiveness, and depersonalization, all hallmarks of burnout. Both conditions can mediate and moderate the relationship between triggers for workplace distress and resulting psychological, physical, and existential harm.
CONCLUSIONS
Moral injury is increasingly recognized as a source of distress among HCPs, resulting from structural constraints on their ability to deliver optimal care and their own unwillingness to stand up for their patients, their oaths, and their professions.1 Unlike the military, where moral injury is inherent in the contract with society, moral injury in health care (and the relational rupture it connotes) is a signal of systemic dysfunction, fractured trust, and the need for relational repair.
Health care is at a crossroads, experiencing a workforce retention crisis while simultaneously predicting a significant increase in care needs by Baby Boomers over the next 3 decades.
Health care does not have the luxury of experimenting another 30 years with interventions that have limited impact. We must design a new generation of approaches, shaped by lessons learned from the pandemic while acknowledging that prepandemic standards were already failing the workforce. A unified definition of moral injury must be integrated to frame clinician distress alongside burnout, recentering ethical decision making, rather than profit, at the heart of health care. Harmonizing the definitions of moral injury and clarifying the relationship of moral injury with burnout reduces the need for further reinterpretations, allowing for more robust, easily comparable studies focused on identifying risk factors, as well as rapidly implementing effective mitigation strategies.
1. Griffin BJ, Weber MC, Hinkson KD, et al. Toward a dimensional contextual model of moral injury: a scoping review on healthcare workers. Curr Treat Options Psych. 2023;10:199-216. doi:10.1007/s40501-023-00296-4
2. National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. The National Academies Press; 2019. doi:10.17226/25521
3. Dean W, Talbot S, Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
4. Gardner HE, Schulman LS. The professions in America today: crucial but fragile. Daedalus. 2005;134(3):13-18. doi:10.1162/0011526054622132
5. Fuchs VR. Major trends in the U.S. health economy since 1950. N Engl J Med. 2012;366(11):973-977. doi:10.1056/NEJMp1200478
6. Molendijk T. Warnings against romanticising moral injury. Br J Psychiatry. 2022;220(1):1-3. doi:10.1192/bjp.2021.114
7. Shay J. Moral injury. Psychoanalytic Psychol. 2014;31(2):182-191. doi:10.1037/a0036090
8. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003
9. Brovont v KS-I Med. Servs., P.A., 622 SW3d 671 (Mo Ct App 2020).
1. Griffin BJ, Weber MC, Hinkson KD, et al. Toward a dimensional contextual model of moral injury: a scoping review on healthcare workers. Curr Treat Options Psych. 2023;10:199-216. doi:10.1007/s40501-023-00296-4
2. National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking Action Against Clinician Burnout: A Systems Approach to Professional Well-Being. The National Academies Press; 2019. doi:10.17226/25521
3. Dean W, Talbot S, Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36(9):400-402.
4. Gardner HE, Schulman LS. The professions in America today: crucial but fragile. Daedalus. 2005;134(3):13-18. doi:10.1162/0011526054622132
5. Fuchs VR. Major trends in the U.S. health economy since 1950. N Engl J Med. 2012;366(11):973-977. doi:10.1056/NEJMp1200478
6. Molendijk T. Warnings against romanticising moral injury. Br J Psychiatry. 2022;220(1):1-3. doi:10.1192/bjp.2021.114
7. Shay J. Moral injury. Psychoanalytic Psychol. 2014;31(2):182-191. doi:10.1037/a0036090
8. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003
9. Brovont v KS-I Med. Servs., P.A., 622 SW3d 671 (Mo Ct App 2020).