User login
Weight a Factor in Risky Sexual Behaviors of Adolescent Females
SAN DIEGO – The reasons why overweight and obese adolescent females are more likely to engage in risky sexual behaviors compared with their normal weight peers remain unclear, results from a large national study demonstrated.
Although previous studies have shown that overweight and obese adolescent females are more likely than their normal weight peers to have intercourse before age 13, have multiple sexual partners, and are less likely to use contraception, "they only imply association; they do not offer any insight into motivations and the underlying actions," Dr. Erin M. Swanson said at the annual meeting of the American College of Obstetricians and Gynecologists. "Our objective was to examine the association of weight with sexual practices, perceptions of sex, and motivations for contraception among adolescent females."
Dr. Swanson of the department of obstetrics and gynecology at Medical University of South Carolina, Charleston, and her associates performed a cross-sectional analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-95 school year. The interviews were 1-2 hours long and focused on survey questions regarding sexual perceptions and behaviors in adolescent females.
Dr. Swanson and her associates categorized study participants into three body mass index percentile categories: less than 85% of expected (normal weight), 85%-95% of expected (overweight), and greater than 95% of expected (obese). Self-esteem was divided into two categories: normal or low based on responses to the Rosenberg self-esteem scale, a validated instrument.
At baseline, the mean age of the females was 15 years, 71% were white, 16% were black, and 13% were Hispanic. In addition, 15% were overweight, 8% were obese, 18% met criteria for low self-esteem, and 37% reported having sexual intercourse. Of those who reported having intercourse, 76% reported being over age 13 at the time.
More than one in five overweight females (22%) and 23% of obese females had low self-esteem, compared with 17% of their normal weight peers, a difference that reached statistical significance (P = .03).
Logistic regression analysis revealed that, compared with their normal weight peers, overweight and obese females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
In addition, obese females were 1.9 times more likely to have been forced to have sex, compared with their normal weight peers.
"Both race and self-esteem were evaluated as possible cofounders and determined to have no effect on the logistic regression model for the reported behaviors," Dr. Swanson said. "Interestingly, the rate of reported gonorrhea and chlamydia did not differ between weight classes."
When asked about their motivations to engage in sex, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response option "your friends would respect you more" (P = .01), which suggests a peer influence, Dr. Swanson commented. "Interestingly, when these answers were compared with self-esteem, there was no difference [between weight groups]," she said.
When asked about their motivations to use birth control, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response options "birth control is too much of a hassle to use" and "it is hard to get a boy to use birth control with you" (P = .01 for both).
While the motivation for overweight and obese females to engage in risky sexual behaviors remains unclear, "our findings suggest that peer influence may be significant," Dr. Swanson said. "An adolescent’s decision to engage in sex is likely multi-factorial, influenced by more than self-esteem and body image."
She went on to note that overweight and obese adolescent females "should be considered a vulnerable population. Clinicians should identify these patients and spend time exploring their thoughts about themselves, their peers, and their decisions to engage in sexual behaviors. It is our job to give accurate information, screen for and treat sexually transmitted infections, provide contraception, encourage parental involvement and, if needed, give good prenatal care. We as obstetricians and gynecologists have a unique opportunity and responsibility to care for, educate, and give feedback to adolescent girls to improve their overall sexual health."
Dr. Swanson said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The reasons why overweight and obese adolescent females are more likely to engage in risky sexual behaviors compared with their normal weight peers remain unclear, results from a large national study demonstrated.
Although previous studies have shown that overweight and obese adolescent females are more likely than their normal weight peers to have intercourse before age 13, have multiple sexual partners, and are less likely to use contraception, "they only imply association; they do not offer any insight into motivations and the underlying actions," Dr. Erin M. Swanson said at the annual meeting of the American College of Obstetricians and Gynecologists. "Our objective was to examine the association of weight with sexual practices, perceptions of sex, and motivations for contraception among adolescent females."
Dr. Swanson of the department of obstetrics and gynecology at Medical University of South Carolina, Charleston, and her associates performed a cross-sectional analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-95 school year. The interviews were 1-2 hours long and focused on survey questions regarding sexual perceptions and behaviors in adolescent females.
Dr. Swanson and her associates categorized study participants into three body mass index percentile categories: less than 85% of expected (normal weight), 85%-95% of expected (overweight), and greater than 95% of expected (obese). Self-esteem was divided into two categories: normal or low based on responses to the Rosenberg self-esteem scale, a validated instrument.
At baseline, the mean age of the females was 15 years, 71% were white, 16% were black, and 13% were Hispanic. In addition, 15% were overweight, 8% were obese, 18% met criteria for low self-esteem, and 37% reported having sexual intercourse. Of those who reported having intercourse, 76% reported being over age 13 at the time.
More than one in five overweight females (22%) and 23% of obese females had low self-esteem, compared with 17% of their normal weight peers, a difference that reached statistical significance (P = .03).
Logistic regression analysis revealed that, compared with their normal weight peers, overweight and obese females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
In addition, obese females were 1.9 times more likely to have been forced to have sex, compared with their normal weight peers.
"Both race and self-esteem were evaluated as possible cofounders and determined to have no effect on the logistic regression model for the reported behaviors," Dr. Swanson said. "Interestingly, the rate of reported gonorrhea and chlamydia did not differ between weight classes."
When asked about their motivations to engage in sex, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response option "your friends would respect you more" (P = .01), which suggests a peer influence, Dr. Swanson commented. "Interestingly, when these answers were compared with self-esteem, there was no difference [between weight groups]," she said.
When asked about their motivations to use birth control, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response options "birth control is too much of a hassle to use" and "it is hard to get a boy to use birth control with you" (P = .01 for both).
While the motivation for overweight and obese females to engage in risky sexual behaviors remains unclear, "our findings suggest that peer influence may be significant," Dr. Swanson said. "An adolescent’s decision to engage in sex is likely multi-factorial, influenced by more than self-esteem and body image."
She went on to note that overweight and obese adolescent females "should be considered a vulnerable population. Clinicians should identify these patients and spend time exploring their thoughts about themselves, their peers, and their decisions to engage in sexual behaviors. It is our job to give accurate information, screen for and treat sexually transmitted infections, provide contraception, encourage parental involvement and, if needed, give good prenatal care. We as obstetricians and gynecologists have a unique opportunity and responsibility to care for, educate, and give feedback to adolescent girls to improve their overall sexual health."
Dr. Swanson said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The reasons why overweight and obese adolescent females are more likely to engage in risky sexual behaviors compared with their normal weight peers remain unclear, results from a large national study demonstrated.
Although previous studies have shown that overweight and obese adolescent females are more likely than their normal weight peers to have intercourse before age 13, have multiple sexual partners, and are less likely to use contraception, "they only imply association; they do not offer any insight into motivations and the underlying actions," Dr. Erin M. Swanson said at the annual meeting of the American College of Obstetricians and Gynecologists. "Our objective was to examine the association of weight with sexual practices, perceptions of sex, and motivations for contraception among adolescent females."
Dr. Swanson of the department of obstetrics and gynecology at Medical University of South Carolina, Charleston, and her associates performed a cross-sectional analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-95 school year. The interviews were 1-2 hours long and focused on survey questions regarding sexual perceptions and behaviors in adolescent females.
Dr. Swanson and her associates categorized study participants into three body mass index percentile categories: less than 85% of expected (normal weight), 85%-95% of expected (overweight), and greater than 95% of expected (obese). Self-esteem was divided into two categories: normal or low based on responses to the Rosenberg self-esteem scale, a validated instrument.
At baseline, the mean age of the females was 15 years, 71% were white, 16% were black, and 13% were Hispanic. In addition, 15% were overweight, 8% were obese, 18% met criteria for low self-esteem, and 37% reported having sexual intercourse. Of those who reported having intercourse, 76% reported being over age 13 at the time.
More than one in five overweight females (22%) and 23% of obese females had low self-esteem, compared with 17% of their normal weight peers, a difference that reached statistical significance (P = .03).
Logistic regression analysis revealed that, compared with their normal weight peers, overweight and obese females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
In addition, obese females were 1.9 times more likely to have been forced to have sex, compared with their normal weight peers.
"Both race and self-esteem were evaluated as possible cofounders and determined to have no effect on the logistic regression model for the reported behaviors," Dr. Swanson said. "Interestingly, the rate of reported gonorrhea and chlamydia did not differ between weight classes."
When asked about their motivations to engage in sex, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response option "your friends would respect you more" (P = .01), which suggests a peer influence, Dr. Swanson commented. "Interestingly, when these answers were compared with self-esteem, there was no difference [between weight groups]," she said.
When asked about their motivations to use birth control, a significantly higher proportion of overweight and obese females compared with their normal weight peers chose the response options "birth control is too much of a hassle to use" and "it is hard to get a boy to use birth control with you" (P = .01 for both).
While the motivation for overweight and obese females to engage in risky sexual behaviors remains unclear, "our findings suggest that peer influence may be significant," Dr. Swanson said. "An adolescent’s decision to engage in sex is likely multi-factorial, influenced by more than self-esteem and body image."
She went on to note that overweight and obese adolescent females "should be considered a vulnerable population. Clinicians should identify these patients and spend time exploring their thoughts about themselves, their peers, and their decisions to engage in sexual behaviors. It is our job to give accurate information, screen for and treat sexually transmitted infections, provide contraception, encourage parental involvement and, if needed, give good prenatal care. We as obstetricians and gynecologists have a unique opportunity and responsibility to care for, educate, and give feedback to adolescent girls to improve their overall sexual health."
Dr. Swanson said that she had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Compared with their normal weight peers, overweight and obese adolescent females were more likely to have sexual intercourse before age 13 (odds ratio, 1.3 and OR, 2.1, respectively), become pregnant (OR, 1.8 and OR, 2.3), and less likely to use oral contraception regularly (OR, 0.44 and OR, 0.28).
Data Source: Analysis of data from wave 1 of the National Longitudinal Study of Adolescent Health, which involved in-home interviews with 3,356 females in grades 7-12 during the 1994-1995 school year.
Disclosures: Dr. Swanson said that she had no relevant financial conflicts to disclose.
Phone Follow-Up to Medical Abortion Called "Feasible"
SAN DIEGO – Almost half of women undergoing a medical abortion could safely avoid an in-person follow-up visit by using phone follow-ups, a review of charts on 118 women suggests.
A typical protocol for medical abortion involves taking 200 mg of oral mifepristone, then 800 mcg of vaginal or buccal misoprostol, with an in-office follow-up visit a week later for a transvaginal ultrasound to make sure the abortion is complete. This study offered alternative follow-up by phone to women in a clinical practice at Magee-Women’s Hospital in Pittsburgh from Jan. 2010 through June 2011.
Phone follow-up included conducting a phone survey at 1 week and having the women perform a urine pregnancy test at 1 month so they could report the results when they were contacted in a 1-month follow-up phone call. Women with a positive urine pregnancy test were asked to return to the office for an ultrasound.
Overall, 44% of the 51 women who chose phone follow-up did not require office visits, Diana W. Samberg and Dr. Beatrice A. Chen reported at the annual meeting of the American College of Obstetricians and Gynecologists.
The proportion of women who were lost to follow-up did not differ significantly between the phone follow-up group (9 of 51 women, or 18%) and the office follow-up group (6 of 67 women, or 9%), reported Ms. Samberg and Dr. Chen of the University of Pittsburgh, where Ms. Samberg is a medical student.
The two groups also did not differ significantly in rates of adverse events, which were seen in 24% of the phone group and 17% of the office group. Among individual adverse events, the phone group was more likely to report heavy bleeding (14% vs. 3%) and to request an office visit for that reason. (Heavy bleeding was defined as any bleeding requiring an office visit.) Other adverse events included minimal bleeding, blood transfusion, emergency department visits, incomplete abortion, additional procedures, heavy pain, and allergic reaction. No women developed infection.
