User login
Bariatric Surgery Risk Scoring Tool May Predict Serious Complications
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
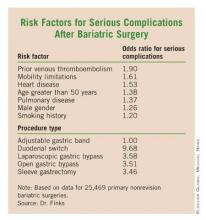
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
BOCA RATON, FLA. – A newly developed risk scoring system for predicting serious complications following bariatric surgery should help surgeons in selecting the best procedure for a given patient.
The population-based risk prediction tool was developed by analyzing all bariatric surgeries performed in the state of Michigan during a recent 4.5-year period. The data came from a comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative, a consortium of hospitals and surgeons.
The 30-day serious complication rate in 25,469 primary nonrevision bariatric surgeries performed in June 2006 through December 2010 was 2.5%, with a 0.1% mortality rate, Dr. Jonathan F. Finks reported at the annual meeting of the American Surgical Association.
Serious complications were defined as those that were life-threatening or associated with lasting disability. Examples included abdominal abscess requiring percutaneous drainage, bowel obstruction necessitating reoperation, bleeding requiring more than 4 units of blood products, respiratory failure, venous thromboembolism, MI, renal failure requiring dialysis, anastomotic leak requiring reoperation or percutaneous drainage, and gastric band complications warranting reoperation, explained Dr. Finks of the University of Michigan, Ann Arbor.
Laparoscopic gastric bypass accounted for 54% of the bariatric procedures, adjustable gastric band 31%, sleeve gastrectomy 9%, open gastric bypass 4%, and duodenal switch 1%. Patients undergoing the various procedures were similar in terms of most baseline variables, with the notable exception that those who underwent open gastric bypass surgery had the highest mean body mass index, at 54 kg/m2, and the highest mean number of comorbid conditions, including heart and lung disease as well as a history of venous thromboembolism.
Multivariate analysis identified seven independent patient-related risk factors and one procedure-related predictor for serious complications within 30 days following bariatric surgery. Patients with two or fewer risk factors had a 1.9% serious complication rate, those with any three to five risk factors had a 3.8% rate, and those with six to eight risk factors had a 7.6% complication rate.
The adjusted C statistic for the risk-scoring system was 0.66, indicative of a moderate level of discrimination, according to Dr. Finks.
He and his colleagues are refining their scoring system and anticipate soon putting out an online risk calculation tool that will be available to surgeons anywhere. It will be found at www.michiganbsc.org.
The investigators anticipate that, in addition to its usefulness in matching individual patients to the best procedure based upon their level of risk for serious complications, the risk scoring tool will be of value in offering institutional and provider benchmarks, facilitating informed consent, and promoting evidence-based insurance coverage guidelines.
Another benefit of the prediction tool is that it will identify patients who have certain risk factors that can be modified perioperatively – for example, prescribing aggressive prophylaxis for patients at high risk for venous thromboembolism and scheduling preoperative physical or occupational therapy for those with mobility limitations, he continued.
Discussant Dr. R. Armour Forse, noting that many patients and primary care physicians have avoided bariatric surgery because of safety concerns, said this study provides accurate and reassuring information based upon a large database.
Of interest, the C statistic in the Michigan study is virtually identical to that associated with a different risk prediction tool developed using National Surgical Quality Improvement Program data in a recent study for which Dr. Forse was senior coauthor (J. Am. Coll. Surg. 2011;212:301-9). Why is it that these two models don’t have greater predictive power? asked Dr. Forse, professor and chairman of the department of surgery at Creighton University, Omaha, Neb.
Dr. Finks replied that bariatric surgery patients are a fairly homogeneous group; it’s elective surgery, and the highest-risk patients simply don’t undergo the procedure. Also, these models focus heavily on patient risk factors, and there are other variables not included in the risk models that contribute importantly to outcome, including provider volume and the surgical techniques employed, he added.
Dr. Henry Buchwald, professor of surgery and biomedical engineering at the University of Minnesota, Minneapolis, observed that the Michigan study makes a key point: "There are few operations that have anything approaching the low morbidity and mortality of bariatric surgery."
Dr. Finks declared having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: A population-based risk prediction tool helped surgeons select the best possible bariatric surgery procedure. Over four years, when the tool was applied, the 30-day serious complication rate in more than 25,000 procedures was 2.5% and the mortality rate was 0.1%.
Data Source: A comprehensive statewide prospective registry maintained by the Michigan Bariatric Surgery Collaborative.
Disclosures: Dr. Fink reported no disclosures.
NSQIP Found Highly Cost Effective for Participating Hospitals
BOCA RATON, FLA. – Hospitals that embrace the National Surgical Quality Improvement Program can expect to face significant expenses initially, but within a couple of years, the program becomes highly cost effective.
That’s been the experience at Pennsylvania State University’s Milton S. Hershey Medical Center, in Hershey, Pa., where the general and vascular surgery postoperative complication rate has dropped steadily as a consequence of NSQIP participation.
Indeed, by the time NSQIP had been in place for 2 years, the cost of avoiding one postop adverse event through NSQIP participation was roughly $9,000 less than the average cost of actually dealing with such a complication, Dr. Peter W. Dillon said at the annual meeting of the American Surgical Association.
"What it means for our institution is that at the end of year 2, treating the complication cost a lot more than paying NSQIP to avoid the complication. By the time we got to year 2, the program had a potential cost savings to the institution," explained Dr. Dillon, professor and chairman of the department of surgery at Hershey Medical Center.
There’s an important lesson here for surgeons and hospital officials elsewhere around the country. Today, only about 5% of U.S. acute care hospitals are on board with NSQIP. A major barrier to implementation is the program’s hefty direct costs. Those costs averaged more than $138,800 annually during the first 2 years of Hershey Medical Center’s participation, including licensing fees, administrative costs, travel for training, and information technology expertise. But after implementation, reduced surgical/medical errors result in substantial cost savings.
At Hershey, the postop adverse event rate fell from 17.1% at baseline to 13.8% after 1 year and to 12.7% after 2 years.
NSQIP was a challenge at the start. During the first 6 months of NSQIP involvement, the hospital was paying $25,471 per complication avoided. That’s a prohibitive cost, especially considering that it was substantially more than the $16,371 average cost of managing a real postop event.
By 2 years, however, the cost of avoiding one postop adverse event had fallen to $7,319, or $9,072 less than the cost attributed to an actual adverse event.
Discussant Dr. Sean J. Mulvihill commented that the Hershey study is important because the nation faces unsustainable escalation in the cost of medical care, and it’s incumbent on surgeons to find ways to increase the value of their services. Along those lines, compelling evidence exists to show that NSQIP reduces surgical morbidity and improves outcomes.
Dr. Mulvihill said he believes the Hershey group’s calculations are too conservative. The actual savings accrued through NSQIP involvement may be substantially greater.
For example, NSQIP can replace previous less-effective surgical quality improvement efforts. That saves institutional costs. Plus, as hospital administrators and department heads know all too well, the time will soon be at hand when hospitals will be punished financially for certain postop complications that are deemed by payers to be preventable. Hospitals will simply no longer receive payment for such events. Thus, preventing those complications from happening will yield additional financial value, explained Dr. Mulvihill, professor and chair of the department of surgery at the University of Utah, Salt Lake City.
"I predict the Hershey group will find additional added value with further passage of time. Our hospitals at University of Utah have been participating in NSQIP since 2001. It took us several years of maturation of the program before we hit our stride with serious quality improvement efforts coming directly from the program," the surgeon said.
The NSQIP program is a project of the American College of Surgeons. Dr. Dillon declared having no financial conflicts of interest.
BOCA RATON, FLA. – Hospitals that embrace the National Surgical Quality Improvement Program can expect to face significant expenses initially, but within a couple of years, the program becomes highly cost effective.
That’s been the experience at Pennsylvania State University’s Milton S. Hershey Medical Center, in Hershey, Pa., where the general and vascular surgery postoperative complication rate has dropped steadily as a consequence of NSQIP participation.
Indeed, by the time NSQIP had been in place for 2 years, the cost of avoiding one postop adverse event through NSQIP participation was roughly $9,000 less than the average cost of actually dealing with such a complication, Dr. Peter W. Dillon said at the annual meeting of the American Surgical Association.
"What it means for our institution is that at the end of year 2, treating the complication cost a lot more than paying NSQIP to avoid the complication. By the time we got to year 2, the program had a potential cost savings to the institution," explained Dr. Dillon, professor and chairman of the department of surgery at Hershey Medical Center.
There’s an important lesson here for surgeons and hospital officials elsewhere around the country. Today, only about 5% of U.S. acute care hospitals are on board with NSQIP. A major barrier to implementation is the program’s hefty direct costs. Those costs averaged more than $138,800 annually during the first 2 years of Hershey Medical Center’s participation, including licensing fees, administrative costs, travel for training, and information technology expertise. But after implementation, reduced surgical/medical errors result in substantial cost savings.
At Hershey, the postop adverse event rate fell from 17.1% at baseline to 13.8% after 1 year and to 12.7% after 2 years.
NSQIP was a challenge at the start. During the first 6 months of NSQIP involvement, the hospital was paying $25,471 per complication avoided. That’s a prohibitive cost, especially considering that it was substantially more than the $16,371 average cost of managing a real postop event.
By 2 years, however, the cost of avoiding one postop adverse event had fallen to $7,319, or $9,072 less than the cost attributed to an actual adverse event.
Discussant Dr. Sean J. Mulvihill commented that the Hershey study is important because the nation faces unsustainable escalation in the cost of medical care, and it’s incumbent on surgeons to find ways to increase the value of their services. Along those lines, compelling evidence exists to show that NSQIP reduces surgical morbidity and improves outcomes.
Dr. Mulvihill said he believes the Hershey group’s calculations are too conservative. The actual savings accrued through NSQIP involvement may be substantially greater.
For example, NSQIP can replace previous less-effective surgical quality improvement efforts. That saves institutional costs. Plus, as hospital administrators and department heads know all too well, the time will soon be at hand when hospitals will be punished financially for certain postop complications that are deemed by payers to be preventable. Hospitals will simply no longer receive payment for such events. Thus, preventing those complications from happening will yield additional financial value, explained Dr. Mulvihill, professor and chair of the department of surgery at the University of Utah, Salt Lake City.
"I predict the Hershey group will find additional added value with further passage of time. Our hospitals at University of Utah have been participating in NSQIP since 2001. It took us several years of maturation of the program before we hit our stride with serious quality improvement efforts coming directly from the program," the surgeon said.
The NSQIP program is a project of the American College of Surgeons. Dr. Dillon declared having no financial conflicts of interest.
BOCA RATON, FLA. – Hospitals that embrace the National Surgical Quality Improvement Program can expect to face significant expenses initially, but within a couple of years, the program becomes highly cost effective.
That’s been the experience at Pennsylvania State University’s Milton S. Hershey Medical Center, in Hershey, Pa., where the general and vascular surgery postoperative complication rate has dropped steadily as a consequence of NSQIP participation.
Indeed, by the time NSQIP had been in place for 2 years, the cost of avoiding one postop adverse event through NSQIP participation was roughly $9,000 less than the average cost of actually dealing with such a complication, Dr. Peter W. Dillon said at the annual meeting of the American Surgical Association.
"What it means for our institution is that at the end of year 2, treating the complication cost a lot more than paying NSQIP to avoid the complication. By the time we got to year 2, the program had a potential cost savings to the institution," explained Dr. Dillon, professor and chairman of the department of surgery at Hershey Medical Center.
There’s an important lesson here for surgeons and hospital officials elsewhere around the country. Today, only about 5% of U.S. acute care hospitals are on board with NSQIP. A major barrier to implementation is the program’s hefty direct costs. Those costs averaged more than $138,800 annually during the first 2 years of Hershey Medical Center’s participation, including licensing fees, administrative costs, travel for training, and information technology expertise. But after implementation, reduced surgical/medical errors result in substantial cost savings.
At Hershey, the postop adverse event rate fell from 17.1% at baseline to 13.8% after 1 year and to 12.7% after 2 years.
NSQIP was a challenge at the start. During the first 6 months of NSQIP involvement, the hospital was paying $25,471 per complication avoided. That’s a prohibitive cost, especially considering that it was substantially more than the $16,371 average cost of managing a real postop event.