The trade-off for fewer office visits in the phone group was more phone calls. The phone group was significantly more likely to make unscheduled phone calls or office visits; some 55% in the phone group and 39% in the office group made unscheduled contacts. Two or more unscheduled contacts were made by 41% in the phone group and 20% in the office group.
In the phone follow-up group, the reasons for not being followed exclusively by phone (other than being lost to follow-up) included a switch by some women to office follow-up before the 1-week phone call; requests by some women to be seen in the office after the 1-week phone call even though the physician didn’t consider it necessary; and visits by some women before the 30-day call to medical clinics or the emergency department, during which follow-up or pregnancy tests were performed.
Among seven women who were advised to come to the office after the 1-week phone call, three required an additional procedure (either misoprostol or a D&C). Among women who were followed by phone at 30 days, three were advised to come to the office based on their positive urine pregnancy test, but only one required a D&C.
"Phone follow-up is feasible for medical abortion and can assess the need for further in-person follow-up," Ms. Samberg said.
The women who chose phone follow-up were significantly older (32 years on average), compared with 27 years in the office group. Women in the phone group were significantly more likely than those in the office group to have had a previous pregnancy (88% vs. 61%) and to have had a prior therapeutic abortion (51% vs. 30%). Parity did not differ significantly between groups. Women choosing phone follow-up were significantly more likely to be white and employed.
The findings follow a 2010 pilot study with 139 women that supported the feasibility of phone follow-up, in which 64% did not require in-person office follow-up (Contraception 2010;81:143-9), Ms. Samberg said.
Doing a urine pregnancy test and taking a good history are among alternatives that have been suggested as a means to avoid some ultrasounds and potentially improve follow-up compliance after medical abortions. Testing serum levels of beta–human chorionic gonadotropin also has been suggested as an alternative.
Ms. Samberg reported having no financial disclosures. Dr. Chen has received research support from Bayer Pharmaceuticals, Medicines360, Agile Therapeutics, and Evofem Inc.
This study provides additional evidence for the feasibility of phone follow-up for medical abortion, such as in Scotland (Contraception 2012, Jan. 5 [Epub ahead of print]). Although rates of unscheduled visits and phone calls were high in the phone follow-up group, the rate of adverse events between the two groups was similar.
This study might have particular applicability for women who live in areas remote from facilities where they can obtain a medical abortion and who have difficulty returning for a follow-up visit. Women who desire long-acting reversible contraceptives – IUDs and implants – may benefit from the follow-up visit for initiation of these highly effective methods.
Eve Espey, M.D., is a professor of obstetrics and gynecology at the University of New Mexico in Albuquerque. Dr. Espey chairs the American College of Obstetricians and Gynecologists’ Working Group on Long-Acting Reversible Contraception (LARC). She said she had no relevant financial disclosures.
This study provides additional evidence for the feasibility of phone follow-up for medical abortion, such as in Scotland (Contraception 2012, Jan. 5 [Epub ahead of print]). Although rates of unscheduled visits and phone calls were high in the phone follow-up group, the rate of adverse events between the two groups was similar.
This study might have particular applicability for women who live in areas remote from facilities where they can obtain a medical abortion and who have difficulty returning for a follow-up visit. Women who desire long-acting reversible contraceptives – IUDs and implants – may benefit from the follow-up visit for initiation of these highly effective methods.
Eve Espey, M.D., is a professor of obstetrics and gynecology at the University of New Mexico in Albuquerque. Dr. Espey chairs the American College of Obstetricians and Gynecologists’ Working Group on Long-Acting Reversible Contraception (LARC). She said she had no relevant financial disclosures.
This study provides additional evidence for the feasibility of phone follow-up for medical abortion, such as in Scotland (Contraception 2012, Jan. 5 [Epub ahead of print]). Although rates of unscheduled visits and phone calls were high in the phone follow-up group, the rate of adverse events between the two groups was similar.
This study might have particular applicability for women who live in areas remote from facilities where they can obtain a medical abortion and who have difficulty returning for a follow-up visit. Women who desire long-acting reversible contraceptives – IUDs and implants – may benefit from the follow-up visit for initiation of these highly effective methods.
Eve Espey, M.D., is a professor of obstetrics and gynecology at the University of New Mexico in Albuquerque. Dr. Espey chairs the American College of Obstetricians and Gynecologists’ Working Group on Long-Acting Reversible Contraception (LARC). She said she had no relevant financial disclosures.
SAN DIEGO – Almost half of women undergoing a medical abortion could safely avoid an in-person follow-up visit by using phone follow-ups, a review of charts on 118 women suggests.
A typical protocol for medical abortion involves taking 200 mg of oral mifepristone, then 800 mcg of vaginal or buccal misoprostol, with an in-office follow-up visit a week later for a transvaginal ultrasound to make sure the abortion is complete. This study offered alternative follow-up by phone to women in a clinical practice at Magee-Women’s Hospital in Pittsburgh from Jan. 2010 through June 2011.
Phone follow-up included conducting a phone survey at 1 week and having the women perform a urine pregnancy test at 1 month so they could report the results when they were contacted in a 1-month follow-up phone call. Women with a positive urine pregnancy test were asked to return to the office for an ultrasound.
Overall, 44% of the 51 women who chose phone follow-up did not require office visits, Diana W. Samberg and Dr. Beatrice A. Chen reported at the annual meeting of the American College of Obstetricians and Gynecologists.
The proportion of women who were lost to follow-up did not differ significantly between the phone follow-up group (9 of 51 women, or 18%) and the office follow-up group (6 of 67 women, or 9%), reported Ms. Samberg and Dr. Chen of the University of Pittsburgh, where Ms. Samberg is a medical student.
The two groups also did not differ significantly in rates of adverse events, which were seen in 24% of the phone group and 17% of the office group. Among individual adverse events, the phone group was more likely to report heavy bleeding (14% vs. 3%) and to request an office visit for that reason. (Heavy bleeding was defined as any bleeding requiring an office visit.) Other adverse events included minimal bleeding, blood transfusion, emergency department visits, incomplete abortion, additional procedures, heavy pain, and allergic reaction. No women developed infection.
The trade-off for fewer office visits in the phone group was more phone calls. The phone group was significantly more likely to make unscheduled phone calls or office visits; some 55% in the phone group and 39% in the office group made unscheduled contacts. Two or more unscheduled contacts were made by 41% in the phone group and 20% in the office group.
In the phone follow-up group, the reasons for not being followed exclusively by phone (other than being lost to follow-up) included a switch by some women to office follow-up before the 1-week phone call; requests by some women to be seen in the office after the 1-week phone call even though the physician didn’t consider it necessary; and visits by some women before the 30-day call to medical clinics or the emergency department, during which follow-up or pregnancy tests were performed.
Among seven women who were advised to come to the office after the 1-week phone call, three required an additional procedure (either misoprostol or a D&C). Among women who were followed by phone at 30 days, three were advised to come to the office based on their positive urine pregnancy test, but only one required a D&C.
"Phone follow-up is feasible for medical abortion and can assess the need for further in-person follow-up," Ms. Samberg said.
The women who chose phone follow-up were significantly older (32 years on average), compared with 27 years in the office group. Women in the phone group were significantly more likely than those in the office group to have had a previous pregnancy (88% vs. 61%) and to have had a prior therapeutic abortion (51% vs. 30%). Parity did not differ significantly between groups. Women choosing phone follow-up were significantly more likely to be white and employed.
The findings follow a 2010 pilot study with 139 women that supported the feasibility of phone follow-up, in which 64% did not require in-person office follow-up (Contraception 2010;81:143-9), Ms. Samberg said.
Doing a urine pregnancy test and taking a good history are among alternatives that have been suggested as a means to avoid some ultrasounds and potentially improve follow-up compliance after medical abortions. Testing serum levels of beta–human chorionic gonadotropin also has been suggested as an alternative.
Ms. Samberg reported having no financial disclosures. Dr. Chen has received research support from Bayer Pharmaceuticals, Medicines360, Agile Therapeutics, and Evofem Inc.
SAN DIEGO – Almost half of women undergoing a medical abortion could safely avoid an in-person follow-up visit by using phone follow-ups, a review of charts on 118 women suggests.
A typical protocol for medical abortion involves taking 200 mg of oral mifepristone, then 800 mcg of vaginal or buccal misoprostol, with an in-office follow-up visit a week later for a transvaginal ultrasound to make sure the abortion is complete. This study offered alternative follow-up by phone to women in a clinical practice at Magee-Women’s Hospital in Pittsburgh from Jan. 2010 through June 2011.
Phone follow-up included conducting a phone survey at 1 week and having the women perform a urine pregnancy test at 1 month so they could report the results when they were contacted in a 1-month follow-up phone call. Women with a positive urine pregnancy test were asked to return to the office for an ultrasound.
Overall, 44% of the 51 women who chose phone follow-up did not require office visits, Diana W. Samberg and Dr. Beatrice A. Chen reported at the annual meeting of the American College of Obstetricians and Gynecologists.
The proportion of women who were lost to follow-up did not differ significantly between the phone follow-up group (9 of 51 women, or 18%) and the office follow-up group (6 of 67 women, or 9%), reported Ms. Samberg and Dr. Chen of the University of Pittsburgh, where Ms. Samberg is a medical student.
The two groups also did not differ significantly in rates of adverse events, which were seen in 24% of the phone group and 17% of the office group. Among individual adverse events, the phone group was more likely to report heavy bleeding (14% vs. 3%) and to request an office visit for that reason. (Heavy bleeding was defined as any bleeding requiring an office visit.) Other adverse events included minimal bleeding, blood transfusion, emergency department visits, incomplete abortion, additional procedures, heavy pain, and allergic reaction. No women developed infection.
The trade-off for fewer office visits in the phone group was more phone calls. The phone group was significantly more likely to make unscheduled phone calls or office visits; some 55% in the phone group and 39% in the office group made unscheduled contacts. Two or more unscheduled contacts were made by 41% in the phone group and 20% in the office group.
In the phone follow-up group, the reasons for not being followed exclusively by phone (other than being lost to follow-up) included a switch by some women to office follow-up before the 1-week phone call; requests by some women to be seen in the office after the 1-week phone call even though the physician didn’t consider it necessary; and visits by some women before the 30-day call to medical clinics or the emergency department, during which follow-up or pregnancy tests were performed.
Among seven women who were advised to come to the office after the 1-week phone call, three required an additional procedure (either misoprostol or a D&C). Among women who were followed by phone at 30 days, three were advised to come to the office based on their positive urine pregnancy test, but only one required a D&C.
"Phone follow-up is feasible for medical abortion and can assess the need for further in-person follow-up," Ms. Samberg said.
The women who chose phone follow-up were significantly older (32 years on average), compared with 27 years in the office group. Women in the phone group were significantly more likely than those in the office group to have had a previous pregnancy (88% vs. 61%) and to have had a prior therapeutic abortion (51% vs. 30%). Parity did not differ significantly between groups. Women choosing phone follow-up were significantly more likely to be white and employed.
The findings follow a 2010 pilot study with 139 women that supported the feasibility of phone follow-up, in which 64% did not require in-person office follow-up (Contraception 2010;81:143-9), Ms. Samberg said.
Doing a urine pregnancy test and taking a good history are among alternatives that have been suggested as a means to avoid some ultrasounds and potentially improve follow-up compliance after medical abortions. Testing serum levels of beta–human chorionic gonadotropin also has been suggested as an alternative.
Ms. Samberg reported having no financial disclosures. Dr. Chen has received research support from Bayer Pharmaceuticals, Medicines360, Agile Therapeutics, and Evofem Inc.
FROM THE ANNUAL MEETING OF AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: In all, 44% of 51 women who chose phone follow-up after a medical abortion did not need in-person office follow-up visits.
Data Source: This was a chart review of 118 women who chose in-office or phone follow-up after medical abortion.