By 2 years, however, the cost of avoiding one postop adverse event had fallen to $7,319, or $9,072 less than the cost attributed to an actual adverse event.
Discussant Dr. Sean J. Mulvihill commented that the Hershey study is important because the nation faces unsustainable escalation in the cost of medical care, and it’s incumbent on surgeons to find ways to increase the value of their services. Along those lines, compelling evidence exists to show that NSQIP reduces surgical morbidity and improves outcomes.
Dr. Mulvihill said he believes the Hershey group’s calculations are too conservative. The actual savings accrued through NSQIP involvement may be substantially greater.
For example, NSQIP can replace previous less-effective surgical quality improvement efforts. That saves institutional costs. Plus, as hospital administrators and department heads know all too well, the time will soon be at hand when hospitals will be punished financially for certain postop complications that are deemed by payers to be preventable. Hospitals will simply no longer receive payment for such events. Thus, preventing those complications from happening will yield additional financial value, explained Dr. Mulvihill, professor and chair of the department of surgery at the University of Utah, Salt Lake City.
"I predict the Hershey group will find additional added value with further passage of time. Our hospitals at University of Utah have been participating in NSQIP since 2001. It took us several years of maturation of the program before we hit our stride with serious quality improvement efforts coming directly from the program," the surgeon said.
The NSQIP program is a project of the American College of Surgeons. Dr. Dillon declared having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Simulator Tops Standard Training for Laparoscopic Hernia Repair
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
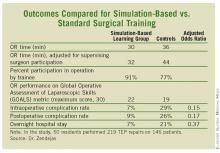
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: General surgery residents who learned laparoscopic totally extraperitoneal inguinal herniorrhaphy through a novel simulation-based training program significantly outperformed those trained in standard fashion.
Data Source: Randomized trial with 50 residents.
Disclosures: Dr. Zendejas reported having no financial conflicts.
Simulator Tops Standard Training for Laparoscopic Hernia Repair
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
BOCA RATON, FLA. – A novel simulation-based training curriculum in laparoscopic totally extraperitoneal inguinal herniorrhaphy for general surgery residents led to shorter operating times, better trainee performance, and fewer patient complications in a randomized clinical trial.
The training program has two elements: a cognitive component featuring Web-based PowerPoint presentations and videos along with assigned readings, and psychomotor training on a totally extraperitoneal inguinal herniorrhaphy (TEP) simulator, Dr. Benjamin Zendejas said at the annual meeting of the American Surgical Association.
A key feature is that the skills training – with one instructor per resident – is performed until mastery is attained, however long that takes. Only then does the resident start performing TEPs in the operating room under supervision, explained Dr. Zendejas of the Mayo Clinic, Rochester, Minn.
He presented a study in which 50 general surgery residents performed a baseline TEP in the operating room, and then were randomized to the simulation-based training program or standard training.
The simulator was the Limbs & Things Ltd.’s TEP Guildford MATTU Hernia Trainer. Mastery was defined by the average 2 minutes required for five experienced instructors to perform a TEP on the simulator. An average of roughly eight attempts was required for fifth-year residents to achieve mastery on the simulator, compared with 26 for first-year residents.
In the operating room, the 50 residents performed 219 TEP repairs on 146 patients. Each repair was evaluated immediately afterward by two independent raters. The simulation-based training group outperformed residents who were trained in the standard fashion in all outcome measures, including the key end point of operative time adjusted for the impact of supervising surgeon takeover for poorly performing trainees. (See box.)
Intraoperative complications, such as peritoneal tears and procedure conversions, occurred in 7% of procedures performed by simulation-trained residents, and in 29% of controls. Urinary retention, seroma, and other postoperative complications resulted from 9% of the simulation-trained residents’ operations, compared with 26% of those performed by residents trained in TEP in standard fashion. In all, 7% of procedures carried out by simulation-trained residents led to an overnight hospital stay, compared with 21% for controls.
"This will become a seminal paper in simulation-based training education," said discussant Dr. Gary L. Dunnington, who called the study "outstanding."
This work suggests that, on an hour-by-hour basis, training in a psychomotor skills laboratory may be more efficient for residents than time spent in the operating room. These data, "if further substantiated, will be of great value with the increasing constraints of decreasing duty hours," noted Dr. Dunnington, professor and chairman of the department of surgery at Southern Illinois University, Springfield.
He was impressed with the investigators’ documentation of improved clinically relevant patient outcomes in the operating room after simulation-based training – the first study to do so. He also liked the investigators’ use of video recordings rather than crude recall to facilitate the study of operative errors.
"This study sets a new bar for simulation researchers," he concluded.
Dr. Zendejas reported having no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: General surgery residents who learned laparoscopic totally extraperitoneal inguinal herniorrhaphy through a novel simulation-based training program significantly outperformed those trained in standard fashion.
Data Source: Randomized trial with 50 residents.
Disclosures: Dr. Zendejas reported having no financial conflicts.
Minimally Invasive Esophagectomy Leads to Low Mortality
BOCA RATON, FLA. — Minimally invasive esophagectomy has advanced to the point where it offers significant advantages over open esophagectomy in terms of operative morbidity and mortality, judging by results of a single-center review of 980 cases.
Published series indicate that the operative mortality of open esophagectomy is 8%-21%, although a very few high-volume medical centers have reported rates as low as 3%.
"There is a perception among patients and physicians that open esophagectomy is to be avoided at all costs because of it substantial morbidity," Dr. James D. Luketich said at the annual meeting of the American Surgical Association.
In his review of 980 consecutive, elective, nonurgent, minimally invasive esophagectomies, the 30-day mortality was just 1.8%. Median operative time was 6.7 hours, which dropped to 4 hours in cases that were not done by residents. The median ICU stay was 2.0 days, with a median hospital length of stay of 8 days. A median 21 lymph nodes were dissected, and 98% of cases had negative surgical margins.
"A less invasive surgical approach for esophageal cancer would improve the standard of care by reducing morbidity and shortening hospital stays and time to return to daily activities. If successful, surgeons might see more early-stage referrals from Barrett’s patients now in surveillance," added Dr. Luketich, professor of surgery and chief of the Heart, Lung and Esophageal Surgery Institute at the University of Pittsburgh Medical Center.
A modified Ivor-Lewis approach involving laparoscopic conduit preparation, videothoracoscopic esophageal mobilization, and intrathoracic anastomosis is preferable to the McKeown approach when the minimally invasive route is chosen. It entails fewer conduit complications and lower mortality, according to Dr. Luketich.
In this series, 49% of patients underwent a modified McKeown approach involving videothoracoscopic esophageal mobilization, laparoscopic conduit preparation, and neck anastomosis, whereas 51% were treated via the modified Ivor-Lewis approach.
This was a nonrandomized study, but patients in the two study arms were essentially the same in terms of baseline characteristics. In all, 95% were operated on for malignant disease, 80% were men, and 31% received preoperative chemotherapy and/or radiotherapy. Patients who were operated on in the most recent years of the series underwent the Ivor-Lewis approach because Dr. Luketich has come to prefer it. He noted that most trainees are more comfortable with it; they have far more experience with operating in the chest than the neck.
Furthermore, outcomes are better than results with the McKeown approach. Indeed, the 30-day mortality rate was just 1.2% with the Ivor-Lewis minimally invasive esophagectomy chest (MIE-chest) approach vs. 2.5% with the McKeown MIE-neck approach. The major morbidity rate was 31% in the MIE-chest group, significantly less than the 36% with the MIE-neck group. This difference was driven by the increased risk of laryngeal nerve injury with the McKeown approach. The incidence of vocal cord paresis or paralysis was 8% in the MIE-neck patients, compared with 1% in the MIE-chest group.
Rates of other complications were closely similar in the two groups: 6% for empyema, 5% for acute respiratory distress syndrome, 5% for pulmonary embolism, 2% for acute MI, 3% for heart failure, and 5% for anastomotic leak requiring surgery.
Quality of life assessments using the Short Form-36 indicate that by 90 days, post-MIE patients scored in the age-adjusted normal range.
"I think by 90 days the patients have bounced back," he concluded. "Laparoscopy–VATS [video-assisted thoracic surgery]–chest anastomosis is now our preferred approach to most esophageal cancers."
Discussant Dr. David J. Sugarbaker called Dr. Luketich’s study "a landmark paper."
"Dr. Luketich has been a pioneer in esophageal resection, and I think has developed a procedure that is rapidly becoming a standard of care worldwide. This is the largest experience reported to date," noted Dr. Sugarbaker, professor of surgical oncology and chief of the division of thoracic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston.
"He’s set the standard, both in quantity and quality, for this operation," agreed Dr. John G. Hunter, professor and chairman of the department of surgery at Oregon Health and Science University, Portland.
Dr. Luketich declared having no financial conflicts of interest.
BOCA RATON, FLA. — Minimally invasive esophagectomy has advanced to the point where it offers significant advantages over open esophagectomy in terms of operative morbidity and mortality, judging by results of a single-center review of 980 cases.
Published series indicate that the operative mortality of open esophagectomy is 8%-21%, although a very few high-volume medical centers have reported rates as low as 3%.
"There is a perception among patients and physicians that open esophagectomy is to be avoided at all costs because of it substantial morbidity," Dr. James D. Luketich said at the annual meeting of the American Surgical Association.
In his review of 980 consecutive, elective, nonurgent, minimally invasive esophagectomies, the 30-day mortality was just 1.8%. Median operative time was 6.7 hours, which dropped to 4 hours in cases that were not done by residents. The median ICU stay was 2.0 days, with a median hospital length of stay of 8 days. A median 21 lymph nodes were dissected, and 98% of cases had negative surgical margins.
"A less invasive surgical approach for esophageal cancer would improve the standard of care by reducing morbidity and shortening hospital stays and time to return to daily activities. If successful, surgeons might see more early-stage referrals from Barrett’s patients now in surveillance," added Dr. Luketich, professor of surgery and chief of the Heart, Lung and Esophageal Surgery Institute at the University of Pittsburgh Medical Center.
A modified Ivor-Lewis approach involving laparoscopic conduit preparation, videothoracoscopic esophageal mobilization, and intrathoracic anastomosis is preferable to the McKeown approach when the minimally invasive route is chosen. It entails fewer conduit complications and lower mortality, according to Dr. Luketich.
In this series, 49% of patients underwent a modified McKeown approach involving videothoracoscopic esophageal mobilization, laparoscopic conduit preparation, and neck anastomosis, whereas 51% were treated via the modified Ivor-Lewis approach.
This was a nonrandomized study, but patients in the two study arms were essentially the same in terms of baseline characteristics. In all, 95% were operated on for malignant disease, 80% were men, and 31% received preoperative chemotherapy and/or radiotherapy. Patients who were operated on in the most recent years of the series underwent the Ivor-Lewis approach because Dr. Luketich has come to prefer it. He noted that most trainees are more comfortable with it; they have far more experience with operating in the chest than the neck.
Furthermore, outcomes are better than results with the McKeown approach. Indeed, the 30-day mortality rate was just 1.2% with the Ivor-Lewis minimally invasive esophagectomy chest (MIE-chest) approach vs. 2.5% with the McKeown MIE-neck approach. The major morbidity rate was 31% in the MIE-chest group, significantly less than the 36% with the MIE-neck group. This difference was driven by the increased risk of laryngeal nerve injury with the McKeown approach. The incidence of vocal cord paresis or paralysis was 8% in the MIE-neck patients, compared with 1% in the MIE-chest group.
Rates of other complications were closely similar in the two groups: 6% for empyema, 5% for acute respiratory distress syndrome, 5% for pulmonary embolism, 2% for acute MI, 3% for heart failure, and 5% for anastomotic leak requiring surgery.
Quality of life assessments using the Short Form-36 indicate that by 90 days, post-MIE patients scored in the age-adjusted normal range.
"I think by 90 days the patients have bounced back," he concluded. "Laparoscopy–VATS [video-assisted thoracic surgery]–chest anastomosis is now our preferred approach to most esophageal cancers."
Discussant Dr. David J. Sugarbaker called Dr. Luketich’s study "a landmark paper."
"Dr. Luketich has been a pioneer in esophageal resection, and I think has developed a procedure that is rapidly becoming a standard of care worldwide. This is the largest experience reported to date," noted Dr. Sugarbaker, professor of surgical oncology and chief of the division of thoracic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston.
"He’s set the standard, both in quantity and quality, for this operation," agreed Dr. John G. Hunter, professor and chairman of the department of surgery at Oregon Health and Science University, Portland.
Dr. Luketich declared having no financial conflicts of interest.
BOCA RATON, FLA. — Minimally invasive esophagectomy has advanced to the point where it offers significant advantages over open esophagectomy in terms of operative morbidity and mortality, judging by results of a single-center review of 980 cases.
Published series indicate that the operative mortality of open esophagectomy is 8%-21%, although a very few high-volume medical centers have reported rates as low as 3%.
"There is a perception among patients and physicians that open esophagectomy is to be avoided at all costs because of it substantial morbidity," Dr. James D. Luketich said at the annual meeting of the American Surgical Association.
In his review of 980 consecutive, elective, nonurgent, minimally invasive esophagectomies, the 30-day mortality was just 1.8%. Median operative time was 6.7 hours, which dropped to 4 hours in cases that were not done by residents. The median ICU stay was 2.0 days, with a median hospital length of stay of 8 days. A median 21 lymph nodes were dissected, and 98% of cases had negative surgical margins.
"A less invasive surgical approach for esophageal cancer would improve the standard of care by reducing morbidity and shortening hospital stays and time to return to daily activities. If successful, surgeons might see more early-stage referrals from Barrett’s patients now in surveillance," added Dr. Luketich, professor of surgery and chief of the Heart, Lung and Esophageal Surgery Institute at the University of Pittsburgh Medical Center.
A modified Ivor-Lewis approach involving laparoscopic conduit preparation, videothoracoscopic esophageal mobilization, and intrathoracic anastomosis is preferable to the McKeown approach when the minimally invasive route is chosen. It entails fewer conduit complications and lower mortality, according to Dr. Luketich.
In this series, 49% of patients underwent a modified McKeown approach involving videothoracoscopic esophageal mobilization, laparoscopic conduit preparation, and neck anastomosis, whereas 51% were treated via the modified Ivor-Lewis approach.
This was a nonrandomized study, but patients in the two study arms were essentially the same in terms of baseline characteristics. In all, 95% were operated on for malignant disease, 80% were men, and 31% received preoperative chemotherapy and/or radiotherapy. Patients who were operated on in the most recent years of the series underwent the Ivor-Lewis approach because Dr. Luketich has come to prefer it. He noted that most trainees are more comfortable with it; they have far more experience with operating in the chest than the neck.
Furthermore, outcomes are better than results with the McKeown approach. Indeed, the 30-day mortality rate was just 1.2% with the Ivor-Lewis minimally invasive esophagectomy chest (MIE-chest) approach vs. 2.5% with the McKeown MIE-neck approach. The major morbidity rate was 31% in the MIE-chest group, significantly less than the 36% with the MIE-neck group. This difference was driven by the increased risk of laryngeal nerve injury with the McKeown approach. The incidence of vocal cord paresis or paralysis was 8% in the MIE-neck patients, compared with 1% in the MIE-chest group.
Rates of other complications were closely similar in the two groups: 6% for empyema, 5% for acute respiratory distress syndrome, 5% for pulmonary embolism, 2% for acute MI, 3% for heart failure, and 5% for anastomotic leak requiring surgery.
Quality of life assessments using the Short Form-36 indicate that by 90 days, post-MIE patients scored in the age-adjusted normal range.
"I think by 90 days the patients have bounced back," he concluded. "Laparoscopy–VATS [video-assisted thoracic surgery]–chest anastomosis is now our preferred approach to most esophageal cancers."
Discussant Dr. David J. Sugarbaker called Dr. Luketich’s study "a landmark paper."
"Dr. Luketich has been a pioneer in esophageal resection, and I think has developed a procedure that is rapidly becoming a standard of care worldwide. This is the largest experience reported to date," noted Dr. Sugarbaker, professor of surgical oncology and chief of the division of thoracic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston.
"He’s set the standard, both in quantity and quality, for this operation," agreed Dr. John G. Hunter, professor and chairman of the department of surgery at Oregon Health and Science University, Portland.
Dr. Luketich declared having no financial conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: The 30-day mortality following minimally invasive esophagectomy with a chest approach was 1.2%, vs. 2.5% with a neck approach. Rates reported with open esophagectomy are typically 5- to 10-fold higher.
Data Source: Retrospective, single-center study of 980 consecutive cases.
Disclosures: Dr. Luketich declared having no financial conflicts of interest.
Minimally Invasive Esophagectomy Leads to Low Mortality
BOCA RATON, FLA. — Minimally invasive esophagectomy has advanced to the point where it offers significant advantages over open esophagectomy in terms of operative morbidity and mortality, judging by results of a single-center review of 980 cases.
Published series indicate that the operative mortality of open esophagectomy is 8%-21%, although a very few high-volume medical centers have reported rates as low as 3%.
"There is a perception among patients and physicians that open esophagectomy is to be avoided at all costs because of it substantial morbidity," Dr. James D. Luketich said at the annual meeting of the American Surgical Association.
In his review of 980 consecutive, elective, nonurgent, minimally invasive esophagectomies, the 30-day mortality was just 1.8%. Median operative time was 6.7 hours, which dropped to 4 hours in cases that were not done by residents. The median ICU stay was 2.0 days, with a median hospital length of stay of 8 days. A median 21 lymph nodes were dissected, and 98% of cases had negative surgical margins.
"A less invasive surgical approach for esophageal cancer would improve the standard of care by reducing morbidity and shortening hospital stays and time to return to daily activities. If successful, surgeons might see more early-stage referrals from Barrett’s patients now in surveillance," added Dr. Luketich, professor of surgery and chief of the Heart, Lung and Esophageal Surgery Institute at the University of Pittsburgh Medical Center.
A modified Ivor-Lewis approach involving laparoscopic conduit preparation, videothoracoscopic esophageal mobilization, and intrathoracic anastomosis is preferable to the McKeown approach when the minimally invasive route is chosen. It entails fewer conduit complications and lower mortality, according to Dr. Luketich.
In this series, 49% of patients underwent a modified McKeown approach involving videothoracoscopic esophageal mobilization, laparoscopic conduit preparation, and neck anastomosis, whereas 51% were treated via the modified Ivor-Lewis approach.
This was a nonrandomized study, but patients in the two study arms were essentially the same in terms of baseline characteristics. In all, 95% were operated on for malignant disease, 80% were men, and 31% received preoperative chemotherapy and/or radiotherapy. Patients who were operated on in the most recent years of the series underwent the Ivor-Lewis approach because Dr. Luketich has come to prefer it. He noted that most trainees are more comfortable with it; they have far more experience with operating in the chest than the neck.
Furthermore, outcomes are better than results with the McKeown approach. Indeed, the 30-day mortality rate was just 1.2% with the Ivor-Lewis minimally invasive esophagectomy chest (MIE-chest) approach vs. 2.5% with the McKeown MIE-neck approach. The major morbidity rate was 31% in the MIE-chest group, significantly less than the 36% with the MIE-neck group. This difference was driven by the increased risk of laryngeal nerve injury with the McKeown approach. The incidence of vocal cord paresis or paralysis was 8% in the MIE-neck patients, compared with 1% in the MIE-chest group.
Rates of other complications were closely similar in the two groups: 6% for empyema, 5% for acute respiratory distress syndrome, 5% for pulmonary embolism, 2% for acute MI, 3% for heart failure, and 5% for anastomotic leak requiring surgery.
Quality of life assessments using the Short Form-36 indicate that by 90 days, post-MIE patients scored in the age-adjusted normal range.
"I think by 90 days the patients have bounced back," he concluded. "Laparoscopy–VATS [video-assisted thoracic surgery]–chest anastomosis is now our preferred approach to most esophageal cancers."
Discussant Dr. David J. Sugarbaker called Dr. Luketich’s study "a landmark paper."
"Dr. Luketich has been a pioneer in esophageal resection, and I think has developed a procedure that is rapidly becoming a standard of care worldwide. This is the largest experience reported to date," noted Dr. Sugarbaker, professor of surgical oncology and chief of the division of thoracic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston.
"He’s set the standard, both in quantity and quality, for this operation," agreed Dr. John G. Hunter, professor and chairman of the department of surgery at Oregon Health and Science University, Portland.
Dr. Luketich declared having no financial conflicts of interest.
BOCA RATON, FLA. — Minimally invasive esophagectomy has advanced to the point where it offers significant advantages over open esophagectomy in terms of operative morbidity and mortality, judging by results of a single-center review of 980 cases.
Published series indicate that the operative mortality of open esophagectomy is 8%-21%, although a very few high-volume medical centers have reported rates as low as 3%.
"There is a perception among patients and physicians that open esophagectomy is to be avoided at all costs because of it substantial morbidity," Dr. James D. Luketich said at the annual meeting of the American Surgical Association.
In his review of 980 consecutive, elective, nonurgent, minimally invasive esophagectomies, the 30-day mortality was just 1.8%. Median operative time was 6.7 hours, which dropped to 4 hours in cases that were not done by residents. The median ICU stay was 2.0 days, with a median hospital length of stay of 8 days. A median 21 lymph nodes were dissected, and 98% of cases had negative surgical margins.
"A less invasive surgical approach for esophageal cancer would improve the standard of care by reducing morbidity and shortening hospital stays and time to return to daily activities. If successful, surgeons might see more early-stage referrals from Barrett’s patients now in surveillance," added Dr. Luketich, professor of surgery and chief of the Heart, Lung and Esophageal Surgery Institute at the University of Pittsburgh Medical Center.
A modified Ivor-Lewis approach involving laparoscopic conduit preparation, videothoracoscopic esophageal mobilization, and intrathoracic anastomosis is preferable to the McKeown approach when the minimally invasive route is chosen. It entails fewer conduit complications and lower mortality, according to Dr. Luketich.
In this series, 49% of patients underwent a modified McKeown approach involving videothoracoscopic esophageal mobilization, laparoscopic conduit preparation, and neck anastomosis, whereas 51% were treated via the modified Ivor-Lewis approach.
This was a nonrandomized study, but patients in the two study arms were essentially the same in terms of baseline characteristics. In all, 95% were operated on for malignant disease, 80% were men, and 31% received preoperative chemotherapy and/or radiotherapy. Patients who were operated on in the most recent years of the series underwent the Ivor-Lewis approach because Dr. Luketich has come to prefer it. He noted that most trainees are more comfortable with it; they have far more experience with operating in the chest than the neck.
Furthermore, outcomes are better than results with the McKeown approach. Indeed, the 30-day mortality rate was just 1.2% with the Ivor-Lewis minimally invasive esophagectomy chest (MIE-chest) approach vs. 2.5% with the McKeown MIE-neck approach. The major morbidity rate was 31% in the MIE-chest group, significantly less than the 36% with the MIE-neck group. This difference was driven by the increased risk of laryngeal nerve injury with the McKeown approach. The incidence of vocal cord paresis or paralysis was 8% in the MIE-neck patients, compared with 1% in the MIE-chest group.
Rates of other complications were closely similar in the two groups: 6% for empyema, 5% for acute respiratory distress syndrome, 5% for pulmonary embolism, 2% for acute MI, 3% for heart failure, and 5% for anastomotic leak requiring surgery.
Quality of life assessments using the Short Form-36 indicate that by 90 days, post-MIE patients scored in the age-adjusted normal range.
"I think by 90 days the patients have bounced back," he concluded. "Laparoscopy–VATS [video-assisted thoracic surgery]–chest anastomosis is now our preferred approach to most esophageal cancers."
Discussant Dr. David J. Sugarbaker called Dr. Luketich’s study "a landmark paper."
"Dr. Luketich has been a pioneer in esophageal resection, and I think has developed a procedure that is rapidly becoming a standard of care worldwide. This is the largest experience reported to date," noted Dr. Sugarbaker, professor of surgical oncology and chief of the division of thoracic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston.
"He’s set the standard, both in quantity and quality, for this operation," agreed Dr. John G. Hunter, professor and chairman of the department of surgery at Oregon Health and Science University, Portland.