Disclosures: Ms. Samberg reported having no financial disclosures. Dr. Chen has received research support from Bayer Pharmaceuticals, Medicines360, Agile Therapeutics, and Evofem Inc.
Binder Helps Subset of Gynecologic Surgery Patients
SAN DIEGO – Gynecologic surgery patients at the highest risk for postoperative complications who wore an abdominopelvic compression binder for 24 hours after surgery had significantly improved ambulation compared with those who did not wear the binder, results from a randomized trial showed.
"The goals of postoperative pain management include early return of normal functions and minimal impact on ambulation," Dr. James Brian Szender said at the annual meeting of the American College of Obstetricians and Gynecologists. "Strategies that decrease morphine use, while at the same time increasing ambulation, have the potential to decrease postoperative pneumonia, prevent thromboembolic events, and lessen postoperative ileus."
Dr. Szender, a third-year resident in the department of obstetrics and gynecology at the University of Texas, and his associates at the Brooke Army Medical Center, both in San Antonio, enrolled 75 patients in a randomized trial to determine the impact of a neoprene abdominopelvic binder on postoperative morphine use, pain, and ambulation in the first 24 hours after abdominal gynecologic surgery. The binder is made by GemTech Medical and is known as the Mott compression garment. Patients were excluded from the study if they received an epidural injection, ketorolac, or oral analgesia, or if they were allergic to morphine.
The binder, which varies in size and retails for about $125, was placed on patients in the OR and remained in place until 24 hours after surgery. It is believed to reduce shear forces at the surgical incision, thereby causing less discomfort when the patient sits, stands, or walks. Patients received a standardized morphine regimen for the first 24 hours; study variables (including age, weight, incision type, total morphine use, postoperative pain score, and total number of ambulatory events) were collected after 24 hours.
Of the 75 patients, 36 received binders and 39 did not. The mean age of the study participants was 45 years and their mean weight was 78 kg. Spearman rank correlation identified a group of patients at high risk for decreased ambulation: those with vertical skin incisions, those older than age 50, and those with gynecologic cancer.
Dr. Szender reported that compared with nonuse of the compression binder, use of the binder increased the number of ambulatory events in the first 24 hours after surgery by 200% in patients with vertical skin incisions, by 150% in those older than age 50, and by 74% in those who had undergone surgery for gynecologic cancer. The researchers observed no statistically significant differences between the two groups in the amount of morphine used or in pain scores. However, "when patient variables were stratified by age, older patients used less morphine, had lower pain, got up earlier, and walked more when they had the binder on," Dr. Szender said.
He added that the binders "were liked [and] well tolerated, and patient compliance was 100%."
GemTech Medical provided the binders used in the study. Dr. Szender said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Gynecologic surgery patients at the highest risk for postoperative complications who wore an abdominopelvic compression binder for 24 hours after surgery had significantly improved ambulation compared with those who did not wear the binder, results from a randomized trial showed.
"The goals of postoperative pain management include early return of normal functions and minimal impact on ambulation," Dr. James Brian Szender said at the annual meeting of the American College of Obstetricians and Gynecologists. "Strategies that decrease morphine use, while at the same time increasing ambulation, have the potential to decrease postoperative pneumonia, prevent thromboembolic events, and lessen postoperative ileus."
Dr. Szender, a third-year resident in the department of obstetrics and gynecology at the University of Texas, and his associates at the Brooke Army Medical Center, both in San Antonio, enrolled 75 patients in a randomized trial to determine the impact of a neoprene abdominopelvic binder on postoperative morphine use, pain, and ambulation in the first 24 hours after abdominal gynecologic surgery. The binder is made by GemTech Medical and is known as the Mott compression garment. Patients were excluded from the study if they received an epidural injection, ketorolac, or oral analgesia, or if they were allergic to morphine.
The binder, which varies in size and retails for about $125, was placed on patients in the OR and remained in place until 24 hours after surgery. It is believed to reduce shear forces at the surgical incision, thereby causing less discomfort when the patient sits, stands, or walks. Patients received a standardized morphine regimen for the first 24 hours; study variables (including age, weight, incision type, total morphine use, postoperative pain score, and total number of ambulatory events) were collected after 24 hours.
Of the 75 patients, 36 received binders and 39 did not. The mean age of the study participants was 45 years and their mean weight was 78 kg. Spearman rank correlation identified a group of patients at high risk for decreased ambulation: those with vertical skin incisions, those older than age 50, and those with gynecologic cancer.
Dr. Szender reported that compared with nonuse of the compression binder, use of the binder increased the number of ambulatory events in the first 24 hours after surgery by 200% in patients with vertical skin incisions, by 150% in those older than age 50, and by 74% in those who had undergone surgery for gynecologic cancer. The researchers observed no statistically significant differences between the two groups in the amount of morphine used or in pain scores. However, "when patient variables were stratified by age, older patients used less morphine, had lower pain, got up earlier, and walked more when they had the binder on," Dr. Szender said.
He added that the binders "were liked [and] well tolerated, and patient compliance was 100%."
GemTech Medical provided the binders used in the study. Dr. Szender said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Gynecologic surgery patients at the highest risk for postoperative complications who wore an abdominopelvic compression binder for 24 hours after surgery had significantly improved ambulation compared with those who did not wear the binder, results from a randomized trial showed.
"The goals of postoperative pain management include early return of normal functions and minimal impact on ambulation," Dr. James Brian Szender said at the annual meeting of the American College of Obstetricians and Gynecologists. "Strategies that decrease morphine use, while at the same time increasing ambulation, have the potential to decrease postoperative pneumonia, prevent thromboembolic events, and lessen postoperative ileus."
Dr. Szender, a third-year resident in the department of obstetrics and gynecology at the University of Texas, and his associates at the Brooke Army Medical Center, both in San Antonio, enrolled 75 patients in a randomized trial to determine the impact of a neoprene abdominopelvic binder on postoperative morphine use, pain, and ambulation in the first 24 hours after abdominal gynecologic surgery. The binder is made by GemTech Medical and is known as the Mott compression garment. Patients were excluded from the study if they received an epidural injection, ketorolac, or oral analgesia, or if they were allergic to morphine.
The binder, which varies in size and retails for about $125, was placed on patients in the OR and remained in place until 24 hours after surgery. It is believed to reduce shear forces at the surgical incision, thereby causing less discomfort when the patient sits, stands, or walks. Patients received a standardized morphine regimen for the first 24 hours; study variables (including age, weight, incision type, total morphine use, postoperative pain score, and total number of ambulatory events) were collected after 24 hours.
Of the 75 patients, 36 received binders and 39 did not. The mean age of the study participants was 45 years and their mean weight was 78 kg. Spearman rank correlation identified a group of patients at high risk for decreased ambulation: those with vertical skin incisions, those older than age 50, and those with gynecologic cancer.
Dr. Szender reported that compared with nonuse of the compression binder, use of the binder increased the number of ambulatory events in the first 24 hours after surgery by 200% in patients with vertical skin incisions, by 150% in those older than age 50, and by 74% in those who had undergone surgery for gynecologic cancer. The researchers observed no statistically significant differences between the two groups in the amount of morphine used or in pain scores. However, "when patient variables were stratified by age, older patients used less morphine, had lower pain, got up earlier, and walked more when they had the binder on," Dr. Szender said.
He added that the binders "were liked [and] well tolerated, and patient compliance was 100%."
GemTech Medical provided the binders used in the study. Dr. Szender said that he had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Use of a neoprene abdominopelvic compression binder after gynecologic surgery increased the number of ambulatory events in the first 24 hours after surgery by 200% in patients with vertical skin incisions, by 150% in those older than age 50, and by 74% in those who had undergone surgery for gynecologic cancer.
Data Source: Data are from a randomized trial of 75 patients conducted to determine the impact of the binder on postoperative morphine use, pain, and ambulation in the first 24 hours after abdominal gynecologic surgery.
Disclosures: GemTech Medical provided the binders used in the study. Dr. Szender said that he had no relevant financial conflicts to disclose.
No Increased VTE Risk Found With NuvaRing
SAN DIEGO – The risk of venous thromboembolism in women using an etonogestrel-containing vaginal ring did not differ significantly from the risk in women on combined oral contraceptives over a 4-year period, a prospective cohort study of 33,704 women found.
There were 56 (less than 1%) venous thromboemboli during the study. The rate of venous thromboembolism (VTE) was approximately 9/10,000 woman-years in 16,884 women using the NuvaRing and in 16,820 women on combined oral contraceptives (OCs), Dr. Klaas Heinemann Jr. and his associates reported at the annual meeting of the American College of Obstetricians and Gynecologists.
Subanalyses also found no significant difference in risk when comparing NuvaRing with combined OC regimens that did not contain desogestrel, gestodene, drospirenone, or combinations of those, said Dr. Heinemann, managing director of a private research institute, the Berlin Center for Epidemiology and Health Research.
There were 1,915 serious adverse events during the TASC (Transatlantic Active Surveillance on Cardiovascular Safety of NuvaRing) study. Rates of serious adverse events were less than 300 events/10,000 woman-years in women on NuvaRing or combined OCs and in women who had stopped treatment, but were not pregnant. The risk of serious adverse events did not differ significantly between those groups, but was significantly higher in women who became pregnant, who had 900 serious adverse events per 10,000 woman-years.
The study defined serious adverse events as any adverse event that results in death, a life-threatening experience, inpatient hospitalization, persistent or significant disability or incapacity, or the need for medical or surgical intervention to prevent one of these events. Most serious adverse events involved injury, the genitourinary system (ovarian cysts, kidney stones, salpingitis, UTI), or the digestive system (appendectomy).
From 2007 to 2012, the investigators followed patients recruited by ob.gyns. at more than 3,000 centers in the United States and five European countries, with 51% of the women enrolled at U.S. centers. Follow-up was by patient questionnaire at 6, 12, 24, 36, and 48 months, with all patient-reported outcomes verified with the attending physician. Three percent of patients were lost to follow-up in each of the NuvaRing and combined OC groups. The investigators controlled for the effects of previous hormonal contraceptive use, the patient’s medical history, and a family history of VTE.
Patients in the NuvaRing and combined OC groups did not differ significantly in age, although use of NuvaRing was slightly lower in women younger than 20 years, compared with use of OCs. In the NuvaRing group, 9% were younger than 20 years, 55% were aged 20-29 years, 27% were aged 30-39 years, and 9% were 40 years or older. In the combined OCs group, the distribution was 16%, 54%, 22%, and 8%, respectively.
The two groups also did not differ significantly in body mass index (BMI), smoking rates, regular use of medications, or history of VTE or arterial thromboembolism. Less than 2% in each group had a history of VTE or arterial thromboembolism, a nonsignificant difference.
Compared with patients in Europe, U.S. patients were more likely to have a BMI of 30 kg/m2 or greater (25% vs. 13%), were half as likely to smoke (16% vs. 30%), and were more likely to be using medication regularly, mainly psychotropic medications (23% vs. 10%), Dr. Heinemann said.
The study won first prize from the ACOG’s committee on the scientific program among meeting papers on current clinical and basic investigations.
The findings are limited by the observational design of the study. Information on specific gene mutations were not available for many patients, but the predictive value of these mutations for VTE is low compared with the predictive value of family history, he said.
The study included women who were using contraceptives for the first time or switching from other contraceptives or previous users of NuvaRing who had at least a 4-week break since previous use. Long-term users of these contraceptive methods were excluded from the study because the risk for VTE is highest in the first few months of use.
The study was funded by Merck, which markets NuvaRing. Dr. Heinemann reported no other financial disclosures.
SAN DIEGO – The risk of venous thromboembolism in women using an etonogestrel-containing vaginal ring did not differ significantly from the risk in women on combined oral contraceptives over a 4-year period, a prospective cohort study of 33,704 women found.
There were 56 (less than 1%) venous thromboemboli during the study. The rate of venous thromboembolism (VTE) was approximately 9/10,000 woman-years in 16,884 women using the NuvaRing and in 16,820 women on combined oral contraceptives (OCs), Dr. Klaas Heinemann Jr. and his associates reported at the annual meeting of the American College of Obstetricians and Gynecologists.