Dr. Luketich declared having no financial conflicts of interest.
BOCA RATON, FLA. — Minimally invasive esophagectomy has advanced to the point where it offers significant advantages over open esophagectomy in terms of operative morbidity and mortality, judging by results of a single-center review of 980 cases.
Published series indicate that the operative mortality of open esophagectomy is 8%-21%, although a very few high-volume medical centers have reported rates as low as 3%.
"There is a perception among patients and physicians that open esophagectomy is to be avoided at all costs because of it substantial morbidity," Dr. James D. Luketich said at the annual meeting of the American Surgical Association.
In his review of 980 consecutive, elective, nonurgent, minimally invasive esophagectomies, the 30-day mortality was just 1.8%. Median operative time was 6.7 hours, which dropped to 4 hours in cases that were not done by residents. The median ICU stay was 2.0 days, with a median hospital length of stay of 8 days. A median 21 lymph nodes were dissected, and 98% of cases had negative surgical margins.
"A less invasive surgical approach for esophageal cancer would improve the standard of care by reducing morbidity and shortening hospital stays and time to return to daily activities. If successful, surgeons might see more early-stage referrals from Barrett’s patients now in surveillance," added Dr. Luketich, professor of surgery and chief of the Heart, Lung and Esophageal Surgery Institute at the University of Pittsburgh Medical Center.
A modified Ivor-Lewis approach involving laparoscopic conduit preparation, videothoracoscopic esophageal mobilization, and intrathoracic anastomosis is preferable to the McKeown approach when the minimally invasive route is chosen. It entails fewer conduit complications and lower mortality, according to Dr. Luketich.
In this series, 49% of patients underwent a modified McKeown approach involving videothoracoscopic esophageal mobilization, laparoscopic conduit preparation, and neck anastomosis, whereas 51% were treated via the modified Ivor-Lewis approach.
This was a nonrandomized study, but patients in the two study arms were essentially the same in terms of baseline characteristics. In all, 95% were operated on for malignant disease, 80% were men, and 31% received preoperative chemotherapy and/or radiotherapy. Patients who were operated on in the most recent years of the series underwent the Ivor-Lewis approach because Dr. Luketich has come to prefer it. He noted that most trainees are more comfortable with it; they have far more experience with operating in the chest than the neck.
Furthermore, outcomes are better than results with the McKeown approach. Indeed, the 30-day mortality rate was just 1.2% with the Ivor-Lewis minimally invasive esophagectomy chest (MIE-chest) approach vs. 2.5% with the McKeown MIE-neck approach. The major morbidity rate was 31% in the MIE-chest group, significantly less than the 36% with the MIE-neck group. This difference was driven by the increased risk of laryngeal nerve injury with the McKeown approach. The incidence of vocal cord paresis or paralysis was 8% in the MIE-neck patients, compared with 1% in the MIE-chest group.
Rates of other complications were closely similar in the two groups: 6% for empyema, 5% for acute respiratory distress syndrome, 5% for pulmonary embolism, 2% for acute MI, 3% for heart failure, and 5% for anastomotic leak requiring surgery.
Quality of life assessments using the Short Form-36 indicate that by 90 days, post-MIE patients scored in the age-adjusted normal range.
"I think by 90 days the patients have bounced back," he concluded. "Laparoscopy–VATS [video-assisted thoracic surgery]–chest anastomosis is now our preferred approach to most esophageal cancers."
Discussant Dr. David J. Sugarbaker called Dr. Luketich’s study "a landmark paper."
"Dr. Luketich has been a pioneer in esophageal resection, and I think has developed a procedure that is rapidly becoming a standard of care worldwide. This is the largest experience reported to date," noted Dr. Sugarbaker, professor of surgical oncology and chief of the division of thoracic surgery at Brigham and Women’s Hospital and Harvard Medical School, Boston.
"He’s set the standard, both in quantity and quality, for this operation," agreed Dr. John G. Hunter, professor and chairman of the department of surgery at Oregon Health and Science University, Portland.
Dr. Luketich declared having no financial conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
ABS Survey Finds Increased Caseloads Among General Surgeons
BOCA RATON, FLA. – General surgeons are working harder than ever, with significantly bigger annual operative case totals than a decade ago, and the overload is expected to worsen, based on findings of a new American Board of Surgery analysis of general surgery workloads and practice patterns during 2007-2009.
"My sense is that there’s a worsening shortage of general surgeons that’s causing them to work harder. There’s more need for them. I don’t know what is the maximum number of operations a general surgeon can do in a year, but I bet it’s pretty close to where we are right now," Dr. R. James Valentine said in presenting the ABS survey findings at the annual meeting of the American Surgical Association.
Nearly 80% of trainees completing general surgery residencies now opt to obtain additional surgical subspecialty fellowship training, which means that the number of general surgeons going directly into practice is decreasing and the number of surgical subspecialists is climbing.
The ABS survey showed that these subspecialist surgeons perform roughly 25% of all core general surgery procedures being done in the United States. But as these subspecialist surgeons narrow their practices over time – which is the norm in response to patient demands and practice referral patterns – the core general surgery procedures that they will no longer be doing will fall squarely on the shoulders of already-overworked general surgeons, explained Dr. Valentine, professor and vice chairman of the department of surgery at the University of Texas Southwestern Medical Center, Dallas.
The ABS study involved analysis of the surgical operative logs of 4,968 surgeons who took the recertification exam in 2007-2009. Some 68% of them were certified only in general surgery, whereas the rest had one or more additional American Board of Medical Specialties certificates.
In all, 88% of all general surgeons seeking recertification were men. They performed an average of 506 operative cases per year, compared with 375 for female general surgeons. These operative caseloads were significantly higher than those reflected in a similar ABS survey conducted a decade earlier. Moreover, in 2007-2009, general surgeons performed more procedures in all areas – abdominal, alimentary, breast, endoscopy, vascular, and laparoscopy – than in 1997-1999.
Among other key study findings were the following:
• Female general surgeons performed far more breast operations and significantly fewer abdominal, alimentary, and laparoscopic operations than did their male counterparts.
• Subspecialist surgeons did 26% of all core general surgery alimentary operations such as appendectomies and cholecystectomies, 10% of all breast operations, 13% of abdominal, 15% of laparoscopic, and 26% of endoscopic procedures.
General surgeons performed 46% of all vascular, 16% of thoracic, 30% of pediatric, and 33% of plastic surgery operations.
• A huge difference in practice patterns between urban and rural general surgeons was identified. Rural general surgeons performed far more endoscopic procedures and significantly fewer abdominal, alimentary, and laparoscopic procedures than did their urban counterparts.
• Within the field of vascular surgery, general surgeons performed 35% of all carotid endarterectomies, 27% of leg bypass procedures, 25% of aneurysm repairs, and 24% of all endovascular procedures.
• U.S. medical school graduates and international medical graduates had similar workloads and distribution of operations.
"We conclude from these data that the reduced general surgery operative experience in residencies with coexisting fellowship programs may negatively impact access to general surgery care. Similarly, narrowing general surgery residency operative experience may impair access to specialty operations," Dr. Valentine said.
Discussant Dr. George F. Sheldon said the message of this and other studies is that there remains a clear need to train general surgeons who are able to care for a wide range of surgical conditions.
"The type of practice and some of the tools may differ, and the setting in which we work may be changing, but I really think the fundamental concept of a broadly trained general surgeon is validated by all of the studies that have been done," said Dr. Sheldon, professor of surgery and social medicine at the University of North Carolina at Chapel Hill.
Dr. E. Christopher Ellison, chair of the ABS, drew attention to the large number of endoscopic procedures being performed by general surgeons, particularly those in rural practice.
"I think with the recent debate about the role of general surgeons in endoscopy, your evidence presents a case that we need to continue a high level of endoscopy training in our general surgery programs. In our rural and less populated areas, the general surgeon provides ready access to endoscopy of the upper and lower GI tract. Certainly, this is a benefit to the patients living in those areas," commented Dr. Ellison, professor and chair of the department of surgery and associate vice president for health sciences at the Ohio State University, Columbus.
Dr. Valentine concurred.
"It certainly looks like general surgeons are doing a lot of endoscopy without the help of our GI colleagues, especially in rural areas. That’s something that we need to remember when we’re challenged by those societies," according to Dr. Valentine.
He said he had no financial conflicts.
BOCA RATON, FLA. – General surgeons are working harder than ever, with significantly bigger annual operative case totals than a decade ago, and the overload is expected to worsen, based on findings of a new American Board of Surgery analysis of general surgery workloads and practice patterns during 2007-2009.
"My sense is that there’s a worsening shortage of general surgeons that’s causing them to work harder. There’s more need for them. I don’t know what is the maximum number of operations a general surgeon can do in a year, but I bet it’s pretty close to where we are right now," Dr. R. James Valentine said in presenting the ABS survey findings at the annual meeting of the American Surgical Association.
Nearly 80% of trainees completing general surgery residencies now opt to obtain additional surgical subspecialty fellowship training, which means that the number of general surgeons going directly into practice is decreasing and the number of surgical subspecialists is climbing.
The ABS survey showed that these subspecialist surgeons perform roughly 25% of all core general surgery procedures being done in the United States. But as these subspecialist surgeons narrow their practices over time – which is the norm in response to patient demands and practice referral patterns – the core general surgery procedures that they will no longer be doing will fall squarely on the shoulders of already-overworked general surgeons, explained Dr. Valentine, professor and vice chairman of the department of surgery at the University of Texas Southwestern Medical Center, Dallas.
The ABS study involved analysis of the surgical operative logs of 4,968 surgeons who took the recertification exam in 2007-2009. Some 68% of them were certified only in general surgery, whereas the rest had one or more additional American Board of Medical Specialties certificates.
In all, 88% of all general surgeons seeking recertification were men. They performed an average of 506 operative cases per year, compared with 375 for female general surgeons. These operative caseloads were significantly higher than those reflected in a similar ABS survey conducted a decade earlier. Moreover, in 2007-2009, general surgeons performed more procedures in all areas – abdominal, alimentary, breast, endoscopy, vascular, and laparoscopy – than in 1997-1999.
Among other key study findings were the following:
• Female general surgeons performed far more breast operations and significantly fewer abdominal, alimentary, and laparoscopic operations than did their male counterparts.
• Subspecialist surgeons did 26% of all core general surgery alimentary operations such as appendectomies and cholecystectomies, 10% of all breast operations, 13% of abdominal, 15% of laparoscopic, and 26% of endoscopic procedures.
General surgeons performed 46% of all vascular, 16% of thoracic, 30% of pediatric, and 33% of plastic surgery operations.
• A huge difference in practice patterns between urban and rural general surgeons was identified. Rural general surgeons performed far more endoscopic procedures and significantly fewer abdominal, alimentary, and laparoscopic procedures than did their urban counterparts.
• Within the field of vascular surgery, general surgeons performed 35% of all carotid endarterectomies, 27% of leg bypass procedures, 25% of aneurysm repairs, and 24% of all endovascular procedures.
• U.S. medical school graduates and international medical graduates had similar workloads and distribution of operations.
"We conclude from these data that the reduced general surgery operative experience in residencies with coexisting fellowship programs may negatively impact access to general surgery care. Similarly, narrowing general surgery residency operative experience may impair access to specialty operations," Dr. Valentine said.
Discussant Dr. George F. Sheldon said the message of this and other studies is that there remains a clear need to train general surgeons who are able to care for a wide range of surgical conditions.
"The type of practice and some of the tools may differ, and the setting in which we work may be changing, but I really think the fundamental concept of a broadly trained general surgeon is validated by all of the studies that have been done," said Dr. Sheldon, professor of surgery and social medicine at the University of North Carolina at Chapel Hill.
Dr. E. Christopher Ellison, chair of the ABS, drew attention to the large number of endoscopic procedures being performed by general surgeons, particularly those in rural practice.
"I think with the recent debate about the role of general surgeons in endoscopy, your evidence presents a case that we need to continue a high level of endoscopy training in our general surgery programs. In our rural and less populated areas, the general surgeon provides ready access to endoscopy of the upper and lower GI tract. Certainly, this is a benefit to the patients living in those areas," commented Dr. Ellison, professor and chair of the department of surgery and associate vice president for health sciences at the Ohio State University, Columbus.
Dr. Valentine concurred.
"It certainly looks like general surgeons are doing a lot of endoscopy without the help of our GI colleagues, especially in rural areas. That’s something that we need to remember when we’re challenged by those societies," according to Dr. Valentine.
He said he had no financial conflicts.
BOCA RATON, FLA. – General surgeons are working harder than ever, with significantly bigger annual operative case totals than a decade ago, and the overload is expected to worsen, based on findings of a new American Board of Surgery analysis of general surgery workloads and practice patterns during 2007-2009.
"My sense is that there’s a worsening shortage of general surgeons that’s causing them to work harder. There’s more need for them. I don’t know what is the maximum number of operations a general surgeon can do in a year, but I bet it’s pretty close to where we are right now," Dr. R. James Valentine said in presenting the ABS survey findings at the annual meeting of the American Surgical Association.
Nearly 80% of trainees completing general surgery residencies now opt to obtain additional surgical subspecialty fellowship training, which means that the number of general surgeons going directly into practice is decreasing and the number of surgical subspecialists is climbing.
The ABS survey showed that these subspecialist surgeons perform roughly 25% of all core general surgery procedures being done in the United States. But as these subspecialist surgeons narrow their practices over time – which is the norm in response to patient demands and practice referral patterns – the core general surgery procedures that they will no longer be doing will fall squarely on the shoulders of already-overworked general surgeons, explained Dr. Valentine, professor and vice chairman of the department of surgery at the University of Texas Southwestern Medical Center, Dallas.
The ABS study involved analysis of the surgical operative logs of 4,968 surgeons who took the recertification exam in 2007-2009. Some 68% of them were certified only in general surgery, whereas the rest had one or more additional American Board of Medical Specialties certificates.
In all, 88% of all general surgeons seeking recertification were men. They performed an average of 506 operative cases per year, compared with 375 for female general surgeons. These operative caseloads were significantly higher than those reflected in a similar ABS survey conducted a decade earlier. Moreover, in 2007-2009, general surgeons performed more procedures in all areas – abdominal, alimentary, breast, endoscopy, vascular, and laparoscopy – than in 1997-1999.
Among other key study findings were the following:
• Female general surgeons performed far more breast operations and significantly fewer abdominal, alimentary, and laparoscopic operations than did their male counterparts.
• Subspecialist surgeons did 26% of all core general surgery alimentary operations such as appendectomies and cholecystectomies, 10% of all breast operations, 13% of abdominal, 15% of laparoscopic, and 26% of endoscopic procedures.
General surgeons performed 46% of all vascular, 16% of thoracic, 30% of pediatric, and 33% of plastic surgery operations.
• A huge difference in practice patterns between urban and rural general surgeons was identified. Rural general surgeons performed far more endoscopic procedures and significantly fewer abdominal, alimentary, and laparoscopic procedures than did their urban counterparts.
• Within the field of vascular surgery, general surgeons performed 35% of all carotid endarterectomies, 27% of leg bypass procedures, 25% of aneurysm repairs, and 24% of all endovascular procedures.
• U.S. medical school graduates and international medical graduates had similar workloads and distribution of operations.
"We conclude from these data that the reduced general surgery operative experience in residencies with coexisting fellowship programs may negatively impact access to general surgery care. Similarly, narrowing general surgery residency operative experience may impair access to specialty operations," Dr. Valentine said.
Discussant Dr. George F. Sheldon said the message of this and other studies is that there remains a clear need to train general surgeons who are able to care for a wide range of surgical conditions.
"The type of practice and some of the tools may differ, and the setting in which we work may be changing, but I really think the fundamental concept of a broadly trained general surgeon is validated by all of the studies that have been done," said Dr. Sheldon, professor of surgery and social medicine at the University of North Carolina at Chapel Hill.
Dr. E. Christopher Ellison, chair of the ABS, drew attention to the large number of endoscopic procedures being performed by general surgeons, particularly those in rural practice.
"I think with the recent debate about the role of general surgeons in endoscopy, your evidence presents a case that we need to continue a high level of endoscopy training in our general surgery programs. In our rural and less populated areas, the general surgeon provides ready access to endoscopy of the upper and lower GI tract. Certainly, this is a benefit to the patients living in those areas," commented Dr. Ellison, professor and chair of the department of surgery and associate vice president for health sciences at the Ohio State University, Columbus.
Dr. Valentine concurred.
"It certainly looks like general surgeons are doing a lot of endoscopy without the help of our GI colleagues, especially in rural areas. That’s something that we need to remember when we’re challenged by those societies," according to Dr. Valentine.
He said he had no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: General surgery operative caseloads are up from a decade ago, even though surgical subspecialists perform one-quarter of all core general surgery procedures.
Data Source: Analysis of the operative logs of nearly 5,000 surgeons who sought recertification in 2007-2009.
Disclosures: Dr. Valentine said he had no financial conflicts.
ABS Survey Finds Increased Caseloads Among General Surgeons
BOCA RATON, FLA. – General surgeons are working harder than ever, with significantly bigger annual operative case totals than a decade ago, and the overload is expected to worsen, based on findings of a new American Board of Surgery analysis of general surgery workloads and practice patterns during 2007-2009.
"My sense is that there’s a worsening shortage of general surgeons that’s causing them to work harder. There’s more need for them. I don’t know what is the maximum number of operations a general surgeon can do in a year, but I bet it’s pretty close to where we are right now," Dr. R. James Valentine said in presenting the ABS survey findings at the annual meeting of the American Surgical Association.
Nearly 80% of trainees completing general surgery residencies now opt to obtain additional surgical subspecialty fellowship training, which means that the number of general surgeons going directly into practice is decreasing and the number of surgical subspecialists is climbing.
The ABS survey showed that these subspecialist surgeons perform roughly 25% of all core general surgery procedures being done in the United States. But as these subspecialist surgeons narrow their practices over time – which is the norm in response to patient demands and practice referral patterns – the core general surgery procedures that they will no longer be doing will fall squarely on the shoulders of already-overworked general surgeons, explained Dr. Valentine, professor and vice chairman of the department of surgery at the University of Texas Southwestern Medical Center, Dallas.
The ABS study involved analysis of the surgical operative logs of 4,968 surgeons who took the recertification exam in 2007-2009. Some 68% of them were certified only in general surgery, whereas the rest had one or more additional American Board of Medical Specialties certificates.
In all, 88% of all general surgeons seeking recertification were men. They performed an average of 506 operative cases per year, compared with 375 for female general surgeons. These operative caseloads were significantly higher than those reflected in a similar ABS survey conducted a decade earlier. Moreover, in 2007-2009, general surgeons performed more procedures in all areas – abdominal, alimentary, breast, endoscopy, vascular, and laparoscopy – than in 1997-1999.
Among other key study findings were the following:
• Female general surgeons performed far more breast operations and significantly fewer abdominal, alimentary, and laparoscopic operations than did their male counterparts.
• Subspecialist surgeons did 26% of all core general surgery alimentary operations such as appendectomies and cholecystectomies, 10% of all breast operations, 13% of abdominal, 15% of laparoscopic, and 26% of endoscopic procedures.
General surgeons performed 46% of all vascular, 16% of thoracic, 30% of pediatric, and 33% of plastic surgery operations.
• A huge difference in practice patterns between urban and rural general surgeons was identified. Rural general surgeons performed far more endoscopic procedures and significantly fewer abdominal, alimentary, and laparoscopic procedures than did their urban counterparts.
• Within the field of vascular surgery, general surgeons performed 35% of all carotid endarterectomies, 27% of leg bypass procedures, 25% of aneurysm repairs, and 24% of all endovascular procedures.
• U.S. medical school graduates and international medical graduates had similar workloads and distribution of operations.
"We conclude from these data that the reduced general surgery operative experience in residencies with coexisting fellowship programs may negatively impact access to general surgery care. Similarly, narrowing general surgery residency operative experience may impair access to specialty operations," Dr. Valentine said.
Discussant Dr. George F. Sheldon said the message of this and other studies is that there remains a clear need to train general surgeons who are able to care for a wide range of surgical conditions.
"The type of practice and some of the tools may differ, and the setting in which we work may be changing, but I really think the fundamental concept of a broadly trained general surgeon is validated by all of the studies that have been done," said Dr. Sheldon, professor of surgery and social medicine at the University of North Carolina at Chapel Hill.
Dr. E. Christopher Ellison, chair of the ABS, drew attention to the large number of endoscopic procedures being performed by general surgeons, particularly those in rural practice.
"I think with the recent debate about the role of general surgeons in endoscopy, your evidence presents a case that we need to continue a high level of endoscopy training in our general surgery programs. In our rural and less populated areas, the general surgeon provides ready access to endoscopy of the upper and lower GI tract. Certainly, this is a benefit to the patients living in those areas," commented Dr. Ellison, professor and chair of the department of surgery and associate vice president for health sciences at the Ohio State University, Columbus.
Dr. Valentine concurred.
"It certainly looks like general surgeons are doing a lot of endoscopy without the help of our GI colleagues, especially in rural areas. That’s something that we need to remember when we’re challenged by those societies," according to Dr. Valentine.
He said he had no financial conflicts.
BOCA RATON, FLA. – General surgeons are working harder than ever, with significantly bigger annual operative case totals than a decade ago, and the overload is expected to worsen, based on findings of a new American Board of Surgery analysis of general surgery workloads and practice patterns during 2007-2009.
"My sense is that there’s a worsening shortage of general surgeons that’s causing them to work harder. There’s more need for them. I don’t know what is the maximum number of operations a general surgeon can do in a year, but I bet it’s pretty close to where we are right now," Dr. R. James Valentine said in presenting the ABS survey findings at the annual meeting of the American Surgical Association.
Nearly 80% of trainees completing general surgery residencies now opt to obtain additional surgical subspecialty fellowship training, which means that the number of general surgeons going directly into practice is decreasing and the number of surgical subspecialists is climbing.
The ABS survey showed that these subspecialist surgeons perform roughly 25% of all core general surgery procedures being done in the United States. But as these subspecialist surgeons narrow their practices over time – which is the norm in response to patient demands and practice referral patterns – the core general surgery procedures that they will no longer be doing will fall squarely on the shoulders of already-overworked general surgeons, explained Dr. Valentine, professor and vice chairman of the department of surgery at the University of Texas Southwestern Medical Center, Dallas.
The ABS study involved analysis of the surgical operative logs of 4,968 surgeons who took the recertification exam in 2007-2009. Some 68% of them were certified only in general surgery, whereas the rest had one or more additional American Board of Medical Specialties certificates.
In all, 88% of all general surgeons seeking recertification were men. They performed an average of 506 operative cases per year, compared with 375 for female general surgeons. These operative caseloads were significantly higher than those reflected in a similar ABS survey conducted a decade earlier. Moreover, in 2007-2009, general surgeons performed more procedures in all areas – abdominal, alimentary, breast, endoscopy, vascular, and laparoscopy – than in 1997-1999.
Among other key study findings were the following:
• Female general surgeons performed far more breast operations and significantly fewer abdominal, alimentary, and laparoscopic operations than did their male counterparts.
• Subspecialist surgeons did 26% of all core general surgery alimentary operations such as appendectomies and cholecystectomies, 10% of all breast operations, 13% of abdominal, 15% of laparoscopic, and 26% of endoscopic procedures.
General surgeons performed 46% of all vascular, 16% of thoracic, 30% of pediatric, and 33% of plastic surgery operations.
• A huge difference in practice patterns between urban and rural general surgeons was identified. Rural general surgeons performed far more endoscopic procedures and significantly fewer abdominal, alimentary, and laparoscopic procedures than did their urban counterparts.
• Within the field of vascular surgery, general surgeons performed 35% of all carotid endarterectomies, 27% of leg bypass procedures, 25% of aneurysm repairs, and 24% of all endovascular procedures.
• U.S. medical school graduates and international medical graduates had similar workloads and distribution of operations.
"We conclude from these data that the reduced general surgery operative experience in residencies with coexisting fellowship programs may negatively impact access to general surgery care. Similarly, narrowing general surgery residency operative experience may impair access to specialty operations," Dr. Valentine said.
Discussant Dr. George F. Sheldon said the message of this and other studies is that there remains a clear need to train general surgeons who are able to care for a wide range of surgical conditions.