Subanalyses also found no significant difference in risk when comparing NuvaRing with combined OC regimens that did not contain desogestrel, gestodene, drospirenone, or combinations of those, said Dr. Heinemann, managing director of a private research institute, the Berlin Center for Epidemiology and Health Research.
There were 1,915 serious adverse events during the TASC (Transatlantic Active Surveillance on Cardiovascular Safety of NuvaRing) study. Rates of serious adverse events were less than 300 events/10,000 woman-years in women on NuvaRing or combined OCs and in women who had stopped treatment, but were not pregnant. The risk of serious adverse events did not differ significantly between those groups, but was significantly higher in women who became pregnant, who had 900 serious adverse events per 10,000 woman-years.
The study defined serious adverse events as any adverse event that results in death, a life-threatening experience, inpatient hospitalization, persistent or significant disability or incapacity, or the need for medical or surgical intervention to prevent one of these events. Most serious adverse events involved injury, the genitourinary system (ovarian cysts, kidney stones, salpingitis, UTI), or the digestive system (appendectomy).
From 2007 to 2012, the investigators followed patients recruited by ob.gyns. at more than 3,000 centers in the United States and five European countries, with 51% of the women enrolled at U.S. centers. Follow-up was by patient questionnaire at 6, 12, 24, 36, and 48 months, with all patient-reported outcomes verified with the attending physician. Three percent of patients were lost to follow-up in each of the NuvaRing and combined OC groups. The investigators controlled for the effects of previous hormonal contraceptive use, the patient’s medical history, and a family history of VTE.
Patients in the NuvaRing and combined OC groups did not differ significantly in age, although use of NuvaRing was slightly lower in women younger than 20 years, compared with use of OCs. In the NuvaRing group, 9% were younger than 20 years, 55% were aged 20-29 years, 27% were aged 30-39 years, and 9% were 40 years or older. In the combined OCs group, the distribution was 16%, 54%, 22%, and 8%, respectively.
The two groups also did not differ significantly in body mass index (BMI), smoking rates, regular use of medications, or history of VTE or arterial thromboembolism. Less than 2% in each group had a history of VTE or arterial thromboembolism, a nonsignificant difference.
Compared with patients in Europe, U.S. patients were more likely to have a BMI of 30 kg/m2 or greater (25% vs. 13%), were half as likely to smoke (16% vs. 30%), and were more likely to be using medication regularly, mainly psychotropic medications (23% vs. 10%), Dr. Heinemann said.
The study won first prize from the ACOG’s committee on the scientific program among meeting papers on current clinical and basic investigations.
The findings are limited by the observational design of the study. Information on specific gene mutations were not available for many patients, but the predictive value of these mutations for VTE is low compared with the predictive value of family history, he said.
The study included women who were using contraceptives for the first time or switching from other contraceptives or previous users of NuvaRing who had at least a 4-week break since previous use. Long-term users of these contraceptive methods were excluded from the study because the risk for VTE is highest in the first few months of use.
The study was funded by Merck, which markets NuvaRing. Dr. Heinemann reported no other financial disclosures.
SAN DIEGO – The risk of venous thromboembolism in women using an etonogestrel-containing vaginal ring did not differ significantly from the risk in women on combined oral contraceptives over a 4-year period, a prospective cohort study of 33,704 women found.
There were 56 (less than 1%) venous thromboemboli during the study. The rate of venous thromboembolism (VTE) was approximately 9/10,000 woman-years in 16,884 women using the NuvaRing and in 16,820 women on combined oral contraceptives (OCs), Dr. Klaas Heinemann Jr. and his associates reported at the annual meeting of the American College of Obstetricians and Gynecologists.
Subanalyses also found no significant difference in risk when comparing NuvaRing with combined OC regimens that did not contain desogestrel, gestodene, drospirenone, or combinations of those, said Dr. Heinemann, managing director of a private research institute, the Berlin Center for Epidemiology and Health Research.
There were 1,915 serious adverse events during the TASC (Transatlantic Active Surveillance on Cardiovascular Safety of NuvaRing) study. Rates of serious adverse events were less than 300 events/10,000 woman-years in women on NuvaRing or combined OCs and in women who had stopped treatment, but were not pregnant. The risk of serious adverse events did not differ significantly between those groups, but was significantly higher in women who became pregnant, who had 900 serious adverse events per 10,000 woman-years.
The study defined serious adverse events as any adverse event that results in death, a life-threatening experience, inpatient hospitalization, persistent or significant disability or incapacity, or the need for medical or surgical intervention to prevent one of these events. Most serious adverse events involved injury, the genitourinary system (ovarian cysts, kidney stones, salpingitis, UTI), or the digestive system (appendectomy).
From 2007 to 2012, the investigators followed patients recruited by ob.gyns. at more than 3,000 centers in the United States and five European countries, with 51% of the women enrolled at U.S. centers. Follow-up was by patient questionnaire at 6, 12, 24, 36, and 48 months, with all patient-reported outcomes verified with the attending physician. Three percent of patients were lost to follow-up in each of the NuvaRing and combined OC groups. The investigators controlled for the effects of previous hormonal contraceptive use, the patient’s medical history, and a family history of VTE.
Patients in the NuvaRing and combined OC groups did not differ significantly in age, although use of NuvaRing was slightly lower in women younger than 20 years, compared with use of OCs. In the NuvaRing group, 9% were younger than 20 years, 55% were aged 20-29 years, 27% were aged 30-39 years, and 9% were 40 years or older. In the combined OCs group, the distribution was 16%, 54%, 22%, and 8%, respectively.
The two groups also did not differ significantly in body mass index (BMI), smoking rates, regular use of medications, or history of VTE or arterial thromboembolism. Less than 2% in each group had a history of VTE or arterial thromboembolism, a nonsignificant difference.
Compared with patients in Europe, U.S. patients were more likely to have a BMI of 30 kg/m2 or greater (25% vs. 13%), were half as likely to smoke (16% vs. 30%), and were more likely to be using medication regularly, mainly psychotropic medications (23% vs. 10%), Dr. Heinemann said.
The study won first prize from the ACOG’s committee on the scientific program among meeting papers on current clinical and basic investigations.
The findings are limited by the observational design of the study. Information on specific gene mutations were not available for many patients, but the predictive value of these mutations for VTE is low compared with the predictive value of family history, he said.
The study included women who were using contraceptives for the first time or switching from other contraceptives or previous users of NuvaRing who had at least a 4-week break since previous use. Long-term users of these contraceptive methods were excluded from the study because the risk for VTE is highest in the first few months of use.
The study was funded by Merck, which markets NuvaRing. Dr. Heinemann reported no other financial disclosures.
FROM THE ANNUAL MEETING OF AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: The 4-year risk of venous thromboembolism was 9 emboli/10,000 woman-years in patients on NuvaRing or combined oral contraceptives.
Data Source: This was a prospective observational cohort study of 33,704 women in six countries.
Disclosures: The study was funded by Merck, which markets NuvaRing. Dr. Heinemann reported no other financial disclosures.
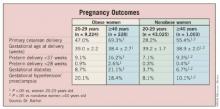
BMI Linked to Success of Arrest of Dilatation Treatment
SAN DIEGO – Women with a body mass index of 35 kg/m2 or greater responded poorly to oxytocin treatment for arrest of dilatation, compared with leaner subjects, results from a single study showed.
"Maternal obesity is increasingly prevalent and is associated with high rates of dysfunctional labor and cesarean delivery, outcomes that are not completely attributable to high fetal weight," researchers led by Dr. Shelly Soni wrote in a poster presented during the annual meeting of the American College of Obstetricians and Gynecologists. "Obesity may inhibit uterine contractility and labor progress."
To test their hypothesis that oxytocin administered to treat arrest of dilatation is less effective in obese women, compared with lean women, Dr. Soni and her associates reviewed an electronic database for women with singleton term pregnancies in cephalic presentation who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011. After excluding patients with medical complications or prior cesarean delivery, the researchers identified 118 consecutive cases diagnosed with arrest of dilatation and grouped them into one of four body mass index (BMI) classifications: BMI of less than 25 kg/m2 (group A; n = 30); BMI of 25-29.9 kg/m2 (group B; n = 33); BMI of 30-34.9 kg/m2 (group C; n = 32), and BMI of 35 kg/m2 or greater (group D; n =23).
An investigator blinded to the patients and to the groups constructed labor curves for each patient. Successful treatment of an arrest of dilatation was defined as attainment of full dilatation.
Dr. Soni, a third-year resident in the department of obstetrics and gynecology at the center, reported that none of the four groups differed significantly in birth weight, gestational age, parity, or maternal age. However, successful treatment of the arrest disorder was achieved in 90% of women in groups A and B, 72% of women in group C, and just 39% of women in group D.
"The amount of oxytocin used as well as time to delivery or cesarean decision after starting oxytocin was significantly higher in group D (P = .001) [and] the cesarean delivery rate was directly related to maternal BMI across the cohort (P = .001)," the researchers noted. "Among patients who had further dilatation after beginning oxytocin, the frequency with which the post-arrest slope was equal to or greater than the pre-arrest slope was inversely related to maternal BMI."
They went on to speculate that obesity "may inhibit uterine contractility and the uterine response to oxytocin, which in turn may explain our results, and the high rates of dysfunctional labor and cesarean delivery among obese women."
In an interview, Dr. Soni noted that one limitation of the analysis was that "it was not designed to see if a higher dose of oxytocin would be effective in obese women."
Dr. Soni said she had no relevant financial conflicts to disclose.
SAN DIEGO – Women with a body mass index of 35 kg/m2 or greater responded poorly to oxytocin treatment for arrest of dilatation, compared with leaner subjects, results from a single study showed.
"Maternal obesity is increasingly prevalent and is associated with high rates of dysfunctional labor and cesarean delivery, outcomes that are not completely attributable to high fetal weight," researchers led by Dr. Shelly Soni wrote in a poster presented during the annual meeting of the American College of Obstetricians and Gynecologists. "Obesity may inhibit uterine contractility and labor progress."
To test their hypothesis that oxytocin administered to treat arrest of dilatation is less effective in obese women, compared with lean women, Dr. Soni and her associates reviewed an electronic database for women with singleton term pregnancies in cephalic presentation who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011. After excluding patients with medical complications or prior cesarean delivery, the researchers identified 118 consecutive cases diagnosed with arrest of dilatation and grouped them into one of four body mass index (BMI) classifications: BMI of less than 25 kg/m2 (group A; n = 30); BMI of 25-29.9 kg/m2 (group B; n = 33); BMI of 30-34.9 kg/m2 (group C; n = 32), and BMI of 35 kg/m2 or greater (group D; n =23).
An investigator blinded to the patients and to the groups constructed labor curves for each patient. Successful treatment of an arrest of dilatation was defined as attainment of full dilatation.
Dr. Soni, a third-year resident in the department of obstetrics and gynecology at the center, reported that none of the four groups differed significantly in birth weight, gestational age, parity, or maternal age. However, successful treatment of the arrest disorder was achieved in 90% of women in groups A and B, 72% of women in group C, and just 39% of women in group D.
"The amount of oxytocin used as well as time to delivery or cesarean decision after starting oxytocin was significantly higher in group D (P = .001) [and] the cesarean delivery rate was directly related to maternal BMI across the cohort (P = .001)," the researchers noted. "Among patients who had further dilatation after beginning oxytocin, the frequency with which the post-arrest slope was equal to or greater than the pre-arrest slope was inversely related to maternal BMI."
They went on to speculate that obesity "may inhibit uterine contractility and the uterine response to oxytocin, which in turn may explain our results, and the high rates of dysfunctional labor and cesarean delivery among obese women."
In an interview, Dr. Soni noted that one limitation of the analysis was that "it was not designed to see if a higher dose of oxytocin would be effective in obese women."
Dr. Soni said she had no relevant financial conflicts to disclose.
SAN DIEGO – Women with a body mass index of 35 kg/m2 or greater responded poorly to oxytocin treatment for arrest of dilatation, compared with leaner subjects, results from a single study showed.
"Maternal obesity is increasingly prevalent and is associated with high rates of dysfunctional labor and cesarean delivery, outcomes that are not completely attributable to high fetal weight," researchers led by Dr. Shelly Soni wrote in a poster presented during the annual meeting of the American College of Obstetricians and Gynecologists. "Obesity may inhibit uterine contractility and labor progress."
To test their hypothesis that oxytocin administered to treat arrest of dilatation is less effective in obese women, compared with lean women, Dr. Soni and her associates reviewed an electronic database for women with singleton term pregnancies in cephalic presentation who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011. After excluding patients with medical complications or prior cesarean delivery, the researchers identified 118 consecutive cases diagnosed with arrest of dilatation and grouped them into one of four body mass index (BMI) classifications: BMI of less than 25 kg/m2 (group A; n = 30); BMI of 25-29.9 kg/m2 (group B; n = 33); BMI of 30-34.9 kg/m2 (group C; n = 32), and BMI of 35 kg/m2 or greater (group D; n =23).
An investigator blinded to the patients and to the groups constructed labor curves for each patient. Successful treatment of an arrest of dilatation was defined as attainment of full dilatation.
Dr. Soni, a third-year resident in the department of obstetrics and gynecology at the center, reported that none of the four groups differed significantly in birth weight, gestational age, parity, or maternal age. However, successful treatment of the arrest disorder was achieved in 90% of women in groups A and B, 72% of women in group C, and just 39% of women in group D.
"The amount of oxytocin used as well as time to delivery or cesarean decision after starting oxytocin was significantly higher in group D (P = .001) [and] the cesarean delivery rate was directly related to maternal BMI across the cohort (P = .001)," the researchers noted. "Among patients who had further dilatation after beginning oxytocin, the frequency with which the post-arrest slope was equal to or greater than the pre-arrest slope was inversely related to maternal BMI."
They went on to speculate that obesity "may inhibit uterine contractility and the uterine response to oxytocin, which in turn may explain our results, and the high rates of dysfunctional labor and cesarean delivery among obese women."
In an interview, Dr. Soni noted that one limitation of the analysis was that "it was not designed to see if a higher dose of oxytocin would be effective in obese women."
Dr. Soni said she had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Successful treatment of arrest of dilatation with oxytocin was achieved in 90% of women with body mass indexes of less than 25 kg/m2 and 25-29.9 kg/m2, 72% in women with a BMI of 30-34.9 kg/m2, and 39% in women with a BMI of 35 kg/m2 or greater.
Data Source: A review of 118 women with singleton pregnancies who labored and delivered at Flushing (N.Y.) Hospital Medical Center between July 2004 and August 2011.
Disclosures: Dr. Soni said she had no relevant financial conflicts to disclose.
Physicians Underestimate Patient Pain from IUD Insertion
SAN DIEGO – Medical providers – especially physicians – underestimate how much pain a woman feels when an IUD is inserted, an analysis of data on 200 patients and their providers suggests.
The data came from a double-blind, randomized, placebo-controlled trial of intracervical lidocaine gel, compared with placebo, for relieving pain during IUD insertion; it found no advantage to lidocaine gel. This secondary analysis looked at patient and provider ratings for patient pain on a 100-mm visual analogue scale (VAS), with no pain at 0 mm and worst pain possible at 100 mm.
The point of maximum pain during the IUD insertion procedure rated a mean score of 64 from patients, compared with a mean rating of 35 from providers. That 29-mm difference was statistically significant, Dr. Karla E. Maguire and her associates reported at the annual meeting of the American College of Obstetricians and Gynecologists.
Nineteen percent of providers rated patient pain within 10 mm of patients’ ratings. Twenty-three percent of providers gave ratings that were 50 mm or farther apart from patients’ pain ratings, said Dr. Maguire, an ob.gyn. at the University of Miami.
The results will be published in the journal Contraception, she said.
Patients rated pain at four points during the procedure: tenaculum placement; uterine sounding; IUD insertion; and speculum removal. Patients and providers agreed about the timing of maximum pain 41% of the time – a very poor level of agreement, she said.
Uterine sounding was rated the most painful point by 40% of patients and 45% of providers. IUD insertion was rated the most painful point by 36% of patients and 15% of providers. Tenaculum placement was rated the most painful point by 14% of patients and 25% of providers. Speculum removal was rated the most painful point by 10% of patients and 5% of providers. No patients and 8% of providers said patients felt no pain. Three percent of providers (and no patients) wrote in some other point of maximum pain for the procedure instead of answering the multiple-choice question.
Ratings by the midlevel providers were slightly but significantly closer to patient ratings, compared with physician ratings – 7 points closer, on average, Dr. Maguire said. The midlevel providers were no better than were attending physicians, however, in estimating the point of maximum patient pain during the procedure.
The mean age of the patients was 27 years. The cohort was 77% Latina/Hispanic, 13% white, and 10% other races/ethnicities. Thirty percent were nulliparous. Their mean pain score for past episodes of dysmenorrhea was 35. They anticipated a pain rating of 57 for the IUD insertion procedure.
Among the providers, 91 (46%) were physicians, 91 (46%) were nurse practitioners, certified nurse-midwives, or physician assistants, and 18 (9%) were residents. Most (52%) had 11-20 years of experience in IUD insertion, while 26% had 5-10 years of experience, and 22% had less than 5 years of experience.
The IUD insertion procedures were done in public clinics in 80% of cases and in private clinics in 20%.
The pain that accompanies IUD insertion may be a barrier to wider use of IUDs, she said. Previous studies suggest that pain is more likely in nulliparous women, those whose last pregnancy is remote from the time of IUD insertion, in women with dysmenorrhea, when pain is highly anticipated, or with the levonorgestrel IUD.
Previous studies have shown that medical providers underestimate patient pain in emergency departments, family medicine clinics, during cystoscopy, and in patients with coronary artery disease. Other studies suggest that differences in pain ratings by patients and physicians are predictive of inadequate pain management. Underestimating pain could result in less research on new methods of pain relief.
The current study’s large sample size and variety of providers were strengths, but it was a secondary analysis and may not be generalizable to other settings, Dr. Maguire said.
"More research needs to be done to provide patients with better anesthesia for IUD insertion," she said.
Approximately 6% of U.S. women who use contraceptives choose IUDs, she said. Both the copper IUD and levonorgestrel IUD have low failure rates (0.8% and 0.2% per year with typical use, respectively) and high percentages of users who choose to continue using the device (78% and 80%, respectively).
Dr. Maguire reported having no relevant financial disclosures.
SAN DIEGO – Medical providers – especially physicians – underestimate how much pain a woman feels when an IUD is inserted, an analysis of data on 200 patients and their providers suggests.
The data came from a double-blind, randomized, placebo-controlled trial of intracervical lidocaine gel, compared with placebo, for relieving pain during IUD insertion; it found no advantage to lidocaine gel. This secondary analysis looked at patient and provider ratings for patient pain on a 100-mm visual analogue scale (VAS), with no pain at 0 mm and worst pain possible at 100 mm.
The point of maximum pain during the IUD insertion procedure rated a mean score of 64 from patients, compared with a mean rating of 35 from providers. That 29-mm difference was statistically significant, Dr. Karla E. Maguire and her associates reported at the annual meeting of the American College of Obstetricians and Gynecologists.
Nineteen percent of providers rated patient pain within 10 mm of patients’ ratings. Twenty-three percent of providers gave ratings that were 50 mm or farther apart from patients’ pain ratings, said Dr. Maguire, an ob.gyn. at the University of Miami.
The results will be published in the journal Contraception, she said.
Patients rated pain at four points during the procedure: tenaculum placement; uterine sounding; IUD insertion; and speculum removal. Patients and providers agreed about the timing of maximum pain 41% of the time – a very poor level of agreement, she said.
Uterine sounding was rated the most painful point by 40% of patients and 45% of providers. IUD insertion was rated the most painful point by 36% of patients and 15% of providers. Tenaculum placement was rated the most painful point by 14% of patients and 25% of providers. Speculum removal was rated the most painful point by 10% of patients and 5% of providers. No patients and 8% of providers said patients felt no pain. Three percent of providers (and no patients) wrote in some other point of maximum pain for the procedure instead of answering the multiple-choice question.
Ratings by the midlevel providers were slightly but significantly closer to patient ratings, compared with physician ratings – 7 points closer, on average, Dr. Maguire said. The midlevel providers were no better than were attending physicians, however, in estimating the point of maximum patient pain during the procedure.
The mean age of the patients was 27 years. The cohort was 77% Latina/Hispanic, 13% white, and 10% other races/ethnicities. Thirty percent were nulliparous. Their mean pain score for past episodes of dysmenorrhea was 35. They anticipated a pain rating of 57 for the IUD insertion procedure.
Among the providers, 91 (46%) were physicians, 91 (46%) were nurse practitioners, certified nurse-midwives, or physician assistants, and 18 (9%) were residents. Most (52%) had 11-20 years of experience in IUD insertion, while 26% had 5-10 years of experience, and 22% had less than 5 years of experience.
The IUD insertion procedures were done in public clinics in 80% of cases and in private clinics in 20%.
The pain that accompanies IUD insertion may be a barrier to wider use of IUDs, she said. Previous studies suggest that pain is more likely in nulliparous women, those whose last pregnancy is remote from the time of IUD insertion, in women with dysmenorrhea, when pain is highly anticipated, or with the levonorgestrel IUD.
Previous studies have shown that medical providers underestimate patient pain in emergency departments, family medicine clinics, during cystoscopy, and in patients with coronary artery disease. Other studies suggest that differences in pain ratings by patients and physicians are predictive of inadequate pain management. Underestimating pain could result in less research on new methods of pain relief.
The current study’s large sample size and variety of providers were strengths, but it was a secondary analysis and may not be generalizable to other settings, Dr. Maguire said.
"More research needs to be done to provide patients with better anesthesia for IUD insertion," she said.
Approximately 6% of U.S. women who use contraceptives choose IUDs, she said. Both the copper IUD and levonorgestrel IUD have low failure rates (0.8% and 0.2% per year with typical use, respectively) and high percentages of users who choose to continue using the device (78% and 80%, respectively).
Dr. Maguire reported having no relevant financial disclosures.
SAN DIEGO – Medical providers – especially physicians – underestimate how much pain a woman feels when an IUD is inserted, an analysis of data on 200 patients and their providers suggests.
The data came from a double-blind, randomized, placebo-controlled trial of intracervical lidocaine gel, compared with placebo, for relieving pain during IUD insertion; it found no advantage to lidocaine gel. This secondary analysis looked at patient and provider ratings for patient pain on a 100-mm visual analogue scale (VAS), with no pain at 0 mm and worst pain possible at 100 mm.
The point of maximum pain during the IUD insertion procedure rated a mean score of 64 from patients, compared with a mean rating of 35 from providers. That 29-mm difference was statistically significant, Dr. Karla E. Maguire and her associates reported at the annual meeting of the American College of Obstetricians and Gynecologists.
Nineteen percent of providers rated patient pain within 10 mm of patients’ ratings. Twenty-three percent of providers gave ratings that were 50 mm or farther apart from patients’ pain ratings, said Dr. Maguire, an ob.gyn. at the University of Miami.
The results will be published in the journal Contraception, she said.
Patients rated pain at four points during the procedure: tenaculum placement; uterine sounding; IUD insertion; and speculum removal. Patients and providers agreed about the timing of maximum pain 41% of the time – a very poor level of agreement, she said.