"The type of practice and some of the tools may differ, and the setting in which we work may be changing, but I really think the fundamental concept of a broadly trained general surgeon is validated by all of the studies that have been done," said Dr. Sheldon, professor of surgery and social medicine at the University of North Carolina at Chapel Hill.
Dr. E. Christopher Ellison, chair of the ABS, drew attention to the large number of endoscopic procedures being performed by general surgeons, particularly those in rural practice.
"I think with the recent debate about the role of general surgeons in endoscopy, your evidence presents a case that we need to continue a high level of endoscopy training in our general surgery programs. In our rural and less populated areas, the general surgeon provides ready access to endoscopy of the upper and lower GI tract. Certainly, this is a benefit to the patients living in those areas," commented Dr. Ellison, professor and chair of the department of surgery and associate vice president for health sciences at the Ohio State University, Columbus.
Dr. Valentine concurred.
"It certainly looks like general surgeons are doing a lot of endoscopy without the help of our GI colleagues, especially in rural areas. That’s something that we need to remember when we’re challenged by those societies," according to Dr. Valentine.
He said he had no financial conflicts.
BOCA RATON, FLA. – General surgeons are working harder than ever, with significantly bigger annual operative case totals than a decade ago, and the overload is expected to worsen, based on findings of a new American Board of Surgery analysis of general surgery workloads and practice patterns during 2007-2009.
"My sense is that there’s a worsening shortage of general surgeons that’s causing them to work harder. There’s more need for them. I don’t know what is the maximum number of operations a general surgeon can do in a year, but I bet it’s pretty close to where we are right now," Dr. R. James Valentine said in presenting the ABS survey findings at the annual meeting of the American Surgical Association.
Nearly 80% of trainees completing general surgery residencies now opt to obtain additional surgical subspecialty fellowship training, which means that the number of general surgeons going directly into practice is decreasing and the number of surgical subspecialists is climbing.
The ABS survey showed that these subspecialist surgeons perform roughly 25% of all core general surgery procedures being done in the United States. But as these subspecialist surgeons narrow their practices over time – which is the norm in response to patient demands and practice referral patterns – the core general surgery procedures that they will no longer be doing will fall squarely on the shoulders of already-overworked general surgeons, explained Dr. Valentine, professor and vice chairman of the department of surgery at the University of Texas Southwestern Medical Center, Dallas.
The ABS study involved analysis of the surgical operative logs of 4,968 surgeons who took the recertification exam in 2007-2009. Some 68% of them were certified only in general surgery, whereas the rest had one or more additional American Board of Medical Specialties certificates.
In all, 88% of all general surgeons seeking recertification were men. They performed an average of 506 operative cases per year, compared with 375 for female general surgeons. These operative caseloads were significantly higher than those reflected in a similar ABS survey conducted a decade earlier. Moreover, in 2007-2009, general surgeons performed more procedures in all areas – abdominal, alimentary, breast, endoscopy, vascular, and laparoscopy – than in 1997-1999.
Among other key study findings were the following:
• Female general surgeons performed far more breast operations and significantly fewer abdominal, alimentary, and laparoscopic operations than did their male counterparts.
• Subspecialist surgeons did 26% of all core general surgery alimentary operations such as appendectomies and cholecystectomies, 10% of all breast operations, 13% of abdominal, 15% of laparoscopic, and 26% of endoscopic procedures.
General surgeons performed 46% of all vascular, 16% of thoracic, 30% of pediatric, and 33% of plastic surgery operations.
• A huge difference in practice patterns between urban and rural general surgeons was identified. Rural general surgeons performed far more endoscopic procedures and significantly fewer abdominal, alimentary, and laparoscopic procedures than did their urban counterparts.
• Within the field of vascular surgery, general surgeons performed 35% of all carotid endarterectomies, 27% of leg bypass procedures, 25% of aneurysm repairs, and 24% of all endovascular procedures.
• U.S. medical school graduates and international medical graduates had similar workloads and distribution of operations.
"We conclude from these data that the reduced general surgery operative experience in residencies with coexisting fellowship programs may negatively impact access to general surgery care. Similarly, narrowing general surgery residency operative experience may impair access to specialty operations," Dr. Valentine said.
Discussant Dr. George F. Sheldon said the message of this and other studies is that there remains a clear need to train general surgeons who are able to care for a wide range of surgical conditions.
"The type of practice and some of the tools may differ, and the setting in which we work may be changing, but I really think the fundamental concept of a broadly trained general surgeon is validated by all of the studies that have been done," said Dr. Sheldon, professor of surgery and social medicine at the University of North Carolina at Chapel Hill.
Dr. E. Christopher Ellison, chair of the ABS, drew attention to the large number of endoscopic procedures being performed by general surgeons, particularly those in rural practice.
"I think with the recent debate about the role of general surgeons in endoscopy, your evidence presents a case that we need to continue a high level of endoscopy training in our general surgery programs. In our rural and less populated areas, the general surgeon provides ready access to endoscopy of the upper and lower GI tract. Certainly, this is a benefit to the patients living in those areas," commented Dr. Ellison, professor and chair of the department of surgery and associate vice president for health sciences at the Ohio State University, Columbus.
Dr. Valentine concurred.
"It certainly looks like general surgeons are doing a lot of endoscopy without the help of our GI colleagues, especially in rural areas. That’s something that we need to remember when we’re challenged by those societies," according to Dr. Valentine.
He said he had no financial conflicts.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Novel Minimally Invasive Surgery Tames Fulminant C. difficile
BOCA RATON, FLA. – For patients with fulminant Clostridium difficile colitis, minimally invasive temporary loop ileostomy with colonic lavage may offer a novel life- and colon-saving alternative to colectomy.
In a series of 42 consecutive patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon, Dr. Brian Zuckerbraun reported at the annual meeting of the American Surgical Association.
This 19% mortality was impressively less than the 50% rate in 42 consecutive historical controls with similar Acute Physiology and Chronic Health Evaluation (APACHE) II scores who underwent subtotal colectomy at the same medical center just prior to introduction of the novel, less invasive operation. And the 50% mortality rate is on the low end of reported series, noted Dr. Zuckerbraun of the University of Pittsburgh.
"This approach may prove to be a better alternative to colectomy, because the colon is usually viable and can recover," he said. "Loop ileostomy and colonic lavage should be considered in all patients with severe complicated C. difficile colitis."
"Also, what we’re finding now because of our outcomes and the smaller insult of this therapy compared to colectomy is that our medical colleagues are willing to consult us earlier in the care of these patients. They’re not just thinking of surgery as a salvage operation when all else has failed," Dr. Zuckerbraun noted.
His presentation drew effusive audience praise.
"Two or three times a year I come across something that causes me to say, ‘I really wish I’d thought of that.’ This is one of those situations. I think this is a wonderful idea," said Dr. Robert G. Sawyer, a discussant.
Dr. Sawyer, professor of surgery and public health sciences and chief of acute care surgery at the University of Virginia, Charlottesville, was particularly impressed that the treatment enabled roughly 90% of patients to save their colon. "I believe this will become the standard technique in the treatment of severe C. difficile colitis in the future," he predicted.
Dr. Merril T. Dayton was equally impressed.
"We may be seeing a bit of history being made here: a new operation. If time bears out your study findings, this is a simpler and effective way to handle these complicated patients," observed Dr. Dayton, professor and chairman of the department of surgery at State University of New York, Buffalo.
Dr. Zuckerbraun explained the rationale for his novel treatment: fulminant C. difficile colitis is a disease of bacterial overgrowth and toxin production in which the colon is usually viable and without necrosis or perforation, meaning that it’s recoverable.
On this basis, he developed a procedure that begins with exploratory laparoscopy or laparotomy. This is followed by creation of a diverting loop ileostomy through which 8 L of propylene glycol electrolyte solution (GoLYTELY) is instilled intraoperatively. Antegrade colonic flushes with 500 mg of vancomycin in 500 mL of diluent are administered every 8 hours for 10 days.
The working hypothesis is that this combination of diversion, propylene glycol lavage, and vancomycin acts in cumulative fashion to reduce C. difficile counts, deprive the pathogen of nutrients, and alter the intraluminal milieu, perhaps changing colonic oxygen tension. Also, there is preliminary evidence to suggest propylene glycol may exert a pharmacologic effect involving protection of the colonic epithelium.
The 42 patients in his series were quite sick, with a mean APACHE II score of 29.7. Many were immunosuppressed. Preoperatively, 90% were in the intensive care unit, where most were intubated and/or on vasopressors.
Loop ileostomy and colonic lavage were accomplished laparoscopically in 35 of 42 patients. With increased experience, Dr. Zuckerbraun and his colleagues have decided that the only indication for open loop ileostomy via laparotomy is abdominal compartment syndrome.
One patient with abdominal compartment syndrome underwent colectomy immediately after loop ileostomy. Two more patients had colectomies during the postoperative period based upon clinical symptoms.
Eight patients died a mean of 13 days after surgery. Of the 34 who survived the 30-day postoperative period, 6 have subsequently died because of comorbid disease – none of these deaths was related to C. difficile.
Twenty-eight patients remain alive at a mean follow-up of 11.4 months. Of the 19 who have been followed for at least 6 months, 15 (79%) have had their ileostomies reversed. Surgeons initially considered performing the reversal during the same hospital stay, but they decided patients with fulminant C. difficile colitis have too many serious comorbidities to be able to handle a second operation early on.
"Most have required months to recover from the illness that brought them into the hospital in the first place, which often wasn’t C. difficile. We wait until they’re back on their feet again," Dr. Zuckerbraun explained.
The indications for temporary loop ileostomy and colonic lavage are, first, diagnosis of C. difficile colitis by toxin assay, a compatible CT scan, or endoscopic findings, along with any one of the following criteria: sepsis, peritonitis, change in mental status, ventilatory failure, vasopressor requirement, worsening abdominal pain or distention, or unexplained clinical deterioration, he said.
At the urging of medical intensivists and transplant physicians, the investigators have also performed this operation in two patients with multiple recurrent episodes of C. difficile colitis who were not critically ill. One patient had 19 prior episodes. The C. difficile was successfully eradicated in both cases. The new procedure, however, was undertaken only after the patients failed a trial of high-volume propylene glycol lavage by nasogastric tube, which the investigators have previously employed successfully to eradicate C. difficile infections in several other patients with multiply recurrent nonfulminant colitis.
Severe, complicated C. difficile colitis occurs in 4%-10% of C. difficile-associated disease, which is now the most common nosocomial infection.
Dr. Zuckerbraun reported no conflicts of interest.
BOCA RATON, FLA. – For patients with fulminant Clostridium difficile colitis, minimally invasive temporary loop ileostomy with colonic lavage may offer a novel life- and colon-saving alternative to colectomy.
In a series of 42 consecutive patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon, Dr. Brian Zuckerbraun reported at the annual meeting of the American Surgical Association.
This 19% mortality was impressively less than the 50% rate in 42 consecutive historical controls with similar Acute Physiology and Chronic Health Evaluation (APACHE) II scores who underwent subtotal colectomy at the same medical center just prior to introduction of the novel, less invasive operation. And the 50% mortality rate is on the low end of reported series, noted Dr. Zuckerbraun of the University of Pittsburgh.
"This approach may prove to be a better alternative to colectomy, because the colon is usually viable and can recover," he said. "Loop ileostomy and colonic lavage should be considered in all patients with severe complicated C. difficile colitis."
"Also, what we’re finding now because of our outcomes and the smaller insult of this therapy compared to colectomy is that our medical colleagues are willing to consult us earlier in the care of these patients. They’re not just thinking of surgery as a salvage operation when all else has failed," Dr. Zuckerbraun noted.
His presentation drew effusive audience praise.
"Two or three times a year I come across something that causes me to say, ‘I really wish I’d thought of that.’ This is one of those situations. I think this is a wonderful idea," said Dr. Robert G. Sawyer, a discussant.
Dr. Sawyer, professor of surgery and public health sciences and chief of acute care surgery at the University of Virginia, Charlottesville, was particularly impressed that the treatment enabled roughly 90% of patients to save their colon. "I believe this will become the standard technique in the treatment of severe C. difficile colitis in the future," he predicted.