Uterine sounding was rated the most painful point by 40% of patients and 45% of providers. IUD insertion was rated the most painful point by 36% of patients and 15% of providers. Tenaculum placement was rated the most painful point by 14% of patients and 25% of providers. Speculum removal was rated the most painful point by 10% of patients and 5% of providers. No patients and 8% of providers said patients felt no pain. Three percent of providers (and no patients) wrote in some other point of maximum pain for the procedure instead of answering the multiple-choice question.
Ratings by the midlevel providers were slightly but significantly closer to patient ratings, compared with physician ratings – 7 points closer, on average, Dr. Maguire said. The midlevel providers were no better than were attending physicians, however, in estimating the point of maximum patient pain during the procedure.
The mean age of the patients was 27 years. The cohort was 77% Latina/Hispanic, 13% white, and 10% other races/ethnicities. Thirty percent were nulliparous. Their mean pain score for past episodes of dysmenorrhea was 35. They anticipated a pain rating of 57 for the IUD insertion procedure.
Among the providers, 91 (46%) were physicians, 91 (46%) were nurse practitioners, certified nurse-midwives, or physician assistants, and 18 (9%) were residents. Most (52%) had 11-20 years of experience in IUD insertion, while 26% had 5-10 years of experience, and 22% had less than 5 years of experience.
The IUD insertion procedures were done in public clinics in 80% of cases and in private clinics in 20%.
The pain that accompanies IUD insertion may be a barrier to wider use of IUDs, she said. Previous studies suggest that pain is more likely in nulliparous women, those whose last pregnancy is remote from the time of IUD insertion, in women with dysmenorrhea, when pain is highly anticipated, or with the levonorgestrel IUD.
Previous studies have shown that medical providers underestimate patient pain in emergency departments, family medicine clinics, during cystoscopy, and in patients with coronary artery disease. Other studies suggest that differences in pain ratings by patients and physicians are predictive of inadequate pain management. Underestimating pain could result in less research on new methods of pain relief.
The current study’s large sample size and variety of providers were strengths, but it was a secondary analysis and may not be generalizable to other settings, Dr. Maguire said.
"More research needs to be done to provide patients with better anesthesia for IUD insertion," she said.
Approximately 6% of U.S. women who use contraceptives choose IUDs, she said. Both the copper IUD and levonorgestrel IUD have low failure rates (0.8% and 0.2% per year with typical use, respectively) and high percentages of users who choose to continue using the device (78% and 80%, respectively).
Dr. Maguire reported having no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: Patients rated their maximum pain during IUD insertion at 64 mm on a 100-mm visual analogue scale, compared with a rating by providers of maximum patient pain of 35.
Data Source: This is a secondary analysis of patient pain ratings by 200 patients and providers following IUD insertion.
Disclosures: Dr. Maguire reported having no relevant financial disclosures.
Abnormal Placenta Linked to Increased Postcesarean Hemorrhage Risk
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
SAN DIEGO – Three of the main risk factors for severe hemorrhage following a cesarean are abnormal placenta, uterine rupture or incision extension, and labor prior to cesarean, results from a large single-center study demonstrated.
For the study, Steven Kyle Thompson, D.O., and his associates at the University of Kansas, Wichita, reviewed the medical records of 3,677 cesarean deliveries performed at Wesley Medical Center, a large hospital in Wichita affiliated with the university, from Jan. 1, 2009 through Oct. 31, 2010. Hemorrhage was defined as having at least 1,000 mL of estimated blood loss (EBL) after the procedure.
Hemorrhage occurred in 303 of the deliveries (8.2%), and there were no maternal or fetal deaths. The researchers observed that the median EBL was greater in cases that involved administration of misoprostol, methylergonovine, or carboprost tromethamine vs. nothing (1,400 mL vs. 1,200 mL, P less than .001), as well as with the use of a Bakri balloon, B-Lynch suture, or cesarean hysterectomy vs. nothing (3,000 mL vs. 1,200 mL, P less .001). Median EBL also was greater in cases that required blood transfusion (2,500 mL vs. 1,200 mL, P less .001) and use of an intensive care unit (2,000 mL vs. 1,200 mL, P less .001).
Dr. Thompson and his associates also observed that a hemoglobin decrease by at least 30% of the preoperative value was significantly associated with abnormal placenta (odds ratio [OR], 5.38), uterine rupture or incision extension (OR, 2.81), labor prior to cesarean (OR, 2.78), and EBL of at least 1,500 mL (OR, 2.44).
Adjusted independent risk factors that were significantly associated with a postoperative decrease in hemoglobin below 7 g/dL were abnormal placenta (OR, 5.50), delivery between 2 a.m. and 7 a.m. (OR, 4.85), preoperative hemoglobin less than 11 g/dL (OR, 4.03), labor before cesarean (OR, 2.61), and EBL of at least 1,500 mL (OR, 2.31), they reported in a poster session at the annual meeting of the American College of Obstetricians and Gynecologists.
"Plan ahead of time if you have an individual who falls into a high-risk category," Dr. Thompson, a fourth-year ob.gyn. resident at the university, advised in an interview.
The researchers are currently replicating the study for vaginal deliveries.
Dr. Thompson said that he had no relevant financial conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: A hemoglobin decrease of at least 30% from the preoperative value was significantly associated with abnormal placenta (OR, 5.38), incision extension or uterine rupture (OR, 2.81), and labor (OR, 2.78).
Data Source: This review involved 3,677 cesarean deliveries performed at a large hospital between Jan. 1, 2009 and Oct. 31, 2010.
Disclosures: Dr. Thompson said that he had no relevant financial conflicts to disclose.
New Staples Add to Options for Cesarean Section
SAN DIEGO – Of 500 consecutive cesarean deliveries closed with subcuticular absorbable staples, only one hematoma occurred, and the overall surgical site infection rate was 1.2%, according to study findings.
"This study was surprising," lead investigator Dr. Kirk A. Shibley said in an interview before a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "I anticipated a low infection rate due to the interrupted and subcuticular nature of the technology, but I did not anticipate that the number of other wound complications would be so low. That is to say that the number of wound hematomas and seromas and separations is almost nonexistent."
Dr. Shibley, who practices obstetrics and gynecology in Edina, Minn., and his associates evaluated data from 500 consecutive cesarean procedures closed with Incisive Surgical’s INSORB absorbable staples. All the operations were performed by five clinicians in a single obstetrics practice during a 4-year period that ended in 2008. The investigators obtained the data from clinic medical records and from 30-day postdischarge infection surveillance programs at two community hospitals.
Dr. Shibley reported that there were only six surgical site infections, for a rate of 1.2%. There was one hematoma, no seromas, and no wound disruptions. In follow-up visits, he said, patients expressed a high level of satisfaction with the results. "The take-home message is that this skin closure technology is fast, and provides low-maintenance, cosmetic wounds with a very low infection and complication rate," he said.
In the poster, Dr. Shibley and his associates postulated that the improved outcomes may be due in part to the fact that the INSORB staples are made of a benign copolymer "of predominately polylactic acid, shown to elicit a very low inflammatory response in animal and human clinical studies, and may account for decreased pain, serous exudate, and other associated complications."
Also, they continued, "absorbable staples are placed entirely within the dermis without the percutaneous insult of metal staples. Absorbable staples avoid the associated patient discomfort and anxiety associated with metal staple removal. The absorbable staples precisely and effectively secure the dermis without tissue strangulation or compression that can occur with ... metal staples."
Dr. Shibley acknowledged that the study is limited as patients were not prospectively randomized to different closure types.
Dr. Shibley disclosed that he is a paid consultant to Incisive Surgical.
SAN DIEGO – Of 500 consecutive cesarean deliveries closed with subcuticular absorbable staples, only one hematoma occurred, and the overall surgical site infection rate was 1.2%, according to study findings.
"This study was surprising," lead investigator Dr. Kirk A. Shibley said in an interview before a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "I anticipated a low infection rate due to the interrupted and subcuticular nature of the technology, but I did not anticipate that the number of other wound complications would be so low. That is to say that the number of wound hematomas and seromas and separations is almost nonexistent."
Dr. Shibley, who practices obstetrics and gynecology in Edina, Minn., and his associates evaluated data from 500 consecutive cesarean procedures closed with Incisive Surgical’s INSORB absorbable staples. All the operations were performed by five clinicians in a single obstetrics practice during a 4-year period that ended in 2008. The investigators obtained the data from clinic medical records and from 30-day postdischarge infection surveillance programs at two community hospitals.
Dr. Shibley reported that there were only six surgical site infections, for a rate of 1.2%. There was one hematoma, no seromas, and no wound disruptions. In follow-up visits, he said, patients expressed a high level of satisfaction with the results. "The take-home message is that this skin closure technology is fast, and provides low-maintenance, cosmetic wounds with a very low infection and complication rate," he said.
In the poster, Dr. Shibley and his associates postulated that the improved outcomes may be due in part to the fact that the INSORB staples are made of a benign copolymer "of predominately polylactic acid, shown to elicit a very low inflammatory response in animal and human clinical studies, and may account for decreased pain, serous exudate, and other associated complications."
Also, they continued, "absorbable staples are placed entirely within the dermis without the percutaneous insult of metal staples. Absorbable staples avoid the associated patient discomfort and anxiety associated with metal staple removal. The absorbable staples precisely and effectively secure the dermis without tissue strangulation or compression that can occur with ... metal staples."
Dr. Shibley acknowledged that the study is limited as patients were not prospectively randomized to different closure types.
Dr. Shibley disclosed that he is a paid consultant to Incisive Surgical.
SAN DIEGO – Of 500 consecutive cesarean deliveries closed with subcuticular absorbable staples, only one hematoma occurred, and the overall surgical site infection rate was 1.2%, according to study findings.
"This study was surprising," lead investigator Dr. Kirk A. Shibley said in an interview before a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "I anticipated a low infection rate due to the interrupted and subcuticular nature of the technology, but I did not anticipate that the number of other wound complications would be so low. That is to say that the number of wound hematomas and seromas and separations is almost nonexistent."
Dr. Shibley, who practices obstetrics and gynecology in Edina, Minn., and his associates evaluated data from 500 consecutive cesarean procedures closed with Incisive Surgical’s INSORB absorbable staples. All the operations were performed by five clinicians in a single obstetrics practice during a 4-year period that ended in 2008. The investigators obtained the data from clinic medical records and from 30-day postdischarge infection surveillance programs at two community hospitals.
Dr. Shibley reported that there were only six surgical site infections, for a rate of 1.2%. There was one hematoma, no seromas, and no wound disruptions. In follow-up visits, he said, patients expressed a high level of satisfaction with the results. "The take-home message is that this skin closure technology is fast, and provides low-maintenance, cosmetic wounds with a very low infection and complication rate," he said.
In the poster, Dr. Shibley and his associates postulated that the improved outcomes may be due in part to the fact that the INSORB staples are made of a benign copolymer "of predominately polylactic acid, shown to elicit a very low inflammatory response in animal and human clinical studies, and may account for decreased pain, serous exudate, and other associated complications."
Also, they continued, "absorbable staples are placed entirely within the dermis without the percutaneous insult of metal staples. Absorbable staples avoid the associated patient discomfort and anxiety associated with metal staple removal. The absorbable staples precisely and effectively secure the dermis without tissue strangulation or compression that can occur with ... metal staples."
Dr. Shibley acknowledged that the study is limited as patients were not prospectively randomized to different closure types.
Dr. Shibley disclosed that he is a paid consultant to Incisive Surgical.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Investigational Contraceptive Patch Shows Promise
SAN DIEGO – Women who were randomized to an investigative low-dose ethinyl estradiol and levonorgestrel contraceptive patch had similar contraceptive efficacy, cycle control, and safety results, compared with those who were randomized to a standard oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel, results from a phase III trial demonstrated.
In addition, efficacy of the once-weekly patch, developed by Princeton, N.J.–based Agile Therapeutics and known as AG200-15, was comparable among obese and nonobese women, a finding that surprised investigators, who were led by Dr. Andrew M. Kaunitz, professor of the department of obstetrics and gynecology at the University of Florida, Jacksonville.
"There has been controversy and concern over the past decade that obese women might experience higher failure rates with some hormonal contraceptive methods, particularly transdermal contraception," Dr. Kaunitz said in an interview in advance of a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "We found that efficacy was comparable regardless of body mass index. That was an unexpected, but welcome, finding."
Pharmacokinetic studies of AG200-15 have shown that it delivers ethinyl estradiol (EE) and levonorgestrel equivalent to that seen with a 30-mg dose of EE and a 120-mg dose of levonorgestrel oral contraceptives. This is in contrast to Ortho Evra (norelgestromin/ethinyl estradiol transdermal system, Ortho-McNeil–Janssen Pharmaceuticals), the first-generation contraceptive patch that gained popularity upon release, but was found to deliver a dose of EE substantially higher than conventional oral contraceptives.
"At the same time, some well-publicized cases of vascular events, including fatal pulmonary emboli, occurred in women using the Ortho Evra patch," Dr. Kaunitz said. "These cases generated a fair amount of medical-legal attention. Ortho Evra went through this boom/bust phenomenon, where it was wildly popular, and now I think I only have one patient who is using it. I think it points out that if there were a lower-[dose] estrogen patch that provided effective contraception, but did not expose women to more estrogen than with current low-dose birth control pills, it could occupy an important contraceptive niche for U.S. women."
For the current study, which was conducted at 96 centers, 1,128 women were treated for 1 year (13 cycles) with AG200-15, and 375 were treated for six cycles with oral contraceptives followed by seven cycles of AG200-15. Blood draws were performed at cycles 2, 6, and 13, and complete physical and gynecologic exams were performed at baseline, cycle 7, and the final visit, which was 14 days after the removal of the last patch or intake of the last oral contraceptive.
The mean age of the study participants was 26 years, 55% were white/non-Hispanic, and their mean body mass index was 27.5 kg/m2. More than half (60%) were new users of hormonal contraceptives; 14% switched from another contraceptive prior to the study.
Dr. Kaunitz reported that there were no clinically meaningful differences in contraceptive efficacy among the intent-to-treat population between the oral contraceptive group and the AG200-15 group (a Pearl Index [PI] of 4.02 vs. 4.92). When the PI was stratified by BMI for the intent-to-treat population in the AG200-15 group, the PI for obese patients (defined as a BMI of 32 kg/m2 or greater) was similar to that of the nonobese patients (PI of 2.85 vs. 3.17).
When the researchers stratified the study participants by race/ethnicity, the PI for the AG200-15 and oral contraceptive groups was lowest in the white subgroup, followed by the Hispanic and the black subgroups. This likely reflects that women of lower socioeconomic status take oral contraceptives less consistently than other women, Dr. Kaunitz said, a phenomenon that has been observed by other investigators (Contraception 2012;85:465-9).
Cycle control was similar between the two treatment groups. In cycle 3, for example, the incidence of breakthrough bleeding and/or spotting episodes was 24.8% in the AG200-15 group, compared with 23.2% in the oral contraceptive group. In cycle 5, the incidence of these events was 22.3% and 21.9.
Nearly half of women (48%) chose to apply AG200-15 to their buttocks, while 40% chose the abdomen, and 12% chose the upper torso. "We found that there was good adhesiveness, as fewer than 3% of women experienced patch detachment," Dr. Kaunitz said. "Also, there was no suggestion that patches would come off with a lot of sweating or vigorous physical activity."
Overall, 80% of women reported no skin irritation. Only 0.1% of women reported severe irritation; 17%, mild skin irritation; and 2%-3%, moderate skin irritation.
The incidence of hormone-related adverse events was similar between the two groups: 1.3% in the AG200-15 group vs. 1.2% in the oral contraceptive group. Breast tenderness was uncommon, reported by fewer than 2% of women in both groups. "That was a reassuring safety signal," Dr. Kaunitz said.
The investigators reported one serious adverse event in the oral contraceptive group (one case with an unspecified liver problem) and three adverse events in the AG200-15 group (one case with a blood clot in the left subclavian vein, one case of uncontrollable nausea and vomiting, and one case of drug overdose with Benadryl) to be possibly or probably related to the study drug.
Going forward, Dr. Kaunitz said that he would like to see clinical trials of AG200-15 that involve shorter hormone intervals than the classic schedule of 21 active tablets followed by 7 hormone-free days as followed in this study. "Newer contraceptives tend to have shorter hormone-free intervals or be continuous," he said. "Going forward, I’d be interested in clinical trials of this patch using hormone-free intervals shorter than 7 days or cycles longer than 1 month."
Agile Therapeutics has submitted a New Drug Application for AG200-15 with the Food and Drug Administration.
The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
SAN DIEGO – Women who were randomized to an investigative low-dose ethinyl estradiol and levonorgestrel contraceptive patch had similar contraceptive efficacy, cycle control, and safety results, compared with those who were randomized to a standard oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel, results from a phase III trial demonstrated.
In addition, efficacy of the once-weekly patch, developed by Princeton, N.J.–based Agile Therapeutics and known as AG200-15, was comparable among obese and nonobese women, a finding that surprised investigators, who were led by Dr. Andrew M. Kaunitz, professor of the department of obstetrics and gynecology at the University of Florida, Jacksonville.
"There has been controversy and concern over the past decade that obese women might experience higher failure rates with some hormonal contraceptive methods, particularly transdermal contraception," Dr. Kaunitz said in an interview in advance of a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "We found that efficacy was comparable regardless of body mass index. That was an unexpected, but welcome, finding."
Pharmacokinetic studies of AG200-15 have shown that it delivers ethinyl estradiol (EE) and levonorgestrel equivalent to that seen with a 30-mg dose of EE and a 120-mg dose of levonorgestrel oral contraceptives. This is in contrast to Ortho Evra (norelgestromin/ethinyl estradiol transdermal system, Ortho-McNeil–Janssen Pharmaceuticals), the first-generation contraceptive patch that gained popularity upon release, but was found to deliver a dose of EE substantially higher than conventional oral contraceptives.
"At the same time, some well-publicized cases of vascular events, including fatal pulmonary emboli, occurred in women using the Ortho Evra patch," Dr. Kaunitz said. "These cases generated a fair amount of medical-legal attention. Ortho Evra went through this boom/bust phenomenon, where it was wildly popular, and now I think I only have one patient who is using it. I think it points out that if there were a lower-[dose] estrogen patch that provided effective contraception, but did not expose women to more estrogen than with current low-dose birth control pills, it could occupy an important contraceptive niche for U.S. women."
For the current study, which was conducted at 96 centers, 1,128 women were treated for 1 year (13 cycles) with AG200-15, and 375 were treated for six cycles with oral contraceptives followed by seven cycles of AG200-15. Blood draws were performed at cycles 2, 6, and 13, and complete physical and gynecologic exams were performed at baseline, cycle 7, and the final visit, which was 14 days after the removal of the last patch or intake of the last oral contraceptive.
The mean age of the study participants was 26 years, 55% were white/non-Hispanic, and their mean body mass index was 27.5 kg/m2. More than half (60%) were new users of hormonal contraceptives; 14% switched from another contraceptive prior to the study.
Dr. Kaunitz reported that there were no clinically meaningful differences in contraceptive efficacy among the intent-to-treat population between the oral contraceptive group and the AG200-15 group (a Pearl Index [PI] of 4.02 vs. 4.92). When the PI was stratified by BMI for the intent-to-treat population in the AG200-15 group, the PI for obese patients (defined as a BMI of 32 kg/m2 or greater) was similar to that of the nonobese patients (PI of 2.85 vs. 3.17).
When the researchers stratified the study participants by race/ethnicity, the PI for the AG200-15 and oral contraceptive groups was lowest in the white subgroup, followed by the Hispanic and the black subgroups. This likely reflects that women of lower socioeconomic status take oral contraceptives less consistently than other women, Dr. Kaunitz said, a phenomenon that has been observed by other investigators (Contraception 2012;85:465-9).
Cycle control was similar between the two treatment groups. In cycle 3, for example, the incidence of breakthrough bleeding and/or spotting episodes was 24.8% in the AG200-15 group, compared with 23.2% in the oral contraceptive group. In cycle 5, the incidence of these events was 22.3% and 21.9.
Nearly half of women (48%) chose to apply AG200-15 to their buttocks, while 40% chose the abdomen, and 12% chose the upper torso. "We found that there was good adhesiveness, as fewer than 3% of women experienced patch detachment," Dr. Kaunitz said. "Also, there was no suggestion that patches would come off with a lot of sweating or vigorous physical activity."
Overall, 80% of women reported no skin irritation. Only 0.1% of women reported severe irritation; 17%, mild skin irritation; and 2%-3%, moderate skin irritation.
The incidence of hormone-related adverse events was similar between the two groups: 1.3% in the AG200-15 group vs. 1.2% in the oral contraceptive group. Breast tenderness was uncommon, reported by fewer than 2% of women in both groups. "That was a reassuring safety signal," Dr. Kaunitz said.
The investigators reported one serious adverse event in the oral contraceptive group (one case with an unspecified liver problem) and three adverse events in the AG200-15 group (one case with a blood clot in the left subclavian vein, one case of uncontrollable nausea and vomiting, and one case of drug overdose with Benadryl) to be possibly or probably related to the study drug.
Going forward, Dr. Kaunitz said that he would like to see clinical trials of AG200-15 that involve shorter hormone intervals than the classic schedule of 21 active tablets followed by 7 hormone-free days as followed in this study. "Newer contraceptives tend to have shorter hormone-free intervals or be continuous," he said. "Going forward, I’d be interested in clinical trials of this patch using hormone-free intervals shorter than 7 days or cycles longer than 1 month."
Agile Therapeutics has submitted a New Drug Application for AG200-15 with the Food and Drug Administration.
The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
SAN DIEGO – Women who were randomized to an investigative low-dose ethinyl estradiol and levonorgestrel contraceptive patch had similar contraceptive efficacy, cycle control, and safety results, compared with those who were randomized to a standard oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel, results from a phase III trial demonstrated.
In addition, efficacy of the once-weekly patch, developed by Princeton, N.J.–based Agile Therapeutics and known as AG200-15, was comparable among obese and nonobese women, a finding that surprised investigators, who were led by Dr. Andrew M. Kaunitz, professor of the department of obstetrics and gynecology at the University of Florida, Jacksonville.
"There has been controversy and concern over the past decade that obese women might experience higher failure rates with some hormonal contraceptive methods, particularly transdermal contraception," Dr. Kaunitz said in an interview in advance of a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "We found that efficacy was comparable regardless of body mass index. That was an unexpected, but welcome, finding."
Pharmacokinetic studies of AG200-15 have shown that it delivers ethinyl estradiol (EE) and levonorgestrel equivalent to that seen with a 30-mg dose of EE and a 120-mg dose of levonorgestrel oral contraceptives. This is in contrast to Ortho Evra (norelgestromin/ethinyl estradiol transdermal system, Ortho-McNeil–Janssen Pharmaceuticals), the first-generation contraceptive patch that gained popularity upon release, but was found to deliver a dose of EE substantially higher than conventional oral contraceptives.
"At the same time, some well-publicized cases of vascular events, including fatal pulmonary emboli, occurred in women using the Ortho Evra patch," Dr. Kaunitz said. "These cases generated a fair amount of medical-legal attention. Ortho Evra went through this boom/bust phenomenon, where it was wildly popular, and now I think I only have one patient who is using it. I think it points out that if there were a lower-[dose] estrogen patch that provided effective contraception, but did not expose women to more estrogen than with current low-dose birth control pills, it could occupy an important contraceptive niche for U.S. women."