Dr. Merril T. Dayton was equally impressed.
"We may be seeing a bit of history being made here: a new operation. If time bears out your study findings, this is a simpler and effective way to handle these complicated patients," observed Dr. Dayton, professor and chairman of the department of surgery at State University of New York, Buffalo.
Dr. Zuckerbraun explained the rationale for his novel treatment: fulminant C. difficile colitis is a disease of bacterial overgrowth and toxin production in which the colon is usually viable and without necrosis or perforation, meaning that it’s recoverable.
On this basis, he developed a procedure that begins with exploratory laparoscopy or laparotomy. This is followed by creation of a diverting loop ileostomy through which 8 L of propylene glycol electrolyte solution (GoLYTELY) is instilled intraoperatively. Antegrade colonic flushes with 500 mg of vancomycin in 500 mL of diluent are administered every 8 hours for 10 days.
The working hypothesis is that this combination of diversion, propylene glycol lavage, and vancomycin acts in cumulative fashion to reduce C. difficile counts, deprive the pathogen of nutrients, and alter the intraluminal milieu, perhaps changing colonic oxygen tension. Also, there is preliminary evidence to suggest propylene glycol may exert a pharmacologic effect involving protection of the colonic epithelium.
The 42 patients in his series were quite sick, with a mean APACHE II score of 29.7. Many were immunosuppressed. Preoperatively, 90% were in the intensive care unit, where most were intubated and/or on vasopressors.
Loop ileostomy and colonic lavage were accomplished laparoscopically in 35 of 42 patients. With increased experience, Dr. Zuckerbraun and his colleagues have decided that the only indication for open loop ileostomy via laparotomy is abdominal compartment syndrome.
One patient with abdominal compartment syndrome underwent colectomy immediately after loop ileostomy. Two more patients had colectomies during the postoperative period based upon clinical symptoms.
Eight patients died a mean of 13 days after surgery. Of the 34 who survived the 30-day postoperative period, 6 have subsequently died because of comorbid disease – none of these deaths was related to C. difficile.
Twenty-eight patients remain alive at a mean follow-up of 11.4 months. Of the 19 who have been followed for at least 6 months, 15 (79%) have had their ileostomies reversed. Surgeons initially considered performing the reversal during the same hospital stay, but they decided patients with fulminant C. difficile colitis have too many serious comorbidities to be able to handle a second operation early on.
"Most have required months to recover from the illness that brought them into the hospital in the first place, which often wasn’t C. difficile. We wait until they’re back on their feet again," Dr. Zuckerbraun explained.
The indications for temporary loop ileostomy and colonic lavage are, first, diagnosis of C. difficile colitis by toxin assay, a compatible CT scan, or endoscopic findings, along with any one of the following criteria: sepsis, peritonitis, change in mental status, ventilatory failure, vasopressor requirement, worsening abdominal pain or distention, or unexplained clinical deterioration, he said.
At the urging of medical intensivists and transplant physicians, the investigators have also performed this operation in two patients with multiple recurrent episodes of C. difficile colitis who were not critically ill. One patient had 19 prior episodes. The C. difficile was successfully eradicated in both cases. The new procedure, however, was undertaken only after the patients failed a trial of high-volume propylene glycol lavage by nasogastric tube, which the investigators have previously employed successfully to eradicate C. difficile infections in several other patients with multiply recurrent nonfulminant colitis.
Severe, complicated C. difficile colitis occurs in 4%-10% of C. difficile-associated disease, which is now the most common nosocomial infection.
Dr. Zuckerbraun reported no conflicts of interest.
BOCA RATON, FLA. – For patients with fulminant Clostridium difficile colitis, minimally invasive temporary loop ileostomy with colonic lavage may offer a novel life- and colon-saving alternative to colectomy.
In a series of 42 consecutive patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon, Dr. Brian Zuckerbraun reported at the annual meeting of the American Surgical Association.
This 19% mortality was impressively less than the 50% rate in 42 consecutive historical controls with similar Acute Physiology and Chronic Health Evaluation (APACHE) II scores who underwent subtotal colectomy at the same medical center just prior to introduction of the novel, less invasive operation. And the 50% mortality rate is on the low end of reported series, noted Dr. Zuckerbraun of the University of Pittsburgh.
"This approach may prove to be a better alternative to colectomy, because the colon is usually viable and can recover," he said. "Loop ileostomy and colonic lavage should be considered in all patients with severe complicated C. difficile colitis."
"Also, what we’re finding now because of our outcomes and the smaller insult of this therapy compared to colectomy is that our medical colleagues are willing to consult us earlier in the care of these patients. They’re not just thinking of surgery as a salvage operation when all else has failed," Dr. Zuckerbraun noted.
His presentation drew effusive audience praise.
"Two or three times a year I come across something that causes me to say, ‘I really wish I’d thought of that.’ This is one of those situations. I think this is a wonderful idea," said Dr. Robert G. Sawyer, a discussant.
Dr. Sawyer, professor of surgery and public health sciences and chief of acute care surgery at the University of Virginia, Charlottesville, was particularly impressed that the treatment enabled roughly 90% of patients to save their colon. "I believe this will become the standard technique in the treatment of severe C. difficile colitis in the future," he predicted.
Dr. Merril T. Dayton was equally impressed.
"We may be seeing a bit of history being made here: a new operation. If time bears out your study findings, this is a simpler and effective way to handle these complicated patients," observed Dr. Dayton, professor and chairman of the department of surgery at State University of New York, Buffalo.
Dr. Zuckerbraun explained the rationale for his novel treatment: fulminant C. difficile colitis is a disease of bacterial overgrowth and toxin production in which the colon is usually viable and without necrosis or perforation, meaning that it’s recoverable.
On this basis, he developed a procedure that begins with exploratory laparoscopy or laparotomy. This is followed by creation of a diverting loop ileostomy through which 8 L of propylene glycol electrolyte solution (GoLYTELY) is instilled intraoperatively. Antegrade colonic flushes with 500 mg of vancomycin in 500 mL of diluent are administered every 8 hours for 10 days.
The working hypothesis is that this combination of diversion, propylene glycol lavage, and vancomycin acts in cumulative fashion to reduce C. difficile counts, deprive the pathogen of nutrients, and alter the intraluminal milieu, perhaps changing colonic oxygen tension. Also, there is preliminary evidence to suggest propylene glycol may exert a pharmacologic effect involving protection of the colonic epithelium.
The 42 patients in his series were quite sick, with a mean APACHE II score of 29.7. Many were immunosuppressed. Preoperatively, 90% were in the intensive care unit, where most were intubated and/or on vasopressors.
Loop ileostomy and colonic lavage were accomplished laparoscopically in 35 of 42 patients. With increased experience, Dr. Zuckerbraun and his colleagues have decided that the only indication for open loop ileostomy via laparotomy is abdominal compartment syndrome.
One patient with abdominal compartment syndrome underwent colectomy immediately after loop ileostomy. Two more patients had colectomies during the postoperative period based upon clinical symptoms.
Eight patients died a mean of 13 days after surgery. Of the 34 who survived the 30-day postoperative period, 6 have subsequently died because of comorbid disease – none of these deaths was related to C. difficile.
Twenty-eight patients remain alive at a mean follow-up of 11.4 months. Of the 19 who have been followed for at least 6 months, 15 (79%) have had their ileostomies reversed. Surgeons initially considered performing the reversal during the same hospital stay, but they decided patients with fulminant C. difficile colitis have too many serious comorbidities to be able to handle a second operation early on.
"Most have required months to recover from the illness that brought them into the hospital in the first place, which often wasn’t C. difficile. We wait until they’re back on their feet again," Dr. Zuckerbraun explained.
The indications for temporary loop ileostomy and colonic lavage are, first, diagnosis of C. difficile colitis by toxin assay, a compatible CT scan, or endoscopic findings, along with any one of the following criteria: sepsis, peritonitis, change in mental status, ventilatory failure, vasopressor requirement, worsening abdominal pain or distention, or unexplained clinical deterioration, he said.
At the urging of medical intensivists and transplant physicians, the investigators have also performed this operation in two patients with multiple recurrent episodes of C. difficile colitis who were not critically ill. One patient had 19 prior episodes. The C. difficile was successfully eradicated in both cases. The new procedure, however, was undertaken only after the patients failed a trial of high-volume propylene glycol lavage by nasogastric tube, which the investigators have previously employed successfully to eradicate C. difficile infections in several other patients with multiply recurrent nonfulminant colitis.
Severe, complicated C. difficile colitis occurs in 4%-10% of C. difficile-associated disease, which is now the most common nosocomial infection.
Dr. Zuckerbraun reported no conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION
Major Finding: In patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon.
Data Source: A series of 42 consecutive patients.
Disclosures: Dr. Zuckerbraun reported no conflicts of interest.
Novel Minimally Invasive Surgery Tames Fulminant C. difficile
BOCA RATON, FLA. – For patients with fulminant Clostridium difficile colitis, minimally invasive temporary loop ileostomy with colonic lavage may offer a novel life- and colon-saving alternative to colectomy.
In a series of 42 consecutive patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon, Dr. Brian Zuckerbraun reported at the annual meeting of the American Surgical Association.
This 19% mortality was impressively less than the 50% rate in 42 consecutive historical controls with similar Acute Physiology and Chronic Health Evaluation (APACHE) II scores who underwent subtotal colectomy at the same medical center just prior to introduction of the novel, less invasive operation. And the 50% mortality rate is on the low end of reported series, noted Dr. Zuckerbraun of the University of Pittsburgh.
"This approach may prove to be a better alternative to colectomy, because the colon is usually viable and can recover," he said. "Loop ileostomy and colonic lavage should be considered in all patients with severe complicated C. difficile colitis."
"Also, what we’re finding now because of our outcomes and the smaller insult of this therapy compared to colectomy is that our medical colleagues are willing to consult us earlier in the care of these patients. They’re not just thinking of surgery as a salvage operation when all else has failed," Dr. Zuckerbraun noted.
His presentation drew effusive audience praise.
"Two or three times a year I come across something that causes me to say, ‘I really wish I’d thought of that.’ This is one of those situations. I think this is a wonderful idea," said Dr. Robert G. Sawyer, a discussant.
Dr. Sawyer, professor of surgery and public health sciences and chief of acute care surgery at the University of Virginia, Charlottesville, was particularly impressed that the treatment enabled roughly 90% of patients to save their colon. "I believe this will become the standard technique in the treatment of severe C. difficile colitis in the future," he predicted.
Dr. Merril T. Dayton was equally impressed.
"We may be seeing a bit of history being made here: a new operation. If time bears out your study findings, this is a simpler and effective way to handle these complicated patients," observed Dr. Dayton, professor and chairman of the department of surgery at State University of New York, Buffalo.
Dr. Zuckerbraun explained the rationale for his novel treatment: fulminant C. difficile colitis is a disease of bacterial overgrowth and toxin production in which the colon is usually viable and without necrosis or perforation, meaning that it’s recoverable.
On this basis, he developed a procedure that begins with exploratory laparoscopy or laparotomy. This is followed by creation of a diverting loop ileostomy through which 8 L of propylene glycol electrolyte solution (GoLYTELY) is instilled intraoperatively. Antegrade colonic flushes with 500 mg of vancomycin in 500 mL of diluent are administered every 8 hours for 10 days.
The working hypothesis is that this combination of diversion, propylene glycol lavage, and vancomycin acts in cumulative fashion to reduce C. difficile counts, deprive the pathogen of nutrients, and alter the intraluminal milieu, perhaps changing colonic oxygen tension. Also, there is preliminary evidence to suggest propylene glycol may exert a pharmacologic effect involving protection of the colonic epithelium.
The 42 patients in his series were quite sick, with a mean APACHE II score of 29.7. Many were immunosuppressed. Preoperatively, 90% were in the intensive care unit, where most were intubated and/or on vasopressors.
Loop ileostomy and colonic lavage were accomplished laparoscopically in 35 of 42 patients. With increased experience, Dr. Zuckerbraun and his colleagues have decided that the only indication for open loop ileostomy via laparotomy is abdominal compartment syndrome.
One patient with abdominal compartment syndrome underwent colectomy immediately after loop ileostomy. Two more patients had colectomies during the postoperative period based upon clinical symptoms.