For the current study, which was conducted at 96 centers, 1,128 women were treated for 1 year (13 cycles) with AG200-15, and 375 were treated for six cycles with oral contraceptives followed by seven cycles of AG200-15. Blood draws were performed at cycles 2, 6, and 13, and complete physical and gynecologic exams were performed at baseline, cycle 7, and the final visit, which was 14 days after the removal of the last patch or intake of the last oral contraceptive.
The mean age of the study participants was 26 years, 55% were white/non-Hispanic, and their mean body mass index was 27.5 kg/m2. More than half (60%) were new users of hormonal contraceptives; 14% switched from another contraceptive prior to the study.
Dr. Kaunitz reported that there were no clinically meaningful differences in contraceptive efficacy among the intent-to-treat population between the oral contraceptive group and the AG200-15 group (a Pearl Index [PI] of 4.02 vs. 4.92). When the PI was stratified by BMI for the intent-to-treat population in the AG200-15 group, the PI for obese patients (defined as a BMI of 32 kg/m2 or greater) was similar to that of the nonobese patients (PI of 2.85 vs. 3.17).
When the researchers stratified the study participants by race/ethnicity, the PI for the AG200-15 and oral contraceptive groups was lowest in the white subgroup, followed by the Hispanic and the black subgroups. This likely reflects that women of lower socioeconomic status take oral contraceptives less consistently than other women, Dr. Kaunitz said, a phenomenon that has been observed by other investigators (Contraception 2012;85:465-9).
Cycle control was similar between the two treatment groups. In cycle 3, for example, the incidence of breakthrough bleeding and/or spotting episodes was 24.8% in the AG200-15 group, compared with 23.2% in the oral contraceptive group. In cycle 5, the incidence of these events was 22.3% and 21.9.
Nearly half of women (48%) chose to apply AG200-15 to their buttocks, while 40% chose the abdomen, and 12% chose the upper torso. "We found that there was good adhesiveness, as fewer than 3% of women experienced patch detachment," Dr. Kaunitz said. "Also, there was no suggestion that patches would come off with a lot of sweating or vigorous physical activity."
Overall, 80% of women reported no skin irritation. Only 0.1% of women reported severe irritation; 17%, mild skin irritation; and 2%-3%, moderate skin irritation.
The incidence of hormone-related adverse events was similar between the two groups: 1.3% in the AG200-15 group vs. 1.2% in the oral contraceptive group. Breast tenderness was uncommon, reported by fewer than 2% of women in both groups. "That was a reassuring safety signal," Dr. Kaunitz said.
The investigators reported one serious adverse event in the oral contraceptive group (one case with an unspecified liver problem) and three adverse events in the AG200-15 group (one case with a blood clot in the left subclavian vein, one case of uncontrollable nausea and vomiting, and one case of drug overdose with Benadryl) to be possibly or probably related to the study drug.
Going forward, Dr. Kaunitz said that he would like to see clinical trials of AG200-15 that involve shorter hormone intervals than the classic schedule of 21 active tablets followed by 7 hormone-free days as followed in this study. "Newer contraceptives tend to have shorter hormone-free intervals or be continuous," he said. "Going forward, I’d be interested in clinical trials of this patch using hormone-free intervals shorter than 7 days or cycles longer than 1 month."
Agile Therapeutics has submitted a New Drug Application for AG200-15 with the Food and Drug Administration.
The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: No clinically meaningful differences in contraceptive efficacy were observed between women who used an oral contraceptive and those who used a transdermal contraceptive patch (a Pearl Index of 4.02 vs. 4.92).
Data Source: A phase III, year-long study of 1,503 women who were randomized to receive either an oral contraceptive containing 20 mg ethinyl estradiol and 0.1 mg levonorgestrel or a once-weekly transdermal patch containing a 30-mg dose of ethinyl estradiol and a 120-mg dose of levonorgestrel.
Disclosures: The study was funded by Agile Therapeutics. Dr. Kaunitz disclosed that he is a consultant for the company.
Maternal Age, Obesity Associated With Adverse Pregnancy Outcomes
SAN DIEGO – Although women who delay pregnancy to age 40 years and older face an increased risk for adverse outcomes, reducing prepregnancy body mass index may reduce their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery, results from a large study demonstrated.
"This is an important issue in the United States as more than 13% of pregnant women are now age 35 and older, and nearly 3% are age 40 and older at delivery," Dr. John R. Barton said in an interview prior to a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "These data underscore the impact of obesity on increasing adverse outcomes in otherwise healthy women."
To examine pregnancy outcomes of healthy nulliparous women aged 40 years or older at delivery, Dr. Barton, director of maternal-fetal medicine at Central Baptist Hospital, Lexington, Ky., and his associates evaluated 53,480 women who were voluntarily enrolled in a pregnancy risk assessment and education program operated by Alere Health between July 1, 2006, and Aug. 1, 2011.
The researchers excluded women who reported heart disease, chronic hypertension, pregestational diabetes, other medical disorders, tobacco use, and conception with assistive reproductive technology. Data were grouped by maternal age (20-29 years or 40 and older) and obesity. Those with a prepregnancy body mass index (PPBMI) of 30 kg/m2 or higher were defined as obese; those with lower BMIs were defined a nonobese.
Within each PPBMI group, nulliparous women 40 years of age and older delivered at a significantly lower gestational age, had a greater incidence of cesarean delivery, gestational diabetes, preterm birth, and both low and very-low birth weight infants, compared with controls aged 20-29 years. In addition, obesity was associated with higher rates of adverse pregnancy outcomes in the group of women aged 40 years and older.
"Throughout the reproductive years, health care providers to women should support and encourage them to maintain a healthy lifestyle and a healthy body habitus," Dr. Barton advised. "In healthy nulliparous women, both advanced maternal age and obesity influence pregnancy outcomes. Women choosing to delay pregnancy until age 40 years and older may modify their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery by reducing their body mass index to nonobese levels prior to conception."
Dr. Barton acknowledged certain limitations of the study, including the fact that while the population included both Medicaid and commercially insured women from across the United States, "we do not know for sure if the same results would be observed in the general population or for those with later prenatal care initiation. It is also important to stress that these women were healthy in that they did not have heart disease, chronic hypertension, diabetes, or other medical disorders such as kidney disease or autoimmune disorders. We also did not include women that reported smoking during pregnancy. The overall rate of obesity was 17.7%, which is not comparable with the general obstetrical population (about 35%) – yet reflects our inclusion/exclusion criteria."
Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
SAN DIEGO – Although women who delay pregnancy to age 40 years and older face an increased risk for adverse outcomes, reducing prepregnancy body mass index may reduce their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery, results from a large study demonstrated.
"This is an important issue in the United States as more than 13% of pregnant women are now age 35 and older, and nearly 3% are age 40 and older at delivery," Dr. John R. Barton said in an interview prior to a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "These data underscore the impact of obesity on increasing adverse outcomes in otherwise healthy women."
To examine pregnancy outcomes of healthy nulliparous women aged 40 years or older at delivery, Dr. Barton, director of maternal-fetal medicine at Central Baptist Hospital, Lexington, Ky., and his associates evaluated 53,480 women who were voluntarily enrolled in a pregnancy risk assessment and education program operated by Alere Health between July 1, 2006, and Aug. 1, 2011.
The researchers excluded women who reported heart disease, chronic hypertension, pregestational diabetes, other medical disorders, tobacco use, and conception with assistive reproductive technology. Data were grouped by maternal age (20-29 years or 40 and older) and obesity. Those with a prepregnancy body mass index (PPBMI) of 30 kg/m2 or higher were defined as obese; those with lower BMIs were defined a nonobese.
Within each PPBMI group, nulliparous women 40 years of age and older delivered at a significantly lower gestational age, had a greater incidence of cesarean delivery, gestational diabetes, preterm birth, and both low and very-low birth weight infants, compared with controls aged 20-29 years. In addition, obesity was associated with higher rates of adverse pregnancy outcomes in the group of women aged 40 years and older.
"Throughout the reproductive years, health care providers to women should support and encourage them to maintain a healthy lifestyle and a healthy body habitus," Dr. Barton advised. "In healthy nulliparous women, both advanced maternal age and obesity influence pregnancy outcomes. Women choosing to delay pregnancy until age 40 years and older may modify their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery by reducing their body mass index to nonobese levels prior to conception."
Dr. Barton acknowledged certain limitations of the study, including the fact that while the population included both Medicaid and commercially insured women from across the United States, "we do not know for sure if the same results would be observed in the general population or for those with later prenatal care initiation. It is also important to stress that these women were healthy in that they did not have heart disease, chronic hypertension, diabetes, or other medical disorders such as kidney disease or autoimmune disorders. We also did not include women that reported smoking during pregnancy. The overall rate of obesity was 17.7%, which is not comparable with the general obstetrical population (about 35%) – yet reflects our inclusion/exclusion criteria."
Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
SAN DIEGO – Although women who delay pregnancy to age 40 years and older face an increased risk for adverse outcomes, reducing prepregnancy body mass index may reduce their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery, results from a large study demonstrated.
"This is an important issue in the United States as more than 13% of pregnant women are now age 35 and older, and nearly 3% are age 40 and older at delivery," Dr. John R. Barton said in an interview prior to a poster session at the annual meeting of the American College of Obstetricians and Gynecologists. "These data underscore the impact of obesity on increasing adverse outcomes in otherwise healthy women."
To examine pregnancy outcomes of healthy nulliparous women aged 40 years or older at delivery, Dr. Barton, director of maternal-fetal medicine at Central Baptist Hospital, Lexington, Ky., and his associates evaluated 53,480 women who were voluntarily enrolled in a pregnancy risk assessment and education program operated by Alere Health between July 1, 2006, and Aug. 1, 2011.
The researchers excluded women who reported heart disease, chronic hypertension, pregestational diabetes, other medical disorders, tobacco use, and conception with assistive reproductive technology. Data were grouped by maternal age (20-29 years or 40 and older) and obesity. Those with a prepregnancy body mass index (PPBMI) of 30 kg/m2 or higher were defined as obese; those with lower BMIs were defined a nonobese.
Within each PPBMI group, nulliparous women 40 years of age and older delivered at a significantly lower gestational age, had a greater incidence of cesarean delivery, gestational diabetes, preterm birth, and both low and very-low birth weight infants, compared with controls aged 20-29 years. In addition, obesity was associated with higher rates of adverse pregnancy outcomes in the group of women aged 40 years and older.
"Throughout the reproductive years, health care providers to women should support and encourage them to maintain a healthy lifestyle and a healthy body habitus," Dr. Barton advised. "In healthy nulliparous women, both advanced maternal age and obesity influence pregnancy outcomes. Women choosing to delay pregnancy until age 40 years and older may modify their risk for cesarean delivery, gestational diabetes, gestational hypertension/preeclampsia, and preterm delivery by reducing their body mass index to nonobese levels prior to conception."
Dr. Barton acknowledged certain limitations of the study, including the fact that while the population included both Medicaid and commercially insured women from across the United States, "we do not know for sure if the same results would be observed in the general population or for those with later prenatal care initiation. It is also important to stress that these women were healthy in that they did not have heart disease, chronic hypertension, diabetes, or other medical disorders such as kidney disease or autoimmune disorders. We also did not include women that reported smoking during pregnancy. The overall rate of obesity was 17.7%, which is not comparable with the general obstetrical population (about 35%) – yet reflects our inclusion/exclusion criteria."
Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.
FROM THE ANNUAL MEETING OF THE AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS
Major Finding: A significantly higher proportion of obese women aged 40 years or older underwent primary cesarean delivery, compared with obese women aged 20-29 years (69.3% vs. 47%, respectively). A similar age-related association was observed among nonobese women (55.4% vs. 28.2%).
Data Source: Data were from a study of 53,480 nulliparous women aged either 20-29 years or 40 years and older who were voluntarily enrolled in a pregnancy risk assessment and education program.
Disclosures: Dr. Barton disclosed that he has received research support from Alere San Diego, a subsidiary of Alere Health. Another study investigator, Dr. Baha M. Sibai, is a consultant for Alere San Diego.