Eight patients died a mean of 13 days after surgery. Of the 34 who survived the 30-day postoperative period, 6 have subsequently died because of comorbid disease – none of these deaths was related to C. difficile.
Twenty-eight patients remain alive at a mean follow-up of 11.4 months. Of the 19 who have been followed for at least 6 months, 15 (79%) have had their ileostomies reversed. Surgeons initially considered performing the reversal during the same hospital stay, but they decided patients with fulminant C. difficile colitis have too many serious comorbidities to be able to handle a second operation early on.
"Most have required months to recover from the illness that brought them into the hospital in the first place, which often wasn’t C. difficile. We wait until they’re back on their feet again," Dr. Zuckerbraun explained.
The indications for temporary loop ileostomy and colonic lavage are, first, diagnosis of C. difficile colitis by toxin assay, a compatible CT scan, or endoscopic findings, along with any one of the following criteria: sepsis, peritonitis, change in mental status, ventilatory failure, vasopressor requirement, worsening abdominal pain or distention, or unexplained clinical deterioration, he said.
At the urging of medical intensivists and transplant physicians, the investigators have also performed this operation in two patients with multiple recurrent episodes of C. difficile colitis who were not critically ill. One patient had 19 prior episodes. The C. difficile was successfully eradicated in both cases. The new procedure, however, was undertaken only after the patients failed a trial of high-volume propylene glycol lavage by nasogastric tube, which the investigators have previously employed successfully to eradicate C. difficile infections in several other patients with multiply recurrent nonfulminant colitis.
Severe, complicated C. difficile colitis occurs in 4%-10% of C. difficile-associated disease, which is now the most common nosocomial infection.
Dr. Zuckerbraun reported no conflicts of interest.
BOCA RATON, FLA. – For patients with fulminant Clostridium difficile colitis, minimally invasive temporary loop ileostomy with colonic lavage may offer a novel life- and colon-saving alternative to colectomy.
In a series of 42 consecutive patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon, Dr. Brian Zuckerbraun reported at the annual meeting of the American Surgical Association.
This 19% mortality was impressively less than the 50% rate in 42 consecutive historical controls with similar Acute Physiology and Chronic Health Evaluation (APACHE) II scores who underwent subtotal colectomy at the same medical center just prior to introduction of the novel, less invasive operation. And the 50% mortality rate is on the low end of reported series, noted Dr. Zuckerbraun of the University of Pittsburgh.
"This approach may prove to be a better alternative to colectomy, because the colon is usually viable and can recover," he said. "Loop ileostomy and colonic lavage should be considered in all patients with severe complicated C. difficile colitis."
"Also, what we’re finding now because of our outcomes and the smaller insult of this therapy compared to colectomy is that our medical colleagues are willing to consult us earlier in the care of these patients. They’re not just thinking of surgery as a salvage operation when all else has failed," Dr. Zuckerbraun noted.
His presentation drew effusive audience praise.
"Two or three times a year I come across something that causes me to say, ‘I really wish I’d thought of that.’ This is one of those situations. I think this is a wonderful idea," said Dr. Robert G. Sawyer, a discussant.
Dr. Sawyer, professor of surgery and public health sciences and chief of acute care surgery at the University of Virginia, Charlottesville, was particularly impressed that the treatment enabled roughly 90% of patients to save their colon. "I believe this will become the standard technique in the treatment of severe C. difficile colitis in the future," he predicted.
Dr. Merril T. Dayton was equally impressed.
"We may be seeing a bit of history being made here: a new operation. If time bears out your study findings, this is a simpler and effective way to handle these complicated patients," observed Dr. Dayton, professor and chairman of the department of surgery at State University of New York, Buffalo.
Dr. Zuckerbraun explained the rationale for his novel treatment: fulminant C. difficile colitis is a disease of bacterial overgrowth and toxin production in which the colon is usually viable and without necrosis or perforation, meaning that it’s recoverable.
On this basis, he developed a procedure that begins with exploratory laparoscopy or laparotomy. This is followed by creation of a diverting loop ileostomy through which 8 L of propylene glycol electrolyte solution (GoLYTELY) is instilled intraoperatively. Antegrade colonic flushes with 500 mg of vancomycin in 500 mL of diluent are administered every 8 hours for 10 days.
The working hypothesis is that this combination of diversion, propylene glycol lavage, and vancomycin acts in cumulative fashion to reduce C. difficile counts, deprive the pathogen of nutrients, and alter the intraluminal milieu, perhaps changing colonic oxygen tension. Also, there is preliminary evidence to suggest propylene glycol may exert a pharmacologic effect involving protection of the colonic epithelium.
The 42 patients in his series were quite sick, with a mean APACHE II score of 29.7. Many were immunosuppressed. Preoperatively, 90% were in the intensive care unit, where most were intubated and/or on vasopressors.
Loop ileostomy and colonic lavage were accomplished laparoscopically in 35 of 42 patients. With increased experience, Dr. Zuckerbraun and his colleagues have decided that the only indication for open loop ileostomy via laparotomy is abdominal compartment syndrome.
One patient with abdominal compartment syndrome underwent colectomy immediately after loop ileostomy. Two more patients had colectomies during the postoperative period based upon clinical symptoms.
Eight patients died a mean of 13 days after surgery. Of the 34 who survived the 30-day postoperative period, 6 have subsequently died because of comorbid disease – none of these deaths was related to C. difficile.
Twenty-eight patients remain alive at a mean follow-up of 11.4 months. Of the 19 who have been followed for at least 6 months, 15 (79%) have had their ileostomies reversed. Surgeons initially considered performing the reversal during the same hospital stay, but they decided patients with fulminant C. difficile colitis have too many serious comorbidities to be able to handle a second operation early on.
"Most have required months to recover from the illness that brought them into the hospital in the first place, which often wasn’t C. difficile. We wait until they’re back on their feet again," Dr. Zuckerbraun explained.
The indications for temporary loop ileostomy and colonic lavage are, first, diagnosis of C. difficile colitis by toxin assay, a compatible CT scan, or endoscopic findings, along with any one of the following criteria: sepsis, peritonitis, change in mental status, ventilatory failure, vasopressor requirement, worsening abdominal pain or distention, or unexplained clinical deterioration, he said.
At the urging of medical intensivists and transplant physicians, the investigators have also performed this operation in two patients with multiple recurrent episodes of C. difficile colitis who were not critically ill. One patient had 19 prior episodes. The C. difficile was successfully eradicated in both cases. The new procedure, however, was undertaken only after the patients failed a trial of high-volume propylene glycol lavage by nasogastric tube, which the investigators have previously employed successfully to eradicate C. difficile infections in several other patients with multiply recurrent nonfulminant colitis.
Severe, complicated C. difficile colitis occurs in 4%-10% of C. difficile-associated disease, which is now the most common nosocomial infection.
Dr. Zuckerbraun reported no conflicts of interest.
BOCA RATON, FLA. – For patients with fulminant Clostridium difficile colitis, minimally invasive temporary loop ileostomy with colonic lavage may offer a novel life- and colon-saving alternative to colectomy.
In a series of 42 consecutive patients with severe complicated C. difficile colitis who underwent the surgery, 30-day mortality was only 19% and 39 patients (93%) preserved their colon, Dr. Brian Zuckerbraun reported at the annual meeting of the American Surgical Association.
This 19% mortality was impressively less than the 50% rate in 42 consecutive historical controls with similar Acute Physiology and Chronic Health Evaluation (APACHE) II scores who underwent subtotal colectomy at the same medical center just prior to introduction of the novel, less invasive operation. And the 50% mortality rate is on the low end of reported series, noted Dr. Zuckerbraun of the University of Pittsburgh.
"This approach may prove to be a better alternative to colectomy, because the colon is usually viable and can recover," he said. "Loop ileostomy and colonic lavage should be considered in all patients with severe complicated C. difficile colitis."
"Also, what we’re finding now because of our outcomes and the smaller insult of this therapy compared to colectomy is that our medical colleagues are willing to consult us earlier in the care of these patients. They’re not just thinking of surgery as a salvage operation when all else has failed," Dr. Zuckerbraun noted.
His presentation drew effusive audience praise.
"Two or three times a year I come across something that causes me to say, ‘I really wish I’d thought of that.’ This is one of those situations. I think this is a wonderful idea," said Dr. Robert G. Sawyer, a discussant.
Dr. Sawyer, professor of surgery and public health sciences and chief of acute care surgery at the University of Virginia, Charlottesville, was particularly impressed that the treatment enabled roughly 90% of patients to save their colon. "I believe this will become the standard technique in the treatment of severe C. difficile colitis in the future," he predicted.
Dr. Merril T. Dayton was equally impressed.
"We may be seeing a bit of history being made here: a new operation. If time bears out your study findings, this is a simpler and effective way to handle these complicated patients," observed Dr. Dayton, professor and chairman of the department of surgery at State University of New York, Buffalo.
Dr. Zuckerbraun explained the rationale for his novel treatment: fulminant C. difficile colitis is a disease of bacterial overgrowth and toxin production in which the colon is usually viable and without necrosis or perforation, meaning that it’s recoverable.
On this basis, he developed a procedure that begins with exploratory laparoscopy or laparotomy. This is followed by creation of a diverting loop ileostomy through which 8 L of propylene glycol electrolyte solution (GoLYTELY) is instilled intraoperatively. Antegrade colonic flushes with 500 mg of vancomycin in 500 mL of diluent are administered every 8 hours for 10 days.
The working hypothesis is that this combination of diversion, propylene glycol lavage, and vancomycin acts in cumulative fashion to reduce C. difficile counts, deprive the pathogen of nutrients, and alter the intraluminal milieu, perhaps changing colonic oxygen tension. Also, there is preliminary evidence to suggest propylene glycol may exert a pharmacologic effect involving protection of the colonic epithelium.
The 42 patients in his series were quite sick, with a mean APACHE II score of 29.7. Many were immunosuppressed. Preoperatively, 90% were in the intensive care unit, where most were intubated and/or on vasopressors.
Loop ileostomy and colonic lavage were accomplished laparoscopically in 35 of 42 patients. With increased experience, Dr. Zuckerbraun and his colleagues have decided that the only indication for open loop ileostomy via laparotomy is abdominal compartment syndrome.
One patient with abdominal compartment syndrome underwent colectomy immediately after loop ileostomy. Two more patients had colectomies during the postoperative period based upon clinical symptoms.
Eight patients died a mean of 13 days after surgery. Of the 34 who survived the 30-day postoperative period, 6 have subsequently died because of comorbid disease – none of these deaths was related to C. difficile.
Twenty-eight patients remain alive at a mean follow-up of 11.4 months. Of the 19 who have been followed for at least 6 months, 15 (79%) have had their ileostomies reversed. Surgeons initially considered performing the reversal during the same hospital stay, but they decided patients with fulminant C. difficile colitis have too many serious comorbidities to be able to handle a second operation early on.
"Most have required months to recover from the illness that brought them into the hospital in the first place, which often wasn’t C. difficile. We wait until they’re back on their feet again," Dr. Zuckerbraun explained.
The indications for temporary loop ileostomy and colonic lavage are, first, diagnosis of C. difficile colitis by toxin assay, a compatible CT scan, or endoscopic findings, along with any one of the following criteria: sepsis, peritonitis, change in mental status, ventilatory failure, vasopressor requirement, worsening abdominal pain or distention, or unexplained clinical deterioration, he said.
At the urging of medical intensivists and transplant physicians, the investigators have also performed this operation in two patients with multiple recurrent episodes of C. difficile colitis who were not critically ill. One patient had 19 prior episodes. The C. difficile was successfully eradicated in both cases. The new procedure, however, was undertaken only after the patients failed a trial of high-volume propylene glycol lavage by nasogastric tube, which the investigators have previously employed successfully to eradicate C. difficile infections in several other patients with multiply recurrent nonfulminant colitis.
Severe, complicated C. difficile colitis occurs in 4%-10% of C. difficile-associated disease, which is now the most common nosocomial infection.
Dr. Zuckerbraun reported no conflicts of interest.
FROM THE ANNUAL MEETING OF THE AMERICAN SURGICAL ASSOCIATION